Abstract
Delayed entry into HIV clinical care and poor retention in care has been associated with increased morbidity and mortality. To characterize the reasons for patients who eventually did enter HIV care after a delay and/or returned to care after a gap of 6 or more months, 130 semi-structured interviews about barriers to and facilitators for prompt entry into and sustained HIV clinical care were conducted in a clinic setting in the Deep South; responses were coded and analyzed quantitatively. Barriers/facilitators were positioned within superordinate categories of personal and structural barriers/facilitators and denial. Personal barriers to entry into care outweighed structural barriers, with denial reported by 74% of the sample. Barriers to retention in care were more evenly distributed between personal and structural barriers, with denial a barrier for 24%. Because of the high incidence of denial-based barriers, the role of this barrier and its resolution should be explored further.
Keywords: barriers, Deep South, engagement in care, facilitators, HIV
The disproportionate burden of HIV and AIDS in the Southern United States is well recognized. Multiple recent studies have documented the increased rates of HIV infection in the Southeastern United States, with growth rates in this region significantly outpacing the national average (Qian, Taylor, Fawal, & Vermund, 2006). Of the top 10 states in growth rates in HIV and AIDS cases, 4 are in the Deep South; a region specifically defined as Alabama, Georgia, Louisiana, Mississippi, North Carolina, and South Carolina (Whetten & Reif, 2006) Although the standard of care for HIV treatment is no different from the rest of the United States, this area of the country traditionally has high rates of poverty, lower education, and lower income than other parts of the country (Konkle-Parker, Erlen, & Dubbert, 2008). The number of new AIDS cases increased 37.6% in the Deep South from 2000 to 2005, compared to 12.6% in other Southern states and 17.0% nationally (excluding the Deep South; Centers for Disease Control and Prevention [CDC], 2005). This has led to increased HIV prevention efforts to address what has now become recognized as an HIV crisis in the Deep South (Copello, 2004).
Besides high rates of AIDS cases in the Deep South, other problems include the issues of delayed HIV diagnosis, further delays in entry into clinical care post-diagnosis, and limited engagement in HIV care over time. Increasing efforts to promote HIV testing is a national priority (CDC, 2005). However, facilitating movement from testing to care has received less attention. The consequences of delayed entry into care include higher odds of mortality and poor treatment responses (Lanoy et al., 2007). Moreover, the phenomenon of delaying entry into HIV care appears to be quite common in the Deep South and elsewhere. Specific to those in the Deep South, Krawczyk and colleagues’ (2006) research with 1,209 newly enrolled patients in a large primary care HIV clinic in Alabama found that 41% already had CDC-defined AIDS at the time of the initial clinic visit. In addition, 34% of those persons delayed entry into care for more than 1 year after their initial HIV diagnosis (Krawczyk, Funkhouser, Kilby, & Vermund, 2006), and 31% of patients in the same clinic site failed to attend their initial HIV care visit (Mugavero et al., 2006).
Once care is initiated, maintaining a level of care that is considered necessary for treatment success presents problems for many HIV-infected patients. For example, one study based in North Carolina found that almost half of a clinic-based sample attended fewer than three HIV-care visits per year (Napravnik et al., 2006) despite the guidelines of clinic visits every 3–4 months for viral load and CD4+ T cell evaluations (Panel on Antiretroviral Guidelines for Adults and Adolescents, 2008). In a study in a Veterans Affairs hospital in Houston, where there are few barriers to care related to insurance, Giordano et al. (2007) found that while only 17% of patients had poor retention in care in the first year after starting antiretroviral therapy as measured by having visits in two quarters of the year or less, this lower utilization of care was significantly related to mortality.
Giordano, Clark, Stapleton, Soriano, and Hwang (2008) recently provided a comprehensive overview of the barriers that have been found to influence the use of HIV care. The literature appears largely focused on systemic aspects of care entry (e.g., location, insurance), other structural barriers (e.g., access, transportation), and patient-level demographic factors (e.g., age, race, education), to the exclusion of more psychological factors. An exception was reported in a recent qualitative exploration of barriers to engagement in care by 76 people living with HIV (PLWH) in six different cities (Rajabiun et al., 2007). These authors identified (a) acceptance of HIV diagnosis; (b) coping with substance use, mental health issues, and stigma; (c) relationship with health care provider; (d) external support system; and (e) ability to navigate practical barriers to care as critical factors throughout the cycle of care engagement. Similarly, Rumptz et al. (2007) found negative health beliefs to be an important factor influencing early engagement in care as well as retention in care.
