Abstract
Background
Despite stem subsidence being a major complication of femoral impaction bone grafting in cemented revision hip arthroplasty, few studies have distinguished subsidence at the prosthesis-cement interface from that at the cement-bone interface. It is unknown how technique developments intended to improve the procedure influence stability of the stem.
Questions/purposes
We used a sensitive technique to measure subsidence of a cemented polished collarless double-taper stem at each interface after femoral impaction grafting and compared subsidence, radiographic loosening, complications, and reoperations over three series of hips defined by technique developments.
Patients and Methods
Three series were defined: Series 1 (n = 23, irradiated allograft), Series 2 (n = 12, double-washed, size-profiled graft, nonirradiated bone, long stems as required), and Series 3 (n = 21, modular tamps). Stem subsidence was analyzed with Ein Bild Röntgen Analyse software. Radiographic loosening, complications, and reoperations were also determined.
Results
The median subsidence at 12 months for Series 1, 2, and 3 were 2.1, 0.5, and 0.7 mm at the prosthesis-cement interface and 1.3, 0.1, and 0.1 mm at the cement-bone interface. There were two postoperative Vancouver B periprosthetic fractures in Series 1, four hips were revised for loosening in Series 1, and there were no fractures or loosening in Series 2 and 3 at minimum 2 years’ followup. There were no surviving hips radiographically classified as possibly or probably loose.
Conclusions
Evolution in techniques of femoral impaction grafting in this study were associated with reduced subsidence of the stem at both the prosthesis-cement interface and cement-bone interface when compared to the original series. Concurrent with reduced stem subsidence was the absence of periprosthetic fracture, radiographic loosening, and complications requiring rerevision.
Level of Evidence
Level II, prognostic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Femoral impaction bone grafting (IBG) in revision THA (rTHA) has potential advantages, including the restoration of bone and the need for long stems in young and middle-aged patients [39]. However, stem subsidence of greater than 5 mm and up to 31 mm [9, 15, 18, 24, 25, 33, 41, 42] and postoperative femoral fracture with a prevalence of up to 15% [6, 10, 12, 25, 29] have been reported for femoral IBG in rTHA.
Impaction bone grafting has evolved with advances in technique and instrumentation aimed at simplifying the procedure and reducing these complications [40]. These advances have led to improved reports of femoral stem survival to rerevision when a cemented collarless double-taper stem has been used for femoral IBG [16, 22, 30, 34]. Using the end point aseptic loosening of the stem, survival of 97% at 4.7 years [22], 99% at 10 to 11 years [16], and 99% at 15 years [30] have been reported.
The polished collarless double-taper femoral stem is designed to undergo self-limiting subsidence within the cement to enhance stability and compressive load distribution through to the bone for effective fixation at the cement-bone interface [13, 44]. Excessive subsidence at the prosthesis-cement interface may suggest inadequate cement thickness or poor support of the cement by inadequately packed graft [7, 15, 40, 44], which may lead to complications, including dislocation, cement fracture, aseptic loosening, and periprosthetic fracture [8, 9, 24]. Excessive subsidence at the cement-bone interface may suggest poor cement interdigitation in the graft, inadequate support by the bone graft, poor graft impaction, or poor graft biology [5, 7, 15, 16].
Although measures of total stem subsidence are routine, few studies have distinguished stem subsidence at the prosthesis-cement interface from that at the cement-bone interface so as to properly describe the pattern of subsidence after femoral IBG [8, 10, 14, 25, 45]. These studies suggest that stem subsidence within the cement mantle occurs in a predictable pattern and support the use of this technique. However, they are limited because manual measurements using plain radiographs were used to distinguish site of subsidence and values were only reported at latest followup, which varied across series. Manual techniques cannot accurately detect subsidence [3, 23] and have a measurement error of ± 5 mm. Recent studies have used more sensitive techniques, such as radiostereometric analysis (RSA) [21, 29, 42], to distinguish subsidence at each interface. However, RSA studies of IBG have only reported prosthesis movement relative to femoral bone [27, 38]. Without sensitive measures of subsidence that distinguish movement at each interface, it is difficult to evaluate the mechanism of failure of stems and how technique changes might reduce subsidence.
The technique of femoral IBG has evolved with the aim of improving early implant stability [19] through better impaction, shear strength, and remodeling potential of the graft. This evolution includes the method of graft preparation, such as the removal of fat by washing, size profiling of the bone particles [7, 28, 40], the use of nonirradiated bone graft [16, 18], and the use of modular tamps.
The purposes of the study were to determine whether (1) developments in technique reduced femoral stem subsidence at the prosthesis-cement and cement-bone interfaces among three sequential series of rTHAs performed with femoral IBG; and (2) developments in technique were associated with a reduced number of patients with postoperative periprosthetic diaphyseal fracture, radiographic loosening, and other complications requiring further surgery.
Patients and Methods
We reviewed 53 patients (56 hips) who have been prospectively studied since undergoing IBG at rTHA with a cemented collarless double-taper stem (Fig. 1) between May 1993 and June 2007. No hips were excluded from review. The criteria for IBG were age younger than 70 years or active older patients with moderate to severe proximal cortical bone loss. In older inactive patients, distal fixation cementless stems were used. The main diagnosis at revision was aseptic loosening of the femoral stem in 49 hips (88%). Using the nomenclature of the Endo-Klinik [11], the majority of hips had Types 2 and 3 femoral deficiencies (Table 1).
