Abstract
Background
The maternal and fetal risk of pregnancy after organ transplantation under tacrolimus has not been reported. This was prospectively studied in 27 pregnancies by 21 female liver recipients who were treated with tacrolimus before and throughout gestation.
Method
Twenty-seven babies were born between October 1990 and April 1996. In 15 cases, samples were obtained at or after delivery and stored (−40°C) for comparison of tacrolimus concentration in the maternal blood with different combinations of cord and infant venous blood, breast milk, or a section of the placenta.
Results
The 21 mothers had surprisingly few serious complications of pregnancy and no mortality. Two infants with 23 and 24 weeks gestation died shortly after birth. The mean birth weight of the other 25 was 2638±781 g after a gestational period of 36.6±3.3 weeks. Mean birth weight percentile for gestational age was 50.2±26.2 (median 40). On the day of delivery, the mean tacrolimus concentrations (ng/ml) were 4.3 in placenta versus 1.5, 0.7, and 0.5 in maternal, cord, and child plasma, and 0.6 in the first breast milk specimens. The infants had a 36% incidence of transient perinatal hyperkalemia (K+ > 7.0 meq/L) and a mild reversible renal impairment, which were thought to reflect in part maternal homeostasis. One newborn had unilateral polycystic renal disease (the only anomaly). All 25 babies have had satisfactory postnatal growth and development with a current mean weight percentile of 62±37 (median 80).
Conclusions
Pregnancy by postliver transplant mothers under tacrolimus was possible with a surprisingly low incidence of the hypertension, preeclampsia, and other maternal complications historically associated with such gestations. As in previous experience with other immunosuppressive regimens, preterm deliveries were common. However, prenatal growth for gestational age and postnatal infant growth for postpartum age were normal.
Successful pregnancies have been reported after liver transplantation under immune suppression based on azathioprine (1–3), cyclosporine (2–5) and tacrolimus. Although the number of reported pregnancies in tacrolimus-treated mothers is still small (6, 7), the experience reported herein suggests that this will be a frequent event with the widespread use of the new drug.
In this prospective study of 27 pregnancies in 21 hepatic recipients treated with tacrolimus, maternal and fetal events were recorded during gestation and afterward. At the time of delivery, tacrolimus concentrations were determined in samples of maternal, infant, and cord blood, and in the placenta and breast milk.
METHODS
Case Material
The 27 deliveries occurred between October 1990 and April 1996 in 21 liver recipients who had undergone transplantation at the University of Pittsburgh Medical Center. All but four of the deliveries were in the mothers’ cities of residence. The progress of the pregnancy and labor as well as results of renal and liver function tests, tacrolimus doses, and trough plasma/whole blood concentrations were communicated regularly to the investigators by the patients, their physicians, and obstetricians. The gestational period and the birth weight were recorded in all cases. Percentile intrauterine development was determined with the nomogram of Lubchenco et al. (8), which relates weight to gestational age at birth. The babies were followed after birth for a median of 39 months (range 10–76 months).
Perinatal Laboratory Studies
Maternal (n=15), cord (n=13), and infant venous blood, and a section of placenta (n=10) were collected at or after the time of delivery for determination of tacrolimus concentration. Serial follow-up samples of venous blood were obtained in 7 infants (11 samples) as well as breast milk from 6 mothers (10 samples). Tacrolimus concentrations were assayed in plasma by an ELISA procedure (9) until August 1994 and subsequently in whole blood by the microparticulate enzyme immunoassay method (IMx, Abbott Laboratories, Abbott Park, IL) (10), which gives a numerical readout approximately 10 times higher. The correlation coefficient with the two assays is r2 = 0.48 (n=101) (our unpublished observation). Placental tacrolimus concentrations were measured by either the ELISA or microparticulate enzyme immunoassay method. Renin and aldosterone concentrations in the maternal and cord plasma were measured with radioimmunoassay.
RESULTS
Maternal
The mean age of the 21 mothers at the time of the 27 deliveries was 28.1±5.2 (18.3 to 36.5). Delivery was by Caesarian section in 12 (44%) of the 27 pregnancies, most frequently because of maternal considerations but in several cases because of fetal danger (Table 1).
Table 1.
