Abstract
Background
THA performed in patients with cognitive deficits or neuromuscular diseases has been associated with a high postoperative dislocation rate. The constrained liner reportedly provides stability in patients with recurrent dislocation. However, achieving stability could be offset by early loosening when used in patients with neurologic diseases.
Questions/purposes
We therefore asked whether constrained liners had a higher risk of loosening when used in primary THA for patients with neurologic diseases.
Methods
We retrospectively reviewed a 144 patients (164 hips) with neuromuscular disease who had a constrained polyethylene insert from 1999 to 2004 and compared them to another 120 patients (132 hips) with neuromuscular disease operated on immediately before this period (from 1994 to 1998) who had a conventional polyethylene insert.
Results
Thirty-three (25%) of the 132 hips without a constrained liner were known to have had at least one dislocation and 21 had revision for recurrent dislocation. Ten other hips had revision for loosening of the cup. The survival rate was 82% at 5 years and 77% at 10 years with revision due to recurrent dislocation or loosening of the cup as the endpoint. With a constrained liner, at minimum 5-year followup (mean, 7 years; range, 5–10 years), the incidence of complications, particularly dislocation, was decreased (three dislocations among 164 hips; 2%), with one revision for recurrent dislocation and one revision for loosening.
Conclusions
This constrained acetabular component provides durable protection against dislocation without substantial increased loosening at midterm followup.
Level of Evidence
Level III, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
THA relieves pain and reduces disability in patients with hip disorders. However, conventional THA performed in patients with cognitive deficits or neuromuscular diseases (NMDs) has been associated with high postoperative dislocation rates from 5% to 20% according to the neurologic disease [10, 16, 26]. These neuromuscular conditions can be divided into three categories: those with decreased muscle tone (eg, poliomyelitis, Down syndrome, and myelomeningocele); those with increased muscle tone as well as contractures or movement disorders (eg, cerebral palsy, Parkinson’s disease, stroke); and those not associated with change in muscle tone (eg, dementia, confusion, psychoses corresponding to cognitively impaired patients). Patients who are cognitively impaired or have NMD may need a THA for four general reasons: a disease process (eg, cerebral palsy) leading to dysplasia or subluxation resulting in degenerative joint disease; a degenerative joint disease independent of the neurologic condition (eg, Parkinson’s disease); a fracture associated with a neurologic condition such as stroke or Parkinson’s disease; or osteonecrosis related to corticosteroids.
Historically, braces and hip spica casts [15, 40] were utilized postoperatively or after dislocation, but they are not well tolerated in this population. One case report [6] has described the use of constrained liners in a patient with NMD. Most constrained liners are associated with an increased risk of loosening from 4% to 9% with a mean followup of 5 years according to the liner [42] and the risk of loosening with a standard liner is also increased in some neurologic diseases (e.g., Parkinson’s disease) from 3% to 4% with a mean followup of 5 years [10, 35]. Thus, achieving stability with a constrained cup could be at the cost of early loosening of the component. Whether these findings apply to patients with neurologically or cognitively impaired patients is unclear.
Therefore, we compared patients with cognitive impairment or NMD with and without constrained liners to determine whether (1) the incidence of dislocation differed between the two groups; (2) the incidence of loosening differed between the groups; and (3) the various types of hip diseases influenced dislocation or loosening.
Patients and Methods
We analyzed the incidence of dislocation, the incidence of loosening in patients with cognitive impairment or NMD with and without constrained liners. The cemented UHMWPE retentive cup (constrained liner; Groupe lépine, Genay, France) became available for use in January 1999 in our hospital. Since that time, it has been used consecutively in patients with cognitive impairment or NMD. We compared the first 144 of these patients receiving the constrained PE insert from 1999 to the end of 2004 with the 120 patients operated on immediately before this date (from 1994 to 1998) who received a conventional PE insert. From 1994 to 2004 eight surgeons performed 3124 THAs in the same hospital. Thus, 296 hip arthroplasties (32 bilateral) were performed in 264 patients (8.5% of the total) with cognitive deficits or NMDs. Of the 264 patients undergoing primary hip arthroplasties, 149 of the patients were cognitively impaired patients (Alzheimer’s, other forms of dementia, confusion, psychosis); 23 had decreased muscle tone (Down syndrome, poliomyelitis, myelomeningocele); 52 had increased muscle tone (Stage IV or V Parkinson’s disease); and 40 had stroke (condition associated with osteoarthritis, osteonecrosis, or neck fracture on the hemiplegic side) (Table 1). All patients experienced pain before surgery and were able to walk with or without crutches.
