Abstract
Objective
Maintaining weight loss is a major challenge in obesity treatment. Individuals often indicate that waning motivation prompts cessation of effective weight management behaviors. Therefore, a novel weight loss maintenance program that specifically targets motivational factors was evaluated.
Design
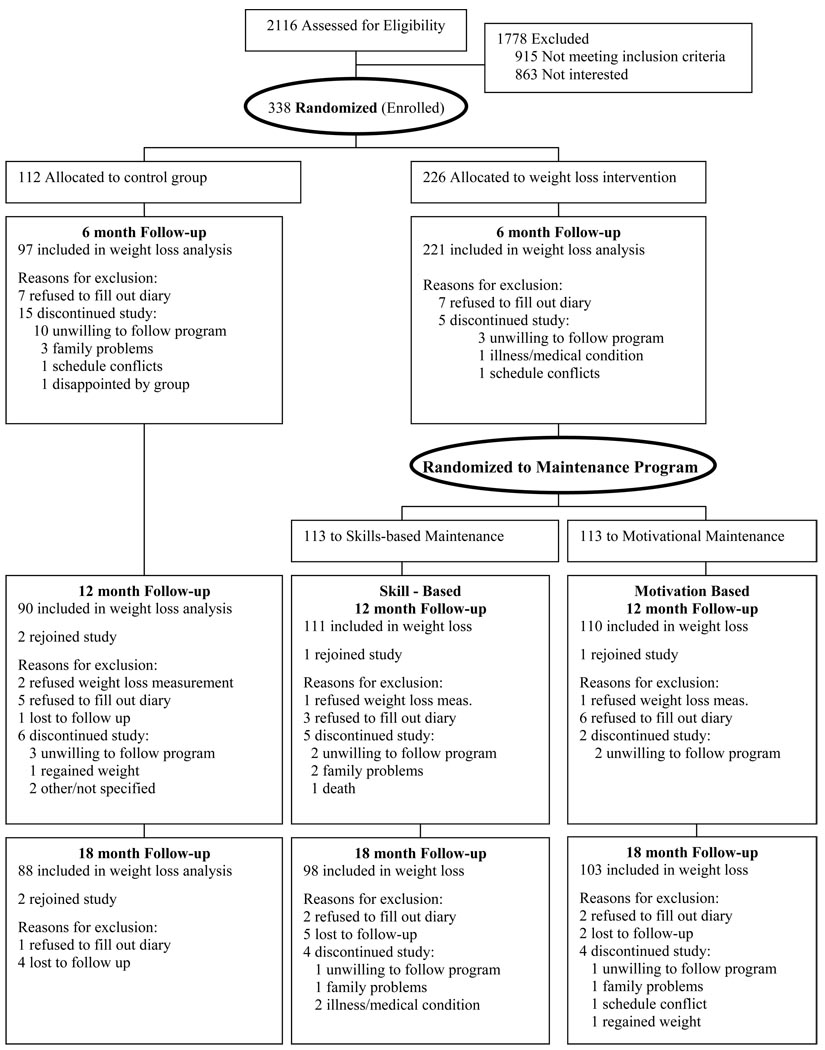
Overweight women (N=338; 19% African American) with urinary incontinence were randomized to lifestyle obesity treatment or control and followed for 18 months. All participants in lifestyle (N=226) received the same initial six-month group behavioral obesity treatment and were then randomized to 1) a novel motivation-focused maintenance program (N=113) or 2) a standard skill-based maintenance approach (N=113).
Main Outcome Measure
Weight assessed at baseline, 6, and 18 months.
Results
Both treatment groups (motivation-focused and skill-based) achieved comparable 18-month weight losses (−5.48% for motivation-focused vs −5.55% in skill-based, p=0.98), and both groups lost significantly more than controls (−1.51%; p=.0012 in motivation-focused and .0021 in skill-based).
Conclusions
A motivation-focused maintenance program offers an alternative, effective approach to weight maintenance expanding available evidence-based interventions beyond traditional skill-based programs.
Keywords: Weight Maintenance, motivation, obesity treatment, autonomy, motivational interviewing
Long-term weight control is an elusive goal in obesity treatment. Although several approaches produce initial weight loss, few have proven successful in preventing regain (1, 2). Individuals who continue to engage in modified dietary and physical activity behaviors are most likely to successfully maintain weight loss (3, 4). Thus, current behavioral weight loss maintenance approaches typically focus on helping participants refine dietary and exercise self-management skills that initially produced weight loss (5, 6). Although existing weight maintenance programs place tremendous emphasis on behavioral skill refinement, it is unlikely that regain is due solely, or even primarily, to a skill deficit. Rather, participants often anecdotally report that they know what to do to control their weight but cannot motivate themselves to continue to implement these behaviors. In existing weight maintenance programs, surprisingly little time is spent addressing motivational issues. A stronger emphasis on motivational factors within a behavioral weight maintenance program offers promise for improving long-term outcomes. We report here on a randomized controlled trial evaluating an innovative, theoretically-based weight loss maintenance program that specifically targets motivation in comparison to a standard behavioral skill-based weight maintenance program and a minimal treatment control group.
Novel Weight Maintenance Program Conceptual Foundation
Several current theories of motivation are relevant to weight loss maintenance and informed the theoretically-based motivation-focused program tested in this trial. For example, Rothman (7) speculated that initiation of behavior change is motivated by the desire to achieve positive future goals; whereas, maintenance is motivated by the desire to avoid returning to an unfavorable baseline state. This distinction forms a central conceptual foundation for the novel maintenance program. Similarly, motivational interviewing (8) is a key component of our novel approach. MI has been demonstrated to be effective in promoting behavior change across a range of health arenas (9), including weight loss (10, 11). The focus of MI on identifying and amplifying personal motivations for behavior change while resolving ambivalence surrounding the behavior change (8) is consistent with other motivational theories, such as self determination theory (12), which suggests that successful long-term weight maintenance is expected when the reasons for self-regulation are volitional or autonomous. Some evidence suggests that higher levels of autonomous self-regulation predict more successful weight management (13, 14), with internalization of perceived autonomous reasons for behavior change hypothesized to prompt continued self regulation and long term success. However, current maintenance approaches do not explicitly cultivate internalization of autonomous self regulation. The novel motivation-focused program evaluated in the current trial integrated these approaches and theories to develop specific treatment strategies designed to promote weight maintenance.
