Abstract
This study examines the impact of ancillary health and social services matched to client needs in substance abuse treatment for African Americans, Latinos and Whites. The study uses data collected from 1992 to 1997 for the National Treatment Improvement Evaluation Study, a prospective cohort study of substance abuse treatment programs and their clients. The analytic sample consists of 3142 clients (1812 African Americans, 486 Latinos, 844 Whites) from 59 treatment facilities. Results show that racial/ethnic minorities are underserved compared to Whites in the substance abuse service system. Different racial/ethnic groups come into treatment with distinct needs and receive distinct services. Although groups respond differentially to service types, substance abuse counseling and matching services to needs is an effective strategy both for retaining clients in treatment and for reducing post-treatment substance use for African Americans and Whites. Receipt of access services was related to reduced post-treatment substance use for Latinos. Study findings are relevant to planning special services for African Americans and Latinos.
Keywords: Substance abuse, Social service delivery, Treatment process, Racial/ethnic groups, Matched services, Special services
1. Introduction
A growing body of evidence indicates that the provision of health and social services in substance abuse treatment, particularly when matched or tailored to specific treatment needs, results in better outcomes (Marsh, Cao, & D’Aunno, 2004; McLellan & McKay, 1998; Smith & Marsh, 2002). Relatively little is known, however, about the impact of ancillary health and social services on specific racial/ethnic groups. Evidence indicates racial/ethnic minorities often enter treatment with limited social and economic resources and numerous co-occurring problems that may result in reduced access to and quality of such ancillary care (Wells, Klap, Koike, & Sherbourne, 2001). Few interventions have been developed to address their specific needs, and, as a result, racial/ethnic minorities are often underserved in relation to their health and social service needs (Alegria et al., 2006; Hansen et al., 2004; Szapocznik, Prado, Berlew, Williams, & Santisteban, 2007).
Despite concerns nationally with health disparities (IOM, 2001), the differential access and impact of services on racial/ethnic groups has received limited attention. Only a small number of service studies provide adequate statistics on the racial/ethnic composition of the samples studied. Even fewer actually compare substance abuse service delivery and outcome across racial/ethnic groups. In large part, this is due to the fact that few substance abuse services data sets are available to adequately analyze major racial/ethnic subgroups. Alegria et al. (2006) note that this results in significant knowledge gaps in relation to the impact of services for racial/ethnic groups. Finally, when racial/ethnic groups are sampled in services research, it is clear that substantial heterogeneity – genetic, social, historical and cultural – exists within groups (Alvarez, Olsen, Jason, Davis, & Ferrari, 2004; Buka, 2002). Thus, while it is increasingly documented that remaining in treatment and receiving services tailored to specific needs is related to improved outcomes, it is not known whether these relations hold for specific racial/ethnic groups. Comparative investigation across groups is needed to document whether tailoring or matching services to the needs of specific groups will ultimately contribute to reductions in racial/ethnic disparities in substance abuse service delivery and outcome (Alegria et al., 2006;Lundgren, Amodeo, Ferguson, & Davis, 2001; Wells et al., 2001).
1.1. Racial/ethnic comparisons of social service access and utilization
Racial/ethnic comparison studies indicate African Americans and Latinos report more mental health and substance abuse problems than do Whites (Wells et al., 2001). In some studies, African Americans have shown greater pre-treatment substance use than other groups (Bluthenthal, Jacobson, & Robinson, 2007). African American and Latino clients also experience more barriers, such as language and culture and resources which reduce their access to services (Alegria et al., 2006; Jayakodi, Danzinger, & Pollack, 2000). In terms of human resources, African Americans and Latinos report lower human capital with respect to education and employment (Jacobson, Robinson, & Bluthenthal, 2006; Tonigan, 2003). Latinos also are more likely than African Americans and Whites to enter treatment at a younger age and without previous treatment experience (Fasados, Evans, & Hser, 2007; Jacobson et al., 2006; Niv & Hser, 2006). Among those with a need for mental health or substance abuse services, according to a study by Wells et al. (2001), minorities were more likely to report their needs not being met in treatment (12.5% of Whites, 25.4% of African Americans, and 22.6% of Latinos).
Available evidence indicates diverse service utilization patterns for different racial and ethnic groups. While some studies indicate Latinos and African Americans have greater or equal access to substance abuse treatment compared to Whites (Daley, 2005; Niv & Hser, 2006; Yan, Huan, & Hser, 2006), still other studies indicate they are less likely to seek and complete treatment (Agosti, Nunes, & Ocepek-Welikson, 1996; Kleinman et al., 1992; Rebach, 1992; Wickizer et al., 1994). Additionally, other research indicates that African American and Latino clients report that they have less access to drug treatment (Robles et al., 2003; Wu, El-Bassel, Gilbert, Piff, & Sanders, 2004; Wu, Kouzis, & Schlenger, 2003), receive fewer services (Jerrell & Wilson, 1997; Wells et al., 2001), and are less like to report overall satisfaction with treatment (Wells et al., 2001; Tonigan, 2003).
Treatment duration, or time spent in treatment, is a robust predictor of reduced post-treatment substance use (Price, 1997; Simpson, 1979; Simpson, Joe, & Brown, 1997; Zhang, Friedmann, & Gerstein, 2003). It is well-established that members of different racial/ethnic groups differ in the length of time they spend in treatment. Latinos and African Americans report shorter service duration compared to Whites (Agosti et al., 1996; McCaul, Svikis, & Moore, 2001; McKay, Lynch, Pettinati, & Shepard, 2003; Tonigan, 2003), although Tonigan (2003) cautions additional studies are needed to identify confounding effects from other variables, such as lower occupational status, that may be more predictive of service duration.
1.2. Components of comprehensive service
Evidence indicates that substance abuse treatment clients who receive comprehensive services show improved outcomes (Friedmann, D’Aunno, Jin, & Alexander, 2000; Marsh et al., 2004; McLellan, Arndt, Metzger, Woody, & O’Brien, 1993; McLellan et al., 1998). Increasingly, studies have identified specific components of comprehensive services that contribute to improved outcomes. In addition to substance abuse counseling, components of access services (McLellan et al., 1998; Smith & Marsh, 2002) and matched services (Friedmann, Hendrickson, Gerstein, & Zhang, 2004; Hser, Polinsky, Maglione, & Anglin, 1999; Smith & Marsh, 2002) have been found to be related to service effectivenss.
1.3. Organizational factors influencing the effectiveness of comprehensive services
It is increasingly recognized that specific organizational characteristics influence the availability of comprehensive services. A set of studies show factors related to organizational effectiveness generally and the provision of ancillary health and social services more specifically include (1) accreditation, (2) ownership (whether an agency is public or private), (3) location (whether services are provided on-site or off-site), and (4) counseling intensity. For example, Friedmann, Alexander, and D’Aunno (1998) found that publicly owned treatment units provide more ancillary services than privately owned units. They also found JCAHO-accredited units and well-resourced units were more likely to provide ancillary health and mental health services. Friedmann et al. (2000) also found that whether services were provided on-site or off-site was positively related to clients’ use of services. Specifically, provision of on-site services was positively related to use of services.
Despite the accumulating evidence indicating that substance abuse treatment clients who receive comprehensive services show improved outcomes, few of these studies provide any or adequate descriptions of the racial and ethnic characteristics of samples. As a result, despite the growing evidence that addressing health and social service needs can improve treatment outcome, there is little evidence of the differential impact of comprehensive services for African Americans, Latinos and Whites.
