Abstract
Objective: Quantitation of D-dimer level during a sickling crisis and its correlation with other clinical abnormalities.
Design: Prospective longitudinal study.
Setting: Armed Forces Hospital, Southern Region, Kingdom of Saudi Arabia.
Patients: Adult patients (12 years and older) admitted acutely with a sickle cell crisis who consent to taking part in the study. Candidates may re-participate if they are readmitted with a further acute painful crisis.
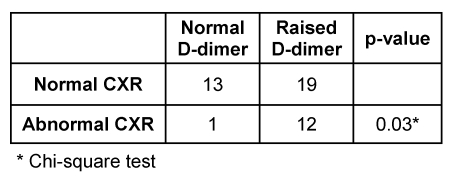
Results: 36 patients with homozygous sickle cell disease consented to take part in the study. D-dimer levels were raised in 31 (68.9%) of 45 episodes of painful crisis of whom 13 had an abnormal chest X-ray. Of those with a normal chest X-ray only one patient had a raised D-dimer level: sensitivity of 92.3%, specificity 40.6%, positive predictive value 38.7% and negative predictive value of 92.9% for an abnormal chest X-ray.
Conclusion: D-dimer levels are frequently raised during an acute painful crisis. A normal level has a high negative predictive value for an abnormal chest X-ray.
Keywords: coagulation, hemoglobinopathy, lung, painful
Abstract
Ziel der Studie: Bestimmung der D-Dimer-Konzentration während Sichelzellkrisen und deren Korrelation mit anderen klinischen Befunden.
Design: Prospektive Longitudinalstudie.
Ort: Armed Forces Hospital, Southern Region, Kingdom of Saudi Arabia.
Patienten: Erwachsene Patienten (ab 12. Lebensjahr), eingewiesen mit akuter Sichelzellkrise, stimmten der Teilnahme an der Studie zu. Entlassene Patienten wurden bei einer wiederholten schmerzhaften Krise erneut in die Studie aufgenommen.
Ergebnisse: 36 Patienten mit homozygoter Sichelzellerkrankung haben freiwillig an der Studie teilgenommen. D-Dimer-Spiegel stiegen bei 31 (68,9%) von 45 Episoden mit schmerzhaften Krisen an, wobei in 13 Fällen abnorme Röntgenbefunde an der Lunge erhoben wurden. Bei Patienten, die einen normalen Lungenbefund hatten, war die D-Dimer-Konzentration nur in einem Fall erhöht: Die diagnostische Sensitivität betrug 92,3%, die diagnostische Spezifität 40,6%. Der positive Vorhersagewert war 38,7% und der negative Vorhersagewert 92,9% bei einem abnormen Lungenbefund.
Schlussfolgerung: Die Konzentrationen von D-Dimeren sind bei akuten, schmerzhaften Sichelzellkrisen häufig erhöht. D-Dimer-Konzentrationen im Referenzbereich haben einen hohen negativen prädiktiven Wert für abnorme Lungenbefunde.
Introduction
Sickle cell disease (SCD) is characterized by a hypercoagulable state, a description that unequivocally portrays disease pathogenesis. Thrombogenic and fibrinolytic activities are elevated in patients with SCD both during the steady state and during crises [1], [2], [3], [4], [5], perturbations that are predictive of painful crises frequency [5]. The increased thrombogenicity is related to an enhanced pro-coagulant property of sickled erythrocytes [6]. Exposed phosphatidyl serine moieties on sickled red blood cells directly augment thrombin generation [6]. The latter is further amplified by the increased adhesiveness of the formed elements to each other and to the endothelium, reduced blood flow and increased transit time. Thrombin generation is coupled with an increased fibrinolytic activity leading to increased D-dimer levels and plasmin-anti-plasmin complexes. Levels of the former are raised in both the acute sickle cell crisis as well as during the steady state and are reportedly markers of sickle cell disease related complications [2], [5], [7], [8]. The objectives of this study are the quantitation of D-dimer level during a painful crisis and its correlation with other clinical abnormalities.
Materials and methods
Design
Prospective longitudinal study.
Setting
Armed Forces Hospital, Southern Region, Kingdom of Saudi Arabia.
Patients
Adult patients (12 years and older) admitted acutely with sickle cell crises who consent to taking part in the study. Patients who are unwilling to participate in the study are excluded. Candidates may re-participate if they are readmitted with a further acute painful crisis.
