Abstract
Background
The treatment of recurrent dislocation after total hip arthroplasty remains challenging. Dual mobility sockets have been associated with a low rate of dislocation but it is not known whether they are useful for treating recurrent dislocation.
Questions/purposes
We therefore asked whether a cemented dual mobility socket would (1) restore hip stability following recurrent dislocation; (2) provide a pain-free and mobile hip; and (3) show durable radiographic fixation.
Methods
We retrospectively reviewed 51 patients treated with a cemented dual mobility socket for recurrent dislocation after total hip arthroplasty between August 2002 and June 2005. The mean age at the time of the index procedure of was 71.3 years. Of the 51 patients, 47 have had complete clinical and radiographic evaluation data at a mean followup of 51.4 months (range, 25–76.3 months).
Results
The cemented dual mobility socket restored complete stability of the hip in 45 of the 47 patients (96%). The mean Merle d’Aubigné hip score was 16 ± 2 at the latest followup. Radiographic analysis revealed no or radiolucent lines less than 1 mm thick located in a single acetabular zone in 43 of 47 hips (91.5%). The cumulative survival rate of the acetabular component at 72 months using revision for dislocation and/or mechanical failure as the end point was 96% ± 4% (95% confidence interval, 90%–100%).
Conclusions
A cemented dual mobility socket was able to restore hip stability in 96% of recurrent dislocating hips. However, longer-term followup is needed to ensure that dislocation and loosening rates will not increase.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
THA is associated with high levels of function, relatively low complication rates, and high survival. However, despite surgical technique and implant design improvements, dislocation continues to be a matter of concern with an incidence of around 3% [6, 42] and with important functional and financial consequences [9, 43]. Among the patients presenting with an episode of dislocation, approximately one-third may experience recurrence after nonoperative treatment [48]. The outcomes of reoperation for recurrent dislocation have been variable with approximately one-third of patients experiencing redislocation despite a number of proposed methods of surgical treatment [6, 11].
Perhaps the most common option for treating recurrent dislocation in the United States is revision with a constrained acetabular component [46]. Two basic designs of constrained components are available: the locking ring system and the constrained tripolar device. Tripolar constrained devices reportedly provide 90% survival at 10-year followup with revision for redislocation or mechanical failure of the constraining mechanism as the end point [16]. However, other reports show lower rates of reducing recurrent dislocation even in the short-term, pointing out specific mechanisms of failure at each interface [10, 13, 20] and rates of actual or potential loosening of 12% after less than 3-year followup [26, 45, 49]. Another concept introduced in the late 1970s by Bousquet [7] to deal with these complex situations is an unconstrained tripolar device, a so-called dual mobility socket. Since this early period, a number of cemented and cementless designs have emerged in Europe, and some have been recently Food and Drug Administration-approved. Several studies have assessed the outcome of such devices in the prevention of dislocation in both primary and revision THAs [3, 14, 22, 28, 29, 37–40] and reported very low dislocation rates. Only two studies have assessed a dual mobility socket in the treatment of recurrent dislocation [21, 30]. These studies that concerned mainly a cementless design showed residual hip instability in 0 and 3.7%, respectively.
We therefore asked whether a cemented dual mobility socket would (1) restore hip stability following recurrent dislocation; (2) provide a pain-free and mobile hip; and (3) show durable radiographic fixation.
Patients and Methods
After a minimum 2-year followup, we retrospectively reviewed 51 patients (51 hips) presenting with recurrent dislocation after primary or revision THA and treated with a cemented dual mobility socket between August 2002 and June 2005 at four tertiary centers. All patients gave informed consent for participation in the study. During this time we treated five patients with recurrent dislocation using other approaches. The indications for use of the dual mobility socket were patients (1) in whom no identifiable cause for dislocation could be identified or corrected; (2) in whom education and a spica cast or surgical attempts at stabilization failed; and (3) with a marked deficiency of the hip abductors. All patients were evaluated preoperatively and returned for followup visit at 6 weeks, 3 months, 6 months, 1 year, and annually thereafter. Of the 51 patients, two died before the minimal 2-year followup. One patient living in a foreign country was evaluated by his local physician, but we could not obtain his followup radiograph. One patient was lost to followup. The remaining 47 patients have had complete adequate clinical and radiographic evaluation at a minimum of 2-year followup with a mean followup of 51.4 ± 1.4 months (range, 25–76.3 months).
