Abstract
Twenty-seven clinical and laboratory data and the subsequent clinical course of 93 consecutive adult patients who underwent orthotopic liver transplantation for various chronic advanced liver diseases were analyzed retrospectively to assess the risk factors of early major bacterial infection and death after the procedure. Forty-one patients (44%) had early major bacterial infection during hospitalization for orthotopic liver transplantation. The mortality rate was 70.7% in patients with early major bacterial infection and was 7.7% in patients without early major bacterial infection (p < 0.001). Total serum bilirubin, total white blood cell count and polymorphonuclear cell count, IgG (all p < 0.05) and plasma creatinine level (p < 0.001) were higher in patients that developed early major bacterial infection than in those who did not. By step-wise discriminant analysis, the strongest risk factor for early major bacterial infection was the serum creatinine level, which achieved an accuracy of 69% for a creatinine level greater than 1.58 mg per dl.
Seven variables (ascites, hepatic encephalopathy, elevated white blood and polymorphonuclear cell count, decreased helper to suppressor T cell ratio and elevated plasma creatinine and bilirubin levels) were associated with a significant increased risk for death. A step-wise discriminant analysis of these seven factors resulted in the demonstration of serum creatinine as the greatest risk factor for mortality. A preoperative serum creatinine either less than or greater than 1.72 mg per dl accurately predicts survival or death, respectively, in 79% of cases. These data suggest that the baseline preoperative serum creatinine level provides the best indication of the short-term prognosis after liver transplantation than does any other preoperatively obtained index of the patient’s status.
Orthotopic liver transplantation (OLTx) has dramatically altered the otherwise fatal outcome for some patients with advanced chronic liver disease and has been reported to obtain a 70.8% survival in adult patients at 1 year after OLTx (1). Because both economic and human resources are limited within the health care system of most countries and institutions, liver transplantation ideally should be restricted to those patients with the greatest possibility of survival after the procedure, so the selection of appropriate candidates for OLTx has become an issue of considerable concern both for physicians and surgeons involved in the management of patients with advanced hepatic disease.
In a recent series of adult patients with OLTx, 75% of the deaths occurred during the first 60 days post-transplantation (2). In this series, infectious complications were the most common cause of death. Ninety percent of the deaths due to infection following OLTx occurred during the first 60 days post-OLTx; 79% of these deaths were caused by bacterial infection. Thus, early bacterial infection appears to be the leading single cause of death after liver transplantation in adults.
The purpose of the present study was to determine: (i) whether easily obtainable preoperative clinical and laboratory data which can be obtained reasonably can identify patients who will develop early postoperative bacterial infections and (ii) whether these same factors can serve as objective predictors of an early death in adult patients undergoing OLTx.
PATIENT POPULATION AND METHODS
Ninety-three consecutive adult patients who received 128 consecutive OLTx procedures at the University of Pittsburgh between February, 1981 and January, 1984 were evaluated retrospectively. Twenty-two patients received 2 transplants while 3 patients had 3 consecutive OLTx. Only those patients who survived the immediate postoperative period (24 hr) after OLTx were included in the study. Thus, 7 patients who did not survive for 24 hr, either dying in the operating room or soon thereafter, were excluded from the analysis leaving 93 patients whose records were available for analysis.
The facilities and details of our patient selection process, regimens for supportive care, OLTx procedures and immunosuppression regimens have been described in detail elsewhere (3–5). In general, patients who were selected for transplantation were required to meet the following requirements based upon the nature of their primary disease:
-
Chronic Advanced Liver Disease
No medical or surgical options available except for transplantation.
-
Two of the four following criteria:
a bilirubin level >15 mg per dl
an albumin level <2.5 gm per dl
a prothrombin time >5 sec above control
encephalopathy not responsive to dietary restrictions, lactulose and neomycin or any combination of these therapies.
-
Hepatic Malignancy
A tumor that was not resectable without hepatectomy.
No evidence of extrahepatic metastasis.
-
Fulminant or Subacute Hepatic Failure
In advanced Grade 3 or 4 encephalopathy.
In the intensive care unit and on a respirator.
All OLTx recipients received comparable clinical management from the same medical and surgical teams throughout the study interval.
