Abstract
BACKGROUND:
Pulmonary rehabilitation (PR) is beneficial for some, but not all, patients with chronic lung disease.
OBJECTIVES:
To determine the success rate of a comprehensive PR program for patients with chronic obstructive pulmonary disease (COPD) and to characterize the differences between responders and nonresponders.
METHODS:
A chart review was performed on patients with a clinical diagnosis of COPD who were referred for PR. Success was defined according to clinically important changes in St George’s Respiratory Questionnaire scores and/or 6 min walk test distance.
RESULTS:
The majority of subjects were men (58%) with a mean (± SD) age of 69±10 years (n=177). Sixty-two per cent of participants had a successful outcome with PR, with proportionally more responders noting subjective improvement than objective improvement on a 6 min walk test (73% versus 51%). Subjects with poor baseline St George’s Respiratory Questionnaire scores tended to improve the most (P=0.011 [ANOVA]). Successful participants had a greater forced expired volume in 1 s (1.1 L versus 0.9 L; P<0.05) and a lower BODE index (body mass index, airflow obstruction, dyspnea, and exercise capacity index) at baseline (9.6 versus 10.3; P<0.05). Success of PR was not correlated with age, sex, chronic hypoxemic respiratory failure or other chronic conditions. Successful participants were more likely to be compliant and to experience fewer adverse events (P≤0.001).
CONCLUSIONS:
Our study reinforced the belief that the majority of participants with COPD benefit from PR. Few baseline characteristics were predictive of success. Subjectively measured improvement occurred more frequently than objectively measured improvement and was greatest in those with the poorest baseline values.
Keywords: Chronic obstructive pulmonary disease, Compliance, Pulmonary rehabilitation, Success
Abstract
HISTORIQUE :
La réadaptation pulmonaire (RP) est bénéfique pour certains patients ayant une maladie pulmonaire chronique, mais pas pour tous.
OBJECTIFS :
Déterminer le taux de succès d’un programme de RP complet destiné aux patients ayant une maladie pulmonaire obstructive chronique (MPOC) et caractériser les différences entre les répondants et les non-répondants.
MÉTHODOLOGIE :
Les chercheurs ont procédé à l’examen des dossiers de patients ayant un diagnostic clinique de MPOC aiguillés en RP. Le succès était défini par des changements cliniques importants aux indices du questionnaire respiratoire de St George ou à la distance à l’épreuve de 6 minutes sur tapis roulant.
RESULTATS :
La majorité des sujets étaient des hommes (58 %) à l’âge moyen (±ÉT) de 69±10 ans (n=177). Chez 62 % des participants, la RP donnait de bons résultats, proportionnellement plus de répondants remarquant une amélioration subjective à l’épreuve de 6 minutes sur tapis roulant (73 % par rapport à 51 %). Les sujets aux indices de départ médiocres au questionnaire respiratoire de St George tendaient être ceux qui s’amélioraient le plus (P=0,011 [ANOVA]). Les participants qui profitaient de la RP avaient un meilleur volume expiratoire maximal par seconde (1,1 L par rapport à 0,9 L; P<0,05) et un indice BODE plus faible (indice de masse corporelle, obstruction des voies aériennes, dyspnée et indice de capacité à l’exercice) au départ (9,6 par rapport à 10,3; P<0,05). Le succès de la RP n’était pas corrélé à l’âge, au sexe, à l’insuffisance respiratoire hypoxémique ou à d’autres maladies chroniques. Les participants profitant de la RP étaient plus susceptibles de respecter le traitement et de vivre moins de réactions indésirables (P≤0,001).
CONCLUSIONS :
La présente étude étaye la croyance selon laquelle la majorité des participants ayant une MPOC profitent de la RP. Peu de caractéristiques de départ était prédictives de succès. L’amélioration mesurée subjectivement était plus fréquente que l’amélioration mesurée objectivement et était plus importante chez les patients ayant les valeurs de départ les plus médiocres.