There were 39 females and 12 males with a mean age at the time of the index procedure of 71.4 ± 11.5 years (range, 41.1–91.8 years). The mean body mass index was 26.4 ± 6.5 kg/m2 (range, 17.6–36.6 kg/m2). The mean number of dislocation was 3.3 ± 1.4 (median, 4; range, 2–9). All patients had been initially treated nonoperatively, including education and a spica-type cast for a minimum of 6 weeks. Three patients had additionally been treated with trochanteric advancement and five with liner augmentation. The initial diagnosis was primary osteoarthritis in 35 hips, congenital hip dysplasia in five hips, inflammatory arthritis in three hips, posttraumatic osteoarthritis in three hips, femoral neck fracture in three hips, and osteonecrosis of the femoral head in two hips. An average 2.0 ± 1.3 (range, 1–6) previous surgical procedures had been performed on these 51 hips. The dislocating hip was a primary arthroplasty in five patients, a first revision in 20, a second revision in 13, a third revision in seven, a fourth revision in five, and a fifth revision in one. Four hips had been previous infected although at the time of the index surgery the infections were controlled. Eleven hips had a Kerboull acetabular reinforcement device [25] that was used in conjunction with allograft in eight hips. The acetabular and the femoral components were loosened in six and four hips, respectively.
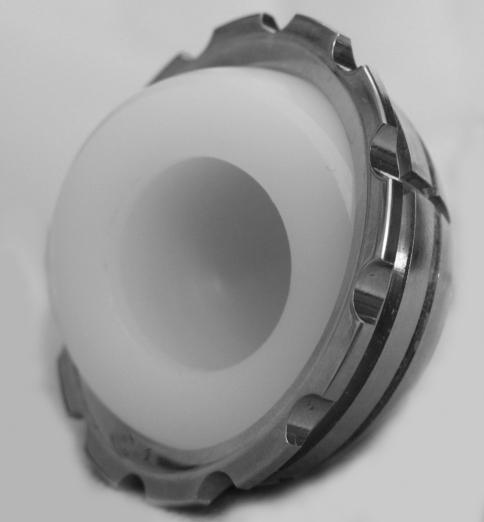
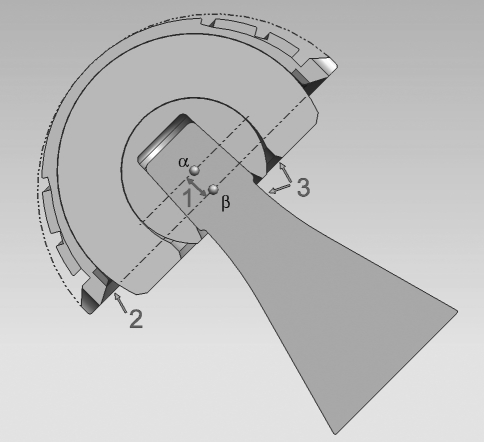
The Medial Cup® (Aston Medical, Saint Etienne, France) cemented dual mobility socket was used in all hips. This device (Fig. 1) consists of a spherocylindrical M30NW stainless steel outer shell with a peripheral rim and concentric grooves for cement fixation with a highly polished inner surface. This shell articulates with a compression-molded GUR 1050 ultrahigh-molecular-weight polyethylene mobile component sterilized with 2.5 Mrad of gamma radiation in a vacuum atmosphere. The opening diameter of the all-polyethylene mobile component is 6% smaller than that of the femoral head, and its minimal thickness ranges from 6.3 mm to 13 mm for 46 and 62 mm outer diameter shells, respectively. The femoral head is captured in the polyethylene component using a snap-fit-type mechanism, the latter acting as a large unconstrained head inside the metal cup. This principle creates two articulations: an inner bearing between the femoral head and the insert and an outer bearing between the insert and the shell. The thickness of the metal shell is 1.7 mm at the apex and 3.4 to 4.2 mm at the equator. This medializes the center of rotation of the polyethylene insert approximately 5 mm when compared with the center of rotation of the metal shell, increasing the stability of the device (Fig. 2). No locking ring or other means of constraint was associated. This device is available for use with either a 22.2- or 28 mm-diameter femoral head. In the current series, only a 22.2-mm femoral head were used, and the mean size of the shell was 51.2 ± 4.2 mm (range, 46–60 mm).
Fig. 1.
Photograph of the Medial Cup® tripolar unconstrained acetabular component (Aston Medical) consisting of, from inside out, a spherical mobile polyethylene insert that accepts a 22.2- or 28-mm femoral head and is not constrained into a spherocylindrical metal shell.
Fig. 2.
Diagram of the Medial cup® design indicating the medialization (1) of the center of rotation of the polyethylene insert (α) when compared with the center of rotation of the metal shell (β), the spherocylindrical design of the metal shell decreasing stresses at the periphery of the shell (2) and the good congruity between the femoral neck and the polyethylene rim (3).
