Abstract
Background
Residual acetabular dysplasia of the hip in most patients can be corrected by periacetabular osteotomy. However, some patients have intraarticular abnormalities causing insufficient coverage, containment or congruency after periacetabular osteotomy, or extraarticular abnormalities that limit either acetabular correction or hip motion. For these patients, we believe an additional proximal femoral osteotomy can improve coverage, containment, congruency and/or motion.
Purposes
We provide algorithms for (1) identifying patients we believe will benefit from proximal femoral osteotomy, (2) selecting the appropriate osteotomy, and (3) choosing the sequence of these osteotomies.
Methods
Anteroposterior, false-profile and functional radiographs and MR can identify most patients we believe will benefit from periacetabular and femoral osteotomies. Recently described techniques, including relative femoral neck lengthening, femoral neck osteotomy and femoral head osteotomy have expanded indications for a combined procedure. Historically performed first, periacetabular osteotomy is now frequently performed following femoral osteotomy.
Results
The rate of intertrochanteric osteotomy performed with periacetabular osteotomy has decreased from approximately 10% in the first 500 surgeries to about 2% currently. Among 151 relative neck lengthenings (23 with PAO), 53 femoral neck osteotomies (4 with PAO) and 14 femoral head osteotomies (11 with PAO), eleven complications occurred including osteonecrosis in two and delayed unions in eight. No complication occurred following a combined procedure.
Conclusion
Although isolated periacetabular osteotomy can provide sufficient coverage, containment and congruency for most patients with residual hip dysplasia, some may benefit from an additional proximal femoral osteotomy. Knowing the appropriate indications, selection, and sequencing of these osteotomies is critical for enhancing patient outcomes.
Level of Evidence
Level V, therapeutic study. See Guidelines for Authors for a complete description of levels of evidence.
Introduction
Despite the institution of clinical and ultrasound screening programs, developmental dysplasia of the hip (DDH) remains one of the more frequent causes of secondary osteoarthritis (OA) of the hip [1]. Until the 1970s, the intertrochanteric osteotomy (ITO) was often used to treat residual dysplasia [28]. More recently, ITO has been supplanted by redirectional osteotomies of the acetabulum [39]. The Bernese periacetabular osteotomy (PAO) [8] is one such procedure [19, 32, 34], and has been frequently reported for treating DDH over the past 15 years [3, 16–18, 20, 22, 30, 33].
As our experience with PAO for DDH increased, we realized that correcting the acetabular deformity alone was not always sufficient when treating more complex hip pathomorphologies. Most aberrations of the femoral head and neck [23, 31] leading to femoroacetabular impingement (FAI) after PAO can be treated by osteochondroplasty through an arthrotomy at the time of PAO. However, we believe more severe hip deformities, frequently involving the entire proximal femur, are better treated with a combined acetabular osteotomy and proximal femoral osteotomy (PFO) [4, 8, 24, 37, 38] to improve joint coverage, containment and congruency.
At short-term followup, combined PAO and ITO for severe deformities has been reported to produce Harris hip scores and radiographic measures of deformity correction similar to those of an isolated PAO for more mild deformities [5]. A prior study [12] retrospectively analyzed which clinical and radiographic variables in hips undergoing a PAO were associated with an additional ITO. The femoral head extrusion index after PAO was found to be 7% when a valgus ITO was performed, 30% when a varus ITO was performed and 13% when an isolated PAO was performed. A similar difference with respect to the acetabular index was identified (36.2° for the valgus ITO group, 28.6° for the varus ITO group and 0.2° for the isolated PAO group). Neck-shaft angles averaged 116° in patients who had a valgus ITO, 149° in those who had a varus ITO and 137° in those who had an isolated PAO. The presence of femoral head deformity, osteoarthritis, and previous hip surgery were also associated with the addition of an ITO. A discriminate analysis predicted the actual treatment (PAO with PFO or PAO alone) in 89% of the cases. However, this study [12] was published prior to the introduction of more recent PFOs such as femoral neck osteotomy (FNO), relative femoral neck lengthening (RFNL) and femoral head reduction osteotomy (FHRO), which have further widened the spectrum of indications for performing a PFO [7].
We describe treatment algorithms to identify hips undergoing a PAO that might benefit from a PFO, to select the appropriate PFO, and to choose the best sequence and timing of these osteotomies.
Patients and Methods
The clinical and radiographic indications for a combined PAO/PFO are similar to those for an isolated PAO. Patients should have clinical symptoms and signs directly related to the deformity, such as inguinal and/or trochanteric pain, abductor weakness, or limited hip motion secondary to a high-riding greater trochanter. These can improve following a combined PAO and PFO [5] and, we believe, justify such a complex surgery. On the other hand, globally limited and painful range of motion, osteoarthritis of Tönnis Grade 2 [35] or worse, and older age generally represent contraindications for a combined procedure. However, in well-selected cases, improvement in Harris Hip (60 to 90) and WOMAC (8.7 to 3) scores have been reported 5 years after PAO in those over the age of 40 [20].
The majority of abnormalities requiring a PFO in addition to a PAO can be categorized as either intraarticular or extraarticular. Intraarticular causes can be divided into inadequate improvement of coverage (lateral center-edge angle < 25°, acetabular index > 10°, extrusion index > 30%) [36], containment (distance between ilioischial line and femoral head > 5 to 7 mm), or congruency (nonconcentric joint space with a width > 3 mm) following an isolated PAO. Intraarticular pathologies represent not only the largest but also the most challenging group with respect to decision-making (Fig. 1). Extraarticular causes include a high-riding greater trochanter with a short neck, a deformity not infrequently seen as sequelae of Perthes disease or following the treatment of hip dysplasia in early childhood (Fig. 2), and prior varus ITO.
