Abstract
We have conducted a unique prospective randomized study to compare the effect of FK506 and cyclosporine (CsA) as the principal immunosuppressive agents after pulmonary transplantation. Between October 1991 and March 1993, 74 lung transplants (35 single lung transplants [SLT], 39 bilateral lung transplant [BLT]) were performed on 74 recipients who were randomly assigned to receive either FK or CsA. Thirty-eight recipients (19 SLT, 19 BLT) received FK and 36 recipients (16 SLT, 20 BLT) received CsA. Recipients receiving FK or CsA were similar in age, gender, preoperative New York Heart Association functional class, and underlying disease. Acute rejection (ACR) was assessed by clinical, radiographic, and histologic criteria. ACR was treated with methylprednisolone, 1 g i.v./day, for three days or rabbit antithymocyte globulin if steroid-resistant.
During the first 30 days after transplant, one patient in the FK group died of cerebral edema, while two recipients treated with CsA died of bacterial pneumonia (1) and cardiac arrest (1) (P=NS). Although one-year survival was similar between the groups, the number of recipients free from ACR in the FK group was significantly higher as compared with the CsA group (P<0.05). Bacterial and viral pneumonias were the major causes of late graft failure in both groups. The mean number of episodes of ACR/100 patient days was significantly fewer in the FK group (1.2) as compared with the CsA group (2.0) (P<0.05). While only one recipient (1/36=3%) in the group treated with CsA remained free from ACR within 120 days of transplantation, 13% (5/38) of the group treated with FK remained free from ACR during this interval (P<0.05). The prevalence of bacterial infection in the CsA group was 1.5 episodes/100 patient days and 0.6 episodes/100 patient days in the FK group. The prevalence of cytomegaloviral and fungal infection was similar in both groups.
Although the presence of bacterial, fungal, and viral infections was similar in the two groups, ACR occurred less frequently in the FK-treated group as compared with the CsA-treated group in the early postoperative period (<90 days). Early graft survival at 30 days was similar in the two groups, but intermediate graft survival at 6 months was better in the FK group as compared with the CsA group.
Significant mortality still occurs due to infection and acute and chronic rejection in adult lung allograft recipients who have received CsA-based immunosuppression (1). In the first year after transplant, infection is the most significant cause of death (55%) followed by primary graft failure (30%), and rejection (15%) (2). Later, obliterative bronchiolitis (OB)* is a major disability and morbidity, (27%) and combined with infection (40%) it is the most troublesome problem. Furthermore, the toxicities of CsA-based therapy—including systemic hypertension, hypercholesterolemia, and diminished renal function—limit its dosage.
FK506 had demonstrated a dramatic immunotherapeutic advantage in our pediatric cardiac recipients (3). Accordingly in 1990 FK506 was introduced as the primary immunosuppressive therapy in our pediatric lung recipients with the hope that this would result in steroid sparing and reduced toxicity (4). Because we were also encouraged by the preliminary results in lung recipients, a prospective randomized clinical trial was initiated in adults designed to compare FK and CsA. The aim of this study was to determine the relative efficacy of FK, low-dose steroid (prednisone 0.10–0.15 mg/kg), and AZA as standard immunosuppression for lung allograft recipients. This communication reports the impact of FK on episodes of rejection and infection during the first year after isolated lung transplantation.
MATERIALS AND METHODS
Patient population
Between October 1991 and March 1993, 74 isolated lung transplants were performed on 74 patients. Patients were randomly assigned by alternate treatments to receive either FK or CsA combined with low-dose steroids and AZA as outlined below. Thirty-eight recipients (19 single lung transplants (SLT], 19 bilateral lung transplants [BLT]) received FK, and thirty-six recipients (16 SLT, 20 BLT) received CsA. Recipients receiving FK or CsA were similar in age, gender, preoperative New York Heart Association functional class, and underlying disease (Table 1).
Table 1.
