Abstract
Objectives
This study examined the rate of tobacco use (cigarette smoking and smokeless tobacco [ST]) at three time points: during the 3 months before pregnancy, during pregnancy, and at 6 weeks postpartum among Alaska Native women residing in the Y-K Delta region of Western Alaska.
Methods
A retrospective, non-randomized observational cohort design was utilized. The sample consisted of 832 Alaska Natives (mean maternal age = 26.2 years, average length of gestation = 3.8 months) seen at their first prenatal visit and enrolled in the women, infant, and children (WIC) program at the Yukon-Kuskokwim Delta Regional Hospital in Bethel, Alaska, during a 2-year-period (2001–2002). Tobacco use was assessed using an interview format at the first prenatal and at the 6-week postpartum visits.
Results
The rates of any tobacco use were 48% (95% CI 45%, 52%) 3 months before pregnancy, 79% (95% CI 76%, 82%) during pregnancy, and 70% (95% CI 67%, 74%) at 6 weeks postpartum. The proportion of women using ST changed significantly (P < 0.001) over the three time points (14%, 60%, and 61%, respectively) as well as the proportion of women who smoked cigarettes (P < 0.001) (40%, 42%, and 19%, respectively).
Conclusions
This study documents the high rate of tobacco use, particularly ST use, during pregnancy among Alaska Native women. Development of tobacco use prevention and cessation interventions during pregnancy for Alaska Native women is warranted.
Keywords: Tobacco, Cessation, Pregnancy, Alaska Native, WIC
Introduction
In 2000, cigarette smoking during pregnancy was most prevalent among American Indian and Alaska Native women (20%) followed by non-Hispanic Whites (16%), non-Hispanic Blacks (9%) and Hispanic women (4%) [1]. Few studies [2–4] have documented the rates of smokeless tobacco (ST) use or cessation during pregnancy, but the rate of ST use among females in the US population (0.4%) is very low [5]. Maternal use of ST is queried on birth certificates only in two states (Alaska and Oregon), and on the pregnancy risk assessment monitoring system (PRAMS) only in Alaska [6]. However, data aggregated at the state and national level can mask the high ST use patterns among select subpopulations [5]. Studies conducted among small, select samples of Alaska Native women residing in the Yukon-Kuskokwim (Y-K) Delta of Western Alaska estimate that over half use ST or smoke cigarettes during pregnancy [7, 8]. The current study examined the rate of tobacco use before, during, and after pregnancy in a large sample of Alaska Native women residing in Western Alaska.
Tobacco use was not originally part of the Alaska Native culture. Early English explorers arriving in Kuskowkim Bay in 1778 discovered that tobacco was unknown to Alaska Natives of this region [9, 10]. Tobacco became a regular trade item from Siberia to Alaska after 1800. The Russians built a trading post along the Kuskokwim River in 1841 where tobacco became one trade item of lasting importance. In the late 1800s, detailed historical accounts about tobacco use in the region noted that men, women, and children used snuff and chewing tobacco, and men smoked tobacco in pipes. Chewing tobacco was made by shredding leaf tobacco and mixing it with ash from birch fungus [9, 10]. Known as Iqmik, this homemade form of chewing tobacco is the most common form of ST used among Y-K Delta Alaska Native people [11, 12]. However, Alaska Natives do not use Iqmik or other tobacco products for ceremonial purposes [11–13].
Focus groups and individual interviews with Y-K Delta Alaska Natives indicate that Iqmik is perceived as stronger and more satisfying than other forms of tobacco [13]. Because of the high pH (10.9) of the fungus ash, almost 100% of the nicotine in Iqmik is in the freebase form [12]. This allows for rapid absorption of nicotine across the buccal mucosal membrane, which likely contributes to the addiction potential of Iqmik. In a prospective pilot study of 60 pregnant women of this region [7], we found that, at delivery, mean maternal serum cotinine concentrations were significantly higher for those using Iqmik only than for women who used other tobacco products (167 ± 116 vs. 81 ± 100 ng/ml). Cord blood cotinine concentrations were also significantly higher for infants born to mothers who used only Iqmik versus other forms of tobacco. The maternal cotinine concentrations were almost five times higher than the average (32.9 ng/ml) observed in mothers who smoked cigarettes before delivery [14]. Nonetheless, our qualitative work suggests a lack of knowledge among Alaska Natives about the health effects of Iqmik use [12, 13]. Most pregnant women who participated in our focus groups who smoked cigarettes before pregnancy reported they switched to Iqmik when they learned they were pregnant, and none believed that Iqmik would cause any adverse effect for her fetus [13]. One reason Iqmik is perceived as safer is because it contains mostly “natural” ingredients (e.g., ash).