The operative approach for the index operation was transtrochanteric (standard, modified, or extended) in 31 hips, posterolateral in 17 hips, and lateral without a trochanteric osteotomy in the remaining three hips. The femoral component was revised in 20 hips, and only the femoral head was exchanged in two hips. Femoral component revision was associated with femoral bone stock reconstruction in three hips, using proximal femoral allograft in two hips, and morselized bone grafting in one hip. The 16 well-fixed cemented femoral components were revised for ease of the acetabular revision. In these hips, a cement-in-cement procedure was performed on the femoral side. On the acetabular side, the socket was systematically removed, and fibrous tissue was completely excised. Bone loss then was assessed and when judged necessary by the operating surgeon, bony reconstruction was performed using a Kerboull acetabular reinforcement device in 22 hips in association with allograft in 13 hips, hydroxyapatite in one hip, autograft in one hip, and cement in the remaining seven hips. Moreover, in an additional hip, allograft was used without a reinforcement device to treat a cavitary defect. The cavity then was washed using pulsatile lavage and dried, and the shell was cemented with CMW Type 3 bone cement loaded with gentamycin (DePuy 3; DePuy, Exeter, Devon, UK) that was mixed in air and hand-packed. The mobile all-polyethylene component was snapped on the femoral head using a specifically designed power press and placed into the metal shell.
Postoperatively, patients received systemic antibiotics for 48 hours, nonsteroidal anti-inflammatory drugs (ketoprofen; 100 mg/day) for 5 days to prevent heterotopic ossification, and anticoagulation therapy (enoxaparin; 40 mg/day) for 5 weeks. Immediately after the operation, passive motion exercises of the involved joint were begun with the assistance of a therapist and were continued until active motion of the hip was possible. The patients were free to walk with two supports after 3 days. Full weightbearing was allowed after 6 weeks for patients operated on through a transtrochanteric approach, and allowed immediately as tolerated in the remaining patients. No specific measures were undertaken to prevent redisolocation, including restrictions to mobility, use of an abduction brace, or a hip spica cast.
Hip functional results were rated according to the Merle d’Aubigné [35] grading system by independent observers (DJB, DH, NB). Instability of the hip was defined as a dislocation or a subluxation. Subluxation was defined as perception by the patient of an abnormal hip movement accompanied by an audible thud or clunk of the hip often associated with pain.
Serial anteroposterior radiographs of the pelvis were analyzed by three independent observers (DJB, DH, NB). The inclination angle of the cup and the presence and progression of radiolucent lines according to the zones described by De Lee and Charnley [12] were evaluated on the pelvic side. Loosening of the socket was defined as cup migration exceeding 3 mm, angular rotation exceeding 3°, or a continuous radiolucent line wider than 2 mm (reflecting the observer’s confidence in his ability to detect radiolucent lines on plain radiographs). Parameters investigated on the femoral side included progression of radiolucent lines according to the seven zones described by Gruen et al. [18] and subsidence of the stem. Loosening of the stem was defined according to the criteria of Barrack et al. [4]. Definite, probable, and potential evidence of loosening were considered in this study. Periprosthetic cystic or scalloped lesions exceeding 2 mm in diameter that had not been noted on the immediate postoperative radiograph were defined as osteolysis (we are unaware of studies of interobserver variability to make this assessment).
We performed a survivorship analysis according to the actuarial method on the entire cohort using revision for redislocation and/or mechanical failure of the acetabular component and redislocation at the time of followup as the end points. The survival curve was derived from the cumulative survival rate over time as calculated from the actuarial life table [33]. We calculated the SE, given as a percentage, and the 95% confidence intervals from the data in the life table [36]. Comparison of preoperative and last followup clinical parameters was performed using the Wilcoxon rank test. We performed analyses with StatView statistical software (Version 5.0; SAS Institute, Cary, NC).
Results
The cemented dual mobility socket restored stability of the hip in 45 of the 47 patients (95.7%). Two patients (4.3%) had further episodes of posterior dislocation. These occurred between the polyethylene insert and the metal shell in one hip, whereas the other occurred between the femoral head and the mobile polyethylene insert 32 and 72 months after the index arthroplasty, respectively. The dislocation that occurred between the mobile insert and the shell was related to a technical error with a highly abducted socket. The intraprosthetic dislocation occurred in an active patient and was due to wear and fatigue deformation of the capturing area. Both hips underwent revision to a new dual mobility socket. With redislocation as the end point, the cumulative survival rate at 36 months was 97.8% ± 3.8% (95% confidence interval, 93.7%–100%).
The mean Merle d’Aubigné functional hip score increased from 13.4 ± 4.1 (median, 14; range, 8–18) preoperatively to 15.8 ± 2.2 (median, 16; range, 9–18) points at the time of the last followup (p = 0.0003). Twenty patients had no pain in the involved joint, fifteen patients had moderate pain that did not restrict their activity level, and twelve patients had pain that limited the duration for which they were able to walk to less than thirty minutes. The range of flexion was greater than 90° in 43 hips and 75° to 85° in four hips. At the latest followup, the mean range of flexion of the series was 101.7° ± 12.6° (median, 100°; range, 70°–130°).
