Abstract
Background
While acetabular structural allografts provide an important alternative for reconstructions, concerns remain with long-term graft resorption, collapse, and failure. Midterm studies of minor column (shelf) allograft suggest reasonable survival but long-term survival is unknown.
Questions/purposes
We therefore assessed long-term graft/cup survivorship, functional scores, radiographic resorption, and complications associated with minor column allograft.
Methods
We retrospectively reviewed 74 patients (85 hips) with a mean age of 54 years (range, 28–83 years) undergoing acetabular cup revision using a minor column allograft. A minor column allograft was used in uncontained acetabular bone defects sized between 30% and 50% of the acetabulum. Graft failure was considered to occur when the graft required revision with another graft, metal augment, reconstruction cage, or excision arthroplasty. The minimum followup was 5 years (mean, 16 years; range, 5.3–25 years).
Results
Twenty-three patients (27 hips) had rerevision for all causes at a mean time to rerevision of 6.9 years (range, 0.1–23). Fifteen grafts failed at a mean time-to-rerevision of 6.1 years (range, 0.5–23.2). The 15- and 20-year Kaplan-Meier survivorships were 61% and 55% for cups and 78% for grafts with rerevision for all causes as end point. With rerevision for aseptic loosening as end point, survivorships were 67% and 61% for cups and 81% for grafts. The mean modified Harris hip scores were 41 (range, 20–60) preoperatively, 73 (range, 40–95) at 1 year postoperatively and 73 (range, 26–93) at last followup.
Conclusion
The data may provide a long-term benchmark by which future treatments for Type III defects can be measured.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Addressing uncontained acetabular bone defects during revision hip arthroplasty is challenging. In the physiologically young and active patient, restoration of host bone stock in addition to a stable functional arthroplasty with relief of pain is desirable to provide adequate support for the implant and to restore the hip center and leg lengths. Further, converting a difficult uncontained acetabular defect to a simpler contained defect would facilitate future rerevision surgery.
The treatment options and corresponding results for such defects depend on the size of the defect. Classification of defect size should reflect treatment options, complication risks, functional outcomes, and survivorships. It should also be sufficiently simple for practical use. We previously classified acetabular bone defects into Type 1, no major bone loss; Type 2, contained bone loss; Type 3, uncontained bone loss with defect size less than 50% of acetabulum; and Type 4, uncontained bone loss with defect size greater than 50% of acetabulum [5, 17]. Although this classification has not been formally validated with implant survivorships, it is more reproducible and reliable than others [19] such as the AAOS/D’Antonio classification [2] and the Paprosky classification [16].
For Type 3 uncontained acetabular bone loss in which there is more than 30% but less than 50% acetabular bone loss, options for acetabular reconstruction include the use of impaction bone grafting [1, 23], acetabular reinforcement ring [6, 18], oblong cup [8, 10], uncemented cup with high hip center [13], structural allograft (minor column or shelf graft) [20, 25], and trabecular metal cup with augment [11, 19, 21, 24]. Concerns have been expressed over early component migration and failure with impaction bone grafting in uncontained segmental acetabular bone defects. Van Haaren et al. [23] reported a 72% survivorship at a mean followup of 7 years (1.6–10) with revision for aseptic loosening as endpoint and Buttaro et al. [1] reported a 91% survivorship (n = 23) at a mean followup of 3 years (2–5) with 2 mm or more migration seen in all cups (median 3 mm, range, 2–25 mm). Acetabular reinforcement rings reportedly have more than 80% cup survivorships at 10 years [6, 18]. The use of high hip center arthroplasty has not been widespread and has been associated with leg shortening, impinging instability, lower functional scores and survivorship. Morag et al. [13] reported poorer survivorship (82% versus 94%), mean WOMAC scores (62 versus 70) and mean Harris Hip scores (70 versus 83) in patients with high hip centers (> 35 mm above radiological teardrop, n = 31) compared to patients without high hip centers (n = 32) after revision at a mean followup of 10 years (range, 3–20). Studies reporting on the use of uncemented oblong cups were few with 90% midterm survivorships, but no long-term results [8, 10]. Trabecular metal cups and augments has been associated with survivorships around 97% at 3 years [11, 19, 21, 24] while minor column acetabular allografts around 80% survivorship at 10 years with cup revision for aseptic loosening as endpoint [7, 20, 25]. However, there remains a concern about further resorption, collapse, and failure.
We have previously reported a cup survivorship of 80% (n = 51) and a graft survivorship of 94% for revision arthroplasty with type 3 acetabular defect [25]. The mean followup period was 9.9 years (5.7 to 16.3) with failure defined as rerevision for aseptic loosening.
