Abstract
Introduction
Exercise improves functional outcome and symptoms for certain cancer populations, but the feasibility, efficacy, and safety of structured exercise in patients with lung cancer is unknown. In this study, we examined the feasibility of a hospital-based exercise program for patients with advanced non-small cell lung cancer.
Methods
This study included patients with newly diagnosed advanced stage non-small cell lung cancer and Eastern Cooperative Oncology Group performance status 0–1. A physical therapist facilitated twice-weekly sessions of aerobic exercise and weight training over an 8-week period. The primary end point was feasibility of the intervention, defined as adherence to the exercise program. Secondary endpoints included functional capacity, measured by the 6-minute walk test and muscle strength, as well as quality of life, lung cancer symptoms and fatigue, measured by the Functional Assessment of Cancer Therapy-lung and Functional Assessment of Cancer Therapy-fatigue scales.
Results
Between October 2004 and August 2007, 25 patients enrolled in the study. All participants received anticancer therapy during the study period. Twenty patients (80%) underwent the baseline physical therapy evaluation. Eleven patients (44%) completed all 16 sessions. An additional 6 patients attended at least 6 sessions (range, 6–15), and 2 patients only attended one session. Study completers experienced a significant reduction in lung cancer symptoms and no deterioration in their 6-minute walk test or muscle strength.
Conclusions
Although the majority of participants attempted the exercise program, less than half were able to complete the intervention. Those who completed the program experienced an improvement in their lung cancer symptoms. Community-based or briefer exercise interventions may be more feasible in this population.
Keywords: Non-small cell lung cancer, Exercise, Supportive care
Exercise plays an important role in both primary and secondary prevention of cancer and may impact the health and functioning of patients with a current cancer diagnosis.1–6 Some of the more debilitating symptoms patients with cancer experience, including fatigue, cachexia, depression, and anxiety, may be ameliorated with exercise.7–10 Both healthy and medically ill patients consistently report quality of life (QOL) improvements with exercise.11–13 The benefits of exercise for individuals with cancer have been described in a number of patient populations.14–21 However, the majority of studies have been performed in patients with breast cancer and in patients undergoing stem cell transplantation.9,10,17,18,22–29 Although these studies have been informative regarding the potential benefits of exercise in patients receiving anticancer therapy, the extent to which these benefits are achievable in other cancer populations, such as those with advanced disease, remains unknown.
Patients with metastatic, incurable solid tumors tend to report the greatest symptom burden compared with other cancer patient populations.30–33 For example, the majority of patients with metastatic lung cancer experience clinically significant fatigue and cachexia.34–38 Similarly, the prevalence of psychologic distress, including depression and anxiety symptoms, is highest among patients with cancers that have poorer prognoses, such as lung and pancreatic malignancies.39 Unfortunately, the results of pharmacotherapy trials for treating cancer-related fatigue and anorexia/cachexia have been disappointing to date.40–45
Targeted nonpharmacological interventions, such as exercise, may serve as useful alternatives for managing cancer-related symptoms in patients with advanced malignancies. Other types of behavioral interventions, such as cognitive behavioral therapy, multidisciplinary symptom management, and other integrative/complementary therapies have been shown to be useful for managing cancer-related symptoms.21,46–49 Exercise is an appealing strategy based on its universal health benefits, potential for mitigating declines in functional status, and its availability to all patients. However, the feasibility of an exercise program for patients with metastatic solid tumors, many of whom are older with comorbid disease, has yet to be established. The few published studies of exercise interventions with mixed cancer populations have generally included patients with both early and late stage disease.50–52
The goal of this study was to assess the feasibility of a structured exercise program for patients with newly diagnosed advanced non-small cell lung cancer (NSCLC). In light of the advanced age and frequency of comorbid conditions in this patient population, we designed a hospital-based, supervised exercise program to allow close monitoring and observation.
PATIENTS AND METHODS
Patient Selection
Patients within 12 weeks of diagnosis of advanced NSCLC (stage IIIB with pleural or pericardial effusions or stage IV) confirmed by histology or cytology were eligible for this study. Other eligibility requirements included the ability to ambulate for 6 minutes, an Eastern Cooperative Oncology Group performance status of 0–1, and the ability to read and respond to questions in English. Patients were excluded from the study if they had unstable cardiac disease (including congestive heart failure, unstable ischemia, or arrhythmia), baseline anemia (Hemoglobin <10 g/dl), or untreated bone or brain metastases that prevented participation. Thoracic oncology clinicians referred eligible patients receiving primary oncology care at Massachusetts General Hospital to the study. The study was reviewed and approved by the Harvard Cancer Center Institutional Review Board. All subjects provided written informed consent.
Assessment of Functional Capacity and Muscle Strength
At baseline, subjects underwent an evaluation with a senior physical therapist who was also responsible for facilitating the structured exercise program. Vital signs were monitored throughout the initial evaluation and any significant changes in heart rate or blood pressure were reported to the patient’s oncologist. Screening for abnormal cardiovascular and pulmonary response to exercise was assessed using a symptom limited, submaximal Modified Bruce treadmill test. By definition, this test may progress to 85% of a participant’s age predicted maximal heart rate (computed by 208 − [0.7 × age]).53 Results of the Modified Bruce treadmill test, including cardiac rhythm measurements, were sent to the oncologist for review.
The baseline evaluation included assessments of exercise response, functional exercise capacity, and muscle strength. Functional exercise capacity was measured with the 6-minute walk test (6MWT), which is a commonly used measurement of functional/exercise capacity in patients with pulmonary morbidity.54,55 The 6MWT is the distance in meters a patient can quickly ambulate on a flat, hard surface in 6 minutes. Finally, the strength of major muscle groups associated with performing activities of daily living, including both the upper extremity (shoulder flexion, elbow flexion, elbow extension) and lower extremity (hip extension, hip abduction, knee extension), was measured by the maximal amount of weight that each muscle group can move through the available range of motion (1 repetition maximum [1RM]).56 All initial visit data were analyzed and interpreted to prescribe individualized exercise rehabilitation programs.