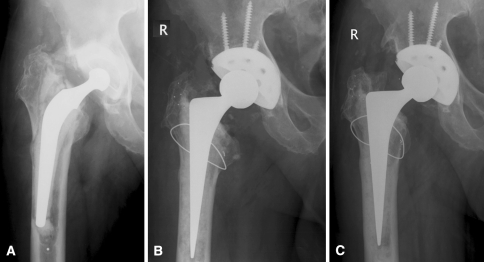
Fig. 1A–C.
(A) A preoperative AP hip radiograph shows a loose Charnley stem in a 64-year-old man in Series 3. AP radiographs show the same hip (B) postoperatively after IBG and revision to a cemented collarless double-taper CPT® stem and (C) at 3 years postoperatively.
Table 1.
Patient and clinical characteristics
| Variable | Series 1 | Series 2 | Series 3 | All hips |
|---|---|---|---|---|
| Number of hips | 23 | 12 | 21 | 56 |
| Age (years)* | 66 (46–82) | 56 (27–75) | 60 (41–88) | 63 (27–88) |
| Male:female | 19:4 | 10:2 | 13:8 | 42:14 |
| Reason for stem revision† | ||||
| Loosening:infection:peripros#:stem# | 22:0:1:0 | 11:1:0:0 | 16:3:1:1 | 49:4:2:1 |
| Exeter:CPT stem | 22:1 | 2:10 | 0:21 | 24:32 |
| Standard:long-length stem | 22:1 | 8:4 | 14:7 | 44:12 |
| Endo-Klinic classification 1:2:3:4 | 2:8:11:2 | 0:7:3:2 | 0:12:7:2 | 2:27:21:6 |
| Followup (years) | 8–15 | 5–10 | 2–5 | 2–15 |
* Values are expressed as mean, with range in parentheses; †peripros# = periprosthetic fracture; stem# = femoral stem fracture.
We defined three series as Series 1, 2, and 3, based on the timing of technical changes to the IBG technique (Table 1). In Series 1 (n = 23), the original femoral IBG technique was used [26, 36]. Fresh-frozen femoral head allograft was sterilized by a dose of 25 kGy gamma-irradiation for 10 hours. Bone chips sized 1 to 3 mm were prepared using a Tracer mill (Tracer Designs, Inc, Santa Paula, CA) and manually impacted with a monobloc tamp. Series 2 (n = 12) was defined by changes to the bone graft preparation. Fine bone chips (2 to 3 mm) for distal impaction, a mixture of fine and coarse bone chips (3 to 4 mm) for the bone mantle around the midstem, and coarse bone chips and croutons (5 to 10 mm) for the proximal femur up to the neck cut were prepared using the Noviomagus mill (Spierings Medische, Nijmegen, The Netherlands) [40]. The graft was double washed in warm saline, drained with a sieve, and manually impacted [40]. Also, from Series 2 onwards, nonirradiated allograft bone was used, and long-length stems [31, 35] and proximal calcar mesh support [2] were used more commonly. From Series 2, the milled bone chips were mixed with vancomycin in a dose of 0.25 g per femoral head. In Series 3 (n = 21), modular impaction tamps were introduced to replace monobloc tamps (Zimmer, Inc, Warsaw, IN) (Fig. 2). The technical advantages of the modular tamps were that they allowed for a quicker build of the bone graft mantle in the midstem area, the loss of desired stem anteversion during proximal impaction was avoided since the modular proximal tamp is guided by the distal tamp, and they facilitated the use of long stems.
Fig. 2.

A photograph showing a set of modular tamps used for Series 3. Tamps were available for standard length and long stems, and there were size and neck angle options. The distal tamp acts as a guide for proximal impaction, while maintaining position and length.
One consultant surgeon (DWH) performed the majority of revisions; however, two additional consultant surgeons (SG and AM) carried out 11 of the earlier cases. A posterior approach was used. Extended femoral osteotomies were used as necessary to extract ingrown or fractured stems. Before IBG, fractures or osteotomies were secured with cables or wires and cortical defects were contained with wire mesh and, in some cases, strut allograft and cables. There were three (13%), two (17%), and one (5%) intraoperative diaphyseal femoral fracture in Series 1, 2, and 3, respectively. One femoral cortical perforation occurred in Series 2 and two in Series 3. After femoral canal preparation, a trial reduction determined the position of the implant at the neck cut. A guide wire for the tamp was inserted with the distal plug or into a preexisting plug, such as a bone pedestal or old cement plug. Bone graft was then progressively introduced in the femoral canal and impacted with the tamp to build a bone graft mantle. The stem, with a wingless stem centralizer, was cemented in place by retrograde insertion of hand-mixed Simplex® antibiotic cement (Howmedica International, Staines, UK; Stryker UK, Newbury, UK) with a gun, a proximal seal, and cement pressurization.