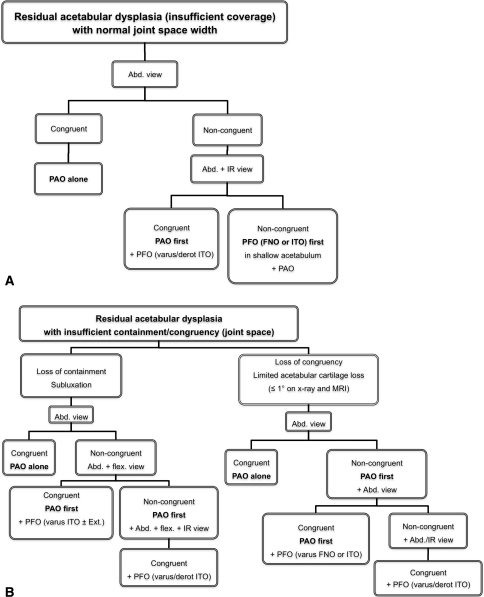
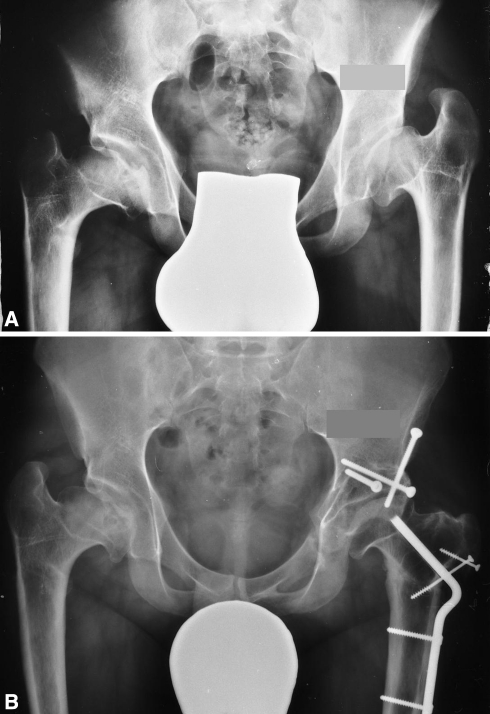
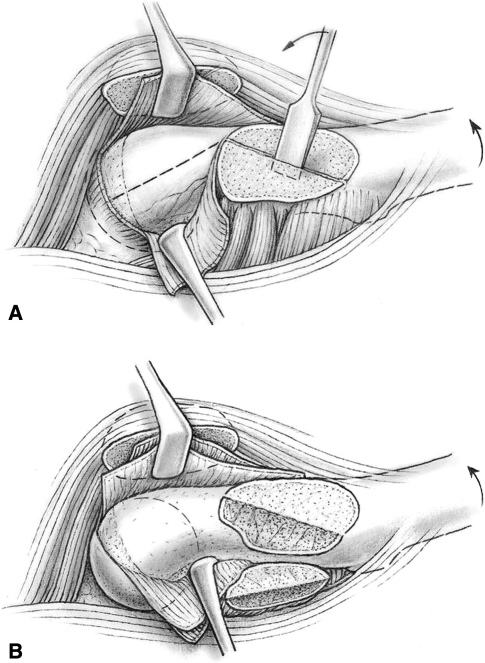
Fig. 1A–B.
(A) This algorithm applies to hips with insufficient coverage and normal joint space. If an abduction view shows good coverage and congruency, PAO alone is indicated. If not, the abduction view is repeated with the hip internally rotated. If congruency is improved, a varus-derotation ITO is performed following the PAO. If relocation of the femoral head remains unsatisfactory, it is preferable to do the PFO first. (B) This algorithm applies to hips with insufficient containment and congruency as well as joint space narrowing. If the narrowing disappears with abduction, subluxation is the cause and PAO alone is indicated. If the narrowing remains, a second abduction view with hip flexion may show the necessary improvement, indicating a PAO together with a PFO (varus ITO +/− extension). If the joint width remains deficient, a third functional radiograph with the addition of internal rotation may show the desired congruency, indicating that the PAO be followed by a varus-derotation ITO. When joint space narrowing is the result of limited cartilage loss (osteoarthritis ≤ Tönnis Grade 1), a congruent abduction view indicates PAO alone is sufficient. If, however, the joint space remains non-congruent, PAO is performed first and followed by an intraoperative abduction view. Not infrequently, this view shows sufficient congruency indicating an additional PFO. If the intraoperative abduction view remains non-congruent, it may be repeated with internal rotation of the hip and then an additional varus-derotation ITO is performed.
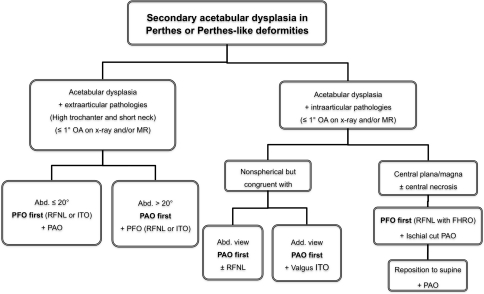
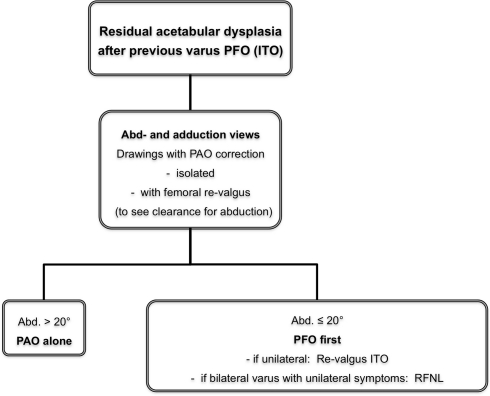
Fig. 2.
Hips with Perthes or Perthes-like deformities and secondary acetabular dysplasia may be governed by extraarticular impingement. When abduction over 20° is possible, the PAO is performed first. The final decision regarding a PFO is determined by intraoperative static and functional views. With abduction 20° or less, it is preferable to start with the PFO to assure sufficient acetabular correction. In more complex hips with intra- and extraarticular pathologies, abduction and adduction views are obtained preoperatively. If the head is severely out of round and too large to be relocated into the acetabulum, a RFNL and FHRO are performed, followed by a PAO. If the pathomorphology is such that a valgus ITO is indicated, the PAO is performed first. In such circumstances, it may be preferable to leave the capsule closed for additional stability of the femoral head.
Standard anteroposterior pelvic, false profile, and functional views (commonly abduction and occasionally adduction) have been the basic imaging modalities used to predict coverage, containment, and congruency following PAO. Differentiation between joint space narrowing caused by anterolateral migration and that caused by cartilage loss can be made with abduction views. Clear improvement of the joint space with abduction indicates that anterolateral subluxation is the cause of the incongruency, and that PAO alone will likely be sufficient (Fig. 3). If the abduction view fails to produce widening of a narrowed joint space, it may be repeated with the hip flexed 10° to 15° and/or internally rotated in the presence of high femoral antetorsion. Joint improvement with this combined view indicates that a PFO may be required in addition to the PAO. An abduction view is also helpful for assessing the adequacy of an isolated PAO for hips with a high fovea. With coxa magna or coxa valga, the high degree of abduction necessary for better containment may indicate that a PAO alone would result in a negative roof angle. Similar to how anterolateral migration can be assessed by abduction radiographs, anterior migration of the head can be estimated by a loss of congruency on the false profile view. These functional views may be repeated intraoperatively to confirm the need for a varus ITO, and to define the necessary angle of correction and amount of derotation, which depends on the clinical range of external and internal rotation (Fig. 4).
