Abstract
Background
Hip resurfacing arthroplasty is a common procedure that improves functional scores and has a reported survivorship between 95% and 98% at 5 years. However, most studies are reported from the pioneering rather than independent centers or have relatively small patient numbers or less than five years followup. Various factors have been implicated in early failure.
Questions/purposes
Our purposes were to determine: (1) the midterm survival of the BHR; (2) the function in patients treated with hip resurfacing; and (3) whether age, gender, BMI, or size of components related to failure.
Methods
We reviewed the first 302 patients (329 hips) on whom we performed resurfacing arthroplasty. We assessed the survivorship, change in functional hip scores (HHS, OHS, WOMAC, UCLA), and analyzed potential risk factors (age, gender, BMI, component size) for failure. The mean age at the time of surgery was 56.0 years (range, 28.2–75.5 years). The minimum followup was 5 years (mean, 6.6 years; range, 5–9.2 years).
Results
Kaplan-Meier analysis showed survival of 96.5% (95% CI, 94.7–98.4) at 9 years taking revision for any cause as the endpoint. All functional hip scores (HHS, OHS, WOMAC, UCLA) improved. Survivorship was higher in men compared with women. The component sizes and body mass index were smaller in the revised group compared with the nonrevised group.
Conclusions
Medium-term survivorship and functional scores of hip resurfacing are comparable to those from the pioneering center. Hip resurfacing remains a good alternative to THA, particularly in the younger male population with relatively large femoral head sizes.
Level of Evidence
Level IV, therapeutic study. See the Guidelines for Authors for a complete description of levels of evidence.
Introduction
Over the last decade, hip resurfacing has become an increasingly common option, predominantly for younger patients with greater physical demand particularly because the revision rates of conventional THA in younger patients are generally higher, ranging from 12% to 67% at 4.5 to 16.2 years [7, 15, 24, 28, 34]. However, Marker et al. [35] reported similar functional hip scores and radiographic assessment in a recent review of the literature comparing hip resurfacing with THA, although a number of studies included in the review did show better clinical outcomes after hip resurfacing [35]. In addition to this, Killampalli et al. [27] reported no differences in functional scores in young patients treated with hip resurfacing compared with THA at a minimum 5-year followup. Despite this, hip resurfacing as an alternative to conventional THA does offer a number of advantages: preservation of the metaphyseal and diaphyseal femoral bone; improved radiographic biomechanical parameters of the hip e.g. femoral offset [16, 45]; larger femoral head sizes reducing the risk of dislocation [9]; and improved wear properties of the metal-on-metal bearing surfaces [23, 36].
Various studies from one pioneering center have reported survivorship of up to 99.8% at a mean of 3.3 years [11] and 98% at 5 years [48] with the Birmingham Hip Resurfacing (BHR; Smith & Nephew, Memphis, TN). Other independent series have reported survivorship with the BHR of up to 99% at 3 years [4] and 96.3% at 5 years [22], although this has been on smaller numbers of patients or studies with followup of 5 years or less. Similar survivorship has also been reported using other brands of hip resurfacing with a 94% survival at 3.4 years [39] and 94% survivorship at 5.5 years [1] using the Conserve Plus hip resurfacing (Wright Medical Technology Inc, Arlington, TN). More recently, other studies with longer followup have also reported midterm survivorship of 95.7% at 7 years [26] and 95% at 8 years [47].
Various studies have also reported substantial improvements in activity levels and functional hip scores after hip resurfacing [1, 11, 22, 39, 42, 48]. In addition, Marker et al. [35] reviewed various comparative studies and found conflicting observations with some studies showing patients with hip resurfacing had higher postoperative activity levels than patients who underwent THA, while other studies [35] demonstrated similar clinical hip scores. Patient selection for hip resurfacing is particularly important and a number of risk factors for failure have been reported [43], including increasing age, female gender [3, 8], low body mass index (BMI) [29], and smaller component sizes [3].
To confirm these previous findings we determined: (1) the midterm survival of the BHR; (2) the functional scores in patients treated with hip resurfacing; and (3) asked whether age, gender, BMI, or size of components related to failure.
