Abstract
Background
The treatment of end-stage hip disease in very young patients is controversial, with advocates for nonoperative treatment, hip arthrodesis and replacement procedures. The functional improvements in this group of patients are not well documented and whether the condition for which the surgery is performed influences function.
Questions/purposes
We determined whether (1) modern THA provides major functional improvements; (2) disease-specific factors impact the magnitude of improvement; (3) these procedures are associated with early failures and complications; and (4) radiographically secure implant fixation is achieved with contemporary implants.
Methods
We retrospectively reviewed 88 patients (102 hips) who had THA and were 25 years or younger at surgery. The most common diagnoses were osteonecrosis (44%) and secondary osteoarthritis (41%). All patients received a cementless socket of varying designs and all except five a cementless stem. Demographic data, Harris hip score, and Charnley classification were recorded. Radiographic evaluation was used to determine implant fixation. We identified complications and failure mechanisms. The minimum followup was 2 years (median, 4.2 years; range, 2–16 years).
Results
The 95 nonrevised hips were followed clinically an average of 61 months. The mean Harris hip scores improved from 42 preoperatively to 83 postoperatively. Lower Harris hip scores were associated with systemic disease (Charnley Class C). Seven hips (7%) underwent revision. There were nine (9%) major complications. One hundred percent of femoral stems and 98% of acetabular components were well-fixed at last followup.
Conclusion
Contemporary total hip arthroplasty in patients 25 years of age and younger is associated with improved hip function, and secure fixation of cementless implants at early followup.
Level of Evidence
Level IV, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Adolescents and young adults can be afflicted with various end-stage conditions of the hip, yet the optimal methods of treatment remain controversial [6, 8]. Treatment options include nonoperative management, hip arthrodesis and replacement procedures. THA is one solution for restoring function and activity yet the majority of published studies on THA in young patients have focused on the treatment of juvenile rheumatoid arthritis (JRA) and have primarily included cemented implants and procedures performed in the 1980s [5, 15, 18–21, 24, 27]. In these reports, failure rates at early- to long-term followup range from 0% to 42.3% with aseptic loosening of cemented components being a common mode of failure [3, 5, 15, 18–21, 24, 27]. These data have limited applicability to contemporary THA, which is performed in a broader patient population, including those with noninflammatory conditions of the hip. Additionally, cementless acetabular and femoral fixation combined with improved bearing surface materials have led to renewed optimism regarding the efficacy and longevity of contemporary THA in the young patient population.
A number of authors have reported THA in younger people (eg, under the age of 30) [2, 3, 5, 10, 11, 15, 16, 18–21, 23, 24, 26, 27] and the data are variable with respect to implant survivorship. Reports with contemporary THA components are limited (Restrepo et al. [23], Wangen et al. [26]), but are important for patient counseling, surgical decision-making and to objectively compare THA with other treatment modalities (eg, nonoperative measures and arthrodesis). Therefore, our study was designed to provide additional information regarding of THA in patients 25 years of age or younger.
We determined whether (1) modern THA provides major functional improvements; (2) disease-specific factors affect the magnitude of improvement; (3) these procedures are associated with early failures and complications; and (4) radiographically secure implant fixation is achieved with contemporary implants.