Maternal and infant characteristicsa
| Patient | Diagnosis before Tx | Mothers’ age (yr) | Months from liver transplantation to delivery | Months on tacrolimus to delivery | Gestation period (wk) | Boy/girl | Birth weight (g) | Birth weight percentile | Vaginal or Caesarian | Reason for Caesarian section | Previous obstetric history | Last infant follow-up time (mo) | Weight of baby on last follow-up (kg) | Growth weight percentile of babies |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1a | Caroli disease | 25.8 | 17.9 | 8.7 | 36 | boy | 2236 | 40 | c/s | Prev. c/s | g1p0b | 76 | 16.4 | <5 |
| 1b | 27.5 | 38.6 | 29.4 | 34 | boy | 2438 | 80 | c/s | Prev. c/s | g2p1 | 56 | 15.9 | 10 | |
| 2a | Pnc-C | 25.5 | 97.0 | 17.1 | 35 | girl | 2180 | 40 | v | g1p0 | 60 | 16.4 | 8 | |
| 2b | 27.4 | 120.6 | 40.6 | 40 | boy | 2410 | 10 | v | g2p1 | 36 | 16.4 | 80 | ||
| 3 | Pnc-E | 32.6 | 34.4 | 21.1 | 34 | girl | 1850 | 30 | c/s | Prev. c/s | g3p3 | 60 | 22.7 | 95 |
| 4 | PBC | 35.4 | 70.4 | 19.6 | 33 | girl | 1712 | 40 | c/s | Placenta abruptio | g1p1 | 60 | 21.8 | 90 |
| 5 | Hepatitis NANB | 31.2 | 22.3 | 22.3 | 40 | girl | 3912 | >90 | v | g2p2 | 63 | 31.4 | >95 | |
| 6 | Hepatitis AI | 18.3 | 20.0 | 20.0 | 38 | boy | 2580 | 25 | v | g1p0 | 60 | 22.9 | 95 | |
| 7 | 20.2 | 6.1 | 5.8 | 23c | – | 587c | v | g1p1 | na | na | na | |||
| 8 | FHF | 33.5 | 43.7 | 24.9 | 35 | girl | 2594 | 75 | v | g1p1 | 59 | 14.5 | 5 | |
| 9a | Pnc-E | 31.5 | 18.4 | 18.4 | 37 | boy | 2438 | 25 | v | g2p2 | 48 | 17.3 | 60 | |
| 9b | 35.6 | 67.6 | 67.6 | 37 | girl | 2585 | 30 | v | g3p3 | 10 | 9.3 | 55 | ||
| 10a | Pnc-C | 34.6 | 17.7 | 17.7 | 24c | – | 510c | c/s | Pre- eclampsia | g0p0 | na | na | na | |
| 10b | 36.5 | 39.7 | 39.7 | 32 | girl | 1565 | 50 | c/s | g1p0 | 36 | 12.7 | 20 | ||
| 11a | Hepatitis AI | 23.5 | 32.8 | 29.7 | 39 | boy | 3374 | 70 | v | g0p0 | 48 | 20.9 | >95 | |
| 11b | 25.8 | 65.3 | 57.2 | 28 | girl | 1632 | >90 | v | g1p1 | 24 | 10.9 | 20 | ||
| 12 | HBV | 24.6 | 45.3 | 41.6 | 31 | boy | 1215 | 15 | c/s | Fetal distress | g7p4 | 48 | 20.9 | >95 |
| 13 | HBV | 30.5 | 29.1 | 28.7 | 40 | boy | 3310 | 60 | c/s | Fetal distress | g0p0 | 40 | 15.4 | 50 |
| 14a | Wilson disease | 32.6 | 49.2 | 48.4 | 40 | boy | 4346 | >90 | v | g2p2 | 29 | 18.6 | >95 | |
| 14b | 34.1 | 67.6 | 67.2 | 40 | girl | 3693 | 80 | v | g3p3 | 10 | 10.0 | 85 | ||
| 15 | PBC | 24.3 | 33.5 | 33.5 | 36 | boy | 2980 | 70 | c/s | Delayed labor | g0p0 | 24 | 17.3 | >95 |
| 16 | PSC | 28.9 | 43.2 | 43.2 | 40 | girl | 2897 | 25 | v | g1p1 | 30 | 15.9 | >95 | |
| 17 | HBV | 23.9 | 66.2 | 46.7 | 36 | boy | 2159 | 20 | v | g0p0 | 24 | 15.9 | >95 | |
| 18 | FHF | 19.8 | 38.5 | 38.5 | 38 | girl | 2711 | 35 | c/s | Failure to progress | g0p0 | 30 | 11.4 | 10 |
| 19 | Wilson disease | 26.8 | 95.1 | 70.9 | 40 | boy | 3324 | 65 | v | g0p0 | 12 | 12.3 | >95 | |
| 20 | Hepatitis AI | 26.9 | 37.2 | 37.2 | 36 | girl | 2280 | 25 | c/s | Placenta previa | g0p0 | 17 | 11.0 | 62 |
| 21 | Con.hep.fibrosis | 22.3 | 31.7 | 31.7 | 40 | boy | 3522 | 75 | c/s | Prophylactic | g0p0 | 12 | 9.1 | 30 |
| Mean | 28.1 | 46.3 | 34.8 | 36.6 | 2638 | 50.2d | 39 | 16 | 62d | |||||
| SD | 5.2 | 27.2 | 19.5 | 3.3 | 781 | 26.2d | 20 | 5 | 37d | |||||
| Median | 27.4 | 38.6 | 31.7 | 37.0 | 2580 | 40d | 36 | 15.9 | 80d |
Abbreviations used in table: AI, autoimmune; C, cryptogenic; c/s, Caesarian; E, ethanol; FHF, fulminant hepatic failure; HBV, hepatitis B virus; NANB, non-A non-B hepatitis; na, not applicable; PBC, primary biliary cirrhosis; Pnc, post necrotic cirrhosis; PSC, primary slerosing cholangitis; v, vaginal.