Data were collected retrospectively from the patients’ hospital charts. Survival was recorded up to the day of discharge from the hospital. The data obtained on bacterial infection were recorded up to the sixtieth day post-OLTx or up to the date of discharge from hospital, whichever occurred earlier. Bacterial infections recognized after this closing date were excluded from the study. Thus, only data relevant to early major bacterial infections (EMBI) were collected. The diagnosis of EMBI was made using clinical and laboratory criteria. An EMBI was defined as any bacterial infection acquired during the patient’s hospitalization after OLTx or until the sixtieth day of posttransplantation, which resulted in a prolongation of the hospitalization, additional surgical procedures or death. Minor afebrile upper respiratory tract infections and catheter-associated bacteriurias were excluded from study. Isolations of bacteria from throat, sputum, nasotracheal aspirates and surgical drainage tubes which occurred without associated clinical abnormalities suggestive of infection were excluded from the analysis. The microorganisms which were isolated were identified using standard procedures in the clinical microbiological laboratory of Presbyterian-University Hospital, Pittsburgh, Pa. In seven patients with pneumonia, no bacterial agent was isolated but the pneumonia was thought to be of bacterial origin because of its improvement after the initiation of antimicrobial therapy.
Twenty-seven clinical and biochemical variables were obtained on each patient preoperatively and were evaluated. Surviving and nonsurviving groups were divided into two subgroups: those who developed postoperative EMBI and those who did not. The clinically obtainable preoperatively items recorded included age, sex, underlying liver disease, presence of encephalopathy, ascites and esophageal varices, variceal bleeding (considered to have occurred any time during the period between the first complaint of disease and subsequent OLTx), previous episodes of systemic sepsis or spontaneous bacterial peritonitis and any immunosuppressive therapy which was applied during the immediate 6 months prior to OLTx. Nineteen biochemical variables were also obtained. These included: total protein, albumin, prothrombin time, total bilirubin, transferrin, white blood cell (WBC) count, polymorphonuclear (PMN) cell count and total lymphocyte count; total T lymphocytes, total suppressor T cells, total helper T cells and the ratio of helper to suppressor T lymphocytes present in peripheral blood; immunoglobulins (IgG, IgM and IgA); complement [C3, C4, properdin factor B (PFB)], and serum complement total capacity (CH100). In 31 patients, one of the following variables had not been recorded: T and B cells (31 patients); CH100 (31 patients); PFB (8 patients); WBC and differential (7 patients), and total proteins and albumin (4 patients). All variables represent the last laboratory value obtained prior to the performance of the OLTx.
Quantitative data are expressed as mean ± S.E. Statistical comparisons between groups for these variables were made using χ2 analysis to compare proportions and the unpaired Student’s t test or U Mann-Whitney test to compare means. A p value less than 0.05 was considered to be significant. Those variables that were related significantly to EMBI or to death by themselves were included subsequently in a step-wise discriminant analysis with the presence or absence of EMBI, or the short-term final outcome (alive or death) after OLTx as the outcome-dependent variable, respectively (6, 7). Because total T and B lymphocyte levels in peripheral blood and CH100 data were unavailable for many of the patients studied, these data were not assessed by this method.
RESULTS
The study population of 93 patients included 37 men and 56 women whose ages ranged from 18 to 53 years, with an average of 32 ± 1 year. Seventeen of these 93 patients (18%) had had at least one episode of major bacterial sepsis before transplantation. Twenty-three (25%) had received immunosuppressive therapy (prednisone, azathioprine or D-penicillamine) during the 6 months before OLTx. Forty-four patients (47%) had ascites. Twenty-one (23%) had suffered at least one episode of variceal bleeding, and 28 (30%) had had clinically evident hepatic encephalopathy pretransplantation.
The underlying hepatic diseases for which OLTx was performed are given in Table 1. If a patient was transplanted for a hepatic malignancy superimposed upon a nonmalignant condition (e.g., hepatocellular carcinoma arising in a cirrhotic liver), only the malignancy was considered for the purpose of analysis.
Table 1.