The mean abduction angle of the socket was 47° ± 8° (median, 45°; range 31°–63°). Of the 47 acetabular components, 35 (75%) had no radiolucent line; four (9%) had a radiolucent line in Zone I, three (6%) in Zone III, and four (9%) in Zones I and III (Fig. 3). In all these hips, the radiolucent lines were less than 1 mm in thickness and were nonprogressive. One hip (2%) had a complete and progressive radiolucent line thicker than 2 mm associated with a migrated acetabular component. This patient had a revision procedure pending at the time of the last followup. On the femoral side, no component was loose or had been revised during the followup period. None of the 47 hips had a lytic lesion (cystic or scalloped) on either the femoral or the acetabular side. With revision for redislocation and/or mechanical failure of the acetabular component as the end point, the cumulative survival rate at 72 months was 95.7% ± 4.6% (95% confidence interval, 90.0%–100%).
Fig. 3A–D.
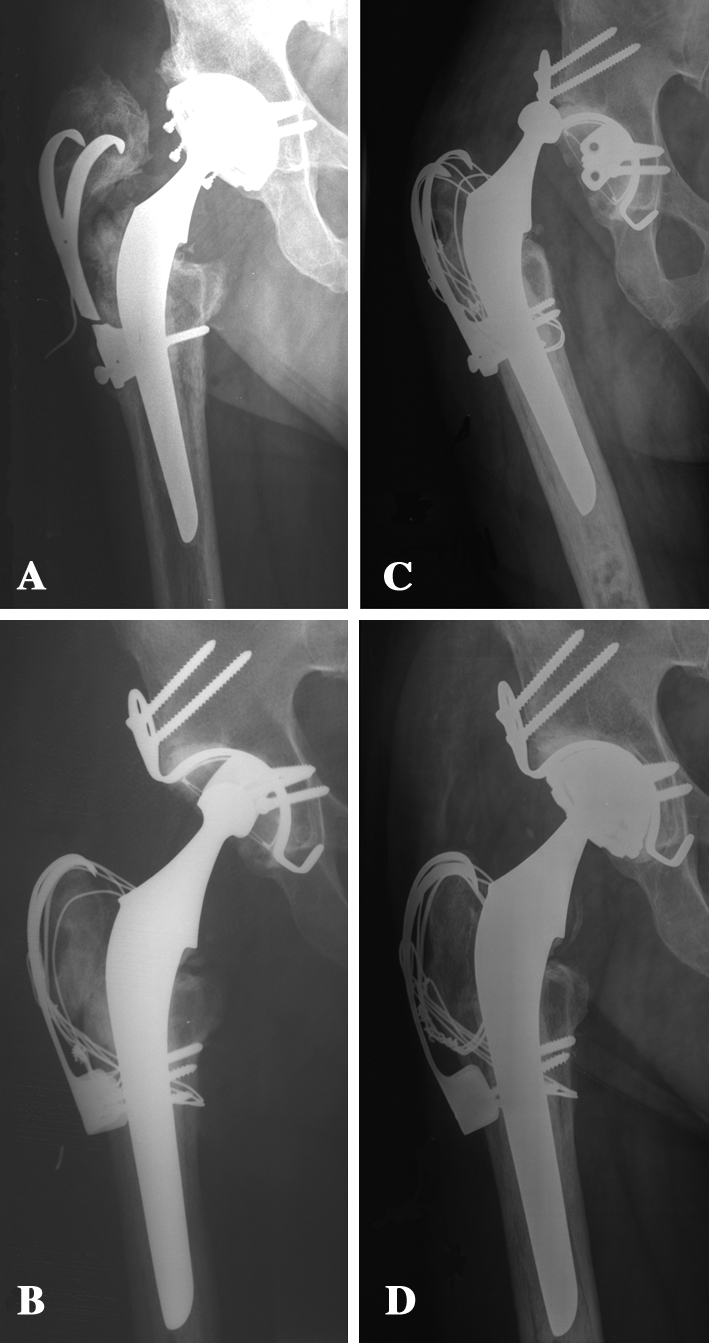
A 66-year-old man presented with recurrent dislocation after revision THA of the right hip. (A) The patient had a THA for posttraumatic osteoarthritis 15 years after a posterior column acetabular fracture that was operated on. He experienced recurrent dislocations that were unsuccessfully treated with trochanteric advancement and augmentation of the acetabular liner. (B) A third revision was performed using a Kerboull acetabular reinforcement device with allograft and trochanteric advancement fixed with wires and a claw plate. (C) Although trochanteric consolidation was obtained, and no component malposition was noted, the patient continued to experience dislocation. (D) The patient underwent revision to a cemented tripolar unconstrained acetabular component. He described episodes of transient instability during stair climbing but is otherwise not limited in his daily activities. Fifty-one months postoperatively, the radiograph shows no radiolucent line and no sign of loosening or impingement.