Patients and Methods
We retrospectively reviewed all 302 patients (329 hips) who underwent resurfacing arthroplasty between May 2000 and June 2004 and the data were collected prospectively. The most common indication was primary osteoarthritis (Table 1). In general, the operation was offered to men younger than age 65 years and women younger than age 60 years with good bone stock as judged on plain radiographs. Contraindications were severe bone loss of femoral head; multiple large femoral head or neck cysts (greater than 1 cm); severe osteopenia or osteoporosis as assessed using dual-energy xray absorptiometry if bone stock was questionable on plain radiographs; and known metal sensitivity. During the study period, we performed 1475 conventional THAs in 1187 patients. All patients had a BHR; this implant is currently the most widely used resurfacing prosthesis, accounting for 47% of all hip resurfacings and 9% of primary hip procedures in the United Kingdom [41]. Among the 302 patients, there were 89 women and 213 men. The mean age at the time of surgery was 56.0 years (range, 28.2–75.5 years). Twenty-seven patients had bilateral procedures, all of which were staged surgeries. Two of the 302 patients were lost to followup and were included in the statistical analysis for both preoperative to postoperative differences in functional hip scores and survivorship analysis up until the last recorded followup. Six patients died during the study period for reasons unrelated to their hip procedure and were also included in the analysis up until the last followup as for the patients who were lost to followup. The minimum followup was 5 years (mean, 6.6 years; range, 5–9.2 years).
Table 1.
Summary of preoperative diagnoses
| Diagnosis | Number of hips (%) |
|---|---|
| Osteoarthritis | 304 (92.4) |
| Dysplasia | 8 (2.4) |
| Avascular necrosis | 4 (1.2) |
| Rheumatoid arthritis | 3 (0.9) |
| Ankylosing spondylitis | 2 (0.6) |
| Other* | 8 (2.4) |
| Total | 329 |
* Includes osteoarthritis secondary to slipped upper femoral epiphysis and Perthes.
All patients underwent a standard pre- and postoperative regimen performed by a single consultant orthopaedic surgeon (SKM-A). All patients received antibiotic prophylaxis with three doses of intravenous cefuroxime perioperatively. After initial templating of preoperative radiographs, surgery was carried out using a standard technique with the patient under a general anesthetic. The patient was placed in the lateral position and an extended posterior approach used. After releasing the short external rotators, the femoral head was dislocated and initially debulked to improve acetabular exposure. The acetabulum was then sequentially reamed but undersized by 1 mm relative to the size of the prosthesis. A trial component was then impacted and any rim osteophytes removed. The definitive component was then impacted into position ensuring that care was taken to obtain the correct amount of inclination and anteversion (40 of inclination and 20 of anteversion) [37]. For preparation of the femoral head, an alignment pin was inserted into the lateral femoral cortex as determined by preoperative templating. The alignment guide (as supplied by the implant company) with the stylus was then used in conjunction with the alignment pin to position the guide rod for preparation of the femoral head. The femoral head was then reamed to accept the appropriate femoral head size. The definitive femoral component was then cemented with Simplex P (Stryker, Newbury, UK) with erythromycin and colistin medium-viscosity bone cement. The femoral component was then reduced and the ROM assessed. The posterior capsule, the short external rotators, and the insertion of the gluteus maximus were then repaired.
Postoperatively, the patients were mobilized fully weightbearing on the day of the operation. All patients received 30 minutes of supervised physiotherapy twice a day, which was continued throughout the inpatient stay as they progressed from using assistive devices as tolerated. All patients received thromboprophylaxis in the form of low-molecular-weight heparin during their inpatient stay, thromboembolic deterrent stockings, pneumatic calf pumps, and on discharge they were given 75 mg aspirin once daily for a duration of 6 weeks.
Postoperatively, the patients were followed up at 4 weeks, 3 months, 1 year, and then at 2-year intervals. For the purposes of this study, a combination of clinical followup and a postal questionnaire (which included a Harris hip score (HHS) [19], Oxford Hip Score (OHS) [13], WOMAC [6], and a modified University of California Los Angeles Activity (UCLA) scale [11]) were used. Of the 302 patients, 213 patients had clinical followup, whereas 89 had only postal questionnaires. In addition, the sizes of the hip resurfacing components were recorded prospectively. For the purposes of this study, radiographic analysis was not performed.
One patient had a superficial wound infection treated with oral antibiotics with resolution. One patient developed a deep vein thrombosis and pulmonary embolus treated with warfarin and with resolution. There were no other major medical or surgical complications in the early postoperative period.