Chronic obstructive pulmonary disease (COPD) is a debilitating disease marked by varying degrees of dyspnea, deconditioning and difficulty with the activities of daily living. Although medications are an integral part of management, pulmonary rehabilitation (PR) has proven to be a more effective modality in improving a patient’s quality of life (1,2). However, some patients have difficulty completing these relatively intense PR programs, while others do not derive the expected benefit. Moreover, this intervention is costly and time consuming, and involves extensive patient screening and treatment by a specialized team. Even if ultimately cost effective, given these limitations, it is important to quantify the success of such programs and the accrued benefit to participants.
In the present study, we evaluated the success of participants in our outpatient PR program. We conducted a retrospective chart review of all patients who had been evaluated for, and subsequently participated in, PR during the previous nine years. We determined the participation rate among screened patients, then used measures of compliance as well as subjective and objective improvement as a means of determining patient success. Finally, we sought to determine whether particular baseline patient characteristics were associated with successful PR among participating subjects.
METHODS
Study design
A chart review of all patients who were evaluated for PR between July 2000 and December 2008 at Mount Sinai Hospital Montreal (Montreal, Quebec) was performed by a single investigator (AS). Admission to the PR program was by referral from community physicians and pulmonary specialists. Referred patients were screened by a pulmonary physician (JF) with expertise in PR. Patients with contraindications to exercise, such as unstable cardiac disease or musculoskeletal conditions that would limit exertion, were excluded. Patients who believed they could not travel the required distance from home or refused for personal reasons, did not participate in PR. For the purpose of the present study, the analysis was confined to patients with COPD. These patients had a clinical diagnosis of COPD, a forced expiratory volume in 1 s (FEV1) of less than 70% predicted and an FEV1/forced vital capacity ratio of less than 70% predicted.
The study was approved by the Mount Sinai Hospital Montreal Ethics Committee.
The outpatient PR program
The PR program consisted of three sessions per week over an eight-week period, for a total of 24 sessions (2). The PR program was conducted by a multidisciplinary team including physicians, nurses, physiotherapists and occupational therapists, respiratory therapists, a recreational therapist, a dietician and a psychologist. Participants received individually tailored exercise of both upper and lower extremity muscles. The exercise prescription included supervised dyspnea- or fatigue-limited exercise training. Supplemental oxygen was used during training for patients with exercise-induced oxygen desaturation (end exercise SpO2 less than 90%) and in patients who were already using home oxygen.
Education included the proper use of medications, breathing exercises, as well as relaxation and energy conservation techniques. The structured time for each patient per week was at least 3 h of exercise conditioning, 3 h with an occupational therapist and 1 h each with the psychologist, nurse educator and recreational therapist.
Data collection
Demographic information and the results of spirometry performed on patients entering the program were collected. A 6 min walk test was performed before and after completion of the PR program using published guidelines (3). Body mass index (BMI) was calculated and used with FEV1, 6 min walk test distance (6MWD) and Medical Research Council (MRC) dyspnea scores to obtain the BMI, airflow obstruction, dyspnea and exercise capacity (BODE) index values (4). Depression was assessed using the Beck depression score (5). All patients had initially undergone a maximal stage I exercise test. Endurance testing on a bicycle ergometer was performed before and after the PR program. The results of these tests were compiled using a prespecified data collection form.
Outcome measures
Compliance was assessed by determining the number of sessions that were attended by each subject. Subjects were deemed to be compliant if they attended 70% or more of the PR sessions (minimum of 17 of 24 sessions). Regardless of compliance, subjects who were unable to complete the final evaluation – rendering it impossible to assess benefit – were considered to be program failures and were included in the ‘unsuccessful’ group. In the present study, success was assessed by determining whether there was a subjective and/or objective improvement following the structured PR program. The former was defined as an improvement in quality of life as measured by a decrease of 4 points or more on the St George’s Respiratory Questionnaire (SGRQ) (6). This widely used instrument consists of a 76-item questionnaire with three domains encompassing symptoms, activity and impact of disease. The total score, between 0 (best status) and 100 (worst possible status), reflects the subjects’ health, including the impact of illness on quality of life. The scoring for each individual domain and totals were recorded before and after PR. The program was also considered to have been successful if there was objective improvement, as indicated by an increase of at least 54 m in 6MWD (7). The 6MWD was determined before and after PR, with dyspnea reported at commencement and on completion of the walk using a modified Borg visual analogue scale (8).