g, gravida; p, parity.
Premature baby–died.
>90, >95, <5 were considered as 90, 95, 5, respectively, for calculation.
The full range of original liver diseases is summarized in Table 1. The adverse effect of liver failure on fecundity was reflected in the pretransplant inability of many patients to conceive (n=9) or to complete pregnancies (n=5) (Table 1).
All 21 women survived their single (n=15) or double (n=6) pregnancies. Nineteen of them are still alive and 18 still bear the same allografts as during the gestations. Patient 11 was noncompliant with immunosuppression throughout the second of two successful pregnancies, and underwent successful retransplantation for rejection 19 months after the birth of her second child.
The two deaths were not directly related to pregnancy. A 20-year-old patient (case 7) died 34 months postpartum. She conceived within 4 weeks after the primary liver transplantation, developed systemic cytomegalovirus during the first trimester of gestation, and gave vaginal birth at 23 weeks to a 587-g infant who died 2 hr later. She recovered promptly but a subsequent de novo hepatitis C virus infection necessitated retransplantation 30 months later with a 16-week survival. A 25-year-old mother (case 12) known for substance abuse died of a crack-cocaine overdose 40 months after delivery.
Hepatic allograft function
Although mean liver function was little affected (Table 2), there were perturbations during (n=4) or after (n=3) 7 of the 27 pregnancies. Anicteric rejections with transaminase or canalicular enzyme increases were observed in patients 4, 5, and 6 at 14, 16, and 33 weeks of gestation, respectively, and in patients 4 and 8 postpartum. These episodes responded to steroid boluses or modest increases in tacrolimus. The only example of chemical jaundice (maximum 2.9 mg/dl) was in pregnancy 11b, and this was attributed at the time to recurrent autoimmune hepatitis. However, with persistent noncompliance that led to rejection subsequent to delivery (and ultimately retransplantation), this earlier diagnosis was suspected to have been incorrect. In addition, liver injury tests were transiently elevated during systemic cytomegalovirus infection in the first trimester of pregnancy 7 and by recrudescent postpartum B virus hepatitis in pregnancy 17.
Table 2.
Effect of pregnancy on maternal liver and renal functiona
| Liver functionb |
Renal Functionb |
||||
|---|---|---|---|---|---|
| Bilirubin | AST | ALT | BUN | Creatinine | |
| Before | |||||
| Mean | 0.6 | 32.5 | 33.2 | 22 | 1.3 |
| SD | 0.3 | 19.5 | 22.7 | 8 | 0.5 |
| Median | 0.6 | 27 | 31 | 21 | 1.2 |
| First Trimester | |||||
| Mean | 0.5 | 28.7 | 25.5 | 18 | 1.2 |
| SD | 0.1 | 15.5 | 12.2 | 7 | 0.4 |
| Median | 0.5 | 26 | 24 | 18 | 1.2 |
| Second Trimester | |||||
| Mean | 0.6 | 30.5 | 30.5 | 15 | 1.1 |
| SD | 0.5 | 18 | 25 | 7 | 0.4 |
| Median | 0.45 | 23 | 23 | 13.5 | 1.1 |
| Third Trimester | |||||
| Mean | 0.6 | 28.9 | 26.5 | 15 | 1.2 |
| SD | 0.5 | 15.3 | 22.8 | 9 | 0.5 |
| Median | 0.4 | 27 | 18.5 | 13 | 1 |
| Postpartum | |||||
| Mean | 0.7 | 38.3 | 25.4 | 20 | 1.3 |
| SD | 0.4 | 50.4 | 21.6 | 12 | 0.5 |
| Median | 0.6 | 25 | 22.5 | 15 | 1.2 |
Abbreviations used in table: ALT, alanine aminotransferase; AST, aspartate aminotransferase; BUN, blood urea nitrogen.