Table 1.
Clinical data of patients with neurologic disease (n = 264) (296 hips)*
| Neurologic disease | Dysplasia related to neurologic disease | Osteoarthritis not related to neurologic disease | Fracture | Osteonecrosis | ||||
|---|---|---|---|---|---|---|---|---|
| UL | CL | UL | CL | UL | CL | UL | CL | |
| Decreased muscle tone | ||||||||
| Poliomyelitis (n = 12) | 5 | 7 | ||||||
| Down syndrome (n = 6) | 2 | 4 | ||||||
| Myelomeningocele (n = 5) | 2 | 3 | ||||||
| Increased muscle tone | ||||||||
| Cerebral palsy (n = 4) | 2 | 2 | ||||||
| Parkinson’s (n = 42) | 7 | 15 | 8 | 12 | ||||
| Syringomyelia (n = 6) | 2 | 4 | ||||||
| Stroke (n = 40) | 18 | 22 | ||||||
| Cognitively impaired | ||||||||
| Dementia (n = 111) | 26 | 31 | 30 | 46 | ||||
| Confusion (n = 17) | 3 | 4 | 5 | 4 | ||||
| Psychosis (n = 21) | 5 | 3 | 4 | 4 | 5 | |||
* There were 164 constrained liners (CL) and 132 unconstrained liners (UL); some patients have bilateral arthroplasties.
The group without constrained liners consisted of 120 patients (132 hips; 60 men, 60 women) with an average age of 70 years (range, 21–92 years). The diagnosis was osteoarthritis in 59 hips, osteonecrosis in six hips, and neck fracture in 64 hips. All patients received a cemented arthroplasty (43 hemiarthroplasties for fractures, 89 standard THAs) performed between 1994 and 1998 in the same hospital. Twenty of the 120 patients died before 5-years followup; in addition, 17 of these patients (14%) were lost to followup after 2 years. The records were queried at the time of their most recent followup or before their death. The minimum followup from time of surgery for the living and available patients without a constrained liner was 10 years (mean, 12 years; range, 10–15 years). Surgery was performed with a posterolateral approach and general anesthesia. All stems were manufactured by Ceraver Osteal (Roissy, France); they were made of a smooth finish anodized titanium alloy (TiAl6V4). In all cases, both components were fixed with cement (Palacos® G; Heraeus Medical GmbH, Hanau, Germany) containing antibiotics (gentamicin). The conventional acetabular component was a standard PE cup manufactured by Ceraver and was always cemented. The alumina head was 32 mm in diameter and anchored through a Morse taper. Twenty-five of these 132 hips with unconstrained device had an adductor tenotomy.
The constrained liner group consisted of 144 patients (164 hips; 86 men, 58 women) with an average age of 67 years (range, 24–98 years). The diagnosis was osteoarthritis in 67 hips, osteonecrosis in nine hips, and neck fracture in 88 hips. All patients received a cemented THA performed between 1999 and 2004. Thirty patients died before 5-years followup and 25 of the 144 patients (17%) were lost to followup after 2 years. The minimum followup from time of surgery for the living and available patients with a constrained liner was 5 years (mean, 7 years; range, 5–10 years). Surgery in these patients was also performed with a posterolateral approach and general anesthesia. The stems were the same and all cemented. The cemented UHMWPE retentive cup (Groupe Lépine, Genay, France) is a novel design incorporating a mobile ring. The principle of retentiveness requires a more enveloping cup than the hemispheric model (Fig. 1). The flange in the equatorial plane permits insertion of a split PE ring reinforced by a stainless steel hoop. This ring plays the role of a retentive clip. On crossing the equator of the cup, the head opens the ring, which then closes through simple elasticity (Fig. 2). Once the head has crossed the ring, it can fall below the equatorial plane and the clip is closed against the enveloping part of the cup (Fig. 3). The internal part of the ring has two surfaces with the chamfered surface precisely fitting over the head sphere. The head can be inserted into the cup without difficulty (Fig. 4); less than 30 N (± 6 N) are required to successfully insert the head; however, dislocation needs 2153 N (± 32 N). The alumina head was 28 mm in diameter and anchored through a Morse taper. The theoretical maximum mobility of the device is 122 degrees. Twenty- eight of these 164 hips with constrained device had an adductor tenotomy.
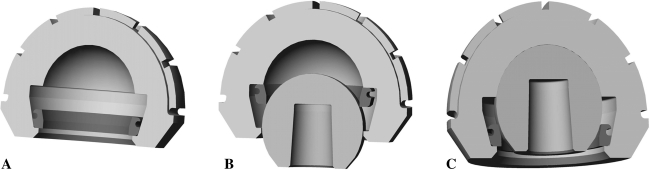
Fig. 1A–B.