Structured Exercise Program
The 16-session exercise program was initiated the week following the baseline evaluation. Sessions occurred twice weekly over the course of 2 months. However, participants were allowed to make up sessions missed due to illness as long as the entire exercise program was completed within a 12-week period.
The structured exercise sessions took place in group format (8–10 patients), each lasting approximately 90 to 120 minutes. Vital signs were assessed before each session. During a 10-minute warm-up period, participants performed range of motion and stretching exercises for the trunk and extremities. Participants then completed 30 minutes of aerobic exercise including 15 minutes on the treadmill and 15 minutes on an upright bicycle. The Modified Borg Scale57 was used to monitor patient symptoms of dyspnea on exertion and perceived exertion. The goal level of intensity for the aerobic exercise was for participants to achieve a heart rate between 70 and 85% of their maximum or an exertion and perceived exertion of 13 (“somewhat hard”) for those unable to achieve their target heart rate. A cool down period of 2 to 5 minutes followed the 15 minutes on both the treadmill and the bicycle.58
For the strength training component of the exercise program, patients performed 3 sets of 10 repetitions of 6 different exercises (i.e., 3 upper extremity and 3 lower extremity movements), starting at 60% of the 1RM and increasing to 80% of the 1RM over the course of 16 sessions. These strength training exercises took approximately 30 to 40 minutes and were modified or discontinued as necessary for participants unable to complete them. During the final exercise session, both the 6MWT and the final weight lifted by the patient’s dominant arm (for 3 sets of 10 repetitions) were recorded for analysis.
Quality of Life (QOL) and Symptom Assessments
The following self-report questionnaires were administered at the baseline physical therapy (PT) evaluation and after completing the final session of the exercise-training program.
To evaluate health-related QOL and cancer-related symptoms, we used the Functional Assessment of Cancer Therapy (FACT).59 Measuring multiple dimensions of QOL during the past week, the FACT-General (FACT-G) is a 26-item questionnaire in which patients rate their physical, functional, emotional, and social well-being on a five-point Likert scale. The FACT-Lung (FACT-L) consists of the FACT-G plus a Lung Cancer Subscale (LCS) that addresses seven symptoms specific to lung cancer, including cough, shortness or breath, and chest discomfort.60 The optional question regarding satisfaction with sex life was eliminated to allow for ease of scoring. Additionally, study participants completed the 13-item fatigue scale from the FACIT-Fatigue questionnaire.61 A higher score on the total FACT or any of its components indicates better QOL. A score of 24 or less on the LCS and 30 or less on the fatigue scale is considered indicative of clinical symptoms.61–63
We also administered the Hospital Anxiety and Depression Scale (HADS), a 14-item self-report instrument designed to assess mood and anxiety symptoms in medically ill patients.64 Used widely in studies of patients with cancer, the HADS consists of two seven-item subscales assessing depression and anxiety symptoms during the past week. Each subscale ranges from 0 to 21, with a score of 8 or greater suggestive of a possible case of depression or anxiety.
Feasibility Criteria for Structured Exercise Program
The primary goal of this pilot study was to assess the feasibility of a structured exercise-training program for patients with advanced NSCLC. Patients who attended all 16 training sessions during a 12-week period were classified as meeting the adherence requirement. In pulmonary rehabilitation programs involving chronic obstructive pulmonary disease patients, reported adherence rates vary between 74 and 83%.65–67 Considering the degree of comorbid disease and poor overall health status of patients with lung cancer, we proposed an adherence rate of 70% to be an acceptable goal. Our target accrual during the 3-year study period was 30 patients.
Statistical Analysis
All analyses were conducted with SPSS 15.0. To determine adherence with the exercise program, we evaluated the level of participation of each participant. We then calculated the rate of adherent patients over the total number of patients to estimate the adherence of the entire sample.
For the secondary outcomes, we prospectively evaluated QOL (FACT-L), symptom burden (LCS; FACT-Fatigue), mood (HADS), functional capacity (6MWT), and muscle strength (RM) in the sample. Descriptive statistics were initially calculated to estimate the frequencies, means, and standard deviations of the study variables. To assess change in the outcome variables before and after participation in the exercise intervention, we conducted two-sided, paired samples t-tests. However, given the small sample size and potential violations of parametric test assumptions, we repeated the analyses and reported p-values using the Wilcoxon Signed Ranks Test. As this was a pilot feasibility study, we did not correct for multiple comparisons.
Survival time was calculated from the date of consent to the date of death using the Kaplan Meier method. Patients who were alive on the date of last follow-up were censored on that date.
RESULTS
Between October 2004 and August 2007, 25 patients were accrued to the study. The baseline characteristics of consented patients are shown in Table 1. All participants received one of the following anticancer therapies: radiation alone (8%), radiation during or followed by chemotherapy (20%), or chemotherapy alone (72%). Chemotherapy regimens included either a platinum-based doublet (19 of 25, 76%), usually with an experimental third agent or with bevacizumab (12 of 19, 63%), or a single oral agent (4 of 25, 16%). The median survival of the study cohort was 12.98 months.
TABLE 1.