We calculated descriptive statistics (mean, SD, and range) for continuous study variables. The Kaplan-Meier method [25] was used to estimate implant survival after surgery, censoring at the date of death or date of last followup for patients who did not experience implant failure. The log rank test was used to compare survivorship between male and female subjects. The Mann-Whitney U-test was used to compare differences in age, BMI, and component sizes between surviving and revised resurfacings.
Results
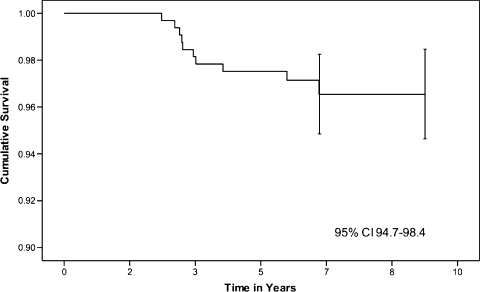
There were 10 revisions (Table 2) at a mean time to revision of 3.7 years (range, 2.5–6.5 years); five (50%) were in women and five (50%) were in men. Kaplan-Meier survival analysis showed a cumulative survival of 96.5% at 9 years (95% confidence interval, 94.7–98.4) using revision for all causes as the end point (Fig. 1).
Table 2.
Summary of revision cases
| Patient number | Age (years) | Gender | Time to revision (years) | Acetabular size (mm) | Femoral head size (mm) | Reason for revision |
|---|---|---|---|---|---|---|
| 1 | 59 | F | 3.0 | 54 | 46 | Pain/effusion |
| 2 | 53 | F | 6.5 | 48 | 42 | Neck fracture |
| 3 | 56 | M | 3.3 | 58 | 50 | Infection |
| 4 | 55 | M | 2.9 | 56 | 50 | Pain/effusion/socket loosening |
| 5 | 48 | M | 4.0 | 54 | 46 | Femoral head collapse |
| 6 | 54 | M | 2.5 | 54 | 46 | Infection |
| 7 | 66 | M | 3.0 | 54 | 46 | Pain/effusion/socket loosening |
| 8 | 58 | F | 5.7 | 50 | 42 | Neck fracture |
| 9 | 48 | F | 2.8 | 46 | 38 | Femoral head collapse |
| 10 | 53 | F | 3.4 | 48 | 42 | Pain/effusion/osteolysis around socket/socket loosening |
F = female; M = male.
Fig. 1.
Kaplan-Meier survival analysis showed a survival of 96.5% at 9 years (95% confidence interval [CI], 94.7–98.4).
The mean HHS was 51.3 (SD, 17.1; range, 7–91) preoperatively and 94.3 (SD 9, range, 24–100) postoperatively. The mean OHS was 38.3 (SD, 9.8; range, 16–60) preoperatively and 15.9 (SD, 4.9; range, 12–46) postoperatively. The mean WOMAC score was 47.9 (SD, 17.4; range, 5–96) preoperatively and 6.9 (SD, 9; range, 0–58) postoperatively. The mean UCLA activity score was 4.7 (SD, 1.9; range, 1–9) preoperatively and 7.5 (SD 1.3; range, 3–10) postoperatively.
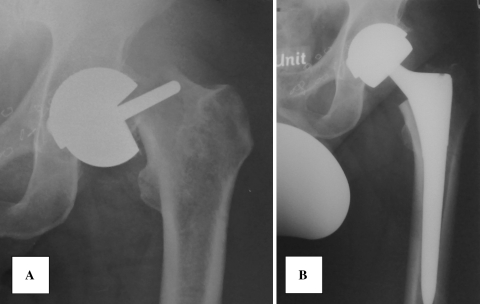
We observed a 2.36 times higher failure rate in females compared with males. There were two revisions for late deep infection, one of which underwent a single-stage revision and the other underwent a two-stage revision procedure; these were both in men. Revisions for aseptic mechanical failure would account for eight revisions with five in women (63%) and three in men (37%) giving a 3.9 times higher failure rate in women compared with men. This equates to a lower survival (p = 0.04) of 94.9% in women compared with 98.7% survival in men. There were in total 10 revisions (Table 2). Two revisions were the result of fractured neck of femur (Fig. 2) giving a fracture rate of 0.6%. For the revision cases, the primary diagnoses were primary osteoarthritis (OA) for nine hips and OA secondary to congenital dislocation [10] for the remaining hip. The mean age of patients who required revision of their resurfacing was (mean ± SD, 54.8 ± 5.5; range, 47.7–66.2 years) was similar to (p = 0.915) that of the unrevised group (56.1 ± 8.2; 28.2–75.5). The femoral head size in the revised hips (mean ± SD, 44.8 ± 3.8 mm; range, 38–50 mm) was smaller (p = 0.01) than the mean femoral head size in the unrevised hips (mean ± SD, 48.2 ± 3.8 mm; range, 38–54 mm). Similarly, the mean ± SD (52.2 ± 3.9 mm; range, 46-58 mm) acetabular size was also smaller (p = 0.02) in the revised hips compared with the unrevised hips (mean ± SD, 55.1 ± 3.6 mm; range, 46–62 mm). BMI was smaller (p = 0.028) in the revised group (23.9 ± 2.7; 18.8–28.1) compared with the unrevised group (26.2 ± 3.8; 18.2–56.2).