(A) A photograph and (B) diagram illustrate the retentive cup. The principle of retentiveness is obtained with a more enveloping cup than the hemispheric model. The flange in the equatorial plane permits insertion of a split PE ring reinforced by a stainless steel hoop.
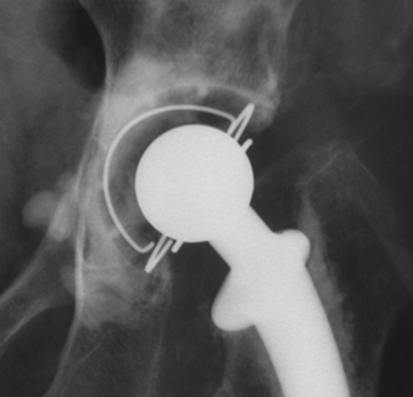
Fig. 2A–C.
(A) The cup without the head is shown. (B) On crossing the equator of the cup, the head opens the ring, (C) which then closes through simple elasticity.
Fig. 3.
Once the head has crossed the ring, it falls below the equatorial plane. Therefore, in most situations, the cup is not really a constrained liner. Only in movements at risk for dislocation is the ring constrained.
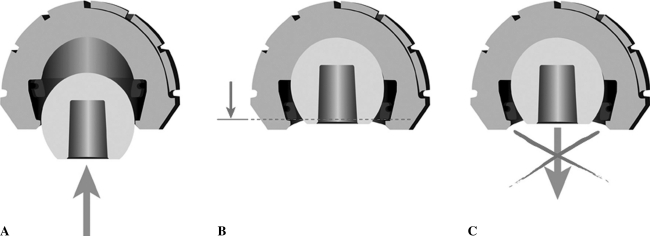
Fig. 4A–C.
(A) Disassembled head; (B) Assembled head. Less than 30 N (± 6 N) is required to successfully insert the head; (C) Dislocation requires 2153 N (± 32 N).
During postoperative rehabilitation, no patient was placed into a hip spica cast to minimize the possibility of hip dislocation. The patients were encouraged to be upright with weight bearing after surgery. Range of motion of the hip and knees was begun immediately and ambulation progressed as tolerated according to the ability of each patient (usually after 48 hours).The physiotherapy was supervised by a medical doctor for three weeks and continued for 45 days.
The followup routine time was at three, six, 12 months and then every year. At each visit, patients had clinical and radiological evaluation. No patients were recalled specifically for this study, the data for which was retrieved from the charts. The function of THA in patients with NMD is not well reflected by the usual hip-rating scores because many of the functional variables are substantially affected by the neurologic disease itself. Therefore the preoperative and postoperative pain was subjectively and retrospectively graded from the charts as severe, moderate, slight, and unknown. The preoperative and postoperative walking status of the patient was graded as unable to walk, able to walk indoors only, able to walk about the community, and able to walk an unlimited distance. All patients, except two with hip infection, subjectively exhibited improved ambulation (they were able to walk about the community, or able to walk an unlimited distance) and decreased pain (no pain or slight pain) after surgery. Plain radiographs (AP and lateral view) were taken to assess migration of the component, wear, and loosening every year until the most recent followup.
We had preoperative and immediate postoperative radiographs in all patients. Radiographs at last followup were available on 83 of the 120 patients with unconstrained implants and 89 of the 144 patients with constrained implants. Three of us (PH, PP, SUB) independently determined osteolysis and loosening [19] on all films. Absence of loosening of the socket was defined as no cup migration exceeding 5 mm, no angular rotation exceeding 5°, and no continuous radiolucent line wider than 2 mm [14] when comparing the immediate postoperative films to those at last followup. Cup position was assessed according to the acetabular position angle [30].
Qualitative data (ie, gender, preoperative diagnosis, and model of liner) are expressed as counts and percentages within groups and quantitative data by mean ± standard deviation or range. Qualitative data between the two groups were compared with use of the chi-square test or Fisher’s exact test, and quantitative data (postoperative acetabular abduction angle) with the Mann-Whitney test. Kaplan-Meier survivorship analysis [21], with 95% confidence intervals, was used to estimate the cumulative probability of not having a dislocation of the cup and to estimate the cumulative probability of not having cup loosening in the whole series. Differences in survival were determined using the log-rank test. The cumulative risk of dislocation as reported by Berry et al. [5] was estimated using the Kaplan-Meier method [21]. Kaplan-Meier survivorship analysis was performed with revision due to recurrent dislocation or loosening as the endpoint. Univariate relative risk estimates for age, gender, underlying neurologic diagnosis, and underlying hip disease were generated using the Cox proportional-hazards model and were adjusted for correlated data, that is, for two hips in patients who had undergone bilateral arthroplasties or had two neurologic diseases (eg, Parkinson’s and dementia).