Discussion
To date, the most widely used surgical option for recurrent instability after THA in the absence of a correctable identified cause is likely the constrained acetabular components [6, 46]. However, this type of device has a complex design involving a number of parts, and several specific failure modes have been described in the literature [5, 10, 12, 15, 20, 24, 32, 34, 47]. The concept of dual mobility introduced in France over 30 years ago combines a low friction inner bearing and an ultralarge effective femoral head. This concept proved effective in the prevention of dislocation following primary and revision THA, even in patients at risk for dislocation [3, 14, 22, 28, 29, 37–40]. However, dual mobility in the treatment of hip instability has been reported only twice in the literature [21, 30]. Both studies used mostly a cementless design which fixation can be changeling in revision surgery. Our aim was to evaluate the ability of a cemented dual mobility socket to restore stability to the recurrently unstable THA, grant a pain-free and mobile hip, and provide durable radiographic fixation.
There are several limitations of our study. First, owing to the retrospective design the group of patients was heterogeneous as it included isolated acetabular revision (with and without bone deficiency) and revision of both components. However, this limitation is inherent to all revision series for recurrent dislocation due to the multifactorial causes that contribute to THA instability. Second, ours is a relatively short-term followup study. The time is adequate for identifying most patients with recurrent dislocation after the procedure, but not to determine long-term survival. However, with similar followup, other designs have proved unsatisfactory in terms of redislocation prevention [2] or worrisome in terms of actual or potential mechanical failures, including constraint mechanism breakage or radiographic loosening [26, 45].
We found a dual mobility socket provided complete restoration of hip stability in 45 of the 47 hips (96%). These results are comparable to those obtained with tripolar constrained components, and appear far better when compared with bipolar constrained components at similar followup (Table 1). Our results are in accordance with those of Guyen et al. [21] who reported on a series of 54 patients with unstable THA treated with a current design of dual mobility socket (cementless in 43 hips). Of the 54 patients, one patient had a single episode of dislocation at the metal-polyethylene insert interface, and two required revision because of dislocation at the inner bearing. Dislocation of the femoral head from the mobile polyethylene component inside the metal shell (so-called intraprosthetic dislocation) represents a specific complication of dual mobility socket [31]. This phenomenon can occur through impingement of the femoral neck or varus tilting of the mobile component leading to rim fatigue damage and wear of the capturing area of the polyethylene insert [1]. To reduce the consequences of the femoral neck to mobile insert impingement (so-called third articulation), it is recommended to use a highly polished surface and thin femoral neck below the Morse taper, and a high head to neck ratio. Also, the use of skirted heads should be avoided. In addition, various design factors of the dual mobility socket can play a role in the occurrence of intraprosthetic dislocation including thickness of the polyethylene at the capturing area, shape of the rim of the metal shell and eccentric rotation center of the metal shell and mobile insert. In the current study, a medialized dual mobility socket has been used to avoid varus tilting of the mobile polyethylene component, this design resulting in a counterbalancing valgus moment as been demonstrated in vitro with a bipolar prosthesis [27]. We are not aware of any study evaluating the advantage of one design over another in clinical practice.
Table 1.
Main published results of constrained acetabular components and dual mobility in the treatment of recurrent dislocation
| Authors | Number of hips | Mean followup (months) | Repeat dislocation (%) | Radiographic loosening |
|---|---|---|---|---|
| Bipolar constrained | ||||
| Anderson et al. [2] | 18 | 31 | 29 | 0% |
| Berend et al. [5] | 138 | 128 | 28.9 | NA |
| Tripolar constrained | ||||
| Goetz et al. [16] | 56 | 122 | 7% | 4% |
| Goetz et al. [17] | 56 | 64 | 4% | NA |
| Khan et al. [26] | 34 | 32 | 3% | 11.8 |
| Shapiro et al. [44] | 87 | 58 | 2.8 | 8.2 |
| Shrader et a. [45] | 110 | 35 | 1.8% | 14% |
| Dual mobility | ||||
| Guyen et al. [21] | 54 | 48 | 3.7% | 0% |
| Leclercq et al. [30] | 13 | 4 | 0% | NA |
| Hamadouche et al. [current study] | 51 | 51 | 4% | 2% |
NA = not available.
Only 35 of our 47 patients had no to moderate pain at the latest followup, reflecting the complexity of this population that had multiple operations about the hip. The mean range of flexion of the current series of 101° is in accordance with the in vitro results obtained by Guyen et al. [19] and higher than the results obtained with constrained acetabular component [26].
Radiographic analysis revealed no or radiolucent lines less than 1 mm thick located in a single acetabular zone in 43 of 47 hips (91.5%), and one socket that was considered loosened with a complete and progressive radiolucent line. Although cemented metal sockets have provided high loosening rates in some reports [8, 23, 41], we did not observe this complication. This might be related to the fact that with a dual mobility device, most of the motion occurs within the inner bearing [1], avoiding overstressing the cement-metal and the bone-cement interfaces. These results appear better when compared to recent studies providing detailed radiographic analysis of constrained acetabular components at less than 3-year followup (Table 1).