Patients and Methods
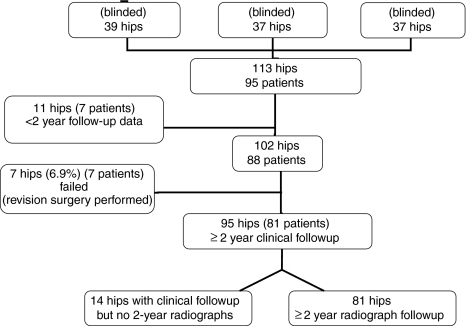
We retrospectively reviewed 95 patients (113 hips) who had THA in one of three institutions (Fig. 1). Thirty-nine THAs were performed at the University of Iowa (JJC) and 37 THAs at both Washington University/Barnes-Jewish Hospital (JCC) and the Rubin Institute for Advanced Orthopedics (MAM). We attempted to have all patients return for clinical and radiographic followup visits. Telephone calls and Internet searches were used to locate patients who were lost to followup. Despite this, seven of the 95 patients (11 hips) had less than 2-year clinical followup data. At last documented followup, there were no failures in these 11 hips. Three of these seven patients (five hips) never returned after surgery and four patients (six hips) were seen between 5 and 18 months after surgery. The mean Harris hip score [17] for these six hips improved from 44 points preoperatively to 84 points at last followup. No major complications (additional procedures were performed or the complication was associated with potential for permanent morbidity or disability) were noted in this patient subgroup. The remaining 88 patients (102 hips) were followed for a minimum of 2 years or until revision and are the focus of this study. The mean patient age at surgery was 20 years (range, 12–25 years). Forty (45%) patients were male and 48 (55%) were female. The mean body mass index [13] of the patients was 29 kg/m2 (range, 16–61 kg/m2). Surgery was performed on the right side in 41% and on the left in 59%. Eighteen patients had bilateral procedures. Fifteen of these were staged and three were performed at the same surgical procedure. Seven of the 102 hips (7%) were revised. Therefore, 81 patients (95 hips) were available at the minimum 2-year clinical followup with a mean followup duration of 59 months (range, 24–197 months). Sixty-nine of these patients (81 hips) had clinical followup and minimum 2-year radiographs, whereas the remaining 12 patients (14 hips) had a telephone interview.
Fig. 1.
A flow chart shows a summary of the entire patient cohort and the reasons for exclusions and the numbers available for final evaluation. The institutions from which the patients were derived is blinded.
The diagnoses were osteonecrosis (44%), secondary osteoarthritis (41%), JRA (12%), idiopathic chondrolysis (1%), osteogenesis imperfecta tarda/protrusio (1%), and spondyloepiphyseal dysplasia (1%). For the 41% of hips with secondary osteoarthritis, the etiologies were determined and included hip dysplasia (13% of the entire cohort), Legg-Calve Perthes disease (10%), slipped capital femoral epiphysis (6%), posttraumatic disease (4%), and “not specified” (8%). Therefore, the osteoarthritic group was comprised of patients with major underlying hip disorders.
Preoperative demographic data recorded included age, gender, height, diagnoses, laterality, and comorbidities. Preoperative Charnley classification was determined [4]. There were 24 Class A, 12 Class B, and 59 Class C patients. Clinical outcomes were measured with the Harris hip score [17] both preoperatively and at followup visits. Failure was defined as the index THA requiring revision surgery. Major orthopaedic complications were events related to the THA requiring an additional procedure (eg, closed reduction or reoperation) or an event with the potential for permanent morbidity/disability (eg, nerve palsy, pulmonary embolism).
All operations were performed by one of the senior authors (JCC, JJC, MAM). Two surgeons used a posterior approach and one surgeon an anterolateral approach. All patients received a cementless acetabular component (Table 1) and all except five received a cementless femoral stem (Table 2). Five hips had cemented stems implanted because of poor femoral bone quality (osteopenia). For the 102 hips followed 2 years or until revision, 46 (45%) had a cobalt-chrome femoral head on a highly crosslinked polyethylene bearing surface. There were, however, 30 (29%) hips with cobalt-chrome on conventional polyethylene. Alternative bearing combinations in the remainder of the hips included ceramic on highly crosslinked polyethylene (seven [7%]), ceramic-on-ceramic (14 [14%]), and metal-on-metal (five [5%]). Head sizes implanted varied from 22 to 50 mm. Postoperatively, patients were mobilized the day after surgery with in-hospital physical therapy. Patients with a hybrid THA were allowed to bear full weight as tolerated. Patients with a cementless THA were maintained at partial weightbearing (30%-50%) for 6 weeks and then advanced to full weightbearing. Crutches or a walker were used until the patient could ambulate with no limp. Formal physiotherapy was received for 4 to 12 weeks depending on the needs of the patient.
Table 1.