Thus, initiating HIV care after a diagnosis of HIV and maintaining care over time is a very real challenge for many PLWH and multiple barriers have been reported (Fowler-Brown, Ashkin, Corbie-Smith, Thaker, & Pathman, 2006; Heckman et al., 1998; Kalichman, Catz, & Ramachandran, 1999; Pathman, Fowler-Brown, & Corbie-Smith, 2006). The consequences for PLWH who delay care until they have AIDS or for those who attend clinic sporadically can be life-threatening. Focused efforts in gaining a better understanding of these phenomena in the Deep South, specifically, is particularly well-warranted given the disproportionate burden of HIV in these communities (Konkle-Parker et al., 2008; Krawczyk, Funkhouser, Kily, & Vermuch 2006; Parsons, Cruise, Davenport, & Jones, 2006; Reif, Geonnotti, & Whetten, 2006; Whetten & Reif, 2006).
The purpose of this study was to obtain detailed information from patients who were enrolled in care in a clinic setting in the Deep South (Mississippi), but had previously experienced a delayed entry into or gaps in their HIV care. Participants were asked about the barriers they encountered to enter HIV care, the facilitators that helped them enter care and the perceived barriers and facilitators in maintaining engagement in HIV clinical care. Because these PLWH were in care at the time of the interviews, the focus of this research was on the identification and exploration of factors that presented and continued to present challenges to individuals who ultimately successfully navigated their way to HIV care. The long-term goal of this research was to identify resources and strategies that could be effective in promoting rapid entry into care and maintenance in care through integrated intervention approaches specifically for this Deep South population.
Method
An anonymous semi-structured interview was conducted in a convenience sample of 130 individuals in clinical care at a large public clinic at a university medical center. The clinic was a public clinic supported by the state as well as by the federal government through Part C of the Ryan White Care Act, which provides federal funds to support HIV care for low income and uninsured PLWH. The clinic population of approximately 1,750 patients was 85% African American, 38% female, 90% low-income (incomes of $10,000 or less per year), and 58% without health insurance. Data were collected by approaching consecutive HIV-infected clinic patients on days when at least one data collector was available.
Inclusion criteria consisted of: (a) self-report of entry into HIV clinical care at least 6 months after HIV diagnosis, or (b) self-report of a gap in care of 6 months or more after entering HIV clinical care. Interviews were conducted in the exam room while waiting for the provider, and took approximately 10 minutes. The study was considered by the institution’s institutional review board to be exempt from the need to gather informed consent because data were gathered anonymously, and each individual was given an informational letter describing the purpose of the study and their right to refuse participation without risk to their medical treatment. Participants received a $5 gift card from a major department store after completing the interview.
Measures
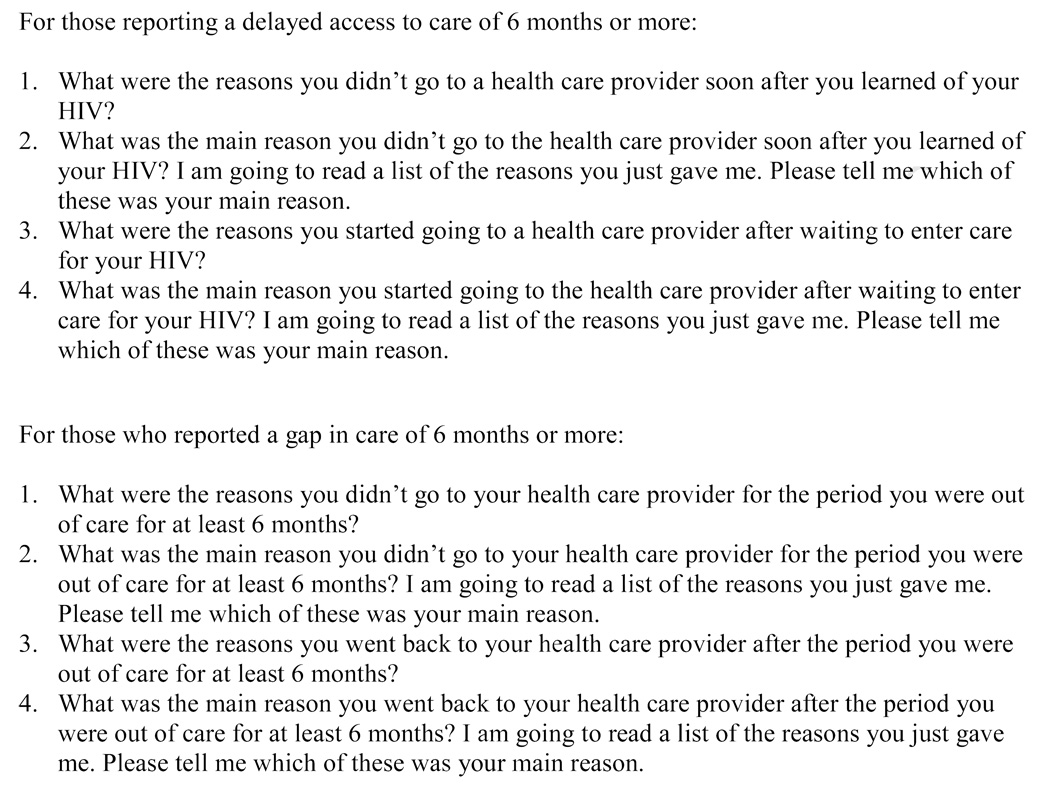
After being asked for demographic information, the interview consisted of open-ended questions (see Figure 1) asking for a description of the barriers to entering HIV clinical care within 6 months of diagnosis and/or maintaining HIV clinical care without a gap of at least 6 months, and then asking about the facilitators for entering and/or restarting HIV clinical care after a gap. For each concept area, participants were asked for all the barriers or facilitators, and after all were given, they were asked to identify the main barrier and main facilitator.