Values after normalization (see the text). Bilirubin, mg/dl (1 mg/dl = 17 μmol/L, SI units); ALT, U/L; AST, U/L; creatinine, mg/dl (1 mg/dl = 88.4 μmol/L, SI units); BUN, mg/dl (1 mg/dl = 0.357 μmol/L, SI units).
Immune suppression
The duration of tacrolimus treatment and the interval from transplantation to delivery is shown for each patient in Table 1. Twelve of the 21 mothers had been switched to tacrolimus from cyclosporine (all before conception) because of persistent rejection and/or excessive steroid dependence. Prednisone was not given before or during 21 of the 27 pregnancies. It was administered during the other six pregnancies in daily doses of 5 (n=3), 7.5 (n=2), or 10 mg/day (n=1).
Patient 6, who required 48 to 64 mg/day tacrolimus to maintain trough plasma concentrations of 0.3–0.5 ng/ml, was the only one treated with adjunct azathioprine (50 mg/day). With omission of this patient’s data, mean doses and trough concentrations of tacrolimus before, during, and after the trimesters are shown in Table 3. Tacrolimus doses were modestly increased during 5 of the 27 pregnancies and decreased in 6.
Table 3.
Effect of pregnancy on immunosuppression
| Tacrolimus dosea (mg/day) | Tacrolimus levelb (ng/ml) | |
|---|---|---|
| Before | ||
| Mean | 10.3 | 0.7 |
| SD | 3.3 | 0.3 |
| Median | 11 | 0.6 |
| First Trimester | ||
| Mean | 9.7 | 0.7 |
| SD | 3.3 | 0.3 |
| Median | 10 | 0.7 |
| Second Trimester | ||
| Mean | 9.3 | 0.7 |
| SD | 3.6 | 0.5 |
| Median | 10 | 0.5 |
| Third Trimester | ||
| Mean | 10.1 | 0.5 |
| SD | 3.9 | 0.3 |
| Median | 10 | 0.45 |
| Postpartum | ||
| Mean | 9.8 | 0.8 |
| SD | 4 | 0.4 |
| Median | 10 | 0.65 |
Excludes patient 6 with colitis, receiving 48–64 mg/day.
Plasma level.
Renal function
Because tacrolimus dose adjustments were made at the first sign of nephrotoxicity, mean blood urea nitrogen and creatinine concentrations were stable during and after pregnancy (Table 2). Patients 8 and 10 had preexisting hypertension, which worsened in the latter case and required intensified treatment. New onset hypertension occurred in patient 5 during the first trimester and was treated for 1 week with methyldopa. Six of the 21 pregnant mothers required fludrocortisone to control hyperkalemia.
Insulin-dependent diabetes mellitus (IDDM*)
Patients 4 and 10 were insulin-dependent before conception, but the second patient had become insulin-free by her second pregnancy and subsequently remained insulin-free. There were no examples of new IDDM.
Infections
Patient 1 had a toenail infection during the second trimester of her first pregnancy. After her second delivery by Caesarian section, she developed wound infection and pneumonia. Except for a Salmonella infection during the third trimester (patient 4) and cytomegalovirus gastroenteritis during the first trimester (patient 7), no other infections were recorded.
Fetal
Survival
The birth weights of the two infants who died 2 hr and 2 days after 23 and 24 weeks gestation, respectively, were 587 (pregnancy 7) and 510 g (pregnancy 10a). The first mother was the one with a serious first trimester cytomegalovirus infection. The second, who had a subsequent successful pregnancy (10b), suffered from progressive hypertension, IDDM, and preeclampsia with proteinuria. The remaining 25 babies are alive and thriving. Except for one example of unilateral nonfunctional cystic kidney disease (pregnancy 14a), none have anomalies.