MATERIALS AND METHODS
Participants
Participants were recruited as part of a randomized clinical trial to determine whether behavioral obesity treatment for overweight women with urinary incontinence produces greater reduction in incontinence frequency than the control condition (Program to Reduce Incontinence through Diet and Exercise; PRIDE). Details of this trial and 6-month outcomes demonstrating that lifestyle intervention is an effective treatment for urinary incontinence have been published (15). In brief, 338 overweight and obese women with urinary incontinence were recruited between July 2004 and April 2006 in Providence, Rhode Island and Birmingham, Alabama. Women were eligible to participate if they were at least 30 years of age, had a body mass index (BMI) between 25 and 50 kg/m2, reported 10 or more episodes of urinary incontinence on a 7-day voiding diary, and were able to walk for exercise. Exclusion criteria included medical conditions that contraindicated weight loss, pregnancy or parturition in the previous 6 months or history of current or persistent urinary tract infection or other medical conditions of the genitourinary tract. To enroll, participants were required to successfully complete a 7-day diary of dietary intake and physical activity. The study was approved by the Institutional Review Board at each site and written consent was obtained from all participants.
Study Design
Eligible women (N=338) were randomized in a 2:1 ratio to a 6-month behavioral lifestyle weight loss program (N=226) or an education control (N=112). Participants in the weight loss arm were further randomized to receive either the novel motivation-focused weight maintenance program (N=113) or a skill-based maintenance program (N=113). Individuals were cluster randomized within their intervention group (N=18 clusters) so that group cohesion and social support developed during the weight loss initiation phase could continue into maintenance. Maintenance conditions were revealed to participants and clinical staff after completion of the 6-month weight loss program so neither participants nor staff knew which maintenance approach individuals would be receiving. Outcome data were collected at baseline, 6, and 18 months.
Interventions
Education Control Group
Women randomized to the control group were offered seven education sessions that provided general information about physical activity, healthy eating habits, and weight loss, following a structured protocol.
Behavioral Weight Control: Weight Loss Induction
The same 6-month weight loss program was offered to all individuals randomized to behavioral weight control regardless of maintenance condition. The 24-session program was modeled after the Diabetes Prevention Program (16) and the Look AHEAD lifestyle interventions (17). Weekly group sessions included an individual weigh in and followed a structured protocol. Participants were encouraged to lose 10% of their baseline body weight. A reduced calorie balanced diet was prescribed and meal replacement product coupons (Slimfast™) were provided to replace two meals and one snack per day. Graded exercise goals that progressed to 200 minutes/week or more of moderate physical activity were provided and participants were given pedometers to promote increased daily steps. To encourage adoption of the dietary and physical activity recommendations, training in specific behavioral skills was provided, including self-monitoring, stimulus control, problem-solving, assertiveness training, social support, goal setting, cognitive restructuring, and relapse prevention.
Common elements of skill-based and motivation-focused maintenance programs
After the initial weight loss program, all lifestyle participants received a 12-month weight maintenance intervention with bi-weekly group meetings. Group meetings were 60 minutes in length and were conducted by dietitians, exercise physiologists, nurses and psychologists following a structured protocol, The overall goal for both programs was to maintain at least a 10% weight loss. Participants in both programs were weighed at each session. Moreover, both groups were given self-monitoring diaries to continue daily recording of dietary intake and physical activity behavior. Exercise goals remained at 200 minutes/week for both conditions and reduced calorie goals were recommended until goal weight was achieved and then intake goals focused on weight stability. Meal replacement coupons (one meal, one snack) continued to be provided to both groups.
Skill-based Maintenance Program
The standard behavioral weight maintenance program reflected current lifestyle program recommendations (4, 17)and focused on reviewing and refining behavioral skills in problem solving, goal setting, social support, and relapse prevention. New skill development topics introduced included reversing small weight gains (18), improving body image and self esteem (19), and expanding exercise options.
Motivation-focused Maintenance Program
This novel maintenance intervention focused on increasing and sustaining motivation to utilize the dietary, physical activity, and behavioral skills introduced in the initial weight loss phase rather than on improving and fine-tuning those skills. The behavioral goals remained the same as in the standard skill-based maintenance and the intervention sought to promote these goals using strategies derived from motivational theories and methods by: 1) strengthening satisfaction with progress; 2) cultivating an identity as a successful weight loser; 3) eliciting personal motivations for engaging in long-term behavior change efforts and supporting autonomous self regulation; and 4) developing an enriched array of non-food related reinforcements and self-care activities to increase motivation to engage in non-food related activities. The theoretical underpinnings of the motivational goals and examples of corresponding treatment strategies are described briefly below and in expanded detail in online supplemental materials.
Motivational Goal #1: Strengthen participants’ satisfaction with their progress
Rothman’s (7) concept that initiation of behavior change is an approach-based self-regulation system fueled by positive expectations about future outcomes and that maintenance of behavior change is an avoidance-based self-regulation system driven by the desire to avoid returning to an unfavorable baseline state served as the foundation for this motivational goal. Accordingly, if individuals perceive their baseline state as aversive and are satisfied with the outcomes they have obtained, they will be more likely to continue maintaining new behaviors. The intuitive appeal of this model is strong, and while empirical tests have produced mixed results (20, 21), in general, greater satisfaction with weight loss outcomes is associated with better long-term maintenance (22). Therefore, the motivation-focused intervention sought to remind participants of unfavorable aspects of their pre-weight loss state and to heighten their satisfaction with their post-weight loss state. Videos of participants were made prior to starting the weight loss program in which they described the impact their weight had on their daily functioning. These videos were viewed by participants as a visual reminder of their pre-weight loss state. To further enhance recall of the aversive impact excessive weight had at baseline, participants wore a backpack with ten pounds of flour while they climbed stairs to recreate the experience of being ten pounds heavier (23). Sessions also emphasized positive progress made by having participants “brag” about their accomplishments.
Motivational Goal #2: Cultivate identity as a successful weight loser
The rich tradition of self-presentation and cognitive dissonance research indicates public presentation fosters private identity (24). One study that used self-presentation theory to promote physical activity among African-American adolescents found that teens who made a video for their peers describing ways to increase physical activity reported greater exercise self-efficacy (25). Similarly, adult dialysis patients who made a video describing their successful coping strategies later reported better psychological adjustment than patients discussing difficulties with their disease (26). Using a paradigm similar to this, participants were videotaped discussing the positive things done to produce weight loss, increase exercise and/or improve eating habits, and strategies to overcome specific challenges encountered. These videos were then reviewed in the group.