Characteristics of recipients in a randomized trial of FK506 vs. CsA
| FK506 | CsA | |
|---|---|---|
| Age | ||
| Mean ± SD | 39 ± 18 | 41 ± 10 |
| Range | 10–66 | 21–66 |
| Gender (male/female) | 15/23 | 15/21 |
| Underlying disease | ||
| Septic obstructive LD | 12 | 10 |
| Nonseptic obstructive LD | 17 | 10 |
| Restrictive LD | 3 | 4 |
| Pulmonary hypertension | 5 | 12 |
| Other | 1 | 0 |
| Type of transplant procedure | ||
| Single lung Tx | 19 | 16 |
| Bilateral lung Tx | 19 | 20 |
Immunosuppressive Protocols
FK group
Immediately before transplantation, all patients were given an intravenous loading dose (4 mg/kg) of AZA, and 500 mg of methyl prednisolone was infused just prior to revascularization of the allograft. AZA was dosed (5–2.5 mg) according to WBC tolerance (5000 mm3), and postoperatively the steroids were continued every 8 hr for three 125 mg doses. FK was given by continuous infusion as soon as the recipient was cardiovascularly stable (usually 6–8 hr after admission to the intensive care unit), at a dose of 0.025 mg/kg/day. The FK dose was then increased toward 0.075 mg/kg/day to reach a target serum level of 1.0–1.5 ng/ml. While most achieved this within three days, at times nephrotoxicity necessitated a low-target or more gradual increased dosage. Once recipients were able to take oral medications, FK was prescribed at a dose of 0.15 mg/kg/day in two divided doses and adjusted accordingly to target levels. FK was measured by enzyme-linked immunosorbent assay technique of Tamaura (5). Additional steroids were not given unless two episodes of acute rejection occurred during the first six weeks. If required, maintenance prednisone was begun at 0.15–0.2 mg/kg/day.
CsA group
Patients randomized to CsA received methylprednisolone and prednisone and similar perioperative doses of AZA and intravenous CsA (2.5 mg/kg/day) were also begun when the recipient was stable postoperatively. When gastrointestinal function resumed, oral CsA was begun at a dose of 2.5 mg/kg/day given twice daily. As with the FK protocol, the dose of CsA was adjusted to an ideal target level of 750–1000 ng/ml, but nephrotoxicity was respected.
Rejection therapy
Acute rejection was treated with methylprednisolone, 1 g i.v. daily, for three successive days for the first and second episodes of acute rejection. Persistant rejection and obliterative bronchiolitis were treated with rabbit antithymocyte globulin prepared in our laboratory and delivered intramuscularly (1.5 mg/kg/day) for five days.
Measure of effectiveness
Rejection of the allograft was assessed by radiograph, spirometry, and biopsy (2,6). Histologic confirmation of at least grade 2 of rejection by transbronchial biopsy (TBBx) was required except for the few with early diffuse radiographic infiltrates that responded promptly to the first dose of methylprednisolone. Surveillance TBBx was performed at two-week intervals during the first 2–3 months and thereafter the interval was increased based on the recipient’s clinical history.
Statistical analysis
Actuarial survival and freedom from acute rejection were computed by the method of life table analysis (7). Linearized rates (events per 100 patient-days) were compared with the maximum likelihood ratio test (8). Comparisons among the FK and CsA groups were made by the Mann-Whitney rank sum test (9). A computer program package (Statsoft, CSS Statistica, Tulsa OK) was used for statistical analysis.
RESULTS
Mortality
One- and 6-month survivals were similar in the groups (Fig. 1): 80% of the FK group and 71% of the CsA group had the cumulative probabilities of being alive one year after transplantation.
Figure 1.
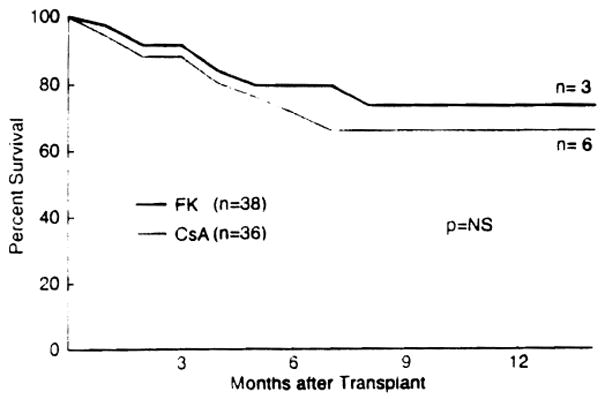
Survival after pulmonary transplantation—a randomized of FK vs. CsA.