Collarless double-taper polished stems used were the stainless steel Exeter™ (Stryker Howmedica Osteonics, Berkshire, UK) modular stem in the first 24 hips. Stainless steel CPT® stems (Zimmer) were used in eight hips and the cobalt-chrome CPT® modular stem (Zimmer) in the last 24 hips (Fig. 1). Twelve long-length CPT® stems were used. The acetabular component was revised to an uncemented PCA™ (Howmedica) component in eight cases, an uncemented Vitalock™ component (Howmedica) in 15 cases, an uncemented Trilogy® component (Zimmer) in 15 cases, an uncemented Trabecular Metal™ component (Zimmer) in one case, and a cemented ZCA® (Zimmer) in one case. In 16 hips, the acetabular liner was exchanged only. All patients received prophylactic antibiotics and were mobilized postoperatively on Day 1, with partial weightbearing of 10 to 15 kg for the first 6 weeks progressing to full weightbearing over the next 6 weeks.
Scheduled clinical reviews were at 3, 6, and 12 months and then 2 to 3 yearly thereafter. No patients were recalled specifically for this study. Eight patients in Series 1 (35%), one patient in Series 2 (8%), and two patients in Series 3 (10%) have died. One patient each in Series 1 (4%) and Series 3 (5%) died within 2 years of IBG. One patient in Series 1 was lost to followup at 8 years after emigration. One patient in Series 3 was lost to followup after hospital discharge. One patient in Series 1 refused further followup after a postoperative periprosthetic fracture at 11 months, but the clinical status of this patient was known. Subsidence data at 1 year or longer were available for 18, 11, and 15 hips in Series 1, 2, and 3, respectively. After excluding deaths, rerevisions, and loss to followup, the clinical status of 10, 9, and 19 hips in Series 1, 2, and 3, respectively, were known. Due to age, distance to be traveled, or comorbidity, telephone interview was used to determine the survival status of three, one, and no hips in Series 1, 2, and 3, respectively, at latest followup. The mean clinical followup time of patients surviving more than 2 years was 10 years (median, 12 years; range, 2–15 years), 7 years (median, 7 years; range, 2–10 years), and 3 years (median, 2 years; range, 2–5.5 years) in Series 1, 2, and 3, respectively.
Radiographs were taken at the time of clinic review. Total stem subsidence (prosthesis-bone) and subsidence at the prosthesis-cement and cement-bone interfaces were measured using Ein Bild Röntgen Analyse (EBRA) (EBRA-Digital software; University of Innsbruck, Innsbruck, Austria) software using digitized radiographs. EBRA was performed on AP hip radiographs or, where these were inadequate, on AP pelvis radiographs by one independent investigator who was not a treating surgeon (SAC). The use of EBRA in femoral component migration analysis has a reported accuracy of 1.5 mm and Cronbach’s coefficient alpha for interobserver reliability of 0.84 [3, 4]. The method had a specificity of 100% and a sensitivity of 78% compared with RSA for the detection of migration of over 1 mm [3]. Stem subsidence at 1 year between the three series were compared using the nonparametric Kruskal-Wallis test and the Dunn’s post-test using GraphPad Prism® software (Version 4.01; GraphPad Software Inc, San Diego, CA). Radiographic loosening was assessed at latest radiographic review using the criteria of Harris et al. [17] by one investigator who was not a treating surgeon (NCR).
Results
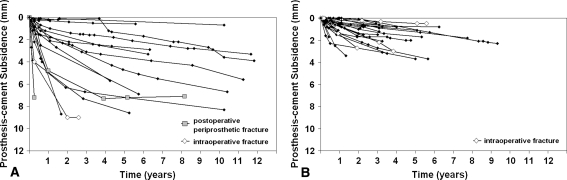
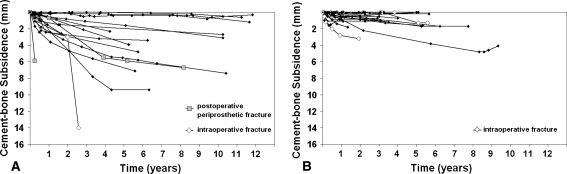
Total stem subsidence (p < 0.001) and subsidence at the prosthesis-cement interface (p < 0.05) and cement-bone interface (p < 0.01) at 12 months were greater for hips in Series 1 than for hips in Series 2 (Table 2). Similarly, total stem subsidence (p < 0.001) and subsidence at the prosthesis-cement interface (p < 0.05) and cement-bone interface (p = 0.05) at 12 months were greater for hips in Series 1 than for hips in Series 3 (Table 2). There were no differences in total, prosthesis-cement, or cement-bone subsidence at 12 months between hips in Series 2 and 3. Subsidence at the prosthesis-cement interface progressed over time in all series (Fig. 3). Three surviving hips that had an intraoperative or postoperative fracture and four other hips in Series 1 subsided in the cement by more than 5 mm at up to 2 years (Fig. 3). The maximum prosthesis-cement subsidence in the three hips with intraoperative fracture in Series 2 or 3 at 2 years was 2.7 mm. Excluding the hips in Series 1 rerevised for aseptic loosening or infection, five hips in Series 1 and no hips in Series 2 and 3 were definitely loose at latest review, defined as subsiding greater than 5 mm at the cement-bone interface (Fig. 4). In Series 2 and 3, cement-bone subsidence was minimal at 12 months, and for the majority of stems, subsidence remained at less than 1 mm over the period of implantation (Fig. 4). No hips were classified as possibly or probably loose at latest radiographic followup.
