Abstract
Background
Valid measurement of physician performance requires accurate identification of patients for whom a physician is responsible. Among all patients seen by a physician, some will be more strongly connected to their physician than others, but the effect of connectedness on measures of physician performance is not known.
Objective
To determine whether patient–physician connectedness affects measures of clinical performance.
Design
Population-based cohort study.
Setting
Academic network of 4 community health centers and 9 hospital-affiliated primary care practices.
Patients
155 590 adults with 1 or more visits to a study practice from 2003 to 2005.
Measurements
A validated algorithm was used to connect patients to either 1 of 181 physicians or 1 of 13 practices in which they received most of their care. Performance measures included breast, cervical, and colorectal cancer screening in eligible patients; hemoglobin A1c measurement and control in patients with diabetes; and low-density lipoprotein cholesterol measurement and control in patients with diabetes and coronary artery disease.
Results
Overall, 92 315 patients (59.3%) were connected to a specific physician, whereas 53 669 patients (34.5%) were connected only to a specific practice and 9606 patients (6.2%) could not be connected to a physician or practice. The proportion of patients in a practice who could be connected to a physician varied markedly (45.6% to 71.2% of patients per practice; P < 0.001). Physician-connected patients were significantly more likely than practice-connected patients to receive guideline-consistent care (for example, adjusted mammography rates were 78.1% vs. 65.9% [P < 0.001] and adjusted hemoglobin A1c rates were 90.3% vs. 74.9% [P < 0.001]). Receipt of preventive care varied more by whether patients were more or less connected to a physician than by race or ethnicity.
Limitation
Patient–physician connectedness was assessed in 1 primary care network.
Conclusion
Patients seen in primary care practices seem to be variably connected with a specific physician, and less connected patients are less likely to receive guideline-consistent care.
Persistent deficiencies exist in the quality of health care in the United States (1– 4). Because primary care physicians are the first source of health care for most patients to receive preventive and chronic illness care, efforts to measure and improve quality of care have often focused on these physicians (5–7). In practice, however, many patients receive episodic care from different physicians (8 –12). Patients without a regular source of care are less likely to receive care consistent with guidelines (13–20). Continuity of care is a shared responsibility between physicians and patients. Even if physicians or practices treated all patients similarly, patients vary in their ability and willingness to adhere to recommendations.
Performance measures originally designed for use in large populations are increasingly used to assess the quality of practices and individual physicians. One concern with this approach is that physicians who care for patients who are less willing or able to adhere to recommendations will seem to perform less well. To investigate this possibility, we developed the concept of physician–patient connectedness. We use the term connectedness to describe the closeness of the relationship between a patient and an individual physician on the basis of a model predicting how likely a physician is to identify a patient as “my patient.” We hypothesized that patients highly connected to a specific physician would be more likely to receive care consistent with guidelines, according to common performance measures. We further hypothesized that differences in connectedness may contribute to health care disparities to the extent that connectedness is correlated with race or ethnicity and insurance status.
We investigated these hypotheses in a network of primary care physicians affiliated with a large teaching hospital. We used a previously developed and validated algorithm (21, 22) to determine the connectedness of more than 150 000 patients with a specific physician. The algorithm used the designated primary care physician field from the practice registration system along with patient age, time since most recent visit, and in-state residence. We then examined variation in the proportion of connected patients among practices and the association of connectedness with the performance of commonly used measures of health care quality.
Methods
Study Setting and Sample
The Massachusetts General Hospital (Boston, Massachusetts) adult primary care network includes 181 primary care physicians working in 13 clinically and demographically diverse practices (4 community health centers and 9 hospital-affiliated practices). The practices use the same electronic billing and scheduling systems, and physicians have the same compensation plan and staffing resources. Patients must designate a primary care physician when registering for care. We identified all patients with a visit to 1 of these practices from 1 January 2003 to 31 December 2005 by using electronic billing records. During this time, 169 024 unique patients were seen for 994 431 visits. We excluded patients if they were younger than 18 years (n = 1924), had died (determined on the basis of review of social security records) (n = 2817), or were registered as having a primary care physician outside of the Massachusetts General Hospital network (n = 8693). The Massachusetts General Hospital institutional review board approved the study.
Connecting Patients With Primary Care Physicians and Practices
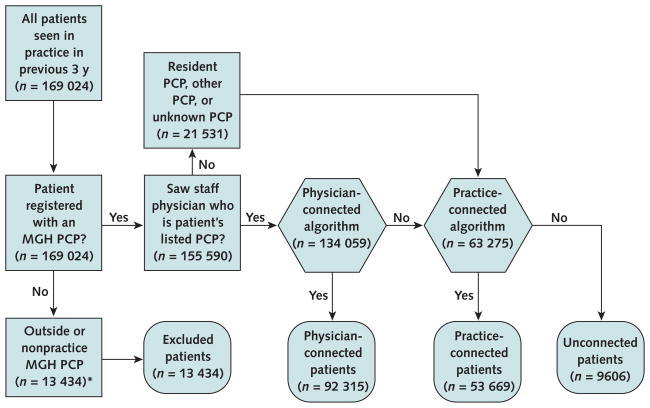
Figure 1 shows the process used to connect patients with a specific physician or practice. We previously developed and validated an algorithm to connect patients with a specific physician by having 18 primary care physicians review a list of all patients seen over 3 years (mean, 1029 patients per physician; range, 226 to 2372 patients per physician) and designate which patients they considered to be “my patient” (21, 22). The algorithm primarily uses the primary care physician designee field from the hospital registration system. However, as a stand-alone variable, its specificity (84.9%) would result in too many patients on a list being incorrectly identified as being connected to that physician (21). As a result, the final algorithm combined the primary care physician designee field with a logistic regression model that included patient age, time since most recent visit, in-state residence, and “physician practice style” (21). We defined the physician practice style variable according to the proportion of all visits by patients registered to the physician. Thus, physicians who were the registered provider for at least 70% of the patients they saw were categorized as following a solo-practice style, whereas physicians who were the registered provider for fewer than 70% of the patients they saw were designated as having a collaborative-practice style. The model variables were designed to provide a highly specific list of patients for a given physician (overall specificity, 93.7%; positive predictive value, 96.5% [range, 90.1% to 100%]) (21).
Figure 1.
Method of connecting patients with specific primary care physicians or practices
MGH = Massachusetts General Hospital; PCP = primary care physician. The square boxes represent the patient population seen in the MGH primary care network and their initial assessment based on listed provider. The hexagonal boxes represent the algorithms that connect patients to a specific physician or practice. The rounded boxes represent the disposition of the primary care population based on patient–physician connectedness.
* Patients younger than 18 years and those who were deceased are also included in this category.
