Abstract
Coeliac disease (CD) is an autoimmune disorder which leads to chronic inflammation of the gut. Furthermore, CD is associated with upper gastrointestinal malignancies, particularly lymphoma of the small intestine. Besides lymphoma, an increased frequency of associated small bowel carcinoma has been described. Here we report the case of a 70-year-old male suffering from CD who was treated with a gluten-free diet presenting with complaints of nausea, vomiting and weight loss of about 8 kg in two months. He underwent esophagogastroduodenoscopy, which identified distention of the stomach and duodenum and in the pars horizontalis a distinct obstruction was suggestive. However, histopathological examination showed a normal mucosal membrane. Additionally, a computed tomography scan of the abdomen was performed which showed an expanded stomach and duodenum up to the ligament of Treitz. During an explorative laparotomy a small tumor was palpated near the ligament of Treitz. Subsequently, a duodenal segment resection was performed. After surgery, the patient recovered well and left our hospital in good condition.
Key Words: Small bowel, Small bowel carcinoma, Carcinoma, Coeliac disease
Background
Coeliac disease (CD), also called gluten-sensitive enteropathy or nontropical sprue, is a unique autoimmune disorder which results from the interaction between gluten and immune, genetic and environmental factors [1]. Originally CD was considered as a malabsorption syndrome of childhood, whereas it is now recognized as a disease which may be diagnosed at any age. Clinical manifestations of CD differ greatly among patients, varying from vague symptoms such as fatigue or malaise to a classical malabsorption syndrome including diarrhoea and steatorrhoea accompanied by abdominal pain or discomfort [2]. The cornerstone of the treatment of CD is a lifelong gluten-free diet (GFD) which leads to noticeable clinical improvement within two weeks in about 70% of patients [3].
Several studies have suggested increased mortality from gastrointestinal malignancies in patients with CD compared to the general population [1, 4,5,6]. Particularly the risk of small bowel malignancies, which is generally an uncommon form of cancer, is increased. We report a case of duodenal carcinoma in a patient suffering for CD.
Case Report
In September 2008, a 70-year-old Caucasian male was referred by his general practitioner due to malaise, nausea, vomiting and weight loss of about 8 kg in two months. In his medical history, the patient had undergone a Hartmann procedure in 1998 because of a perforated diverticulitis. In 1999 a reversal of the Hartmann procedure had occurred. In 2001 the patient had been diagnosed with CD by an esophagogastroduodenoscopy with duodenal biopsies for which he was treated with a GFD on which he responded well clinically and which he followed meticulously.
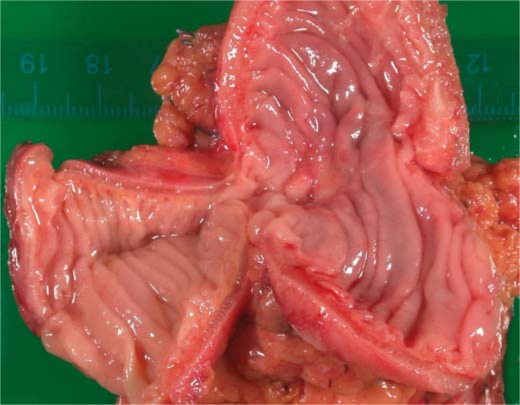
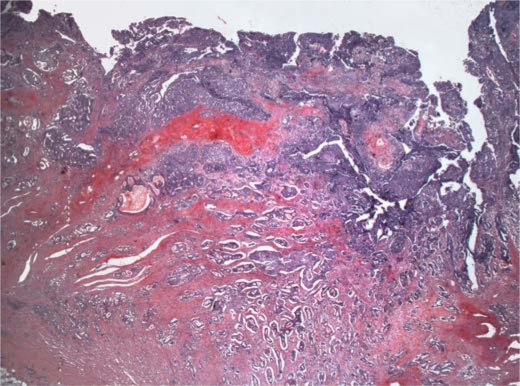
At admission, we performed an esophagogastroduodenoscopy which showed distention of the stomach and duodenum with retention of gastric and enteric fluid; more than 500 ml was aspirated. There was no problem in passing the pylorus. At the point of maximal intubation in the pars horizontalis, a distinct obstruction was suggestive with kinking and fixation but without evident pathology of the mucosa. Biopsies were taken but probably not at the point of maximum obstruction, which could not be reached because of kinking. Histology showed a normal mucosal membrane of the duodenum, without villous atrophy or increased intraepithelial lymphocytes. Additionally, a computed tomography scan of the abdomen was performed which showed an expanded stomach and duodenum up to the ligament of Treitz. An explorative laparotomy was performed, during which a small tumor was palpated near the ligament of Treitz. Subsequently, a duodenal segment resection was performed. Histological analyses revealed a moderately differentiated, infiltrating adenocarcinoma of 1.5 cm penetrating the muscularis propria and serosa, without invasion of local lymph nodes (stage T3N0M0 AJCC VI ed 2002) (fig. 1, fig. 2). After surgery, patient recovered well and left our hospital in good condition.