Baseline Patient Characteristics
| Variable | Number (%) |
|---|---|
| Age, years | |
| Median | 68 |
| Range | 48–81 |
| Race, white | 25 (100%) |
| Sex, female | 16 (64%) |
| Performance status | |
| 0 | 10 (40%) |
| 1 | 15 (60%) |
| Cancer stage | |
| IIIB with effusions | 4 (16%) |
| IV | 21 (84%) |
| Smoking status | |
| Current/former smoker | 22 (88%) |
| Never smoker | 3 (12%) |
| Initial therapy | |
| Chemotherapy | 18 (72%) |
| Chemotherapy and radiation | 5 (20%) |
| Radiation | 2 (8%) |
Study Feasibility
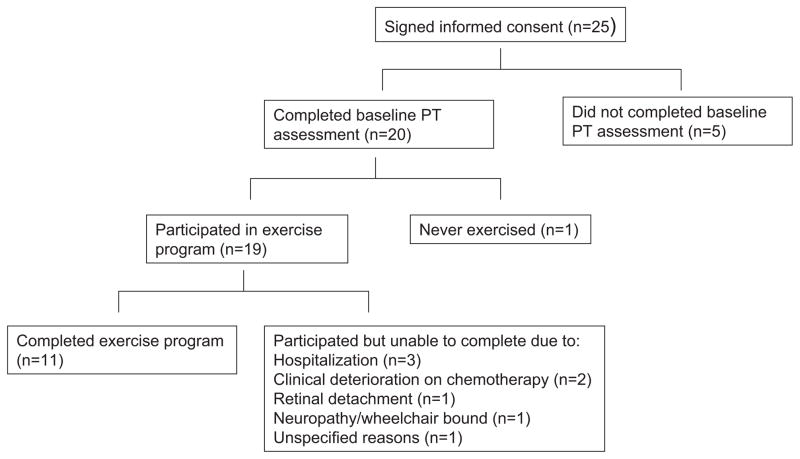
Of the 25 patients who signed informed consent, 20 (80%) completed the baseline PT evaluation (Figure 1). The remaining five patients who did not receive the initial evaluation withdrew from the study due to rapid physical decline (n = 2), feeling unwell (n = 2), or concerns about the amount of travel (n = 1).
FIGURE 1.
Patient flow.
Subsequent to the baseline PT evaluation, one patient never participated in the exercise program. Two additional patients withdrew from the study after only a single session: one for clinical deterioration on chemotherapy (sustained a fall) and the other for unspecified reasons. Of those who participated in the exercise program, 11 patients attended all 16 sessions, resulting in a completion rate of 44%. Six patients attended at least 6 sessions (range, 6–15) before withdrawing due to deterioration in their health status (Figure 1).
Quality of Life and Symptom Assessment
The results regarding QOL, cancer-related symptoms and mood are shown in Table 2 for the study participants who completed baseline and poststudy assessments (n = 11). There were no statistically significant changes in QOL, fatigue, or mood symptoms in participants from baseline to post assessment. However, lung cancer symptoms significantly improved over the course of the study, as measured by the LCS.
TABLE 2.
Mean Pre-Post Scores for QOL and Mood
| Variable (n = 11) | Base Mean (SD) | Post Mean (SD) | 95% CI of Difference |
|---|---|---|---|
| FACT-L total score | 103.44 (14.19) | 104.66 (14.51) | −8.69 to 6.24 |
| Personal well-being | 22.30 (5.48) | 21.44 (6.59) | −4.13 to 5.86 |
| Social well-being | 23.00 (3.00) | 22.09 (3.02) | −0.06 to 1.88 |
| Functional well-being | 18.45 (6.46) | 18.82 (5.40) | −4.00 to 3.27 |
| Emotional well-being | 19.45 (3.30) | 19.91 (4.35) | −2.46 to 1.55 |
| Lung cancer subscale | 20.23 (4.70) | 22.77 (3.01) | −4.94 to −0.15a |
| Trial outcome index | 60.89 (13.24) | 62.48 (12.34) | −9.32 to 6.14 |
| FACT-fatigue scale | 35.35 (12.64) | 38.77 (11.42) | −11.17 to 4.32 |
| HADS | |||
| Anxiety symptoms | 2.91 (3.02) | 2.36 (2.20) | −1.46 to 2.55 |
| Depression symptoms | 3.73 (4.29) | 4.45 (3.98) | −4.02 to 2.57 |
p < 0.05.
CI, confidence interval; FACT, Functional Assessment of Cancer Therapy; FACT-L, FACT-Lung; HADS, Hospital Anxiety and Depression Scale.
Exercise Outcomes
Table 3 details the results for the 6MWT as well as upper and lower extremity strength-training exercises. Among participants who completed baseline and poststudy assessments, the distance walked in 6 minutes increased over the study period, though this difference was not statistically significant. The maximum weight lifted also increased for all six muscle group exercises, achieving statistical significance for elbow extension. For the strength training component of the program, the final weight lifted was recorded not only at baseline and postintervention, but also at each session. Therefore, we repeated the analyses carrying the last end point forward for all patients who completed strength training as long as physically able (n = 16). These findings replicated those of the study completers shown in Table 3.
TABLE 3.
Mean Pre-Post Scores for Functional Capacity and Muscle Strength
| Variable | Base Mean (SD) | Post Mean (SD) | 95% CI of Difference |
|---|---|---|---|
| Functional capacity (n = 11) | |||
| 6 minute walk test | 410.55 (83.28) | 435.73 (72.66) | −57.25 to 6.89 |
| Muscle strength | |||
| Shoulder flexion (n = 11) | 5.50 (1.96) | 6.09 (2.66) | −1.60 to 0.42 |
| Elbow flexion (n = 11) | 11.23 (5.59) | 12.36 (6.71) | −3.00 to 0.73 |
| Elbow extension (n = 11) | 5.64 (2.77) | 6.82 (3.76) | −2.12 to −0.24a |
| Hip extension (n = 10) | 8.15 (4.90) | 9.05 (6.88) | −3.48 to 1.68 |
| Hip abduction (n = 10) | 8.20 (1.81) | 9.75 (5.64) | −4.56 to 1.46 |
| Knee extension (n = 9) | 23.11 (11.56) | 27.83 (19.43) | −12.90 to 3.45 |
p < 0.05.
CI, confidence interval.