The purpose of the current study is to examine (1) differences in the organizational characteristics and services provided to specific racial/ethnic groups and (2) the differential impact of matched health and social services on outcomes for these groups. This study of treatment process addresses the question of specific group benefits by examining race/ethnicity as a moderator of treatment effects (Finney, 1995; Moos & Finney, 1995).
2. Methods
2.1. Design and sample
This study analyzed data collected for the National Treatment Improvement Evaluation Study (NTIES) (Gerstein et al., 1997). NTIES is a longitudinal, multi-site study of substance abuse treatment programs serving vulnerable and underserved populations including minorities, pregnant women, youth, public housing residents, welfare recipients and those involved in the criminal justice system. The data were collected by the National Opinion Research Center with assistance from the Research Triangle Institute from a sample of programs receiving funding from the CSAT. NTIES employed a pre/post-panel design to measure the outcome of treatment. Data were collected at both the client and program level. At the client level, client characteristics, services, and outcomes were collected from client interviews obtained at treatment intake, treatment exit and 12 months after treatment exit. Organizational data were collected from interviews with treatment program administrators.
The sampling procedure selected treatment programs funded by the CSAT at the first stage and probability sampling of clients within programs at the second sampling stage. Thus, the treatment organizations in the sample are not representative of the population of substance abuse treatment organizations in the U.S. As a result, although clients were selected in the study with probability sampling at the second stage, they are representative only of clients entering programs funded by the Center for Substance Abuse Treatment during a specific time period.
The analytic sample for this study was a subset of the 4526 clients who completed all intake, treatment discharge, and follow-up interviews. After excluding clients from correctional facilities (n = 1384), the final analytic sample consisted of 3142 clients from 59 service delivery units. The sample included data on organizational, service, and individual client characteristics for 1812 African Americans, 486 Latinos, and 844 Whites. The age range of the sample is 17–51. NTIES investigators report that this sample is largely comparable (e.g., in terms of distribution by gender, educational levels, prior drug treatment experience, criminal justice referrals) with other large scale follow-up studies, except that NTIES oversampled for African Americans and Latinos (Gerstein et al., 1997). With an 83% completion rate on the 12-month follow-up questionnaire, NTIES reported a very high response level compared to other national studies (Gerstein & Johnson, 2000).
2.2. Measures
The NTIES study provides prospective data on organizational, service, and individual client characteristics and, as such, offers the opportunity to examine the relation of service, organizational and client factors to client outcome. Prior to the availability of NTIES, few substance abuse treatment data sets included client-level data along with organizational-level data. The analysis includes organizational-level factors that have been shown to be important in previous substance abuse services research. Thus, the NTIES data set permits the examination of the relation of service characteristics to outcome while controlling for treatment organizational and individual characteristics.
2.2.1. Dependent variables
The study has two dependent variables at the individual level, treatment duration and post-treatment substance use. Treatment duration was measured as a continuous variable indicating the length of treatment in weeks between first and last day of treatment. Post-treatment substance use was measured approximately 12 months after completion of the program when respondents were asked the number of days in the last 30 that they used the five most frequently used licit and illicit substances, including marijuana, crack, cocaine powder, heroin, or alcohol. This dependent variable was continuous, a sum of the number of days respondents reported using the five drugs. The distribution of this variable was right-skewed reflecting the Poisson nature of counting data.
2.2.2. Explanatory variables
Explanatory variables include three components of services received: access services, substance abuse counseling services, and matched services. At discharge, clients reported on the services they received during substance abuse treatment. Reports included receipt of access services (including transportation and child care), substance abuse counseling services (including drug/alcohol counseling, 12-step meetings, drug prescription for alcohol/drug problems). Since each service category was constructed from a different number of services, the measurement of each category was normalized by its mean and standard deviation to allow for comparison of coefficients. Matched services measured by a needs-service ratio was the ratio of services clients reported receiving to those they reported needing in the areas of family and life skills (parenting, domestic violence counseling, family services, assertiveness training, life skills, family planning, non-medical pregnancy services), health services (primary health care, AIDS prevention services, medical pregnancy services), mental health (mental health counseling or treatment), concrete services (school, job skills, housing, help collecting benefits, English training, help getting alimony/child support). Service need was measured as a response to an item in the intake interview, “How important is help with (the problem)?” Service receipt was measured as a response to a question in the discharge questionnaire as to whether they received service in one of the four areas. To create the needs-service ratio, the percentage of self-reported needs that were matched was computed. Clients who reported no need were excluded (n = 27) from multivariate analysis with needs-service ratio as the explanatory variable.
Duration, both an explanatory and dependent variable, was measured as a continuous variable indicating length of treatment in weeks between first and last day of treatment.
2.2.3. Control variables
Individual characteristics included demographic information, such as gender (women and men, where women were the reference category), age, education (years in school), marital status (ever married), work status (whether work full time) and family status (whether live with minor child). Respondents also reported on psychosocial characteristics: health status (whether health limits the work they can do), whether they had ever been beaten (whether attacked or seriously beaten by husband, wife or partner), and mental health status (measured in terms of 24-hour psychiatric visits in the last year). Respondents also were asked to describe their source of payment for services: private, public, or uninsured. They also reported on previous alcohol or drug treatment experience and their pre-treatment drug use. The pre-treatment drug use variable was constructed in exactly the same way as the dependent variable, post-treatment drug use, by summing the number of days in the last 30 days that each respondent used the five most frequently use substances: alcohol, marijuana, crack cocaine, cocaine powder, and heroin.
The treatment organization characteristics derived from administrative interviews, included accreditation, modality, ownership, on-site service availability, and frequency of counseling. For accreditation, administrators reported whether their program was Joint Commission on Accreditation of Healthcare Organizations (JCAHO)-accredited. Lack of accreditation was the referent category. For treatment modality, administrators indicated whether a program was a methadone, outpatient non-methadone, short-term residential, or long-term residential program. Out-patient non-methadone program was the referent category. Ownership was a dichotomous variable in which administrators indicated whether a facility was private (either private for-profit or private not-for-profit) or public (local, state, federal, or tribal government), where public was the referent category. On-site service availability measures the number of on-site services (academic training, vocational training, medical, psychiatric, or pregnancy services) provided by the treatment center. Frequency of counseling was a measure of resource allocation in which the administrator indicated whether the typical client is scheduled to receive individual counseling or therapy less than once per week, once per week, or more than once a week. Less than once per week was the referent category.
2.3. Statistical analysis
2.3.1. Missing data imputation
In the NTIES data set, 0–15% of data were missing (except for the accreditation variable where up to 60% of data were missing for African Americans). Thus, a multiple imputation procedure (Rubin, 1987) was conducted to fill in the missing values by assuming the data were missing at random (Little & Rubin, 1987). Unlike single imputation for missing values, which tends to overestimate sample size but underestimate variance and standard errors, multiple imputation represents uncertainty about the right value to fill in and thus overcomes the problem with single imputation. In the multiple imputation procedure, each missing value was replaced with five plausible values using the Markov Chain Monte Carlo (MCMC) method (Schafer, 1997). Imputation was conducted for the organizational variables and client-level variables independently. Then, the resulting data sets for organizational and client-level data were merged to generate five two-level data sets. Analytic results for each of the five datasets were combined.