Development at birth
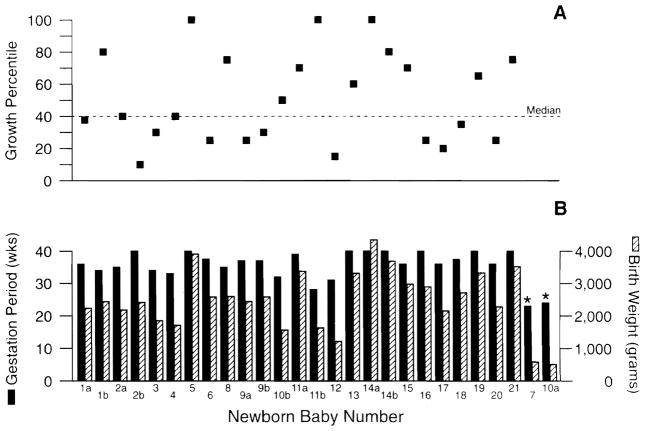
Birth weights and gestational periods for individual infants are shown in Table 1. Fourteen (52%) of the 27 babies were premature (gestational period <37 weeks) and the remaining 13 (48%) were term babies. Mean birth weight percentile for gestational age was 50.2±26.2 (range <10 to >90; median 40) (8); values are depicted for each surviving infant in Figure 1. Thirteen of the 25 were at or below the 40th percentile and 12 were above it. The two infants who died were off the Lubchenco scale.
Figure 1.
(A) Birth weight percentile of the newborn, derived from the weight for gestational age nomogram of Lubchenco et al. (8). (B) Gestation period in weeks (solid bar) and birth weight in grams (striped bar) for each newborn baby (*premature baby died).
Current development of newborn babies
The 25 babies who survived the perinatal period have been followed until January 1997 for a mean of 39±20 months (median 36). Their weight for age percentiles, calculated from the National Center for Health Statistics percentiles (11), are shown in Table 1. Some of the current scores reflect the degree of prematurity and low weight at birth. Five of the 25 babies have percentile growth of ≤10, whereas 10 babies have percentile growth >95. Both parents of the only infant with a current weight <5 percentile (case 1a) are of short stature (mother=4′11″, father=5′6″).
Perinatal complications
Most of the babies did not need unusual care. However, the small infants from pregnancies 11b and 18 required temporary ventilator support. After delivery by Caesarian section (because of fetal distress), the child from pregnancy 12 had prolonged hospitalization on oxygen.
Many of the first infants in the series had the postpartum sampling shown in Table 4. Elevations in the infants’ serum creatinine concentration, as well as hyperkalemia, were observed. Except for case 4, these abnormalities resolved spontaneously in 24–48 hr. In case 4, Caesarian section was performed at 33 weeks for abruptio placentae. The 1712-g infant was anuric for 36 hr, but the birth creatinine (3.2 mg, Table 4) peaked at 4.8 mg/100 ml and began to decline to normal by the third postnatal day.
Table 4.
Metabolic studies at the time of delivery
| Patient | Plasma aldosterone (ng/dl)a |
Plasma renin (ng/ml/hr) |
Newborn (Serum) |
|||
|---|---|---|---|---|---|---|
| Mother | Cord | Mother | Cord | Creatinineb | K+ (MEq/L) | |
| 1a | 62 | 43 | – | – | 1.1 | 10.9 |
| 1b | 8 | 15 | 2.8 | 1.2 | 1.3 | 6.8 |
| 2b | – | 11 | 5 | 3.2 | – | 5.5 |
| 3 | – | – | – | – | – | 8.2 |
| 4 | 61 | 32 | – | 1.3 | 3.2 | 6.1 |
| 5 | 58 | – | – | – | 1 | 4 |
| 6 | – | 40 | – | – | 0.9 | 7 |
| 8 | – | – | 15.4 | 27.1 | – | 5.8 |
| 9 | 13 | 15 | 8.4 | 17.2 | 2 | 7.5 |
| 10 | 3 | 4 | – | – | – | – |
| 11 | 27 | 49 | – | – | – | 6 |
| 12 | 80 | 70 | 7 | 4 | 0.8 | 6.6 |
| 13 | 28 | 23 | 10 | 8.6 | – | – |
Aldosterone, ng/dl (1 ng/dl = 0.028 nmol/L, SI units).
Creatinine, mg/dl (1 mg/dl = 88.4 μmol/L, SI units).