Table 2.
Rerevisions, complications, stem subsidence, and Harris pain and hip scores
| Series | Number of hips | Stem rerevision for | Vancouver A or B postoperative fracture | Subsidence (mm) at 12 months* | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Aseptic loosening | Infection | Prosthesis-bone interface | P value† | Prosthesis-cement interface | P value† | Cement-bone interface | P value† | |||
| 1 | 23 | 4 | 1 | 3 | 4.1 (0.3–13.1)‡ | 1v2 < 0.001 | 2.1 (0.1–7.2)‡ | 1v2 < 0.05 | 1.3 (0–5.9)‡ | 1v2 < 0.01 |
| 2 | 12 | 0 | 1 | 0 | 1.0 (0–1.6) | 2v3 > 0.05 | 0.5 (0–2.5) | 2v3 > 0.05 | 0.1 (0–0.9) | 2v3 > 0.05 |
| 3 | 21 | 0 | 0 | 0 | 0.8 (0–4.2) | 1v3 < 0.001 | 0.7 (0–1.6) | 1v3 < 0.05 | 0.1 (0–1.8) | 1v3 < 0.05 |
* Values are expressed as median, with range in parentheses; †nonparametric Kruskal-Wallis test; ‡excludes cases revised for loosening.
Fig. 3A–B.
Graphs show stem subsidence at the prosthesis-cement interface, measured by EBRA, for unrevised hips at last followup from (A) Series 1 and (B) Series 2 and 3. Cases of intraoperative and postoperative periprosthetic fracture are identified. (A) In Series 1, the extent of stem subsidence at the prosthesis-cement interface is variable and progresses over time and, in nearly 1/2 of the hips, exceeds 5 mm. (B) In contrast, in Series 2 and 3, the extent of subsidence at the prosthesis-cement interface is more consistent between hips. While there is some progression of subsidence over time, no hips exceed 5 mm of subsidence at latest followup.
Fig. 4A–B.
Graphs of stem subsidence at the cement-bone interface, measured by EBRA, for (A) Series 1 and (B) Series 2 and 3. Cases of intraoperative and postoperative periprosthetic fracture are identified. (A) In Series 1, the extent of stem subsidence at the cement-bone is variable and, in the majority of hips, exceeds 1 mm. (B) In contrast, in Series 2 and 3, the cement-bone subsidence data are more consistent between hips, and for the majority of hips, subsidence was less than 1 mm over the followup period.
Major stem rerevision involving removal of stem and cement was required due to stem loosening in four hips at 14, 22, 32, and 41 months after IBG. At the time of index femoral IBG, an extended trochanteric osteotomy was required to extract an ingrown stem in one hip and a second hip had an intraoperative diaphyseal fracture. Subsidence at the prosthesis-cement interface at 12 months for these hips were 4.1, 1.2, 0, and 3 mm (median, 2.1 mm), respectively. Subsidence at the cement-bone interface at 12 months were 0, 10.9, 14.7, and 35 mm (median, 12.8 mm), respectively. One hip in Series 1 underwent major rerevision for infection at 10 months. In one hip, cement-within-cement stem exchange was performed to assist with the revision of a loose acetabular component at 12 years. In Series 2, there has been one major stem revision for infection at 61 months. There have been no stem revisions in Series 3. Two periprosthetic Vancouver B1 fractures occurred postoperatively in hips in Series 1. Both fractures were sustained at 11 weeks and were treated with open reduction internal fixation without stem revision. One Vancouver A fracture occurred in Series 1 at 8 years, after multiple dislocations, and was managed nonoperatively. In Series 2 and 3, there were no postoperative periprosthetic fractures. One or more dislocations occurred in four hips, two hips, and no hips in Series 1, 2, and 3, respectively.
Discussion
Despite stem subsidence being a major complication of femoral impaction bone grafting in cemented revision hip arthroplasty, few studies have distinguished subsidence at the prosthesis-cement interface from that at the cement-bone interface. Due to the site of subsidence not being adequately reported, it is unknown how technique developments aimed at improving the procedure influence stability of the stem. We, therefore, used a sensitive measurement technique to compare femoral stem subsidence at the prosthesis-cement and cement-bone interfaces among three consecutive series of rTHAs performed with femoral IBG, with each series being defined by technique developments. We also determined the prevalence of postoperative periprosthetic diaphyseal fracture, radiographic loosening, and complications requiring further surgery to evaluate whether developments in technique were associated with a reduction in these complications.
This study has several limitations. First, the prospective series are small and heterogeneous. Despite each series being defined by distinct technical changes that aimed to improve early graft and implant stability, normal variations in patient and clinical characteristics existed within and across series, which may have confounded the subsidence and complications results. These include the instrumentation used, the need for femoral osteotomy, diagnosis, and the use of long-length stems, proximal calcar mesh, and prophylactic cerclage. The differences in patterns of subsidence and the prevalence of complications cannot, therefore, be attributed definitively to the defined technique changes. Second, as a low frequency procedure, learning curve effects may have also been important, particularly in Series 1 as a new procedure. Ornstein et al. [30], in their study of 1305 IBG procedures, attributed their finding that year of implantation predicted rerevision to both learning curve and technique improvements. Third, we acknowledge recent studies report subsidence of the polished double-taper stem in IBG using RSA, which has superior accuracy over EBRA [21, 29, 42] (Table 3). The latter relies on manual identification of bone landmarks, which contributes to its inferior accuracy compared with RSA. RSA was, however, not available for Series 1 and 2. Fourth, the length of followup is not equal among groups. Although rerevisions occurred at up to 4 years in Series 1, these failures were evident radiographically or clinically by 12 months. These features have not been observed in Series 2 and 3 by 12 months.