Motivational Goal #3: Elicit personal motivations for engaging in long-term behavior change efforts and support autonomous self-regulation
Individuals who discontinue exercise and dietary habits that had previously produced weight loss characterize themselves as losing motivation. MI seeks to augment an individual’s motivation to change (or sustain a successful change) by identifying personal goals for change, eliciting behavior change strategies from the individual, and increasing self efficacy for engaging in the behaviors (8). Motivation is increased by highlighting the discrepancy between current behavior (slips and lapses) and desired outcomes (long-term weight control, superior quality of life, self confidence, health). The addition of MI to skill-based weight loss programs has been shown to enhance weight loss outcomes compared with the skill-based approach alone (10, 11) and MI techniques are consistent with efforts to support autonomous self regulation (12, 27). In the motivation-focused program, women were encouraged to identify their personal reasons for weight management and to identify their core personal values (e.g. religion, family, health) to determine how weight maintenance efforts might support or conflict with their overall value system. Eliciting personally-relevant reasons for change and supporting the congruence between personal values and weight loss behaviors were used to support and promote internalization of autonomous motivations to engage in recommended weight maintenance behaviors. (28). An autonomy-supportive approach such as this has recently been demonstrated useful in weight maintenance by investigators using a self-determination theory based intervention (14).
Motivational Goal #4: Increase motivation to engage in non-food related activities
Traditional behavioral weight management programs tend to pay minimal attention to aspects of daily functioning outside of eating and physical activity patterns. Addiction research suggests that developing a balanced lifestyle that includes hobbies and other sources of pleasurable activity can provide positive coping strategies to replace more dysfunctional patterns (29). Further, increasing the frequency of pleasant events can reduce dysphoric moods (30), and higher levels of depressive symptoms may interfere with sustained weight maintenance (3). Early obesity treatment research focused on increasing alternative sources of reinforcement (31), but recent treatment recent has emphasized this less. Thus, a systematic focus on developing a balanced lifestyle that includes hobbies and other enjoyable activities that do not contribute negatively to energy balance was incorporated. Participants were given opportunities to identify hobbies and activities which they previously enjoyed and new ones they might enjoy, with specific goals set to experiment with identifying an enhanced range of pleasurable activities to reward themselves and reduce stress.
Intervention Fidelity Procedures
Fidelity to and distinction between the motivation-focused and the skills-based maintenance program protocols were addressed with explicit training of the intervention staff and ongoing supervision of treatment delivery. Audiotapes of 10% of both the skills-based and motivation-focused maintenance group sessions were reviewed by an independent rater to assure consistency with the protocol, with attention paid both to inclusion of all prescribed elements and exclusion of prohibited elements. Corrective feedback was provided to intervention staff as necessary to assure treatment fidelity.
Data Collection
Assessments occurred at baseline, 6, 12, and 18 months. Measures were obtained by research staff blinded to treatment condition. Body weight was measured in street clothes with shoes removed using a calibrated digital scale (Tanita BWB 800) and recorded to the nearest 0.1 kg. Height was measured at baseline to the nearest centimeter using a calibrated, wall-mounted stadiometer and a horizontal measuring block. Body mass index was calculated as kg/m2. Demographic characteristics and medical, behavioral, and incontinence histories were obtained by self-report questionnaires at baseline.
Motivational Measures
The Treatment Self-Regulation Questionnaire (TSRQ) (13) derived from self regulation theory was used to measure both autonomous reasons for engaging in weight control efforts (personal reasons that reflect a self-selected rationale for change) and controlled or extrinsic motivation (reasons that are imposed externally). The two TSRQ subscales (Autonomous Self Regulation and Controlled Self Regulation) have been demonstrated to be valid across health behaviors (32), with higher scores indicating greater levels of motivation. Autonomous regulation measured by this questionnaire predicts successful weight loss among morbidly obese individuals engaged in a very low calorie diet (13). Further, an MI-based intervention for dietary change demonstrated increased autonomous motivation on this measure (33).
Participants indicated the degree to which they focused on positive progress to sustain engagement in weight control behaviors using a single-item question (“the way I keep trying to maintain my weight is by thinking about how far I have come and the progress I have made”) with a 7-point response. Frequency in which an individual engaged in self-reinforcing, pleasurable activities was assessed using a 5-item scale developed for the study. Higher scores indicate higher levels of non-food related, self-reinforcing activities.
Measures of Self Identity
Self identify was assessed using an adaptation of the Exercise Identity Scale (EIS) (34, 35). EIS items inquire about the degree to which an individual agrees with statements reflecting greater self identity as an exerciser using a 5-point scale, with higher scores denoting greater salience of exercise to self identity. The measure has established reliability and good construct validity (34, 35) and has been shown to be sensitive to changes following a physical activity intervention (36). Four items from the EIS were administered and items were also adapted to examine self concept as a successful weight maintainer and a successful dieter.
Treatment Adherence
Adherence data collected during the maintenance program included attendance at group sessions and submission of self-monitoring diaries. Both of these parameters are consistently associated with better obesity treatment outcomes (16, 37, 38).
Data Analysis
Baseline demographic and clinical characteristics by treatment condition at both levels of randomization (initial allocation and maintenance randomization) and characteristics of those participants lost to follow-up or retained were compared using either a Student t-tests or Wilcoxon tests for continuous variables. Categorical variables were analyzed using chi-square or Fishers exact tests, as appropriate. The primary analysis compares weight change during the maintenance phase between the motivation-focused and skill-based intervention groups with adjustment for weight loss at six months. Weight reduction from baseline visit to follow-up (month 6, 12, or 18) was compared across the three study conditions and adjusted for baseline weight. Mixed models were utilized to estimate weight and weight changes, accounting for recruitment and randomization clusters, and logistic regression was employed to estimate the likelihood of achieving weight loss of 5% or more. To avoid introducing bias associated with attrition due to weight regain, missing weight values were imputed conservatively assuming there would be no weight change from baseline (entry into weight loss trial) among subjects lost to follow-up. Summary effect estimates and standard errors were computed using standard methods for imputed data (39). The effect of the intervention method on weight maintenance was evaluated for moderation effects of race and autonomous self regulation and body weight at the beginning of the maintenance phase. No moderation effects were found.
Treatment adherence variables (attendance and self-monitoring diaries submitted) and motivational parameters (TSRQ, self-identify, focus on progress, reinforcing activities) were compared between groups with either Student t-tests or Wilcoxon tests for continuous variables, and for categorical variables using chi-square or Fishers exact tests. Spearman correlations were employed to determine associations between weight change and adherence parameters. Multiple regression models were used to examine the relative contribution of adherence and motivational variables to weight change over the maintenance period.
All statistical analyses were performed using SAS Version 9.1 (SAS Institute, Cary, NC). A p-value of < .05 was considered statistically significant.
