INTRODUCTION
Epithelioid hemangioendothelioma (EHE) is a low-grade malignant neoplasm derived from endothelial cells. It was first recognized in soft tissues (1), with later reports showing that the liver may also serve as a primary site (2). We have treated 17 cases of primary hepatic EHE with orthotopic liver transplantation (OLT), and they are the subject of this report.
CASE MATERIALS AND METHODS
A) Patient profile
Between November 1976 and February 1993, 17 patients with the diagnosis of EHE were treated with OLT either at the University Health Sciences Center of Colorado (1971–1980) or at the University of Pittsburgh Medical Center (1981–1993). There were 8 males and 9 females, with their ages ranging from 28 to 58 years (mean of 36 years). Follow-up intervals ranged from 1 to 15 years (median of 4.7 years).
B) Clinical Features
The most common presentation was abdominal pain and hepatomegaly. Less common signs and symptoms included weight loss, jaundice, fatigue, anorexia, ascites, shoulder pain, splenomegaly, and dyspnea (Table 1). In five patients the tumor was found incidentally: in two patients during follow-up for previously treated cancer (squamous cell carcinoma of the nasopharynx and melanoma of the back), in one patient during evaluation of a back injury, in one patient during a laparotomy for endometriosis, and, finally, one patient discovered multiple lesions in her liver while performing an ultrasound examination on herself. Four of the nine women had taken oral contraceptives for indeterminate periods. No patient in this series had a history of exposure to hepatotoxins.
TABLE 1.
CLINICAL PRESENTATION
| SYMPTOMS AND SIGNS | # OF CASES | MEAN DURATION (IN MONTHS) |
|---|---|---|
| ABDOMINAL PAIN | 9 | 12.5 |
| WEIGHT LOSS | 3 | 10 |
| FATIGUE | 1 | 2 |
| ANOREXIA | 1 | 6 |
| JAUNDICE | 2 | 9.5 |
| ASCITES | 1 | 12 |
| SHOULDER PAIN | 1 | 1 |
| SPLENOMEGALY | 1 | 24 |
| DYSPNEA | 1 | 2 |
| CHOLANGITIS | 1 | 1 |
| HEPATOMEGALY | 4 | 7 |
| INCIDENTAL | 5 | 8 |
C) Diagnosis
In fourteen patients the diagnosis was confirmed prior to transplantation: in seven by percutaneous liver biopsy and in seven by open liver biopsy. In the remaining three patients the diagnosis was obtained at the time of the transplant.
Five patients had been originally misdiagnosed. In three cases, 1 to 5 years prior to transplant, the liver biopsies were interpreted as hemangiomas (and one of these patients had a separate biopsy interpreted as a sarcoma). One patient was thought to have a hemangioma, a diagnosis he carried for 15 years without biopsy support, and only when the development of liver failure necessitated transplantation was the real nature of these lesions established. The last patient had a non-diagnostic percutaneous biopsy.
The extent of tumor was staged according to the TNM classification (3,4). Fifteen patients were stage IV-A and two were stage IV-B.
D) Treatment
All patients underwent a standard orthotopic liver transplantation (5). The first patient in our series also had a concomitant excision of a pulmonary nodule. Five patients received chemotherapy with Adriamycin-based regimens: one preoperative, three postoperative, and in one case before and after the transplant. An additional three patients had radiotherapy, two preoperatively and one after surgery. Baseline immunosuppression was accomplished with azathioprine and prednisone in one patient, cyclosporine and prednisone in 11 patients and FK506 in the remaining 5 patients.
E) Statistical Analysis
Kaplan-Meir curves were used for survival analysis. Differences between groups were tested for significance using Breslow’s test, with the significance level set at 0.05.