DISCUSSION
This investigation is one of the first studies to examine the feasibility and potential benefit of a structured outpatient exercise program in a homogenous, well-defined cohort of patients with advanced cancer. Our study sample consisted of 25 patients with newly diagnosed incurable NSCLC. Because these patients experience considerable fatigue, dyspnea, and cachexia, they represent an ideal population to investigate an intervention that may alleviate symptom burden and enhance physical functioning.33 Additionally, consistent with previous investigations of individuals with advanced lung cancer, the patients in our sample tended to be older and have a history of tobacco use. Should structured exercise interventions prove feasible despite poor health status and comorbidity in patients, such programs could substantially impact symptom control and QOL.
The findings demonstrate that the majority of the sample (76%) either completed the exercise program or participated as long as physically able, despite failing to achieve the target adherence rate to establish feasibility. Many patients were unable to attend all sessions due to progressive/intervening medical complications, resulting in a final completion rate of 44%. Notably, participants did not experience any significant detriment to their QOL or exacerbation of fatigue symptoms over the study period. Those who completed the program did experience a significant improvement in their lung cancer symptoms, which is encouraging and may warrant further investigation. However, the findings should be interpreted cautiously given the single-arm nature of this study, small sample size, and use of multiple comparisons for outcome variables.
In contrast to our study of patients with newly diagnosed advanced NSCLC, previous investigators have generally explored the benefits of exercise by sampling patients with different types of cancer at variable times during the course of disease. For example, one study examined the effect of exercise in a sample of patients with mixed incurable cancers receiving palliative care.51,52 Similar to our findings, 46% of enrolled patients completed the 6-week program and experienced improvements in the 6MWT and some QOL measures. However, only 27% of patients (9 of 34) received chemotherapy during the study period. In another study, Adamsen et al. demonstrated the feasibility of a multidimensional exercise program for patients undergoing chemotherapy. Yet, their study sample also included participants with diverse malignancies, many of whom received adjuvant therapy or chemotherapy with curative intent.50,68 In the only study to evaluate the feasibility of an exercise program specifically for individuals with lung cancer, potential participants were referred for a nutrition and rehabilitation program at any point during the course of their illness.69 Of the 168 patients referred to the program, only 92 were prescribed exercise, since many patients were excluded due to pain (66%) or cardiovascular instability (17%), among other reasons. Of the patients eligible for exercise, 38 (40%) refused the intervention, and only 17 (19%) completed at least 6 sessions in a 2-month period. The paucity of data in patients with advanced lung cancer underscores the need for further research to identify effective methods for reducing symptom burden in patients with such significant morbidity.
Cancer-related fatigue may in part be the result of cachexia associated with disease progression and anticancer therapy.70 Therefore, in this novel study of patients with advanced lung cancer, we sought to examine the effect of exercise on muscle strength and level of functioning. Although one recent investigation showed that, among patients with lung cancer receiving chemotherapy, functional capacity significantly declined as measured by the 6MWT, no such decrements in functioning were seen in our study completers, despite undergoing concurrent anticancer therapy.71 Similarly, patients who participated in the exercise program maintained or improved their muscle strength on average over the course of the study. These results suggest that the physical benefits of exercise seen in other cancer populations also apply to lung cancer patients.
Our study has a number of important strengths. First, we included a well-defined homogenous population of patients with a new diagnosis of advanced NSCLC. Second, due to overlapping symptoms and comorbid disease in patients with lung cancer and chronic obstructive pulmonary disease, the study intervention consisted of a pulmonary rehabilitation exercise program. Additionally, the structured program was supervised, which, in contrast to home-based programs, ensured not only the safety of medically ill participants but also the accuracy and reliability of adherence rates. Finally, our intervention included both aerobic and strength training components, optimizing the potential for maintaining and enhancing physical performance.7,15
Several limitations of the study also deserve mention. Because this was a small, pilot investigation, we did not collect data on the total number of patients seen in the clinic who met eligibility criteria as well as those who were offered but deferred study participation. Although these data are lacking, the average age and overall survival of our participants are fairly consistent with previous estimates for patients with metastatic lung cancer.72 Additionally, although the data suggest a clinical benefit from exercise with improvement in lung cancer symptoms and muscle strength, these findings will need to be confirmed with a randomized study. Finally, as a single institution study performed at a tertiary care center, the findings may not generalize to patients with advanced cancer seeking oncology care in the community. Because the study took place in an academic medical center, many patients were simultaneously enrolled in clinical trials for anticancer therapy, which may have influenced patients’ willingness to participate in additional trials, including the present study.
Accrual to the study was slow, and we failed to meet our goal of 30 patients. We did not collect data on why patients who were offered the study opted not to participate. Certainly, the challenges of facing a new lung cancer diagnosis and the accompanying symptoms and psychologic distress may have impacted patients’ willingness and ability to participate in an exercise study. Anecdotally, clinic physicians and nurse practitioners also commented that patients deferred study participation because of concerns about commuting to the hospital twice weekly. Therefore, offering the exercise program within the community may have increased enrollment. In addition, our exercise program was quite intensive and rigorous, requiring twice weekly visits for up to 2 hours. Although we modeled our program after pulmonary rehabilitation programs for patients with chronic obstructive pulmonary disease, twice weekly visits during anticancer therapy may not be feasible for most patients with advanced cancer.66,73,74 Modifying the exercise program to be less frequent, less intensive, or perhaps home-based may be more acceptable and reasonable for patients with metastatic NSCLC. Lastly, we chose to limit the study sample to those with advanced disease given the degree of morbidity and potential benefit from the intervention. However, as demonstrated in populations with breast cancer, exercise programs may also be useful for patients with earlier stages of lung cancer, such as those receiving adjuvant chemotherapy.23
Findings from the present study suggest that a structured, supervised exercise program may improve symptom burden and functional capacity in patients with advanced NSCLC. However, given the slow accrual and somewhat low completion rates, a less intensive, more accessible program may be more feasible. Although a supervised program is still preferable for those with comorbid disease and poor health status, a weekly, community-based program would likely be more acceptable to patients. Future research in this area would also benefit from a multi-institutional study, as many obstacles limit the accrual of patients with advanced cancer to supportive care trials. Despite these challenges, preliminary findings from the present investigation provide encouraging evidence supporting the feasibility and benefit of structured exercise in patients with advanced NSCLC receiving anticancer therapy.