Methods
A sickle cell crisis was defined as any increase in bodily pains necessitating hospital admission. Demographic data, routine chemistry, hematology, chest X-ray and D-dimer were recorded on admission. D-dimer level was checked by ELISA (D-Dimer Plus-Dade Behring Marburg GmbH, normal range up to 250 ug/l). Readings are reported as less than 250 ug/l or otherwise the exact figure is quoted. The former are categorized as normal and the latter as raised. For mathematical calculations any reading reported as less or equal to 250 ug/l is computer-entered as 250. All chest X-rays are reported by one radiologist who is blinded to the D-dimer and other laboratory results. The following findings on a chest X-ray were considered abnormal: atelectasis, infiltrate, consolidation or pleural effusion. Numerical data are statistically tested for significance using the two-sample t-test or the Mann-Whitney test. Categorical data are tested using the chi-square test. A p-value of less than 0.05 is considered significant and the exact figure quoted.
Results
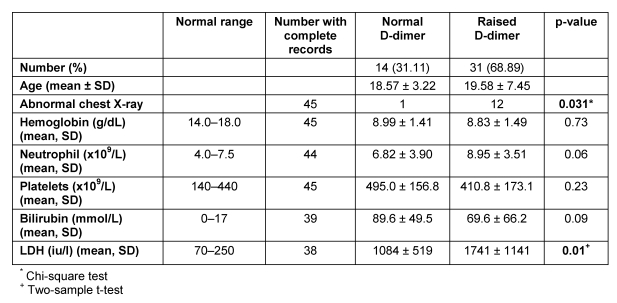
Results for 45 painful sickle cell crisis episodes in 36 patients were available. Twenty patients were male (55.6%). Mean age for males was 18.6 years and for females 20.6 years with a range of 12–37 years. D-dimer levels were raised in 31 episodes (68.89%) (Table 1 (Tab. 1)). Mean level for these episodes was 1379 ug/l with a range of 274–9143 ug/l. Seven patients contributed to 17 episodes (2–4 episodes each), 11 of which demonstrated a raised D-dimer level. The chest X-ray was reported as abnormal in 13 of the 45 episodes (28.9%), 12 (92.3%) of which had a raised D-dimer (chi-square test, p=0.031) (Table 1 (Tab. 1)). Of the 32 episodes where a chest X-ray was reported as normal, 19 (59.4%) had a raised D-dimer level (Table 1 (Tab. 1)). Mean D-dimer level was 584.2 ug/l in those with a normal chest X-ray (range 250–3119 ug/l) and 2117.0 ug/l in those with an abnormal one (range 250–9143 ug/l). An elevated D-dimer level has a sensitivity of 92.3%, specificity 40.6%, positive predictive value 38.7% and negative predictive value of 92.9% for an abnormal chest X-ray. The likelihood ratio for an abnormal chest X-ray if the D-dimer test is positive is 1.6. There was no correlation between the D-dimer level and hemoglobin, neutrophil, platelet or bilirubin levels. Lactate dehydrogenase levels were however, significantly raised in those with elevated D-dimer readings (Table 2 (Tab. 2)).
Table 1. Chest X-ray (CXR).
Table 2. D-dimer levels and results of other clinical investigations.
Discussion
This study confirms the presence of raised D-dimer levels during painful sickle cell crises in Saudi patients. Similar findings in other patient populations have previously been reported [1], [2], [4], [7]. This study also shows that an abnormal chest X-ray is almost always associated with an elevated D-dimer level. Conversely, the chest X-ray was reported as normal in the majority of patients with a normal level giving the latter finding a high negative predictive value. Respiratory complications are currently the most common cause of death and second most common cause of hospitalization in patients with sickle cell disease [9], [10]. Earlier diagnosis of the acute chest syndrome and the prompt institution of treatment are paramount if mortality from this complication is to be reduced. One of the earliest features of the acute chest syndrome is the development of new pulmonary infiltrates in the chest X-ray. Early detection of radiological changes is thus therapeutically and prognostically very important. In the Armed Forces Hospital (Southern Region) where this study was conducted, guidelines for the management of sickle cell crises emphasize the need for the prompt implementation of a sickle chest therapeutic protocol upon the discovery of any new pulmonary shadowing on X-ray. The above findings may therefore be useful in the clinical decision process in that a normal D-dimer level may provide some assurance that the patient is not having the sickle chest complication. On the other hand, a raised D-dimer should encourage a prompt and thorough assessment of the chest X-ray and may be the need for requesting serial X-rays to exclude the development of this potentially fatal complication. Recent literature suggests that anticoagulation with low-dose warfarin significantly reduces the D-dimer levels during a vaso-occlusive crisis [11]. Furthermore, in a more recent double-blind randomized trial, tinzaparin administration to patients with an acute vaso-occlusive crisis resulted in a statistically significant reduction in the number of days with the severest pain score, overall duration of painful crisis, and duration of hospitalization [12].
In conclusion, our findings confirm the raised D-dimer levels during acute sickle cell painful crises and that the majority of patients with an abnormal chest X-ray have a raised level. Studies to qualitatively and quantitatively assess the value of D-dimer testing in sickling crises severity scoring, possible emergency interventional therapies and acute prognostication are needed.