Figure 1.
Interview questions.
The tool used for the structured interview was developed by the Medical Monitoring Project from the CDC (Division of HIV/AIDS Prevention, 2008). The responses to the open-ended questions were spontaneous, not guided by the interviewer, and coded by the interviewer during the interview using a set of 20 codes predetermined by the CDC, with options of “other” for those responses that could not be considered as one of the available codes. Data collectors were trained by the first author, using role-plays to compare data collectors’ coding.
Data Analysis
Codes were analyzed with SPSS 15.0. In addition to frequency distributions of each code, the first and third authors grouped the responses into the superordinate categories of Personal Barriers and Structural Barriers, with 100% agreement on the appropriate category for each barrier and facilitator. Frequency distributions were calculated for each of these categories. Personal barriers were considered to be those intrinsic to the respondent, such as attitudes, beliefs, and emotions. Structural barriers were extrinsic factors affecting the respondent, such as barriers related to resources, support, or living situations. Tables 2 and 3 list the predetermined codes with the superordinate category of Personal or Structural barriers or facilitators.
Table 2.
Barriers Causing Delayed Access to Care and Gap in Care
| Barrier | Category | Delayed Entry into Care (n = 61) | Gap in Care (n = 94) | ||
|---|---|---|---|---|---|
| n (%) | Main Barrier n (%) |
n (%) | Main Barrier n (%) |
||
| Felt good, didn’t need to go | P(denial) | 29 (48%) | 14 (22%) | 20 (21%) | 12 (13%) |
| Other: denial | P(denial) | 14 (23%) | 8 (13%) | 7 (7%) | 6 (6%) |
| Didn’t want to think about being HIV positive |
P(denial) | 10 (16%) | 2 (3%) | 4 (4%) | 1 (1%) |
| Didn’t believe test result | P(denial) | 6 (10%) | 3 (5%) | 2 (2%) | 1 (1%) |
| Was worried about my privacy | P | 19 (31%) | 8 (13%) | 10 (11%) | 3 (3%) |
| Drinking or using drugs | P | 8 (13%) | 4 (7%) | 13 (14%) | 10 (11%) |
| Missed my appointment(s) | P | 1 (2%) | 1 (2%) | 11 (12%) | 6 (6%) |
| Other: scared | P | 9 (15%) | 3 (5%) | 0 | 0 |
| Other: codes related to not enough information about HIV |
P | 4 (7%) | 2 (3%) | 0 | 0 |
| Other: depression | P | 2(3%) | 0 | 7 (7%) | 3 (3%) |
| Didn’t like the clinic (for gap in care only) | P | N/A | - | 1 (1%) | 0 |
| Didn’t like the doctor or NP (for gap in care only) |
P | N/A | - | 3 (3%) | 3 (3%) |
| Other: I didn’t care because I was going to die soon |
P | 3 (5%) | 3 (5%) | 2 (2%) | 1 (1%) |
| Other: Just didn’t want to go | P | 3 (5%) | 0 | 0 | 0 |
| Forgot to go | P | 0 | 0 | 1 (1%) | 1 (1%) |
| Too busy to go | P | 1 (2%) | 0 | 2 (2%) | 0 |
| Initial CD4 count and viral load were good | P | 0 | 0 | 1 (1%) | 1 (1%) |
| Didn’t have money | St | 3 (5%) | 1(2%) | 8 (8%) | 3 (3%) |
| Didn’t have insurance | St | 2 (3%) | 0 | 9 (10%) | 6 (6%) |
| Incarcerated | St | 5 (8%) | 5 (8%) | 2 (2%) | 1 (1%) |
| Unable to get transportation | St | 3 (5%) | 1(2%) | 19 (20%) | 12 (13%) |
| Inconvenient (location, hours, time, etc.) | St | 1 (2%) | 0 | 7 (7%) | 4 (4%) |
| Didn’t know where to go | St | 6 (10%) | 1 (2%) | 2 (2%) | 1 (1%) |
| Moved or out of town | St | 0 | 0 | 20 (21%) | 8 (8%) |
| Other (Uncoded) | -- | 9 (15%) | 7 (12%) | 19 (20%) | 11 (12%) |
Note: P = personal barriers; NP = nurse practitioner; St: structural barriers; Barriers that had no endorsement, either for delayed entry into care or gap in care were: Living on the street; Hard to find the right doctor or a good doctor for me; Unable to get an earlier appointment; or Unable to get childcare. These were considered to be Structural Barriers
Table 3.