Acknowledgments
Supported by 5RO3CA110779 and the Mary Ellen and Dick Denning Foundation, and NIH K24 Mid-career Investigator Award (5K24CA121990) (to M.R.S.).
Footnotes
Disclosure: The authors declare no conflicts of interest.
References
- 1.Holmes MD, Chen WY, Feskanich D, et al. Physical activity and survival after breast cancer diagnosis. JAMA. 2005;293:2479–2486. doi: 10.1001/jama.293.20.2479. [DOI] [PubMed] [Google Scholar]
- 2.Meyerhardt JA, Giovannucci EL, Holmes MD, et al. Physical activity and survival after colorectal cancer diagnosis. J Clin Oncol. 2006;24:3527–3534. doi: 10.1200/JCO.2006.06.0855. [see comment] [DOI] [PubMed] [Google Scholar]
- 3.Meyerhardt JA, Heseltine D, Niedzwiecki D, et al. Impact of physical activity on cancer recurrence and survival in patients with stage III colon cancer: findings from CALGB 89803. J Clin Oncol. 2006;24:3535–3541. doi: 10.1200/JCO.2006.06.0863. [see comment] [DOI] [PubMed] [Google Scholar]
- 4.Giovannucci E, Ascherio A, Rimm EB, Colditz GA, Stampfer MJ, Willett WC. Physical activity, obesity, and risk for colon cancer and adenoma in men. Ann Intern Med. 1995;122:327–334. doi: 10.7326/0003-4819-122-5-199503010-00002. [DOI] [PubMed] [Google Scholar]
- 5.Thune I, Brenn T, Lund E, Gaard M. Physical activity and the risk of breast cancer. N Engl J Med. 1997;336:1269–1275. doi: 10.1056/NEJM199705013361801. [see comment] [DOI] [PubMed] [Google Scholar]
- 6.McTiernan A, Kooperberg C, White E, et al. Recreational physical activity and the risk of breast cancer in postmenopausal women: the Women’s Health Initiative Cohort Study. JAMA. 2003;290:1331–1336. doi: 10.1001/jama.290.10.1331. [see comment] [DOI] [PubMed] [Google Scholar]
- 7.Galvao DA, Newton RU. Review of exercise intervention studies in cancer patients. J Clin Oncol. 2005;23:899–909. doi: 10.1200/JCO.2005.06.085. [DOI] [PubMed] [Google Scholar]
- 8.Cramp F, Daniel J. Exercise for the management of cancer-related fatigue in adults. Cochrane Database Syst Rev. 2008:CD006145. doi: 10.1002/14651858.CD006145.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Courneya KS, Keats MR, Turner AR. Physical exercise and quality of life in cancer patients following high dose chemotherapy and autologous bone marrow transplantation. Psychooncology. 2000;9:127–136. doi: 10.1002/(sici)1099-1611(200003/04)9:2<127::aid-pon438>3.0.co;2-l. [DOI] [PubMed] [Google Scholar]
- 10.Dimeo FC, Stieglitz RD, Novelli-Fischer U, Fetscher S, Keul J. Effects of physical activity on the fatigue and psychologic status of cancer patients during chemotherapy. Cancer. 1999;85:2273–2277. [PubMed] [Google Scholar]
- 11.Hung C, Daub B, Black B, Welsh R, Quinney A, Haykowsky M. Exercise training improves overall physical fitness and quality of life in older women with coronary artery disease. Chest. 2004;126:1026–1031. doi: 10.1378/chest.126.4.1026. [see comment] [DOI] [PubMed] [Google Scholar]
- 12.Belardinelli R, Georgiou D, Cianci G, Purcaro A. Randomized, controlled trial of long-term moderate exercise training in chronic heart failure: effects on functional capacity, quality of life, and clinical outcome. Circulation. 1999;99:1173–1182. doi: 10.1161/01.cir.99.9.1173. [see comment] [DOI] [PubMed] [Google Scholar]
- 13.Brach JS, FitzGerald S, Newman AB, et al. Physical activity and functional status in community-dwelling older women: a 14-year prospective study. Arch Intern Med. 2003;163:2565–2571. doi: 10.1001/archinte.163.21.2565. [DOI] [PubMed] [Google Scholar]
- 14.Courneya KS, Friedenreich CM, Quinney HA, et al. A randomized trial of exercise and quality of life in colorectal cancer survivors. Eur J Cancer Care. 2003;12:347–357. doi: 10.1046/j.1365-2354.2003.00437.x. [DOI] [PubMed] [Google Scholar]
- 15.Schneider CM, Hsieh CC, Sprod LK, Carter SD, Hayward R. Cancer treatment-induced alterations in muscular fitness and quality of life: the role of exercise training. Ann Oncol. 2007;18:1957–1962. doi: 10.1093/annonc/mdm364. [DOI] [PubMed] [Google Scholar]
- 16.Segal RJ, Reid RD, Courneya KS, et al. Resistance exercise in men receiving androgen deprivation therapy for prostate cancer. [comment] J Clin Oncol. 2003;21:1653–1659. doi: 10.1200/JCO.2003.09.534. [DOI] [PubMed] [Google Scholar]
- 17.Dimeo F, Fetscher S, Lange W, Mertelsmann R, Keul J. Effects of aerobic exercise on the physical performance and incidence of treatment-related complications after high-dose chemotherapy. Blood. 1997;90:3390–3394. [PubMed] [Google Scholar]
- 18.Daley AJ, Crank H, Saxton JM, Mutrie N, Coleman R, Roalfe A. Randomized trial of exercise therapy in women treated for breast cancer. J Clin Oncol. 2007;25:1713–1721. doi: 10.1200/JCO.2006.09.5083. [DOI] [PubMed] [Google Scholar]