The aims of this study conducted among Alaska Native pregnant women residing in Western Alaska were: (1) To estimate the proportion of women using tobacco (cigarette smoking and ST) during the 3 months before pregnancy, during pregnancy, and at 6 weeks postpartum; (2) To examine changes in cigarette consumption during pregnancy and at 6 weeks postpartum among women who smoked cigarettes before pregnancy; (3) To examine differences in maternal age between tobacco users and non-users before pregnancy; and (4) To examine the association between age and tobacco abstinence status during pregnancy and postpartum.
Methods
Study Design
This study was approved by the Yukon-Kuskokwim Health Corporation, Alaska Native Tribal Health Consortium, Alaska Area IRB, and the Mayo Clinic IRB. We utilized a retrospective, non-randomized observational cohort design. We used existing data collected for women seen at their first prenatal visit and enrolled in the women, infant, and children (WIC) program at the Yukon-Kuskokwim Delta Regional Hospital (YKDRH) in Bethel, Alaska, between 2001 and 2002. A de-identified WIC database was obtained from the State of Alaska.
Study Setting
The Y-K Delta covers an area in Western Alaska about the size of the state of Ohio with a total population of 25,000. The village of Bethel (population 6,000) is the regional hub for the 58 villages comprising the Y-K Delta region. Approximately 94% of the population outside of Bethel is Alaska Native—either Yup’ik or Cup’ik—and is fairly homogenous with respect to socioeconomic status, language, and culture. Most residents live subsistence lifestyles, hunting and fishing and gathering berries and plants, and receive some monetary assistance from the federal and state governments. The 58 villages are not linked by a common road system and are accessible only by boat, airplane, or snowmobile. The majority of residents of this region receive their health care through the village-based health aides and the YKDRH. The Yukon-Kuskokwim Health Corporation is a private, non-profit 501(c) [3] organization that owns and operates the YKDRH through the Indian Health Service P.L. 93–638.
The WIC program at the YKDRH is a federally funded program, directed by one of our co-authors (E.O.). The program does not include prevention of or intervention for tobacco use. However, each woman was provided with a brochure on the risks of tobacco use of all forms during pregnancy, and she was advised to quit using tobacco.
Study Sample
The sample consisted of all Y-K Delta women enrolled in the WIC Program at their 1st prenatal visit between January 1, 2001 and December 31, 2002 who met the criteria for inclusion in the study. Deliveries occurred from 2001 to 2003, during which time there were 1,801 deliveries. Inclusion criteria were: [1] were Alaska Native; [2] enrolled in WIC during prenatal care 2001–2002 and re-enrolled in WIC postpartum; [3] had complete data on their tobacco use status at all three time points—before, during, and after pregnancy; and [4] had data on length of gestation. A total of 832 women form the basis of this report.
Nearly all (96%) women from the Y-K Delta region are seen for prenatal care at the YKDRH. Of those seen for prenatal care, 95% enroll in the WIC program. Reasons for not enrolling in WIC are lack of information that the woman is eligible, lack of knowledge of the benefits of being in the program, or choosing not to be in the program for stigma (common for teen moms). Of women who are seen for prenatal care in Bethel, about 70% return for a 6-week postpartum visit, and among these women, re-enrollment in WIC is excellent (99%). In addition to not returning for a postpartum visit and moving out of the area after delivery, reasons for not re-enrolling postpartum are similar to those noted above.
Clinical data indicate that 1,672 women enrolled in WIC during the period 2001–2002 (362 during their 1st trimester, 573 during their 2nd trimester, and 737 during their 3rd trimester), of which 99% (1,656) were Alaska Native. Of these 1,656 Alaska Native women, we estimate that 1,160 (70%) returned for a postpartum visit, of which 1,149 (99%) re-enrolled in WIC postpartum. The remaining women were excluded from the database provided by the state of Alaska because of missing data on tobacco use or gestational age. Our sample of 832 therefore represents about half of the women enrolled in WIC during the time period 2001–2002.