Statistical analysis
Descriptive statistics (means, SDs, counts and frequencies in per cent) are used to present patients’ baseline characteristics. Differences between the successful and unsuccessful groups were calculated using unpaired t tests. Pearson correlations were also performed to evaluate the relationship between baseline variables and outcomes. One-way ANOVA was used to assess any differences in improvement in the SGRQ and 6MWD after PR using quartiles of baseline measures. Post hoc analysis with Bonferroni’s correction for multiple comparisons was performed for the between-quartile differences for the same variables. A two-sided P≤0.05 was considered to be statistically significant; 95% CIs were calculated.
RESULTS
Subjects
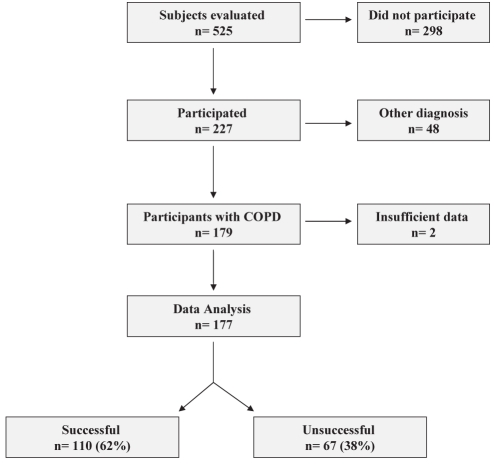
The medical records of 525 patients who had been referred for PR between 2000 and 2008 were reviewed (Figure 1). A total of 298 patients (57%) did not subsequently participate in the program because they had a medical contraindication to exercise, physical or psychological limitations, or could not arrange for regularly required transportation to the hospital. Despite the recommendation of their physician and appearing to be a suitable candidate after our initial evaluation, some patients refused to participate for personal reasons or because they did not believe they would derive the expected benefits. After initial evaluation, 227 patients (43%) were identified as having participated in the program. The participants had the following various diagnoses: 179 (79%) subjects had COPD while the other participants had asthma, pulmonary fibrosis, sarcoidosis, bronchiectasis or obesity associated with dyspnea. Data for two patients were incomplete; therefore, the remaining 177 subjects with COPD represent the group in which our analysis was based. The mean (± SD) age of the participants was 69.1±9.6 years, and 103 (58%) were men.
Figure 1).
Study flow diagram. COPD Chronic obstructive pulmonary disease
A total of 110 participants (62%) had a successful outcome after PR. Among successful participants, 54 (49%) improved only subjectively (according to SGRQ scores), 30 (27%) improved only objectively (according to 6MWD) and 26 subjects (24%) improved on both tests. Thus, overall, among successful patients, 73% improved subjectively while 51% improved objectively. The baseline characteristics of these patients stratified according to their level of success are summarized in Table 1. The successful participants had a greater BMI (P=0.02) and lower BODE index score (P=0.046). The reported information regarding comorbid illnesses was similar between groups except that the unsuccessful group had proportionally more subjects with hypertension.
TABLE 1.
Baseline characteristics stratified according to outcome
| Characteristics |
Outcome |
|
|---|---|---|
| Successful (n=110) | Unsuccessful (n=67) | |
| Age, years (mean ± SD) | 68.1±8.8 | 71.1±10.4 |
| Men | 65 (59) | 38 (57) |
| Body mass index, kg/m2 (mean ± SD) | 29.5±7.2 | 26.9±6.2* |
| BODE index, total ± SD | 9.6±2.1 | 10.3 ±1.6* |
| Comorbid illness | ||
| Coronary artery disease | 21 (19) | 14 (21) |
| Arrhythmia | 12 (11) | 4 (6) |
| Heart failure | 4 (4) | 3 (4) |
| Hypertension | 21 (19) | 20 (31) |
| Diabetes | 13 (12) | 6 (9) |
| Musculoskeletal | 31 (28) | 21 (31) |
| Depression | 6 (5) | 3 (4) |
| Beck depression score (n=114) | 1.6 (0.9) | 1.3 (0.6) |
Data presented as n (%) unless indicated otherwise. BODE Body mass index, airway Obstruction, Dyspnea and Exercise capacity.