RESULTS
Participant Characteristics
Of the 2116 participants screened by telephone, 1778 were excluded during screening and 338 (19% African American) were randomized (Figure 1). Participants in both weight loss conditions and the control group were similar with respect to sociodemographic and weight variables at baseline. Study-wide, the mean (±SD) age was 53 (±10) years, and mean baseline BMI (36 ± 6 kg/m2) and number of incontinent episodes (24±18) were similar between groups. Retention rates were high (≥ 80% at all assessments across all treatment arms) and did not differ significantly between conditions. There were no differences in baseline demographic characteristics, BMI, or urinary incontinence frequency among those women who attended data collection visits and those who did not.
Figure 1.
6-Month Weight Loss Induction Outcomes
Weight losses following the induction phase and prior to initiation of weight maintenance programs were similar for participants who would go on to receive the motivation-focused maintenance and those who would receive the skill-based maintenance program (−7.98% in both groups; Table 1). Both active weight loss groups experienced significantly greater 6-month weight loss compared to the control group.
Table 1.
Mean Weight Changes by Treatment Condition
| Variable | Motivation-focused | Skill-based | Control |
|---|---|---|---|
| Weight Change, baseline to 6 months ** | |||
| Weight loss (kg), estimated mean (95% CI) | −7.82 (−9.07 - −6.57)a | −7.64 (−9.26 - −6.03) b | −1.45 (−2.55 - −0.35) ab |
| Percent weight change, estimated mean (95% CI) | −7.98 (−9.22 - −6.73) a | −7.98 (−9.64 - −6.33) b | −1.48 (−2.59 - −0.37) ab |
| Weight Change, 6 to 12 months * | |||
| Weight loss (kg), estimated mean (95% CI) | 0.69 (−0.51 - 1.88) | 0.73 (−0.29 - 1.76) | −0.66 (−1.58 - 0.26) |
| Percent weight change, estimated mean (95% CI) | 0.67 (−0.71 - 2.06) | 0.73 (−0.33 - 1.78) | −0.74 (−1.77 - 0.28) |
| Weight Change, 12 to 18 months * | |||
| Weight loss (kg), estimated mean (95% CI) | 1.88 (1.09 - 2.66) a | 1.94 (1.13 - 2.75) b | 0.33 (−0.58 - 1.24) ab |
| Percent weight change, estimated mean (95% CI) | 2.17 (1.31 - 3.02) a | 1.99 (1.14 - 2.84) b | 0.35 (−0.65 - 1.35) ab |
| Weight Change, 6 to 18 months * | |||
| Weight loss (kg), estimated mean (95% CI) | 2.55 (1.02 - 4.08) a | 2.66 (1.41 - 3.90) b | −0.31 (−1.68 - 1.06) ab |
| Percent weight change, estimated mean (95% CI) | 2.83 (1.09 - 4.57) a | 2.75 (1.41 - 4.09) b | −0.37 (−1.85 - 1.12) ab |
| Weight Change, baseline to 18 months ** | |||
| Weight loss (kg), estimated mean (95% CI) | −5.34 (−6.95 - −3.73) a | −5.22 (−7.24 - −3.20) b | −1.38 (−3.08 - 0.33) ab |
| Percent weight change, estimated mean (95% CI) | −5.48 (−7.09 - −3.87) a | −5.55 (−7.47 - −3.64) b | −1.51 (−3.30 - 0.28) ab |
| Weight loss of >=5% or greater, n(%) | |||
| Month 6 | 76 (42.37%) a | 77 (43.24%) b | 26 (14.39%) ab |
| Month 12 | 67 (40.40%) a | 72 (43.32%) b | 27 (16.29%) ab |
| Month 18 | 55 (38.35%) a | 57 (39.79%) b | 31 (21.86%) ab |
Motivationally Focused differed from Control at the p <0.05 level
Skill-Based differed from Control at the p <0.05 level
Controlling for weight change, 0–6 months, as well as clinic site
Controlling for baseline weight, as well as clinic site
Maintenance treatment conditions had similar attendance at group sessions during the 6-month weight loss induction, with individuals receiving motivation-focused maintenance attending an average of 17 sessions during the initial 6-month program (71%) and those in the standard skill-based maintenance attending 18 (75%).
18-Month Weight Maintenance Outcomes
Weight losses at 18-month follow-up were comparable for the two maintenance approaches, with both maintenance groups achieving clinically and statistically significant greater 18-month weight losses than the control group. Weight regain in the 12-month maintenance programs (i.e., from months 6 to 18) was comparable between the two approaches. Minimal regain was apparent from months 6 to 12, with no significant differences between the groups. Greater regain was apparent in the interval from months 12 to 18, but there were no significant differences in the trajectory of weight regain between the active maintenance groups at any point.
Attendance at maintenance sessions tended to be greater for those in the skill-based maintenance program (12.6 ± 6.8 or 52% of available sessions) than participants in the motivation-focused approach (10.8 ± 7.1 or 45% of sessions; p=.05). Further, participants in the skill-based maintenance program submitted more self-monitoring diaries during maintenance (15.9 ±15.5 or 33%) than those in the motivation-focused maintenance arm (11.3 ±14.5 or 24%; p=.01). In both maintenance interventions, attendance at treatment sessions was related to submission of self-monitoring diaries (rho= 0.77 for motivation-focused [p< .0001] and rho=0.76 for skill-based groups [p< .0001]).
Adherence, specifically attendance at sessions and self-monitoring diaries, has consistently been associated with magnitude of weight loss in previous studies (16, 37, 38). The correlation between attendance and weight change from months 6 to 18 within the skill-based group was −0.36 (p=.0003), indicating that greater attendance at skill-based sessions was associated with smaller weight increases during maintenance. In contrast, attendance was not significantly correlated with weight change in the motivation-focused arm (rho= −0.15). Likewise, there was a non-significantly stronger association between the number of self-monitoring diaries submitted during maintenance and weight change in the skill-based group (rho = −0.39; p0003C.0001) than in the motivation-focused group (rho = −0.22; p = .02). There correlations between self-monitoring behavior and weight change did not differ significantly between treatment conditions (p=.19).