To confirm the longer-term fate of these allografts, we assessed the (1) rerevision rates for cup and graft with 15- and 20-year Kaplan-Meier survivorships; (2) radiographic graft union, graft resorption and cup migration; (3) functional scores preoperatively, at 1 year and at last followup; and (4) other associated complications.
Patients and Methods
We retrospectively reviewed prospectively collected data on 74 patients (85 grafts) who had revision of the acetabular components using minor column allografts between 1984 and 2003. We considered a minor column (shelf) allograft was indicated when the acetabular defect was uncontained and involved more than 30% but less than 50% of the acetabulum. The acetabular defect size was assessed preoperatively by radiographs but mainly determined by intraoperative assessment. We included 21 patients in the survivorship analysis even though they died (4) or were lost to followup (17) before the 5-year followup mark. Of the 17 who were lost to followup before the 5-year followup mark, nine were operated in the 1980s, seven in the 1990s. The remaining 53 patients (64 hips) had a mean age of 54 years (range, 28–83) at the time of surgery and a mean followup duration of 16 years (range, 5–25). Among the 53 patients, five patients died after a mean followup of 12 years (range, 7–15) and 10 were lost to followup after a mean followup of 12 years (range, 5–17). There were 36 patients with more than 15 years followup and 16 patients with more than 20 years followup.
We classified the defects using a previously published practical and simple classification system on acetabular defects [17]. Type I referred to no major loss of bone stock; Type II, contained loss of bone stock (cavitary); Type III, uncontained loss of bone stock involving less than 50% of acetabulum; Type IV, uncontained loss of bone stock involving more than 50% of acetabulum; and Type V, pelvic discontinuity with uncontained loss of bone stock. A minor column allograft was indicated for a Type III acetabular defect when the defect was less than 50% but more than 30% of the acetabulum. A defect less than 30% did not need grafting and a defect more than 50% needed a major column allograft in conjunction with a protective Burch-Schneider ilioischial cage or a Muller reinforcement roof ring [5].
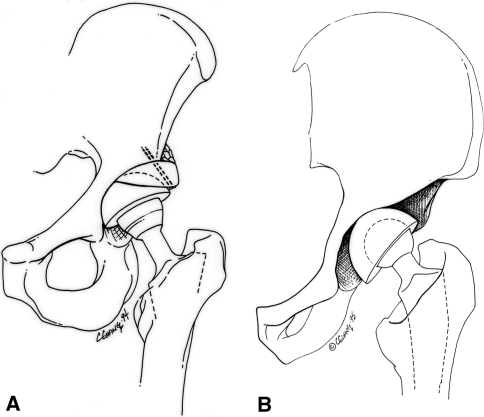
A single surgeon (AEG) performed all surgery. The surgical technique and postoperative care program have been previously described [7]. The surgical approach was transgluteal or through a modified trochanteric slide or extended trochanteric osteotomy. The hip was dislocated to remove the failed acetabular component, cement, and soft tissue debris. The acetabular bed was reamed and a trail cup was inserted to assess host acetabular percentage defect [11]. This was achieved by visually dividing the trial cup into 4 quadrants and assessing the amount of component uncoverage in each quadrant. We then determined the total amount of acetabular uncoverage that equated the acetabular defect size. Bone allograft was obtained from our institutional bone bank. Patient donor selection, harvesting, and processing of allografts were in accordance with the Musculoskeletal Council of the American Association of Tissue Banks [4, 14]. The allografts obtained were deep frozen at −70°C and irradiated with 2.5 megarads. Intraoperatively, the thawed structural allograft was shaped into the defect and routinely fixed with two 4.5-mm malleolar or 6.5-mm cancellous screws with washers. We placed morselized autografts or allografts at the graft–host junction on the ilium to act as a buttress graft. The acetabular bed was further prepared and part of the graft carefully reamed for optimal cup surface contact before the definitive acetabular component was cemented (during the early part of the study) or press-fitted (during the later part of the study) into the socket (Fig. 1A–B).
Fig. 1A–B.
(A) A drawing showing an uncontained defect involving less than 50% of the acetabulum. (B) A minor column (shelf) graft supporting less than 50% of the cup is held with two cancellous screws. The flying buttress graft is cancellous autograft bone. (Reprinted with permission from Woodgate IG, Saleh KJ, Jaroszynski G, Agnidis Z, Woodgate MM, Gross AE. Minor column structural acetabular allografts in revision hip arthroplasty. Clin Orthop Relat Res. 2000;371:75–85, Fig. 1A–B. Reproduced with permission of Catherine Chang, Medical Illustrator.)