Fig. 2A–B.
A fracture of the femoral neck is shown at 1 year postoperatively (A) and revised to a THA (B) in a 51-year-old woman.
Discussion
Hip resurfacing arthroplasty has become a common option as an alternative to THA, particularly in the younger patient with greater physical demand. There are a number of advantages of hip resurfacing over conventional THA as noted earlier, and various studies have reported high midterm survival and functional scores. We determined the midterm prosthetic survival and functional scores of the BHR in this independent series. In addition, we examined whether age, gender, BMI, or size of components was related to failure.
We acknowledge some limitations of our study. First, we had no radiographic followup and cannot determine how many of these patients might have had asymptomatic loosening which required revision in the foreseeable future. Second, we retrospectively analyzed risk factors for failure. A prospective study design controlled for other potential risk factors [43] would yield more robust data, for example, the role of femoral head cysts and bone density. Third, while ours is a relatively large single-surgeon series that would reduce some forms of variability resulting from surgeon-related factors, the findings may not be generalizable. In addition the total number of resurfacings performed represents 18% of the surgeon’s workload of primary hip arthroplasty, which is a relatively high percentage. Fourth, we do not have data on metal ion levels which has been a major concern in patients with large metal-on-metal bearing surfaces. Nonetheless, this study represents a cohort of hip resurfacing arthroplasty with prospectively collected data.
We found an overall cumulative survival at 9 years of 96.5%. This is well within the guidelines set by the National Institute of Clinical Excellence [40]. These results from an independent single-surgeon series are similar to other published studies (Table 3). The results presented here compare well with those of THA, particularly in the younger population [7, 15, 24, 28, 34], although the etiology, the indications and patient demographic data may be different between patients in hip resurfacing arthroplasty and those in THA. There is also a potential advantage of conservation of proximal femoral bone when compared with THA, although further comparative studies are required to elucidate the benefits. An important cause of failure in hip resurfacing arthroplasty is fracture of the femoral neck (Fig. 2). In this series, there were two femoral neck fractures; both of these cases were in women (and were converted to THA), giving a fracture rate of 0.61%; this is substantially lower than previously reported rates of 1.62% [26] and 1.46% [44]. This result correlates favorably with those by Treacy et al. [48] who reported one fracture in 144 hip resurfacings. The variability is likely to be related to surgical technique and accuracy as well as patient selection, confirming its importance. Beaule et al. [5] reported a low neck-shaft angle was a risk factor for lower functional scores in hip resurfacing arthroplasty, reiterating the importance of careful patient selection in potentially excluding patients with a varus femoral neck and ensuring the femoral component is placed in a relative valgus position without notching of the superior cortex. The two femoral fractures in this series were at a later time period (Table 2) than one would expect [44]; however, no precipitating factors were identified. In addition to ensuring surgical accuracy with regard to the femoral component, surgical accuracy is also important with regard to the acetabular component because a high inclination angle has also been associated with high blood metal ion levels [14, 20] with potential adverse effects. In all 10 revisions there was no intraoperative evidence of “pseudotumor”, which has been a particular concern.
Table 3.