P<0.05
Baseline cardiorespiratory characteristics stratified according to successful outcome are summarized in Table 2. Both groups had similar numbers of subjects undergoing long-term oxygen therapy at rest and/or exercise. The absolute FEV1 was slightly but significantly higher at baseline in the successful group (P=0.03). However, baseline exercise parameters, quality of life scores (SGRQ) and mean MRC dyspnea scores were similar between groups. Among patients with mild shortness of breath at baseline (MRC grades 1 to 2), 73% (27 of 37) were successful. Of those with moderate shortness of breath (MRC grades 3 to 4), 64% (73 of 113) were successful; of those with more severe dyspnea (MRC grade 5), 75% (three of four) were successful.
TABLE 2.
Baseline cardiorespiratory characteristics stratified according to outcome
| Characteristics |
Outcome |
|
|---|---|---|
| Successful (n=110) | Unsuccessful (n=67) | |
| Patients with oxygen therapy | 21±19 | 11±16 |
| FEV1, L | 1.1±0.4* | 0.9±0.4 |
| FEV1, % predicted | 40.7±16* | 36.6±13 |
| FVC, L | 1.9±0.7 | 1.8±0.7 |
| FVC, % predicted | 55.7±18.4 | 53.1±14.5 |
| Peak work rate, W | 51.0±23.9 | 46.1±22.9 |
| Peak VO2, L/min | 1.0±0.7 | 0.9±0.4 |
| 6 min walk test distance, m | 327±108 | 310±104 |
| Borg dyspnea score after baseline 6 min walk test (1–10) | 3.5±1.8 | 3.8±1.6 |
| Cycling endurance work, W | 43.5±19.4 | 39.1±18.3 |
| Cycling endurance time, min | 10.2±6.2 | 9.6±6.3 |
| Baseline SGRQ scores, % (total) | 54.5±10.6 | 51.8±11.6 |
| Symptoms | 60.0±18.8 | 54.6±20.1 |
| Activity | 68±13.5 | 67.7±12.8 |
| Impact | 45.0±13.1 | 42.2±14.2 |
| Medical Research Council dyspnea score category | 2.9±0.9 | 3.1±0.8 |
Data presented as mean ± SD unless indicated otherwise.
P<0.05. FEV1 Forced expiratory volume in 1 s; FVC Forced vital capacity; SGRQ St George’s Respiratory Questionnaire; VO2 Maximal oxygen uptake
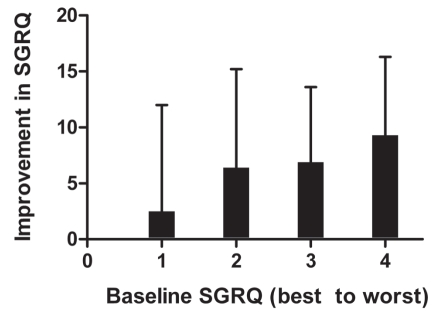
Figure 2 depicts the mean improvement in the quality of life measure (SGRQ) related to the baseline values from best to worst; thus, patients who perceived the greatest impairment in their quality of life at the start of PR reported the most improvement after PR (P=0.011 [ANOVA]). Post hoc analysis confirmed a significant difference between quartile 1 (best) and quartile 4 (worst), with quartile 4 having more improvement (95% CI −12.3 to −1.25); P<0.05). The greatest improvement in the SGRQ score occurred in the impact domain (P<0.05). The improvements in 6MWD after PR varied considerably among patients with similar baseline values (P not significant [ANOVA]). Among those most impaired, as defined by a baseline 6MWD of less than or equal to the median of 330 m, 40% (31 of 78) improved by 54 m or more, whereas 35% (25 of 71) of those with a baseline 6MWD of more than 330 m had an improvement of 54 m or more after PR.
Figure 2).