Results
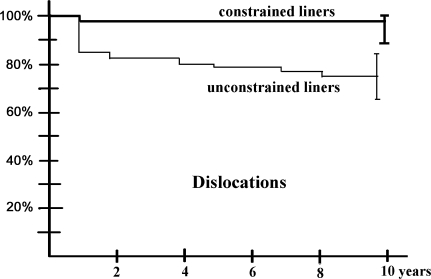
With a similar (p = 0.24) abduction acetabular angle in the two groups (mean angle 47° ± 8° in the standard group versus 49 ± 11°in the constrained group), the incidence of dislocation was reduced by the constrained liner (Fig. 5). With an unconstrained liner, 33 (25%) of the 132 hips were known to have had at least one dislocation. When the data were stratified according to treatment (hemiarthroplasty or THA), we found a similar (p = 0.16) risk of dislocation in patients with a THA versus hemiarthroplasty, and a trend (p = 0.074) toward a higher dislocation rate in patients with a too-vertical cup position when a THA was used. Thirteen first-time dislocations occurred within 60 days after arthroplasty, eight occurred 2 months to 12 months after arthroplasty, and 12 occurred 1 to 10 years after arthroplasty. Twenty patients (23 hips) had recurrent hip dislocation (more than two). Twenty-one hips had revision for this problem. The cumulative risk of dislocation for patients without constrained liner was 10% at 2 months and 16% at 1 year. The risk then rose at a constant rate of approximately 1% every year to 25% at 10 years for the surviving patients who had not had a revision by this followup. In the group of patients with a constrained liner at mean 7-year followup (range, 5–10 years), the incidence of dislocation was lower (p = 0.01) (three dislocations among 164 hips or 2%) than in the patients with a standard cup (33 dislocations among 132 hips or 25%) (Table 2). There was one head dissociation from the stem, and two dislocations without locking ring breakage. All these dislocations without locking ring breakage could be treated with closed reduction [20, 27], and this was also possible for the case with dissassemblage of the head from the Morse taper. One of these three patients had recurrent dislocation. No other patient had dislocation after 12 months’ followup. Two locking ring breakages were also observed but without dislocation and without revision.
Fig. 5.
Kaplan-Meier curves depicting failure as dislocation. The survival rate was lower (p = 0.006, log-rank test) in patients with unconstrained liners.
Table 2.
Dislocations, recurrent dislocations, and revisions in patients with unconstrained liners (n = 132) and with constrained liners (n = 164)
| Complications | Unconstrained liners | Constrained liners |
|---|---|---|
| One dislocation | 33 (25%) | 3 (2%) |
| Decreased muscle tone | 1 | 0 |
| Increased muscle tone | 10 | 0 |
| Cognitively impaired | 22 | 3 |
| Recurrent dislocation | 23 (17%) | 0 |
| Decreased muscle tone | 1 | 0 |
| Increased muscle tone | 6 | 0 |
| Cognitively impaired | 16 | 0 |
| Revision for dislocation | 21 (16%) | 1 (1%) |
| Decreased muscle tone | 0 | 0 |
| Increased muscle tone | 6 | 0 |
| Cognitively impaired | 15 | 1 |
| Revision for loosening | 10 (7%) | 1 (1%) |
| Decreased muscle tone | 0 | 0 |
| Increased muscle tone | 8 | 1 |
| Cognitively impaired | 2 | 0 |
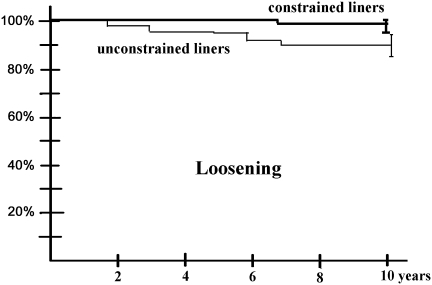
The survival rate was similar (p = 0.01) with an unconstrained and constrained implant: 100% at 5 years and 99% at 7 years with revision due to loosening of the constrained cup as the end point, compared with 95% at 5 years and 91% at 7 years in the unconstrained group (Fig. 6). In the patients with an unconstrained liner ten hips had revision for loosening of the cup. The abduction angle of the cup had no influence (p = 0.48) on this risk. Among patients with a constrained liner, one had loosening and the patient underwent revision 9 years after the original surgery. At the most recent followup, there was no progressive radiolucent line or osteolytic lesions observed that could be determined radiographically about the acetabular component or proximal femur.