Facilitators for Entry into Clinical Care and for Return to Care
| Facilitator | Category | Delayed Entry into Care (n = 61) |
Gap in Care (n = 94) |
||
|---|---|---|---|---|---|
| N (%) | Main Facilitator N (%) |
N (%) | Main Facilitator N (%) |
||
| Felt worse/in hospital | P(denial) | 32 (52%) | 24 (39%) | 29 (31%) | 21 (22%) |
| Accepted my diagnosis of HIV | P(denial) | 7 (11%) | 2 (3%) | 2 (2%) | 1 (1%) |
| Family and friends convinced me to believe test result |
P(denial) | 1 (2%) | 1 (2%) | 0 | 0 |
| Decided I needed to take care of my health | P | 24 (39%) | 12 (19%) | 47 (50%) | 31 (33%) |
| Stopped drinking or using drugs | P | 4 (7%) | 1 (2%) | 7 (7%) | 3 (3%) |
| Other: Wanted to live (for entry into care) | P | 4 (7%) | 2 (3%) | N/A | - |
| Other: Fear of dying (for entry into care) | P | 4 (7%) | 2 (3%) | N/A | - |
| CD4 count and viral load got worse | P | 2 (3%) | 1 (2%) | 5 (5%) | 2 (2%) |
| Got a place to live | P | 1 (2%) | 1 (2%) | 0 | 0 |
| Came back into town | P | 0 | 0 | 10 (11%) | 3 (3%) |
| Felt less worried about my privacy | P | 2 (3%) | 1 (2%) | 2 (3%) | 1 (1%) |
| Other: For my kids (for entry into care and return to care |
P | 2 (3%) | 1 (2%) | 5 (5%) | 2 (2%) |
| Other: made new appt (for return to care) | P | N/A | - | 3 (3%) | 3 (3%) |
| Other: needed refills (for return to care) | P | N/A | - | 8 (8%) | 3 (3%) |
| Other: codes related to finding out more information about HIV |
P | 2 (3%) | 1 (2%) | 0 | 0 |
| Family members/friends made me go | St | 5 (7%) | 3 (5%) | 5 (5%) | 3 (3%) |
| Got out of jail | St | 4 (7%) | 1 (2%) | 1 (1%) | 0 |
| Health care provider reminded me | St | 2 (3%) | 2 (3%) | 2 (2%) | 2 (2%) |
| Was able to get transportation | St | 1 (2%) | 0 | 7 (7%) | 5 (5%) |
| It fit into my life better (location, hours, time, etc.) |
St | 0 | 0 | 4 (4%) | 1 (1%) |
| Found out where to go | St | 1 (2%) | 0 | 0 | 0 |
| Money not a problem | St | 0 | 0 | 2 (2%) | 1 (1%) |
| Insurance not a problem | St | 0 | 0 | 4 (4%) | 2 (2%) |
| Other (uncoded) | -- | 7 (11%) | 7 (11%) | 12 (13%) | 10 (11%) |
Note: P = personal facilitators; St = structural facilitators; Facilitators for entry into care or return to care that had no endorsement included: Was less busy; Childcare no longer a problem; Insurance not a problem; and Found the right doctor. The first was considered to be a Personal Facilitator, and the other 3 were considered to be Structural facilitators.
In addition to the two main superordinate categories, four different codes were grouped together to describe a category called “denial or avoidance coping.” This category included responses to the codes of “Felt good, didn’t need to go,” “Didn’t want to think about being HIV positive,” “Didn’t believe the test result,” or the use of the word “denial.” Because this was an anonymous survey, barriers and facilitators could not be evaluated in relation to objective data, such as actual clinic attendance, disease progression, or other information extracted from the medical chart.
Results
Participants
In July and August, 2007, 437 consecutive HIV-infected patients seeking routine clinical care were approached and 270 (62%) agreed to speak with research staff; 130 (48%) were eligible for the study as determined by self-reporting a 6-month or greater delay in initiating care or a 6-month or greater gap in clinical care. Of the 130 eligible for the survey, 61 (23%) reported that they had delayed entry into care, 94 (35%) reported that they had a previous gap in care, and 25 (9%) reported both delaying access to care and experiencing subsequent gaps in care.