Indications for OLTx in the 93 consecutive patients studied
| Diagnosis | No. of cases | No. surviving | No. of EMBI |
|---|---|---|---|
| Primary biliary cirrhosis | 27 | 22 | 6 |
| Postnecrotic cirrhosis | 20 | 1.1 | 13 |
| Hepatic malignancya | 16 | 13 | 6 |
| Sclerosing cholangitis | 13 | 7 | 5 |
| α2-antitrypsin deficiency | 3 | 2 | 2 |
| Acute hepatic failure | 3 | 0 | 2 |
| Caroli’s disease | 3 | 1 | 2 |
| “Lupoid” chronic active hepatitis | 2 | 1 | 2 |
| Hemochromatosis | 2 | 1 | 1 |
| Recurrent adenomatosis | 1 | 1 | 0 |
| Venooclusive disease | 1 | 0 | 1 |
| Wilson’s disease | 1 | 1 | 0 |
| Cryptococcus cholangitis | 1 | 0 | 1 |
| Total | 93 | 60 | 41 |
Includes hepatocellular carcinoma (12 cases), fibrolamellar hepatoma (2 cases), angiosarcoma (1 case) and cholangiocarcinoma (1 case).
Incidence, Types of and Clinical Course of EMBI Occurring following OLTx
A total of 45 individual episodes of EMBI occurred in 41 of the 93 patients studied. Twenty of the 45 EMBI (44%) occurred in the first 2 weeks after OLTx; by the first month, 73% of all EMBI episodes had occurred (Figure 1). Twenty-nine of the patients (70.7%) who had
Fig. 1.
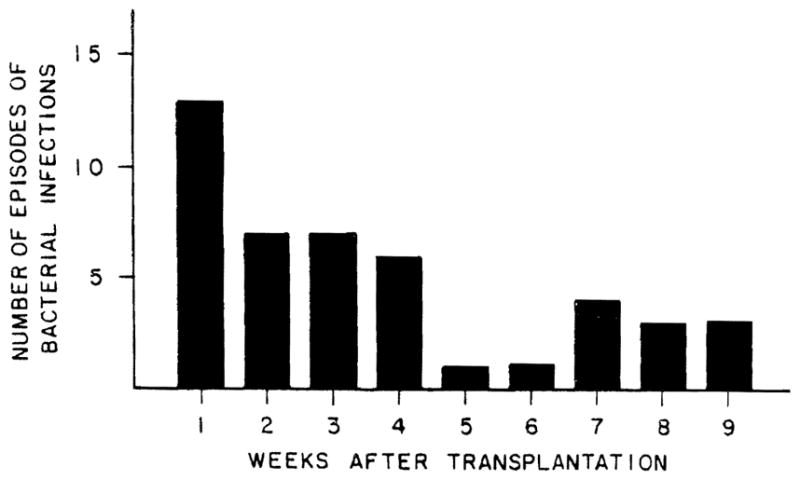
Time of onset of early major bacterial infection after surgery in liver transplant recipients.
EMBI died compared to 4 of the 52 patients (7.7%) who did not develop EMBI after transplantation (p < 0.001). Thirty-three of the 93 total patients evaluated (35.5%) died during the study period, and in 15 of these (45.4%), bacterial infection was the major cause of death. The various microorganisms isolated from these patients with EMBI are listed in Table 2. Gram-negative bacteria predominated over Gram-positive organism. Pseudomonas was isolated from 17 of the 45 cases of EMBI and was involved in 9 of the 15 cases in which EMBI contributed to the death of the patient. The types of infection and their outcome in the patients studied are summarized in Table 2.
Table 2.
Types and outcome of EMBI in 93 consecutive recipients of OLTx
| Type of infection | No. of episodes | No. of patients | Agents recovered (No. of times) | No. of episodes associated with deatha |
|---|---|---|---|---|
| Sepsis | 18 | 17 |
Pseudomonas (9) Enterobacter (6) Staphylococcus coagulation negative (5) Klebsiella (3) Streptococcus (2) E. coli (2) Proteus (1) Salmonella (1) Difteroides (1) |
14b |
| Pneumonia | 16 | 13 |
Pseudomonas (5) E. coli (1) Legionella (1) Unknown (9) |
3c |
| Pericarditis | 1 | 1 | Legionella | |
| Abdominal abscesses | 10 | 10 |
Pseudomonas (3) Enterobacter (2) E. coli (1) Unknown (6) |
5c |
Some patients had two or more types of microorganisms. For each patient, the full spectrum of clinically significant microbiologic data has been entered into the table.
Four cases coexisted with fungemia.
All of these patients developed sepsis and died because of sepsis.