Fig. 6.
Kaplan-Meier curves depicting failure as loosening. The survival rate was similar (p = 0.01, log-rank test) in patients with constrained and unconstrained liners.
The various types of hip diseases influenced dislocation or loosening. Two underlying hip diagnoses (osteonecrosis of the femoral head, acute fracture) were associated with a greater (p = 0.03) risk of dislocation than osteoarthritis in the group without constrained liner: the cumulative risk of dislocation at 10 years was 31% for patients with fracture of the femoral head, compared with 15% for patients with osteoarthritis (p = 0.01); the cumulative risk of dislocation was higher (p = 0.01) for patients who were cognitively impaired and for patients who had neurologic conditions associated with increased muscle tone (Table 2) compared with patients who had neurologic conditions associated with decreased muscle tone. The ten hips with revision of the cup for loosening were observed in patients with Parkinson’s disease, cerebral palsy, and stroke.
Discussion
Despite a general suggestion that there is a higher rate of dislocation and recurrent dislocation in patients with NMDs [36, 41], there is very little literature about the frequency of this problem and about the methods to avoid it. Therefore, we compared patients with cognitive impairment or NMD with and without constrained liners to determine in the two groups the incidence of dislocation, of loosening, and the influence of the various types of hip diseases.
Several limitations must be considered when interpreting the presented data. First, ours was a retrospective study of a nonrandomized patient population. The two different procedures were performed at two different periods of time, although the surgeons were the same and generally used the same approaches and same perioperative treatments except for the liner. Second, the head size used in the different groups was different: hemiarthroplasties with large femoral heads or 32 mm diameter heads in the unconstrained group, and 28 mm diameter heads in the group with constrained liners; however this difference is not really a problem since the 28 mm diameter heads are perhaps a little more prone to dislocation. Third, some patients were lost to followup during this study; other died. It is possible some patients had unknown dislocation treated in another hospital and not related because of the status of cognitively impaired patients. Fourth, the size of our population is small concerning some neurologic diseases. However we did include all patients admitted during a long period and the total number of patients is relatively large despite small subcohorts. Finally, we have only midterm followup on these patients, and shorter followup in those with constrained liners owing to more recent availability of the implants. We cannot say whether the differences in loosening rates will emerge longer term.
We retrospectively reviewed the clinical and radiographic outcomes of 296 consecutive hip arthroplasties performed in patients with cognitive deficits or neurologic diseases during a 10-year period; during the same 10-year period, the total number of hip arthroplasties performed in the same hospital was 3124. The frequency of patients with THAs who have diagnoses of stroke, Parkinson’s disease, or confusion and dementia and other neurologic diseases is higher than expected. One report [26] has demonstrated a rate of 10% or more and our data (296 with NMDs among 3124 hips) are consistent with this observation. In our experience as in other reports [10], the risk of dislocation remains high with conventional liners (Table 3) with the posterolateral or trochanteric approach. We do not know whether the anterolateral operative approaches currently used more commonly by some surgeons would have changed the risk of dislocation. We also do not know whether the high cumulative probability of dislocation reported here would have been the same for these patients if they had received implants with the larger femoral head sizes [3, 9, 22] now in common use; we can only remark the risk of dislocation was not reduced in our experience with hemiarthroplasties when they were used. Although it has become clear there is markedly decreased dislocation when constrained liners are used for the treatment of recurrent dislocation in THA [32–34] as compared with other solutions [13, 28, 29, 36], no analysis has been conducted using constrained liners in the prevention of dislocation in patients with NMDs, except (to our knowledge) one case report [6]. Our findings (decrease of the risk of dislocation with a constrained liner in neurologically impaired patients) are supported by this case report in neurologic patients and by those of other large series for other indications. From review of the literature [32], there is evidence that the constrained liner is successful in providing stability in patients with recurrent dislocation. Our rate of dislocation with the design of this implant was not higher than the rates of dislocation observed for different implants in the literature (Table 4). However, the success in achieving stability could have been balanced by the evidence of early loosening of the component in our neurologically impaired patients.
Table 3.