Table 3.
Literature review of subsidence of cemented collarless double-taper stems 12 months after impaction bone grafting and after primary THA
| Study | Cemented collarless double taper stem, (technique) | Number of hips | Method | Subsidence at 12 months (mm)* | ||
|---|---|---|---|---|---|---|
| Total (prosthesis-bone) | Prosthesis-cement | Cement-bone | ||||
| Howie et al. [current study] | Exeter (irradiated) | 16 | EBRA | 4.4 (2.8–6.0) | 2.9 (1.7–4.1) | 1.6 (0.8–2.5) |
| Exeter/CPT (nonirradiated, washed) | 12 | EBRA | 0.9 (0.6–1.2) | 0.8 (0.3–1.3) | 0.3 (0.1–0.5) | |
| CPT (modular tamp) | 17 | EBRA | 1.2 (0.6–1.8) | 0.8 (0.5–1.0) | 0.4 (0.2–0.7) | |
| Wraighte and Howard [43] | Exeter (nonirradiated) | 38 | Manual | 2.0† (1.0–3.0)‡ | ||
| Ornstein et al. [29] | Exeter (nonirradiated, washed) | 15 | RSA | 2.3§ | ||
| van Doorn et al. [42] | Exeter (nonirradiated) | 11 | RSA | 1.3 (0.8–2.2)‖ | ||
| Alfaro-Adrian et al. [1] | Exeter Primary THA | 14 | RSA | 1.1 (0.8–1.4) | 0§ | |
| Stefánsdottir et al. [37] | Exeter Primary THA | 14 | RSA | 1.2† (1.0–1.5) | 0.02† (−0.1– 0.1) | |
* Values are expressed as mean, with 95% confidence interval in parentheses, except where noted; †median; ‡interquartile range; §estimate from graph; ‖range; EBRA = Ein Bild Röntgen Analyse; RSA = radiostereometric analysis.
Using sensitive measures of stem subsidence that distinguish movement at the prosthesis-cement and cement-bone interfaces, our data suggest evolution in the technique of femoral IBG is associated with reductions in total stem subsidence and subsidence at both the prosthesis-cement and cement-bone interfaces. In Series 3, the consistent stem subsidence data and the minimal complications of Series 2 were maintained after the introduction of modular impaction tamps. What have historically been the main complications of femoral IBG at rTHA, early gross subsidence leading to rerevision and postoperative periprosthetic diaphyseal fracture seen in Series 1, did not occur in Series 2 and 3.
Adequate stem fixation at the prosthesis-cement and cement-bone interfaces has now been achieved when modern techniques of IBG are used. The range of total subsidence values at 1 year, reported for Series 2 and 3, compares closely to the 0.8 to 2.2 mm, determined by RSA, reported by van Doorn et al. [42] and is slightly lower than the values reported by Ornstein et al. [29] (Table 3). The pattern of stem fixation achieved is also comparable to that reported for primary THA using the same stem design [1, 37] (Table 3). Most of the subsidence occurred at the prosthesis-cement interface and is comparable to the 1 to 2 mm of self-limiting subsidence reported for primary stems which have 100% survival with revision of the stem for aseptic loosening at ten years’ follow-up (Table 3) [1, 44]. The amount of subsidence at the prosthesis-cement interface is also comparable for cement-alone rTHA with the same stem design [20]. As also reported by Ornstein et al. [29] using RSA, subsidence at the prosthesis-cement interface continued to progress after 1 year and up to 5 years, albeit minimally in Series 2 and 3 without complication. Despite the majority of unrevised hips in Series 1 subsiding more than 1.5 mm at the cement-bone interface by 1 year, they remained unrevised at latest followup. These include the hips with intraoperative fractures and those radiographically defined as definitely loose. These findings agree with the results of Yim et al. [45] who found femoral fracture and early subsidence in their series of 56 hips with femoral IBG did not necessarily lead to failure at an average of 39 months’ followup. For the majority of stems in Series 2 and 3, cement-bone subsidence was less than 2 mm at 12 months and at up to a maximum of 8 years. The stability of this subsidence data is consistent with the findings of Wraighte and Howard [43], in their review of 75 IBG hips, showing excellent fixation at 1 year was maintained with longer-term followup for the majority of hips.
In Series 1, two of the 23 patients had a postoperative periprosthetic diaphyseal fracture. This compares to a rate reported in previous studies of femoral IBG [25, 32] but is markedly higher than the 0.5% reported for standard rTHA using a cemented collarless double-taper stem and no IBG [20]. Both fractures in Series 1 occurred at 11 weeks postoperatively, during the period when patients are transitioning from partial weightbearing to full weightbearing. With modification of technique in Series 2 and 3 aimed at achieving a stronger stem-graft-bone construct and more frequent use of prophylactic cerclage and long stems, there were no cases of postoperative periprosthetic fracture.