- 19.Jacobsen PB, Donovan KA, Vadaparampil ST, Small BJ. Systematic review and meta-analysis of psychological and activity-based interventions for cancer-related fatigue. Health Psychol. 2007;26:660–667. doi: 10.1037/0278-6133.26.6.660. [erratum appears in Health Psychol 2008;27:42] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Knols R, Aaronson NK, Uebelhart D, Fransen J, Aufdemkampe G. Physical exercise in cancer patients during and after medical treatment: a systematic review of randomized and controlled clinical trials. J Clin Oncol. 2005;23:3830–3842. doi: 10.1200/JCO.2005.02.148. [DOI] [PubMed] [Google Scholar]
- 21.Mustian KM, Morrow GR, Carroll JK, Figueroa-Moseley CD, Jean-Pierre P, Williams GC. Integrative nonpharmacologic behavioral interventions for the management of cancer-related fatigue. Oncologist. 2007;12 (Suppl 1):52–67. doi: 10.1634/theoncologist.12-S1-52. [DOI] [PubMed] [Google Scholar]
- 22.Mutrie N, Campbell AM, Whyte F, et al. Benefits of supervised group exercise programme for women being treated for early stage breast cancer: pragmatic randomised controlled trial. BMJ. 2007;334:517. doi: 10.1136/bmj.39094.648553.AE. [see comment] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Courneya KS, Segal RJ, Mackey JR, et al. Effects of aerobic and resistance exercise in breast cancer patients receiving adjuvant chemotherapy: a multicenter randomized controlled trial. J Clin Oncol. 2007;25:4396–4404. doi: 10.1200/JCO.2006.08.2024. [see comment] [DOI] [PubMed] [Google Scholar]
- 24.Pinto BM, Frierson GM, Rabin C, Trunzo JJ, Marcus BH. Home-based physical activity intervention for breast cancer patients. J Clin Oncol. 2005;23:3577–3587. doi: 10.1200/JCO.2005.03.080. [see comment] [DOI] [PubMed] [Google Scholar]
- 25.Schneider CM, Hsieh CC, Sprod LK, Carter SD, Hayward R. Effects of supervised exercise training on cardiopulmonary function and fatigue in breast cancer survivors during and after treatment. Cancer. 2007;110:918–925. doi: 10.1002/cncr.22862. [DOI] [PubMed] [Google Scholar]
- 26.Courneya KS, Mackey JR, Bell GJ, Jones LW, Field CJ, Fairey AS. Randomized controlled trial of exercise training in postmenopausal breast cancer survivors: cardiopulmonary and quality of life outcomes. J Clin Oncol. 2003;21:1660–1668. doi: 10.1200/JCO.2003.04.093. [comment] [DOI] [PubMed] [Google Scholar]
- 27.Segal R, Evans W, Johnson D, et al. Structured exercise improves physical functioning in women with stages I and II breast cancer: results of a randomized controlled trial. J Clin Oncol. 2001;19:657–665. doi: 10.1200/JCO.2001.19.3.657. [DOI] [PubMed] [Google Scholar]
- 28.Dimeo F, Rumberger BG, Keul J. Aerobic exercise as therapy for cancer fatigue. Med Sci Sports Exerc. 1998;30:475–478. doi: 10.1097/00005768-199804000-00001. [DOI] [PubMed] [Google Scholar]
- 29.Dimeo FC, Tilmann MH, Bertz H, Kanz L, Mertelsmann R, Keul J. Aerobic exercise in the rehabilitation of cancer patients after high dose chemotherapy and autologous peripheral stem cell transplantation. Cancer. 1997;79:1717–1722. [PubMed] [Google Scholar]
- 30.Vainio A, Auvinen A. Prevalence of symptoms among patients with advanced cancer: an international collaborative study. Symptom Prevalence Group. J Pain Symptom Manage. 1996;12:3–10. doi: 10.1016/0885-3924(96)00042-5. [DOI] [PubMed] [Google Scholar]
- 31.Temel JS, Pirl WF, Lynch TJ. Comprehensive symptom management in patients with advanced-stage non-small-cell lung cancer. Clin Lung Cancer. 2006;7:241–249. doi: 10.3816/CLC.2006.n.001. [DOI] [PubMed] [Google Scholar]
- 32.Degner LF, Sloan JA. Symptom distress in newly diagnosed ambulatory cancer patients and as a predictor of survival in lung cancer. J Pain Symptom Manage. 1995;10:423–431. doi: 10.1016/0885-3924(95)00056-5. [DOI] [PubMed] [Google Scholar]
- 33.Hopwood P, Stephens RJ. Symptoms at presentation for treatment in patients with lung cancer: implications for the evaluation of palliative treatment. The Medical Research Council (MRC) Lung Cancer Working Party. Br J Cancer. 1995;71:633–636. doi: 10.1038/bjc.1995.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Temel JS, Jackson VA, Billings JA, et al. Phase II study: integrated palliative care in newly diagnosed advanced non-small-cell lung cancer patients. J Clin Oncol. 2007;25:2377–2382. doi: 10.1200/JCO.2006.09.2627. [DOI] [PubMed] [Google Scholar]
- 35.Ross PJ, Ashley S, Norton A, et al. Do patients with weight loss have a worse outcome when undergoing chemotherapy for lung cancers? Br J Cancer. 2004;90:1905–1911. doi: 10.1038/sj.bjc.6601781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cooley ME, Short TH, Moriarty HJ. Symptom prevalence, distress, and change over time in adults receiving treatment for lung cancer. Psychooncology. 2003;12:694–708. doi: 10.1002/pon.694. [DOI] [PubMed] [Google Scholar]