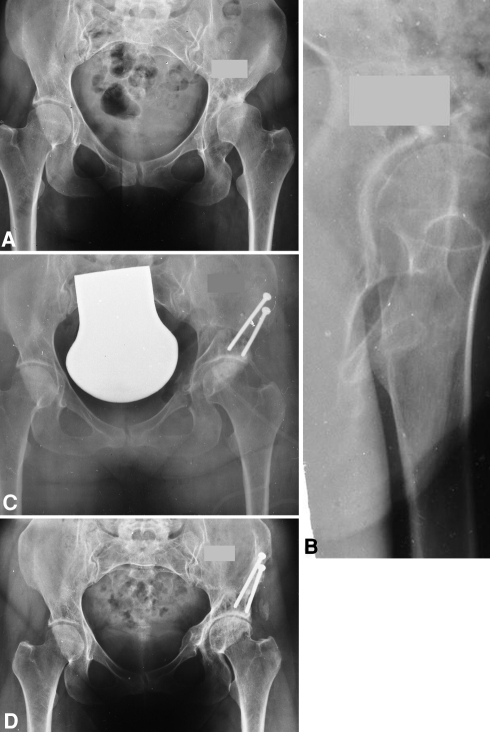
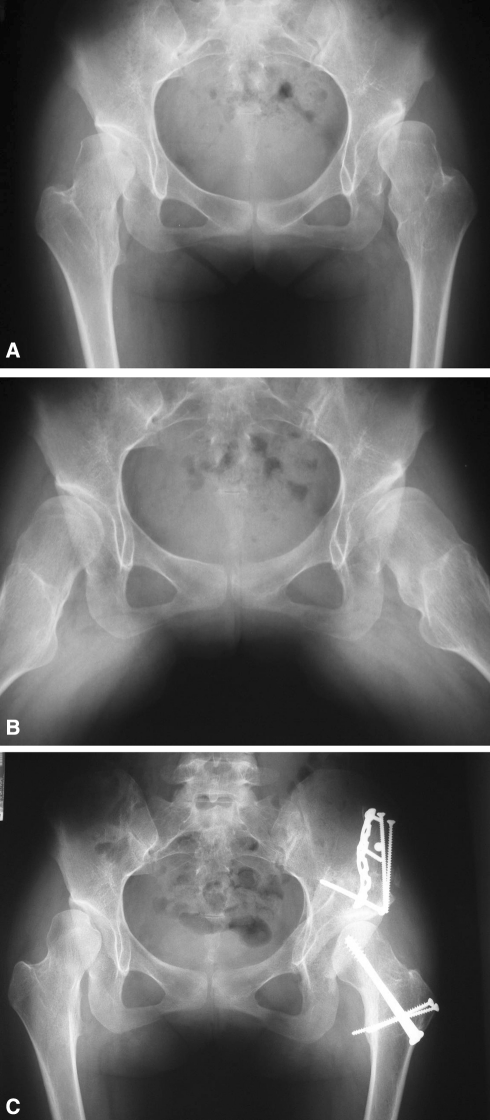
Fig. 3A–D.
(A) This AP pelvic radiograph shows acetabular dysplasia of the left hip with severe joint space narrowing and subchondral sclerosis mimicking advanced OA. (B) However, the false profile view shows normal superior joint space width, indicating anterior subluxation of the femoral head is the cause of narrowing. Fluoroscopic views confirmed the need for PAO by showing normalized joint space width and congruency in flexion-abduction but less improvement in isolated abduction. The patient was informed that an additional PFO may be necessary, but that the final decision would depend on intraoperative radiography after acetabular correction. (C) The postoperative radiograph shows a reasonably wide joint space due to relocation of the femoral head. (D) The joint survived for 15 years before needing replacement.
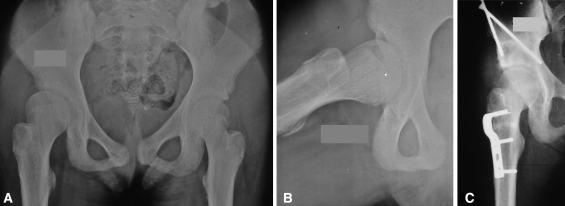
Fig. 4A–C.
(A) This AP pelvic radiograph of a 12 year-old girl shows coxa valga and magna with acetabular dysplasia of the right hip. (B) An abduction view of the right hip shows acceptable congruency but marginal containment, indicating that PFO should be combined with PAO. (C) A varus ITO was performed during the same anesthesia as the PAO after intraoperative functional radiographs confirmed the indication for ITO.
In Perthes and Perthes-like deformities with secondary acetabular dysplasia, the high-riding trochanter may prevent adequate acetabular correction and may lead to the persistence of restricted hip abduction (Fig. 2). This limits the information obtained from abduction radiography and may prevent the detection of concomitant intraarticular impingement. A MR arthrogram may allow further assessment of intraarticular pathology, including possible FAI that may remain after acetabular correction. Additionally, an adduction radiograph can provide information regarding the benefit of a valgus osteotomy, especially for hips with a congruent but nonspherical joint (Fig. 5). With such pathomorphology, a classic trochanteric advancement may be insufficient, but RFNL through a surgical dislocation approach may substantially enhance hip motion [7].
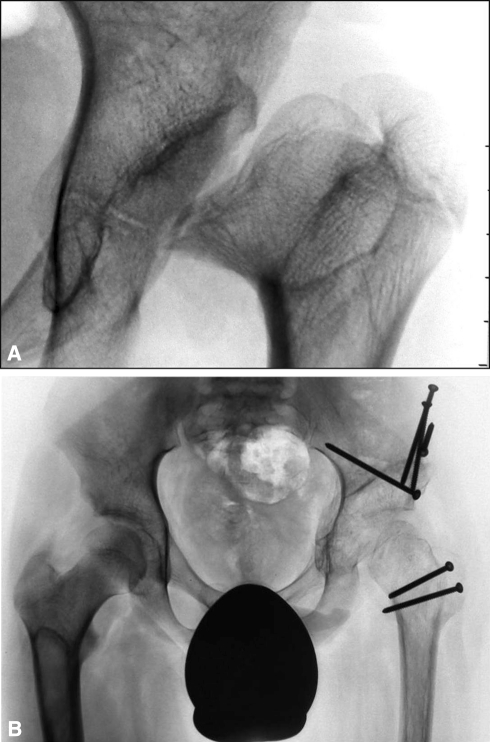
Fig. 5A–B.
(A) This AP pelvic radiograph shows bilateral sequelae of Perthes disease. A high acetabular index, mushroom-shaped femoral head, short neck and high-riding greater trochanter are apparent on the left side, although the joint space remains fairly congruent. (B) The AP radiograph 8 years after combined PAO and valgus ITO with distal advancement of the greater trochanter shows that congruency was maintained and that the acetabular index was normalized.
For hips previously treated with a varus osteotomy, acetabular correction during the PAO may not be restricted but hip motion following the PAO may be limited and become painful over time (Fig. 6). Preoperative drawings with both acetabular reorientation and revalgization of the proximal femur can demonstrate the need for a combined approach. With unilateral varus, the femoral correction may be accomplished by a revalgization ITO with increases in both leg length and abductor lever arm. However, with bilateral varus deformity and unilateral symptoms, relative neck lengthening and trochanteric advancement may be a more effective approach.
Fig. 6.