One operative death occurred in the FK group, and two deaths occurred in the CsA group (Table 1). The majority of late deaths were related to allograft infection in both groups. In the CsA group, ACR contributed to fatal graft failure in both instances, whereas the death in the FK group was not related to ACR.
Rejection
A total of 45 episodes of rejection were diagnosed among the recipients who received FK. Forty-two episodes of rejection were confirmed histologically, while three episodes were diagnosed by radiograph. Seventy-eight episodes of rejection (76 episodes by TBBx, two by clinical findings) were diagnosed in the CsA group. The mean frequency of rejection per 100 patient days in the FK group (1.2) was significantly lower as compared with the CsA group (2.0) (P<0.05 by Mann-Whitney) (Fig. 2). The average times to rejection were 26 and 22 days, respectively, in the FK and CsA patients, and the CsA recipients required additional 3-day courses of methylprednisolone as compared with FK recipients, although this difference barely reached statistically significant levels (P=0.05) (Fig. 3). Moreover, 13/38 (34%) of the FK recipients were steroid-free; whereas, only 2/36 (6%) of the CsA recipients were steroid-free (P<0.0001 by chi-square analysis). At 90 days the average dose of prednisone was 11±4 mg/day in the CsA group and 9±4 mg/day in the FK patients (NS).
Figure 2.
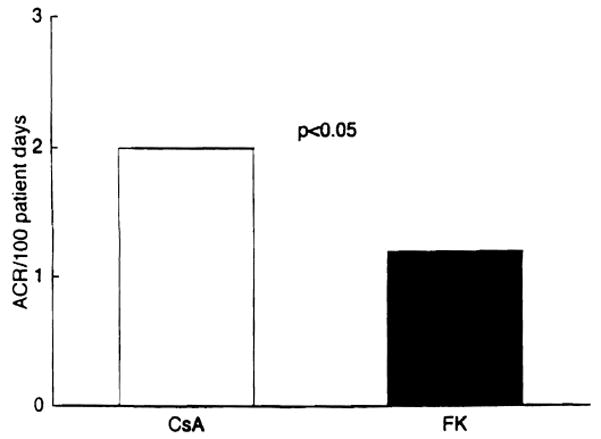
Frequency of acute rejection after pulmonary transplantation—a randomized trial of FK vs. CsA (P<0.05 by Mann-Whitney analysis).
Figure 3.
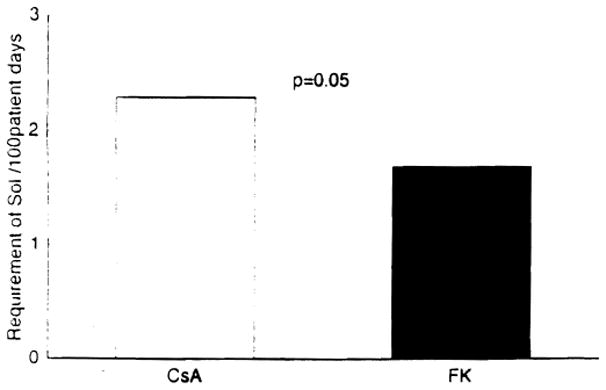
Requirement of methylprednisolone for episodes of acute rejection—a randomized trial of FK vs. CsA. (P=0.05 by Mann-Whitney analysis).
All of the recipients in the CsA group experienced at least one episode of rejection within 6 months posttransplant, and 11% (4/38) of FK recipients were free from rejection (Fig. 4). Two recipients in the FK group and four recipients in the CsA group developed OB during this observation period between October 1991 and April 1993. All of the recipients with OB were diagnosed by surveillance TBBx and currently are in remission following adjunctive immunosuppressive therapy with methylprednisolone and/or rabbit antithymocyte globulin.
Figure 4.