Acetabular compoenets of the 102 hips followed a minimum of two years or until revision
| Acetabular implant type | Number | Percent |
|---|---|---|
| Zimmer Trilogy | 32 | 31.3 |
| Zimmer Trabecular Metal | 1 | 1.0 |
| Stryker Trident HA coated | 28 | 27.5 |
| DeuPuy Ultamet | 3 | 2.9 |
| Wright Conserve Plus Surface Beaded | 2 | 2.0 |
| Zimmer HG | 11 | 10.8 |
| DeuPuy Pinnacle | 16 | 15.7 |
| DePuy Duraloc | 7 | 6.9 |
| DeuPuy Pinnacle Bantam | 2 | 2.0 |
| Totals | 102 | 100 |
Table 2.
Femoral components of the 102 hips followed a minimum of two years or until revision
| Femoral implant type | Number | Percent |
|---|---|---|
| Zimmer Versys | 49 | 48.0 |
| DePuy Prodigy | 20 | 19.7 |
| DePuy AML | 8 | 7.8 |
| Bantam Porocoat | 7 | 6.9 |
| Depuy Summit | 4 | 3.9 |
| Stryker Accolade HA coated | 4 | 3.9 |
| Wright Perfecta Surface Plasma Spray | 1 | 1.0 |
| Osteonics Omniflex | 1 | 1.0 |
| Osteonics Secure-Fit | 1 | 1.0 |
| Osteonics HA Coated | 1 | 1.0 |
| Zimmer Heritage Cemented | 4 | 3.9 |
| Custom Polished Cemented | 2 | 2.0 |
| Totals | 102 | 100.0 |
Patient followup was performed in a similar fashion at each institution. All patients were recommended to followup annually or every 2 years. Hip function was assessed with the Harris hip score [17]. Gait and hip ROM were assessed. Radiographic evaluation included an AP pelvis and cross-table lateral view. For patients unable to return for clinical and radiographic followup, a telephone interview was performed (by a study coordinator at each site) to obtain clinical outcome data and information on complications, failures, and reoperations.
Preoperative, immediately postoperative, and final followup AP pelvis and cross-table lateral radiographs were available for 69 patients (81 hips). All radiographs were assessed by one of the coauthors (JMO, TMS, SSL) independent of the treating surgeons. One observer at each institution performed the radiographic analysis. We assessed acetabular component migration by determining the vertical and horizontal position of the component. The vertical position was determined by measuring the distance between the interteardrop line and a parallel line tangential to the most superior aspect of the acetabular component. The horizontal position was determined by measuring the distance between a vertical line drawn through the medial aspect of the teardrop and a parallel line drawn tangential to the most medial aspect of the acetabular component [7]. Subsidence resulting from loosening was defined as any change in acetabular component position greater than 4 mm in either the vertical or horizontal position in relationship to the teardrop [22]. We examined the acetabular component interface radiographically for lucency according to the methods previously described by DeLee and Charnley [9]. Lysis was defined as any area of radiolucency greater than 3 mm at the implant-bone interface. If there was greater than 2 mm of lucency in all three DeLee and Charnley zones or if the implant had subsided, the acetabular component was considered loose. We evaluated femoral loosening using the AP and cross-table lateral radiographs observing for lucency at the bone-implant interface in Zones 1 through 14 as described by Gruen et al. [14]. Any subsidence of the femoral stem more than 2 mm or a continuous radiolucent line at the implant bone interface also classified the implant as loose [12]. The presence of a subsided stem was determined by measuring the distance from the tip of the trochanter to the top of the femoral stem. We assessed ingrowth by the presence or absence of reactive lines adjacent to the porous-coated portion of the implant and the presence of spot welds of endosteal bone [12].
The differences in hip function (Harris hip score) were compared among different Charnley classification groups (A, B, C), and between different preoperative hip diagnoses (osteonecrosis versus osteoarthritis). These analyses were performed with use of repeated measures analysis of variance. The Bonferroni test was used to detect differences between the groups. The data analysis was generated using SPSS statistical software (Version 16.0; SPSS Inc, Chicago, IL).