2.3.2. Racial/ethnic comparisons
Descriptive comparisons were made of organizational, service, individual, and outcome characteristics for each racial/ethnic group. To compare differences among racial/ethnic groups, logistic regression was used for a categorical variable, and linear regression was used for a continuous variable with Whites as the reference category for each imputed dataset and the results were combined. Bonferroni correction was used to adjust the significance level for multiple statistical comparisons (Miller, 1981).
2.3.3. Generalized linear mixed model
Generalized linear mixed models (GLMM, Breslow & Clayton, 1993) were used to assess the relation of service variables to outcome. GLMMs are extensions of linear mixed models for non-Gaussian distributed outcome variables. GLMMs can be used for longitudinal data analysis as well as hierarchical data analysis. GLMMs were fitted to address two issues in the data. First, both outcome variables, treatment duration and post-treatment substance use, were count data and had skewed distributions. As a result, a Poisson distribution was assumed with a log link function and an over-dispersion parameter in the models. Secondly, to analyze multi-level data and account for clustering effect within service delivery units (SDU), an exchangeable covariance structure was assumed among clients within the same SDU. The explanatory service variables for the treatment duration were access services, substance abuse counseling and the needs-service ratio. Treatment duration was included as an explanatory variable for the post-treatment substance use outcome along with access services, substance abuse counseling and the needs-service ratio. To test hypotheses regarding whether race/ethnicity appears to moderate the relationship between service variables outcome, the interactions between race/ethnicity and service variables were included in the GLMMs (Baron & Kenny, 1986). Organizational and individual variables were used as controls. Since access service, substance abuse counseling services were constructed from a different number of services, the measurement of each category was normalized by its mean and SD to allow for a comparison of coefficients.
3. Results
3.1. Racial/ethnic differences in substance abuse treatment organizations, services and outcome
Table 1 provides descriptive analyses comparing African American, Latino, and White clients in terms of individual, organizational and services characteristics. The racial/ethnic differences in organizational characteristics shown in Table 1 indicate that program administrators report that while only a small percentage of clients were served by JCAHO-accredited organizations, Latino clients were more likely to be served in these organizations than others. This may be explained by the fact that Latino clients were significantly more likely to be served by methadone maintenance organizations; White clients were significantly more likely to be served in short-term residential treatment; and African Americans clients were significantly more likely to be served in long-term residential treatment than Latinos or Whites. Methadone maintenance organizations were more frequently accredited through JCAHO than are other substance abuse treatment modalities. African American and White clients were much more likely than Latino clients to be served in privately supported programs. When program administrators described the number of services provided on-site in their service organizations, Latinos were served in organizations with the fewest services offered on-site (1.85 for Latinos, 2.15 for African Americans, and 2.45 for Whites). Finally, when administrators were asked how frequently they scheduled substance abuse counseling for clients, Latinos were most likely to receive counseling on infrequent schedules (i.e., less than once per week) (17% for Latinos, 13% for African Americans and 6% for Whites).
Table 1.
NTIES organizational, service and client characteristics.
| Variablesa | African American (AA, n = 1812) |
Latino (n = 486) |
White n = 844) |
P-valueb |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | % | Mean | SD | N | % | Mean | SD | N | % | Mean | SD | A A-White | Latino–White | |
| Organizational characteristics | ||||||||||||||
| Accreditation/JCAHO | 32 | 1.8 | 95 | 19.5 | 69 | 8.2 | 0.2384 | <.001 | ||||||
| Missing | 1072 | 59.2 | 201 | 41.4 | 272 | 32.2 | ||||||||
| Treatment modality | 0.099 | <.001 | ||||||||||||
| Methadone | 194 | 10.7 | 99 | 20.4 | 117 | 13.9 | ||||||||
| Non-methadone outpatient | 708 | 39.1 | 195 | 40.1 | 297 | 35.2 | ||||||||
| Short-term residential | 435 | 24.0 | 110 | 22.6 | 253 | 30.0 | ||||||||
| Long-term residential | 475 | 26.2 | 82 | 16.9 | 177 | 21.0 | ||||||||
| Ownership | 0.2899 | <.001 | ||||||||||||
| Private | 1362 | 75.2 | 269 | 55.3 | 659 | 78.1 | ||||||||
| Public | 174 | 9.6 | 203 | 41.8 | 143 | 16.9 | ||||||||
| Missing | 276 | 15.2 | 14 | 2.9 | 42 | 5.0 | ||||||||
| Onsite services | ||||||||||||||
| Academic training | 743 | 41.0 | 219 | 45.1 | 361 | 42.8 | 0.4458 | 0.7851 | ||||||
| Missing | 260 | 14.3 | 10 | 2.1 | 30 | 3.6 | ||||||||
| Vocational training | 195 | 10.8 | 117 | 24.1 | 315 | 37.3 | 0.0055 | <.001 | ||||||
| Missing | 260 | 14.3 | 10 | 2.1 | 30 | 3.6 | ||||||||
| Medical service | 758 | 41.8 | 183 | 37.7 | 339 | 40.2 | 0.1782 | 0.2884 | ||||||
| Missing | 260 | 14.3 | 10 | 2.1 | 30 | 3.6 | ||||||||
| Psychiatric service | 863 | 47.6 | 203 | 41.8 | 449 | 53.2 | 0.4887 | <.001 | ||||||
| Missing | 260 | 14.3 | 10 | 2.1 | 30 | 3.6 | ||||||||
| Pregnancy service | 782 | 43.2 | 159 | 32.7 | 510 | 60.4 | 0.0489 | <.001 | ||||||
| Missing | 260 | 14.3 | 10 | 2.1 | 30 | 3.6 | ||||||||
| Available onsite services | 2.15 | 1.21 | 1.85 | 1.18 | 2.43 | 1.5 | 0.0456 | <.001 | ||||||
| Frequency counseling | 0.2493 | 0.0292 | ||||||||||||
| Less than once a week | 234 | 12.9 | 81 | 16.7 | 53 | 6.3 | ||||||||
| Once a week | 935 | 51.6 | 286 | 58.8 | 577 | 68.4 | ||||||||
| More than once a week | 383 | 21.1 | 109 | 22.4 | 184 | 21.8 | ||||||||
| Missing | 260 | 14.3 | 10 | 2.1 | 30 | 3.6 | ||||||||
| Client characteristics | ||||||||||||||
| Gender | <.001 | <.001 | ||||||||||||
| Male | 1078 | 59.5 | 339 | 69.8 | 602 | 71.3 | ||||||||
| Female | 734 | 40.5 | 147 | 30.2 | 242 | 28.7 | ||||||||
| Age | <.001 | 0.0395 | ||||||||||||
| 20 or younger | 90 | 5.0 | 111 | 22.8 | 139 | 16.5 | ||||||||
| 21–30 | 573 | 31.6 | 144 | 29.6 | 278 | 32.9 | ||||||||
| 31–40 | 819 | 45.2 | 167 | 34.4 | 282 | 33.4 | ||||||||