As indicated in Table 1, the sample of participants was reflective of the demographics of the clinic from which it was drawn in that the great majority of patients were African American and low-income, more than half reported a heterosexual orientation, and almost half were women. Coded categories of barriers as well as the respective superordinate categories for each are presented in Table 2. Reported facilitators categories and superordinate categories are presented in Table 3.
Table 1.
Sample Characteristics
| Characteristic | N (%) | |
|---|---|---|
| Race | Black | 105 (81%) |
| Hispanic | 1 (1%) | |
| White | 23 (18%) | |
| Missing | 1 | |
| Gender | Male | 80 (62%) |
| Female | 48 (37%) | |
| Transgender | 1 (1%) | |
| Missing | 1 | |
| Age | M (SD) | 40.5 (9.3) |
| Sexual orientation | Gay or bisexual | 40 (31%) |
| Straight | 88 (68%) | |
| Unsure or refused | 2 (1%) | |
| Education | Some HS or less | 31 (24%) |
| HS or GED | 40 (31%) | |
| Some college | 44 (34%) | |
| College degree or above | 15 (11%) | |
| Current employment | Unemployed | 28 (22%) |
| Full time | 36 (28%) | |
| Part time | 11 (8%) | |
| Disability | 55 (42%) | |
| Income | < $10,000 (very low income) | 74 (57%) |
| 10,000 – 20,000 (low to mid-income) | 39 (30%) | |
| 20,000 – 50,000 (mid-income) | 14 (11%) | |
| Refused | 3 (2%) | |
| Diagnosis date | 1990 or before | 19 (15%) |
| 1991 – 1995 | 37 (28%) | |
| 1996–2000 | 42 (32%) | |
| 2001–2006 | 32 (25%) | |
| Entered care > 6 months after diagnosis |
Yes | 61 (47%) |
| Gap in care of > 6 months | No | 36 (28%) |
| 6–12 months | 49 (38%) | |
| 1–2 years | 27 (21%) | |
| 2–3 years | 13 (10%) | |
| 3–5 years | 3 (2%) | |
| > 5 years | 2 (2%) | |
Note: SD = standard deviation; HS = High School, grades 9–12; GED = Graduate Equivalent Degree, considered to be equivalent to a high school education.
Delayed Entry into HIV Care
Barriers to entering HIV care promptly
As presented in Table 2, the most commonly reported barriers to entering HIV care within 6 months of diagnosis included feeling good and thus feeling that care was not needed (48%), having concerns about privacy (31%), and self-reported denial (23%). When all barriers reflective of personal denial or active avoidance were combined (which included “Felt good, didn’t need to go,” “Denial,” “Didn’t want to think about being HIV-positive,” and “Didn’t believe test result”), 74% of those delaying entry into care reported experiencing one or more barriers within this global category, and almost half of the sample (43%) further identified one of these as the main barrier to their entry into care. Across all participants providing a main reason that could be coded (n = 54), 72% were personal and 13% were structural. Uncoded reasons (n = 7) included “just did not want to go” (reason unspecified) and “working hard to save my home.”
Facilitators to entering HIV care promptly
Facilitators were evaluated through responses to: What were the reasons you started going to a health care provider after waiting to enter care for your HIV? More than half of the sample of participants who delayed entry into HIV care reported having felt worse or being hospitalized as a facilitator to getting into HIV care (52%). Two other barriers were reported with some frequency: “Deciding I needed to take care of my health” (39%) and “Accepted my HIV diagnosis” (11%). Across all participants providing a main reason that could be coded (n = 54), 89% were personal and 11% were structural. Uncoded reasons (n = 7) included “I know I needed to come” (reason unspecified) and “Wanted something more for myself.”
Gap in HIV Care
Barriers to remaining in HIV care
Participants were queried with: What were the reasons you didn’t go to your health care provider for the period you were out of care for at least 6 months? Barriers reported most frequently included that they felt good and didn’t feel the need to come in for care (21%), had moved or were out of town (21%), and were unable to get transportation (20%). Twenty-four percent reported a denial-based barrier as their main reason for dropping out of care. Across all participants providing a main reason that could be coded (n = 84), 68% were personal and 48% were structural. Uncoded reasons (n = 10) included starting a new job, taking care of sick parents, or simply did not have the time to go.