Summary of literature for implant survival
| Source | Implant type | Number of hips | Followup (years)* | Survivorship (%) |
|---|---|---|---|---|
| Daniel et al. [11] | BHR | 446 | 3.3 (1.1–8.2) | 99.78 |
| Treacy et al. [48] | BHR | 144 | 5 | 98 |
| Nishii et al. [42] | BHR | 50 | 5.6 (5–7) | 96 |
| Heilpern et al. [22] | BHR | 110 | 5.9 (5–12) | 96.3 |
| Steffan et al. [46] | BHR | 610 | 4.2 (2–7.6) | 95 |
| Khan et al. [26] | BHR | 679 | 6 (5–8) | 95.7 |
| Madhu et al. [33] | BHR | 117 | 7 (5–9.4) | 91.5 |
| Amstutz et al. [1] | Conserve Plus | 687 | 5.5 (2–9) | 94 |
| Mont et al. [39] | Conserve Plus | 84 | 3.4 (2–5) | 94 |
| Mont et al. [38] | Conserve Plus | 49 | 1.5 (1–2) | 100 |
| Lilikakis et al. [31] | Cormet 2000 | 70 | 2.3 (2–3) | 97 |
| Grigoris et al. [17] | Durom | 200 | 2.2 (1–3) | 100 |
| Beaule et al. [5] | Conserve Plus | 94 | 3 (2–5.6) | 97 |
| Rahman et al. [current study] | BHR | 329 | 6.6 (5–9.2) | 96.5 |
* Ranges in parentheses.
The patients with surviving hips also showed improvement in function as assessed by the HHS, WOMAC, and OHS scores. Activity levels also improved. This confirms previous findings from a number of studies [1, 11, 22, 39, 42, 48].
Various risk factors for failure of hip resurfacings have been reported in the literature. These include female gender, smaller component sizes, increasing age [2, 3, 5, 8, 43], and increased BMI [29]. Although Khan et al. [26] reported no effect of gender on survivorship, our data show a higher failure rate in women. Our failures also had smaller component sizes when compared with the hips that have not failed. This is in agreement with findings from Amstutz et al. [2] and Steffan et al. [47]. Amstutz et al. [2] reported individuals with smaller femoral component head sizes had more femoral loosening and radiolucencies. The authors concluded femoral fixation is critical to long-term durability, and individuals with smaller head sizes have a smaller area available for cement fixation. The coverage angle, which represents the coverage of the femoral head by the acetabular component, is also less in the BHR relative to conventional hip arthroplasties. The relative coverage of the femoral head decreases as the size of the components decrease; this results in a reduction in peripheral cover for the femoral head and is less forgiving of minor surgical errors in component positioning and can lead to edge wear and device failure [12]. Furthermore, smaller component sizes have also been directly associated with higher wear rates [30]. Other factors that may also contribute to an unfavorable functional hip score or early failure after resurfacing include short stature, preoperative low horizontal femoral offset, and high femoral anteversion [42].
There are various concerns regarding hip resurfacing arthroplasty, particularly with regard to the large metal-on-metal bearing surfaces and high blood cobalt and chromium levels [21] and potential hypersensitivity reactions [18, 32] and carcinogenic effects [32]. Long-term followup is the only way to clearly answer these questions. Despite these concerns, hip resurfacing remains a common alternative to THA, particularly in the younger male population with relatively large femoral head sizes. The midterm survival and functional scores in this independent series are similar to those from other centers, including results from the pioneering center for this particular implant.
Acknowledgments
We thank Verna Gilmartin, RN, and Phillipa Hoxha, RN, for their assistance in collecting preoperative hip scores.
Footnotes
One of the authors (SKM-A) was paid for consultancy work by Smith & Nephew, DePuy, a Johnson & Johnson Company, and Zimmer.
Each author certifies that his or her institution approved the human protocol for this investigation, that all investigations were conducted in conformity with ethical principles of research, and that informed consent for participation in the study was obtained.
This work was performed at The London Hip Unit, London, UK.
References
- 1.Amstutz HC, Ball ST, Duff MJ, Dorey FJ. Resurfacing THA for patients younger than 50 year: results of 2 to 9 year followup. Clin Orthop Relat Res. 2007;460:159–164. doi: 10.1097/BLO.0b013e318041f0e7. [DOI] [PubMed] [Google Scholar]
- 2.Amstutz HC, Beaule PE, Dorey FJ, Le Duff MJ, Campbell PA, Gruen TA. Metal-on-metal hybrid surface arthroplasty: two to six-year follow-up study. J Bone Joint Surg Am. 2004;86:28–39. [PubMed] [Google Scholar]
- 3.Australian Orthopaedic Association National Joint Replacement Registry Annual Report. Adelaide: AOA; 2009. Available at: www.dmac.adelaide.edu.au/aoanjrr/documents/aoanjrrreport_2009.pdf. Accessed March 1, 2010.