Patients who could not be connected to a specific physician were connected to the primary care practice in which they received most of their care. Patients were not connected to a specific physician because they had a primary care physician in a given practice but did not meet threshold criteria (using the patient–physician connectedness algorithm), were only seen by physicians other than their registered primary care physician, were followed by a resident physician, or received care in a given practice but were not registered with a primary care physician in that practice. Patients who were followed by a resident physician were assigned to the practice in which the resident provided care. We developed criteria for connecting patients to individual practices by consensus in collaboration with physician practice representatives (Table 1). Patients who could not be assigned to either a physician or a practice with these methods were designated as “unconnected.”
Table 1.
Criteria Used to Define Whether Patients Not Connected to a Specific Physician Were Connected to a Specific Primary Care Practice
| Criterion | Response Category* |
|---|---|
| Listed PCP in practice, but not physician connected | |
| Patient age | |
| <40 y | >1 total visit to practice in 3 y |
| ≥40 y | >1 total visit to practice in 2 y |
| Listed PCP in practice who is a resident physician or preceptor | |
| Patient age | |
| <40 y | >1 total visit to practice in 3 y |
| ≥40 y | >1 total visit to practice in 2 y |
| Listed PCP is listed as “none” or “unknown” | |
| Patient age | |
| <40 y | >1 total visit to practice in 2 y |
| ≥40 y | >1 total visit to practice in 1 y |
PCP = primary care physician.
These responses allowed us to connect a patient with the practice in which they receive the most care.
Patient and Provider Characteristics and Performance Measures
We obtained data from an electronic record repository for Massachusetts General Hospital and affiliated institutions (23). Available patient characteristics included date of birth, sex, race or ethnicity, primary language spoken, insurance status, number of outpatient office visits during the previous 3 years, and months since most recent out-patient visit. We obtained physician characteristics (age, sex, practice location, and years since medical school graduation) from the hospital registrar database.
Physician performance measures focused on cancer screening and chronic disease management. Cancer screening measures were mammography for women age 42 to 69 years in the previous 2 years and without previous bilateral mastectomy; Papanicolaou cervical screening in the previous 3 years for women age 21 to 64 years without hysterectomy; and colonoscopy within 10 years, sigmoidoscopy or double-contrast barium enema within 5 years, or home fecal occult blood testing within 1 year for patients age 52 to 69 years without total colectomy. For patients with diabetes, we assessed 2 measures: hemoglobin A1c (HbA1c) and low-density lipoprotein cholesterol measured in the previous year (24). For patients with coronary artery disease, we assessed low-density lipoprotein cholesterol measured in the previous year (25). For persons who had HbA1c and low-density lipoprotein cholesterol testing, we also assessed the most recent value available and categorized HbA1c level as less than 8.0% or not and low-density lipoprotein cholesterol level as less than 2.59 mmol/L (<100 mg/dL) or not (26). We extracted data for these measures from electronic laboratory and imaging reports or billing data within the Partners Healthcare System on the basis of Healthcare Effectiveness Data and Information Set criteria (27).
Statistical Analysis
We first grouped patients by connectedness status and compared characteristics of physician-connected, practice-connected, and unconnected patients. To account for the repeated measures of patients from the same physician, we used generalized estimating equations techniques with compound symmetry correlation structure (PROC GENMOD [SAS, version 9.1.3, SAS Institute, Cary, North Carolina]) (28) in all statistical analyses for clustering effects. The physician was considered as the unit of cluster for physician-connected patients, and each patient was considered as an individual cluster for practice-connected patients. Because of the variability among practices, we included practice as a fixed effect in each model. Chart review revealed that many unconnected patients were transitioning in or out of the primary care network (unpublished data). Because we could not obtain performance measures done outside of our network for most of these transitional patients, we excluded this group from further analyses. We then compared proportions of completed performance tests among physician-connected and practice-connected patients. We also included patient age, sex (when applicable), race or ethnicity, insurance status, and number of practice visits over 3 years in the models to adjust for potential confounders. We assessed comorbid conditions by using the Charlson Comorbidity Index from medical problems listed in the patient’s electronic medical record (excluding 1 practice for which this information was unavailable) (29).
We did many secondary analyses to examine the effect of connectedness on clinical performance measures in relevant subpopulations. First, because commercial managed care plans require patients to select a primary care physician and patients may have fewer cost barriers to obtaining care, we assessed outcomes in those who were commercially insured. Second, because of the strong association between the number of practice visits during 3 years and patient–physician connectedness, we stratified outcomes on the basis of the number of practice visits among eligible patients into high, middle, and low tertiles. Third, we stratified outcomes by patient race or ethnicity because initial analyses showed that this variable was strongly associated with patient connectedness. Fourth, we examined chronic disease management outcomes in patients who had a visit to the physician or practice in the past year to exclude persons who may have primarily received their chronic disease care outside of our practice network. Fifth, we examined the effect of connectedness when patients of resident physicians were excluded because they may provide different quality of care from established attending physicians. Sixth, we compared models with and without the Charlson Comorbidity Index to determine whether adjusted results were affected by differences in patients with comorbid conditions. Finally, we excluded patients (n = 2173) of physicians who joined or left the network during the study period (transitioning physicians).
Role of the Funding Source
The National Cancer Institute and the Massachusetts General Hospital Primary Care Operations Improvement Program provided funding for the study. The funding sources had no role in the design, data collection, analysis, interpretation, implementation, or conduct of the study; drafting, revision, or approval of the manuscript; or the decision to submit the manuscript for publication.
Results
Physician and Practice Characteristics
The 181 primary care physicians in our 13-practice network had been physicians for approximately 20 years (median, 18 years); 48.1% were women, and 64.1% practiced in a collaborative-practice style. Twenty-nine transitioning physicians had an average panel of 75 physician-connected patients (range, 1 to 366), whereas the remaining 152 physicians had an average panel of 593 physician-connected patients (range, 22 to 2297). Resident physicians cared for 6.6% of patients seen in these practices.
Patient Characteristics
Of 155 590 eligible patients, 92 315 (59.3%) were connected to a specific primary care physician (physician-connected), 53 669 (34.5%) were connected to a specific practice (practice-connected), and 9606 (6.2%) could not be assigned to either a physician or a practice (unconnected). Patient characteristics varied significantly by connectedness (Table 2). Physician-connected patients were significantly older; were more likely to be women, non-Hispanic white, and English speaking; and had significantly higher Charlson Comorbidity Index scores than practice-connected patients (P < 0.001). Physician-connected patients were much more likely to be insured by a managed care plan or Medicare, whereas practice-connected or unconnected patients were more likely to be either uninsured or insured by Medicaid (P < 0.001).
Table 2.