Facilitators to re-entering care after a gap
Facilitators were evaluated through responses to: What were the reasons you went back to your health care provider after the period you were out of care for at least 6 months? As presented in Table 3, 50% reported deciding to take care of their health as a facilitator to getting back into care, and 31% reported that feeling worse or being in the hospital helped them re-engage in clinical care. Across participants providing main reasons for re-engagement in HIV care that could be coded (n = 84), the vast majority (84%) were classified as personal, with only 13% falling in the structural category. Main reasons falling in the uncoded category included becoming pregnant, increased fear of death for unexplained reasons, or because of a personal experience.
Higher Order Categories
As presented in Table 4, when considering reasons that created barriers to and that facilitated prompt entry into care and consistent engagement in HIV care at the clinic, there was some degree of consistency in the personal and structural higher order categories. The pattern was for more participants to report reasons that were personal in nature (not directly related to the structure of HIV care and access to it) for delays and gaps. Gaps in care, however, appeared more balanced between the personal and structural categories for barriers but not so for facilitators. Facilitators appeared largely personal in nature.
Table 4.
Summary of Proportion Reporting Personal or Structural Categories for Main Barriers and Facilitators for Delay and Gaps in Care
| Delay in care | Gap in care | |||
|---|---|---|---|---|
| Barriers | Facilitators | Barriers | Facilitators | |
| Personal | 72% | 89% | 68% | 84% |
| Structural | 13% | 11% | 48% | 13% |
Discussion
To characterize the barriers and facilitators of prompt enrolment into HIV care and continued engagement in clinical care among HIV-infected individuals who eventually enrolled in and/or re-initiated HIV care, semi-structured interviews were conducted with a sample of patients presently enrolled in clinical care but who had experienced either a delay in entering or a subsequent gap in HIV care. In open-ended spontaneous responses to questions regarding barriers and facilitators for experienced delays and/or gaps, coded patient responses revealed some common barriers and common facilitators, but also had substantial variability. Patterns that emerged suggested that denial of HIV status and active avoidance were pertinent deterrents to prompt entry into care as well as subsequent gaps in care of greater than 6 months.
Reasons reflective of denial or avoidance included self-expressed denial, disbelief, and lack of acceptance of the potential for poor health in the future. The extent of reporting of denial-based barriers was high in this Deep South sample (74% with at least 1 of these reasons for delaying entry into care), especially as the literature has primarily reported structural barriers. While “difficulty accepting the diagnosis” has been found as a reason to delay entering care in other studies, this study showed an exceptionally high percentage of individuals reporting this barrier, which could be speculated to be a result of the environment of the rural Deep South. This environment is one where HIV is highly stigmatized and where few resources for support or assistance exist, and where the primary social support structure in the community, the church, is not generally supportive.
Further, when main reasons for delays and gaps were considered in terms of their personal or structural nature related to the HIV-care system or access, results suggested that these barriers to engagement in care were predominantly personal. More specifically, where delays (barriers and facilitators) and gaps (facilitators) were clearly dominated by reasons reflecting personal experiences and reactions, reasons for a gap in care were more balanced between personal and structural causes. Thus, for patients who had successfully navigated their way back into care, personal facilitators appeared to be critical to engagement and re-engagement, but structural factors influencing on-going HIV care were also important to consider as possible factors influencing “dropping out” of care.
HIV continues to be highly stigmatized in the Deep South, thus we anticipated a higher frequency of privacy concerns within this sample of patients from a Deep South clinic. However, an important qualification to this and other findings is that our sample consisted of PLWH who had, at time of interview, successfully negotiated entry and re-entry into care and thus barriers and facilitators identified by this group may have differed from those never in care. The possibility that privacy could be a strong barrier for those individuals who had never entered clinical care at all should be explored in future research.
Limitations of the present research included possible influences from conducting the interview in the clinical care setting: Participants may have restrained themselves from describing clinic-based barriers. Because interviewers were not the care providers and provided detailed assurances of anonymity, privacy, and confidentiality of data collected, self-presentation bias was not likely to have highly influenced the data. In addition, these data were collected in only one clinic, which limits its generalizability.
The retrospective nature of the interviews, which asked participants to report on events that may have occurred over 5 years ago, limited results to what individuals perceived and recalled as main barriers and facilitators. Prospective studies capturing barriers and facilitators and then assessing the relation between these and subsequent enrollment in care or gaps in care are needed.
In terms of the coding system used, between 11% and 12% of the sample provided responses that interviewers could not place into a single category. Interviewers coded “on the fly” thus in-vivo reliability checks were not possible. Role-plays conducted throughout the data collection period were used to train and check reliability of code assignments. In these exercises coders continued to show some variability in applying the codes, although group discussions quickly led to consensus.
The response rate of 62% may have influenced the results, as the group of individuals who did not agree to speak with a researcher may have been qualitatively different from the group that did agree. Those not agreeing to speak with a researcher may have been influenced by distrust or concern about privacy, and these individuals may have reflected a greater proportion with delayed access to care and/or gaps in care. These individuals may have reported different barriers than those reported by respondents, which may have focused more on problems with the clinical care setting and less on personal barriers.