Prophylactic antibiotics were started intravenously at induction and were continued for 5 days after surgery. Deep vein thrombosis prophylaxis with subcutaneous enoxaparin was continued for 21 days after operation. Patients were instructed to avoid active abduction for 6 weeks but passive assisted abduction with physiotherapist was permitted. Nonweightbearing mobilization with 2 crutches was allowed but weight bearing was avoided for 3 months until radiographic evidence of graft host union was confirmed. Physiotherapy to improve gait pattern was occasionally prescribed thereafter, for example, for hip extensor or abductor strengthening for 2 to 6 months. All patients were routinely seen postoperatively at 6 weeks, 3 months, 6 months, 1 year and then annually. Routine clinical assessment included gait, leg length, wound, range of motion and neurological status. Radiological assessment included an anteroposterior pelvic view and a lateral view of the hip and entire prosthesis.
Our clinical outcomes measures were (1) survivorships for acetabular component and graft; (2) radiographic graft union, resorption and cup migration; (3) changes in the modified Harris hip scores [15] at 1 year and at last followup; and (4) other major complications.
Two of us (PTHL, GR) independently assessed radiographs in 38 of the 53 patients (40 of 64 grafts). This was because most of the 15 patients without radiographs for graft assessment had the index surgery and rerevision surgery in the 1980s and 1990s. The institution converted to digital imaging in 2003 and this resulted in loss of a proportion of the hard-copy radiographic archive. We assessed graft union, graft resorption and cup migration. Graft union was considered to occur when there was radiographic evidence of trabecular bridging at the graft-host interface. Graft resorption was assessed and classified using the techniques described by Jasty and Harris [9]. Graft resorption was considered to occur when there was an area of lucency within the graft on an AP pelvic radiograph. Resorption was considered “mild” when the area of resorption involved, seen as lucency, was less than one-third of the length of the graft; “moderate” when it involved more than a third but less than half of the length of the graft; and “severe” when it involved more than half of the length of the graft. Assessments were made by comparing radiographs obtained soon after the index operation and radiographs obtained at last followup visit. The presence of cup migration was grouped into less than 3 mm, between 3–5 mm and more than 5 mm. Cup migration of < 3 mm was considered not significant. We expressed interobserver variability as a percentage of the difference in observations between the two observers for each radiological outcome measure. Our interobserver differences were 20% (8/40) for the presence or extent of graft resorption and 28% (11/40) for the presence or extent of cup migration. When migration of < 3 mm was considered as not significant, the interobserver difference on the presence of major cup migration was 5% (2/40). There were no interobserver differences on the assessment of graft union.
The Kaplan-Meier survivorship [3] for acetabular component was calculated with the four endpoints: (1) failure of the graft for non-septic causes; (2) failure of graft for any cause; (3) cup rerevision for aseptic loosening; and (4) cup rerevision for any cause. We defined graft failure when there was an uncontained acetabular defect during rerevision that required additional structural support in the form of structural allograft graft, metal augment, or reconstruction cage to achieve primary stability. A two-stage rerevision or excisional arthroplasty was considered as graft failure while rerevision with cup-only exchange was considered as graft success. We used the Mann-Whitney U test to compare the modified Harris hip scores at 1 year after surgery and at the last followup assessment with the scores before surgery.
Results
Twenty-three patients (27 cups) required rerevision for any cause at a mean time-to-rerevision of 6.9 years (range, 0.1–23). The cup rerevision rate was 32%. The causes for cup failure were aseptic loosening or osteolysis (22), infection (two), dislocation (one), graft nonunion (one), and acetabular component fracture (one). The treatment for cup failure included cup-only exchange (12), cup rerevision with structural allograft, cage or metal augment (12), excision arthroplasty (two) and two-stage revision arthroplasty (one).
Fifteen patients had graft failures at a mean time to rerevision of 6.1 years (range, 0.5–23). The graft failure rate was 18%. Causes for graft failure included aseptic loosening or osteolysis (11), infection (two), acetabular component fracture (one), and graft nonunion (one). Treatments included minor column graft (six), major column graft (four), metal augment (one), excision arthroplasty (two), trabecular metal cup-cage reconstruction (one), and two-stage revision arthroplasty (one). The 2-stage revision and one of the excision arthroplasties were performed for infection.