Hip arthroplasty in patients with neurological conditions
| Study | Number of hips | Liner type | Neurologic condition | Dislocation (%) | Loosening (%) |
|---|---|---|---|---|---|
| Buly et al. [8] | 19 | Unconstrained | Cerebral palsy | 2 (11%) | 3 (16%) |
| Weber and Cabanela [38] | 16 | Unconstrained | Cerebral palsy | no | 1 (6%) |
| Turcotte et al. [35] | 47 | Unconstrained | Parkinson | 5 (11%) | 2 (4%) |
| Weber et al. [39] | 107 | Unconstrained | Parkinson | 6 (6%) | 3 (3%) |
| Blake et al. [6] | 2 | Constrained | Cerebral palsy | no | no |
| Weber and Cabanela [37] | 3 | Unconstrained | Myelomeningocele | 3 (100%) | 1 (33%) |
| Hernigou et al. [current study] | 132 | Unconstrained | Mixed conditions | 33 (25%) | 10 (8%) |
| Hernigou et al. [current study] | 164 | Constrained | Mixed conditions | 3 (2%) | 1 (1%) |
Table 4.
Dislocations and loosening in patients with constrained liners
Our finding of nearly an absence of loosening (only one case) at 7 years’ followup is lower than that reported in other studies with constrained liners (Table 4). However, comparisons of loosening rates between different constrained (cementless or cemented) components [17, 24, 25] should be made cautiously, since patient populations may not be similar. For example, in neurologically impaired patients, a cemented liner is recommended according to their osteoporotic status, and these patients usually have a lower activity level than other patients. Also, the constrained acetabular component was often used as a salvage procedure (recurrent dislocations and revisions) when other options have failed in other series [1, 2, 7, 11]. Our low rate of loosening may also be related to the new design of the implant. Since, once the head has crossed the ring, it falls below the equatorial plane, the clip is no longer constrained and the cup works as conventionally except in extreme movements.
The risk of dislocation varied according to the various types of hip diseases and neurological condition. In our cohort of patients, the incidence of dislocation was 10% in the first 2 months, but the cumulative risk of at least one dislocation was 25% for the subgroup of patients who lived for 10 years. An explanation is that in many patients, particularly cognitively impaired patients or those with increased muscle tone, neurologic function deteriorated over time compared with the status at surgery. We found the risk of dislocation was not the same for all the patients with NMD in the absence of a constrained liner (Table 3). This is consistent with the other series of the literature (Table 3). In patients with an increased tendency to subluxate or dislocate, such as those with cerebral palsy [31] or myelomeningocele [37], the use of unconstrained liners is associated with a high risk of dislocation. In patients with Parkinson’s disease the evaluation of the risk of dislocation with standard liners is different according to the authors: high for Turcotte et al. [35] and not increased for Weber et al. [39].
The use of constrained liners in primary THA in cognitively impaired patients or in neurologically impaired patients with increased muscle tone reduces the risk postoperative hip dislocation without increased risk of loosening up to mid-term. It should particularly be considered in this select at-risk population when the hip disease is a fracture or an osteonecrosis or when the patient has a hip with an increased tendency to subluxate or dislocate, such as in those with cerebral palsy.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research.
This work was performed at Hôpital Henri Mondor.
References
- 1.Alberton GM, High WA, Morrey BF. Dislocation after revision total hip arthroplasty: an analysis of risk factors and treatment options. J Bone Joint Surg Am. 2002;84:1788–1792. [PubMed] [Google Scholar]
- 2.Anderson MJ, Murray WR, Skinner HB. Constrained acetabular components. J Arthroplasty. 1994;9:17–23. doi: 10.1016/0883-5403(94)90133-3. [DOI] [PubMed] [Google Scholar]