| 41 or older | 330 | 18.2 | 64 | 13.2 | 145 | 17.2 | ||||||||
| Graduate high school | 899 | 49.6 | 170 | 35.0 | 459 | 54.4 | 0.0068 | <.001 | ||||||
| Worked full time | 1242 | 68.5 | 276 | 56.8 | 587 | 69.5 | 0.2684 | 0.0008 | ||||||
| Missing | 223 | 12.3 | 102 | 21.0 | 120 | 14.2 | ||||||||
| Live with minor child or pregnant | 774 | 42.7 | 202 | 41.6 | 261 | 30.9 | <.001 | <.001 | ||||||
| Health limited work | 595 | 32.8 | 177 | 36.4 | 266 | 31.5 | 0.6704 | 0.0952 | ||||||
| Ever beaten by spouse/partner | 419 | 23.1 | 76 | 15.6 | 171 | 20.3 | 0.5168 | 0.1281 | ||||||
| Missing | 60 | 3.3 | 66 | 13.6 | 81 | 9.6 | ||||||||
| Prior drug/alcohol treatment | 1115 | 61.5 | 227 | 46.7 | 596 | 70.6 | <.001 | <.001 | ||||||
| Payment source | ||||||||||||||
| Private ins/self/family | 389 | 21.5 | 125 | 25.7 | 273 | 32.3 | <.001 | 0.0481 | ||||||
| Missing | 65 | 3.6 | 19 | 3.9 | 22 | 2.6 | ||||||||
| Government | 1163 | 64.2 | 293 | 60.3 | 520 | 61.6 | <.001 | 0.6101 | ||||||
| Missing | 65 | 3.6 | 19 | 3.9 | 22 | 2.6 | ||||||||
| Uninsured | 130 | 7.2 | 57 | 11.7 | 52 | 6.2 | 0.2964 | <.001 | ||||||
| Missing | 65 | 3.6 | 19 | 3.9 | 22 | 2.6 | ||||||||
| Pre-treatment mental visit | 0.29 | 0.84 | 0.21 | 0.71 | 0.42 | 0.98 | 0.0008 | 0.0002 | ||||||
| Pre-treatment drug use | 15.88 | 18.25 | 16.79 | 17.69 | 14.13 | 16.62 | 0.0423 | 0.0150 | ||||||
| Service variables | ||||||||||||||
| Service access | 781 | 43.1 | 253 | 52.1 | 334 | 39.6 | 0.1437 | <.001 | ||||||
| Substance abuse counseling | 1606 | 88.6 | 370 | 76.1 | 681 | 80.7 | <.001 | 0.0568 | ||||||
| Family counseling | 1103 | 60.9 | 299 | 61.5 | 560 | 66.4 | 0.0234 | 0.1458 | ||||||
| Health counseling | 1811 | 99.94 | 486 | 100 | 844 | 100 | 0.7084 | 0.9642 | ||||||
| Mental health counseling | 348 | 19.2 | 141 | 29.0 | 304 | 36.0 | <.001 | 0.0052 | ||||||
| Concrete service | 732 | 40.4 | 227 | 46.7 | 384 | 45.5 | 0.002 | 0.7037 | ||||||
| Need-service ratio | 0.34 | 0.29 | 0.35 | 0.28 | 0.42 | 0.31 | <.001 | 0.0005 | ||||||
| Ourcome variables | ||||||||||||||
| Service duration | 14.60 | 14.14 | 14.62 | 14.35 | 18.84 | 15.94 | <.001 | <.001 | ||||||
| Post-treatment drug use | 8.26 | 13.63 | 9.34 | 14.82 | 6.67 | 11.48 | 0.0107 | 0.0013 | ||||||
| Prior minus post-drug use | 7.58 | 19.91 | 7.45 | 19.18 | 7.44 | 17.53 | 0.9541 | 0.9174 | ||||||
Summary statistics are shown in mean and SD for continuous variables or N and % for categorical variables.
p-Values are obtained from linear regression for continuous variables or logistic regression for categorical variables, using multiple imputed datasets. Bonfernnoi correction is used for the significance level due to multiple comparisons. There are 33 independent tests, so p-values < 0.001 are considered to be significant.
Client and service characteristics were examined at the individual level. Racial/ethnic differences in individual client characteristics were divided into two theoretically relevant dimensions: human capital issues and types of problems clients bring into substance abuse treatment. All comparisons discussed achieve statistical significance. (See final column in Table 1 for comparisons of African Americans and Whites and Latinos and Whites.) Regarding the human capital dimension, findings shown in Table 1 are consistent with other studies (e.g., Tonigan, 2003)in that Latino clients are younger. Consistent with national population trends, they also are less likely than African Americans and Whites to have graduated from high school and to be working full time. In addition, Latinos and African Americans are more likely than Whites to be connected to a family system because of their status as being pregnant or living with a minor. Thus, racial/ethnic differences exist at the individual level, particularly in relation to Latinos and the human capital they bring into treatment.
With respect to problems clients bring into treatment, Latino and African American clients in this sample report higher pre-treatment substance use than White clients (with Latinos reporting highest pre-treatment drug use), but both have lower reports of previous substance abuse or mental health treatment. Further, Latino clients are less likely to report that health problems interfere with their ability to work and much less likely to report a history of domestic violence. Thus, Latino and African American clients report somewhat higher levels of pre-treatment drug use, but also report less previous exposure to the mental health and substance abuse service system.
This study also found significant differences in services received. Clients reported different types of services received. Latinos reported receiving the most access services and concrete services, while African Americans reported receiving the most substance abuse counseling services and Whites reported receiving the most family counseling and mental health counseling services. African Americans and Latinos also had fewer service needs met than Whites as reflected by the lower needs-service ratio. They also remain in treatment for less time than Whites (on average for 15 weeks for Latinos and African Americans and 19 weeks for Whites).
The outcome variables in Table 1 show differences in level of post-treatment substance use with Latinos showing the highest and Whites showing the lowest use with only the Latino–White comparison approaching statistical significance. However, differences in pre-treatment substance use minus post-treatment substance use, i.e., change in drug use, was not significant across groups. Thus, African Americans and Latinos show the highest post-treatment drug use, but the overall pre-treatment to post-treatment reduction in drug use is comparable across the three groups.
3.2. Relation of matched services to duration and post-treatment substance use
Table 2 presents the results of the GLMM, specifically for the predictors of interest and their associated model parameter estimates for treatment duration and post-treatment drug use outcome variables. When treatment duration is examined as the outcome variable, only the interaction between access services and Latinos is significant with a positive coefficient, indicating that compared to Whites, access is significantly more positively associated with treatment duration in Latinos. On the other hand, the significant main effects of substance abuse counseling and the ratio of matched services indicate that they can predict length of stay in treatment for all race/ethnicity groups.
Table 2.