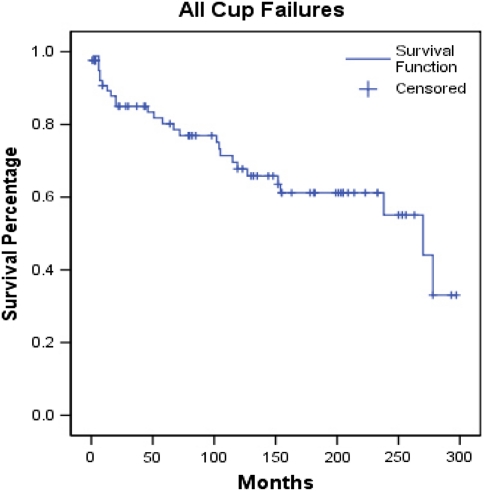
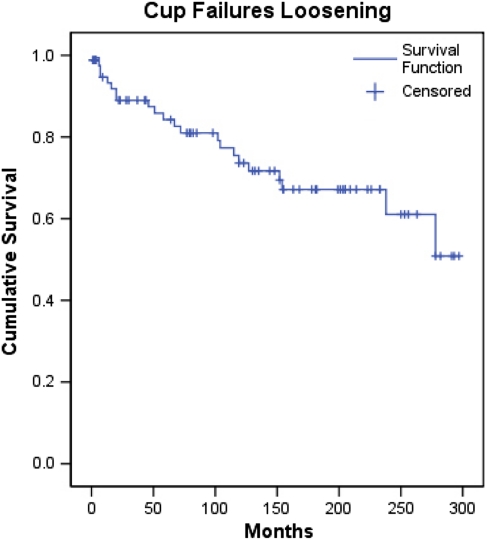
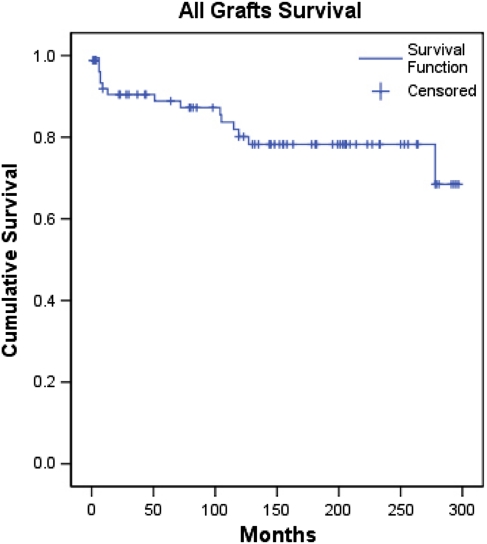
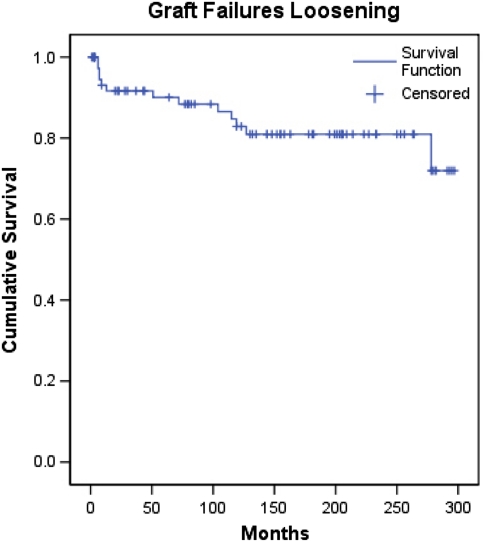
The 15- and 20-year Kaplan-Meier survivorships for cup were 61% and 55% with the end point defined as rerevision for any cause (Fig. 2). With the end point defined as rerevision for aseptic loosening, the survivorships were 67% and 61% (Fig. 3). The 15- and 20-year Kaplan-Meier survivorships for graft were 78% with the end point defined as rerevision for any cause (Fig. 4). With the end point defined as rerevision for nonseptic failure, the 15- and 20-year survivorships were 81% (Fig. 5).
Fig. 2.
Kaplan-Meier survivorship is shown for cup with revision for any cause as the end point.
Fig. 3.
Kaplan-Meier survivorship is shown for cup with revision for aseptic loosening as the end point.
Fig. 4.
Kaplan-Meier survivorship is shown for graft with revision for any cause as the end point.
Fig. 5.
Kaplan-Meier survivorship is shown for graft with revision for aseptic loosening as the end point.
All grafts healed radiographically with trabecular bridging at the graft–host junction except for one. All patients had resorption except for seven (17.5%). Graft resorption was considered mild in 28 patients (70%), moderate in three (7.5%), and severe in two (5%). There were six cup rerevisions and one graft failure in patients with mild resorption at a minimum followup of 4.4 years (mean, 16.2 years; range, 4.4–24.8 years) (one case was included with less than 5 years followup because of cup and graft failure). None of the three patients with moderate graft resorption had rerevision at a minimum followup of 11 years (mean, 14.7 years; range, 11–22). The two patients with severe resorption had graft failure and rerevision at 4 and 23 years after the index surgery. Cup migration occurred in 18 patients. Ten patients migrated less than 3 mm, of which there were three cup rerevisions, including one graft failure. Five had migrated between 3 and 5 mm but subsequently stabilized and did not required rerevision surgery. Three patients had migrated more than 5 mm and underwent rerevisions. Of the 25 patients for whom radiographs of the graft were not available for assessment, there were 19 cup failures, which included 13 graft failures that were mostly rerevised in the 1980s and 1990s.