RESULTS
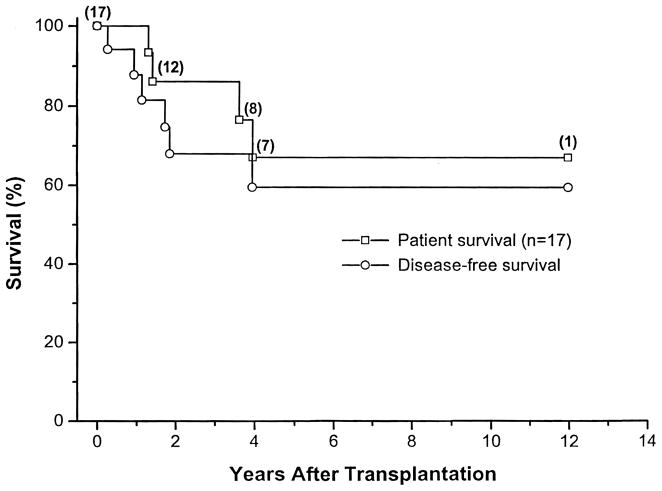
Actuarial patient survival at 1, 3, and 5 year was 100%, 86% and 67%, respectively. Nine of 17 patients (53%) are alive and free of tumor; 7 of the patients have had follow-up intervals greater than 5 years (median of 7.5 years). One patient died of chronic rejection, without tumor, 10 months after OLT. Diffuse metastatic disease was responsible for death in five patients. Two patients are alive with metastases: one with lung metastases three years after surgery, and the other with tumor in the liver four years after her transplant. This last patient was re-transplanted but, unfortunately, there was residual tumor at the margins of the resection.
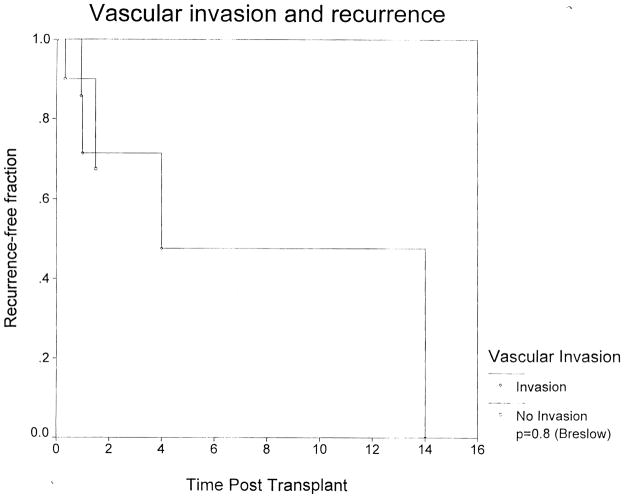
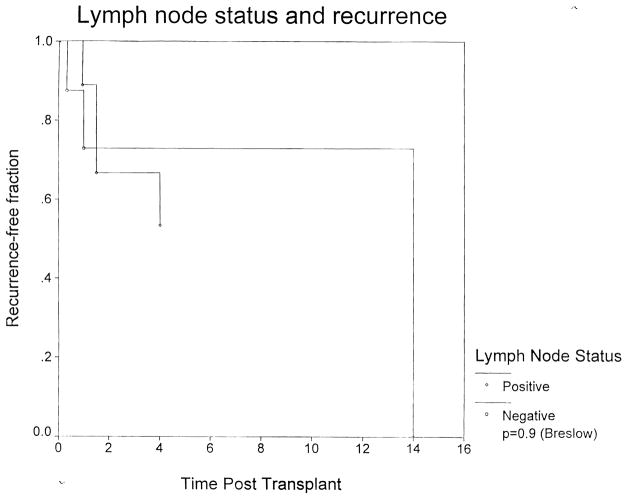
Disease-free survival at 1, 3, and 5 years was 88%, 68%, and 59%, respectively (Fig. 1). The most common sites of recurrence were the liver, lung, and bone. Involvement of the hilar lymph nodes or vascular invasion were frequent features, being present in nine patients (52%). Yet half of those patients are currently alive and free of disease. There was no difference in the recurrence rates among patients with positive or negative nodes (Fig. 2). Likewise, vascular invasion did not affect the recurrence rate (Fig. 3).
Figure 1.
Figure 2.
Figure 3.