Effects of services on treatment duration and post-treatment substance usea.
| Independent variables | Outcome variables |
|||||
|---|---|---|---|---|---|---|
| Treatment duration |
Post-treatment drug use |
|||||
| Coef | Stderr | p-Value | Coef | Stderr | p-Value | |
| African American | −0.046 | 0.027 | 0.099 | 0.581 | 0.053 | <.001 |
| Latino | −0.081 | 0.036 | 0.032 | 0.149 | 0.065 | 0.041 |
| Treatment duration | NA | NA | NA | −0.003 | 0.001 | 0.022 |
| Access | 0.013 | 0.019 | 0.489 | −0.117 | 0.035 | 0.004 |
| Substance abuse counseling | 0.042 | 0.012 | 0.002 | 0.109 | 0.024 | 0.001 |
| Ratio of matched service | 0.654 | 0.033 | <.001 | −0.642 | 0.065 | <.001 |
| African American × treatment duration | NA | NA | NA | −0.015 | 0.001 | <.001 |
| African American × access | 0.032 | 0.022 | 0.151 | 0.132 | 0.039 | 0.004 |
| African American × substance abuse counseling | −0.006 | 0.015 | 0.707 | −0.187 | 0.026 | <.001 |
| African American × ratio of matched services | −0.046 | 0.038 | 0.241 | 0.198 | 0.081 | 0.043 |
| Latino × treatment duration | NA | NA | NA | −0.006 | 0.002 | 0.002 |
| Latino × access | 0.131 | 0.031 | <.001 | 0.011 | 0.052 | 0.835 |
| Latino × substance abuse counseling | −0.005 | 0.021 | 0.824 | −0.123 | 0.030 | 0.001 |
| Latino × ratio of matched services | 0.072 | 0.057 | 0.231 | 0.718 | 0.102 | <.001 |
From generalized linear mixed models controlling for individual and organizational characteristics. Client characteristics included gender, age, education, health limited work, ever beaten, number of mental health visit, pre-treatment drug use, pre-treatment drug/alcohol treatment, and pay source. Organizational characteristics included accreditation, treatment modality, ownership, organizational onsite service availability, and frequency counseling. p-values <.05 are considered to be significant.
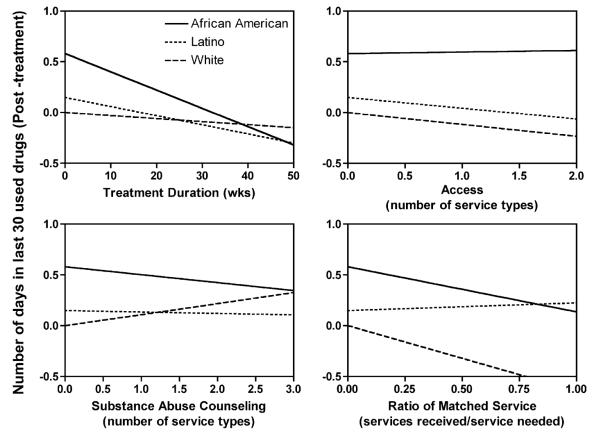
When post-treatment substance use is the outcome variable and treatment duration is included as an explanatory variable, all the interaction terms between race/ethnicity and service variables were significant except the interaction between Latinos and access services. These significant interactions indicate that the effect of service on post-treatment drug use is different among the race/ethnicity groups. To depict the interactions, Fig. 1 shows post-treatment substance use (the number of days used drug in the last 30 days) as a function of treatment duration, access services, substance abuse counseling, and ratio of matched service in African Americans, Latinos and Whites, assuming all other control factors are equal. Fig. 1 is informative as it indicates the magnitude and direction of change in post-treatment substance use with changes in each of the service variables. Overall, treatment duration and substance abuse counseling are effective in reducing post-treatment substance use for African Americans and Latinos but not for Whites; Access services are effective in reducing post-treatment substance use for Latinos and Whites but not for African Americans; while the ratio of matched services are effective for African Americans and Whites but not for Latinos. This close analysis of interaction terms reveals specific differential effects of specific services on post-treatment substance use for African Americans, Latinos and Whites.
Fig. 1.
Post-treatment drug use (the number of days used the five major drugs in the last 30 days) as a function of treatment duration, access, substance abuse counseling and ratio of matched service for African Americans, Latinos and Whites. The estimated lines for each race/ethnicity group were based on the fitted coefficients of the main effect and interaction in Table 2, assuming all other controlling variables are equal. The main effect of race/ethnicity, 0.18 for Black and −0.233 for Latinos, determined the intercepts, while the main effect of service and the interaction term determined the slope of the lines. For instance, the main effect of ratio of matched service was −0.642, while the interaction term between the ratio of matched service and race/ethnicity was 0.198 (ratio × Black) or 0.718 (ratio × Latinos). The estimated slope of the ratio of matched service was −0.444 (−0.642 + 0.198), 0.076 (−0.642 + 0.718) and −0.642 for African Americans, Latinos and Whites respectively. Note the units in the X and Y axes are real world units, since the treatment duration, access, substance abuse counseling and ratio of matched service were not standardized in the model fitting. For illustration purpose, the post-treatment drug use with zero service was set to be 0 for whites in each panel. The interactions between race/ethnicity and service are all significant except the interaction between Latinos and access.
4. Discussion
Study findings add to accumulating evidence that racial/ethnic minorities are underserved in the substance abuse service system. Further, although matched health and social services have been advocated for some time as part of substance abuse treatment for all groups, Whites more than African Americans and Latinos receive and benefit from these services. Findings indicate African Americans and Latinos are less likely to receive tailored services and the impact is less for Latinos than for Whites or African Americans.
Results indicate African American and Latino clients in this sample enter substance abuse treatment with serious substance abuse problems, with limited social and economic resources and receive fewer and lower quality services. Specifically, African Americans and Latinos report higher pre- and post-treatment substance use, have less previous exposure to the substance abuse and mental health service system, and remain in treatment for less time. Further, African Americans and Latinos are less likely than White clients to receive the services they say they need. Findings also document that treatment organizations serving Latinos are distinct from those serving African Americans and Whites as Latinos are served more often in organizations offering the least number of services on-site and the thinnest counseling schedules. Overall, results indicate that racial/ethnic minority clients are underserved in relation to their health and social needs in substance abuse treatment organizations.
Given the perceived value of tailored or matched health and social services, it is important to understand whether there is a differential impact of these services for specific racial/ethnic groups. Findings from the study show matched health and social services are related to treatment duration, i.e., matched services are associated with spending more time in treatment for the total sample. Further, matched health and social services also are predictive of reduced post-treatment substance use for the total sample. Examination of the race/ethnicity × matched service interaction reveals receiving matched services is differentially related to post-treatment substance use for the three groups. Specifically, receiving more matched services is related to reduced post-treatment substance use for African Americans and Whites but not for Latinos.
There are several implications of study findings for the development of treatment models for African American and Latino clients. The development of special programs tailored to particular needs of these client groups requires knowledge of the problems, needs and strengths that distinct client groups bring to treatment. Promising directions for tailoring programs can be identified from the results of this study. For example, the social and economic resources (such as limited education and employment) that create barriers to treatment for African American and Latino clients point to the value of access services (such as transportation and child care) that provide resources enabling clients to take advantage of substance abuse treatment. The numerous co-occurring problems (such as health problems or exposure to trauma) that clients bring to treatment point to the value of comprehensive health and social services for these clients. Second, the fact that Latino and African American clients are more likely to be pregnant or living with a minor child suggests that treatment models designed to address the entire family system – models that provide services for parents as well as for the children themselves – could be especially effective. Third, given that duration is known to be an important predictor of positive substance abuse treatment outcomes, treatment elements like matching services to client needs – that increase duration for African American and Latino clients – can be viewed as an important treatment element. Thus, findings from this study inform the underlying logic of “special” substance abuse treatment programs, i.e., that specific groups have specific needs and that when services are provided to resolve these needs, substance abuse treatment outcomes will improve.