The mean modified Harris hip score was 40.5 (range, 20–60) before surgery, 72.8 (range, 40–95) at 1 year after surgery and 73.1 (range, 26–93) at last followup assessment.
Associated complications included three dislocations treated with closed reduction, three nerve injuries that resolved with nonoperative treatment, and one minor column fracture during reduction that was treated nonoperatively without further complications. There was one intraoperative death from vascular complications despite pelvic angiography and iliac vessel embolization. This was due to screw placement outside the ‘safe zone’ [12].
Discussion
The main concerns with minor column allograft in revision hip arthroplasty are longterm graft resorption, collapse, and failure. Despite reasonable function and survival from midterm reports [20, 25], reports of long-term results are lacking. In this long-term study on minor column allograft, we have assessed and reported on the (1) rerevision rates for cup and graft with 15- and 20-year Kaplan-Meier survivorships for aseptic loosening and for all causes; (2) radiographic graft union rates, the presence/extent of graft resorption and the presence/extent of cup migration; (3) functional outcomes at 1 year and at last followup; and (4) other associated complications.
There were several limitations to our study. First, we lost 17 patients to followup. Most of these patients were operated in the 1980s and 1990s and were without known failures. Although they were lost before the 5-year mark, we have included them in the at risk population of the survivorship analysis and have censored them at the end of their respective followup period. Second, only 38 of 53 patients (40 of 64 grafts) had radiographs available for graft assessment. This was because most of the 15 patients without radiographs for graft assessment had the index surgery and rerevision surgery in the 1980s and 1990s. The institution converted to digital imaging in 2003 and this resulted in loss of a proportion of the hard-copy radiographic archive. This was unfortunate because among this group of 15 patients (24 grafts), there were 13 graft failures that might help to show a relationship between graft resorption and failure. Third, the study consisted of a heterogeneous group of patients with regard to the number of previous hip arthroplasties ranging from one to six and the extent of surgery on the femoral side. Although we restricted the cohort to an acetabular defect of 30% to 50% of the acetabulum, it was difficult to quantify soft tissue function, which was generally indirectly related to the number of previous hip arthroplasties the patient had. Fourth, as experienced by other authors [23], we experienced difficulty in quantifying the extent of graft resorption on AP pelvic radiographs. We had high interobserver consistency with the assessment of graft union and substantial cup migration of > 3 mm but a 20% inconsistency with regard to the extent of graft resorption. Previous studies have not reported on interobserver variabilities on these radiographic assessments and we were unable to make comparison.
We could find only two midterm reports on the use of acetabular structural allografts in revision hip arthroplasty that specifically addressed Type III acetabular defects (Table 1). We could not find any long-term reports on revision arthroplasty using minor column allografts specifically for Type 3 acetabular defects. Two previous studies reported cup survivorships of 78 and 80% and graft survivorships of 100% and 94%, both with aseptic loosening as endpoints and similar mean followup durations of 10 years [20, 25]. Our long-term data at 15 and 20 years support the trend of graft survivorship in relation to cup survivorship. Almost half of the rerevisions for cups in our study were cup-only exchanges. This showed that the minor column graft was able to convert the previously uncontained segmental defect into a contained defect that did not require reconstructive augmentation with structural graft, metal augment, or cage during rerevision surgery for primary stability.
Table 1.
Comparison of results for studies on the use of minor column shelf allograft in revision hip arthroplasty
| Study | Woodgate and Gross [25] | Sporer et al. [20] | Lee et al. [current study] |
|---|---|---|---|
| Number of patient cases | 51 | 23 | 85 |
| Mean (range) followup in years | 9.9 (5.7–6.3) |
10.3 (7–15) |
16 (5–25) |
| Acetabular defect type | Type III | Paprosky: Type IIIa | Type III |
| Allograft type | Bulk femoral head | Distal femur | Bulk femoral head |
| Endpoint | Rerevision for aseptic loosening | Rerevision for aseptic loosening | Rerevision for aseptic loosening |
| Cup survivorship in % | 80 | 78 | 67 (KM at 15 yrs) 61 (KM at 20 yrs) |
| Graft survivorship in % | 94 | 100 | 81 (KM at 15 and 20 yrs) |
| Graft host interdigitation | 98% | 95% | 98% |
| Graft resorption | None: 5 Minor: 32 Moderate: 9 Severe: 5 |
None: 14 Mild: 2 Moderate: 4 Severe: 2 |
None: 7 Mild: 28 Moderate: 3 Severe: 2 |
| Cup migration | Not reported | Not reported | None: 7 < 3 mm: 25 3–5 mm: 5 > 5 mm: 3 |
| Mean functional scores at last followup | No preoperative scores | MAPS: Improved by 5 | HHS: Improved by 32 |
MAPS = Merle d’Aubigne-Postel Score; HHS = Harris Hip Score; KM = Kaplan-Meier.