- 4.Back DL, Dalziel R, Young D, Shimmin A. Early results of primary Birmingham hip resurfacings: an independent prospective study of the first 230 hips. J Bone Joint Surg Br. 2005;87:324–329. doi: 10.1302/0301-620X.87B3.15556. [DOI] [PubMed] [Google Scholar]
- 5.Beaulé PE, Dorey FJ, LeDuff M, Gruen T, Amstutz HC. Risk factors affecting outcome of metal-on-metal surface arthroplasty of the hip. Clin Orthop Relat Res. 2004;418:87–93. doi: 10.1097/00003086-200401000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Bellamy N, Buchanan W, Goldsmith C, Campbell J, Stitt LW. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15:1833–1840. [PubMed] [Google Scholar]
- 7.Bizot P, Banallec L, Sedel L, Nizard R. Alumina-on-alumina total hip prostheses in patients 40 years of age or younger. Clin Orthop Relat Res. 2000;379:68–76. doi: 10.1097/00003086-200010000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Buergi ML, Walter WL. Hip resurfacing arthroplasty: the Australian experience. J Arthroplasty. 2007;22:61–65. doi: 10.1016/j.arth.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 9.Burroughs BR, Hallstrom B, Golladay GJ, Hoeffel D, Harris WH. Range of motion and stability in total hip arthroplasty with 28-, 32-, 38-, and 44-mm femoral head sizes. J Arthroplasty. 2005;20:11–19. doi: 10.1016/j.arth.2004.07.008. [DOI] [PubMed] [Google Scholar]
- 10.Crowe JF, Mani VJ, Ranawat CS. Total hip replacement in congenital dislocation and dysplasia of the hip. J Bone Joint Surg Am. 1979;61:15–23. [PubMed] [Google Scholar]
- 11.Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177–184. doi: 10.1302/0301-620X.86B2.14600. [DOI] [PubMed] [Google Scholar]
- 12.Daniel J, Ziaee H, McMinn DJW. Acetabular bone conservation. In: McMinn D, ed. Modern Hip Resurfacing. London: Springer-Verlag; 2009:129–130.
- 13.Dawson J, Fitzpatrick R, Carr A, Murray D. Questionnaire on the perceptions of patients about total hip replacement. J Bone Joint Surg Br. 1996;78:185–190. [PubMed] [Google Scholar]
- 14.Haan R, Pattyn C, Gill HS, Murray DW, Campbell PA, Smet K. Correlation between inclination of the acetabular component and metal ion levels in metal-on-metal hip resurfacing replacement. J Bone Joint Surg Br. 2008;90:1291–1297. doi: 10.1302/0301-620X.90B10.20533. [DOI] [PubMed] [Google Scholar]
- 15.Dorr LD, Kane TJ, III, Conaty JP. Long-term results of cemented total hip arthroplasty in patients 45 years old or younger: a 16-year follow-up study. J Arthroplasty. 1994;9:453–456. doi: 10.1016/0883-5403(94)90090-6. [DOI] [PubMed] [Google Scholar]
- 16.Girard J, Lavigne M, Vendittoli PA, Roy AG. Biomechanical reconstruction of the hip: a randomised study comparing total hip resurfacing and total hip arthroplasty. J Bone Joint Surg Br. 2006;88:721–726. doi: 10.1302/0301-620X.88B6.17447. [DOI] [PubMed] [Google Scholar]
- 17.Grigoris P, Roberts P, Panousis K, Bosch H. The evolution of hip resurfacing arthroplasty. Orthop Clin North Am. 2005;36:125–134, vii. [DOI] [PubMed]
- 18.Hallab N. Metal sensitivity in patients with orthopedic implants. J Clin Rheumatol. 2001;7:215–218. doi: 10.1097/00124743-200108000-00004. [DOI] [PubMed] [Google Scholar]
- 19.Harris WH. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty: an end-result study using a new method of result evaluation. J Bone Joint Surg Am. 1969;51:737–755. [PubMed] [Google Scholar]
- 20.Hart AJ, Buddhdev P, Winship P, Faria N, Powell JJ, Skinner JA. Cup inclination angle of greater than 50 degrees increases whole blood concentrations of cobalt and chromium ions after metal-on-metal hip resurfacing. Hip Int. 2008;18:212–219. doi: 10.1177/112070000801800304. [DOI] [PubMed] [Google Scholar]
- 21.Hart AJ, Skinner JA, Winship P, Faria N, Kulinskaya E, Webster D, Muirhead-Allwood S, Aldam CH, Anwar H, Powell JJ. Circulating levels of cobalt and chromium from metal-on-metal hip replacement are associated with CD8+ T-cell lymphopenia. J Bone Joint Surg Br. 2009;91:835–842. doi: 10.1302/0301-620X.91B6.21844. [DOI] [PubMed] [Google Scholar]