Predictor Factors Analysis
Risk Factors for EMBI
To determine whether any of various preoperative clinical or biochemical factors obtained as part of the pretransplant evaluation could be associated with an increased risk of EMBI, factor analysis was performed and the results of an initial univariate analysis are summarized in Table 3. Total bilirubin, IgG, total WBC and PMN leukocyte cell count (p < 0.05) and creatinine level (p < 0.001) were higher in patients who developed post-OLTx bacterial infections than in those who did not. The other data analyzed were unrelated statistically to the risk of EMBI occurring after OLTx. By step-wise discriminant analysis, the strongest risk factor for EMBI was the creatinine level, followed in order of relative strength by the PMN leukocyte count, IgG level, bilirubin level and WBC count (Table 4). Preoperative creatinine values greater or lower than 1.52 mg per dl assigned patients to the infected or noninfected group, respectively, with a 68.8% accuracy. Using creatinine and a PMN leukocyte count greater than 4,847 per mm3, accuracy increased further to 72.1%. With the addition of the third step using IgG, accuracy actually decreased to 70.5%.
Table 3.
Univariate analysis of risk factors for each bacterial infection after OLTx
| Risk factor | Postoperative EMBI (n = 41) | No postoperative EMBIa (n = 52) | Significance level |
|---|---|---|---|
| Age (yr) | 34 ± 1.4 | 36 ± 1.4 | |
| Sex (male/female) | 21/20 | 16/36 | |
| Previous infectiona | 23% | 13% | |
| Previous immunosuppressive therapya | 28% | 17% | |
| Ascitesa | 61% | 47% | |
| Variceal bleedinga | 33% | 21% | |
| Hepatic encephalopathya | 42% | 28% | |
| Total bilirubin levela (mg/dl) | 21.9 ± 2.4 | 14.2 ± 1.8 | p < 0.05 |
| Prothrombin time (sec)b | 15.7 ± 0.5 | 16.7 ± 2.2 | |
| Total serum proteins (mg/dl)b | 6.5 ± 0.2 | 7.1 ± 0.2 | |
| Serum albumin (mg/dl)b | 3.1 ± 0.1 | 3.4 ± 0.1 | |
| Transferrin (μg/dl)b | 343 ± 15 | 345 ± 14 | |
| WBC count (cells/mm3)b | 8,799 ± 866 | 6,680 ± 520 | p < 0.05 |
| PMN cell count (cells/mm3)b | 6,223 ± 685 | 4,235 ± 341 | p < 0.05 |
| Lymphocytes (cells/mm3)b | 1,122 ± 140 | 1,242 ± 109 | |
| Lymphocyte T cells (cells/mm3)b | 604 ± 90 | 659 ± 50 | |
| Helper T lymphocytes (cells/mm3)b | 189 ± 26 | 189 ± 22 | |
| Suppressor T lymphocytes (cells/mm3)b | 423 ± 59 | 477 ± 33 | |
| Ratio of helper to suppressor T lymphocytesb | 2.87 ± 0.26 | 3.68 ± 0.33 | |
| IgG (mg/dl)b | 1,655 ± 129 | 1,343 ± 70 | p < 0.05 |
| IgM (mg/dl)b | 284 ± 30 | 316 ± 26 | |
| IgA (mg/dl)b | 372 ± 42 | 351 ± 27 | |
| C′3 (mg/dl) | 109 ± 10 | 123 ± 10 | |
| C′4 (mg/dl) | 18 ± 2 | 24 ± 3 | |
| CHIOOb | 48 ± 5 | 72 ± 6 | |
| PFB (mg/dl) | 32 ± 3 | 42 ± 8 | |
| Creatinine (mg/dl) | 2.3 ± 0.4 | 1.3 ± 0.3 | p < 0.001 |
Between first complaint and transplantation.
Preoperative evaluation.
Table 4.
Step-wise discriminant of risk factors of EMBI
| Risk factor for EMBIa | Step | Discriminant value | Accuracy (%) |
|---|---|---|---|
| Creatinine (mg/dl) | 1 | ≥1.52 mg% | 68.8 |
| PMN cells (cells/mm3) | 2 | ≥4,847 cells/mm3 | 72.1 |
| IgG (mg/dl) | 3 | ≥1,546 mg/dl | 70.5 |
| Bilirubin (mg/dl) | 4 | ≥18.28 mg/dl | 68.9 |
| WBCs (cells/mm3) | 5 | ≥7,211 cells/mm3 | 62.3 |
In order of highest to lowest relative strength.