There were six postoperative complications that occurred in five patients. One patient bled from the Rouxen-Y loop requiring exploration on the fourth post-operative day. Eight months later he developed a biliary stricture that required percutaneous dilatation. Two patients needed a second graft because of primary nonfunction, at two and four days post-transplant. One patient required thrombectomy on the fourth postoperative day due to hepatic artery thrombosis. Finally, one patient that received a second graft (for liver recurrence, four years after the primary transplant), developed a biliary leak and intra-abdominal abscess, 10 and 14 days after her re-transplant. She was eventually discharged, following a prolonged hospital course. All patients recovered from their complications.
DISCUSSION
Epithelioid hemangioendothelioma is a soft tissue malignant tumor that is characterized by its epithelial-like appearance and vascular endothelial histogenesis. It was histologically identified by Weiss and Enzinger in 1982 (1), and in 1984 Ishak et al., first reported a series of 32 primary EHE of the liver (2). In 1988, we reported the first series of patients (10 cases) (6) with unresectable EHE that were treated with liver transplantation. This report updates that initial series, and adds an additional seven cases that we have treated since.
Liver transplantation for hepatic malignancy remains surrounded by controversy, stemming from the fact that hepatocellular carcinomas and cholangiocarcinomas are associated with a high recurrence rate after liver transplantation (7,8).
The clinical presentation of EHE is usually non-specific. The true incidence of this tumor is not yet known, and it is possible that many of these tumors have been misdiagnosed, especially before Ishak’s report in 1984 (9). The only risk factors known in these patients were the use of oral contraceptives (10). The final diagnosis of this neoplasm requires interpretation supplemented by immunohistochemical staining (2). Often, a wedge biopsy of the tumor is necessary to recognize the architectural features such as the intravascular or intrasinusoidal growth pattern characteristic of the neoplasm (2, 11). Because of the variable cellularity within any given tumor nodule, needle biopsy may be non-diagnostic if only a fibrous tissue area is sampled. Relying on only the cytologic appearance may result in overgrading the lesion as a highly malignant angiosarcoma, rather than a low grade malignancy. This, obviously, could result in limiting the treatment plan to conservative medical management, excluding the possibility of a liver transplant. In point of fact, 5 of 17 patients in the current series had an initial incorrect diagnosis.
A direct comparison between the report of Ishak et al.,(2), of 32 patients with EHE, and the current series of 17 patients treated with liver transplantation, is not possible. However, it is interesting to note that only nine of 32 (28%) of the Ishak et al., patients survived more than five years. The actuarial survival rate of the EHE patients treated with liver transplantation in the current series (67% at 5 years) is satisfactory, and compares favorably with that seen in patients transplanted for nonmalignant disease (12).
Obviously, it remains difficult to propose a single standard therapeutic approach for these tumors because of their rarity and unpredictable natural history. Long-term survival without any specific therapy has been reported by Ishak et al. in primary hepatic EHE (nine of their 30 patients survived more than five years) (2). According to Weiss and Enzinger (1) the histologic features of EHE do not predict tumor behavior, and consequently it is not possible to use the histologic characteristic of a given liver EHE as a guide for therapeutic decisions. Hepatic EHE is usually multifocal (1,2,11) and, therefore, not suitable for partial hepatectomy (6,13,14). Thus, total hepatectomy and OLT is the surgical therapeutic procedure of choice. The long-term survival and disease-free survival after liver transplantation reported in this paper puts EHE into a unique category of primary liver tumors. Even following the development of metastases three patients survived for more than two years. It is also interesting that even in the presence of vascular invasion and positive hilar lymph nodes at transplant (findings that usually condemn to a rapid death from recurrence in all the other primary liver tumors), nine patients are alive and free of disease. Seven patients recurred, and five of them died as a result of it. The survival was similar in patients with positive and negative nodes. We do not have sufficient data to define a role for chemotherapy, radiotherapy, or both in the treatment of this neoplasm. Thus, prospective studies will be required in this area. Also, it is not known whether lymph node dissection in conjunction with the liver transplant would affect survival. In this series, however, lymph node dissection was not systematically performed.