The use of a cemented dual mobility socket has provided restoration of hip stability in 96% of patients presenting with recurrent dislocation, with less mechanical complication and loosening rates than have been reported with constrained systems. However, longer-term followup is needed to ensure dislocation and loosening rates will not increase. We believe this device should be limited to the prevention of dislocation in high risk patients and to the treatment of THA instability with abductor mechanism disruption, or in patients in whom no identifiable cause for dislocation could be identified or corrected.
Acknowledgments
We dedicate this paper to the memory of Frantz Langlais, MD. We thank O. Chaix, MD, and Jean Pierre Courpied, MD, for contributing patients and Nicolas Barba, MD, for help in gathering data.
Footnotes
One or more of the authors (TM, FG) has received funding (royalties) from Aston Medical. MH is a nonpaid consultant for Aston-Medical.
Each author certifies that his or her institution has approved or waived approval for the human protocol of this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at The Clinical Orthopaedic Research Centre, Department of Reconstructive and Orthopaedic Surgery, Université René Descartes, Hôpital Cochin (AP-HP), Paris France; the Department of Orthopaedic Surgery and Traumatology, University Hospital, Rennes, France; The Clinique du Ter, Ploemeur, France; and The Centre Hospitalier de Pont l’Abbé, France.
References
- 1.Adam P, Farizon F, Fessy MH. Dual articulation retentive acetabular liners and wear: surface analysis of 40 retrieved polyethylene implants [in French] Rev Chir Orthop. 2005;91:627–636. doi: 10.1016/s0035-1040(05)84466-6. [DOI] [PubMed] [Google Scholar]
- 2.Anderson MJ, Murray WR, Skinner HB. Constrained acetabular components. J Arthroplasty. 1994;9:17–23. doi: 10.1016/0883-5403(94)90133-3. [DOI] [PubMed] [Google Scholar]
- 3.Aubriot J, Lesimple P, Leclercq S. Study of Bousquet’s non-cemented acetabular implant in 100 hybrid total hip prostheses (Charnley type cemented femoral component). Average 5-year follow-up [in French] Acta Orthop Belg. 1993;59((Suppl 1)):267–271. [PubMed] [Google Scholar]
- 4.Barrack RL, Mulroy RD, Harris WH. Improved cementing techniques and femoral component loosening in young patients with hip arthroplasty. A 12-year radiographic review. J Bone Joint Surg Br. 1992;74:385–389. doi: 10.1302/0301-620X.74B3.1587883. [DOI] [PubMed] [Google Scholar]
- 5.Berend KR, Lombardi AV, Mallory TH, Adams JB, Russell JH, Groseth KL. The long-term outcome of 755 consecutive constrained acetabular components in total hip arthroplasty examining the successes and failures. J Arthroplasty. 2005;20(Suppl 3):93–102. doi: 10.1016/j.arth.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 6.Berry DJ. Unstable total hip arthroplasty: detailed overview. Instr Course Lect. 2001;50:265–274. [PubMed] [Google Scholar]
- 7.Bousquet G, Gazielly DF, Giradin P, Debiesse JL, Relave M, Israeli A. The ceramic coated cementless total hip arthroplasty. Basic concepts and surgical technique. J Orthop Surg Tech. 1985;1:15–28. [Google Scholar]
- 8.Cates HE, Faris PM, Keating EM, Ritter MA. Polyethylene wear in cemented metal-backed acetabular cups. J Bone Joint Surg Br. 1993;75:249–253. doi: 10.1302/0301-620X.75B2.8444945. [DOI] [PubMed] [Google Scholar]
- 9.Chandler RW, Dorr LD, Perry J. The functional cost of dislocation following total hip arthroplasty. Clin Orthop Relat Res. 1982;168:168–172. [PubMed] [Google Scholar]
- 10.Cooke CC, Hozack W, Lavernia C, Sharkey P, Shastri S, Rothman RH. Early failure mechanisms of constrained tripolar acetabular sockets used in revision total hip arthroplasty. J Arthroplasty. 2003;18:827–833. doi: 10.1016/S0883-5403(03)00325-5. [DOI] [PubMed] [Google Scholar]
- 11.Daly PJ, Morrey BF. Operative correction of an unstable total hip arthroplasty. J Bone Joint Surg Am. 1992;74:1334–1343. [PubMed] [Google Scholar]