Fig. 1.
Duodenal segment resection showing the stenotic section.
Fig. 2.
Histology of the stenotic segment of the duodenum revealing a moderately differentiated infiltrative adenocarcinoma penetrating the muscularis propria and serosa.
Discussion
Malignancies involving the small bowel occur very infrequently in the general population. In the Netherlands, less than 100 cases a year of small bowel malignancies are revealed while at least 10,000 colorectal carcinomas are diagnosed. Despite the fact that the small bowel represents about 75% of the length and 90% of the surface area of the gastrointestinal tract, small bowel malignancies comprise about 2% of all gastrointestinal malignancies [7]. Next to the rarity of these lesions, the signs and symptoms patients present are usually vague and poorly defined, often delaying a correct diagnosis. Furthermore, conventional radiographic studies of the upper and lower intestinal tract often appear normal [8].
The association between carcinoma of the small bowel and CD was first reported in 1958 [9]. Since then, the association between CD and small bowel carcinoma is persistent although only based on a small number of patients of which the greater part is in the form of case reports. Swinson et al.[10] indicated that CD patients have an increased risk of developing small bowel adenocarcinoma (relative risk 82.6-fold). In addition, results of a national survey in the United States revealed similar results (relative risk 67-fold) [11]. A large population-based study of malignancy in patients which CD performed in Sweden confirmed the increased risk for small bowel cancer, although the risk was less compared to previous studies (10-fold) [12].
The etiologic factors predisposing to malignancy in CD are uncertain. Possibilities include immunologic disturbance associated with mucosal lymphocyte infiltration, premalignant changes in the damaged surface epithelial cells, increased permeability to oncogenic factors and malabsorption of protective substances such as vitamins A and E [10, 11]. Another hypothesis which has been postulated is that small bowel adenocarcinoma in CD arises through an adenoma-carcinoma sequence [13]. However, currently there are conflicting results regarding this hypothesis [14,15,16,17].
Despite the fact that a lifelong GFD leads to noticeable clinical and histological improvement in about 70% of patients [3], studies about the protective effect of GFD on malignancy are scarce. Most studies suggest that a GFD leads to a decreased incidence of lymphoma, cancer of the mouth, pharynx and oesophagus and a decreased mortality in CD [18,19,20,21]. However, according to our knowledge only one case report was published about the specific role of GFD concerning small bowel malignancy [22]. This report did not show a protective effect of GFD, however, further research is needed to confirm this hypothesis.
In conclusion, the present patient is an illustration that CD is a serious disease with possible serious complications such as duodenal adenocarcinoma. Despite the association between CD and small bowel malignancy, currently there are no recommendations for screening for this type of malignancy nor specific protocols for the follow-up of patients with CD. In view of our finding and based on the present scientific literature, we recommend that clinicians should take into account the possibility of small bowel malignancy in CD patients with vague symptoms such as fatigue or malaise, especially in combination with weight loss, despite a well-maintained GFD. In these patients early upper gastrointestinal endoscopy with duodenal biopsy should be performed.
Footnotes
This is an Open Access article licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 License (www.karger.com/OA-license), applicable to the online version of the article only. Distribution for non-commercial purposes only.