Procedure
All women who enrolled in WIC received a face-to-face interview by a nutritionist at two time periods: (1) Prenatal Visit—at the time of application and enrollment into the WIC Program at the 1st visit, and (2) Postpartum Visit—at the time of re-enrollment into the WIC Program at the 6-week postpartum check.
Self-reported tobacco use status was assessed for three time points: during the 3 months before pregnancy, during pregnancy, and at 6 weeks postpartum. The questions used to assess tobacco use were consistent over the study period. Table 1 describes the timing of the assessments and questions used to assess tobacco use. The WIC forms assessed both ST use and cigarette smoking. Responses were recorded on WIC forms primarily as yes/no by the means of check boxes. For ST use, the WIC forms did not differentiate chewing tobacco, snuff, or Iqmik use; thus for analysis purposes a positive response to this response option was classified as ST use. Unlike cigarette smoking (see Table 1), data on frequency or amount of ST used was not assessed for any time point.
Table 1.
Assessment of tobacco use in WIC Program, Bethel, Alaska, 2001–2002
| Questions asked for each time point |
WIC interview | |
|---|---|---|
| 1st Prenatal visit enrollment into WIC |
6-Week postpartum visit WIC re-enrollment |
|
| 3 Months before pregnancy | ||
| In the 3 months before you got pregnant, did you smoke? | X | |
| How many cigarettes did you smoke in a day? | X | |
| In the 3 months before you got pregnant, did you use chewing tobacco or snuff? | X | |
| During pregnancy | ||
| Have you smoked during this pregnancy? | X | |
| How many cigarettes did [do] you smoke a day? | X | |
| During this pregnancy, have you used chewing tobacco or snuff? | X | |
| At 6 weeks postpartum | ||
| During this pregnancy, did you smoke? | X | |
| How many cigarettes a day? | X | |
| During this pregnancy did you use chewing tobacco or snuff? | X | |
| Do you smoke now? | X | |
| How many cigarettes a day? | X | |
| Are you using chewing tobacco/snuff now? | X | |
At the prenatal visit interview, women were asked to recall their use of ST and cigarette smoking during the 3-month-period before they learned they were pregnant. The postpartum visit interview assessed current cigarette smoking and use of ST. Cigarette smoking and use of ST during pregnancy was ascertained at both the prenatal and postpartum visit interviews. Women were classified as using tobacco if they reported tobacco use during this pregnancy at either or both visits.
Statistical Methods
The percentage of women who reported using tobacco (cigarettes and ST) at each of the three time points was calculated and summarized using a point-estimate and 95% confidence interval (CI). Additional analyses were restricted to women reporting tobacco use before pregnancy. For this subset of women, the percentage reporting abstinence from smoking during pregnancy and at 6 weeks postpartum was summarized. A repeated measure analysis was performed for any tobacco use, ST use, and cigarette smoking using data from all three assessment points to examine if tobacco use status changed over time. This analysis was performed using generalized estimating equations (GEE) [15] with tobacco use status as the dependent variable and time as the independent variable. The GEE model was fit using a logit link function and an autoregressive (AR1) working correlation matrix.
For women who reported cigarette smoking before pregnancy, the prepregnancy rate of consumption was compared to that reported during pregnancy using the paired t-test. This analysis was restricted to women that reported smoking during pregnancy. Similar analyses were performed to assess change in cigarettes per day from prepregnancy to 6 weeks postpartum.
Data on age was compared for women that did and did not report tobacco use before pregnancy using the two-sample t-test. Analyses were also performed separately for each tobacco product. Logistic regression was used to identify whether maternal age was associated with tobacco abstinence during pregnancy and postpartum for the subset of women who reported using tobacco before pregnancy. Analyses were performed for any tobacco use (cigarettes or ST) and also separately for each tobacco product. For the 6-week postpartum time point, the analysis was restricted to women who delivered a live birth (95% of the sample). In all analyses, two-sided tests were performed with P-values ≤0.05 used to denote statistical significance.
Results
Participants
The 832 Alaska Native women ranged in age from 14 to 44 years; mean (SD) = 26.3 (6.5), median = 25.4. There were 51 (6.1%) participants less than 18 years of age, 300 (36.1%) were between 18 and 24 years of age, and 481 (57.8%) were >24 years old. They were on average at 3.8 months of gestation (113.1 ± 59.9 days, range 17–277 days) when seen at their first prenatal visit and enrolled in WIC. Forty-five percent (n = 373) were at less than 90 days gestation, 327 (39.5%) were between 90 and180 days, and 129 were at >180 days gestation.