Results
For the 95 nonrevised hips, the mean Harris hip score improved from 43 points (range, 5–86 points) preoperatively to 83 points (range, 26–100 points) at last followup (average, 61 months; range, 23–197 months). Sixty-six percent of the hips had a Harris hip score greater than 80 points. The mean preoperative and final followup hip scores were higher for Charnley Class A cases and for Class A and B cases combined when compared with Class C patients (p < 0.001 for both comparisons) (Table 3). Additionally, the followup Harris hip scores were higher (p = 0.015) for patients with a preoperative diagnosis of osteonecrosis when compared with a diagnosis of osteoarthritis (Table 4).
Table 3.
Harris hip score improvements according to Charnley class for the 95 non-revised hips
| Charnley class | Number | Preoperative HHS average range | Postoperative HHS average range | p Value |
|---|---|---|---|---|
| A | 24 | 54 (24–86) | 86 (44–100) | < 0.001 |
| B | 12 | 44 (26–57) | 86 (52–100) | < 0.001 |
| C | 59 | 39 (5–74) | 81 (26–100) | < 0.001 |
HHS = Harris Hip Score.
Table 4.
Harris hip score improvements according to preoperative diagnoses for the 95 nonrevised hips
| Diagnosis | Number | Preoperative HHS average range | Postoperative HHS average range | p Value |
|---|---|---|---|---|
| Osteonecrosis | 42 | 43.1 (12–86) | 90.0 (70–100) | < 0.001 |
| Osteoarthritis | 38 | 44.2 (24–70) | 77.5 (26–100) | < 0.001 |
| JRA | 12 | 40.1 (5–73) | 79.6 (45–100) | < 0.001 |
| Other | 3 | 26.2 (21–32) | 57.7 (34–94) | N/A |
JRA = juvenile rheumatoid arthritis; N/A = not applicable (N = 3); HHS = Harris hip score.
Of the 102 hips (88 patients) followed for a minimum of 2 years, seven hips (7%) in seven patients failed and underwent revision surgery. The mean time between index surgery and revision for these patients was 64 months (range, 9–125 months). No hips were revised for aseptic loosening of either component. Three of the seven revisions were acetabular cup, head, and liner; and three others were head and liner exchanges with implant retention. No femoral components were revised. All revisions for polyethylene wear and osteolysis were resulting from failure of conventional polyethylene liners (Table 5).
Table 5.
Failures and revision
| Diagnosis | Charnley class | Femoral head type | Femoral head size | Acetabular liner | Revision reason | Time to revision (months) |
|---|---|---|---|---|---|---|
| Osteonecrosis | C | Ceramic | 32 | Ceramic | Infection | 34.5 |
| Osteonecrosis | C | Ceramic | 28 | HCLPE | Dislocation | 33 |
| Osteonecrosis | C | CoCr | 26 | CPE | Dislocation | 8.7 |
| Osteoarthritis | A | CoCr | 22 | CPE | Anterior Subluxation Groin Pain | 45.01 |
| Osteoarthritis | A | CoCr | 26 | CPE | Wear | 92.99 |
| Osteoarthritis | A | CoCr | 26 | CPE | Wear/Subluxation | 124.8 |
| Osteoarthritis | A | CoCr | 26 | CPE | Wear/Lysis | 107.6 |
CoCr = cobalt chrome; HCLPE = highly cross-linked polyethylene; CPE = conventional polyethylene.
There were nine (9%) major orthopaedic complications related to the index THA. These included four dislocations (3 revised) one periprosthetic fracture, two peroneal nerve palsies, a femoral artery intimal tear requiring surgical repair, and a deep implant infection. The patient with infection had a resection arthroplasty and died of unrelated causes 26 months postoperatively. The periprosthetic fracture was treated with open reduction internal fixation without the need for component revision. The vascular injury was repaired and not associated with long-term problems. One patient’s nerve palsy completely resolved over 1 year and the other patient continues to have dysesthesia over the foot without motor weakness. For this group of patients the average Harris hip score (after revision or treatment of the complication) was 76.5 (range, 34–99) at an average followup of 76 months (range, 27.5–134 months).