Patient Characteristics, by Patient Connectedness*
| Patient Characteristic | Physician-Connected Patients (n = 92 315) | Practice-Connected Patients (n = 53 669) | Unconnected Patients (n = 9606) |
|---|---|---|---|
| Age, y | |||
| Mean (SD) | 52.0 (16.4) | 39.9 (15.0) | 51.6 (15.1) |
| Median | 51 | 36 | 49 |
| Women, n (%) | 53 612 (58.1) | 30 402 (56.6) | 4744 (49.4) |
| Race or ethnicity, n (%) | |||
| Non-Hispanic white | 74 914 (81.2) | 37 280 (69.5) | 6467 (67.3) |
| Hispanic | 6436 (7.0) | 6013 (11.2) | 1218 (12.7) |
| Black | 4358 (4.7) | 3517 (6.5) | 610 (6.4) |
| Asian | 3788 (4.1) | 3013 (5.6) | 368 (3.8) |
| Other | 1654 (1.8) | 2244 (4.2) | 433 (4.5) |
| Unknown | 1165 (1.3) | 1602 (3.0) | 510 (5.3) |
| English as a primary language, n (%) | 86 441 (93.6) | 48 342 (90.1) | 8345 (86.9) |
| Insurance status, n (%) | |||
| Commercial health insurance | 63 950 (69.3) | 36 788 (68.5) | 5634 (58.7) |
| Managed care plan | 34 188 (37.0) | 12 368 (23.0) | 866 (9.0) |
| Government insurance | 23 413 (25.4) | 9432 (17.6) | 2137 (22.2) |
| Medicare | 17 920 (19.4) | 4586 (8.5) | 1408 (14.7) |
| Medicare with secondary Medicaid | 3513 (3.8) | 1469 (2.7) | 398 (4.1) |
| Medicaid | 5493 (6.0) | 4846 (9.0) | 729 (7.6) |
| No insurance, self-pay | 4952 (5.4) | 7449 (13.9) | 1835 (19.1) |
| Time since last physician visit, mo | |||
| Mean (SD) | 4.4 (4.3) | 13.4 (9.5) | 29.0 (5.2) |
| Median | 2.9 | 11.3 | 29.7 |
| Practice visits in the past 3 y, n† | |||
| Mean (SD) | 7.7 (6.3) | 4.2 (4.1) | 2.0 (1.7) |
| Median | 6.0 | 3.0 | 1.0 |
| Charlson Comorbidity Index score‡ | 7411 | ||
| Patients with score, n | 68 206 | 43 473 | |
| Mean score (SD) | 0.7 (1.2) | 0.4 (0.9) | 0.3 (0.8) |
All P values <0.05 comparing patient-connectedness groups.
Any visit to the patient’s primary care physician, another physician, nurse practitioner, or registered nurse.
Among the 12 practices with problem list information available.
Variation in Connectedness Among Practices
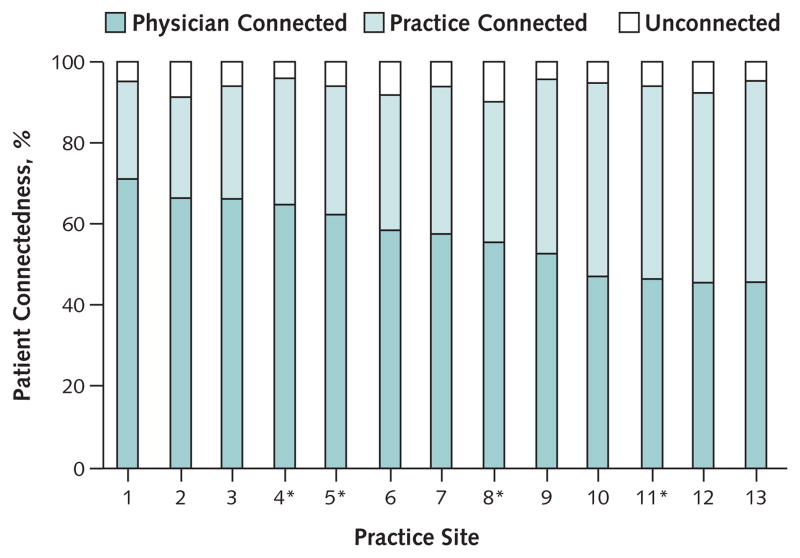
Figure 2 shows the proportion of physician-connected patients for each of the 13 primary care practices. The percentage of physician-connected (45.6% to 71.2%), practice-connected (24.0% to 49.8%), and unconnected (4.2% to 9.7%) patients varied considerably across practices (P < 0.001). Patients seen in community health centers were less likely to be connected to a physician than patients seen in private practices (56.8% and 60.4%, respectively; P < 0.001).
Figure 2.
Patient connectedness in the 13 practice sites
*Community health center.
Performance Measures and Physician Connectedness
Adjusted cancer screening rates were significantly higher for physician-connected patients (P < 0.001) (Table 3). For example, mammography was done among eligible women in 78.1% of physician-connected patients and 65.9% of practice-connected patients. These results did not change when we excluded patients of transitioning physicians or resident physicians or when the model included a variable controlling for the Charlson Comorbidity Index. However, there was an interaction between Charlson score and patient–physician connectedness, with a larger difference in performance measures between physician-connected patients and practice-connected patients for patients with a Charlson score of 0 than for those with a score of 1 or more.
Table 3.