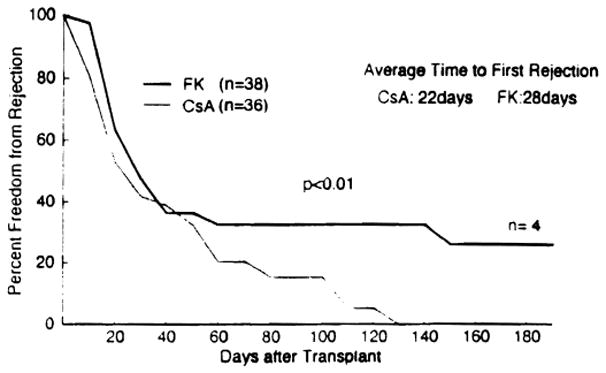
Freedom from acute rejection alter pulmonary transplantation—randomized trial of FK vs. CsA (P<0.05 by generalized Wilcoxon test).
CsA to FK switch
Thirteen nonrandomized recipients initially treated with CsA were switched to FK because of uncontrollable multiple episodes of ACR. Acute rejection resolved in eight patients, improved in two, was unaffected in two, and persisted in one.
Infection
Although prevalence of infection in the FK group (0.6 episodes/100 patient days) was less as compared with that of the CsA group (1.5 episodes/100 patient days), this did not reach statistical significance (Fig. 5). Bacterial and viral pneumonia were the primary causes of death after 30 days posttransplant (Table 2). Although donor and recipient serostatus was similar between the groups, only one recipient in the FK group experienced symtomatic CMV compared with five recipients in the CsA group during the first 120 days after transplant. The prevalence of fungal infection in the FK (7 episodes) and CsA (5 episodes) groups was similar.
Figure 5.
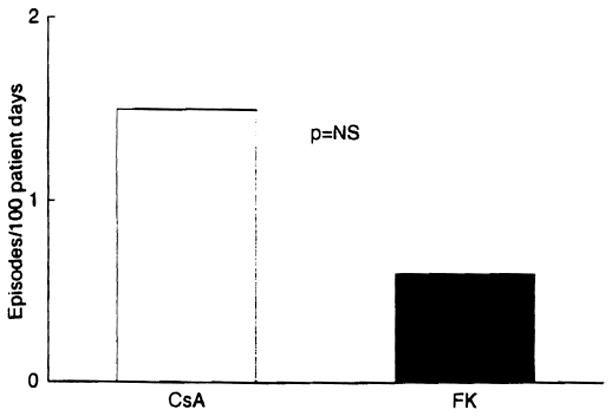
Frequency of infection after pulmonary transplantation—a randomized trial of FK vs. CsA.
Table 2.
Causes of early and late morbidity following lung TX in a randomized trial of FK506 vs. CsA
| Group | Mortality (≤30 days) | Cause of death (n) |
|---|---|---|
| Early | ||
| FK506 | 3% (1/38) | Toxoplasmosis (1) |
| CsA | 6% (2/36) | Bacterial pneumonia (1) |
| Cardiac arrest (1) | ||
| Late | ||
| FK506 | 13% (5/38) | P aeruginosa pneumonia (2) |
| Adenoviral pneumonia (2) | ||
| CMV pneumonia (1) | ||
| CsA | 16% (6/36) | P aeruginosa pneumonia (3) |
| Adenoviral pneumonia (1) | ||
| PTLD (1) | ||
| Respiratory failure (reason unknown) (1) | ||
Metabolic studies and side effects
Although transient renal dysfunction immediately after transplantation was frequently observed with intravenous administration of FK or CsA, the majority of cases were well controlled with concomitant administration of low-dose prostaglandin E1 (0.01 μg/kg/hr). Notably absent in the FK group were complaints of gingival hyperplasia or hirsutism, which have frequently been seen in CsA recipients. Systolic and diastolic arterial pressures were similar in the two groups during this observation period. Twelve recipients in the FK group (12/38) and 15 recipients in the CsA group (15/36) required antihypertensive therapy, consisting of enalapril maleate or diltiazem hydrochloride.