Aldosterone and renin concentrations in maternal plasma and cord plasma and serum creatinine and potassium in the newborn are summarized in Table 4. Because of wide variations in the aldosterone and renin concentrations, valid correlations could not be made between aldosterone, renin, and serum creatinine levels.
Maternal/fetal and blood brain barriers to tacrolimus
The maternal plasma concentrations of tacrolimus at the time of delivery and trough levels on subsequent days are shown in Table 5. These values exceeded those of cord blood in 11 of the 12 pregnancies from which samples were available. The only exception was in the pregnancy terminated by abruptio placentae (case 4), after which the infant had transient postnatal anuria. The median ratio of the cord plasma to maternal plasma concentration was 0.36.
Table 5.
Tacrolimus concentrations in perinatal specimens
| Patient | Days delivery | Tacrolimus concentrationa |
||||
|---|---|---|---|---|---|---|
| Mother blood (ng/ml) | Colostrum (ng/ml) | Placenta (ng/g) | Cord blood (ng/ml) | Baby blood (ng/ml) | ||
| 1a | 0b | 0.4 | 5.6 | 0.1 | ||
| 1 | 0.5 | 0.4 | ||||
| 2 | 4.1 | 1.9 | ||||
| 3 | 0.4 | |||||
| 1b | 0 | 3.2 | 0.4 | |||
| 1 | 1.1 | |||||
| 2b | 0 | 0.5 | 8.8 | |||
| 3 | 0 | 0.9 | 0.4 | |||
| 1 | 2.6 | 1 | 0.4 | |||
| 2 | 0.7 | 0.1 | ||||
| 4 | 0 | 2.1 | 1.9 | 3.1 | ||
| 1 | 4.3 | 1.4 | ||||
| 2 | 1.9 | 0.6 | ||||
| 5 | 0 | 2.6 | 0.2 | |||
| 1 | ||||||
| 2 | 0.3 | 0.1 | ||||
| 3 | 0.3 | 0.3 | 0.1 | |||
| 6 | 0 | 3.2 | 9.3 | 0.9 | ||
| 2 | 1.6 | 0.4 | ||||
| 7 | 0 | 1.2 | ||||
| 8 | 0 | 1.6 | 8.5 | 0.5 | ||
| 1 | 1.3 | 0.5 | ||||
| 2 | 2 | 0.9 | ||||
| 3 | 1.6 | 0.6 | ||||
| 9 | 0 | 0.8 | 1.1 | 0.4 | ||
| 1 | 0.8 | 0.4 | ||||
| 2 | 0.3 | 0.8 | ||||
| 10 | 0 | 2.5 | 1.6 | 0.9 | ||
| 11 | 0 | 1.1 | 0.9 | |||
| 12 | 0 | 2.1 | 3 | |||
| 13 | 0 | 1.7 | 0.3 | |||
| 1 | 0.6 | 1.7 | ||||
| 2 | 0.4 | 0.1 | ||||
| 14 | 0 | 1.1 (11.3)c | 5.9 (58.6)c | 0.8 (8.4)c | 0.8 (8.1)c | |
| 18 | 0 | .6 (6.1)c | 0.3 (2.9)c | 0.2 (1.7)c | ||
| Mean | 1.46 | 0.79 | 4.30 | 0.71 | 0.54 | |
| SD | 1.10 | 0.48 | 3.40 | 0.77 | 0.56 | |
| Median | 1.15 | 0.7 | 2.8 | 0.4 | 0.4 | |
Except for patients 14 and 18, values of maternal, cord, and baby blood were for plasma, and the plasma method was modified for the placenta and colostrum assays.
Day O=day of delivery.
Plasma estimated concentration is about one tenth of the whole blood or tissue concentration measured by IMx in patients 14 and 18.
In four infants, plasma tacrolimus was measured on consecutive days. Its rapid decline (cases 3, 4, and 13; Table 5) showed the ability of the newborn children to clear the drug.
The infants were protected from drug toxicity in utero by a partial placental barrier. In 9 of 10 placental samples, the tacrolimus concentration was 2 to 56 times that in cord blood, the only exception being with abruptio placentae (case 4). Placental tacrolimus also usually exceeded that of maternal plasma (median fourfold). A venous sample from an infant at the same time as placental delivery was obtained only in pregnancy 14; the placental concentration was seven times higher (Table 5).
In pregnancies 1b and 7, amniotic fluid concentration of tacrolimus was <0.2 ng/ml. The cerebrospinal fluid of the newborn baby from pregnancy 3 had a tacrolimus concentration of <0.1 ng/ml (immeasurable). Tacrolimus was present in all 10 breast milk samples from 6 mothers at almost half the concentration as in contemporaneous maternal samples (median ratio was 0.5).