- 12.Lee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 13.Della Valle CJ, Chang D, Sporer S, Berger RA, Rosenberg AG, Paprosky WG. High failure rate of a constrained acetabular liner in revision total hip arthroplasty. J Arthroplasty. 2005;20(Suppl 3):103–107. doi: 10.1016/j.arth.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 14.Farizon F, de LR, Azoulai JJ, Bousquet G. Results with a cementless alumina-coated cup with dual mobility. A twelve-year follow-up study. Int Orthop. 1998;22:219–224. doi: 10.1007/s002640050246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fisher DA, Kiley K. Constrained acetabular cup disassembly. J Arthroplasty. 1994;9:325–329. doi: 10.1016/0883-5403(94)90088-4. [DOI] [PubMed] [Google Scholar]
- 16.Goetz DD, Bremner BR, Callaghan JJ, Capello WN, Johnston RC. Salvage of a recurrently dislocating total hip prosthesis with use of a constrained acetabular component. A concise follow-up of a previous report. J Bone Joint Surg Am. 2004;86:2419–2423. doi: 10.2106/00004623-200411000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Goetz DD, Capello WN, Callaghan JJ, Brown TD, Johnston RC. Salvage of a recurrently dislocating total hip prosthesis with use of a constrained acetabular component. A retrospective analysis of fifty-six cases. J Bone Joint Surg Am. 1998;80:502–509. doi: 10.2106/00004623-199804000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Gruen TA, McNeice GM, Amstutz HC. ‘Modes of failure’ of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 19.Guyen O, Chen QS, Bejui-Hugues J, Berry DJ, An KN. Unconstrained tripolar hip implants: effect on hip stability. Clin Orthop Relat Res. 2007;455:202–208. doi: 10.1097/01.blo.0000238796.59596.1f. [DOI] [PubMed] [Google Scholar]
- 20.Guyen O, Lewallen DG, Cabanela ME. Modes of failure of Osteonics constrained tripolar implants: a retrospective analysis of forty-three failed implants. J Bone Joint Surg Am. 2008;90:1553–1560. doi: 10.2106/JBJS.G.00317. [DOI] [PubMed] [Google Scholar]
- 21.Guyen O, Pibarot V, Vaz G, Chevillotte C, Bejui-Hugues J. Use of a dual mobility socket to manage total hip arthroplasty instability. Clin Orthop Relat Res. 2009;467:465–472. doi: 10.1007/s11999-008-0476-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Guyen O, Pibarot V, Vaz G, Chevillotte C, Carret JP, Bejui-Hugues J. Unconstrained tripolar implants for primary total hip arthroplasty in patients at risk for dislocation. J Arthroplast. 2007;22:849–58. [DOI] [PubMed]
- 23.Harris WH, Penenberg BL. Further follow-up on socket fixation using a metal-backed acetabular component for total hip replacement. A minimum ten-year follow-up study. J Bone Joint Surg Am. 1987;69:1140–1143. [PubMed] [Google Scholar]
- 24.Kaper BP, Bernini PM. Failure of a constrained acetabular prosthesis of a total hip arthroplasty. A report of four cases. J Bone Joint Surg Am. 1998;80:561–565. doi: 10.2106/00004623-199804000-00013. [DOI] [PubMed] [Google Scholar]
- 25.Kerboull M, Hamadouche M, Kerboull L. The Kerboull acetabular reinforcement device in major acetabular reconstructions. Clin Orthop Relat Res. 2000;378:155–168. doi: 10.1097/00003086-200009000-00025. [DOI] [PubMed] [Google Scholar]
- 26.Khan RJ, Fick D, Alakeson R, Haebich S, Cruz M, Nivbrant B, Wood D. A constrained acetabular component for recurrent dislocation. J Bone Joint Surg Br. 2006;88:870–876. doi: 10.1302/0301-620X.88B7.17644. [DOI] [PubMed] [Google Scholar]
- 27.Krein SW, Chao EY. Biomechanics of bipolar hip endoprostheses. J Orthop Res. 1984;4:356–368. doi: 10.1002/jor.1100020408. [DOI] [PubMed] [Google Scholar]
- 28.Langlais F, Ropars M, Gaucher F, Musset T, Chaix O. Dual mobility cemented cups have low dislocation rates in THA revisions. Clin Orthop Relat Res. 2008;466:389–395. doi: 10.1007/s11999-007-0047-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lautridou C, Lebel B, Burdin G, Vielpeau C. Survival of the cementless Bousquet dual mobility cup: Minimum 15-year follow-up of 437 total hip arthroplasties [in French] Rev Chir Orthop Reparatrice Appar Mot. 2008;94:731–739. doi: 10.1016/j.rco.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 30.Leclercq S, El Bidi S, Aubriot JH. Bousquet’s device in the treatment of recurrent dislocation of a total hip prosthesis. Apropos of 13 cases [in French] Rev Chir Orthop Reparatrice Appar Mot. 1995;81:389–394. [PubMed] [Google Scholar]