DISCUSSION
This randomized trial of FK versus CsA after isolated pulmonary transplantation suggests that FK based-immunosuppression resulted in less-frequent moderate and severe acute rejection. In addition, 11% of FK recipients were free from rejection 6 months posttransplant, whereas all of the CsA recipients experienced at least one episode of rejection during the same period. This is noteworthy primarily because lung transplant recipients experience a much higher incidence of acute rejection as compared with the cardiac transplant recipients (10) and more frequent and more severe acute rejection were most significant risk factors for the subsequent development of OB, the leading cause of late morbidity and mortality. The potential impact of FK on OB has yet to be determined. However, the lower prevalence of acute rejection in the FK group is encouraging (11).
Infection remains the most significant cause of early and intermediate mortality in this randomized study, and no significant differences were observed between the two groups in the prevalence of infection and death from infection. Thus better immunosuppressive protocols and aggressive antimicroorganic therapy for adequate control of infection are still warranted for further improvement of the quality of life and survival after pulmonary transplantation.
Although transient renal dysfunction was observed in the significant number of patients in both the FK and CsA groups, neurological complications and gingival hyperplasia or hirsutism were not encountered in the FK group.
In summary, the current randomized trial of FK versus CsA demonstrated fewer episodes of rejection in the FK group, although the prevalence of infection and survival were similar in the groups. The impact of FK on long-term follow-up is unclear and needs to be determined.
Footnotes
Presented at the 19th Annual Meeting of the American Society of Transplant Surgeons, May 19–21, 1993, Houston, TX.
Abbreviations: ACR, acute rejection; BLT, bilateral lung transplant; OB, obliterative bronchiolitis; SLT, single lung transplant; TBBx, transbronchial biopsy.
References
- 1.Griffith BP, Hardesty RL, Armitage JM, et al. Acute rejection of lung allografts with various immunosuppressive protocols. Ann Thorac Surg. 1992;54:846. doi: 10.1016/0003-4975(92)90635-h. [DOI] [PubMed] [Google Scholar]
- 2.Griffith BP, Hardesty RL, Armitage JM, et al. A decade of lung transplantation. Ann Thorac Surg. 1993;218:310. doi: 10.1097/00000658-199309000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Armitage JM, Fricker FJ, del Nido P, et al. A decade (1982–1992) of pediatric cardiac transplantation and the impact of FK 506 immunosuppression. J Thorac Cardiovasc Surg. 1993;105:464. [PMC free article] [PubMed] [Google Scholar]
- 4.Armitage JM, Fricker FJ, Kurland J, et al. Pediatric lung transplantation: the years 1985 to 1992 and the clinical trial of FK 506. J Thorac Cardiovasc Surg. 1993;105:337. [PMC free article] [PubMed] [Google Scholar]
- 5.Tamaura K, Kobayashi M, Hashimoto K, et al. A highly sensitive method to assay FK 506 levels in plasma. Transplant Proc. 1987;19:23. [PubMed] [Google Scholar]
- 6.Yousem SA, Berry GJ, Brunt, et al. A working formulation for the standardization of nomenclature in the diagnosis of heart and lung rejection: lung rejection study group. J Heart Lung Transplant. 1990;9:593. [PubMed] [Google Scholar]
- 7.Matlson DE. Public health data and analysis. In: Matlson DE, editor. Statistics. Oak Park, Ill: 1986. p. 390. [Google Scholar]
- 8.Gross AJ, Clark VA. Survival distribution: reliability application in the biomedical sciences. New York: J Wiley; 1975. p. 331. [Google Scholar]
- 9.Giants SA. Alternatives to analysis of variance and the t test based on ranks. In: Glants SA, editor. Primer of biostatistics. New York: McGraw-Hill; 1981. p. 284. [Google Scholar]
- 10.Armitage JM, Kormos RL, Morita S, et al. Clinical trial of FK 506 immunosuppression in adult cardiac transplantation. Ann Thorac Surg. 1992;54:205. doi: 10.1016/0003-4975(92)91371-f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bando K, Paradis IL, Konishi H, et al. Obliterative bronchiolitis after lung and heart-lung transplantation: an analysis of risk factors and management. J Thorac Cardiovasc Surg. doi: 10.1016/S0022-5223(05)80003-0. in press. [DOI] [PubMed] [Google Scholar]