Predictors of Death
The mortality rate during the study period was 35.5%. For the initial analysis, 27 separate variables were compared between survivors and nonsurvivors. As is shown in Table 5, preoperative ascites and hepatic encephalopathy were more frequent (p < 0.05) in patients who died than in patients who survived. Bilirubin and creatinine levels, WBC counts, PMN cell counts and the helper to suppressor T cell ratio were greater (p < 0.05) in patients dying after OLTx than they were in those who survived. The remaining 20 preoperatively obtained variables were statistically unrelated to the risk of mortality after OLTx.
Table 5.
Risk factors for death in adult patients after liver transplantation
| Risk factor | Survivors (n = 60) | Nonsurvivors (n=33) | p value |
|---|---|---|---|
| Age (yr) | 36.0 ± 1.3 | 33.0 ± 1.7 | |
| Sex (male/female) | 22/38 | 16/17 | |
| Previous infectiona | 16% | 22% | |
| Previous immunosuppressive therapya | 24% | 25% | |
| Ascitesa | 51% | 71% | <0.05 |
| Variceal bleedinga | 21% | 42% | |
| Hepatic encephalopathya | 24% | 58% | <0.05 |
| Total bilirubin level (mg/dl)b | 14.1 ± 1.7 | 25.8 ± 1.7 | <0.01 |
| Prothrombin time (secb) | 16.4 ± 1.8 | 16.2 ± 0.6 | |
| Total serum proteins (mg/dl)b | 7.1 ± 0.2 | 6.4 ± 0.2 | |
| Serum albumin (mg/dl)b | 3.3 ± 0.1 | 3.1 ± 0.1 | |
| Transferrin (μg/dl)b | 352 ± 13 | 328 ± 18 | |
| WBC count (cells/mm3)b | 6,882 ± 473 | 9,157 ± 1,068 | <0.05 |
| PMN leukocytes (cells/mm3) | 4,480 ± 306 | 6,497 ± 866 | <0.05 |
| Total lymphocyte count (cells/mm3)b | 1,248 ± 97 | 1,055 ± 171 | |
| Total T lymphocytes (cells/mm3)b | 613 ± 47 | 672 ± 114 | |
| Helper T lymphcytes (cells/mm3)b | 181 ± 20 | 211 ± 31 | |
| Suppressor T lymphocytes (cells/mm3)b | 429 ± 29 | 490 ± 80 | |
| Helper to suppressor T lymphocytes ratiob | 3.7 ± 0.3 | 2.3 ± 0.2 | <0.05 |
| IgG (mg/dl)b | 1,432 ± 82 | 1,567 ± 130 | |
| IgM (mg/dl)b | 311 ± 23 | 288 ± 38 | |
| IgA (mg/dl)b | 370 ± 29 | 340 ± 42 | |
| C′3 (mg/dl) | 120 ± 9 | 106 ± 11 | |
| C′4 (mg/dl) | 23 ± 2 | 19 ± 2 | |
| CH100b | 68 ± 6 | 45 ± 4 | |
| PFB (mg/dl) | 42 ± 4 | 30 ± 3 | |
| Plasma creatinine (mg/dl)b | 1.3 ± 0.2 | 2.7 ± 0.4 | <0.05 |
Between first complaint and transplantation.
Preoperative evaluation.
The results of a step-wise discriminant analysis of these variables are shown in Table 6. This analysis establishes which of these factors is the most important and then ranks them in terms of their relative influence. The preoperatively obtained factors that carried an increased risk of death following OLTx in order of relative strength were creatinine, bilirubin, hepatic encephalopathy, ascites, WBC and PMN cell counts and the helper to suppressor T cell ratio.
Table 6.
Step-wise discriminant analysis of risk factors for death occurring after liver transplantation
| Risk factor for deatha | Step | Discriminant value | Sensitivity | Specificity | Positive predictive value | Negative predictive value | Accuracy (%) |
|---|---|---|---|---|---|---|---|
| Creatinine (mg/dl) | 1 | ≥1.7 mg% | 52 | 96 | 73 | 81 | 79 |
| Bilirubin (mg/dl) | 2 | ≥18.66 mg% | 57 | 85 | 63 | 81 | 76 |
| Encephalopathy | 3 | – | 57 | 85 | 63 | 81 | 76 |
| Ascites | 4 | – | 57 | 85 | 63 | 81 | 76 |
| WBCs (cells/mm3) | 5 | ≥7,632 (cells/mm3) | 57 | 87 | 67 | 82 | 76 |
| PMN leukocytes (cells/mm3) | 6 | ≥1,300 (cells/mm3) | 57 | 85 | 63 | 81 | 76 |
In order of highest to lowest relative strength.