Culturally specific interventions for African American and Latino substance abuse treatment clients is widely discussed in the literature (Alegria et al., 2006; Miranda et al., 2005; Szapocznik et al., 2007). Although no clear consensus exists regarding the role of culture in treatment effectiveness, one argument in favor of culturally tailored treatment is that groups are likely to respond more positively to interventions that respect and respond to their specific values, traditions and needs (Betancourt, Green, Carillo, & Anaheh-Firempong, 2003; Brach & Fraserirector, 2000). Although this study does not test this argument, it does provide support for the value of asking clients what services they need and then explicitly matching services to those needs. It could be argued that providing services to address the specific needs of ethnic minority clients can be considered culturally responsive services. In this study, although African American and Latino client were less likely to received matched services, these services were relevant for helping African American and Latinos to remain in treatment and African Americans to reduce their post-treatment drug use.
4.1. Data limitations
Given the important subgroup differences that emerge in this study, it is necessary to consider the possibility that differences accounted for are specific to this data set. First, the oversampling of African Americans and Latinos in the NTIES data set represents a strength that allows for racial/ethnic comparisons. Despite this oversampling, the Latino group remained small relative to the other groups. Nonetheless, the oversampling of all groups, along with the methods used in this analysis to adjust for missing data, made possible the comparison across groups and served to enhance the precision and reduce the bias in estimates for each group. Second, the prospective nature of the data, i.e., the fact that organizational and service characteristics were examined in relation to substance use pre-, post- and 12 months post-treatment, strengthened the causal inferences about the relation between services received and service outcomes.
Limitations of the NTIES data set derive, first, from the fact that treatment facilities sampled were not representative of treatment organizations in the substance abuse service system. This sampling procedure limits generalizability of study findings as discussed by Gerstein and Johnson (2000). A further limitation of the data relates to the fact that data were collected between 1993 and 1995 and became publicly available in 1997. Concern that the racial/ethnic composition of the public substance abuse services system or the types of services offered have changed over time are mitigated by other available data. For example, examination of the Treatment Episode Data Set (TEDS) data to compare racial/ethnic composition of clients entering the public substance abuse service system are consistent with the composition of the NTIES data set and have not changed significantly when measured in 1995, 2000, and 2005 (SAMSHA/OAS, 2007). Further, data examining the availability of health and social services has changed little since 1990 (Friedmann, Lemon, Durkin, & D’Aunno, 2003). Thus, while not representative, the NTIES data remain a valuable resource for examining differential service delivery for racial/ethnic subgroups. A final limitation derives from the fact that all data analyzed here are self-report data. Self-report data are widely used in substance abuse treatment studies and recent research indicates self-report procedures can provide useful estimates of drug use that can have a high level of consistency with physiological measures (Neale & Robertson, 2003; DelBoca & Noll, 2000).
4.2. Lessons learned
This study provides several valuable lessons for treatment process research that seeks to identify the specific mechanisms of effective treatment for specific treatment groups. Studies of the impact of comprehensive health and social services provided as part of substance abuse treatment are beginning to conceptualize and test the strategies and mechanisms resulting in effective treatment. For example, several studies have examined the relation of service duration to post-treatment substance use (Simpson, 1981; Simpson et al., 1997; Zhang et al., 2003). Others have explored specific service mechanisms such as linkage or access services (Friedmann et al., 2000; Marsh, D’Aunno, & Smith, 2000), co-located services (Friedmann, Alexander, & D’Aunno, 1999) or matched services (Friedmann et al., 2004; Smith & Marsh, 2002). Findings from this study are consistent with other studies of need-service matching that have indicated that this mechanism is related to retention in treatment and to reduced post-treatment substance use. Findings from this study make a particular contribution by indicating these service elements have a differential impact for African Americans, Latinos and Whites. In this sample, matched services were helpful to African Americans and Whites, but not Latinos.
An additional set of lessons relate to the definition and measurement of ancillary health and social service needs and receipt in substance abuse treatment research. Across service research studies, a broad range of services have been measured in a variety of ways. The NTIES data set measured 22 services that were organized in this study into three categories, i.e., access servicesd, substance abuse counseling, and matched services, i.e., the relation between client perceived service need and service receipt in areas of family/life skill counseling, health, mental health and concrete services. While the findings regarding the relation of these service categories to outcomes are consistent with previous studies, different definitions of services found in different studies may influence the relationships found. For example, Smith and Marsh (2002) defined concrete services as housing, job training, and legal services and determined that when these services were matched to client needs in these areas, clients were more satisfied with services but did not necessarily reduce their substance use. Another study using the NTIES data (Friedmann et al., 2004) examined need-service matching in specific service domains and found vocational counseling and housing services to significantly improve overall drug use. Despite the differences, all of these studies contribute to ongoing efforts to conceptualize and measure components of comprehensive services in substance abuse treatment (McCaul et al., 2001; Moos & Finney, 1995; Orwin, Ellis, Williams, & Maaramda, 2000; Simpson, 2004).
Overall, this study provides information relevant to the planning of special services for Latinos and African Americans. The information is valuable for developing services that meet the specific needs of cultural groups that may be under-served or ineffectively served. Specific findings from this study indicate that different racial/ethnic groups do come to substance abuse treatment with distinct needs and receive distinct services. Matching services to needs is an effective strategy for retaining clients in treatment for all groups. Matching services to needs also is an effective strategy for reducing post-treatment substance use for all groups except Latinos. Given the majority of substance abuse treatment is provided in special programs tailored to the needs of particular groups, information about the specific service needs of racial/ethnic groups is necessary for the design of services tailored to the needs of these groups.
Acknowledgements
The research was supported by NIDA grant R01-DA018741-02. The authors thank Professor Michael Wooley for his thoughtful review of the manuscript and Ms. Tanya Hines for assistance in preparing the manuscript. Aspects of the analysis were presented at the Addiction Health Services Research meeting in Athens, GA, in October 2007 and the Society for Social Work Research in Washington, DC, in January 2008.
Biography
Jeanne C. Marsh, PhD is dean and George Herbert Jones professor at the University of Chicago School of Social Service Administration. Her research focuses on treatment process research, substance abuse, health and social service delivery, practitioner decision-making and program evaluation and planning.
Dingcai Cao, PhD is a senior biostatistician in the Department of Health Studies and a research scholar in the Department of Ophthalmology and Visual Science, University of Chicago. His expertise includes computational/statistical modeling and experimental research on human visual system.
Erick Guerrero, MA is a PhD candidate at the University of Chicago School of Social Service Administration. His research and teaching interests are in organizational effectiveness, diversity management, culturally competent practices and adoption of innovation.
Hee-Choon Shin, PhD is senior survey statistician at the National Opinion Research Center at the University of Chicago. His research interests are sampling, analysis of complex survey data, and categorical data analysis.