Performance Measures Among Physician-Connected and Practice-Connected Patients
| Performance Measure | Physician-Connected Patients |
Practice-Connected Patients |
|||
|---|---|---|---|---|---|
| Patients with Event/Patients at Risk, n/n (%) | Adjusted Percentage (95% CI) | Patients with Event/Patients at Risk, n/n (%) | Adjusted Percentage (95% CI) | P Value* | |
| Total patients | |||||
| Cancer screening | |||||
| Breast (mammography)† | 22 221/28 439 (78.1) | 78.1 (77.0–79.2) | 4578/7426 (61.6) | 65.9 (64.7–67.1) | <0.001 |
| Cervical (Pap smear)‡ | 33 215/39 087 (85.0) | 86.4 (85.0–87.8) | 20 469/26 773 (76.5) | 80.2 (79.3–81.1) | <0.001 |
| Colorectal§ | 22 333/31 215 (71.5) | 72.1 (70.5–73.7) | 3460/6453 (53.6) | 58.0 (56.7–59.4) | <0.001 |
| Chronic disease management¶ | |||||
| Diabetes mellitus | |||||
| HbA1c measurement in past year | 6684/7556 (88.5) | 90.3 (89.2–91.2) | 1362/2076 (65.6) | 74.9 (72.3–77.3) | <0.001 |
| HbA1c level <8% | 4942/6684 (73.9) | 74.7 (73.4–76.0) | 922/1362 (67.7) | 70.5 (67.8–73.0) | 0.004 |
| LDL cholesterol monitoring in past year | 6224/7556 (82.4) | 83.2 (81.6–84.7) | 1191/2076 (57.4) | 61.2 (58.7–63.6) | <0.001 |
| LDL level <2.59 mmol/L (<100 mg/dL) | 4144/6224 (66.6) | 66.4 (64.9–67.9) | 768/1191 (64.5) | 67.2 (64.3–70.0) | 0.64 |
| Coronary artery disease | |||||
| LDL cholesterol monitoring in past year | 4311/5341 (80.7) | 81.7 (79.8–83.5) | 765/1271 (60.2) | 61.2 (58.7–63.6) | <0.001 |
| LDL cholesterol level <2.59 mmol/L (<100 mg/dL) | 3294/4311 (76.4) | 77.0 (75.7–78.4) | 570/765 (74.5) | 77.6 (74.4–80.5) | 0.74 |
| Patients with commercial managed care insurance | |||||
| Cancer screening | |||||
| Breast (mammography)† | 10 205/11 906 (85.7) | 86.5 (85.6–87.4) | 1395/1854 (75.2) | 80.8 (78.8–82.7) | <0.001 |
| Cervical (Pap smear)‡ | 16 308/18 142 (89.9) | 90.6 (89.7–91.5) | 6041/6847 (88.2) | 90.0 (89.0–90.9) | 0.37 |
| Colorectal§ | 9437/12 291 (76.8) | 77.1 (75.4–78.6) | 803/1235 (65.0) | 69.5 (66.6–72.2) | <0.001 |
| Chronic disease management¶ | |||||
| Diabetes mellitus | |||||
| HbA1c measurement in past year | 1392/1569 (88.7) | 95.3 (93.6–96.6) | 121/186 (65.1) | 92.1 (87.5–95.2) | 0.014 |
| HbA1c level <8% | 1011/1392 (72.6) | 78.7 (75.6–81.5) | 77/121 (63.6) | 75.4 (65.9–82.9) | 0.39 |
| LDL cholesterol monitoring in past year | 1350/1569 (86.0) | 91.5 (89.5–93.2) | 104/186 (55.9) | 80.7 (73.0–86.7) | <0.001 |
| LDL cholesterol level <2.59 mmol/L (<100 mg/dL) | 861/1350 (63.8) | 68.8 (65.6–71.9) | 61/104 (58.7) | 72.6 (62.2–81.0) | 0.43 |
| Coronary artery disease | |||||
| LDL cholesterol monitoring in past year | 732/842 (86.9) | 93.1 (89.7–95.4) | 60/74 (81.1) | 93.5 (85.8–97.2) | 0.86 |
| LDL cholesterol level <2.59 mmol/L (<100 mg/dL) | 539/732 (73.6) | 77.7 (73.0–81.9) | 37/60 (61.7) | 72.4 (58.2–83.1) | 0.36 |
HbA1c = hemoglobin A1c; LDL = low-density lipoprotein; Pap = Papanicolaou.
P values compare patient-connectedness groups, controlling for age, sex (if relevant), insurance status, ethnicity, practice, and number of practice visits over 3 years using logistic regression models with generalized estimating equations methods for cluster adjustment.
Mammography done during the previous 2 years in eligible women age 42 to 69 years without bilateral mastectomy.
Pap smear done during the previous 3 years in eligible women age 21 to 64 years without hysterectomy.
Colorectal cancer screening test done in all patients age 52 to 69 years without colectomy: colonoscopy in the previous 10 years, flexible sigmoidoscopy or double-contrast barium enema in the previous 5 years, or fecal occult blood testing in the previous year.
Among the total population with the chronic condition.
Among 9632 diabetic patients, adjusted HbA1c screening rates were significantly higher in physician-connected patients (90.3% vs. 74.9%; P < 0.001) (Table 3). We found similar results for low-density lipoprotein cholesterol testing, although overall rates were lower (83.2% vs. 61.2%; P < 0.001). For patients who had testing done, more physician-connected patients had HbA1c scores less than 8.0% (74.7% vs. 70.5%, P = 0.004), but the adjusted percentage with low-density lipoprotein cholesterol levels less than 2.59 mmol/L (<100 mg/dL) were similar among physician-connected and practice-connected patients. Among 6612 patients with coronary artery disease, low-density lipoprotein cholesterol levels less than 2.59 mmol/L (<100 mg/dL) were again significantly higher for physician-connected than practice-connected patients (81.7% vs. 61.2%; P < 0.001), but the adjusted percentage with low-density lipoprotein cholesterol values less than 2.59 mmol/L (<100 mg/dL) did not differ by connectedness. Examining only patients who had a visit to the physician or practice in the past year did not change our findings. Excluding patients of resident physicians in most cases further reduced the rates for the practice-connected group, whereas excluding patients of transitional physicians slightly increased rates for the physician-connected group.
Performance Measures for Managed Care Patients
When we limited the analysis to patients with commercial managed care insurance (n = 47 422 [30.5%]), we found smaller differences, but several were still clinically and statistically significant (Table 3). For example, colorectal cancer screening was done in 77.1% of eligible physician-connected patients and 69.5% of practice-connected patients (P < 0.001). However, for cervical cancer screening, the absolute difference was small (90.6% vs. 90.0% for physician- and practice-connected patients, respectively) and not statistically significant (P = 0.37). Among patients with diabetes (n = 1755), rates of HbA1c and low-density lipoprotein cholesterol screening were significantly higher in physician-connected patients, but the percentage who achieved specified levels was similar.
Patient–Physician Connectedness and Visit Frequency
To examine whether the effect of physician connectedness on performance measures was independent of visit frequency, we examined outcomes stratified across tertiles of practice visits (Table 4). Adjusted cancer screening rates were significantly higher for physician-connected patients than for practice-connected patients within each visit tertile. Similarly, for patients with diabetes or coronary artery disease, screening rates were significantly higher for physician-connected patients within each visit tertile.
Table 4.
Performance Measures Among Physician-Connected and Practice-Connected Patients, by Tertile of Practice Visits
| Performance Measure | Tertile of Practice Visits |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| High |
Middle |
Low |
|||||||
| Physician- Connected Patients |
Practice- Connected Patients |
Adjusted P Value* | Physician- Connected Patients |
Practice- Connected Patients |
Adjusted P Value* | Physician- Connected Patients |
Practice- Connected Patients |
Adjusted P Value* | |
| Cancer screening rate (95% CI), % | |||||||||
| Breast (mammography)† | 82.8 (81.6–83.9) | 77.4 (75.2–79.4) | <0.001 | 79.8 (78.6–81.0) | 68.8 (66.4–71.2) | < 0.001 | 69.4 (67.8–70.9) | 54.8 (53.2–56.5) | <0.001 |
| Cervical (Pap smear)‡ | 91.3 (90.4–92.2) | 89.9 (89.0–90.7) | 0.033 | 87.3 (86.0–88.5) | 85.0 (84.1–85.9) | 0.009 | 75.1 (73.2–76.9) | 67.5 (66.6–68.4) | <0.001 |
| Colorectal§ | 78.0 (76.4–79.6) | 71.2 (68.5–73.6) | <0.001 | 72.0 (70.4–73.7) | 61.2 (58.3–64.0) | < 0.001 | 61.3 (59.2–63.4) | 45.2 (43.4–46.9) | <0.001 |
| Chronic disease management rate (95% CI), %¶ | |||||||||
| Diabetes mellitus** | |||||||||
| HbA1c measurement in past year | 96.2 (95.1–97.0) | 86.2 (81.9–89.6) | <0.001 | 90.2 (89.0–91.4) | 74.6 (70.5–78.4) | < 0.001 | 77.1 (74.6–79.4) | 51.5 (48.1–54.8) | <0.001 |
| LDL cholesterol monitoring in past year | 88.9 (87.0–90.5) | 76.8 (72.0–81.1) | <0.001 | 83.6 (81.7–85.4) | 64.3 (59.9–68.5) | < 0.001 | 72.9 (70.2–75.4) | 45.8 (42.4–49.2) | <0.001 |
| Coronary artery disease†† | |||||||||
| LDL cholesterol monitoring in past year | 88.1 (85.5–90.3) | 75.1 (69.5–80.0) | <0.001 | 82.2 (79.5–84.7) | 66.7 (60.7–72.2) | < 0.001 | 72.4 (69.6–75.1) | 48.1 (43.9–52.3) | <0.001 |
HbA1c = hemoglobin A1c; LDL = low-density lipoprotein; Pap = Papanicolaou.