References
- 1.Green PH, Cellier C. Celiac disease. N Engl J Med. 2007;357:1731–1743. doi: 10.1056/NEJMra071600. [DOI] [PubMed] [Google Scholar]
- 2.Green PH. The many faces of celiac disease: clinical presentation of celiac disease in the adult population. Gastroenterology. 2005;128:S74–S78. doi: 10.1053/j.gastro.2005.02.016. [DOI] [PubMed] [Google Scholar]
- 3.Pink IJ, Creamer B. Response to a gluten-free diet of patients with the coeliac syndrome. Lancet. 1967;1:300–304. doi: 10.1016/s0140-6736(67)91238-x. [DOI] [PubMed] [Google Scholar]
- 4.Howdle PD, Jalal PK, Holmes GK, Houlston RS. Primary small-bowel malignancy in the UK and its association with coeliac disease. QJM. 2003;96:345–353. doi: 10.1093/qjmed/hcg058. [DOI] [PubMed] [Google Scholar]
- 5.Catassi C, Bearzi I, Holmes GK. Association of celiac disease and intestinal lymphomas and other cancers. Gastroenterology. 2005;128:S79–S86. doi: 10.1053/j.gastro.2005.02.027. [DOI] [PubMed] [Google Scholar]
- 6.West J, Logan RF, Smith CJ, Hubbard RB, Card TR. Malignancy and mortality in people with coeliac disease: population based cohort study. BMJ. 2004;329:716–719. doi: 10.1136/bmj.38169.486701.7C. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, Thun MJ. Cancer statistics, 2008. CA Cancer J Clin. 2008;58:71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- 8.Buckley O, Brien JO, Ward E, Doody O, Govender P, Torreggiani WC. The imaging of coeliac disease and its complications. Eur J Radiol. 2008;65:483–490. doi: 10.1016/j.ejrad.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 9.CASE RECORDS of the Massachusetts General Hospital: case 44362. N Engl J Med. 1958;259:491–495. doi: 10.1056/NEJM195809042591011. [DOI] [PubMed] [Google Scholar]
- 10.Swinson CM, Slavin G, Coles EC, Booth CC. Coeliac disease and malignancy. Lancet. 1983;1:111–115. doi: 10.1016/s0140-6736(83)91754-3. [DOI] [PubMed] [Google Scholar]
- 11.Green PH, Fleischauer AT, Bhagat G, Goyal R, Jabri B, Neugut AI. Risk of malignancy in patients with celiac disease. Am J Med. 2003;115:191–195. doi: 10.1016/s0002-9343(03)00302-4. [DOI] [PubMed] [Google Scholar]
- 12.Askling J, Linet M, Gridley G, Halstensen TS, Ekstrom K, Ekbom A. Cancer incidence in a population-based cohort of individuals hospitalized with celiac disease or dermatitis herpetiformis. Gastroenterology. 2002;123:1428–1435. doi: 10.1053/gast.2002.36585. [DOI] [PubMed] [Google Scholar]
- 13.Sellner F. Investigations on the significance of the adenoma-carcinoma sequence in the small bowel. Cancer. 1990;66:702–715. doi: 10.1002/1097-0142(19900815)66:4<702::aid-cncr2820660419>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 14.Fishman MJ, Jeejeebhoy KN, Gopinath N, Girotti MJ, Yeung EY, Cullen JB. Small intestinal villous adenoma and celiac disease. Am J Gastroenterol. 1990;85:748–751. [PubMed] [Google Scholar]
- 15.Marsch SC, Heer M, Sulser H, Hany A. Adenocarcinoma of the small intestine in celiac disease: case report and literature review. Schweiz Med Wochenschr. 1990;120:135–141. [PubMed] [Google Scholar]
- 16.Rampertab SD, Fleischauer A, Neugut AI, Green PH. Risk of duodenal adenoma in celiac disease. Scand J Gastroenterol. 2003;38:831–833. doi: 10.1080/00365520310004515. [DOI] [PubMed] [Google Scholar]
- 17.Johnston SD, Watson RG. Small bowel lymphoma in unrecognized coeliac disease: a cause for concern? Eur J Gastroenterol Hepatol. 2000;12:645–648. doi: 10.1097/00042737-200012060-00012. [DOI] [PubMed] [Google Scholar]
- 18.Corrao G, Corazza GR, Bagnardi V, Brusco G, Ciacci C, Cottone M, Sategna GC, Usai P, Cesari P, Pelli MA, Loperfido S, Volta U, Calabro A, Certo M. Mortality in patients with coeliac disease and their relatives: a cohort study. Lancet. 2001;358:356–361. doi: 10.1016/s0140-6736(01)05554-4. [DOI] [PubMed] [Google Scholar]
- 19.Holmes GK, Prior P, Lane MR, Pope D, Allan RN. Malignancy in coeliac disease – effect of a gluten free diet. Gut. 1989;30:333–338. doi: 10.1136/gut.30.3.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Collin P, Reunala T, Pukkala E, Laippala P, Keyrilainen O, Pasternack A. Coeliac disease – associated disorders and survival. Gut. 1994;35:1215–1218. doi: 10.1136/gut.35.9.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Logan RF, Rifkind EA, Turner ID, Ferguson A. Mortality in celiac disease. Gastroenterology. 1989;97:265–271. doi: 10.1016/0016-5085(89)90060-7. [DOI] [PubMed] [Google Scholar]
- 22.Kingham JG, Ramanaden D, Dawson A. Metachronous small-bowel adenocarcinoma in coeliac disease: gluten-free diet is not protective. Scand J Gastroenterol. 1998;33:218–222. doi: 10.1080/00365529850166987. [DOI] [PubMed] [Google Scholar]