Notes
Conflicts of interest
None declared.
Acknowledgement
The authors wish to thank Dr. Ahmad Haddad FRCR (Consultant Radiologist) for reporting on the chest X-rays.
References
- 1. Francis RB., JR Elevated fibrin D-dimer fragment in sickle cell anemia: evidence for activation of coagulation during the steady state as well as in painful crisis. Haemostasis. 1989;19(2):105–111. doi: 10.1159/000215901. [DOI] [PubMed] [Google Scholar]
- 2. Nsiri B, Gritli N, Bayoudh F, Messaoud T, Fattoum S, Machghoul S. Abnormalities of coagulation and fibrinolysis in homozygous sickle cell disease. Hematol Cell Ther. 1996;38(3):279–284. doi: 10.1007/s00282-996-0279-2. Available from: http://dx.doi.org/10.1007/s00282-996-0279-2. [DOI] [PubMed] [Google Scholar]
- 3. Kurantsin-Mills J, Ofosu FA, Safa TK, Siegel RS, Lessin LS. Plasma factor VII and thrombin-antithrombin III levels indicate increased tissue factor activity in sickle cell patients. Br J Haematol. 1992;81(4):539–544. doi: 10.1111/j.1365-2141.1992.tb02989.x. Available from: http://dx.doi.org/10.1111/j.1365-2141.1992.tb02989.x. [DOI] [PubMed] [Google Scholar]
- 4. Devine DV, Kinney TR, Thomas PF, Rosse WF, Greenberg CS. Fragment D-dimer levels: an objective marker of vaso-occlusive crisis and other complications of sickle cell disease. Blood. 1986;68(1):317–319. [PubMed] [Google Scholar]
- 5. Tomer A, Harker LA, Kasey S, Eckman JR. Thrombogenesis in sickle cell disease. J Lab Clin Med. 2001;137(6):398–407. doi: 10.1067/mlc.2001.115450. Available from: http://dx.doi.org/10.1067/mlc.2001.115450. [DOI] [PubMed] [Google Scholar]
- 6. Setty BN, Rao AK, Stuart MJ. Thrombophilia in sickle cell disease: the red cell connection. Blood. 2001;98(12):3228–3233. doi: 10.1182/blood.V98.12.3228. Available from: http://dx.doi.org/10.1182/blood.V98.12.3228. [DOI] [PubMed] [Google Scholar]
- 7. Hagger D, Wolff S, Owen J, Samson D. Changes in coagulation and fibrinolysis in patients with sickle cell disease compared with healthy black controls. Blood Coagul Fibrinolysis. 1995;6(2):93–99. doi: 10.1097/00001721-199504000-00001. Available from: http://dx.doi.org/10.1097/00001721-199504000-00001. [DOI] [PubMed] [Google Scholar]
- 8. Ataga KI. Hypercoagulability and thrombotic complications in hemolytic anemias. Haematologica. 2009;94(11):1481–1484. doi: 10.3324/haematol.2009.013672. Available from: http://dx.doi.org/10.3324/haematol.2009.013672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vichinsky EP, Styles LA, Colangelo LH, Wright EC, Castro O, Nickerson B. Acute chest syndrome in sickle cell disease: clinical presentation and course. Cooperative Study of Sickle Cell Disease. Blood. 1997;89(5):1787–1792. [PubMed] [Google Scholar]
- 10. Thomas AN, Pattison C, Serjeant GR. Causes of death in sickle-cell disease in Jamaica. Br Med J (Clin Res Ed) 1982;285(6342):633–635. doi: 10.1136/bmj.285.6342.633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Ahmed S, Siddiqui AK, Iqbal U, Sison CP, Shahid RK, Sheth M, Patel DV, Russo LA. Effect of low-dose warfarin on D-dimer levels during sickle cell vaso-occlusive crisis: a brief report. Eur J Haematol. 2004;72(3):213–216. doi: 10.1111/j.0902-4441.2003.00209.x. Available from: http://dx.doi.org/10.1111/j.0902-4441.2003.00209.x. [DOI] [PubMed] [Google Scholar]
- 12. Qari MH, Aljaouni SK, Alardawi MS, Fatani H, Alsayes FM, Zografos P, Alsaigh M, Alalfi A, Alamin M, Gadi A, Mousa SA. Reduction of painful vaso-occlusive crisis of sickle cell anaemia by tinzaparin in a double-blind randomized trial. Thromb Haemost. 2007;98(2):392–396. doi: 10.1160/TH06-12-0718. Available from: http://dx.doi.org/10.1160/TH06-12-0718. [DOI] [PubMed] [Google Scholar]