The mean improvement in St George’s Respiratory Questionnaire (SGRQ) scores after pulmonary rehabilitation in relation to baseline measures of SGRQ according to quartile from best to worst
A total of 138 COPD patients (76%) were compliant with the PR program according to the definition, having attended at least 70% of the sessions. Attendance, measured in weeks, was significantly higher among successful patients (Table 3). Twenty-three patients (13%) failed to complete the program including the final evaluation. This group represented 34% of the unsuccessful patients. The remainder of the unsuccessful patients were those who had no subjective or objective improvement. There was a greater proportion of adverse events in the unsuccessful patient group (34% versus 13%). However, COPD exacerbations accounted for the majority of adverse events among successful patients (10 of 14 [71%]). Among unsuccessful patients, COPD exacerbations represented less than one-half of the adverse events (11 of 23 [48%]). These patients more frequently had other medical complications that accounted for the majority of adverse events. These complications included the following: musculoskeletal conditions (n=4), extreme fatigue (n=4), dizziness (n=2), cardiac instability (n=1) and a diagnosis of anemia.
TABLE 3.
Rehabilitation program outcomes stratified according to outcome
| Characteristics |
Outcome |
|
|---|---|---|
| Successful (n=110) | Unsuccessful (n=67) | |
| Weeks attended, mean ± SD | 7.5±1.4* | 5.8±2.4 |
| Failure to complete the final evaluation, n (%) | 0 (0) | 23 (34) |
| Adverse events, n (%) | 14 (13) | 23 (34)* |
| COPD exacerbations, n (% of total adverse events) | 10 (71) | 11 (48) |
P<0.05. COPD Chronic obstructive pulmonary disease
DISCUSSION
Almost two-thirds of the participants with COPD in the present study improved with PR. These patients had a compliance rate of 76%, while 13% failed to complete the final evaluation at the end of the program. In other studies (9–13), compliance ranged from 56% to 88%, with completion rates ranging from 21% to 69%. Many factors have been identified as risk factors for poor compliance in PR programs including the following: whether a subject is widowed or divorced; living alone; has poor social support; depression and or anxiety; and is living a significant distance from the PR program centre (12–15). In our study, noncompliance was primarily due to adverse events.
We defined success based on improvement in either the SGRQ and/or the 6MWD using values representing the minimal change believed to be clinically relevant (7). The successful group had fewer adverse events, but proportionally more exacerbations of COPD. The unsuccessful group experienced more adverse events unrelated to COPD.
Among successful patients, subjective improvement measured by quality of life scores was more common than improved 6MWD (73% and 51%, respectively). In a study by Evans et al (9), 58% of patients were reported to have been successful. In that study, contrary to ours, more participants experienced clinically important objective rather than subjective improvement. One explanation for this difference is that their PR program consisted of exercise training set at 85% of peak maximal oxygen uptake, whereas our PR program was set at an exercise intensity targeted to a Borg score of 5 or higher.
The participants who had a higher baseline FEV1 in our study were more likely to be successful – a predictive characteristic found in some investigations (9–11). One study (10) reported a correlation between FEV1/forced vital capacity and significant improvement in exercise tolerance and quality of life. Other baseline pulmonary function parameters have not been identified to be predictive of PR efficacy. The BODE index score, which is an integration of BMI, FEV1, MRC dyspnea and 6MWD, was found to be statistically lower at baseline in our successful participants. Cote and Celli (16) reported that PR improved BODE index scores and was associated with better outcomes in patients with COPD.
The change in the SGRQ score after PR was correlated with baseline values, showing that subjects starting with worse scores had greater improvements than those starting with better scores. Our findings suggest that subjects with a lower quality of life are more likely to benefit from PR and demonstrate the greatest relative improvement. This relationship was not observed for the 6 min walk test; however, among those who were most impaired at baseline, greater improvements were observed after PR. Other investigators have evaluated the relationship between baseline characteristics and subsequent improvements with PR. After PR, Vagaggini et al (11) observed a significant improvement in exercise tolerance and quality of life, which correlated with baseline 6MWD and SGRQ scores, respectively.
Obesity is not considered to be a contraindication to PR (17). In our study, a baseline BMI of greater than 25 kg/m2 was associated with PR success, a finding also noted by others (11). This reinforces the potential benefit of this intervention for these patients. Conversely, although it is well established that being underweight is associated with a poor prognosis in COPD, we found that four of seven patients with a BMI of less than 20 kg/m2 improved with PR. It remains to be determined whether PR can ultimately reduce mortality in this patient group (18).