Stable implant fixation was achieved for 100% of femoral stems and 98% of the acetabular components. The minimum radiographic followup was 24 months (mean, 55 months; range, 24–133 months). The two radiographically loose acetabular components were not associated with symptoms requiring revision surgery. One additional asymptomatic patient had acetabular lysis of 1 cm2 in Zone 2, but the acetabular component was well-fixed. There were no loose femoral stems. Femoral lysis was seen in two hips with a 1-cm2 lesion in Gruen Zone 7 and Zones 1 and 7, respectively. All hips with osteolysis had conventional polyethylene liners.
Discussion
THA is occasionally necessary for end-stage hip disease in very young patients (25 years of age or younger). Nevertheless, the literature regarding THA in this age group primarily focuses on cemented THA for treating patients with a diagnosis of JRA (Table 6) [5, 15, 18–21, 24, 27]. The published information on contemporary THA in this age group is limited [23]. Therefore, we studied a relatively large, multicenter patient cohort to provide additional data on this controversial topic. We first determined if modern THA provides major functional improvement and if disease-specific factors impact the magnitude of functional improvement; second, if these procedures were associated with low early failure and complication rates; third, if radiographically secure implant fixation was achieved with contemporary implants.
Table 6.
Summary of selected studies for THA in adolescent and young adult patients is presented in this table
| Study | Number of hips/patients | Average age (years; range) | Followup years (range) | Percent JRA | Percent cemented THA | Number/Percent Revisions | Number and percent radiographic loosening (excluding revisions) |
|---|---|---|---|---|---|---|---|
| Bilsel et al. (2008) [1] | 37/23 | 22.3 (17–30) | 11.3 (4.8–17.7) | 100% | 62% | 3 (8%) | NA |
| Chandler et al. (1981) [3] | 33/29 | 23 (14–30) | 5.6 (4.8–7) | 12% | 100% | 7 (21.2%) | 11 (42.3%) |
| Dorr et al. (1990) [10] | 81/69 | 30 (14–45) | 9.2 (5–16.5) | NA | 100% | 29 (33%) | 29 (56%) |
| Haber and Goodman (1998) [15] | 29/16 | 20 (14–35) | 4.4 (2–8.3) | 100% | 31% femoral 6.9% cup | 1 (3.4%) | 3 (10.2%) |
| Lachiewicz et al. (1986) [19] | 62/34 | 26 (14–49) | 6 (2–11) | 100% | 100% | 2 (3.2%) | 16 (25.8%) acetabular 4 (6.6%) femoral |
| Learmonth et al. (1989) [20] | 14/7 | 16 (12–22) | 8.5 (4–11) | 100% | 100% | 0 | 8 (57%) |
| Restrepo et al. (2008) [23] | 29/21 | 17.6 (13.5–20) | 6.6 (4.2–10) | 26% | 0% | 2 (6.9%) | 0% |
| Witt et al. (1991) [27] | 96/54 | 16.7 (11.3–26.6) | 11.5 (5.3–18.3) | 100% | 100% | 24 (25.0%) | 17 (23.6%) |
JRA = juvenile rheumatoid arthritis; NA = not applicable due to lack of data.
There are several limitations of this study. First, the followup is only short-term with some patients having only 2-year data. Clearly, additional followup is needed to assess the long-term durability of contemporary THA in young patients. Second, drawing patients from three centers means there was no specific coordination of surgical technique or implants used in the study. However, the data likely allow greater generalizability. Third, although the goal of this study was to obtain an overview of THA outcomes in patients younger than 25 years old, grouping patients with all diagnoses may not be ideal because the functional improvement (Harris hip score) for THA performed for various diagnoses may vary. Fourth, wear data were not collected as a result of various implants/bearing surfaces and the multicenter nature of the study. Finally, activity level data were not collected on the patients and cannot be analyzed as a risk factor for failure.