While barriers and facilitators for the group of patients included in this research may be distinct from those reported by PLWH who remain lost to care, assessing perceived determinants of engagement in clinical care among active clinic patients is relevant in characterizing populations that may benefit from retention interventions positioned within clinical care. This patient group can effectively speak to the facilitators that promoted their eventual entry and re-entry into care. Thus, they can provide unique insights into overcoming certain barriers successfully.
The results of this study suggest that denial and avoidance may be a major factor in delayed entry into HIV clinical care, and interventions that can effectively address denial are important in both entry and ongoing engagement in HIV care. While access to HIV care has been explored in terms of environmental and patient characteristics, considering enabling and hindering factors as “personal” (associated with one’s internal beliefs about HIV care, its utility, and its meaning in her/his life) and “structural” (the interaction between the patient and his/her resources and the system of care) may offer unique perspectives into how individual-level behavior change may be effective in promoting sustained engagement in one’s care. Our results suggest that multiple personal and psychological factors may be influential in engagement in HIV care that could be addressed at a personal level, at least from patients’ perspectives. Frequent assessment of potential barriers and facilitators to maintaining HIV clinical care could help clinic staff provide tailored interventions prior to the disruption of continuity of care. Our study suggests that a greater understanding and recognition of the importance of these personal barriers and facilitators, in addition to structural barriers, may inform policymakers and providers working on addressing the issues of loss to care.
Acknowledgement
This research was supported by Award Number K23NR09186 from the National Institute of Nursing Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors report no real or perceived vested interests that relate to this article (including relationships with pharmaceutical companies, biomedical device manufacturers, grantors, or other entities whose products or services are related to topics covered in this manuscript) that could be construed as a conflict of interest.
Contributor Information
Deborah J. Konkle-Parker, Division of Infectious Diseases, University of Mississippi Medical Center, Jackson, MS.
K. Rivet Amico, Department of Psychology, CHIP, University of Connecticut, Storrs, CT.
Harold M. Henderson, Division of Infectious Diseases, University of Mississippi Medical Center, Jackson, MS.
References
- Centers for Disease Control and Prevention. AIDS Cases by state and metropolitan area provided for the Ryan White CARE Act. HIV/AIDS Surveillance Supplemental Report. 2005 June;11(1) Retrieved from http://www.cdc.gov/hiv/stats/HASRSuppVol11No1.pdf.
- Copello G. Fighting HIV/AIDS in the Southern United States. 2004 Retrieved from www.theaidsinstitute.org/downloads/fightaidsouth.doc.
- Division of HIV/AIDS Prevention. Medical Monitoring Project (MMP) 2008 June 28; Retrieved from http://www.cdc.gov/hiv/topics/treatment/mmp/index.htm.
- Fowler-Brown A, Ashkin E, Corbie-Smith G, Thaker S, Pathman DE. Perception of racial barriers to health care in the rural South. Journal of Health Care for the Poor and Underserved. 2006;17(1):86–100. doi: 10.1353/hpu.2006.0022. doi:10.1353/hpu.2006.0022. [DOI] [PubMed] [Google Scholar]
- Giordano T, Clark A, Stapleton S, Soriano E, Hwang L. Facilitators and barriers to remaining in HIV-care among recently diagnosed patients; Paper presented at the 29th Annual Meeting and Scientific Sessions of the Society of Behavioral Medicine; San Diego, CA. 2008. Mar 26–29, [Google Scholar]
- Giordano TP, Gifford AL, White AC, Jr, Suarez-Almazor ME, Rabeneck L, Hartman C, Morgan RO. Retention in care: A challenge to survival with HIV infection. Clinical Infectious Diseases. 2007;44(11):1493–1499. doi: 10.1086/516778. doi:10.1086/516778. [DOI] [PubMed] [Google Scholar]
- Heckman TG, Somlai AM, Peters J, Walker J, Otto-Salaj L, Galdabini CA, Kelly JA. Barriers to care among persons living with HIV/AIDS in urban and rural areas. AIDS Care. 1998;10(3):365–375. doi: 10.1080/713612410. doi:10.1080/713612410. [DOI] [PubMed] [Google Scholar]