- 37.Okuyama T, Tanaka K, Akechi T, et al. Fatigue in ambulatory patients with advanced lung cancer: prevalence, correlated factors, and screening. J Pain Symptom Manage. 2001;22:554–564. doi: 10.1016/s0885-3924(01)00305-0. [DOI] [PubMed] [Google Scholar]
- 38.Tanaka K, Akechi T, Okuyama T, Nishiwaki Y, Uchitomi Y. Impact of dyspnea, pain, and fatigue on daily life activities in ambulatory patients with advanced lung cancer. J Pain Symptom Manage. 2002;23:417–423. doi: 10.1016/s0885-3924(02)00376-7. [DOI] [PubMed] [Google Scholar]
- 39.Zabora J, BrintzenhofeSzoc K, Curbow B, Hooker C, Piantadosi S. The prevalence of psychological distress by cancer site. Psychooncology. 2001;10:19–28. doi: 10.1002/1099-1611(200101/02)10:1<19::aid-pon501>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 40.Bruera E, El Osta B, Valero V, et al. Donepezil for cancer-related fatigue: a double-blind, randomized, placebo-controlled study. American Society of Clinical Oncology; Chicago, IL: 2007. [DOI] [PubMed] [Google Scholar]
- 41.Bruera E, Valero V, Driver L, et al. Patient-controlled methylphenidate for cancer fatigue: a double-blind, randomized, placebo-controlled trial. J Clin Oncol. 2006;24:2073–2078. doi: 10.1200/JCO.2005.02.8506. [DOI] [PubMed] [Google Scholar]
- 42.Loprinzi CL, Schaid DJ, Dose AM, Burnham NL, Jensen MD. Body-composition changes in patients who gain weight while receiving megestrol acetate. J Clin Oncol. 1993;11:152–154. doi: 10.1200/JCO.1993.11.1.152. [DOI] [PubMed] [Google Scholar]
- 43.Loprinzi CL, Michalak JC, Schaid DJ, et al. Phase III evaluation of four doses of megestrol acetate as therapy for patients with cancer anorexia and/or cachexia. J Clin Oncol. 1993;11:762–767. doi: 10.1200/JCO.1993.11.4.762. [DOI] [PubMed] [Google Scholar]
- 44.Jatoi A, Rowland K, Loprinzi CL, et al. An eicosapentaenoic acid supplement versus megestrol acetate versus both for patients with cancer-associated wasting: a North Central Cancer Treatment Group and National Cancer Institute of Canada collaborative effort. J Clin Oncol. 2004;22:2469–2476. doi: 10.1200/JCO.2004.06.024. [DOI] [PubMed] [Google Scholar]
- 45.Jatoi A, Windschitl HE, Loprinzi CL, et al. Dronabinol versus megestrol acetate versus combination therapy for cancer-associated anorexia: a North Central Cancer Treatment Group study. J Clin Oncol. 2002;20:567–573. doi: 10.1200/JCO.2002.20.2.567. [DOI] [PubMed] [Google Scholar]
- 46.Cassileth BR, Deng GE, Gomez JE, et al. Complementary therapies and integrative oncology in lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition) Chest. 2007;132:340S–354S. doi: 10.1378/chest.07-1389. [DOI] [PubMed] [Google Scholar]
- 47.Gielissen MF, Verhagen S, Witjes F, Bleijenberg G. Effects of cognitive behavior therapy in severely fatigued disease-free cancer patients compared with patients waiting for cognitive behavior therapy: a randomized controlled trial. J Clin Oncol. 2006;24:4882–4887. doi: 10.1200/JCO.2006.06.8270. [DOI] [PubMed] [Google Scholar]
- 48.Given C, Given B, Rahbar M, et al. Effect of a cognitive behavioral intervention on reducing symptom severity during chemotherapy. J Clin Oncol. 2004;22:507–516. doi: 10.1200/JCO.2004.01.241. [DOI] [PubMed] [Google Scholar]
- 49.Rummans TA, Clark MM, Sloan JA, et al. Impacting quality of life for patients with advanced cancer with a structured multidisciplinary intervention: a randomized controlled trial. J Clin Oncol. 2006;24:635–642. doi: 10.1200/JCO.2006.06.209. [DOI] [PubMed] [Google Scholar]
- 50.Adamsen L, Midtgaard J, Rorth M, et al. Feasibilty, physical capacity, and health benefits of a multidimensional exercise program for cancer patients undergoing chemotherapy. Support Care Cancer. 2003;11:707–716. doi: 10.1007/s00520-003-0504-2. [DOI] [PubMed] [Google Scholar]
- 51.Oldervoll LM, Loge JH, Paltiel H, et al. Are palliative cancer patients willing and able to participate in a physical exercise program? Palliat Support Care. 2005;3:281–287. doi: 10.1017/s1478951505050443. [DOI] [PubMed] [Google Scholar]
- 52.Oldervoll LM, Loge JH, Paltiel H, et al. The effect of a physical exercise program in palliative care: a phase II study. J Pain Symptom Manage. 2006;31:421–430. doi: 10.1016/j.jpainsymman.2005.10.004. [see comment] [DOI] [PubMed] [Google Scholar]
- 53.Gibbons RJ, Balady GJ, Bricker JT, et al. ACC/AHA 2002 guideline update for exercise testing: summary article: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Update the 1997 Exercise Testing Guidelines) Circulation. 2002;106:1883–1892. doi: 10.1161/01.cir.0000034670.06526.15. [DOI] [PubMed] [Google Scholar]
- 54.ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166:111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 55.de Torres JP, Pinto-Plata V, Ingenito E, et al. Power of outcome measurements to detect clinically significant changes in pulmonary rehabilitation of patients with COPD. Chest. 2002;121:1092–1098. doi: 10.1378/chest.121.4.1092. [DOI] [PubMed] [Google Scholar]