Our data confirm that THA provides major functional improvement in this patient population. Specifically, the Harris hip score improved an average 40 points at a mean followup of 5 years. The mean hip score for our patients at final followup was 83 points. Other investigators have also used the Harris hip score to determine functional improvement after THA in the very young patient [1, 15, 23]. Bisel et al. [1] reported on 37 JRA hips in patients averaging 22 years of age at the time of surgery and followed for a mean of 11.3 years. They noted a mean Harris hip score improvement from 27.2 to 79.5 after THA. Similarly, Haber and Goodman [15] studied 29 THAs in patients with JRA averaging 20 years of age at surgery and followed for an average of 4.4 years. Mean Harris hip scores in this patient cohort improved from 42 to 78 after THA. Most importantly, Restrepo et al. [23] recently described their functional scores of modern uncemented THA in 29 hips followed an average of 6.6 years. Similar to our study, their patient population included a variety of diagnoses. Their mean preoperative Harris hip score of 52 improved to 77 at most recent followup. Collectively, these studies demonstrate 25- to 50-point improvements in Harris hip scores after THA. It should be noted that the final mean scores range from 77 to 83 points. We speculate functional limitations resulting from systematic disease, severe hip deformities preoperatively, and previous hip procedures may hamper the functional status in some of these young patients after THA. In fact, our data demonstrate patients with systematic disease (Charnley C) had lower hip scores than patients with isolated unilateral or bilateral hip disease (Charnley A and B) (Table 1). These findings are consistent with those of Halley and Charnley [16]. Furthermore, we observed that patients with a diagnosis of osteonecrosis had higher hip scores than patients with osteoarthritis. The explanation for this difference is not evident, yet may be related to the fact that patients with osteonecrosis are more likely to have systematic disease and perhaps a lower functional demand when compared with patients with hip osteoarthritis. Again, osteoarthritis hips in this age group are commonly associated with severe deformity and/or previous surgical procedures, both of which could limit clinical function after THA.
In our series, seven hips (7%) failed and had revision surgery. Reasons for revision included instability (three hips), polyethylene wear/osteolysis (three hips), and infection (one hip). None of the revised implants had aseptic loosening and all three cases of polyethylene wear/osteolysis had conventional polyethylene acetabular liners implanted at the index procedure. THA failure and the need for revision surgery have been reported at various rates by different investigators. A recent study analyzing contemporary THA in 35 hips in a patient cohort with various diagnoses [23] reported a similar failure rate to our study. In this series, four patients (six hips) were lost to followup and two hips (one patient) of the remaining 29 hips were revised for severe polyethylene wear. This is similar to our revision rate. Other studies analyzing failure rates have primarily reported on cemented THA in JRA patient cohorts (Table 4). In the studies with follow-up durations similar to our cohort, the need for revision surgery ranges from 3.2% to 21.2% at early to midterm followup [3, 19].
We also noted nine (9%) major complications, all of which resolved with treatment except one nerve palsy with partial recovery and a persistent dysesthesia. Other studies in the literature report complications sporadically and do not follow a consistent definition of complication grading. Nevertheless, one study carefully documented complications associated with 62 cemented THAs in patients with JRA using our definition of major complication. This study had four (6%) major complications, including two pulmonary emboli and two hips with severe heterotopic ossification. Although these complications are distinct from those in our study, these combined data indicate that THA in the very young patient is associated with a 6–8% complication rate. Analysis of implant fixation at a mean followup of 55 months revealed 100% of the femoral stems and 98% of the acetabular components were radiographically well-fixed in our patient cohort. None of the implants were revised for aseptic loosening. Similarly, a recent study analyzing uncemented THA in patients younger than 20 years of age documented 100% fixation of femoral and acetabular components at a mean 6.6 years followup [23]. Although reporting relatively early followup, these two studies indicate secure implant fixation is predictably achieved with cementless implants in this patient population. In contrast, studies with similar followup durations for cemented implants [3, 19] have noted higher rates of radiographic loosening ranging from 25.8% to 42.3% excluding revisions (Table 4). These data suggest that fixation of cementless implants is superior to the cemented fixation of these earlier studies. Our data and that of Restrepo et al. [23] support the use of cementless hip reconstruction in the adolescent and young adult patient undergoing primary THA.