References
- Agosti V, Nunes E, Ocepek-Welikson K. Patient factors related to early attrition from an outpatient cocaine research clinic. American Journal of Drug Alcohol Abuse. 1996;22:29–39. doi: 10.3109/00952999609001643. [DOI] [PubMed] [Google Scholar]
- Alegria M, Page JB, Hansen H, Cauce AM, Robles R, Blanco C, et al. Improving drug treatment services for Hispanics: Research gaps and scientific opportunities. Drug and Alcohol Dependence. 2006;84S:S76–S84. doi: 10.1016/j.drugalcdep.2006.05.009. [DOI] [PubMed] [Google Scholar]
- Alvarez J, Olsen BD, Jason LA, Davis MI, Ferrari JR. Heterogeneity among Latina and Latinos entering substance abuse treatment: Findings from a national database. Journal of Substance Abuse Treatment. 2004;26:277–284. doi: 10.1016/j.jsat.2004.02.003. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator–mediator variables distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Betancourt JR, Green AR, Carillo JE, Anaheh-Firempong O. Defining cultural competence: A practical framework for addressing racial/ethnic disparities in health and health care. Public Health Reports. 2003;118(4):293–302. doi: 10.1016/S0033-3549(04)50253-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bluthenthal RN, Jacobson JO, Robinson PL. Are racial disparaiaties in alcohol treatment completion associated with racial differences in treatment modality entry? Comparison of outpatient treatment and residential treatment in Los Angeles County, 1998–2000. Alcoholism: Clinical and Experimental Research. 2007;31:1920–1926. doi: 10.1111/j.1530-0277.2007.00515.x. [DOI] [PubMed] [Google Scholar]
- Brach C, Fraserirector I. Can cultural competency reduce racial and ethnic health disparities? A review and conceptual model. Medical Care Research and Review. 2000;57(1):181–217. doi: 10.1177/1077558700057001S09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslow NE, Clayton DG. Approximate inference in generalized linear mixed models. Journal of the American Statistical Association. 1993;88:9–25. [Google Scholar]
- Buka SL. Disparities in health status and substance abuse: Ethnicity and socioeconomic factors. Public Health Reports. 2002;117(Suppl. 1):118–125. [PMC free article] [PubMed] [Google Scholar]
- Daley MC. Race, managed care, and the quality of substance abuse treatment. Administration Policy in Mental Health. 2005;32:457–476. doi: 10.1007/s10488-004-1670-3. [DOI] [PubMed] [Google Scholar]
- DelBoca FK, Noll JA. Truth or consequences: The validity of self-report data in health services research on addictions. Addiction. 2000;95(Suppl. 3):S349–360. doi: 10.1080/09652140020004278. [DOI] [PubMed] [Google Scholar]
- Finney JW. Enhancing substance abuse treatment evaluations: Examining mediators and moderators of treatment effects. Journal of Substance Abuse. 1995;7(1):135–150. doi: 10.1016/0899-3289(95)90310-0. [DOI] [PubMed] [Google Scholar]
- Fasados R, Evans E, Hser Y. Ethnic differences in utilization of drug treatment services and outcomes among proposition offenders in California. Journal of Substance Abuse Treatment. 2007;33(4):391–399. doi: 10.1016/j.jsat.2007.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedmann PD, Alexander JA, D’Aunno TA. Organizational correlates of access to primary care and mental health services in drug treatment units. Journal of Substance Abuse Treatment. 1998;16(1):71–80. doi: 10.1016/s0740-5472(98)00018-x. [DOI] [PubMed] [Google Scholar]
- Friedmann PD, Alexander JA, D’Aunno TA. On site primary care and mental health services in outpatient drug abuse treatment units. Journal of Behavioral Health Services and Research. 1999;26(1):80–94. doi: 10.1007/BF02287796. [DOI] [PubMed] [Google Scholar]
- Friedmann PD, D’Aunno TA, Jin L, Alexander JA. Medical and psychosocial services in drug abuse treatment: Do stronger linkages promote client utilization? Health Services Research. 2000;26(1):80–94. [PMC free article] [PubMed] [Google Scholar]
- Friedmann PD, Lemon SC, Durkin EM, D’Aunno TA. Trends in comprehensive service availability in outpatient drug abuse treatment. Journal of Substance Abuse Treatment. 2003;24:81–88. doi: 10.1016/s0740-5472(02)00323-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedmann PD, Hendrickson JC, Gerstein DR, Zhang Z. The effect of matching comprehensive services to patients’ needs on drug use improvement in addiction treatment. Addiction. 2004;99(8):962–972. doi: 10.1111/j.1360-0443.2004.00772.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gerstein DR, Datta AR, Ingels JS, Johnson RA, Rasinski KA, Schildhaus S, et al. Final report. NTIES: National Treatment Improvement Evaluation Study. Center for Substance Abuse Treatment, Substance Abuse and Mental Health Services Administration; Rockville, MD: 1997. [Google Scholar]
- Gerstein DR, Johnson RA. Non-response and selection bias in treatment follow-up studies. Substance Use and Misuse. 2000;35(6–8):971–1014. doi: 10.3109/10826080009148429. [DOI] [PubMed] [Google Scholar]
- Hansen H, Alegria M, Caban CA, Pena M, Lai S, Shrout P. Drug treatment, health and social service utilization by substance abuseing women from a community-based sample. Medical Care. 2004;42(11):1117–1124. doi: 10.1097/00005650-200411000-00011. [DOI] [PubMed] [Google Scholar]
- Hser Y, Polinsky ML, Maglione M, Anglin MD. Matching clients’ needs with drug treatment services. Journal of Substance Abuse Treatment. 1999;16(4):299–305. doi: 10.1016/s0740-5472(98)00037-3. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine (IOM) Unequal treatment: Confronting racial and ethnic disparities in health care. National Academy of Sciences; Washington, DC: 2001. [Google Scholar]
- Jacobson JO, Robinson PL, Bluthenthal RN. Racial disparities in completion rates from publicly funded alcohol treatment: Economic resources explain more than demographics and addiction severity. Health Research and Educational Trust. 2006;42:773–794. doi: 10.1111/j.1475-6773.2006.00612.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayakodi R, Danzinger S, Pollack H. Welfare reform, substance use and mental health. Journal of Health, Politics and Law. 2000;25(623):651. doi: 10.1215/03616878-25-4-623. [DOI] [PubMed] [Google Scholar]
- Jerrell JM, Wilson JL. Ethnic differences in the treatment of dual mental and substance disorders: A preliminary analysis. Journal of Substance Abuse Treatment. 1997;14:133–140. doi: 10.1016/s0740-5472(96)00125-0. [DOI] [PubMed] [Google Scholar]
- Kleinman PA, Kang S, Lipton DS, Woody GE, Kemp J, Millman RB. Retention of cocaine abusers in outpatient psychotherapy. American Journal of Drug Alcohol Abuse. 1992;18(1):29–43. doi: 10.3109/00952999209001609. [DOI] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. John Wiley & Sons; New York: 1987. [Google Scholar]
- Lundgren LM, Amodeo M, Ferguson F, Davis K. Racial and ethnic differences in drug treatment entry of injection drug users in Massachusetts. Journal of Substance Abuse Treatment. 2001;21:145–153. doi: 10.1016/s0740-5472(01)00197-0. [DOI] [PubMed] [Google Scholar]
- Marsh JC, D’Aunno TA, Smith BD. Increasing access and providing social services in drug abuse treatment for women with children. Addiction. 2000;95:1237–1247. doi: 10.1046/j.1360-0443.2000.958123710.x. [DOI] [PubMed] [Google Scholar]