Reported Tobacco Use Status During and After Pregnancy, 2001–2003
Table 2 shows the tobacco use status among the women before, during, and after pregnancy. These data show use of any tobacco use. For example, the rates for any ST use combine those who used ST only and those who both used ST and smoked cigarettes. The rates of any tobacco use were 48% (95% CI 45%, 52%) before pregnancy, 79% (95% CI 76%, 82%) during pregnancy, and 70% (95% CI 67%, 74%) at 6 weeks postpartum. Based on GEE repeated measures analysis, the use of any tobacco changed significantly (P < 0.001) across the three time points. Moreover, the rates of ST use (P < 0.001) and of cigarette smoking (P < 0.001) significantly changed over time. Similar results were obtained when adjusting for age and length of gestation (P < 0.001 in each case).
Table 2.
Tobacco use before, during, and after pregnancy among 832 Alaska Native women from Western Alaska enrolled in the WIC Program, 2001–2002
| Time pointa | Percentage (%) |
95% confidence interval (%) |
|---|---|---|
| 3 Months before pregnancy | ||
| Any cigarette smoking | 40 | 36%, 43% |
| Any ST use | 14 | 12%, 17% |
| Any tobacco use | 48 | 45%, 52% |
| During pregnancy | ||
| Any Cigarette smoking | 42 | 38%, 45% |
| Any ST use | 60 | 57%, 63% |
| Any tobacco use | 79 | 76%, 82% |
| At 6 weeks Postpartum | ||
| Any cigarette smoking | 19 | 16%, 21% |
| Any ST use | 61 | 57%, 64% |
| Any tobacco use | 70 | 67%, 74% |
Categories not mutually exclusive. For example, women who both smoked cigarettes and used ST during pregnancy were counted in the respective percentages for any cigarette smoking and any ST use during pregnancy
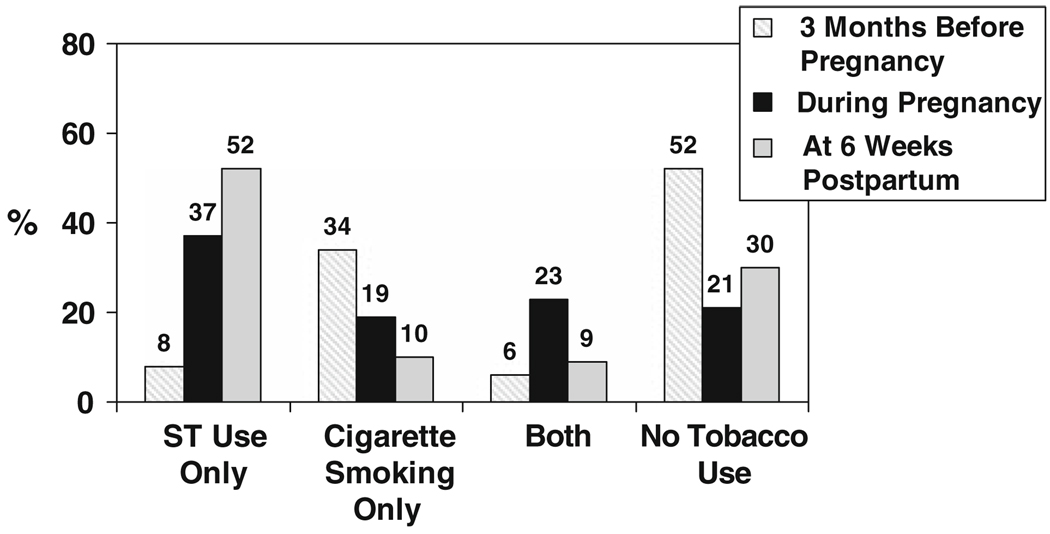
We also examined the data from a different perspective of exclusive use of a tobacco product (ST only, cigarette smoking only). Figure 1 shows the rates for smoking only, chewing only, both, or neither at the three time points.
Fig. 1.