Our data show developments in techniques of femoral IBG are associated with reduced subsidence of the femoral stem at both the prosthesis-cement and cement-bone interface. Subsidence after rTHA with IBG are now similar to those reported for primary THA using the cemented collarless double-taper stem. Associated with this minimal subsidence is a reduction in postoperative mechanical complications requiring further surgery.
Acknowledgments
We thank Dr Roumen Stamenkov, Allograft Bone Fellow; Professor Stephen Graves and Mr Andrew Mintz, Consulting Surgeons; and Sue Pannach for assisting with patient review.
Footnotes
One or more of the authors (DWH) have received research funding from Zimmer Inc (Warsaw, IN).
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with the ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at the Royal Adelaide Hospital.
References
- 1.Alfaro-Adrian J, Gill HS, Murray DW. Cement migration after THR: a comparison of Charnley Elite and Exeter femoral stems using RSA. J Bone Joint Surg Br. 1999;81:130–134. doi: 10.1302/0301-620X.81B1.8904. [DOI] [PubMed] [Google Scholar]
- 2.Barker R, Takahashi T, Toms A, Gregson P, Kuiper JH. Reconstruction of femoral defects in revision hip surgery: risk of fracture and stem migration after impaction bone grafting. J Bone Joint Surg Br. 2006;88:832–836. doi: 10.2106/JBJS.D.02834. [DOI] [PubMed] [Google Scholar]
- 3.Biedermann R, Krismer M, Stockl B, Mayrhofer P, Ornstein E, Franzen H. Accuracy of EBRA-FCA in the measurement of migration of femoral components of total hip replacement: Einzel-Bild-Röntgen-Analyse-femoral component analysis. J Bone Joint Surg Br. 1999;81:266–272. doi: 10.1302/0301-620X.81B2.8842. [DOI] [PubMed] [Google Scholar]
- 4.Biedermann R, Stockl B, Krismer M, Mayrhofer P, Ornstein E, Franzén H. Evaluation of accuracy and precision of bone markers for the measurement of migration of hip prostheses: a comparison of conventional measurements. J Bone Joint Surg Br. 2001;83:767–771. doi: 10.1302/0301-620X.83B5.10575. [DOI] [PubMed] [Google Scholar]
- 5.Brewster NT, Gillespie WJ, Howie CR, Madabhushi SP, Usmani AS, Fairbairn DR. Mechanical considerations in impaction bone grafting. J Bone Joint Surg Br. 1999;81:118–124. doi: 10.1302/0301-620X.81B1.8480. [DOI] [PubMed] [Google Scholar]
- 6.Cabanela ME, Trousdale RT, Berry DJ. Impacted cancellous graft plus cement in hip revision. Clin Orthop Relat Res. 2003;417:175–182. doi: 10.1097/01.blo.0000096817.78689.ac. [DOI] [PubMed] [Google Scholar]
- 7.Dunlop DG, Brewster NT, Madabjushi SP, Usmani AS, Pankaj P, Howie CR. Techniques to improve the shear strength of impacted bone graft. J Bone Joint Surg Am. 2003;85:639–646. doi: 10.2106/00004623-200304000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Edwards SA, Pandit HG, Grover ML, Clarke HJ. Impaction bone grafting in revision hip surgery. J Arthroplasty. 2003;18:852–859. doi: 10.1016/S0883-5403(03)00281-X. [DOI] [PubMed] [Google Scholar]
- 9.Eldridge JD, Smith EJ, Hubble MJ, Whitehouse SL, Learmonth ID. Massive early subsidence following femoral impaction grafting. J Arthroplasty. 1997;12:S35–S40. doi: 10.1016/S0883-5403(97)90176-5. [DOI] [PubMed] [Google Scholar]
- 10.Elting JJ, Mikhail WE, Zicat BA, Hubbell JC, Lane LE, House B. Preliminary report of impaction grafting for exchange femoral arthroplasty. Clin Orthop Relat Res. 1995;319:159–167. [PubMed] [Google Scholar]
- 11.Engelbrecht E, Heinert K. Klassifikation und Behandlungsricgtlinien von Knochensubstanzverlusten bei Revisionsoperationen am Hüftgelenk-mittelfristige Ergebnisse. Primär und Revisionsalloarthroplastik Hüft und Kniegelank. Berlin, Germany: Springer-Verlag; 1987:189–201.