- 22.Heilpern GN, Shah NN, Fordyce MJ. Birmingham hip resurfacing arthroplasty: a series of 110 consecutive hips with a minimum five-year clinical and radiological follow-up. J Bone Joint Surg Br. 2008;90:1137–1142. doi: 10.1302/0301-620X.90B9.20524. [DOI] [PubMed] [Google Scholar]
- 23.Howie DW, McCalden RW, Nawana NS, Costi K, Pearcy MJ, Subramanian C. The long-term wear of retrieved McKee-Farrar metal-on-metal total hip prostheses. J Arthroplasty. 2005;20:350–357. doi: 10.1016/j.arth.2004.09.028. [DOI] [PubMed] [Google Scholar]
- 24.Joshi AB, Porter ML, Trail IA, Hunt LP, Murphy JC, Hardinge K. Long-term results of Charnley low-friction arthroplasty in young patients. J Bone Joint Surg Br. 1993;75:616–623. doi: 10.1302/0301-620X.75B4.8331119. [DOI] [PubMed] [Google Scholar]
- 25.Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc. 1958;53:457–481. doi: 10.2307/2281868. [DOI] [Google Scholar]
- 26.Khan M, Kuiper JH, Edwards D, Robinson E, Richardson JB. Birmingham hip arthroplasty: five to eight years of prospective multicenter results. J Arthroplasty. 2009;24:1044–1050. doi: 10.1016/j.arth.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 27.Killampalli VV, Kundra RK, Chaudhry F, Chowdhry M, Fisher NE, Reading AD. Resurfacing and uncemented arthroplasty for young hip arthritis: functional outcomes at 5 years. Hip Int. 2009;19:234–238. doi: 10.1177/112070000901900308. [DOI] [PubMed] [Google Scholar]
- 28.Kobayashi S, Eftekhar NS, Terayama K, Joshi RP. Comparative study of total hip arthroplasty between younger and older patients. Clin Orthop Relat Res. 1997;339:140–151. doi: 10.1097/00003086-199706000-00019. [DOI] [PubMed] [Google Scholar]
- 29.Le Duff MJ, Amstutz HC, Dorey FJ. Metal-on-metal hip resurfacing for obese patients. J Bone Joint Surg Am. 2007;89:2705–2711. doi: 10.2106/JBJS.F.01563. [DOI] [PubMed] [Google Scholar]
- 30.Leslie I, Williams S, Brown C, Isaac G, Jin Z, Ingham E, Fisher J. Effect of bearing size on the long-term wear, wear debris, and ion levels of large diameter metal-on-metal hip replacements—an in vitro study. J Biomed Mater Res B Appl Biomater. 2008;87:163–172. doi: 10.1002/jbm.b.31087. [DOI] [PubMed] [Google Scholar]
- 31.Lilikakis AK, Vowler SL, Villar RN. Hydroxyapatite-coated femoral implant in metal-on-metal resurfacing hip arthroplasty: minimum of two years follow-up. Orthop Clin North Am. 2005;36:215–222, ix. [DOI] [PubMed]
- 32.MacDonald SJ. Metal-on-metal total hip arthroplasty: the concerns. Clin Orthop Relat Res. 2004;429:86–93. doi: 10.1097/01.blo.0000150309.48474.8b. [DOI] [PubMed] [Google Scholar]
- 33.Madhu TS, Akula MR, Raman RN, Sharma HK, Johnson VG. The Birmingham Hip Resurfacing prosthesis an independent single surgeon’s experience at 7-year follow-up. J Arthroplasty. 2010 Jan 5. [Epub ahead of print] [DOI] [PubMed]
- 34.Mäkelä KT, Eskelinen A, Pulkkinen P, Paavolainen P, Remes V. Total hip arthroplasty for primary osteoarthritis in patients fifty-five years of age or older. An analysis of the Finnish arthroplasty registry. J Bone Joint Surg Am. 2008;90:2160–2170. doi: 10.2106/JBJS.G.00870. [DOI] [PubMed] [Google Scholar]
- 35.Marker DR, Strimbu K, McGrath MS, Zywiel MG, Mont MA. Resurfacing versus conventional total hip arthroplasty—review of comparative clinical and basic science studies. Bull NYU Hosp Jt Dis. 2009;67:120–127. [PubMed] [Google Scholar]
- 36.McKellop H, Park SH, Chiesa R, Doorn P, Lu B, Normand P, Grigoris P, Amstutz H. In vivo wear of three types of metal on metal hip prostheses during two decades of use. Clin Orthop Relat Res. 1996;329(Suppl):S128–S140. doi: 10.1097/00003086-199608001-00013. [DOI] [PubMed] [Google Scholar]
- 37.McMinn DJW. Acetabular preparation and insertion of the standard Birmingham Hip Resurfacing cup. In: McMinn D, ed. Modern Hip Resurfacing. London, England: Springer-Verlag; 2009:223–236.