Motivational and Self Identity Measures
At the end of the initial 6-month weight loss program, participants in both active treatment arms had higher autonomous motivations for self regulation than controls (Table 2), with no difference between them. However, participants in the motivation-focused maintenance program sustained a high level of autonomous reasons for self regulation; whereas, decreases in autonomous motivations for self regulation occurred in the skill-based group, resulting in significantly higher levels of autonomous self regulation in the motivation-focused program than the skill-based program at 12 months and similar trends at 18 months. The motivation-focused group maintained significantly higher levels of autonomous self regulation than seen among controls at all follow-up points, indicating that the motivational intervention resulted in the targeted changes. In contrast the skill-based program did not differ significantly from controls with respect to autonomous self regulation during the maintenance phase. Further, there were no differences between skill-based and motivation-focused groups in controlled motivations for self regulation. Autonomous self regulation was associated with weight change during maintenance in the motivation-focused group (r = −0.24, p=.02) but not within the skill-based group (r = −0.08, p= .45). Controlled self regulation was not associated with weight loss in either maintenance group (r = 0.17, p=.09 in the motivation-focused group; r = 0.13, p=.22 in the skill-based group).
Table 2.
Motivational and Self Concept Measures
| Variable | Visit | Motivation- Focused N |
Skill- Based N |
Control N |
Motivation- Focused |
Skill-Based | Control |
|---|---|---|---|---|---|---|---|
| Self Regulation | |||||||
| Autonomous | 0 Months | 113 | 113 | 110 | 6.62 (±0.50) | 6.54 (±0.61) | 6.56 (±0.53) |
| 6 Months | 109 | 109 | 94 | 6.61 (±0.61) a | 6.57 (±0.59) | 6.29 (±0.95) a | |
| 12 Months | 106 | 104 | 88 | 6.59 (±0.63) ac | 6.47 (±0.65) c | 6.23 (±0.93) a | |
| 18 Months | 103 | 98 | 88 | 6.53 (±0.72) a | 6.39 (±0.76) | 6.27 (±0.87) a | |
| Controlled | 0 Months | 113 | 113 | 110 | 3.33 (±1.35) c | 2.92 (±1.17) bc | 3.40 (±1.30) b |
| 6 Months* | 109 | 109 | 94 | 3.40 (±1.37) | 2.99 (±1.22) | 3.55 (±1.44) | |
| 12 Months* | 106 | 104 | 88 | 3.62 (±1.49) a | 3.13 (±1.38) | 3.36 (±1.40) a | |
| 18 Months* | 103 | 98 | 88 | 3.54 (±1.46) | 3.05 (±1.34) | 3.39 (±1.50) | |
| Focus on Progress | 0 Months | 113 | 113 | 110 | 2.66 (±1.01) | 2.69 (±0.90) | 2.69 (±0.98) |
| 6 Months | 109 | 109 | 94 | 3.90 (±0.88) a | 3.86 (±0.89) b | 3.17 (±0.93) ab | |
| 12 Months | 106 | 104 | 88 | 3.32 (±0.95) a | 3.44 (±0.88) b | 3.02 (±0.91) ab | |
| 18 Months | 103 | 98 | 88 | 3.20 (±1.03) | 3.26 (±0.94) | 2.98 (±1.01) | |
| Self Reinforcement | 0 Months | 113 | 113 | 110 | 18.5 (±4.36) | 19.5 (±4.16) | 18.6 (±4.06) |
| 6 Months | 109 | 109 | 94 | 19.7 (±4.01) a | 19.8 (±4.12) b | 18.3 (±4.47) ab | |
| 12 Months | 106 | 104 | 88 | 19.2 (±4.17) | 20.0 (±4.02) b | 18.6 (±4.34) b | |
| 18 Months | 103 | 98 | 88 | 19.4 (±4.18) | 20.2 (±4.29) b | 18.3 (±4.41) b | |
| Self Concept | |||||||
| Exerciser Identity | 0 Months | 113 | 113 | 110 | 9.10 (±4.50) | 9.81 (±4.75) | 8.96 (±4.36) |
| 6 Months | 109 | 109 | 94 | 11.8 (±4.45) a | 12.4 (±4.75) b | 9.30 (±4.35) ab | |
| 12 Months | 106 | 104 | 88 | 11.9 (±4.95) a | 11.9 (±4.92) b | 9.01 (±4.70) ab | |
| 18 Months | 103 | 98 | 88 | 11.9 (±5.20) a | 12.1 (±5.16) b | 8.96 (±4.71) ab | |
| Dieter Identity | 0 Months | 113 | 113 | 110 | 8.04 (±4.08) | 8.11 (±3.53) | 7.94 (±3.48) |
| 6 Months | 109 | 109 | 94 | 12.1 (±3.87) a | 12.4 (±4.18) b | 9.40 (±4.14) ab | |
| 12 Months | 106 | 104 | 88 | 12.3 (±4.24) a | 11.7 (±4.29) b | 9.42 (±3.91) ab | |
| 18 Months | 103 | 98 | 88 | 11.9 (±4.15) a | 12.1 (±4.32) b | 8.80 (±4.11) ab | |
| Weight Loser Identity | 0 Months | 113 | 113 | 110 | 8.94 (±3.63) | 9.28 (±3.42) | 9.15 (±3.27) |
| 6 Months | 109 | 109 | 94 | 12.7 (±3.62) a | 12.6 (±3.71) b | 9.71 (±3.64) ab | |
| 12 Months | 106 | 104 | 88 | 12.4 (±3.92) a | 12.4 (±3.84) b | 9.90 (±3.80) ab | |
| 18 Months | 103 | 98 | 88 | 12.2 (±4.12) a | 12.3 (±4.05) b | 9.22 (±3.53) ab | |
Motivationally Focused differed from Control at the p <0.05 level
Skill-Based differed from Control at the p <0.05 level
Motivationally Focused differed from Skill-Based at the p <0.05 level
P-values were calculated from Wilcoxon test
Adjusted for baseline value
Focusing on previous progress was specifically addressed as a strategy to stay motivated in the motivation-focused program only; yet both groups reported significantly greater focus on progress at 6- and 12-months compared with controls and no differences between the maintenance conditions with respect to the importance of this strategy were observed. By 18-month follow up, there were no differences between the intervention conditions and controls. The degree to which participants indicated they focused on their progress was correlated with weight maintenance in both programs, with great focus on progress associated with smaller regains (in motivation-focused, r = 0.50, p< .001 and in skill-based, r = −0.38, p< .001). Higher frequency of reinforcing, pleasurable activities was associated with smaller weight gains during maintenance among both the motivation-focused group (r = -0.20, p< .05), which was instructed to increase reinforcing activities, and in the skill-based group (r = −0.27, p < .01), which was not.