A history of previous varus ITO can be a particular problem when a PAO is indicated for the treatment of residual acetabular dysplasia. Paper drawings made from functional abduction and adduction views are completed with the desired position of the acetabulum after PAO. An additional paper drawing of the femoral side is rotated around the center of the head until impingement with the acetabulum is encountered. This determines the clearance angle for abduction. This process may be repeated with a revalgization ITO. If the measured abduction is over 20°, a PAO alone is sufficient. If abduction is 20° or less, the clearance may be increased by adding a PFO. In the situation of a unilateral former varus ITO, a revalgization ITO is preferred to equalize limb lengths. When bilateral varus osteotomies are present and one side is asymptomatic and expected to remain so, RFNL with resultant relative valgus is preferred.
If the surgeon presumes cartilage destruction is the primary reason for persistent joint space narrowing in the abduction view, an MR arthrogram may give further information regarding the thickness and structure of the acetabular cartilage. MR can also suggest impending migration by showing a gap between cartilage surfaces. Additionally, the cartilage of the femoral head may be assessed in the anticipation of joint space normalization by a varus osteotomy. If the MR arthrogram shows substantial articular damage, we do not believe joint preservation surgery should be offered, even to patients in their twenties.
In the majority of patients, clinical assessment of hip range of motion, conventional radiographs, and MR arthrography in cases with questionable cartilage will provide adequate information to determine whether we will recommend a PFO. However, the definitive decision for a PFO usually depends on intraoperative and/or postoperative functional views (Fig. 7). Therefore, we obtain patient consent for additional procedures whenever a PFO is considered. The possibility that a varus or extension ITO may lead to subsequent impingement [10] must be considered during surgical planning and managed with appropriate osteochondroplasty.
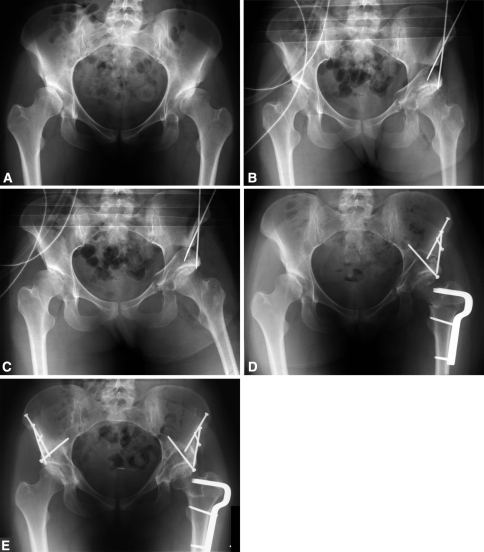
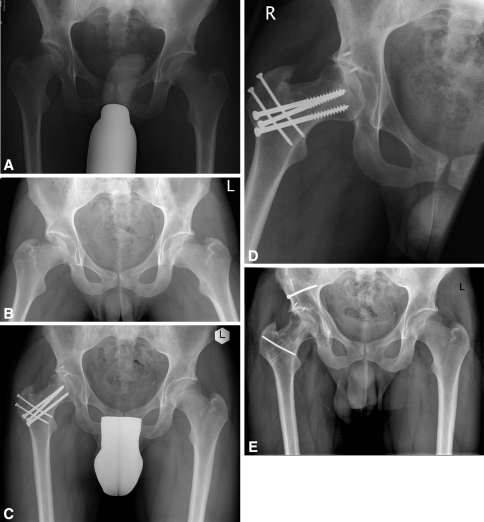
Fig. 7A–E.
(A) This AP pelvic radiograph shows bilateral acetabular dysplasia with marked subluxation and lateral joint space narrowing. (B) An intraoperative AP radiograph after left PAO shows residual lateral joint space narrowing. (C) The intraoperative abduction view shows improved lateral joint space. This indicated a varus ITO, which was performed under the same anesthesia. (D) The postoperative AP radiograph demonstrates good coverage, containment and congruency as well as increased lateral joint space. (E) The AP radiograph 10 years after combined PAO and PFO shows a preserved space.
Historically, PFOs have been intertrochanteric or subtrochanteric osteotomies, which have been used extensively [9, 14, 21, 26, 29] and are accepted as techniques that effectively alter proximal femoral anatomy with low rates and severity of complications. However, since these osteotomies are performed at a distance from the deformity, they produce several side effects. They either medialize or lateralize the femoral shaft and alter the mechanical axis of the lower extremity. They also shorten or lengthen the limb depending on whether a varus or valgus osteotomy is implemented. The more distal these osteotomies are executed, the larger these side effects. In certain circumstances these may be desired effects; however, in the majority of cases, they are undesired consequences. Although most of these side effects can be minimized by choosing an appropriate implant and modifying the surgical technique, unilateral shortening of the femur by varus ITO remains a major problem, especially for female patients.
Recently, osteotomies have been performed at the femoral head and neck levels through the surgical dislocation approach [6]. The key element in executing a RFNL, FNO, or FHRO is the extended retinacular soft-tissue flap, which provides sustained and reliable protection of the blood supply to the femoral head throughout the procedure [7]. To develop the retinacular flap, the posterosuperior portion of the stable trochanter is resected subperiosteally to the level of the femoral neck. In the presence of an open physis, this piece can be mobilized as a single unit. However, with a closed physis, piece-meal resection is necessary. Following resection of the stable trochanter, the retinaculum and posterior periosteum are carefully elevated from the proximal femur to develop a single sleeve of tissue comprised of the retinaculum and external rotators. This flap extends from the lesser trochanter distally to the level at which the retinacular vessels enter the femoral head proximally. A similar subperiosteal dissection, including elevation of Weitbrecht’s ligament, is performed around the medial and posteromedial neck producing one contiguous semi-tubular periosteal sleeve, which contains the blood supply to the epiphysis and allows circumferential access to the neck. The extended length of the flap allows for forces, particularly tension, on the vessels to be better distributed.
One osteotomy performed through this approach is RFNL [7]. This technique effectively treats extraarticular and intraarticular impingement caused by a high-riding greater trochanter and/or a short femoral neck and normalizes muscular and joint biomechanics (Fig. 8). Again, the key element of this osteotomy is the extended retinacular soft-tissue flap, although the flap does not have to be developed circumferentially as with the neck osteotomy (Fig. 9) [7]. RFNL can be performed in combination with osteochondroplasty of the head-neck junction to reduce FAI. This technique has decreased the need for true femoral neck lengthening [40].
Fig. 8A–B.
(A) This AP radiograph of the left hip of a 12 year-old patient shows a deformity of unknown etiology with necrosis of the medial portion of the femoral head. Severe subluxation, a short neck and high-riding greater trochanter are apparent, along with secondary acetabular dysplasia. The femoral approach was performed first to reshape the femoral head and allow its relocation into the acetabulum. Again, the first ischial cut of the PAO was executed via the femoral approach. (B) The AP radiograph 18 months after surgery is shown. The remodeled femoral head is well-centered, the neck is longer, the greater trochanter is advanced and the acetabulum is oriented correctly.
Fig. 9A–B.