Our study supports previous studies on the high incidence of graft healing onto host bone [20, 25]. Radiographically the graft-host interdigitation presented as trabecular bridging at the graft-host junction in more than 95% of patients. Similar to previous studies [20, 25], most of our patients experienced graft resorption and the majority of the resorptions were mild and severe resorptions were few. Also, patients with severe graft resorption almost all experienced graft failure but patients with minor graft resorption also experienced graft failure, although less frequently. In previous studies [20, 25], there was no mention of the frequency or extent of cup migration for us to compare.
Similar to previous studies [20, 25], there was substantial improvement in functional scores in general, despite frequent extensive concurrent or previous femoral side surgery and several previous acetabular side operations.
For type III acetabular defects, other options include the use of impaction bone grafting, reinforcement rings, high hip center arthroplasty, oblong cups and trabecular metal cups and augments (Table 2). Concerns over migration and early failure remain with the use of impaction morselized allograft for uncontained acetabular segmental defects [1, 23]. The survivorships associated with the use of reinforcement ring were between 80 and 90% but with only 6 years mean followup duration [6, 18]. The use of high hip center arthroplasty has been associated with inferior results to arthroplasty with normal hip centers [13]. The survivorship with uncemented oblong cups is reportedly between 86% and 93% at mean followup durations between 6 to 9 years [8, 10]. However, these studies involved contained and uncontained defects. The result on trabecular metal cups and augments were encouraging with survivorships above 95% but these were short-term studies with mean followup durations of about 3 years [11, 19, 21, 22, 24].
Table 2.
Comparison of results on studies of various treatment options for revision surgery with acetabular bone defects
| Technique | Study | No. of patient cases | Mean (range) followup in years | Acetabular defect type | Endpoint | Cup survivor-ship in % | Change in pre- and post-op function | Comments |
|---|---|---|---|---|---|---|---|---|
| Impacting bone grafting | Buttaro et al. [1] | 23 | 3 (2–4.7) | AAOS: Type III | Rerevision for any cause | 90 | No pre-op functional scores | All cups migrated (mean 5.1 mm, range, 2–25 mm) |
| Van Haaren et al. [23] | 71 | 7 (1.6–9.7) | AAOS: 13 type I 17 type II 35 type III 6 Type IV |
Rerevision for aseptic loosening | 72 | No functional scores | 70% of the failed group had AAOS type III and IV defects | |
| High hip center arthroplasty | Morag et al. [13] | 31 | 10 (3–20) | Congenital acetabular dysplasia | Revision for non-septic causes | 82 (HHC) compared to 94 (non-HHC) for 10-year KM | No pre-op functional scores | Poorer results with HHC - hip centre is more than 35 mm above teardrop |
| Uncemented oblong cup | Herrera et al. [8] | 35 | 6.3 (4–8) | AAOS: 29 type III 6 type IV |
Revision for cup stability | 86 | mean HHS improved by 42 | |
| Koster and Rading [10] | 56 | 9 (8–12) | Paprosky: 3 type I 39 type II 14 type III |
Rerevision for any cause | 93 | mean HHS improved by 31 | ||
| Acetabular reinforcement rings | Gerber et al. [6] | 50 | 6 (5–8.4) | AAOS: 24 type II 24 type III 2 type IV |
Rerevision or radio-graphic loosening | 81 (KM at 10 years) | mean MAPS improved by 5 | |
| Schlegel et al. [18] | 164 | 6 (2–17) | AAOS: 11 type I 33 type II 92 type III 8 type IV 20 without defect |
Rerevision for any cause | 90 | No pre-op functional scores | ||
| Trabecular metal and augments | Lakstein et al. [11] | 53 | 3.8 (2–6) | contained defects of more than 50% of the acetabulum | Rerevision for cup migration | 96 | mean MAPS improved by 5.2 | |
| Sporer and Paprosky [21] | 28 | 3.1 (1–4) | Type III | Rerevision for any causes | 96 | mean MAPS improved by 3.8 | ||
| Weeden and Schmidt [24] | 43 | 2.8 (2–4) | 33 Type III 10 Type IV |
Rerevision for any causes | 98 | mean MAPS improved by 4.9 mean HHS improved by 52 |
MAPS = Merle d’Aubigne-Postel Score; HHS = Harris Hip Score; KM = Kaplan-Meier; HHC = High hip center.