- 12.Farfalli GL, Buttaro MA, Piccaluga F. Femoral fractures in revision hip surgeries with impacted bone allograft. Clin Orthop Relat Res. 2007;462:130–136. doi: 10.1097/BLO.0b013e318137968c. [DOI] [PubMed] [Google Scholar]
- 13.Fowler JL, Gie GA, Lee AJ, Ling RS. Experience with the Exeter total hip replacement since 1970. Orthop Clin North Am. 1988;19:477–489. Erratum in: Orthop Clin North Am. 1989;20:preceding 519. [PubMed]
- 14.Gie GA, Linder L, Ling RS, Simon JP, Slooff TJ, Timperley AJ. Impacted cancellous allografts and cement for revision total hip arthroplasty. J Bone Joint Surg Br. 1993;75:14–21. doi: 10.1302/0301-620X.75B1.8421012. [DOI] [PubMed] [Google Scholar]
- 15.Gokhale S, Soliman A, Dantas JP, Richardson JB, Cook F, Kuiper JH, Jones P. Variables affecting initial stability of impaction grafting for hip revision. Clin Orthop Relat Res. 2005;432:174–180. doi: 10.1097/01.blo.0000150103.75134.10. [DOI] [PubMed] [Google Scholar]
- 16.Halliday BR, English HW, Timperley AJ, Gie GA, Ling RS. Femoral impaction grafting with cement in revision total hip replacement. J Bone Joint Surg Br. 2003;85:809–817. [PubMed] [Google Scholar]
- 17.Harris WH, McCarthy JC, O’Neil DA. Femoral component loosening using contemporary techniques of femoral cement fixation. J Bone Joint Surg Am. 1982;64:1063–1067. [PubMed] [Google Scholar]
- 18.Hassaballa M, Mehendale S, Poniatowski S, Kalantzis G, Smith E, Learmonth ID. Subsidence of the stem after impaction bone grafting for revision hip replacement using irradiated bone. J Bone Joint Surg Br. 2009;91:37–43. doi: 10.1302/0301-620X.91B1.20376. [DOI] [PubMed] [Google Scholar]
- 19.Höstner J, Hultmark P, Kärrholm J, Malchau H, Tveit M. Impaction technique and graft treatment in revisions of the femoral component: laboratory studies and clinical validation. J Arthroplasty. 2001;16:76–82. doi: 10.1054/arth.2001.9830. [DOI] [PubMed] [Google Scholar]
- 20.Howie DW, Wimhurst JA, McGee MA, Carbone TA, Badaruddin BS. Revision total hip replacement using cemented collarless double-taper femoral components. J Bone Joint Surg Br. 2007;89:879–886. doi: 10.2106/JBJS.E.01305. [DOI] [PubMed] [Google Scholar]
- 21.Karrholm J, Hultmark P, Carlsson L, Malchau H. Subsidence of a non-polished stem in revisions of the hip using impaction allograft: evaluation with radiostereometry and dual-energy x-ray absorptiometry. J Bone Joint Surg Br. 1999;81:135–142. doi: 10.1302/0301-620X.81B1.8922. [DOI] [PubMed] [Google Scholar]
- 22.Mahoney CR, Fehringer EV, Kopjar B, Garvin KL. Femoral revision with impaction grafting and a collarless, polished, tapered stem. Clin Orthop Relat Res. 2005;432:181–187. doi: 10.1097/01.blo.0000150320.73465.82. [DOI] [PubMed] [Google Scholar]
- 23.Malchau H, Kärrholm J, Wang YX, Herberts P. Accuracy of migration analysis in hip arthroplasty: digitized and conventional radiography, compared to radiostereometry in 51 patients. Acta Orthop Scand. 1995;66:418–424. doi: 10.3109/17453679508995578. [DOI] [PubMed] [Google Scholar]
- 24.Masterson EL, Masri BA, Duncan CP. The cement mantle in the Exeter impaction allografting technique: a cause for concern. J Arthroplasty. 1997;12:759–764. doi: 10.1016/S0883-5403(97)90005-X. [DOI] [PubMed] [Google Scholar]
- 25.Meding JB, Ritter MA, Keating EM, Faris PM. Impaction bone-grafting before insertion of a femoral stem with cement in revision total hip arthroplasty: a minimum two-year follow-up study. J Bone Joint Surg Am. 1997;79:1834–1841. doi: 10.2106/00004623-199712000-00009. [DOI] [PubMed] [Google Scholar]
- 26.Nelson IW, Bulstrode CJ, Mowat AG. Femoral allografts in revision of the hip replacement. J Bone Joint Surg Br. 1990;72:151–152. doi: 10.1302/0301-620X.72B1.2298782. [DOI] [PubMed] [Google Scholar]
- 27.Nivbrant B, Kärrholm J, Röhrl S, Hassander H, Wesslén B. Bone cement with reduced proportion of monomer in total hip arthroplasty: preclinical evaluation and randomized study of 47 cases with 5 years’ follow-up. Acta Orthop Scand. 2001;72:572–584. doi: 10.1080/000164701317268987. [DOI] [PubMed] [Google Scholar]
- 28.Oakley J, Kuiper JH. Factors affecting the cohesion of impaction bone graft. J Bone Joint Surg Br. 2006;88:828–831. doi: 10.1302/0301-620X.88B6.17278. [DOI] [PubMed] [Google Scholar]