DISCUSSION
Pregnancy under azathioprine or cyclosporine-based immune suppression has been a period of maternal and infant risk, even under the simpler circumstances of renal transplantation (12). The 1987 literature compilation by Davison (13) of 1569 completed pregnancies in 1009 kidney recipients revealed a 30% incidence of new onset hypertension and/or preeclampsia, significant loss of renal allograft function (most commonly caused by serious rejection) in 15% of the mothers, and a preterm delivery rate of 45–60% with intrauterine growth retardation in at least 20% of all gestations. The complication profile was much the same before and after the widespread use of cyclosporine (before and after 1983) except for more severe hypertension in the later period. Similar problems in 154 kidney recipients treated exclusively with cyclosporine regimens have been reported from a Pregnancy Registry established in Philadelphia in 1991 (14).
In contrast to the burgeoning pregnancies in the kidney transplant population, Scantlebury et al. (2) reported only 20 pregnancies in 17 patients who had undergone liver transplantation at the University of Colorado (n=3) or University of Pittsburgh (n=14) programs between June 1973 and June 1987. The first four pregnancies were under azathioprine immune suppression. The fourth mother permanently discontinued both azathioprine and prednisone shortly after delivery and remains drug-free 17 years later (15). The last 16 pregnancies were under cyclosporine-based therapy. The complications encountered were similar to those in kidney recipients of the two eras, and included an incidence of hepatic allograft dysfunction that was 37% during pregnancy and 53% in the postpartum period. Hypertension, preeclampsia, and premature delivery were common.
The increase of pregnancies in liver recipients with the advent of cyclosporine also was evident in a multicenter report 5 years later from the Philadelphia-based National Cyclosporine Registry (4) summarizing 500 live infant pregnancies in 335 women after kidney and extrarenal organ transplantation. Thirty-five (7%) of the 500 pregnancies were in patients whose liver transplantation was under cyclosporine and two were under tacrolimus. The 35 mothers had a high rate of serious hypertension (46%), eclampsia (21%), allograft rejection (17%), and graft loss (5.7%) (5). The infants tended to be small and premature.
This historically defined pattern of premature delivery and low infant birth weight was similar in the tacrolimus series reported herein. Although intrauterine immune suppression from any of the drugs used to date may be responsible per se for the subnormal fetal growth, it clearly is a reversible effect and does not distort embryogenesis unevenly. Two of the babies born to liver recipients under azathioprine/cyclosporine are now teenagers, and the first child of the tacrolimus era is 6.4 years old. In the tacrolimus babies reported herein, there was one (3.8%) nonlethal anomaly (unilateral nonfunctional cystic renal disease).
Tacrolimus given to the mother is transmitted in significant amounts to the fetus despite its concentration in the placenta, similar to cyclosporine (16–18). Temporary impairment of the infants’ renal function may be caused by tacrolimus, as has been previously reported with cyclosporine (19, 20). However, higher serum creatinine in newborn babies has been described after the pregnancies of normal women, and in part reflects the maternal creatinine (21, 22) as opposed to drug damage to the infant kidneys. Similarly, transient postnatal hyperkalemia due to incomplete maturation of the newborn kidneys’ potassium transport is not an unusual finding under normal circumstances (23). The obvious risk of adding potentially nephrotoxic drugs to these normal perinatal factors could be perpetuated by allowing the baby access to the mother’s milk with its high drug content. The hyperkalemia caused by tacrolimus has been ascribed in adults to low aldosterone and renin levels (24), a hypothesis that could not be adequately tested in the present study.
In contrast to the striking similarities of infant problems no matter what the baseline immune suppression (azathioprine, cyclosporine, and tacrolimus), maternal welfare was not commonly perturbed when tacrolimus was used from conception to delivery. The low incidence of hypertension, preeclampsia, and abnormalities in allograft function compared favorably with our, or any other, reported liver transplant experience. No allograft loss was attributed to pregnancy. These improvements are readily explained by advantages of tacrolimus versus cyclosporine in our own experience (25, 26) and in multicenter randomized trials (27–29): better control of rejection, less arterial hypertension, and reduced dependence on prednisone.