Percentage of Alaska Native women using tobacco 3 months before pregnancy, during pregnancy, and at 6 weeks postpartum, WIC Program, 2001–2002 (n = 832). The categories of tobacco users in this figure are mutually exclusive. The percentages do not add to 100 due to rounding
Maternal Age and Tobacco Use
Younger age was significantly (P < 0.001) associated with any tobacco use before pregnancy. The average (SD) age was 25.0 (5.8) among those using any tobacco product and 27.4 (6.8) years among those not reporting tobacco use during this time. Women who smoked cigarettes before pregnancy were significantly younger than those who did not, 24.5 (5.4) vs. 27.4 (6.8); P < 0.001. However, no age difference was found for any use of ST before pregnancy.
Tobacco Use Patterns
We explored whether there was any evidence that women switched from cigarette smoking before pregnancy to ST use during pregnancy (Table 3). Of the 281 women who reported smoking only before pregnancy, during pregnancy 31% reported smoking only, 15% indicated ST use only, and 48% reported both. Conversely, of the 70 women who reported use of ST only before pregnancy, 20% smoked only during pregnancy, 17% used ST only, but none reported both. Table 3 also shows that there were 432 women who did not use tobacco before pregnancy of which 75% used some form of tobacco during pregnancy, with most reporting ST use. Conversely, of 400 women who used tobacco before pregnancy, few (17%) were not using during pregnancy.
Table 3.
Tobacco use patterns before and during pregnancy among 832 Alaska Native women from Western Alaska enrolled in the WIC Program, 2001–2002a
| Tobacco use 3 months before pregnancy |
N | Tobacco use during pregnancy | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No tobacco use | Any tobacco use | Smoking only | ST use only | Both smoking & ST use | |||||||
| % | n | % | n | % | n | % | n | % | n | ||
| No tobacco use | 432 | 25 | 109 | 75 | 323 | 5 | 23 | 58 | 251 | 11 | 49 |
| Any tobacco use | 400 | 17 | 67 | 83 | 333 | 33 | 133 | 14 | 57 | 36 | 143 |
| Type of tobacco users | |||||||||||
| Smoking only | 281 | 6 | 18 | 94 | 263 | 31 | 88 | 15 | 41 | 48 | 134 |
| ST use only | 70 | 63 | 44 | 37 | 26 | 20 | 14 | 17 | 12 | 0 | 0 |
| Both | 49 | 10 | 5 | 90 | 44 | 63 | 31 | 8 | 4 | 18 | 9 |
% reflect percentage of the N (denominator) for each row. For example, of the 432 who did not use any tobacco before pregnancy, 75% used tobacco during pregnancy. The sum of the percentages using no and any tobacco use add to 100% and the sum of the percentages using no tobacco and the percentages for smoking only, ST use only and both add to about 100%
Cigarettes Smoked Per Day (CPD)
Women smoked relatively few CPD at each of the three time points. The number of women with available data on CPD was 324 of the 330 who smoked before pregnancy, 324 of the 348 who smoked during pregnancy, and 115 of the 155 women who smoked after pregnancy. The mean (SD) CPD for these respective time points was 5.6 (4.1), 4.0 (3.1), and 4.2 (2.8).
With respect to changes in CPD over time, 262 women reported both smoking before and during pregnancy, and had available data on CPD at both time points. Among these women, a statistically significant (P < 0.001) mean (SD) reduction of 1.8 (3.3) CPD, range 8–19 was detected. Moreover, 101 women reported smoking both before and after pregnancy and had available data on CPD at both time points. For these women, we observed a statistically significant (P < 0.001) mean reduction of 2.3 (4.1) CPD, range 5–19.
Tobacco Cessation
Among the 400 women who used any form of tobacco before pregnancy, 67 (17%; 95% CI 13%, 21%) reported no tobacco use during pregnancy and 122 (31%; 95% CI 26%, 35%) reported no tobacco use at 6 weeks postpartum. Older maternal age was significantly associated with an increased likelihood of quitting tobacco use during pregnancy (odds ratio [OR] = 1.10; 95% CI 1.06, 1.15, P < 0.001) but maternal age was not associated with tobacco abstinence postpartum.
Postpartum Relapse to Tobacco Use
Sixty-seven women reported some type of tobacco use before pregnancy but no tobacco use during pregnancy. Of these, 42 women (63%) reported tobacco use at 6 weeks postpartum. The respective relapse rates for smoking and ST use were 18% (12 of 68) and 63% (59 of 94).