- 29.Ornstein E, Franzen H, Johnsson R, Karlsson MK, Linder L, Sundberg M. Hip revision using the Exeter stem, impacted morselized allograft bone and cement: a consecutive 5-year radiostereometric and radiographic study in 15 hips. Acta Orthop Scand. 2004;75:533–543. doi: 10.1080/00016470410001385. [DOI] [PubMed] [Google Scholar]
- 30.Ornstein E, Linder L, Ranstam J, Lewold S, Eisler T, Torper M. Femoral impaction bone grafting with the Exeter stem—the Swedish Experience: survivorship analysis of 1305 revisions performed between 1989 and 2002. J Bone Joint Surg Br. 2009;91:441–446. doi: 10.1302/0301-620X.91B4.21319. [DOI] [PubMed] [Google Scholar]
- 31.Panjabi MM, Trumble T, Hult E, Southwick WO. Effect of femoral stem length on stress raisers associated with revision hip arthroplasty. J Orthop Res. 1985;3:447–455. doi: 10.1002/jor.1100030407. [DOI] [PubMed] [Google Scholar]
- 32.Pekkarinen J, Alho A, Lepisto J, Ylikoski M, Ylinen P, Paavilainen T. Impaction bone grafting in revision hip surgery: a high incidence of complications. J Bone Joint Surg Br. 2000;82:103–107. doi: 10.1302/0301-620X.82B1.9802. [DOI] [PubMed] [Google Scholar]
- 33.Robinson DE, Lee MB, Smith EJ, Learmonth ID. Femoral impaction grafting in revision hip arthroplasty with irradiated bone. J Arthroplasty. 2002;17:834–840. doi: 10.1054/arth.2002.34533. [DOI] [PubMed] [Google Scholar]
- 34.Schreurs BW, Arts JJ, Verdonschot N, Buma P, Slooff TJ, Gardeniers JW. Femoral component revision with use of compaction bone-grafting and a cemented polished stem. J Bone Joint Surg Am. 2005;87:2499–2507. doi: 10.2106/JBJS.D.02547. [DOI] [PubMed] [Google Scholar]
- 35.Sierra RJ, Charity J, Tsiridis E, Timperley JA, Gie GA. The use of long cemented stems for femoral impaction grafting in revision total hip arthroplasty. J Bone Joint Surg Am. 2008;90:1330–1336. doi: 10.2106/JBJS.G.00055. [DOI] [PubMed] [Google Scholar]
- 36.Simon JP, Fowler JL, Gie GA, Ling RS, Timperley AJ.Impaction cancellous grafting of the femur in cemented total hip revision arthroplasty J Bone Joint Surg Br 199173Suppl 1731991780 [Google Scholar]
- 37.Stefánsdőttir A, Franzén H, Johnsson R, Ornstein E, Sundberg M. Movement pattern of the Exeter stem: a radiostereometric analysis of 22 primary hip arthroplasties followed for 5 years. Acta Orthop Scand. 2004;75:408–414. doi: 10.1080/00016470410001169-1. [DOI] [PubMed] [Google Scholar]
- 38.Thanner J, Freij-Larsson C, Kärrholm J, Malchau H, Wesslén B. Evaluation of Boneloc. Chemical and mechanical properties, and a randomized clinical study of 30 total hip arthroplasties. Acta Orthop Scand. 1995;66:207–214. doi: 10.3109/17453679508995525. [DOI] [PubMed] [Google Scholar]
- 39.Toms AD, Barker RL, Jones RS, Kuiper JH. Impaction bone-grafting in revision joint replacement surgery. J Bone Joint Surg Am. 2004;86:2050–2060. doi: 10.2106/00004623-200409000-00028. [DOI] [PubMed] [Google Scholar]
- 40.Ullmark G. Bigger size and defatting of bone chips will increase cup stability. Arch Orthop Trauma Surg. 2000;120:445–447. doi: 10.1007/s004029900122. [DOI] [PubMed] [Google Scholar]
- 41.Biezen FC, ten Have BL, Verhaar JA. Impaction bone-grafting of severely defective femora in revision total hip surgery: 21 hips followed for 41–85 months. Acta Orthop Scand. 2000;71:135–142. doi: 10.1080/000164700317413094. [DOI] [PubMed] [Google Scholar]
- 42.Doorn WJ, ten Have BL, Biezen FC, Hop WC, Ginai AZ, Verhaar JA. Migration of the femoral stem after impaction bone grafting: first results of an ongoing, randomised study of the Exeter and Elite Plus femoral stems using radiostereometric analysis. J Bone Joint Surg Br. 2002;84:825–831. doi: 10.1302/0301-620X.84B6.13004. [DOI] [PubMed] [Google Scholar]
- 43.Wraighte PJ, Howard PW. Femoral impaction bone allografting with an Exeter cemented collarless, polished, tapered stem in revision hip replacement: a mean follow-up of 10.5 years. J Bone Joint Surg Br. 2008;90:1000–1004. doi: 10.1302/0301-620X.90B8.20390. [DOI] [PubMed] [Google Scholar]
- 44.Yates PJ, Burston BJ, Whitley E, Bannister GC. Collarless polished tapered stem. Clinical and radiological results at a minimum of ten years’ follow-up. J Bone Joint Surg Br. 2008;90:16–22. doi: 10.1302/0301-620X.90B1.19546. [DOI] [PubMed] [Google Scholar]
- 45.Yim SJ, Kim MY, Suh YS. Impaction allograft with cement for the revision of the femoral component: a minimum 39-month follow-up study with the use of the Exeter stem in Asian hips. Int Orthop. 2007;31:297–302. doi: 10.1007/s00264-006-0201-0. [DOI] [PMC free article] [PubMed] [Google Scholar]