Participants entered the study without strong self concepts as either an exerciser or a successful weight control agent (Table 2). However, both active treatment groups indicated greater self identity as both an exerciser and as successful at weight control than controls at every post-treatment assessment point, with no differences between the skill-based and motivation-focused groups. Furthermore, greater self identification as an exerciser was associated with weight change during the maintenance phase for both skill-based (r = −0.29, p < .01) and motivation-focused programs (r = −0.43, p < .001).
Variables Associated with Weight Loss within the Two Maintenance Programs
Multivariate models to predict weight change during the maintenance phase within each program considered adherence variables (attendance and self monitoring diaries) and motivational parameters (autonomous self regulation, controlled self regulation, self concept as exerciser, self concept as weight loss success, focus on progress, and reinforcing activities). Different predictors emerged for the two programs. Within the skill-based program, self-monitoring diaries and successful weight maintainer self concept predicted weight change during the maintenance phase. Each additional diary submitted in this group was associated with a reduction of 0.13 kg (p = .001) in weight regain and each additional unit increase on the weight maintainer self-identity scale was associated with a reduction in 0.56 kg (p < .001) in regain. In the motivation-focused program, focus on progress and self concept as an exerciser predicted weight change, where each unit increase on the focus on progress scale was associated with a reduction of 2 kg (p<.001) in regain and each unit increase on the self-concept as an exerciser scale was associated with a reduction of 0.28 kg (p = .02). Thus, the typical predictors of standard behavioral weight control outcomes (adherence measures) were not predictive in the novel maintenance program. Furthermore, while the effect of autonomous self regulation was unaffected by the adherence measures, it was completely attenuated by focus on progress and exercise self identify; focus on progress attenuated 85% of the effect of autonomous self regulation and exercise self identity attenuated 69% of the effect of autonomous self regulation, and together the two factors fully attenuated the relationship between weight loss and autonomous self regulation.
DISCUSSION
The PRIDE study demonstrated effective weight maintenance outcomes at 18 months with similarly positive results achieved by the traditional skill-based approach and the novel motivation-focused program. The final 18-month weight loss average of −5.5% among women in the skill-based group is comparable to outcomes reported for the Diabetes Prevention Program (40) and other behavioral obesity programs (5). Thus, the skill-based approach implemented in the current study reflected best practices of obesity treatment clinical trials, and the finding that the motivation-focused approach was as effective as the successful standard skill-based method suggests that this novel weight maintenance program offers a viable evidence-based alternative approach for weight maintenance.
The pursuit of strategies to enhance weight maintenance has been a pressing challenge for obesity researchers. Although the novel maintenance program did not result in superior outcomes than the standard skills approach, the success of this new motivationally-based approach provides clinicians and researchers with an attractive intervention alternative to utilize when addressing the challenge of sustaining weight loss. To maximize the clinical utility of this novel approach, further research is warranted to identify whether some women prefer one approach over the other and if congruence between preference and treatment approach has any implications for success in weight maintenance.
Prior studies have examined specific motivational components in weight loss or weight maintenance programs, but to our knowledge, this is the first study to examine a theory-based weight maintenance program that incorporates multiple motivational strategies. The intervention demonstrated some of the anticipated benefits in targeted motivational constructs in the program. The specific focus on eliciting personalized reasons for behavior change, a central feature of the motivation-focused program, resulted in sustained autonomous self regulation levels in this group. Significantly higher autonomous motivations for self regulation during maintenance in the motivation-focused group than the skill-based group would suggest that consistent and specific attention on eliciting and supporting personally-relevant motivations for weight management promoted internalization of autonomous self regulation and forestalled the decline in autonomous self regulation seen over the course of the skill-based program. Previous research with morbidly obese individuals undergoing a medically-supervised diet similarly demonstrated a relationship between autonomous self regulation and weight change (13). However, Williams and colleagues found an association between autonomous self regulation and attendance which was not observed in the current study, perhaps reflecting the shorter, 6-month period examined in that study or greater pressure to attend their program which provided medical supervision and food. More recently, Silva and colleagues demonstrated that a self-determination theory guided weight control treatment approach that shared some characteristics with the current motivation-focused maintenance program demonstrated significantly better weight losses than a more standard health education approach (14). Responses to several other motivational constructs changed over time in both the motivation-focused and skill-based programs, and these were associated with weight loss outcomes in both conditions. Specifically, stronger self concept as a successful weight loss maintainer and self-identity as an exerciser emerged in both groups, even though there was no explicit focus on these parameters within the skill-based program. This might be due to the fact that both maintenance groups were successful in achieving weight maintenance. Self identity theory would suggest that the more an individual engages in a behavior, the more that behavior will become central to the person’s self-concept. Inasmuch as participants in both maintenance programs were successful and engaged in appropriate weight regulation behaviors to support long-term weight maintenance, it might be expected that participants in both programs would experience changes in their self concepts. The specific efforts within the motivation-focused maintenance program to cultivate an identity as an exerciser did not confer any added benefits compared to the standard skill-based approach, perhaps because of the emphasis in both programs on sustaining a high level of physical activity (200 min/week).
The focus on progress was associated with better weight maintenance in both maintenance approaches. Interestingly, although the strategy was manifestly addressed in the motivation-focused program, it was self-initiated in the skill-based program. The beneficial impact of emphasizing progress is consistent with Rothman’s (7) hypotheses and indicates the potential importance for this strategy in weight maintenance broadly, even in more traditional programs.
Participant treatment engagement in the skill-based maintenance program resembles that of other weight loss studies (16, 38). Specifically, greater attendance was significantly correlated with reduced weight regain and better overall weight loss outcomes. Interestingly, a different pattern emerged in the motivation-focused program. Attendance at sessions of the motivation-focused program was not associated with weight loss outcomes, raising a question about whether their sustained higher levels of autonomous self regulation facilitated their ability to achieve weight maintenance without the external monitoring of intervention staff. Submission of self-monitoring diaries was significantly correlated with weight loss outcomes in both the conditions; however, the relationship was much stronger in the skill-based program, accounting for 14% of the variance in weight change, compared to 5% in the motivationally-based program. The lack of association between attendance and weight loss outcomes and the minimal contribution of self-monitoring diaries to understanding the variability in weight change during maintenance in the motivation-focused program stands in stark contrast to previous literature and raises questions about whether there are different parameters that are associated with success within this novel approach. Internalization of perceived autonomous self regulation for the behaviors necessary to sustain weight loss would be argued as the mechanism of sustained behavior change by self determination theory and thus greater elucidation of this process as a potential mediator in the novel motivation-focused maintenance program is warranted. Self determination theory would further posit that supporting basic human needs of autonomy and competence are critical for sustained implementation of behavior change and therefore continued examination of the interplay between autonomy support and the cultivation of perceived competence (i.e., skill level) may be a fruitful avenue for future weight maintenance research.