In conclusion, liver transplantation appears to be a very reasonable therapeutic approach for hepatic EHE when the tumor is not resectable (other than with a total hepatectomy). The long-term survival obtained in this series justifies liver transplantation for these tumors even in the presence of limited extra-hepatic disease.
References
- 1.Weiss SW, Enzinger FM. Epithelioid hemangioendothelioma. Cancer. 1982;50:970–981. doi: 10.1002/1097-0142(19820901)50:5<970::aid-cncr2820500527>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 2.Ishak KG, Sesterhen IA, Goodman MZD, Rabin L, Stromeyer FW. Epithelioid hemangioendothelioma of the liver: a clinicopathologic and follow-up study or 32 cases. Hum Pathol. 1984;15:839–852. doi: 10.1016/s0046-8177(84)80145-8. [DOI] [PubMed] [Google Scholar]
- 3.American Joint Committee on Cancer. Manual for staging of cancer. 3. Philadelphia: JB Lippincott; 1987. pp. 87–92. [Google Scholar]
- 4.Hermanek P, Sobin LH, editors. TNM classification or malignant tumors. 4. Berlin: Springer-Verlag; 1987. pp. 53–55. [Google Scholar]
- 5.Starzl TE, Iwatsuki S, Esquivel CO, et al. Refinements in the surgical technique of liver transplantation. Semin Liver Dis. 1985;5:349–350. doi: 10.1055/s-2008-1040632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marino IR, Todo S, Tzakis AG, Klintmalm G, Kelleher M, Iwatsuki S, Starzl TE, et al. Treatment of hepatic hemangioendothelioma with liver transplantation. Cancer. 1988:2079–2084. doi: 10.1002/1097-0142(19881115)62:10<2079::aid-cncr2820621002>3.0.co;2-j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koneru B, Cassavilla A, Bowman J, Iwatsuki S, Starzl TE. Liver transplantation for malignant tumors. Gastroenerol Clin North Am. 1988;17:177–93. [PMC free article] [PubMed] [Google Scholar]
- 8.Iwatsuki S, Starzl TE, Sheahan DG, Yokoyama I, Demetris AJ, Todo S, Tzakis AG, et al. Hepatic resection versus transplantation for hepatocellular carcinoma. Ann Surg. 1991;214:221–229. doi: 10.1097/00000658-199109000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weiss SW, Ishak KG, Dail DH, Enzinger FM. Epithelioid hemangioendothelioma - a vascular tumor often mistaken for a carcinoma. Cancer. 1982;50:970–81. doi: 10.1002/1097-0142(19820901)50:5<970::aid-cncr2820500527>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 10.Dean PJ, Haggitt C, O’Hara CJ. Malignant epitheliohemangioendothelioma of the liver in young women. Relationship to oral contraceptive use. Am J Surg Pathol. 1985:695–704. doi: 10.1097/00000478-198510000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Kelleher MB, Iwatsuki S, Sheahan DG. Epithelioid hemangioendothelioma or liver. Am J Surg Pathol. 1989;13:999–1008. doi: 10.1097/00000478-198912000-00001. [DOI] [PubMed] [Google Scholar]
- 12.Gordon RD, Fung J, Tzakis AG, Todo S, Stieber A, Bronsther O, Martin M, et al. Clinical Transplants 1991. Los Angeles, CA: UCLA Tissue Typing Laboratory; 1991. Liver transplantation at the University of Pittsburgh 1984–1990; pp. 105–118. [PMC free article] [PubMed] [Google Scholar]
- 13.Scoazec JY, Lamy P, Degott C, Reynes M, Feldmann G, Bismuth H, Benhamon GP. Epithelioid hemangioendothelioma of the liver. Diagnostic features and role of liver transplantation. Gastroenterology. 1988;94:1447–1453. doi: 10.1016/0016-5085(88)90685-3. [DOI] [PubMed] [Google Scholar]
- 14.O’Grady JG, Polson RJ, Rollo SK, Calne RY, Williams R. Liver transplantation for malignant disease. Results in 93 consecutive patients. Ann Surg. 1988;207:373–9. doi: 10.1097/00000658-198804000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]