- 3.Beaule PE, Schmalzried TP, Udomkiat P, Amstutz HC. Jumbo femoral head for the treatment of recurrent dislocation following total hip replacement. J Bone Joint Surg Am. 2002;84:256–263. doi: 10.2106/00004623-200202000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Berend KR, Lombardi AV, Jr, Mallory TH, Adams JB, Russell JH, Groseth KL. The long-term outcome of 755 consecutive constrained acetabular components in total hip arthroplasty examining the successes and failures. J Arthroplasty. 2005;20(7 Suppl 3):93–102. doi: 10.1016/j.arth.2005.06.001. [DOI] [PubMed] [Google Scholar]
- 5.Berry DJ, Knoch M, Schleck CD, Harmsen WS. The cumulative long-term risk of dislocation after primary charnley total hip arthroplasty. J Bone Joint Surg Am. 2004;86:9–14. doi: 10.2106/00004623-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Blake SM, Kitson J, Howell JR, Gie GA, Cox JP. Constrained total hip arthroplasty in a paediatric patient with cerebral palsy and painful dislocation of the hip. J Bone Joint Surg Br. 2006;88:655–657. doi: 10.1302/0301-620X.88B5.17206. [DOI] [PubMed] [Google Scholar]
- 7.Bremner BR, Goetz DD, Callaghan JJ, Capello WN, Johnston RC. Use of constrained acetabular components for hip instability: an average 10-year follow-up study. J Arthroplasty. 2003;18:131–137. doi: 10.1016/S0883-5403(03)00295-X. [DOI] [PubMed] [Google Scholar]
- 8.Buly RL, Huo M, Root L, Binzer T, Wilson PD. Total hip arthroplasty in cerebral palsy: long-term follow-up results. Clin Orthop Relat Res. 1993;296:148–153. [PubMed] [Google Scholar]
- 9.Bystrom S, Espehaug B, Furnes O, Havelin LI. Norwegian Arthroplasty Register. Femoral head size is at risk factor for total hip luxation: a study of 42, 987 primary hip arthroplasties from the Norwegian Arthroplasty Register. Acta Orthop Scand. 2003;74:514–524. doi: 10.1080/00016470310017893. [DOI] [PubMed] [Google Scholar]
- 10.Cabanela ME, Weber M. Instructional course lecture: Total hip arthroplasty in patients with neuromuscular disease. J Bone Joint Surg Am. 2000;82:426–432. doi: 10.1302/0301-620X.82B3.10215. [DOI] [PubMed] [Google Scholar]
- 11.Callaghan JJ, O’Rourke MR, Goetz DD, Lewallen DG, Johnston RC, Capello WN. Use of a constrained tripolar acetabular liner to treat intraoperative instability and postoperative dislocation after total hip arthroplasty: a review of our experience. Clin Orthop Relat Res. 2004;429:117–123. doi: 10.1097/01.blo.0000150276.98701.95. [DOI] [PubMed] [Google Scholar]
- 12.Cooke CC, Hozack W, Lavernia C, Sharkey P, Shastri S, Rothman RH. Early failure mechanisms of constrained tripolar acetabular sockets used in revision total hip arthroplasty. J Arthroplasty. 2003;18:827–833. doi: 10.1016/S0883-5403(03)00325-5. [DOI] [PubMed] [Google Scholar]
- 13.Daly PJ, Morrey BF. Operative correction of an unstable total hip arthroplasty. J Bone Joint Surg Am. 1992;74:1334–1343. [PubMed] [Google Scholar]
- 14.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 15.Dewal H, Maurer SL, Tsai P, Su E, Hiebert R, Di Cesare PE. Efficacy of abduction bracing in the management of total hip arthroplasty dislocation. J Arthroplasty. 2004;19:733–738. doi: 10.1016/j.arth.2004.02.041. [DOI] [PubMed] [Google Scholar]
- 16.Dorr LD, Wolf AW, Chandler R, Conaty JP. Classification and treatment of dislocations of total hip arthroplasty. Clin Orthop Relat Res. 1983;173:151–158. [PubMed] [Google Scholar]
- 17.Fisher DA, Kiley K. Constrained acetabular cup disassembly. J Arthroplasty. 1994;9:325–329. doi: 10.1016/0883-5403(94)90088-4. [DOI] [PubMed] [Google Scholar]
- 18.Goetz DD, Bremner BR, Callaghan JJ, Capello WN, Johnston RC. Salvage of a recurrently dislocating total hip prosthesis with use of a constrained acetabular component. A concise follow-up of a previous report. J Bone Joint Surg Am. 2004;86:2419–2423. doi: 10.2106/00004623-200411000-00009. [DOI] [PubMed] [Google Scholar]
- 19.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 20.Harman MK, Hodge WA, Banks SA. Closed reduction of constrained total hip arthroplasty. Clin Orthop Relat Res. 2003;414:121–128. doi: 10.1097/01.blo.0000073342.50837.4a. [DOI] [PubMed] [Google Scholar]
- 21.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.2307/2281868. [DOI] [Google Scholar]