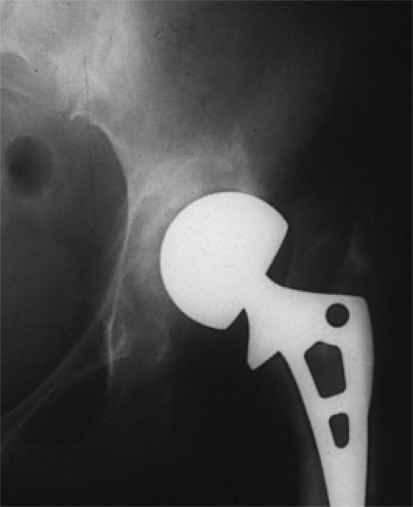
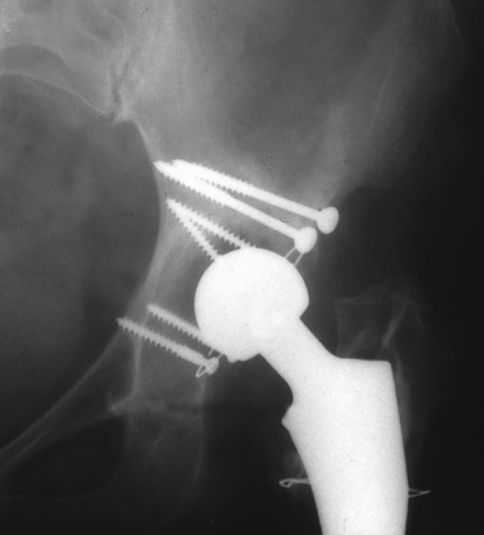
Our data may provide a long term benchmark by which future treatments such as trabecular metal can be measured. We have started to use trabecular metal cups and augments in revision arthroplasty with type III acetabular defects (Fig. 6). Although the early results are encouraging and comparable to minor column grafts with similar followup duration, we cautioned its use as only short term results are available. In patients who are more likely to require further revision surgery, we continue to use minor column allografts to facilitate future potential rerevisions (Fig. 7).
Fig. 6.
Preoperative AP hip radiograph with Type 3 acetabular defect is shown.
Fig. 7.
Postoperative AP hip radiograph at 23 years shows minor column allograft clinically and radiographically intact.
Acknowledgment
We thank Mathew MacDonald for help with data collection and processing.
Footnotes
One or more of the authors (PTHL) received funding from the Royal College of Surgeons of England/Harry Morton Fellowship, the British Orthopaedic Association/British Orthopaedic Foundation Trust, and the John Charnley Trust.
Each author certifies that his or her institution has approved the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
References
- 1.Buttaro MA, Comba F, Pusso R, Piccaluga F. Acetabular revision with metal mesh, impaction bone grafting, and a cemented cup. Clin Orthop Relat Res. 2008;466:2482–2490. doi: 10.1007/s11999-008-0442-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.D’Antonio JA. Periprosthetic bone loss of the acetabulum. Classification and management. Orthop Clin North Am. 1992;23:279. [PubMed] [Google Scholar]
- 3.Dorey F, Amstutz HC. Survivorship analysis in the evaluation of joint replacement. J Arthroplasty. 1986;1:63–69. doi: 10.1016/S0883-5403(86)80010-9. [DOI] [PubMed] [Google Scholar]
- 4.Fawcett K, Barr AR. Tissue Banking. Arlington, VA: American Association of Tissue Banks; 1987. [Google Scholar]
- 5.Garbuz D, Morsi E, Mohamed N, Gross AE. Classification and reconstruction in revision acetabular arthroplasty with bone stock deficiency. Clin Orthop Relat Res. 1996;323:98–107. doi: 10.1097/00003086-199603000-00012. [DOI] [PubMed] [Google Scholar]
- 6.Gerber A, Pisan M, Zurakowski D, Isler B. Ganz reinforcement ring for reconstruction of acetabular defects in revision total hip arthroplasty. J Bone Joint Surg Am. 2003;85:2358–2364. doi: 10.2106/00004623-200312000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Gross AE, Allan DG, Catre M, Garbuz DG, Stockley I. Bone grafts in hip replacement surgery. The pelvic side. Orthop Clin North Am. 1993;24:679–695. [PubMed] [Google Scholar]
- 8.Herrera A, Martínez AA, Cuenca J, Canales V. Management of types III and IV acetabular deficiencies with the longitudinal oblong revision cup. J Arthroplasty. 2006;21:857–864. doi: 10.1016/j.arth.2005.08.026. [DOI] [PubMed] [Google Scholar]
- 9.Jasty M, Harris W. Salvage total hip reconstruction in patients with major acetabular bone deficiency using structural femoral head allografts. J Bone Joint Surg Br. 1990;72:63–67. doi: 10.1302/0301-620X.72B1.2298796. [DOI] [PubMed] [Google Scholar]
- 10.Koster G, Rading S. Revision of failed acetabular components utilizing a cementless oblong cup: an average 9-year follow-up study. Arch Orthop Trauma Surg. 2009;129:603–608. doi: 10.1007/s00402-008-0624-8. [DOI] [PubMed] [Google Scholar]