Patients younger than 25 years of age with advanced hip disease represent a unique population with a need for extremely long-term survivorship of prosthetic reconstructions. The goal of surgical treatment in this patient population is to provide a long-term solution with pain relief and restoration of function. Our data indicate contemporary THA provides improved hip function and stable implant fixation at short- to midterm followup. All bearing surface failures were the result of conventional polyethylene wear and/or osteolysis, which suggests future studies should investigate the performance of alternative bearing materials [25]. Cementless fixation combined with improved THA bearing materials may provide long-term survivorship even in the young patient population. Prospective, multicenter clinical trials to establish large patient cohorts should be considered to investigate THA in adolescent and young adult patients.
Acknowledgments
We thank Gail Pashos and Debbie Long for their assistance with the manuscript preparation.
Footnotes
One or more of the authors received funding from the Curing Hip Disease Fund (JCC) and Stryker Orthopedics (MAM), Mahwah, NJ, for this study. Each author certifies that he or she has or may receive payments or benefits from a commercial entity: DePuy (MAM, JJC), Stryker (MAM), Wright Medical (MAM), National Institutes of Health (NIAMS and NICHD) (MAM), and Tissue Gene (MAM) related to this work.
Each author certifies that his or her institution has approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at Washington University School of Medicine, St Louis, MO, USA.
References
- 1.Bilsel N, Gokce A, Kesmezacar H, Mumcuoglu E, Ozdogan H. [Long-term results of total hip arthroplasty in patients with juvenile rheumatoid arthritis] Acta Orthop Traumatol Turc. 2008;42:119–124. doi: 10.3944/aott.2008.42.2.119. [DOI] [PubMed] [Google Scholar]
- 2.Bsila RS, Inglis AE, Ranawat CS. Joint replacement surgery in patients under thirty. J Bone Joint Surg Am. 1976;58:1098–1104. [PubMed] [Google Scholar]
- 3.Chandler HP, Reineck FT, Wixson RL, McCarthy JC. Total hip replacement in patients younger than thirty years old. A five-year follow-up study. J Bone Joint Surg Am. 1981;63:1426–1434. [PubMed] [Google Scholar]
- 4.Charnley J. The long-term results of low-friction arthroplasty of the hip performed as a primary intervention. J Bone Joint Surg Br. 1972;54:61–76. [PubMed] [Google Scholar]
- 5.Chmell MJ, Scott RD, Thomas WH, Sledge CB. Total hip arthroplasty with cement for juvenile rheumatoid arthritis. Results at a minimum of ten years in patients less than thirty years old. J Bone Joint Surg Am. 1997;79:44–52. doi: 10.2106/00004623-199701000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Clohisy JC, Beaule PE, O’Malley A, Safran MR, Schoenecker P. AOA symposium. Hip disease in the young adult: current concepts of etiology and surgical treatment. J Bone Joint Surg Am. 2008;90:2267–2281. doi: 10.2106/JBJS.G.01267. [DOI] [PubMed] [Google Scholar]
- 7.Clohisy JC, Harris WH. The Harris-Galante porous-coated acetabular component with screw fixation. An average ten-year follow-up study. J Bone Joint Surg Am. 1999;81:66–73. doi: 10.2106/00004623-199901000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Clohisy JC, Keeney JA, Schoenecker PL. Preliminary assessment and treatment guidelines for hip disorders in young adults. Clin Orthop Relat Res. 2005;441:168–179. doi: 10.1097/01.blo.0000193511.91643.2a. [DOI] [PubMed] [Google Scholar]
- 9.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 10.Dorr LD, Luckett M, Conaty JP. Total hip arthroplasties in patients younger than 45 years. A nine- to ten-year follow-up study. Clin Orthop Relat Res. 1990;260:215–219. [PubMed] [Google Scholar]