(A) This schematic drawing shows the first step of the extended retinacular soft-tissue flap during the surgical hip dislocation approach. After Z-shaped capsulotomy, the posterosuperior portion of the stable trochanter is trimmed down to the level of the neck. With an open physis, it is easier to mobilize this as one piece since this piece must be resected subperiosteally. With a closed physis, a subperiosteal piece-meal resection is necessary. (B) Following resection of the stable trochanter, the retinaculum and the posterior periosteum are carefully dissected from bone in one piece to develop a retinaculum-external rotators flap from the lesser trochanter to the level of perforation of the retinacular vessels into the epiphysis. A similar subperiosteal dissection is subsequently performed around the medial and posteromedial neck, including Weitbrecht’s ligament, to ultimately create one contiguous semitubular periosteal sleeve that contains the blood supply to the epiphysis and allows circumferential access to the neck. The extended length of the flap allows better distribution of adverse forces, especially stretching, on the vessels. (Reprinted with permission from Leunig M, Slongo T, Ganz R. Subcapital realignment in slipped capital femoral epiphysis: Surgical hip dislocation and trimming of the stable trochanter to protect the perfusion of the epiphysis, In: Duwelius PJ, Azar FM (eds). Instructional Course Lectures 57. Rosemont, IL: American Academy of Orthopaedic Surgeons; 2008:499–507.)
Another intracapsular osteotomy, FNO, produces corrections that are closer to the deformity, more effective in influencing the superior joint space and result in less medialization/lateralization of the femoral shaft and less alteration of limb-length than an ITO. Also, the heads of the screws used for fixation of the femoral neck osteotomy are less noticeable and irritating to the patient compared to the lateral plating used for fixation of an ITO (Fig. 10). The presence of a previous ITO reportedly does not influence the long-term survival of THA [2, 11]. We expect that FNO will also not decrease subsequent THA survival and will, additionally, lessen the technical difficulty of total hip conversion compared to that following an ITO [2].
Fig. 10A–C.
(A) This AP pelvic radiograph of a patient with multiple exostoses demonstrates bilateral complex hip dysplasia characterized by shallow acetabula marked coxa valga and exostoses of the posterior neck. On the left side, the exostosis was impinging against the ischium, an occurrence accentuated by the small head-neck offset. (B) An abduction view shows good congruency between the acetabular roof and femoral head but minimal head-neck offset. (C) The postoperative radiograph 1 year after combined acetabular and femoral surgery is shown. The femoral approach was performed first to increase the head-neck offset. A varus closing-wedge FNO was executed using the extended retinacular soft tissue flap that also allowed easy resection of the posterior exostosis. The femoral approach was also used for direct access to the ischial osteotomy site of the PAO.
Certain hips with marked residual DDH are associated with deformities of the femoral head that cannot be corrected by a classic PFO since the head itself must be reshaped. The deformity may involve the medial or the lateral contour of the head or exhibit coxa plana with medial and lateral convexity, complicated by subluxation or severe extrusion. These complex deformities may benefit from the addition of a FHRO [7]. Once again, the key element of this osteotomy is the extended retinacular flap that allows preservation of the blood supply to the medial and lateral portions of the head while a central section is resected. Although the femoral head can be sufficiently perfused by the superior retinacular branches of the medial femoral circumflex artery alone, there is a constant branch of the medial femoral circumflex artery that runs within Weitbrecht’s ligament and supplies a medial sector of the epiphysis [7]. Therefore, the blood supply to the femoral head can be preserved while a central segment of the head is resected. While the medial epiphyseal pillar remains connected with the metaphysis, the lateral pillar, supplied by vessels within the retinacular flap, is osteotomized from the metaphysis to allow the resection gap to be closed and the cartilage surfaces to be adjusted. This procedure produces a smaller and rounder head that can stably be reduced into the reoriented socket (Fig. 11).
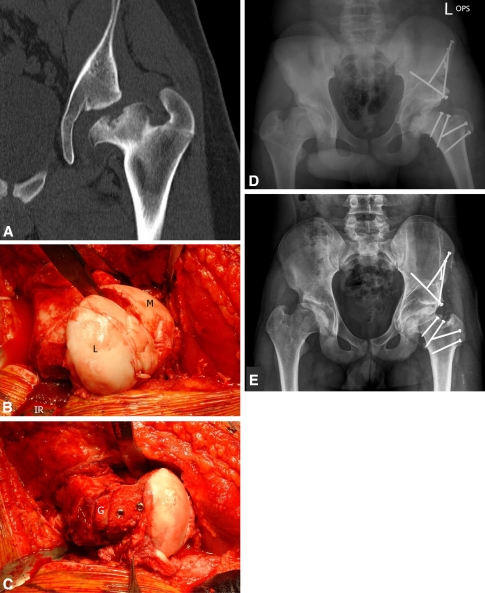
Fig. 11A–E.
(A) Coronal CT cut of a 15 year-old with Perthes disease showing an enlarged femoral head with central necrosis hinging on the acetabular rim. Also seen are a short neck, high-riding greater trochanter and partially convex and dysplastic acetabulum. To recenter and recontour the femoral head, its transverse diameter must be reduced. (B) This intraoperative photo shows resection of the central head segment. The stable medial portion (M) is perfused by the medial branch of the medial femoral circumflex artery while the mobile lateral segment (L) is perfused by retinacular vessels protected by the inferior retractor (IR). (C) The lateral gap is filled with autologous graft (G) and the new head is fixed with screws. The forceps points towards the retinaculum. The ischial osteotomy of the PAO was performed through this incision after abduction radiographs verified the head position. (D) A postoperative radiograph demonstrates a well-centered femoral head within the reoriented acetabulum, reasonable neck length and advanced greater trochanter. (E) A radiograph three years postoperatively shows reasonable joint space.
As previously mentioned, preoperative radiographic evaluation of obtainable coverage, containment, and congruency will identify the majority of hips in need of an adjunctive PFO in addition to PAO [12]. When performing a combined PAO/PFO, we previously completed the PAO first unless the proximal femoral deformity prevented acetabular reorientation. The reasoning was that the amount of acetabular correction is predetermined by the need to achieve a nearly horizontal roof and a neutral version, both of which can be estimated with an intraoperative orthograde radiograph of the pelvis. In contrast, the correction on the femoral side does not have such defined limits and can more easily be adjusted to the conditions of each case. Recently, we have adhered less strictly to this guideline. When using the surgical dislocation approach to make intracapsular corrections, the ischial cut at the infracotyloid groove can be made under direct visualization by developing the interval between the inferior gemellus and obturator externus muscles. Simultaneously, the sciatic nerve can be visualized and appropriately retracted (Fig. 12). Performing the incomplete osteotomy of the ischium at this point adds very little time. The patient can be positioned and prepped in a way that both the lateral and anterior incisions are included and, therefore, reprepping is not needed when changing from the lateral to supine position. If necessary, the surgeon can return to the lateral approach after performing the PAO. For these reasons, it is preferable to perform the femoral and acetabular corrections under one general anesthetic.