Some limitations to the study must be noted. Participants were all overweight women with urinary incontinence; thus, weight maintenance outcomes may not generalize outside this population. Optimism that these results translate to overweight women more broadly can be found in the similarities between the baseline characteristics of PRIDE participants and those of other studies of overweight populations with obesity-related co-morbidities (41). Further, the weight losses observed during the initial weight loss induction period of PRIDE are quite similar to those reported in other studies, (38, 42) and the weight change in the skill-based maintenance program is comparable to what has been reported by others (5). Whether this motivation-focused intervention would also be effective among overweight men remains to be seen. Further, assessment of motivational variables was limited, with several measures consisting of single items. Despite these cautions, this novel maintenance approach offers great promise for expanding effective treatment alternatives for sustained weight control.
Future explorations of motivational maintenance approaches would benefit from a more extensive approach to assessing the range of motivational constructs and analyses examining whether these constructs mediate treatment outcomes. Furthermore, inclusion of self efficacy measures consistent with the social cognitive theory based skills building approach would permit examination of separate and combined effects of self determination theory and social cognitive theory derived constructs. Such a research agenda will further the identification of individuals most likely to benefit from motivationally-focused maintenance (or from skills-based approaches) and the mechanism(s) of action by which the interventions are effective. This will also allow further refinement of the motivational goals addressed in treatment and the strategies most likely effective in achieving them.
Supplementary Material
ACKNOWLEDGEMENTS
This research was supported in part by grants U01DK067860, U01 DK067861 and U01 DK067862 from the National Institute of Diabetes and Digestive and Kidney Diseases. Funding was also provided by the Office of Research on Women’s Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health. See online supplemental materials for full author acknowledgements.
Footnotes
Trial Registration: clinicaltrials.gov identifier: NCT00091988
Supplemental information is available at International Journal of Obesity’s website.
Conflict of Interest
The authors have no financial interests in relation to the work reported in this manuscript.
Contributor Information
Delia Smith West, University of Arkansas for Medical Sciences.
Amy A. Gorin, University of Connecticut, Storrs
Leslee L. Subak, University of California, San Francisco and San Francisco VA Medical Center
Gary Foster, Temple University.
Charlotte Bragg, University of Alabama at Birmingham.
Jacki Hecht, The Miriam Hospital, Providence RI.
Michael Schembri, University of California, San Francisco.
Rena R. Wing, Warren Alpert Medical School at Brown University
REFERENCES
- 1.Jeffery RW, Drewnowski A, Epstein LH, Stunkard A, Wilson TG, Wing RR, et al. Long-term maintenance of weight loss: Current status. Health Psychology. 2000;19:5–16. doi: 10.1037/0278-6133.19.suppl1.5. [DOI] [PubMed] [Google Scholar]
- 2.Wing RR, Gorin AA. Oxford Textbook of Primary Medical Care. Oxford: Oxford University Press; 2003. Obesity. [Google Scholar]
- 3.Wing RR, Papandonatos G, Fava JL, Gorin AA, Phelan S, McCaffery J, et al. Maintaining large weight losses: the role of behavioral and psychological factors. Journal of Consulting & Clinical Psychology. 2008;76:1015–1021. doi: 10.1037/a0014159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wing RR, Phelan S. Long-term weight loss maintenance. American Journal of Clinical Nutrition. 2005;82(suppl):222S–225S. doi: 10.1093/ajcn/82.1.222S. [DOI] [PubMed] [Google Scholar]
- 5.Perri MG, Corsica JA. Improving maintenance of weight loss in behavioral treatment of obesity. In: Wadden TA, Stunkard AJ, editors. Handbook of obesity treatment. New York: The Guilford Press; 2002. pp. 357–379. [Google Scholar]
- 6.Wing RR. Behavioral Weight Control. In: Wadden TA, Stunkard AJ, editors. Handbook of Obesity Treatment. New York: Guilford Press; 2002. pp. 301–316. [Google Scholar]
- 7.Rothman AJ. Toward a theory-based analysis of behavioral maintenance. Health Psychology. 2000;19:64–69. doi: 10.1037/0278-6133.19.suppl1.64. [DOI] [PubMed] [Google Scholar]
- 8.Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd edn. New York: Guilford Press; 2002. [Google Scholar]
- 9.Burke BL, Arkowitz H, Dunn C. The efficacy of motivational interviewing and it's applications: What we know so far. In: Miller WR, Rollnick S, editors. Motivational Interviewing: Preparing People to Change. 2nd edn. New York: Guilford Press; 2002. pp. 217–250. [Google Scholar]
- 10.West DS, Gore SA, DiLillo Vi, Greene PG, Bursac Z. Motivational interviewing improves weight loss in women with Type 2 Diabetes. Diabetes Care. 2007;30:1081–1087. doi: 10.2337/dc06-1966. [DOI] [PubMed] [Google Scholar]
- 11.Carels RA, Darby L, Cacciapaglia HM, Konrad K, Coit C, Harper J, et al. Using motivational interviewing as a supplement to obesity treatment: A stepped-care approach. Health Psychology. 2007;26:369–374. doi: 10.1037/0278-6133.26.3.369. [DOI] [PubMed] [Google Scholar]
- 12.Deci E, Ryan R. Intrinsic motivation and self-determination in human behavior. New York: Plenum; 1985. [Google Scholar]
- 13.Williams GC, Grow VM, Freedman ZR, Ryan RM, Deci EL. Motivational predictors of weight loss and weight loss maintenance. Journal of Personality and Social Psychology. 1996;70:115–126. doi: 10.1037//0022-3514.70.1.115. [DOI] [PubMed] [Google Scholar]
- 14.Silva MN, Vieira PN, Coutinho SR, Minderico CS, Matos MG, Sardinha LB, et al. Using self-determination theory to promote physical activity and weight control: a randomized controlled trial in women. Journal of Behavioral Medicine. 2010;33:110–122. doi: 10.1007/s10865-009-9239-y. [DOI] [PubMed] [Google Scholar]