Creatinine values greater or lower than 1. 72 mg per dl assigned patients to the nonsurvivor or survivor group, respectively, with a 79.1% accuracy. Using bilirubin levels, the second factor in order of relative strength, accuracy, decreased to 76.1 %. Thus, it is evident that the preoperative creatinine level is the major clinical variable useful in predicting postoperative survival following OLTx.
DISCUSSION
The prognosis following OLTx has steadily improved during the last 20 years since Starzl first performed the procedure in a human being. Progress in defining the relative indications and contraindications for OLTx, refinements in the surgical technique, improved methods for diagnosing and treating rejection and more effective protocols to treat posttransplantation complications have resulted in establishing this procedure as an important addition to the clinical management of patients with chronic advanced liver disease. As the result of these accomplishments, OLTx is viewed currently as a rational long-term treatment for selected patients who have end-stage liver disease and would otherwise surely die.
The indications for liver transplantation, like those for any other surgical procedure, will vary and continue to evolve as success with the procedure improves. But because human and economic resources are limited, liver transplantation should be restricted, at least initially, to those patients with the greatest possibility of survival after the procedure. Thus, the selection of appropriate candidates for OLTx is a very important issue of interest to surgeons and physicians in an effort to delete from the cohort of potential candidates for the procedure those who will not survive the effort.
The prognosis for survival after OLTx surgery for any individual patient is not easily determined prior to the procedure. However, the availability of sophisticated methods of analysis and a large patient-specific database obtained prior to performance of the procedure makes attempts at such prognostication possible.
Child’s classification remains the most successful factor in predicting the operative mortality and estimating the surgical risk accrued in patients undergoing porta-systemic shunting procedures (8, 9). Elevated preoperative bilirubin levels and the presence of peroperative ascites have been shown to differentiate between probable survivors and nonsurvivors in several studies examining the prognosis of nonshunt laparotomy in cirrhotic patients (9). Previous studies by our own group have shown that the plasma levels of several thyroid hormones, T3, T4 and rT3, are important predictors of survival long enough to experience a transplant (10). The present study differs markedly from this earlier one, however, in that the population studied is quite different (those patients actually transplanted vs. those patients evaluated for transplantation), and the endpoints are very different (EMBI and survival after OLTx vs. survival long enough to have a transplant) (10).
To assess the risk factors associated with death and the development of a bacterial infection postoperatively, the latter being the most common fatal complication known to occur in adult patients undergoing liver transplantation (2), we reviewed the clinical and laboratory data obtained at admission from 93 consecutive adults who underwent liver transplantation at our institution. Because our analysis was retrospective, it should be remembered that there is a risk that some of our findings may be accidental.
Moreover because the pathogenesis of the variables examined are quite different in the various conditions studied (Table 1), it must be remembered that the current results represent mean observations for a wide spectrum of hepatic diseases, and as a result, the data obtained from this large unselected disease group may not apply directly to those in the smaller more selective disease groups. Certainly, it is well known that selected prognostic variables for mortality in primary biliary cirrhosis and alcoholic liver disease are not the same (11–13).
Nonetheless, we found seven preoperative variables that differentiated between survivors and nonsurvivors in patients undergoing liver transplantation. These variables included the presence of ascites and hepatic encephalopathy, elevated WBC and PMN leukocyte counts, bilirubin and creatinine levels, and a decreased helper to suppressor T lymphocyte ratio. However, when each of these seven preoperative variables was subjected to step-wise multivariant discriminant analysis, the plasma creatinine level was found to be the best predictor of survival or death. Using a properative creatinine level as the only predictor, a postoperative death could be predicted with an accuracy of 79% for those candidates with a creatinine level greater than 1.72 mg%. Adding the predictor effect of the second strongest factor, the total bilirubin level actually decreased the accuracy of the prediction to 76.1%.
As part of this analysis, we also have attempted to relate the risk of a posttransplantation bacterial infection with the same baseline clinical and laboratory data, with major infection being the endpoint. Only five preoperative variables (bilirubin, WBC and PMN leukocyte counts, IgG level and the creatinine level) were greater in patients who developed posttransplantation bacterial infections than in those who did not. The greatest risk factor for EMBI was the creatinine level, followed by the PMN leukocyte count. The risk of EMBI could be predicted with an accuracy of 72.2%.