The cohort we studied had baseline MRC scores that ranged from 1 to 5, and a similar distribution of each score was found within the successful and unsuccessful groups. We also noted that a similar proportion of patients at each level of dyspnea were able to improve with PR. Although guidelines recommend that patients with MRC dyspnea scores of 3 to 5 be referred for PR, our study and others (9,10,19) demonstrated that individuals with little dyspnea may also benefit.
In the present study, we used subjective (SGRQ) and objective (6MWD) measures to define success in our PR patients. Although many patients were able to do more after PR, subjective improvement occurred more frequently. Intuitively, this would seem to be beneficial because one would believe that most patients are concerned with feeling better and less dyspneic as opposed to performing slightly better on a walk test. However, the outcome measures we used may not reflect the many potential benefits of PR. We are only beginning to realize that patient’s expectations and goals with PR may vary considerably, and may not necessarily coincide with the objectives of a PR program designed and conducted by treating physicians. We previously reported (20) on a questionnaire currently used in our institution to attempt to better define personal and specific goals that individual patients describe when considering PR. The markers of success used in the present study are limited in scope, and more work will need to be performed to adapt PR programs to the perceived needs and specific goals of the individual patient.
The current study had several limitations. First, the patients who participated in our program were a selected group who agreed to be screened for participation following referral by a general physician or pulmonologist. Therefore, the results reported are not necessarily generalizable to all COPD patients, but rather to those healthy enough and suitably motivated to participate. Second, we were not able to adequately report the reasons for nonparticipation among referred patients because this information was insufficiently charted. However, when noted, it appeared that most individuals who refused did so for personal reasons, usually because they concluded that they could not participate in such an intense program or derive benefit. Finally, it should be noted that in our study – unlike some others – we placed patients who did not complete the final evaluation in the unsuccessful group analysis. Had we confined our analysis of benefit only to patients who completed the program as designed, our success rate would have been approximately 10% higher than reported.
CONCLUSION
The results of the present study reinforce the importance of PR as a therapeutic intervention for patients with COPD (21,22). Those most impaired may derive the greatest relative benefit with PR, and overall patient success may be improved by implementing methods to increase patient compliance and reduce adverse events.
Acknowledgments
The authors thank the Department of Physical and Occupational Therapy at Mount Sinai Hospital Center (Montreal, Quebec) for their dedication to the pulmonary rehabilitation program. They also acknowledge the continued financial support of the Mount Sinai Hospital Center Research Fund.
REFERENCES
- 1.Donohue JF, van Noord JA, Bateman ED, et al. A 6-month, placebo-controlled study comparing lung function and health status changes in COPD patients treated with tiotropium or salmeterol. Chest. 2002;122:47–55. doi: 10.1378/chest.122.1.47. [DOI] [PubMed] [Google Scholar]
- 2.Maltais F, Bourbeau J, Shapiro S, et al. Effects of home-based rehabilitation in patients with chronic obstructive pulmonary disease. Ann Int Med. 2009;149:869–78. doi: 10.7326/0003-4819-149-12-200812160-00006. [DOI] [PubMed] [Google Scholar]
- 3.ATS Statement: Guidelines for the 6-minute walk test. Am J Respir Crit Care Med. 2002;166:111–7. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 4.Celli BR, Cote CG, Marin JM, et al. The body mass index, airflow obstruction, dyspnea, exercise performance (BODE) index in chronic obstructive pulmonary disease. N Eng J Med. 2004;350:1005–12. doi: 10.1056/NEJMoa021322. [DOI] [PubMed] [Google Scholar]