- 56.Kraemer WJ, Adams K, Cafarelli E, et al. American College of Sports Medicine position stand. Progression models in resistance training for healthy adults. Med Sci Sports Exerc. 2002;34:364–380. doi: 10.1097/00005768-200202000-00027. [DOI] [PubMed] [Google Scholar]
- 57.Borg G, Hassmen P, Lagerstrom M. Perceived exertion related to heart rate and blood lactate during arm and leg exercise. Eur J Appl Physiol Occup Physiol. 1987;56:679–685. doi: 10.1007/BF00424810. [DOI] [PubMed] [Google Scholar]
- 58.Whaley MH, Woodall T, Kaminsky LA, Emmett JD. Reliability of perceived exertion during graded exercise testing in apparently healthy adults. J Cardiopulm Rehabil. 1997;17:37–42. doi: 10.1097/00008483-199701000-00005. [DOI] [PubMed] [Google Scholar]
- 59.Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. J Clin Oncol. 1993;11:570–579. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 60.Cella DF, Bonomi AE, Lloyd SR, Tulsky DS, Kaplan E, Bonomi P. Reliability and validity of the Functional Assessment of Cancer Therapy-Lung (FACT-L) quality of life instrument. Lung Cancer. 1995;12:199–220. doi: 10.1016/0169-5002(95)00450-f. [DOI] [PubMed] [Google Scholar]
- 61.Cella D, Eton DT, Lai JS, Peterman AH, Merkel DE. Combining anchor and distribution-based methods to derive minimal clinically important differences on the Functional Assessment of Cancer Therapy (FACT) anemia and fatigue scales. J Pain Symptom Manage. 2002;24:547–561. doi: 10.1016/s0885-3924(02)00529-8. [DOI] [PubMed] [Google Scholar]
- 62.Cella D, Herbst RS, Lynch TJ, et al. Clinically meaningful improvement in symptoms and quality of life for patients with non-small-cell lung cancer receiving gefitinib in a randomized controlled trial. J Clin Oncol. 2005;23:2946–2954. doi: 10.1200/JCO.2005.05.153. [DOI] [PubMed] [Google Scholar]
- 63.Kris MG, Natale RB, Herbst RS, et al. Efficacy of gefitinib, an inhibitor of the epidermal growth factor receptor tyrosine kinase, in symptomatic patients with non-small cell lung cancer: a randomized trial. JAMA. 2003;290:2149–2158. doi: 10.1001/jama.290.16.2149. [see comment] [DOI] [PubMed] [Google Scholar]
- 64.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 65.Troosters T, Gosselink R, Decramer M. Short- and long-term effects of outpatient rehabilitation in patients with chronic obstructive pulmonary disease: a randomized trial. Am J Med. 2000;109:207–212. doi: 10.1016/s0002-9343(00)00472-1. [DOI] [PubMed] [Google Scholar]
- 66.Normandin EA, McCusker C, Connors M, Vale F, Gerardi D, ZuWallack RL. An evaluation of two approaches to exercise conditioning in pulmonary rehabilitation. Chest. 2002;121:1085–1091. doi: 10.1378/chest.121.4.1085. [DOI] [PubMed] [Google Scholar]
- 67.Guell R, Casan P, Belda J, et al. Long-term effects of outpatient rehabilitation of COPD: a randomized trial. Chest. 2000;117:976–983. doi: 10.1378/chest.117.4.976. [DOI] [PubMed] [Google Scholar]
- 68.Adamsen L, Quist M, Midtgaard J, et al. The effect of a multidimensional exercise intervention on physical capacity, well-being and quality of life in cancer patients undergoing chemotherapy. Support Care Cancer. 2006;14:116–127. doi: 10.1007/s00520-005-0864-x. [DOI] [PubMed] [Google Scholar]
- 69.Dalzell MA, Kreisman H, Dobson S, et al. Exercise in patients with advanced non-small cell lung cancer (NSCLC): compliance and population characteristics of patients referred to the McGill Cancer Nutrition-Rehabilitation Program (CNRP) American Society of Clinical Oncology; Atlanta, GA: 2006. [Google Scholar]
- 70.Lucia A, Earnest C, Perez M. Cancer-related fatigue: can exercise physiology assist oncologists? Lancet Oncol. 2003;4:616–625. doi: 10.1016/s1470-2045(03)01221-x. [DOI] [PubMed] [Google Scholar]
- 71.Kasymjanova G, Kreisman H, Pepe C, et al. Effect of chemotherapy on exercise capacity in patients with advanced non-small cell lung cancer (NSCLC) American Society of Clinical Oncology; Chicago, IL: 2007. [Google Scholar]
- 72.Sandler A, Gray R, Perry MC, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med. 2006;355:2542–2550. doi: 10.1056/NEJMoa061884. [DOI] [PubMed] [Google Scholar]
- 73.Pulmonary rehabilitation: joint ACCP/AACVPR evidence-based guidelines. ACCP/AACVPR Pulmonary Rehabilitation Guidelines Panel. American College of Chest Physicians. American Association of Cardiovascular and Pulmonary Rehabilitation. Chest. 1997;112:1363–1396. [PubMed] [Google Scholar]
- 74.Griffiths TL, Burr ML, Campbell IA, et al. Results at 1 year of outpatient multidisciplinary pulmonary rehabilitation: a randomised controlled trial. Lancet. 2000;355:362–368. doi: 10.1016/s0140-6736(99)07042-7. [comment] (erratum appears in Lancet 2000;355:1280 Note: Lonescu AA [corrected to Ionescu AA]) [DOI] [PubMed] [Google Scholar]