Discussion
This is one of the first studies to document tobacco use before, during, and after pregnancy in a large sample of Alaska Native women residing in Western Alaska. Consistent with earlier, smaller studies [7, 8] we found that tobacco use was very high [79%] during pregnancy. This was primarily due to the increase in use of ST from 14% before pregnancy to 60% during pregnancy. Our tobacco use rates can be contrasted to national rates of ST use among females in the US population [<0.4%] [5], and to the rates of cigarette smoking during pregnancy that range from 4 to 20% depending on ethnic group [1]. Our results are consistent with an unpublished analysis from the statewide pregnancy risk assessment monitoring system [PRAMS] study [16] which examined tobacco use in a representative sample of 5,255 Alaska women who delivered a live infant during 1996–1999. Among non-Alaska Natives, 0.9% indicated prenatal ST use compared with 22.5% of Alaska Natives statewide. The rates of ST use (61%) and cigarette smoking (16%) were markedly higher among women residing in the Y-K Delta region. In addition to geographic region, younger age and less education were significant risk groups for prenatal ST use.
Many women in our prior focus groups [13] reported switching from cigarette smoking to Iqmik use when they learned they were pregnant because they perceived it as safer. Somewhat in support of this hypothesis is the finding that among those who smoked cigarettes only before their pregnancy, 62% reported ST use during pregnancy. The reverse behavior was less common among those who used ST only before pregnancy, 20% of these women reported smoking during pregnancy. Nonetheless, most women who smoked before pregnancy but added ST use during pregnancy also continued to smoke and very few (15%) used ST exclusively during pregnancy. Thus, whether product switching occurs during pregnancy needs to be explored in future prospective work. Alternatively, women may add or use ST to help them cut down on their cigarette consumption, as indicated by the observation that the average number of CPD dropped over the course of pregnancy among women who smoked before pregnancy. The average CPD smoked during pregnancy (4.0) is consistent with national data [17]. In 2000, about seven in 10 women who smoked during pregnancy smoked less than 10 CPD [18].
Limitations
This study has several limitations. First, we relied on an existing database of all women who enrolled in WIC and did not have access to non-respondents. Therefore, we are unable to evaluate whether our sample of about half of all WIC enrollees is similar to or different than all enrollees. Second, because we relied on an existing, administrative database we are unable to validate the data collected, either at the time of collection or through review of corresponding medical records. Moreover, we were limited by the questions used to assess tobacco use in the WIC program. In particular, the “dose” (frequency or amount) of ST used before, during, or after pregnancy was not assessed, and Iqmik use was not distinguished from commercial ST use. However, prior research indicates that Iqmik is the most common form of ST used among Alaska Natives residing in Western Alaska [7, 8, 11, 13]. The WIC data also relied on self-reported tobacco use status and biochemical confirmation was not conducted.
The rates of tobacco use and cessation must be interpreted with caution as the number of women that received intervention for tobacco use is not known. Moreover, the pattern [e.g., by age group) of such interventions may have affected study results as well. However, while all obstetrical providers ask about tobacco use, they lack a mechanism to refer tobacco-using patients to the Nicotine Control and Research Program. Thus, very few women would be expected to have participated in this program. Moreover, no systematic programs or resources are available in the villages for tobacco cessation.
Implications for Research and Practice
Other subgroups of women in the US report high ST use rates [19] when compared to overall national data [5], and some populations worldwide report increased rates of ST use during pregnancy. A growing body of evidence suggests maternal ST use poses risks to both the mother and infant [2–4, 17, 20]. Collectively, the public health implication of these findings is to alert researchers and health care providers in other geographic areas to monitor ST use among women of childbearing age. For example, statewide surveys such as the PRAMS could add core questions on ST use during pregnancy.
This project addressed a community need in that the health and welfare of the children are paramount [13]. Together with the Yukon-Kuskokwim Health Corporation Board of Directors, we have developed a long-term plan to address this community need, which includes prevention of and intervention for tobacco use. Three quarters of the women in our sample who did not use any tobacco before their pregnancy reported prenatal tobacco use, and most of these used ST during pregnancy. Thus, even among women who report no tobacco use before pregnancy, ST use should be queried at every prenatal visit. The reasons why women begin using ST during pregnancy, including sociocultural and psychosocial factors, need exploration. In addition, educational efforts need to be developed, implemented, and evaluated that target Alaska Native women as early as possible to prevent smoking and other tobacco use during pregnancy.