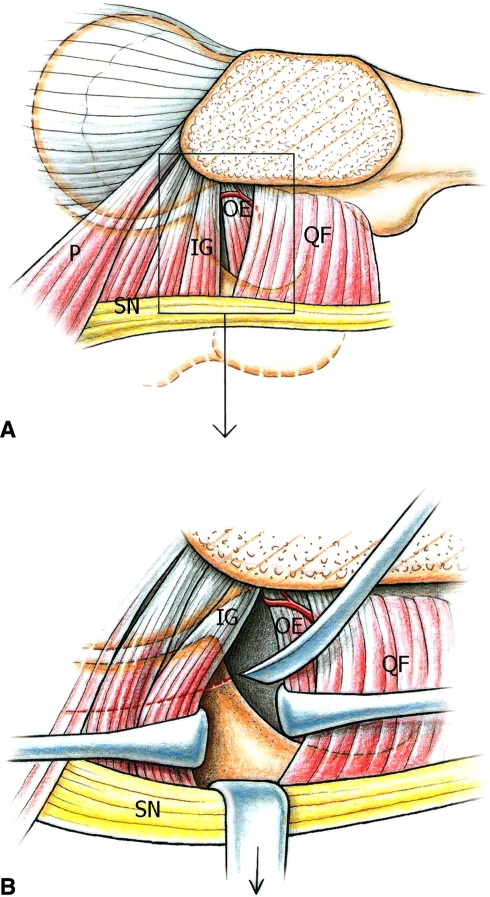
Fig. 12A–B.
(A) This drawing shows the approach to the ischium through a lateral incision for performing the first ischial osteotomy of the PAO. The gap between inferior gemellus and obturator externus/quadratus femoris muscles is identified by palpation before it is visualized. If dissection remains close to the ischium and distant from the tendon insertion, interference with the deep branch of the medial femoral circumflex artery can be avoided. Tension of the sciatic nerve can be decreased with flexion of the knee and the nerve is carefully retracted throughout the procedure. (B) The osteotomy is performed after visualizing the posteroinferior border of the acetabulum. This can be performed without or with a trochanteric osteotomy as shown here: piriformis (P); inferior gemellus (IG); obturator externus (OE); quadratus femoris (QF); sciatic nerve (SN).
In some cases, a PAO may be indicated for hips with lateral joint space narrowing and MR evidence of acetabular cartilage damage, but with a widened and congruent joint space in the abduction view. For these patients it is wise to obtain preoperative consent for a PFO in case the intraoperative AP radiograph after PAO does not show a sufficiently widened and congruent joint space but the abduction film does. In this rare instance, the PFO is performed after the PAO under the same anesthesia (Fig. 7). Likewise, hips with acceptable acetabular morphology but a pronounced femoral deformity are a special challenge, for which preoperative evaluation may indicate a femoral procedure only. However, residual problems may be encountered which would lead to the recommendation of a PAO at a later time (Fig. 13). Although such rare exceptions for performing the PAO and PFO as staged procedures do exist, the general goal should be to perform both osteotomies under one anesthesia.
Fig. 13A–E.
(A) This AP pelvic radiograph of a 19 year-old patient shows marginal acetabular dysplasia, acetabular retroversion, nonspherical extension of the femoral epiphysis and a short neck. MR indicated that the femoral reshaping required would exceed that achievable through a capsulotomy at the time of PAO and that acetabular reorientation would not be prudent due to anterolateral acetabular cartilage damage. (B) An abduction view of the right hip shows good congruency and containment, suggesting an isolated femoral approach with reshaping of the head-neck junction, RFNL and varus osteotomy should be sufficient. Following RFNL and osteochondroplasty, an intraoperative abduction radiograph showed congruent joint surfaces, Therefore, it was decided to perform a varus osteotomy of the femoral neck instead of a PAO. (C) A postoperative AP pelvic radiograph showed slight lateral joint space narrowing. (D) Repeat abduction radiography, more than one year after the femoral surgery, showed joint space widening and indicated that a PAO should be performed. (E) An AP pelvic radiograph two years after PAO is shown.
Results
Over the last 25 years, we have reduced our use of the combined PAO/ITO. In an earlier series of over 500 PAO’s [12], the frequency of combined PAO/ITO was nearly 10% (46 combined procedures). In a recent review of 100 cases, we observed a 2% rate (2 cases) of combined PAO/ITO (Ganz R., unpublished data). This decline is largely due to the fact that the earlier study [12] contained more patients who had previously been treated with a varus ITO. To a lesser degree, the decline is influenced by the decision to perform a FNO instead of an ITO. Complications occurred in 8% (4 of 48 cases) of all patients in these two series treated with combined PAO/ITO (Table 1). There were two cases of subsequent osteonecrosis (ON) of the femoral head that required conversion to THA. They both occurred in hips treated with a revalgization ITO secondary to a prior varus ITO. Two additional hips required refixation following improper placement of the blade plate and subsequent failure of fixation.
Table 1.
Postoperative complications of proximal femoral osteotomies (PFO)
| Treatment | ITO | RFNL | FNO | FHRO |
|---|---|---|---|---|
| Number of cases | 48 | 151 | 53 | 14 |
| Cases plus PAO | 48 | 23* | 4* | 11* |
| Age range (yrs) | 19–39 | 10–41 | 9–34 | 9–21 |
| Osteonecrosis | 2 | – | 2 | – |
| Failure trochanter | – | 3 | – | – |
| Failure osteotomy | 2 | – | 5 | – |
| Neck fracture | – | 1 | – | – |
ITO (ITO, intertrochenteric osteotomy; RFNL, relative femoral neck lengthening; FNO, femoral neck osteotomy; FHRO, femoral head reduction osteotomy).
* no complication.
Since 1998, RFNL has been performed in 151 cases, excluding those in which an additional femoral procedure such as a subcapital realignment osteotomy or FNO was performed. There were a total of four complications among these 151 cases. One patient over 40 years fell in the immediate postoperative period and incurred a femoral neck fracture that required conversion to THA. Three hips had delayed unions of the trochanteric osteotomy that were treated with refixation. None of the 151 cases developed ON. In the subgroup of 23 patients treated with PAO/RFNL, none had complications.
An isolated FNO has been performed in 49 hips since 2000, including four hips with substantial deformity after SCFE that were treated with a closing-wedge flexion FNO. One of these 49 hips subsequently underwent a PAO and four additional hips have been treated with a combined PAO/FNO. Complications occurred in 14% (7 of 49) of cases treated with FNO alone. There was delayed union of the neck osteotomy in five hips, including four of the 12 hips that underwent opening-wedge osteotomy. All five were treated with hardware exchange. Two hips developed ON, even though the epiphysis was bleeding throughout surgery in both cases. Possible causes of ON include excessively tight closure of the capsule as observed by Nötzli et al. [25], tamponade secondary to a hematoma and a retinacular fold under the refixed trochanter leading to compression of the retinacular vessels. There have been no additional cases of ON within the last 5 years, although more than half of the FNOs were performed during this period. No complication occurred in the five hips that underwent both PAO and FNO.
Since 2001, FHRO has been performed in 14 hips. Eight hips were also treated with a PAO at the time of the index procedure, and three subsequently underwent PAO at a later date; all PAOs were performed to improve coverage. In an earlier case, a varus ITO was successfully completed 8 weeks postoperatively to prevent subluxation of the femoral head. In another hip, a Colonna procedure was performed in addition to the FHRO. Therefore, only one of 14 cases did not require additional surgery to stabilize the reduced head within the secondarily deformed acetabulum. None of the 14 hips developed ON.