- 11.Lakstein D, Backstein DJ, Safir O, Kosashvili Y, Gross AE. Trabecular metal for acetabular defects with 50% of less host bone contact. Clin Orthop Relat Res. 2009;467:2318–2324. doi: 10.1007/s11999-009-0772-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu Q, Zhou YX, Xu HJ, Tang J, Guo SJ, Tang QH. Safe zone for transacetabular screw fixation in prosthetic acetabular reconstruction of high developmental dysplasia of the hip. J Bone Joint Surg Am. 2009;91:2880–2885. doi: 10.2106/JBJS.H.01752. [DOI] [PubMed] [Google Scholar]
- 13.Morag G, Zalzal P, Liberman B, Safir O, Flint M, Gross AE. Outcome of revision hip arthroplasty in patients with a previous total hip replacement for developmental dysplasia of the hip. J Bone Joint Surg Br. 2005;87:1068–1072. doi: 10.1302/0301-620X.87B8.15949. [DOI] [PubMed] [Google Scholar]
- 14.Mowe JC. Standards for Tissue Banking. Arlington, VA: American Association of Tissue Banks; 1988. [Google Scholar]
- 15.Murray D. The hip. In: Pynsent D, Fairbank J, Carr A, eds. Outcome Measurements in Orthopaedics. Oxford, UK: Butterworth-Heinemann; 1993:198–227.
- 16.Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994;9:33–44. doi: 10.1016/0883-5403(94)90135-X. [DOI] [PubMed] [Google Scholar]
- 17.Saleh KJ, Holtzman J, Gafni A, Saleh L, Jaroszynski G, Wong P, Woodgate I, Davis A, Gross AE. Development, test reliability and validation of a classification for revision hip arthroplasty. J Orthop Res. 2001;19:50–56. doi: 10.1016/S0736-0266(00)00021-8. [DOI] [PubMed] [Google Scholar]
- 18.Schlegel UJ, Bitsch RG, Pritsch M, Clauss M, Mau H, Breusch SJ. Mueller reinforcement rings in acetabular revision: outcome in 164 hips followed for 2–17 years. Acta Orthop. 2006;77:234–241. doi: 10.1080/17453670610045966. [DOI] [PubMed] [Google Scholar]
- 19.Siegmeth A, Duncan CP, Masri BS, Kim WY, Garbuz DS. Modular tantalum augments for acetabular defects in revision hip arthroplasty. Clin Orthop Relat Res. 2009;467:199–205. doi: 10.1007/s11999-008-0549-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sporer SM, O’Rourke M, Chong P, Paprosky WG. The use of structural distal femoral allografts for acetabular reconstruction Average ten-year follow-up. J Bone Joint Surg Am. 2005;87:760–765. doi: 10.2106/JBJS.D.02099. [DOI] [PubMed] [Google Scholar]
- 21.Sporer SM, Paprosky WG. The use of trabecular metal acetabular component and trabecular metal augment for severe acetabular defects. J Arthroplasty. 2006;21:83–86. doi: 10.1016/j.arth.2006.05.008. [DOI] [PubMed] [Google Scholar]
- 22.Unger AS, Lewis RJ, Gruen T. Evaluation of a porous tantalum uncemented acetabular cup in revision total hip arthroplasty: clinical and radiological results of 60 hips. J Arthroplasty. 2005;20:1002–1009. doi: 10.1016/j.arth.2005.01.023. [DOI] [PubMed] [Google Scholar]
- 23.Haaren EH, Heyligers IC, Alexander FG, Wuisman PI. High rate of failure of impaction grafting in large acetabular defects. J Bone Joint Surg Br. 2007;89:296–300. doi: 10.1302/0301-620X.89B3.18080. [DOI] [PubMed] [Google Scholar]
- 24.Weeden SH, Schmidt RH. The use of tantalum porous metal implants for Paprosky 3A and 3B defects. J Arthroplasty. 2007;22:151–155. doi: 10.1016/j.arth.2007.04.024. [DOI] [PubMed] [Google Scholar]
- 25.Woodgate I, Gross AE. Minor column structural acetabular allografts in revision hip arthroplasty. Clin Orthop Relat Res. 2000;371:75–85. doi: 10.1097/00003086-200002000-00009. [DOI] [PubMed] [Google Scholar]