- Kalichman SC, Catz S, Ramachandran B. Barriers to HIV/AIDS treatment and treatment adherence among African-American adults with disadvantaged education. Journal of the National Medical Association. 1999;91(8):439–446. [PMC free article] [PubMed] [Google Scholar]
- Konkle-Parker DJ, Erlen JA, Dubbert PM. Barriers and facilitators to medication adherence in a Southern minority population with HIV disease. Journal of the Association of Nurses in AIDS Care. 2008;19(2):98–104. doi: 10.1016/j.jana.2007.09.005. doi:10.1016/j.jana.2007.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krawczyk CS, Funkhouser E, Kilby JM, Kaslow RA, Bey AK, Vermund SH. Factors associated with delayed initiation of HIV medical care among infected persons attending a southern HIV/AIDS clinic. Southern Medical Journal. 2006;99(5):472–481. doi: 10.1097/01.smj.0000215639.59563.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krawczyk CS, Funkhouser E, Kilby JM, Vermund SH. Delayed access to HIV diagnosis and care: Special concerns for the Southern United States. AIDS Care. 2006;18 Suppl 1:S35–S44. doi: 10.1080/09540120600839280. doi:10.1080/09540120600839280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lanoy E, Mary-Krause M, Tattevin P, Perbost I, Poizot-Martin I, Dupont C, Costagliola D. Frequency, determinants and consequences of delayed access to care for HIV infection in France. Antiviral Therapy. 2007;12(1):89–96. doi: 10.1177/135965350701200111. [DOI] [PubMed] [Google Scholar]
- Mugavero M, Ostermann J, Whetten K, Leserman J, Swartz M, Stangl D, Thielman N. Barriers to antiretroviral adherence: The importance of depression, abuse, and other traumatic events. AIDS Patient Care & STDs. 2006;20(6):418–428. doi: 10.1089/apc.2006.20.418. doi:10.1089/apc.2006.20.418. [DOI] [PubMed] [Google Scholar]
- Napravnik S, Eron JJ, Jr, McKaig RG, Heine AD, Menezes P, Quinlivan E. Factors associated with fewer visits for HIV primary care at a tertiary care center in the Southeastern U.S. AIDS Care. 2006;18 Suppl 1:S45–S50. doi: 10.1080/09540120600838928. doi:10.1080/09540120600838928. [DOI] [PubMed] [Google Scholar]
- Panel on Antiretroviral Guidelines for Adults and Adolescents. Guidelines for the use of antiretroviral agents for HIV-infected adults and adolescents. 2008 January 29; Retrieved from http://www.aidsinfo.nih.gov/ContentFiles/AdultandAdolescentGL.pdf.
- Parsons SK, Cruise PL, Davenport WM, Jones V. Religious beliefs, practices and treatment adherence among individuals with HIV in the southern United States. AIDS Patient Care & STDs. 2006;20(2):97–111. doi: 10.1089/apc.2006.20.97. doi:10.1089/apc.2006.20.97. [DOI] [PubMed] [Google Scholar]
- Pathman DE, Fowler-Brown A, Corbie-Smith G. Differences in access to outpatient medical care for Black and White adults in the rural South. Medical Care. 2006;44(5):429–438. doi: 10.1097/01.mlr.0000207487.85689.a8. doi:10.1097/01.mlr.0000207487.85689.a8. [DOI] [PubMed] [Google Scholar]
- Qian H-Z, Taylor RD, Fawal HJ, Vermund SH. Increasing AIDS case reports in the South: U.S. trends from 1981–2004. AIDS Care. 2006;18 Suppl 1:S6–S9. doi: 10.1080/09540120600839074. doi:10.1080/09540120600839074. [DOI] [PubMed] [Google Scholar]
- Rajabiun S, Mallinson RK, McCoy K, Coleman S, Drainoni ML, Rebholz C, Holbert T. "Getting me back on track": The role of outreach interventions in engaging and retaining people living with HIV/AIDS in medical care. AIDS Patient Care & STDs. 2007;21 Suppl 1:S20–S29. doi: 10.1089/apc.2007.9990. doi:10.1089/apc.2007.9990. [DOI] [PubMed] [Google Scholar]
- Reif S, Geonnotti KL, Whetten K. HIV infection and AIDS in the Deep South. American Journal of Public Health. 2006;96(6):970–973. doi: 10.2105/AJPH.2005.063149. doi:10.2105/AJPH.2005.063149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rumptz MH, Tobias C, Rajabiun S, Bradford J, Cabral H, Young R, Cunningham WE. Factors associated with engaging socially marginalized HIV-positive persons in primary care. AIDS Patient Care and STDs. 2007;21 Suppl 1:S30–S39. doi: 10.1089/apc.2007.9989. doi:10.1089/apc.2007.9989. [DOI] [PubMed] [Google Scholar]
- Whetten K, Reif S. Overview: HIV/AIDS in the deep south region of the United States. AIDS Care. 2006;18 Suppl 1:S1–S5. doi: 10.1080/09540120600838480. doi:10.1080/09540120600838480. [DOI] [PubMed] [Google Scholar]