P values compare patient-connectedness groups, controlling for age, sex (if relevant), insurance status, ethnicity, practice, and number of practice visits over 3 years using logistic regression models with generalized estimating equations methods for cluster adjustment.
Mammography done during the previous 2 years in eligible women age 42 to 69 years without bilateral mastectomy. The number of practice visits for patients eligible for mammography was stratified into low (≤4 visits), middle (>4 and ≤7 visits), and high (>7 visits) tertiles.
Pap smear done during the previous 3 years in eligible women age 21 to 64 years without hysterectomy. The number of practice visits for patients eligible for Pap smears was stratified into low (≤3 visits), middle (>3 and ≤6 visits), and high (>6 visits) tertiles.
Colorectal cancer screening test in all patients age 52 to 69 years without total colectomy: colonoscopy in the previous 10 years, flexible sigmoidoscopy or double-contrast barium enema in the previous 5 years, or fecal occult blood testing in the previous year. The number of practice visits for patients eligible for colorectal cancer screening was stratified into low (≤4 visits), middle (>4 and ≤7 visits), and high (>7 visits) tertiles.
Among the total population with the chronic condition.
The number of practice visits for patients with diabetes mellitus was stratified into low (≤7 visits), middle (>7 and ≤13 visits), and high (>13 visits) tertiles.
The number of practice visits for patients with coronary artery disease was stratified into low (≤6 visits), middle (>6 and ≤11 visits), and high (>11 visits) tertiles.
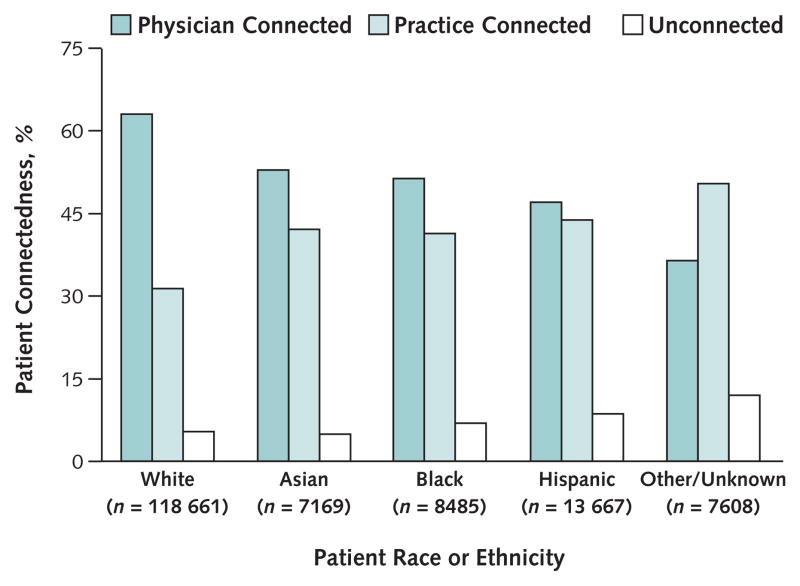
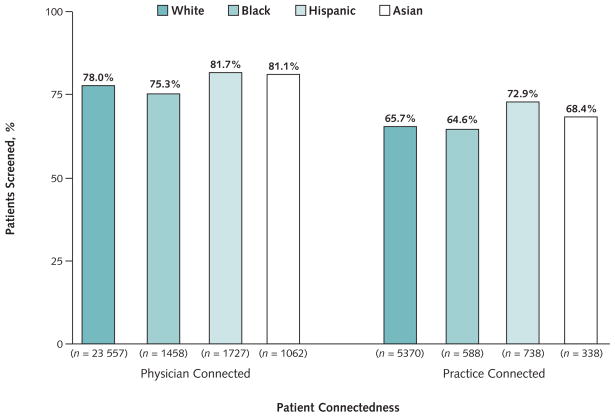
Race and Ethnicity
Racial and ethnic minorities were less likely than non-minority patients to be physician-connected (Figure 3) and less likely to receive guideline-adherent care by our performance measures. Overall, disparities in performance measures were much greater by patient–physician connectedness status within race or ethnic category than the differences across race or ethnicity categories (Figure 4). For example, for breast cancer screening rates, the magnitude of the disparity between non-Hispanic white and black women was smaller (absolute difference, 2.7% in physician-connected patients and 1.1% in practice-connected patients) compared with that between physician-connected and practice-connected women (absolute difference, 12.3% for non-Hispanic white women and 10.7% for black women). Similarly, for colon cancer screening, the magnitude of the disparity between non-Hispanic white patients and black patients was minimal (absolute difference, 1.1% in physician-connected and −0.1% in practice-connected patients) compared with that between physician-connected and practice-connected persons (absolute difference, 13.8% for non-Hispanic white patients and 12.6% for black patients).
Figure 3.
Patient connectedness, by race or ethnicity.
Figure 4.
Breast cancer screening rates, by patient connectedness and by race or ethnicity
Adjusted rates of breast cancer screening with mammography in the previous 2 years among eligible women age 42 to 69 years.
Discussion
We examined the relationship between physician connectedness and measures of physician performance by categorizing all patients seen in a large primary care network on the basis of their connectedness to a specific primary care physician. Our results indicate that many patients did not have a close continuous relationship with their designated primary care physician, the prevalence of physician-connected patients was variably distributed between practices, patients without a close relationship with a specific physician were less likely to complete recommended testing for preventive and chronic illness care, and differences in performance measures by race or ethnicity were smaller than differences in patient–physician connectedness within racial or ethnic groups. Controlling for patient–physician connectedness attenuated some differences among racial and ethnic groups in the receipt of guideline-recommended care.