Discussion
The combination of PAO and PFO is not new. A PAO was performed by one of the authors (RG) in 1984 and combined with a revalgization ITO to enhance joint congruency; this patient continues to function well today [33]. In our initial experience, the need to restore normal femoral anatomy after previous varus ITO was the most frequent indication for an additional PFO. Recently, new techniques such as RFNL, FNO, and FHRO have expanded the indications for PFO, although the overall number of these combined procedures has decreased.
Even though PAO can correct the majority of dysplastic acetabula, a PFO may further improve joint coverage, containment, or congruency. Trousdale et al. [38], who reported a combined surgery rate of nearly 30% among hips with osteoarthritis greater than Grade 1, described that survivorship decreased with increasingly degenerative changes. However, they did not specifically assess the subgroup with additional ITO. Mayo et al. [18] evaluated the effectiveness of PAO in treating patients with and without previous hip surgery. Intermediate-term Harris hip and Merle d’Aubigné scores were similar for both groups. Additionally, no major differences were found with respect to acetabular coverage, Tönnis arthrosis grade and complication rate. Clohisy et al. [5] demonstrated that combined procedures for complex deformities with lower clinical scores provide similar outcomes to isolated PAOs for simpler deformities.
Recently, intracapsular osteotomies have increased the spectrum of treatable conditions to now include hips with severe intracapital step deformities [7]. These osteotomies have the distinct advantage of increased comfort for the patient as compared to classic ITO. The ability to perform these osteotomies with low rates of ON is a result of a detailed understanding of the vascularity of the femoral head [13] and the capacity to maintain this blood supply with an extended retinacular soft-tissue flap [7]. All intracapsular osteotomies, particularly the FNO, are susceptible to technical errors, leading others to discontinue performing these procedures [27]. In our experience, the morbidity of surgical hip dislocation, RFNL, FNO, and even FHRO (0% to 17% depending on the osteotomy) [7] is low and continues to decrease with experience. We had two unfortunate cases of ON during our early series of FNO, but have had no additional cases for the last 5 years. Due to prolonged consolidation time, opening-wedge FNO is performed infrequently.
While the optimal position of the acetabulum is similar for all hips, the range of acceptable proximal femoral positions is considerably wider. This led to the “PAO first” principle that dictated the sequence of early combined procedures, especially those without femoral obstacles to acetabular correction (extraarticular impingement). Other surgeons, apparently with more rigid femoral parameters, recommended starting with the femoral side [37]. With an increasing utilization of intracapsular surgery, our protocol has also partially moved towards “PFO first”. The accessibility of the ischium provided by the femoral approach, as well as direct visualization of the sciatic nerve, made this an obvious decision. With the surgical dislocation approach, one could argue that both the acetabular reorientation and proximal femoral procedures could be performed through one incision as with the rotational acetabular osteotomy (RAO) [15, 24]. However, capsulotomy is explicitly avoided with spherical osteotomies due to the tenuous acetabular perfusion (40). Although preservation of the blood supply to the osteotomized periacetabular bone from extra-pelvic vessels is possible, it is delicate and time consuming [15]. Therefore, we use this approach infrequently and only under favorable morphological conditions.
In conclusion, we believe combined acetabular osteotomy and PFO is appropriate for select, complex deformities of the hip. In our experience, the recently described intracapsular techniques provide advantages over the classic ITO for certain morphological conditions. However, these procedures, particularly the technically demanding techniques of FNO and FHRO, require further assessment of outcomes and complications. When one of these PFOs is indicated, the first ischial cut of the PAO can be performed directly and under visual control of the sciatic nerve via this approach. In the absence of a clear contraindication, it is preferable to complete both procedures under one anesthesia. Returning at a later date to perform a subsequent PFO or PAO should be a rare exception.
Footnotes
Each author certifies that he or she has no commercial associations (eg, consultancies, stock ownership, equity interest, patent/licensing arrangements, etc) that might pose a conflict of interest in connection with the submitted article.
Each author certifies that his or her institution approved or waived approval for the human protocol for this investigation and that all investigations were conducted in conformity with ethical principles of research.
This work was performed at the University of Berne, Switzerland.
References
- 1.Aronson J. Osteoarthritis of the young adult hip: etiology and treatment. Instr Course Lect. 1986;35:119–128. [PubMed] [Google Scholar]
- 2.Boos N, Krushell R, Ganz R, Muller ME. Total hip arthroplasty after previous proximal femoral osteotomy. J Bone Joint Surg Br. 1997;79:247–253. doi: 10.1302/0301-620X.79B2.6982. [DOI] [PubMed] [Google Scholar]
- 3.Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL. Periacetabular osteotomy for the treatment of severe acetabular dysplasia. J Bone Joint Surg Am. 2005;87:254–259. doi: 10.2106/JBJS.D.02093. [DOI] [PubMed] [Google Scholar]
- 4.Clohisy JC, Nunley RM, Curry MC, Schoenecker PL. Periacetabular osteotomy for the treatment of acetabular dysplasia associated with major aspherical femoral head deformities. J Bone Joint Surg Am. 2007;89:1417–1423. doi: 10.2106/JBJS.F.00493. [DOI] [PubMed] [Google Scholar]
- 5.Clohisy JC, St John LC, Nunley RM, Schutz AL, Schoenecker PL. Combined periacetabular and femoral osteotomies for severe hip deformities. Clin Orthop Relat Res. 2009;467:2221–2227. doi: 10.1007/s11999-009-0810-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ganz R, Gill TJ, Gautier E, Ganz K, Krugel N, Berlemann U. Surgical dislocation of the adult hip a technique with full access to the femoral head and acetabulum without the risk of avascular necrosis. J Bone Joint Surg Br. 2001;83:1119–1124. doi: 10.1302/0301-620X.83B8.11964. [DOI] [PubMed] [Google Scholar]