- 22.Lachiewicz Kelley SS, PF Hickman JM, Paterno SM. Relationship of femoral head and acetabular size to the prevalence of dislocation. Clin Orthop Relat Res. 1998;355:163–170. doi: 10.1097/00003086-199810000-00017. [DOI] [PubMed] [Google Scholar]
- 23.Khan RJ, Fick D, Alakeson R, Haebich S, Cruz M, Nivbrant B, Wood D. A constrained acetabular component for recurrent dislocation. J Bone Joint Surg Br. 2006;88:870–876. doi: 10.1302/0301-620X.88B7.17644. [DOI] [PubMed] [Google Scholar]
- 24.Lombardi AV, Jr, Mallory TH, Kraus TJ, Vaughn BK. Preliminary report on the S-ROM constraining acetabular insert: a retrospective clinical experience. Orthopedics. 1991;14:297–303. [PubMed] [Google Scholar]
- 25.McCarthy J, Lee JN. Components in complex revision total hip arthroplasty. Clin Orthop Relat Res. 2005;441:210–215. doi: 10.1097/01.blo.0000194069.15086.1b. [DOI] [PubMed] [Google Scholar]
- 26.Meek RM, Allan DB, McPhillips GP, Kerr LP, Howie CR. Epidemiology of dislocation after total hip arthroplasty. Clin Orthop Relat Res. 2006;447:9–18. doi: 10.1097/01.blo.0000218754.12311.4a. [DOI] [PubMed] [Google Scholar]
- 27.Miller CW, Zura RD. Closed reduction of a dislocation of a constrained acetabular component. J Arthroplasty. 2001;16:504–505. doi: 10.1054/arth.2001.21504. [DOI] [PubMed] [Google Scholar]
- 28.Olerud S, Karlstrom G. Recurrent dislocation after total hip replacement: treatment by fixing an additional sector to the acetabular component. J Bone Joint Surg Br. 1985;67:402–405. doi: 10.1302/0301-620X.67B3.3997949. [DOI] [PubMed] [Google Scholar]
- 29.Parvizi J, Morrey BF. Bipolar hip arthroplasty as a salvage treatment for instability of the hip. J Bone Joint Surg Am. 2000;82:1132–1139. doi: 10.2106/00004623-200008000-00010. [DOI] [PubMed] [Google Scholar]
- 30.Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am. 1997;79:1202–1210. doi: 10.2106/00004623-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 31.Samilson RL, Tsou P, Aamoth G, Green WM. Dislocation and subluxation of the hip in cerebral palsy: pathogenesis, natural history and management. J Bone Joint Surg Am. 1972;54:863–873. [PubMed] [Google Scholar]
- 32.Shapiro GS, Weiland DE, Markel DC, Padgett DE, Sculco TP, Pellicci PM. The use of a constrained acetabular component for recurrent dislocation. J Arthroplasty. 2003;18:250–258. doi: 10.1054/arth.2003.50090. [DOI] [PubMed] [Google Scholar]
- 33.Shrader MW, Parvizi J, Lewallen DG. The use of a constrained acetabular component to treat instability after total hip arthroplasty. J Bone Joint Surg Am. 2003;85:2179–2183. doi: 10.2106/00004623-200311000-00019. [DOI] [PubMed] [Google Scholar]
- 34.Su EP, Pellicci PM. The role of constrained liners in total hip arthroplasty. Clin Orthop Relat Res. 2004;420:122–129. doi: 10.1097/00003086-200403000-00017. [DOI] [PubMed] [Google Scholar]
- 35.Turcotte R, Godin C, Duchesne R, Jodoin A. Hip fractures and Parkinson’s disease: a clinical review of 94 fractures treated surgically. Clin Orthop Relat Res. 1990;256:132–136. [PubMed] [Google Scholar]
- 36.Turner RS. Postoperative total hip prosthetic femoral head dislocations: incidence, etiologic factors, and management. Clin Orthop Relat Res. 1994;301:196–204. [PubMed] [Google Scholar]
- 37.Weber M, Cabanela ME. Total hip arthroplasty in patients with low-lumbar-level myelomeningocele. Orthopedics. 1998;21:709–713. doi: 10.3928/0147-7447-19980601-14. [DOI] [PubMed] [Google Scholar]
- 38.Weber M, Cabanela ME. Total hip arthroplasty in patients with cerebral palsy. Orthopedics. 1999;22:425–427. doi: 10.3928/0147-7447-19990401-12. [DOI] [PubMed] [Google Scholar]
- 39.Weber M, Cabanela ME, Sim FH, Frassica FJ, Harmsen WS. Total hip arthroplasty in patients with Parkinson’s disease. Int Orthop. 2002;26:66–68. doi: 10.1007/s00264-001-0308-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Williams JF, Gottesman MJ, Mallory TH. Dislocation after total hip arthroplasty: treatment with an above-knee hip spica cast. Clin Orthop Relat Res. 1982;171:53–58. [PubMed] [Google Scholar]
- 41.Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–1306. [PubMed] [Google Scholar]
- 42.Yang C, Goodman SB. Outcome and complications of constrained acetabular components. Orthopedics. 2009;32:115–123. [PubMed] [Google Scholar]