Most definitions of primary care include reference to a continuous longitudinal relationship (5, 30). Although patients may have different preferences for continuous longitudinal relationships, with some patients preferring to avoid this type of arrangement altogether, primary care physicians can do much to promote greater connectedness with their patients (31–33). Nonetheless, a close continuous relationship requires the active participation of both the patient and the physician. We developed a novel method to define how closely patients were connected to physicians. This method used a prediction model that was based on the physician’s assessment, regardless of whether patients having office visits with them actually belonged in their panel. Although similar to measures of continuity (15, 17, 18, 32), our measure differed because it was validated against physicians’ assessments of who they considered to be “my patient.” Our measure was also based on data obtained as part of usual care and can therefore be applied routinely to categorize all patients seen in a network. The validation did not ask the physician to identify their adherent patients but rather to identify all of the patients in their panel (21). Although this method has some distinct and important limitations, the results suggest that physician connectedness may play an important role in understanding measures of physician performance.
Among the more striking findings of our study was the extent to which patients who were connected to a specific physician were more likely to receive guideline-recommended care than patients who were not connected to a specific physician. This finding is consistent with previous studies that demonstrated the benefit of a regular source of care on the likelihood of received guideline-recommended care (14, 15, 19, 34, 35). However, studies comparing patients with and without a regular physician show better access to care (17, 18, 36, 37) but less consistent results on guideline-recommended care (38–41). In addition, almost all studies examining continuity of care have used patient survey data for determining continuity of care. Thus, while useful for addressing health policy questions, such patient-derived measures would be difficult for health care systems to apply to their large patient populations for ongoing quality assessment and improvement programs.
Patients who were connected to a physician were more likely have insurance, speak English, and be non-Hispanic white. This strong relationship between patient–physician connectedness and race or ethnicity suggests that disparities in care may be mediated in part by the degree of connectedness to primary care physicians (42, 43). While some residual differences remained between groups, we found that connectedness was associated with larger disparities in screening rates than was race or ethnicity. The process of establishing a strong relationship with a specific physician may represent an important key to understanding disparities in care (13). Greater insight into the role of patient-, provider-, or practice-level barriers to establishing a closely connected primary care relationship may lead to improved quality of care for vulnerable patients (44).
The primary care physician is a key target of quality improvement efforts, such as pay-for-performance (45–47). A key assumption in such programs is that patients who prefer not to (or cannot) follow a physician’s recommendations will be relatively equally distributed among physicians or practices. We found that the proportion of patients who were connected to physicians varied widely among practices. This variation may reflect differences in practice organization, physician practice styles, or patient characteristics. Because all our practices have a uniform management structure with integrated administrative and clinical information systems and nearly all our physicians have closed panels, variation in practice structure probably contributed little to the observed variation in patient connectedness. All physicians in our network receive reminders when patients are due and overdue for all of the measures used in this study. In addition, practice-based nurses call commercially insured patients and encourage them to complete these recommended tests. Despite all of these systems designed to decrease variation, we found the same association between physician connectedness and performance of guideline-recommended care in the subpopulation of commercially insured patients.
The association of connectedness with performance measures underscores the importance of accurately defining the eligible (or “denominator”) patient population for quality measurement. As demonstrated in our analysis, many patients receive episodic care from different providers without necessarily establishing a strong relationship with any 1 provider, even their listed primary care physician (48, 49). Pay-for-performance initiatives are based on the ability to accurately assign performance measures to practitioners who have some control over the outcome. Our results suggest that physicians with a relatively low percentage of connected patients are likely to receive lower scores on performance measures than physicians with a higher proportion of connected patients. If connectedness is determined in part by patient rather than just physician or practice characteristics, the disproportionate effect of connectedness on performance measurement may penalize physicians and practices caring for vulnerable populations with lower rates of physician connectedness. The potential result may be to direct resources away from those who care for populations with lower performance scores based on the patient’s ability or willingness to establish a long-term connection with a physician rather than the physician or practice’s efforts (7).
Our results must be interpreted in the context of the study design. We did our study in 1 practice network, and our findings require confirmation in other settings. Although the concept of continuity of care is well established (5), including continuity with a regular physician, the approach we used to measure patient–physician connectedness is relatively novel and is but 1 of several possible methods. For example, we based physician connectedness on a physician-derived standard, but other standards (for example, patient-derived) could also be used (50). Simpler models to designate connectedness may also be possible, especially in more homogeneous care delivery settings. Nonetheless, the association of better performance with closer physician connection will probably remain robust by any valid measure of connectedness. Physician connectedness was strongly associated with visit frequency, and higher visit frequency is associated with better results on performance measures. However, when examined within strata of similar visit frequency, physician-connected patients continued to have improved outcomes. This argues that the concept of connectedness is more than simply a reflection of how often a patient is seen. Because we had limited access to tests obtained outside of our network, we may have underreported performance measures, particularly for patients with less physician connectedness. For this reason, we did not assess performance measures in unconnected patients. Nonetheless, we are informed of all tests, even those conducted outside our system, for our commercially insured patients. Finally, we did not collect data directly from patients and physicians and thus cannot report on the underlying reasons for the differences observed.
The concept of connectedness and its relationship to performance measures suggest strategies to efficiently organize quality-improvement interventions. Although one could simply hold physicians and practices accountable for assuring connectedness, this does not address relevant patient preferences. Alternatively, strategies could be implemented that take advantage of established connectedness patterns. For example, for patients closely connected to a single primary care physician, complex quality-improvement tasks, such as changing medications on the basis of laboratory test results, can be designed that rely on the physician as the “care catalyst” (51). For patients who are not connected to a specific physician, organizational redesign that uses nonphysician case managers as an alternative to strong patient–physician connectedness may be an efficient model of care (15, 19, 52, 53).
In summary, many patients in a large adult primary care network were not closely connected to a specific primary care physician. The proportion of physician-connected patients varied considerably among practices and was strongly associated with the completion of recommended tests. In addition, patient characteristics, such as race or ethnicity, were associated with physician connectedness and with completion of recommended care.
Context
Continuity of care is a basic tenet of high-quality primary care, but the relationship between quality of care and the connection between patient and physician has not been rigorously studied.
Contribution
The researchers defined whether 155 590 adults in a primary care network received most of their care from a specific physician, practice, or neither. Patients who were connected to a particular physician were more likely to have received recommended care than patients who were connected to a practice but not a physician.
Caution
The study involved only 1 network, which is one of many potential definitions of continuity, and selected quality measures.
—The Editors
Acknowledgments
The authors thank Jeffrey Ashburner, MPH, for manuscript preparation and statistical analyses.
Grant Support: By the National Cancer Institute (grant NCI 1 R21 CA121908) and institutional funding from the Massachusetts General Hospital Primary Care Operations Improvement Program. Dr. Grant is supported by a National Institute of Diabetes and Digestive and Kidney Diseases Career Development Award (K23 DK067452), and Dr. Ferris was supported in part by the Agency for Healthcare Research and Quality (grant 5R01 HS015002).
Funding: National Cancer Institute.