Findings from the current study served as the basis for development of a prenatal tobacco cessation intervention program for Alaska Native women of the Y-K Delta region. From our focus groups [13], we learned that interventions that can be delivered via telephone or video are likely most feasible. Moreover, most participants recommended the use of personal stories by appropriate role models as a potentially acceptable intervention component. Two important learning mechanisms among Alaska Native people are role modeling and story telling, both of which can be incorporated into a video [21, 22]. Personal stories or talking circles have been used to preserve traditions of the Native culture, to explain health and illness, and serve social modeling functions and as teaching tools [23]. Thus, a video highlighting personal stories of Alaska Native pregnant women who have quit tobacco may be an effective intervention component.
Acknowledgments
This study was supported by the National Cancer Institute through a supplement to grant U01 CA86098. We wish to thank Eric Bendor, Stephanie Birch, Kathleen Wayne, and others at the State of Alaska for their assistance with obtaining the data set used in this study. We appreciate the assistance and support of the Yukon-Kuskokwim Delta Regional Hospital OB/prenatal health care providers including R. N. Ann Glasheen, R. N. Claire Lewis, M. D. Leigh Gill, and M. D. Ellen Hodges. We also acknowledge the assistance of Gail Bierbaum, Mayo Clinic, Rochester, for her assistance with manuscript production.
Contributor Information
Christi A. Patten, Email: patten.christi@mayo.edu, Mayo Clinic College of Medicine, Mayo Clinic Cancer Center, Charlton 6-273, 200 First Street SW, Rochester, MN 55905, USA.
Caroline C. Renner, Alaska Native Tribal Health Consortium, Anchorage, AK, USA
Paul A. Decker, Mayo Clinic College of Medicine, Mayo Clinic Cancer Center, Charlton 6-273, 200 First Street SW, Rochester, MN 55905, USA
Ester O’Campo, Yukon-Kuskokwim Health Corporation, Bethel, AK, USA.
Karin Larsen, Mayo Clinic College of Medicine, Mayo Clinic Cancer Center, Charlton 6-273, 200 First Street SW, Rochester, MN 55905, USA.
Carrie Enoch, Yukon-Kuskokwim Health Corporation, Bethel, AK, USA.
Kenneth P. Offord, Mayo Clinic College of Medicine, Mayo Clinic Cancer Center, Charlton 6-273, 200 First Street SW, Rochester, MN 55905, USA
Richard D. Hurt, Mayo Clinic College of Medicine, Mayo Clinic Cancer Center, Mayo Clinic College of Medicine, Mayo Clinic Cancer Center, MN 55905, USA
Anne Lanier, Alaska Native Tribal Health Consortium, Anchorage, AK, USA.
Judith Kaur, Mayo Clinic College of Medicine, Mayo Clinic Cancer Center, Charlton 6-273, 200 First Street SW, Rochester, MN 55905, USA.
References
- 1.Martin JA, Hamilton BE, Ventura SJ, Menacker F, Park MM. Births: final data for 2000. National Vital Statistics. 2002;50(5):1–104. [PubMed] [Google Scholar]
- 2.Gupta PC, Sreevidya S. Smokeless tobacco use, birth weight, and gestational age: population based, prospective cohort study of 1,217 women in Mumbai, India. BMJ. 2004 doi: 10.1136/bmj.38113.687882.EB. doi: 10.1136/bmj.38113.687882.EB. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krishna K. Tobacco chewing in pregnancy. British Journal of Obstetrics and Gynaecology. 1978;85:726–728. [PubMed] [Google Scholar]
- 4.Krishnamurthy S, Joshi S. Gender differences and low birth weight with maternal smokeless tobacco use in pregnancy. Journal of Tropical Pediatrics. 1993;39:253–254. doi: 10.1093/tropej/39.4.253. [DOI] [PubMed] [Google Scholar]
- 5.Substance Abuse and Mental Health Services Administration. Results from the 2005 National Survey on Drug Use and Health: National Findings. Rockville, MD: 2006 (Office of Applied Studies, NSDUH Series H-30, DHHS Publication No. SMA 06-4194).