- 15.Subak LL, Wing R, West DS, Franklin F, Vittinghoff E, Creasman JM, et al. Randomized trial of a behavioral weight loss program for urinary incontinence in overweight and obese women. New England Journal of Medicine. 2009;360:481–490. doi: 10.1056/NEJMoa0806375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Diabetes Prevention Program Research Group. Achieving weight and activity goals among Diabetes Prevention Program lifestyle participants. Obesity Research. 2004;12:1426–1435. doi: 10.1038/oby.2004.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wadden TA, West D, Delahanty L, Jakicic J, Rejeski W, Williamson D, et al. The Look AHEAD Study: A description of the lifestyle intervention and the evidence supporting it. Obesity. 2006;14:737–752. doi: 10.1038/oby.2006.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wing RR, Tate DF, Gorin AA, Raynor HA, Fava JL. A self-regulation program for maintenance of weight loss. New England Journal of Medicine. 2006;355:1563–1571. doi: 10.1056/NEJMoa061883. [DOI] [PubMed] [Google Scholar]
- 19.Crerand C, Wadden T, Foster G, Sarwer D, Paster L, Berkowitz R. Changes in obesity-related attitudes in women seeking weight reduction. Obesity. 2007;15:740–747. doi: 10.1038/oby.2007.590. [DOI] [PubMed] [Google Scholar]
- 20.Jeffery RW, Linde JA, Finch EA, Rothman AJ, King CM. A satisfaction enhancement intervention for long-term weight loss. Obesity. 2006;14:863–869. doi: 10.1038/oby.2006.100. [DOI] [PubMed] [Google Scholar]
- 21.Linde JA, Jeffery RW, Finch EA, Ng DM, Rothman AJ. Are unrealistic weight loss goals associated with outcomes for overweight women? Obesity Research. 2004;12:569–576. doi: 10.1038/oby.2004.65. [DOI] [PubMed] [Google Scholar]
- 22.Finch EA, Linde JA, Jeffery RW, Rothman AJ, King CM, Levy RL. The effects of outcome expectations and satisfaction on weight loss and maintenance: Correlational and experimental analyses--a randomized trial. Health Psychology. 2005;24:608–616. doi: 10.1037/0278-6133.24.6.608. [DOI] [PubMed] [Google Scholar]
- 23.Smith C, Burke L, Wing R. 6-month outcome of two behavioral weight loss treatments focusing on primary motivations for weight loss. Obesity Research. 1999;7 [Google Scholar]
- 24.Festinger LA. A Theory of Cognitive Dissonance. Stanford: Stanford Press; 1957. [Google Scholar]
- 25.Wilson DK, Friend R, Teasley N, Green S, Reaves IL, Sica DA. Motivational versus social cognitive interventions for promoting fruit and vegetable intake and physical activity in African American Adolescents. Annals of Behavioral Medicine. 2002;24:310–319. doi: 10.1207/S15324796ABM2404_07. [DOI] [PubMed] [Google Scholar]
- 26.Leake R, Friend R, Wadhwa N. Improving adjustment to chronic illness through strategic self-presentation: an experimental study on a renal dialysis unit. Health Psychology. 1999;18:54–62. doi: 10.1037//0278-6133.18.1.54. [DOI] [PubMed] [Google Scholar]
- 27.Vansteenkiste M, Sheldon KM. There's nothing more practical than a good theory: Interviewing and self-determination theory. British Journal of Clinical Psychology. 2006;45:63–82. doi: 10.1348/014466505X34192. [DOI] [PubMed] [Google Scholar]
- 28.Silva MN, Markland D, Minderico CS, Vieira PN, Castro MM, Coutinho SR, et al. A randomized controlled trial to evaluate self-determination theory for exercise adherence and weight control: rationale and intervention description. BMC Public Health. 2008;8:234–246. doi: 10.1186/1471-2458-8-234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hunt GM, Azrin NH. A community reinforcement approach to alcoholism. Behavior Research and Therapy. 1973;11:91–104. doi: 10.1016/0005-7967(73)90072-7. [DOI] [PubMed] [Google Scholar]
- 30.Lewinsohn P, Libet J. Pleasant Events, Activity Schedules and Depressions. Journal of Abnormal Psychology. 1972;79:291–295. doi: 10.1037/h0033207. [DOI] [PubMed] [Google Scholar]
- 31.Stuart RB. Behavioral control of overeating. Behavior Therapy. 1967;5:357–365. [Google Scholar]
- 32.Levesque CS, Williams GC, Elliot D, Pickering MA, Bodenhamer B, Finley PJ. Validating the theoretical structure of the Treatment Self-Regulation Questionnaire (TSRQ) across three different health behaviors. Health Education Research. 2007;22:691–702. doi: 10.1093/her/cyl148. [DOI] [PubMed] [Google Scholar]
- 33.Resnicow K, Campbell MK, Carr C, McCarty F, Wang T, Periasamy S, et al. Body and Soul: a dietary intervention conducted through African-American churches. American Journal of Preventive Medicine. 2004;27:97–105. doi: 10.1016/j.amepre.2004.04.009. [DOI] [PubMed] [Google Scholar]
- 34.Anderson DF, Cychosz CM. Development of an Exercise Identify Scale. Perceptual and Motor Skills. 1994;78:747–751. doi: 10.1177/003151259407800313. [DOI] [PubMed] [Google Scholar]
- 35.Anderson DF, Cychosz CM. Exploration of the relationship between exercise behavior and exercise identity. Journal of Sports Behavior. 1995;21:233–241. [Google Scholar]
- 36.Cardinal BJ, Cardinal MK. Changes in exercise behavior and exercise identify associated with a 14-week aerobic exercise class. Journal of Sports Behavior. 1997;20:377–386. [Google Scholar]
- 37.Boutelle KN, Kirschenbaum DS. Further support for consistent self-monitoring as a vital component of successful weight control. Obesity Research. 1998;6:219–224. doi: 10.1002/j.1550-8528.1998.tb00340.x. [DOI] [PubMed] [Google Scholar]
- 38.Wadden TA, West DS, Neiberg R, Wing RR, Ryan DH, Johnson KC, et al. One-Year Weight Losses in the Look AHEAD Study: Factors Associated with Success. Obesity. 2009;17:713–722. doi: 10.1038/oby.2008.637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Little RJA, Rubin DB. Statistical analysis with missing data. New York: Wiley; 1987. [Google Scholar]
- 40.West DS, Prewitt TE, Bursac Z, Felix HC. Weight loss of Black, White and Hispanic Men and Women in the Diabetes Prevention Program (DPP) Obesity. 2008;16:1413–1420. doi: 10.1038/oby.2008.224. [DOI] [PubMed] [Google Scholar]
- 41.Diabetes Prevention Program Research Group. The Diabetes Prevention Program: Baseline characteristics of the randomized cohort. Diabetes Care. 2000;23:1619–1629. doi: 10.2337/diacare.23.11.1619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. New England Journal of Medicine. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.