Footnotes
Potential Financial Conflicts of Interest: None disclosed.
Reproducible Research Statement: Study protocol: Patient–physician connected algorithm and methods available from Dr. Atlas (satlas@partners.org). Statistical code: Available from Dr. Atlas (satlas@partners.org). Data set: Not available.
Author Contributions: Conception and design: S.J. Atlas, R.W. Grant, T.G. Ferris, M.J. Barry.
Analysis and interpretation of the data: S.J. Atlas, R.W. Grant, T.G. Ferris, Y. Chang, M.J. Barry.
Drafting of the article: S.J. Atlas, T.G. Ferris.
Critical revision of the article for important intellectual content: R.W. Grant, T.G. Ferris, M.J. Barry.
Final approval of the article: S.J. Atlas, R.W. Grant, T.G. Ferris, Y. Chang, M.J. Barry.
Provision of study materials or patients: S.J. Atlas.
Statistical expertise: Y. Chang.
Obtaining of funding: S.J. Atlas, M.J. Barry.
Administrative, technical, or logistic support: M.J. Barry.
References
- 1.Ma J, Stafford RS. Quality of US outpatient care: temporal changes and racial/ethnic disparities. Arch Intern Med. 2005;165:1354–61. doi: 10.1001/archinte.165.12.1354. [DOI] [PubMed] [Google Scholar]
- 2.Chassin MR, Galvin RW. The urgent need to improve health care quality. Institute of Medicine National Roundtable on Health Care Quality. JAMA. 1998;280:1000–5. doi: 10.1001/jama.280.11.1000. [DOI] [PubMed] [Google Scholar]
- 3.Schuster MA, McGlynn EA, Brook RH. How good is the quality of health care in the United States? Milbank Q. 1998;76:517–63. 509. doi: 10.1111/1468-0009.00105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The quality of health care delivered to adults in the United States. N Engl J Med. 2003;348:2635–45. doi: 10.1056/NEJMsa022615. [DOI] [PubMed] [Google Scholar]
- 5.Starfield B. Primary Care: Concept, Evaluation, and Policy. New York: Oxford Univ Pr; 1992. [Google Scholar]
- 6.Landon BE, Normand SL, Blumenthal D, Daley J. Physician clinical performance assessment: prospects and barriers. JAMA. 2003;290:1183–9. doi: 10.1001/jama.290.9.1183. [DOI] [PubMed] [Google Scholar]
- 7.Casalino LP, Alexander GC, Jin L, Konetzka RT. General internists’ views on pay-for-performance and public reporting of quality scores: a national survey. Health Aff (Millwood) 2007;26:492–9. doi: 10.1377/hlthaff.26.2.492. [DOI] [PubMed] [Google Scholar]
- 8.Bohmer R. The rise of in-store clinics—threat or opportunity? N Engl J Med. 2007;356:765–8. doi: 10.1056/NEJMp068289. [DOI] [PubMed] [Google Scholar]
- 9.Cherry DK, Burt CW, Woodwell DA. National Ambulatory Medical Care Survey: 2001 summary. Adv Data. 2003:1–44. [PubMed] [Google Scholar]
- 10.Pham HH, Schrag D, O’Malley AS, Wu B, Bach PB. Care patterns in Medicare and their implications for pay for performance. N Engl J Med. 2007;356:1130–9. doi: 10.1056/NEJMsa063979. [DOI] [PubMed] [Google Scholar]
- 11.Forrest CB, Shi L, von Schrader S, Ng J. Managed care, primary care, and the patient-practitioner relationship. J Gen Intern Med. 2002;17:270–7. doi: 10.1046/j.1525-1497.2002.10309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hargraves JL, Hadley J. The contribution of insurance coverage and community resources to reducing racial/ethnic disparities in access to care. Health Serv Res. 2003;38:809–29. doi: 10.1111/1475-6773.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Baker DW, Stevens CD, Brook RH. Regular source of ambulatory care and medical care utilization by patients presenting to a public hospital emergency department. JAMA. 1994;271:1909–12. [PubMed] [Google Scholar]
- 14.Ettner SL. The timing of preventive services for women and children: the effect of having a usual source of care. Am J Public Health. 1996;86:1748–54. doi: 10.2105/ajph.86.12.1748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bindman AB, Grumbach K, Osmond D, Vranizan K, Stewart AL. Primary care and receipt of preventive services. J Gen Intern Med. 1996;11:269–76. doi: 10.1007/BF02598266. [DOI] [PubMed] [Google Scholar]
- 16.Sox CH, Dietrich AJ, Tosteson TD, Winchell CW, Labaree CE. Periodic health examinations and the provision of cancer prevention services. Arch Fam Med. 1997;6:223–30. doi: 10.1001/archfami.6.3.223. [DOI] [PubMed] [Google Scholar]
- 17.Sox CM, Swartz K, Burstin HR, Brennan TA. Insurance or a regular physician: which is the most powerful predictor of health care? Am J Public Health. 1998;88:364–70. doi: 10.2105/ajph.88.3.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ettner SL. The relationship between continuity of care and the health behaviors of patients: does having a usual physician make a difference? Med Care. 1999;37:547–55. doi: 10.1097/00005650-199906000-00004. [DOI] [PubMed] [Google Scholar]
- 19.DeVoe JE, Fryer GE, Phillips R, Green L. Receipt of preventive care among adults: insurance status and usual source of care. Am J Public Health. 2003;93:786–91. doi: 10.2105/ajph.93.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Pirraglia PA, Sanyal P, Singer DE, Ferris TG. Depressive symptom burden as a barrier to screening for breast and cervical cancers. J Womens Health (Larchmt) 2004;13:731–8. doi: 10.1089/jwh.2004.13.731. [DOI] [PubMed] [Google Scholar]
- 21.Atlas SJ, Chang Y, Lasko TA, Chueh HC, Grant RW, Barry MJ. Is this “my” patient? Development and validation of a predictive model to link patients to primary care providers. J Gen Intern Med. 2006;21:973–8. doi: 10.1111/j.1525-1497.2006.00509.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lasko TA, Atlas SJ, Barry MJ, Chueh HC. Automated identification of a physician’s primary patients. J Am Med Inform Assoc. 2006;13:74–9. doi: 10.1197/jamia.M1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Murphy SN, Chueh HC. A security architecture for query tools used to access large biomedical databases. Proc AMIA Symp. 2002:552–6. [PMC free article] [PubMed] [Google Scholar]
- 24.Grant RW, Cagliero E, Sullivan CM, Dubey AK, Estey GA, Weil EM, et al. A controlled trial of population management: diabetes mellitus: putting evidence into practice (DM-PEP) Diabetes Care. 2004;27:2299–305. doi: 10.2337/diacare.27.10.2299. [DOI] [PubMed] [Google Scholar]