- 5.Beck AT, Ward CH, Mendelson M, et al. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–71. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 6.Jones PW, Quirk FH, Baveystock CM, et al. A self-complete measure of health status for chronic airflow limitation. The St Georges’s Respiratory Questionnaire. Am Respir Dis. 1992;145:1321–7. doi: 10.1164/ajrccm/145.6.1321. [DOI] [PubMed] [Google Scholar]
- 7.Redelmeier DA, Bayoumi AM, Goldstein RS, et al. Interpreting small differences in functional status: The six-minute walk test in chronic lung disease patients. Am J Respir Crit Care Med. 1997;155:1278–82. doi: 10.1164/ajrccm.155.4.9105067. [DOI] [PubMed] [Google Scholar]
- 8.Wilson RC, Jones PW. A comparison of the visual analogue scale and modified Borg scale for the measurement of dyspnoea during exercise. Clin Sci. 1989;76:277–82. doi: 10.1042/cs0760277. [DOI] [PubMed] [Google Scholar]
- 9.Evans RA, Singh SJ, Collier R, et al. Pulmonary rehabilitation is successful for COPD irrespective of MRC dyspnoea grade. Respir Med. 2009;103:1070–5. doi: 10.1016/j.rmed.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 10.Garrod R, Marshall J, Barley E, et al. Predictors of success and failure in pulmonary rehabilitation. Eur Respir J. 2006;27:788–94. doi: 10.1183/09031936.06.00130605. [DOI] [PubMed] [Google Scholar]
- 11.Vagaggini B, Costa F, Antonelli S, et al. Clinical predictors of the efficacy of a pulmonary rehabilitation programme in patients with COPD. Respir Med. 2009;103:1224–30. doi: 10.1016/j.rmed.2009.01.023. [DOI] [PubMed] [Google Scholar]
- 12.Young P, Dewse M, Fergusson W, et al. Respiratory rehabilitation in chronic obstructive pulmonary disease: Predictors of nonadherence. Eur Respir J. 1999;13:855–9. doi: 10.1034/j.1399-3003.1999.13d27.x. [DOI] [PubMed] [Google Scholar]
- 13.Sabit R, Griffiths L, Watkins A, et al. Predictors of poor attendance at an out-patient pulmonary rehabilitation programme. Respir Med. 2008;102:819–24. doi: 10.1016/j.rmed.2008.01.019. [DOI] [PubMed] [Google Scholar]
- 14.Fan VS, Giardino ND, Blough DK, et al. Costs of pulmonary rehabilitation and predictors of adherence in the National Emphysema Treatment Trial. COPD. 2008;5:105–16. doi: 10.1080/15412550801941190. [DOI] [PubMed] [Google Scholar]
- 15.Reardon J, Casaburi R, Morgan M, et al. Pulmonary rehabilitation for COPD. Respir Med. 2005;99(Suppl B):S19–27. doi: 10.1016/j.rmed.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 16.Cote CG, Celli BR. Pulmonary rehabilitation and the BODE index in COPD. Eur Respir J. 2005;26:630–6. doi: 10.1183/09031936.05.00045505. [DOI] [PubMed] [Google Scholar]
- 17.Ramachandran K, McCusker C, Connors M, et al. The influence of obesity on pulmonary rehabilitation outcomes in patients with COPD. Chron Respir Dis. 2008;5:205–9. doi: 10.1177/1479972308096711. [DOI] [PubMed] [Google Scholar]
- 18.Gray-Donald K, Gibbons L, Shapiro SH, et al. Nutritional status and mortality in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1996;153:961–6. doi: 10.1164/ajrccm.153.3.8630580. [DOI] [PubMed] [Google Scholar]
- 19.British Thoracic Society Standards of Care Subcommittee on Pulmonary Rehabilitation Pulmonary rehabilitation. Thorax. 2001;56:827–34. doi: 10.1136/thorax.56.11.827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sully J, Demers L, Baltzan M, et al. Development of a patients’ needs assessment questionnaire for pulmonary rehabilitation. Am J Respir Crit Care Med. 2007;175:A233. (Abst) [Google Scholar]
- 21.Ghassan FS, Mosier M, Beasley B, et al. Rehabilitation for patients with chronic obstructive pulmonary disease. Chest. 2003;18:213–21. doi: 10.1046/j.1525-1497.2003.20221.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.ZuWallack R, Hedges H. Primary care of the patient with chronic obstructive pulmonary disease – part 3: Pulmonary rehabilitation and comprehensive care for the patient with chronic obstructive pulmonary disease. Am J Med. 2008;121(Suppl 7):S25–S32. doi: 10.1016/j.amjmed.2008.04.004. [DOI] [PubMed] [Google Scholar]