- 6.Centers for Disease Control and Prevention. Pregnancy Risk Assessment Monitoring System. [Accessed 7 Dec 2007]; http://www.cdc.gov/PRAMS/states.htm.
- 7.Hurt RD, Renner CC, Patten CA, et al. Iqmik—a form of smokeless tobacco used by pregnant Alaska Natives: Nicotine exposure in their neonates. Journal of Maternal Fetal Neonatal Medicine. 2005;17(4):281–289. doi: 10.1080/14767050500123731. [DOI] [PubMed] [Google Scholar]
- 8.Renner CC, Patten CA, Day G, Hurt RD, Lanier AP. Tobacco use during pregnancy among Alaska Natives. Alaska Medicine. 2005;47(1):12–16. [PubMed] [Google Scholar]
- 9.Oswalt W. Bashful no longer: An Alaskan Eskimo ethnohistory, 1778–1988. OK: University of Oklahoma Press; 1990. [Google Scholar]
- 10.Winter JC. Tobacco use by Native North Americans: Sacred smoke and silent killer. OK: Oklahoma Press; 2001. [Google Scholar]
- 11.Blanchette RA, Renner CC, Held B, Enoch C, Angstman S. The current use of Phellinus igniarius by the Eskimos of Western Alaska. Mycologist. 2002;16(4):142–145. [Google Scholar]
- 12.Renner CC, Enoch C, Patten CA, et al. Iqmik: A form of smokeless tobacco used among Alaska natives. American Journal of Health Behavior. 2005;29(6):588–594. doi: 10.5555/ajhb.2005.29.6.588. [DOI] [PubMed] [Google Scholar]
- 13.Renner CC, Patten CA, Enoch C, et al. Focus groups of Y-K Delta Alaska Natives: Attitudes toward tobacco use and tobacco dependence interventions. Preventive Medicine. 2004;38(4):421–431. doi: 10.1016/j.ypmed.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 14.Law KL, Stroud LR, LaGasse LL, Niaura R, Lester BM. Smoking during pregnancy and newborn neurobehavior. Pediatrics. 2003;111(6 Pt 1):1318–1323. doi: 10.1542/peds.111.6.1318. [DOI] [PubMed] [Google Scholar]
- 15.Zeger SL, Liang KY, Albert PS. Models for longitudinal data: A generalized estimating equation approach. Biometrics. 1988;44(4):1049–1060. [PubMed] [Google Scholar]
- 16.Perham-Hester KA. Prenatal smokeless tobacco use in Alaska, 1996–1999 Seventh Annual Maternal Child Health Epidemiology Conference; Clearwater Beach, FL. 2001. [Google Scholar]
- 17.US Department of Health and Human Services. Women and smoking: Report of the Surgeon General. Washington, DC: 2001
- 18.Ventura SJ, Hamilton BE, Mathews TJ, Chandra A. Trends and variations in smoking during pregnancy and low birth weight: Evidence from the birth certificate, 1990–2000. Pediatrics. 2003;111(5):1176–1180. [PubMed] [Google Scholar]
- 19.Agni M, Asma S, Yeong C, Vaithinathan R. Initiation and maintenance of tobacco use. In: Sarnet J, Yoon S, editors. Women and the tobacco epidemic: Challenges for 21st century. Canada: World Health Organization; 2001. [Google Scholar]
- 20.England LJ, Levine RJ, Mills JL, et al. Adverse pregnancy outcomes in snuff users. American Journal of Obstetrics Gynaecology. 2003;189(4):939–943. doi: 10.1067/s0002-9378(03)00661-6. [DOI] [PubMed] [Google Scholar]
- 21.Pelusi J, Krebs LU. Understanding cancer—Understanding the stories of life and living. Journal of Cancer Education. 2005;20 Suppl:12–16. doi: 10.1207/s15430154jce2001s_04. [DOI] [PubMed] [Google Scholar]
- 22.Stillwater B, Echavarria VA, Lanier AP. Pilot test of a cervical cancer prevention video developed for Alaska Native women. Public Health Reports. 1995;110:211–214. [PMC free article] [PubMed] [Google Scholar]
- 23.Tom-Orme L. Native Americans explaining illness: Storytelling as illness experience. In: Whaley BB, editor. Explaining illness: Research, theory, and strategies. New Jersey: Mahwah; 2000. pp. 237–257. [Google Scholar]