- Marsh JC, Cao D, D’Aunno TA. Gender differences in the impact of comprehensive services in substance abuse treatment. Journal of Substance Abuse Treatment. 2004;27(4):289–300. doi: 10.1016/j.jsat.2004.08.004. [DOI] [PubMed] [Google Scholar]
- McCaul ME, Svikis DS, Moore RD. Predictors of outpatient treatment retention: Patient versus substance use characteristics. Drug and Alcohol Dependence. 2001;62:9–17. doi: 10.1016/s0376-8716(00)00155-1. [DOI] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Pettinati HM, Shepard DS. An examination of potential sex and race effects in a study of continuing care for alcohol- and cocaine-dependent patients. Alcoholism: Clinical & Experimental Research. 2003;27(8):1321–1323. doi: 10.1097/01.ALC.0000080347.11949.B7. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Arndt IO, Metzger DS, Woody GE, O’Brien CP. The effects of psychosocial services in substance abuse treatment. Journal of the American Medical Society. 1993;269(15):1953–1959. [PubMed] [Google Scholar]
- McLellan AT, Hagan TA, Levine M, Gould F, Meyers K, Bencivengo M, et al. Supplemental social services improve outcomes in public addiction treatment. Addiction. 1998;93(10):1498–1499. doi: 10.1046/j.1360-0443.1998.931014895.x. [DOI] [PubMed] [Google Scholar]
- McLellan AT, McKay JR. The treatment of addiction: What can research offer practice? In: Lamb S, Greenlick MR, McCarty D, editors. Bridging the gap between practice and research: Forging partnerships with community-based drug and alcohol treatment. National Academy Press; Washington, DC: 1998. pp. 147–186. [PubMed] [Google Scholar]
- Miller RG. Simultaneous statistical inference. 2nd ed Springer Verlag; 1981. pp. 6–8. [Google Scholar]
- Miranda J, Bernal G, Lau A, Kohn L, Hwang WC, La Fromboise T. State of the science on psychosocial interventions for ethnic minorities. Annual Review of Clinical Psychology. 2005;1:113–142. doi: 10.1146/annurev.clinpsy.1.102803.143822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moos RH, Finney JW. Substance abuse treatment programs and processes: Linkages to patient needs and outcomes. Journal of Substance Use. 1995;7(1):1–8. doi: 10.1016/0899-3289(95)90302-x. [DOI] [PubMed] [Google Scholar]
- Neale J, Robertson M. Comparisons of self-report data and oral fluid testing in detecting drug use amongst new treatment clients. Drug and Alocohol Dependence. 2003;71(1):57–64. doi: 10.1016/s0376-8716(03)00053-x. [DOI] [PubMed] [Google Scholar]
- Niv N, Hser Y. Navigating health care systems: Drug treatment service utilization and outcomes for Hispanic and White methamphetamine abusers. Health Research and Educational Trust. 2006;41:1242–1257. doi: 10.1111/j.1475-6773.2006.00530.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orwin RG, Ellis B, Williams V, Maaramda M. Relationships between treatment components, client-level factors, and positive treatment outcomes. Journal of Psychopathology and Behavioral Assessment. 2000;22(4):383–397. [Google Scholar]
- Price R. What we know and what we actually do: Best practices and their prevalence in substance abuse treatment. In: Egertson JA, Fox DM, Leshner AI, editors. Treating drug abusers effectively. Blackwell; Malden, MA: 1997. pp. 125–158. [Google Scholar]
- Rebach H. Alcohol and drug use among American minorities. In: Trime JE, Boleck CS, Niemcry SJ, editors. Ethnic and multicultural drug abuse: Perspectives on current research. Haworth Press; Binghampton, New York: 1992. [Google Scholar]
- Robles RR, Matos TD, Colon HM, Deren S, Reyes JC, Andia J, et al. Determinants of health care use among Puerto Rican drug users in Puerto Rico and New York City. Clinical Infectious Diseases. 2003;37:392–403. doi: 10.1086/377552. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation for non-response in surveys. John Wiley & Sons Inc.; New York: 1987. [Google Scholar]
- Schafer JL. Analysis of incomplete multivariate data. Chapman and Hall; New York: 1997. [Google Scholar]
- Simpson DD. The relation of time spent in drug abuse treatment to post-treatment outcome. The American Journal of Psychiatry. 1979;136:1449–1453. doi: 10.1176/ajp.136.11.1449. [DOI] [PubMed] [Google Scholar]
- Simpson DD. Treatment for drug abuse: Follow-up outcomes and length of time spent. Archives of General Psychiatry. 1981;38(8):875–880. doi: 10.1001/archpsyc.1981.01780330033003. [DOI] [PubMed] [Google Scholar]
- Simpson DD. A conceptual framework for drug treatment process and outcome. Journal of Substance Abuse Treatment. 2004;27(2):99–121. doi: 10.1016/j.jsat.2004.06.001. [DOI] [PubMed] [Google Scholar]
- Simpson DD, Joe GW, Brown BS. Treatment retention and follow-up outcomes in the drug abuse treatment outcome study (DATOS) Psychology of Addictive Behaviors. 1997;11(4):294–307. [Google Scholar]
- Smith BD, Marsh JC. Client-service matching in substance abuse treatment for women with children. Journal of Substance Abuse Treatment. 2002;22:161–168. doi: 10.1016/s0740-5472(02)00229-5. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. Office of Applied Studies . Treatment Episode Data Set (TEDS): 1995–2005. National admissions to substance abuse treatment services, DASIS Series: S-37, DHHS publication no. (SMA) 07-4234. Rockville, MD: 2007. [Google Scholar]
- Szapocznik J, Prado G, Berlew AK, Williams RA, Santisteban D. Drug abuse in African American and Hispanic adolescents: Culture, development and behavior. Annual Review of Clinical Psychology. 2007;3:77–105. doi: 10.1146/annurev.clinpsy.3.022806.091408. [DOI] [PubMed] [Google Scholar]
- Tonigan JS. Project match treatment participation and outcome by self-reported ethnicity. Alcoholism: Clinical & Experimental Research. 2003;27:1340–1344. doi: 10.1097/01.ALC.0000080673.83739.F3. [DOI] [PubMed] [Google Scholar]
- Yan JC, Huan D, Hser Y. Long-term morbidity and mortality among a simple of cocaine-dependent Black and White veterans. Journal of Urban Health. 2006;83:926–940. doi: 10.1007/s11524-006-9081-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wells K, Klap R, Koike A, Sherbourne A. Ethnic disparities in unmet need for alcoholism, drug abuse and mental health care. American Journal of Psychiatry. 2001;158:2027–2032. doi: 10.1176/appi.ajp.158.12.2027. [DOI] [PubMed] [Google Scholar]
- Wickizer T, Maynard C, Atherly A, Frederick M, Koepsell T, Krupski A, et al. Completion rates of clients discharged from drug and alcohol treatment programs in Washington State. American Journal of Public Health. 1994;84:215–221. doi: 10.2105/ajph.84.2.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu E, El-Bassel N, Gilbert L, Piff J, Sanders G. Sociodemographic disparities in supplemental service utilization among male methadone patients. Journal of Substance Abuse Treatment. 2004;26:197–202. doi: 10.1016/S0740-5472(03)00246-0. [DOI] [PubMed] [Google Scholar]
- Wu L, Kouzis AC, Schlenger WE. Substance use, dependence, and service utilization among the US uninsured nonelderly population. American Journal of Public Health. 2003;93:2079–2085. doi: 10.2105/ajph.93.12.2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Z, Friedmann PD, Gerstein DR. Does retention matter? Treatment duration and improvement in drug use. Addiction. 2003;98:673–684. doi: 10.1046/j.1360-0443.2003.00354.x. [DOI] [PubMed] [Google Scholar]