- 11.Dudkiewicz I, Salai M, Israeli A, Amit Y, Chechick A. Total hip arthroplasty in patients younger than 30 years of age. Isr Med Assoc J. 2003;5:709–712. [PubMed] [Google Scholar]
- 12.Engh CA, Jr, Culpepper WJ, II, Engh CA. Long-term results of use of the anatomic medullary locking prosthesis in total hip arthroplasty. J Bone Joint Surg Am. 1997;79:177–184. doi: 10.1302/0301-620X.79B2.7640. [DOI] [PubMed] [Google Scholar]
- 13.Gallagher D, Heymsfield SB, Heo M, Jebb SA, Murgatroyd PR, Sakamoto Y. Healthy percentage body fat ranges: an approach for developing guidelines based on body mass index. Am J Clin Nutr. 2000;72:694–701. doi: 10.1093/ajcn/72.3.694. [DOI] [PubMed] [Google Scholar]
- 14.Gruen TA, McNeice GM, Amstutz HC. “Modes of failure” of cemented stem-type femoral components: a radiographic analysis of loosening. Clin Orthop Relat Res. 1979;141:17–27. [PubMed] [Google Scholar]
- 15.Haber D, Goodman SB. Total hip arthroplasty in juvenile chronic arthritis: a consecutive series. J Arthroplasty. 1998;13:259–265. doi: 10.1016/S0883-5403(98)90170-X. [DOI] [PubMed] [Google Scholar]
- 16.Halley DK, Charnley J. Results of low friction arthroplasty in patients thirty years of age or younger. Clin Orthop Relat Res 1975(112):180–191. [PubMed]
- 17.Harris WH. Etiology of osteoarthritis of the hip. Clin Orthop Relat Res. 1986;213:20–33. [PubMed] [Google Scholar]
- 18.Kitsoulis PB, Stafilas KS, Siamopoulou A, Soucacos PN, Xenakis TA. Total hip arthroplasty in children with juvenile chronic arthritis: long-term results. J Pediatr Orthop. 2006;26:8–12. doi: 10.1097/01.bpo.0000187997.84213.d9. [DOI] [PubMed] [Google Scholar]
- 19.Lachiewicz PF, McCaskill B, Inglis A, Ranawat CS, Rosenstein BD. Total hip arthroplasty in juvenile rheumatoid arthritis. Two to eleven-year results. J Bone Joint Surg Am. 1986;68:502–508. [PubMed] [Google Scholar]
- 20.Learmonth ID, Heywood AW, Kaye J, Dall D. Radiological loosening after cemented hip replacement for juvenile chronic arthritis. J Bone Joint Surg Br. 1989;71:209–212. doi: 10.1302/0301-620X.71B2.2925736. [DOI] [PubMed] [Google Scholar]
- 21.Maric Z, Haynes RJ. Total hip arthroplasty in juvenile rheumatoid arthritis. Clin Orthop Relat Res. 1993;290:197–199. [PubMed] [Google Scholar]
- 22.McKellop H, Shen FW, Lu B, Campbell P, Salovey R. Effect of sterilization method and other modifications on the wear resistance of acetabular cups made of ultra-high molecular weight polyethylene. A hip-simulator study. J Bone Joint Surg Am. 2000;82:1708–1725. doi: 10.2106/00004623-200012000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Restrepo C, Lettich T, Roberts N, Parvizi J, Hozack WJ. Uncemented total hip arthroplasty in patients less than twenty-years. Acta Orthop Belg. 2008;74:615–622. [PubMed] [Google Scholar]
- 24.Ruddlesdin C, Ansell BM, Arden GP, Swann M. Total hip replacement in children with juvenile chronic arthritis. J Bone Joint Surg Br. 1986;68:218–222. doi: 10.1302/0301-620X.68B2.3958006. [DOI] [PubMed] [Google Scholar]
- 25.Shia DS, Clohisy JC, Schinsky MF, Martell JM, Maloney WJ. THA with highly cross-linked polyethylene in patients 50 years or younger. Clin Orthop Relat Res. 2009;467:2059–2065. doi: 10.1007/s11999-008-0697-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wangen H, Lereim P, Holm I, Gunderson R, Reikeras O. Hip arthroplasty in patients younger than 30 years: excellent ten to 16-year follow-up results with a HA-coated stem. Int Orthop. 2008;32:203–208. doi: 10.1007/s00264-006-0309-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Witt JD, Swann M, Ansell BM. Total hip replacement for juvenile chronic arthritis. J Bone Joint Surg Br. 1991;73:770–773. doi: 10.1302/0301-620X.73B5.1894663. [DOI] [PubMed] [Google Scholar]