- 38.Mont MA, Ragland PS, Marker D. Resurfacing hip arthroplasty: comparison of a minimally invasive versus standard approach. Clin Orthop Relat Res. 2005;441:125–131. doi: 10.1097/01.blo.0000195100.09313.b0. [DOI] [PubMed] [Google Scholar]
- 39.Mont MA, Seyler TM, Marker DR, Marulanda GA, Delanois RE. Use of metal-on-metal total hip resurfacing for the treatment of osteonecrosis of the femoral head. J Bone Joint Surg Am. 2006;88(Suppl 3):90–97. doi: 10.2106/JBJS.F.00543. [DOI] [PubMed] [Google Scholar]
- 40.National Institute for Clinical Excellence. Guidance on the use of metal on metal hip resurfacing arthroplasty. 2002. Available at: www.nice.org.uk/nicemedia/pdf/HipResurfacing-FinalGuidance.pdf. Accessed October 13, 2009.
- 41.National Joint Registry 6th Annual Report. Available at: www.njrcentre.org.uk/NjrCentre/LinkClick.aspx?fileticket=V5%2bELEMfw20%3d&tabid=86&mid=523. Accessed October 13, 2009.
- 42.Nishii T, Sugano N, Miki H, Takao M, Koyama T, Yoshikawa H. Five-year results of metal-on-metal resurfacing arthroplasty in Asian patients. J Arthroplasty. 2007;22:176–183. doi: 10.1016/j.arth.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 43.Nunley RM, Della Valle CJ, Barrack RL. Is patient selection important for hip resurfacing? Clin Orthop Relat Res. 2009;467:56–65. doi: 10.1007/s11999-008-0558-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shimmin AJ, Back D. Femoral neck fractures following Birmingham Hip Resurfacing. J Bone Joint Surg Br. 2005;87:463. doi: 10.1302/0301-620X.87B4.15498. [DOI] [PubMed] [Google Scholar]
- 45.Silva M, Lee KH, Heisel C, Dela Rosa MA, Schmalzried TP. The biomechanical results of total hip resurfacing arthroplasty. J Bone Joint Surg Am. 2004;86:40–46. doi: 10.2106/00004623-200401000-00007. [DOI] [PubMed] [Google Scholar]
- 46.Steffen RT, Foguet PR, Krikler SJ, Gundle R, Beard DJ, Murray DW. Femoral neck fractures after hip resurfacing. J Arthroplasty. 2009;24:614–619. doi: 10.1016/j.arth.2008.04.008. [DOI] [PubMed] [Google Scholar]
- 47.Steffen RT, Pandit HP, Palan J, Beard DJ, Gundle R, McLardy-Smith P, Murray DW, Gill HS. The five-year results of the Birmingham Hip Resurfacing arthroplasty: an independent series. J Bone Joint Surg Br. 2008;90:436–441. doi: 10.1302/0301-620X.90B4.19648. [DOI] [PubMed] [Google Scholar]
- 48.Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty: a minimum follow-up of five years. J Bone Joint Surg Br. 2005;87:167–170. doi: 10.1302/0301-620X.87B2.15030. [DOI] [PubMed] [Google Scholar]