- 25.DeFaria Yeh D, Freeman MW, Meigs JB, Grant RW. Risk factors for coronary artery disease in patients with elevated high-density lipoprotein cholesterol. Am J Cardiol. 2007;99:1–4. doi: 10.1016/j.amjcard.2006.07.053. [DOI] [PubMed] [Google Scholar]
- 26.Saydah SH, Fradkin J, Cowie CC. Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA. 2004;291:335–42. doi: 10.1001/jama.291.3.335. [DOI] [PubMed] [Google Scholar]
- 27.National Committee for Quality Assurance. HEDIS and quality measurement. Washington, DC: National Committee for Quality Assurance; 2007. [4 October 2007]. Accessed at web.ncqa.org/tabid/59/Default.aspx. [Google Scholar]
- 28.Zeger SL, Liang KY. Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986;42:121–30. [PubMed] [Google Scholar]
- 29.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 30.Institute of Medicine, Committee on the Future of Primary Care. Primary Care: America’s Health in a New Era. Washington, DC: National Academies Pr; 1996. [Google Scholar]
- 31.Murphy J, Chang H, Montgomery JE, Rogers WH, Safran DG. The quality of physician-patient relationships. Patients’ experiences 1996–1999. J Fam Pract. 2001;50:123–9. [PubMed] [Google Scholar]
- 32.Rodriguez HP, Rogers WH, Marshall RE, Safran DG. The effects of primary care physician visit continuity on patients’ experiences with care. J Gen Intern Med. 2007;22:787–93. doi: 10.1007/s11606-007-0182-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Safran DG, Montgomery JE, Chang H, Murphy J, Rogers WH. Switching doctors: predictors of voluntary disenrollment from a primary physician’s practice. J Fam Pract. 2001;50:130–6. [PubMed] [Google Scholar]
- 34.Bernstein AB, Thompson GB, Harlan LC. Differences in rates of cancer screening by usual source of medical care. Data from the 1987 National Health Interview Survey. Med Care. 1991;29:196–209. [PubMed] [Google Scholar]
- 35.O’Malley AS, Mandelblatt J, Gold K, Cagney KA, Kerner J. Continuity of care and the use of breast and cervical cancer screening services in a multiethnic community. Arch Intern Med. 1997;157:1462–70. [PubMed] [Google Scholar]
- 36.Stewart AL, Grumbach K, Osmond DH, Vranizan K, Komaromy M, Bindman AB. Primary care and patient perceptions of access to care. J Fam Pract. 1997;44:177–85. [PubMed] [Google Scholar]
- 37.Lambrew JM, DeFriese GH, Carey TS, Ricketts TC, Biddle AK. The effects of having a regular doctor on access to primary care. Med Care. 1996;34:138–51. doi: 10.1097/00005650-199602000-00006. [DOI] [PubMed] [Google Scholar]
- 38.Donahue KE, Ashkin E, Pathman DE. Length of patient-physician relationship and patients’ satisfaction and preventive service use in the rural south: a cross-sectional telephone study. BMC Fam Pract. 2005;6:40. doi: 10.1186/1471-2296-6-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Xu KT. Usual source of care in preventive service use: a regular doctor versus a regular site. Health Serv Res. 2002;37:1509–29. doi: 10.1111/1475-6773.10524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Doescher MP, Saver BG, Fiscella K, Franks P. Preventive care. J Gen Intern Med. 2004;19:632–7. doi: 10.1111/j.1525-1497.2004.21150.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Somkin CP, McPhee SJ, Nguyen T, Stewart S, Shema SJ, Nguyen B, et al. The effect of access and satisfaction on regular mammogram and Papanicolaou test screening in a multiethnic population. Med Care. 2004;42:914–26. doi: 10.1097/01.mlr.0000135832.28672.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Beal AC, Doty MM, Hernandez SE, Shea KK, Davis K. Results From the Commonwealth Fund 2006 Health Care Quality Survey. New York: The Commonwealth Fund; 2007. Closing the Divide: How Medical Homes Promote Equity in Health Care. [Google Scholar]
- 43.Heisler M, Faul JD, Hayward RA, Langa KM, Blaum C, Weir D. Mechanisms for racial and ethnic disparities in glycemic control in middle-aged and older Americans in the health and retirement study. Arch Intern Med. 2007;167:1853–60. doi: 10.1001/archinte.167.17.1853. [DOI] [PubMed] [Google Scholar]
- 44.Bach PB, Pham HH, Schrag D, Tate RC, Hargraves JL. Primary care physicians who treat blacks and whites. N Engl J Med. 2004;351:575–84. doi: 10.1056/NEJMsa040609. [DOI] [PubMed] [Google Scholar]
- 45.Rosenthal MB, Frank RG, Li Z, Epstein AM. Early experience with pay-for-performance: from concept to practice. JAMA. 2005;294:1788–93. doi: 10.1001/jama.294.14.1788. [DOI] [PubMed] [Google Scholar]
- 46.Epstein AM. Paying for performance in the United States and abroad [Editorial] N Engl J Med. 2006;355:406–8. doi: 10.1056/NEJMe068131. [DOI] [PubMed] [Google Scholar]
- 47.Doran T, Fullwood C, Gravelle H, Reeves D, Kontopantelis E, Hiroeh U, et al. Pay-for-performance programs in family practices in the United Kingdom. N Engl J Med. 2006;355:375–84. doi: 10.1056/NEJMsa055505. [DOI] [PubMed] [Google Scholar]
- 48.Gray DP, Evans P, Sweeney K, Lings P, Seamark D, Seamark C, et al. Towards a theory of continuity of care. J R Soc Med. 2003;96:160–6. doi: 10.1258/jrsm.96.4.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Parkerton PH, Smith DG, Straley HL. Primary care practice coordination versus physician continuity. Fam Med. 2004;36:15–21. [PubMed] [Google Scholar]
- 50.Rodriguez HP, von Glahn T, Chang H, Rogers WH, Safran DG. Patient samples for measuring primary care physician performance: who should be included? Med Care. 2007;45:989–96. doi: 10.1097/MLR.0b013e318074ce63. [DOI] [PubMed] [Google Scholar]
- 51.Lester WT, Grant RW, Barnett GO, Chueh HC. Randomized controlled trial of an informatics-based intervention to increase statin prescription for secondary prevention of coronary disease. J Gen Intern Med. 2006;21:22–9. doi: 10.1111/j.1525-1497.2005.00268.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Asplin BR, Rhodes KV, Levy H, Lurie N, Crain AL, Carlin BP, et al. Insurance status and access to urgent ambulatory care follow-up appointments. JAMA. 2005;294:1248–54. doi: 10.1001/jama.294.10.1248. [DOI] [PubMed] [Google Scholar]
- 53.Shojania KG, Ranji SR, McDonald KM, Grimshaw JM, Sundaram V, Rushakoff RJ, et al. Effects of quality improvement strategies for type 2 diabetes on glycemic control: a meta-regression analysis. JAMA. 2006;296:427–40. doi: 10.1001/jama.296.4.427. [DOI] [PubMed] [Google Scholar]