- 7.Ganz R, Huff TW, Leunig M. Extended retinacular soft-tissue flap for intra-articular hip surgery: surgical technique, indications, and results of application. Instr Course Lect. 2009;58:241–255. [PubMed] [Google Scholar]
- 8.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988;232:26–36. [PubMed] [Google Scholar]
- 9.Ganz R, MacDonald SJ. Indications and modern techniques of proximal femoral osteotomies in the adult. Sem Arthroplasty. 1997;8:38–50. [Google Scholar]
- 10.Ganz R, Parvizi J, Beck M, Leunig M, Notzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;417:112–120. doi: 10.1097/01.blo.0000096804.78689.c2. [DOI] [PubMed] [Google Scholar]
- 11.Haverkamp D, Jong PT, Marti RK. Intertrochanteric osteotomies do not impair long-term outcome of subsequent cemented total hip arthroplasties. Clin Orthop Relat Res. 2006;444:154–160. doi: 10.1097/01.blo.0000194066.10227.1e. [DOI] [PubMed] [Google Scholar]
- 12.Hersche O, Casillas M, Ganz R. Indications for intertrochanteric osteotomy after periacetabular osteotomy for adult hip dysplasia. Clin Orthop Relat Res. 1998;347:19–26. doi: 10.1097/00003086-199802000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Kalhor M, Beck M, Huff TW, Ganz R. Capsular and pericapsular contributions to acetabular and femoral head perfusion. J Bone Joint Surg Am. 2009;91:409–418. doi: 10.2106/JBJS.G.01679. [DOI] [PubMed] [Google Scholar]
- 14.Leunig M, Puloski S, Beck M, Siebenrock K, Ganz R. Proximal femoral osteotomy: Current indications and techniques. Sem Arthroplasty. 2005;16:53–62. doi: 10.1053/j.sart.2004.12.006. [DOI] [Google Scholar]
- 15.Leunig M, Rothenfluh D, Beck M, Nork SE, Gautier E, Kerboull M, Ganz R. Surgical dislocation and periacetabular osteotomy through a posterolateral approach: a cadaveric feasibility study and intial clinical experience. Oper Tech Orthop. 2004;14:49–57. doi: 10.1053/j.oto.2004.04.005. [DOI] [Google Scholar]
- 16.Leunig M, Siebenrock KA, Ganz R. Rationale of periacetabular osteotomy and background work. Instr Course Lect. 2001;50:229–238. [PubMed] [Google Scholar]
- 17.Matta JM, Stover MD, Siebenrock K. Periacetabular osteotomy through the Smith-Petersen approach. Clin Orthop Relat Res. 1999;363:21–32. [PubMed] [Google Scholar]
- 18.Mayo KA, Trumble SJ, Mast JW. Results of periacetabular osteotomy in patients with previous surgery for hip dysplasia. Clin Orthop Relat Res. 1999;363:73–80. doi: 10.1097/00003086-199906000-00010. [DOI] [PubMed] [Google Scholar]
- 19.Miller NH, Krishnan SG, Kamaric E, Noble PC. Long-term results of the dial osteotomy in the treatment of high-grade acetabular dysplasia. Clin Orthop Relat Res. 2005;433:115–123. doi: 10.1097/01.blo.0000153992.17554.67. [DOI] [PubMed] [Google Scholar]
- 20.Millis MB, Kain M, Sierra R, Trousdale R, Taunton MJ, Kim YJ, Rosenfeld SB, Kamath G, Schoenecker P, Clohisy JC. Periacetabular osteotomy for acetabular dysplasia in patients older than 40 years: a preliminary study. Clin Orthop Relat Res. 2009;467:2228–2234. doi: 10.1007/s11999-009-0824-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Millis MB, Murphy SB, Poss R. Osteotomies about the hip for the prevention and treatment of osteoarthrosis. Instr Course Lect. 1996;45:209–226. [PubMed] [Google Scholar]
- 22.Murphy SB, Millis MB. Periacetabular osteotomy without abductor dissection using direct anterior exposure. Clin Orthop Relat Res. 1999;364:92–98. doi: 10.1097/00003086-199907000-00013. [DOI] [PubMed] [Google Scholar]
- 23.Myers SR, Eijer H, Ganz R. Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:93–99. doi: 10.1097/00003086-199906000-00012. [DOI] [PubMed] [Google Scholar]
- 24.Ninomiya S, Tagawa H. Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg Am. 1984;66:430–436. [PubMed] [Google Scholar]
- 25.Notzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002;84:556–560. doi: 10.1302/0301-620X.84B4.12014. [DOI] [PubMed] [Google Scholar]
- 26.Poss R. Intertrochanteric osteotomy in osteoarthritis of the hip. Instr Course Lect. 1986;35:129–143. [PubMed] [Google Scholar]
- 27.Rebello G, Spencer S, Millis MB, Kim YJ. Surgical dislocation in the management of pediatric and adolescent hip deformity. Clin Orthop Relat Res. 2009;467:724–731. doi: 10.1007/s11999-008-0591-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Santore RF, Turgeon TR, Phillips WF, III, Kantor SR. Pelvic and femoral osteotomy in the treatment of hip disease in the young adult. Instr Course Lect. 2006;55:131–144. [PubMed] [Google Scholar]
- 29.Schatzker J. The intertrochnateric osteotomy. Berlin: Springer Verlag; 1984. [Google Scholar]
- 30.Siebenrock KA, Leunig M, Ganz R. Periacetabular osteotomy: the Bernese experience. Instr Course Lect. 2001;50:239–245. [PubMed] [Google Scholar]
- 31.Siebenrock KA, Scholl E, Lottenbach M, Ganz R. Bernese periacetabular osteotomy. Clin Orthop Relat Res. 1999;363:9–20. doi: 10.1097/00003086-199906000-00003. [DOI] [PubMed] [Google Scholar]
- 32.Steel HH. Triple osteotomy of the innominate bone. J Bone Joint Surg Am. 1973;55:343–350. [PubMed] [Google Scholar]
- 33.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008;466:1633–1644. doi: 10.1007/s11999-008-0242-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sutherland DH, Greenfield R. Double innominate osteotomy. J Bone Joint Surg Am. 1977;59:1082–1091. [PubMed] [Google Scholar]
- 35.Tönnis D. Congenital Dysplasia and Dislocation of the Hip in Children and Adults. New York, NY: Springer; 1987. [Google Scholar]
- 36.Tönnis D, Itoh K, Heinecke A, Behrens K. The management of congenital hip luxation with arthrographic control, an individual risk-reducing and time-saving method. I. Choice of method and risk assessment based on arthrographic findings [in German] Z Orthop Ihre Grenzgeb. 1984;122:50–61. doi: 10.1055/s-2008-1044584. [DOI] [PubMed] [Google Scholar]
- 37.Tönnis D, Kasperczyk W. Acetabulum reorientation osteotomies: acetabuloplasty, spherical osteotomy, triple osteotomy of the pelvis. In: Reynolds D, Freeman M, editors. Osteoarthritis in the Young Adult Hip. Edinburgh, Scotland: Churchill Livingstone; 1989. pp. 85–119. [Google Scholar]
- 38.Trousdale RT, Ekkernkamp A, Ganz R, Wallrichs SL. Periacetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg Am. 1995;77:73–85. doi: 10.2106/00004623-199501000-00010. [DOI] [PubMed] [Google Scholar]
- 39.Turgeon TR, Phillips W, Kantor SR, Santore RF. The role of acetabular and femoral osteotomies in reconstructive surgery of the hip: 2005 and beyond. Clin Orthop Relat Res. 2005;441:188–199. doi: 10.1097/01.blo.0000193541.72443.73. [DOI] [PubMed] [Google Scholar]
- 40.Wagner H. Femoral osteotomies for congenital hip dislocation. In: Weil UH, editor. Acetabular Dysplasia, Skeletal Dysplasias in Childhood. Berlin, Germany: Springer-Verlag; 1978. pp. 85–105. [Google Scholar]