In contrast with a previous report (14), we have not found the preoperative lymphocyte count, an indirect index of host resistance, to be useful index for predicting the development of a postoperative bacterial infection. In the same way, the helper to suppressor lymphocyte ratio, a reflection of the level of function of the cell-mediated immune system, was of no value in predicting the risk of a posttransplantation EMBI.
In conclusion, our results suggest that the preoperative creatinine level provides the best guide to the short-term prognosis of a given patient following OLTx. As a result, and based upon our earlier work (10), we believe that among a group of potential transplant candidates, the creatinine level and the level of various thyroid hormones in serum should be used to select the best candidates for liver transplantation.
Acknowledgments
Dr. Cuervas-Mons is the recipient of a grant from the Fonda de Investigaciones Sanitarias de la Seguridad Social of Spain.
References
- 1.Starzl TE, Iwatsuki S, Shaw BW, Jr, et al. Analysis of liver transplantation. Hepatology. 1984;4:47S–49S. doi: 10.1002/hep.1840040714. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cuervas-Mons V, Martinez AJ, Dekker A, et al. Adult liver transplantation: an analysis of the cause of death in 40 consecutive cases. Hepatology. 1986;6:495–501. doi: 10.1002/hep.1840060329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Starzl TE, Iwatsuki S, Van Thiel DH, et al. Evolution of liver transplantation. Hepatology. 1982;2:614–636. doi: 10.1002/hep.1840020516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van Thiel DH, Schade RR, Starzl TE, et al. Liver transplantation in adults. Hepatology. 1982;2:637–640. doi: 10.1002/hep.1840020517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van Thiel DH, Schade RR, Shaw BW, Jr, et al. Medical aspects of liver transplantation. Hepatology. 1984;4:79S–83S. doi: 10.1002/hep.1840040721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Romeder TM, Gremy F. In: Methods et programmes di analyse discriminante. Romeder TM, Maronda-Duhamel M, Garcon C, et al., editors. Paris, France: Dunod; 1971. pp. 109–130. [Google Scholar]
- 7.Sox HC. Probability theory in the use of diagnostic tests. Ann Intern Med. 1986;104:60–66. doi: 10.7326/0003-4819-104-1-60. [DOI] [PubMed] [Google Scholar]
- 8.Child CG, Turcotte JG. Surgery and portal hypertension. In: Child CG, editor. The liver and portal hypertension. Philadelphia, Pennsylvania: W. B. Saunders; 1964. pp. 1–85. [PubMed] [Google Scholar]
- 9.Doberneck RC, Sterling WA, Allison DC. Morbidity and mortality after operation in nonbleeding cirrhotic patients. Am J Surg. 1983;146:306–309. doi: 10.1016/0002-9610(83)90402-6. [DOI] [PubMed] [Google Scholar]
- 10.Van Thiel DH, Udani M, Schade RR, et al. Prognostic value of thyroid hormone levels in patients evaluated for liver transplantation. Hepatology. 1985;5:862–866. doi: 10.1002/hep.1840050526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Christensen E, Neuberger J, Crowe J, et al. Beneficial effects of azathioprine and prediction of prognosis in primary biliary cirrhosis. Gastroenterology. 1985;89:1084–1091. doi: 10.1016/0016-5085(85)90213-6. [DOI] [PubMed] [Google Scholar]
- 12.Christensen E, Schlichting P, Fauerbaldt L, et al. Changes of laboratory variables with time in cirrhosis: prognostic and therapeutic significance. Hepatology. 1985;5:843–853. doi: 10.1002/hep.1840050523. [DOI] [PubMed] [Google Scholar]
- 13.Orrego H, Israel Y, Blake JE, et al. Assessment of prognostic factors in alcoholic liver disease: toward a global quantitative expression of severity. Hepatology. 1983;3:896–905. doi: 10.1002/hep.1840030602. [DOI] [PubMed] [Google Scholar]
- 14.Lewis RT, Klein H. Risk factors in postoperative sepsis: significance of preoperative lymphocytopenia. J Surg Res. 1979;26:365–371. doi: 10.1016/0022-4804(79)90021-0. [DOI] [PubMed] [Google Scholar]