- 31.Lecuire F, Benareau I, Rubini J, Basso M. [Intra-prosthetic dislocation of the Bousquet dual mobility socket] [in French].Rev Chir Orthop Reparatrice Appar Mot. 2004;90:249–255. [DOI] [PubMed]
- 32.Lombardi AV, Mallory TH, Kraus TJ, Vaughn BK. Preliminary report on the S-ROM constraining acetabular insert: a retrospective clinical experience. Orthopedics. 1991;14:297–303. [PubMed] [Google Scholar]
- 33.Mantel N, Haenzel W. Statistical aspects of the analysis of data from retrospective studies of disease. J Natl Cancer Inst. 1959;22:719–748. [PubMed] [Google Scholar]
- 34.McCarthy JC, Lee JA. Constrained acetabular components in complex revision total hip arthroplasty. Clin Orthop Relat Res. 2005;441:210–215. doi: 10.1097/01.blo.0000194069.15086.1b. [DOI] [PubMed] [Google Scholar]
- 35.Merle d’aubigné R. Numerical classification of the function of the hip [in French] Rev Chir Orthop Reparatrice Appar Mot. 1970;56:481–486. [PubMed] [Google Scholar]
- 36.Murray DW, Carr AJ, Bulstrode C. Survival analysis of joint replacements. J Bone Joint Surg Br. 1993;75:697–704. doi: 10.1302/0301-620X.75B5.8376423. [DOI] [PubMed] [Google Scholar]
- 37.Philippot R, Adam P, Farizon F, Fessy MH, Bousquet G. Survival of cementless dual mobility sockets: ten-year follow-up [in French] Rev Chir Orthop Reparatrice Appar Mot. 2006;92:326–331. doi: 10.1016/s0035-1040(06)75762-2. [DOI] [PubMed] [Google Scholar]
- 38.Philippot R, Adam P, Reckhaus M, Delangle F, Verdot FX, Curvale G, Farizon F. Prevention of dislocation in total hip revision surgery using a dual mobility design [in French] Rev Chir Orthop Reparatrice Appar Mot. 2009;95:407–413. doi: 10.1016/j.otsr.2009.04.016. [DOI] [PubMed] [Google Scholar]
- 39.Philippot R, Camilleri JP, Boyer B, Adam P, Farizon F. The use of a dual-articulation acetabular cup system to prevent dislocation after primary total hip arthroplasty: analysis of 384 cases at a mean follow-up of 15 years. Int Orthop. 2009;33:927–932. doi: 10.1007/s00264-008-0589-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Philippot R, Farizon F, Camilleri JP, Boyer B, Derhi G, Bonnan J, Fessy MH, Lecuire F. Survival of dual mobility socket with a mean 17 years follow-up [in French] Rev Chir Orthop Reparatrice Appar Mot. 2008;94:43–48. doi: 10.1016/j.rco.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 41.Ritter MA. The cemented acetabular component of a total hip replacement. All polyethylene versus metal backing. Clin Orthop Relat Res. 1995;311:69–75. [PubMed] [Google Scholar]
- 42.Sanchez-Sotelo J, Berry DJ. Epidemiology of instability after total hip replacement. Orthop Clin North Am. 2001;32:543–552, vii. [DOI] [PubMed]
- 43.Sanchez-Sotelo J, Haidukewych GJ, Boberg C. Hospital cost of dislocation after primary total hip arthroplasty. J Bone Joint Surg Am. 2006;88:290–294. doi: 10.2106/JBJS.D.02799. [DOI] [PubMed] [Google Scholar]
- 44.Shapiro G, Weiland D, Markel D, Padgett D, Sculco T, Pellicci P. The use of a constrained acetabular component for recurrent dislocation. J Arthroplasty. 2003;18:250–258. doi: 10.1054/arth.2003.50090. [DOI] [PubMed] [Google Scholar]
- 45.Shrader MW, Parvizi J, Lewallen DG. The use of a constrained acetabular component to treat instability after total hip arthroplasty. J Bone Joint Surg Am. 2003;85:2179–2183. doi: 10.2106/00004623-200311000-00019. [DOI] [PubMed] [Google Scholar]
- 46.Su EP, Pellicci PM. The role of constrained liners in total hip arthroplasty. Clin Orthop Relat Res. 2004;420:122–129. doi: 10.1097/00003086-200403000-00017. [DOI] [PubMed] [Google Scholar]
- 47.Tufescu TV, Dust W. Failure of a new constrained acetabular insert: a report of 2 cases. J Arthroplasty. 2004;19:238–239. doi: 10.1016/j.arth.2003.08.016. [DOI] [PubMed] [Google Scholar]
- 48.Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–1306. [PubMed] [Google Scholar]
- 49.Yun AG, Padgett D, Pellicci P, Dorr LD. Constrained acetabular liners: mechanisms of failure. J Arthroplasty. 2005;20:536–541. doi: 10.1016/j.arth.2004.12.054. [DOI] [PubMed] [Google Scholar]