It is noteworthy that the two infant losses in the current series were by mothers whose conceptions were temporally close to liver transplantation. In pregnancy 7, the intervening period was only a few weeks, and in case 10a it was 11.7 months. In the failed pregnancy of case 10a, preexisting hypertension evolved into preeclampsia at a time when steroid weaning was incomplete and while the mother had temporary IDDM. After a 14-month rest and resolution of these problems, she conceived again and delivered a viable baby. We advise women of childbearing age to avoid pregnancy for 2 years after liver replacement, and for longer when there are (or have been) transplant-related management problems including steroid dependence.
In conclusion, successful pregnancy by postliver transplant mothers under tacrolimus was associated with a lower incidence of hypertension and preeclampsia than reported with previous immune suppression regimens, but with a similar trend of preterm delivery, low birth weight, and spontaneously resolving renal impairment of the infants.
Footnotes
This work was aided by project grant DK 29961 from the National Institutes of Health, Bethesda, Maryland.
Abbreviation: IDDM, insulin-dependent diabetes mellitus.
References
- 1.Penn I, Makowski EL, Harris P. Parenthood following renal and hepatic transplantation. Transplantation. 1980;30:397. doi: 10.1097/00007890-198012000-00001. [DOI] [PubMed] [Google Scholar]
- 2.Scantlebury V, Gordon R, Tzakis A, et al. Childbearing after liver transplantation. Transplantation. 1990;49:317. doi: 10.1097/00007890-199002000-00018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Laifer SA, Darby MJ, Scantlebury VP, Harger JH, Caritis SN. Pregnancy and liver transplantation. Obstet Gynecol. 1990;76(6):1083. [PubMed] [Google Scholar]
- 4.Radomski JS, Ahlswede BA, Jarrell BE, et al. Outcomes of 500 pregnancies in 335 female kidney, liver, and heart transplant recipients. Transplant Proc. 1995;27(1):1089. [PubMed] [Google Scholar]
- 5.Radomski JS, Moritz MJ, Munoz SJ, Cater JR, Jarrell BE, Armenti VT. National Transplantation Pregnancy Registry: analysis of pregnancy outcomes in female liver transplant recipients. Liver Transplant Surg. 1995;1(5):281. doi: 10.1002/lt.500010502. [DOI] [PubMed] [Google Scholar]
- 6.Jain A, Venkataramanan R, Lever J, et al. FK506 and pregnancy in liver transplant patients. Transplantation. 1993;56:1588. [PMC free article] [PubMed] [Google Scholar]
- 7.Winkler ME, Niesert S, Ringe B, Pichlmayr R. Successful pregnancy in a patient after liver transplantation maintained on FK506. Transplantation. 1993;56:1589. [PubMed] [Google Scholar]
- 8.Lubchenco LO, Hansman C, Boyd E. Intrauterine growth in length of head circumference as estimated from live birth at gestational ages from 26 to 42 weeks. Pediatrics. 1966;37:403. [PubMed] [Google Scholar]
- 9.Warty VS, Venkataramanan R, Zendelhrough P, et al. Practical aspects of FK506 analysis (Pittsburgh experience) Transplant Proc. 1991;23:2730. [PMC free article] [PubMed] [Google Scholar]
- 10.Grenier FC, Luczkiw T, Bergman M, et al. A whole blood FK506 assay for the IMx analyzer. Transplant Proc. 1991;23:2748. [PubMed] [Google Scholar]
- 11.Hamill PVV, Drizd TA, Johnson CL, Read RB, Roche AF, Moore WM. Physical growth: National Center for Health Statistics percentiles. Am J Clin Nutr. 1979;32:607. doi: 10.1093/ajcn/32.3.607. [DOI] [PubMed] [Google Scholar]
- 12.Bumgardner GL, Matas AJ. Transplantation and pregnancy. Transplant Rev. 1992;6(3):139. [Google Scholar]
- 13.Davison JM. Renal transplantation and pregnancy. Am J Kidney Dis. 1987;9(4):374. doi: 10.1016/s0272-6386(87)80140-3. [DOI] [PubMed] [Google Scholar]
- 14.Armenti VT, Ahlswede KM, Ahlswede BA, et al. National Transplantation Pregnancy Registry: outcomes of 154 pregnancies in cyclosporine-treated female kidney transplant recipients. Transplantation. 1994;57(4):502. [PubMed] [Google Scholar]
- 15.Starzl TE, Demetris AJ, Murase N, Trucco M, Thomson AW, Rao AS. The lost chord: microchimerism. Immunol Today. 1996;17:577. doi: 10.1016/s0167-5699(96)10070-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Venkataramanan R, Koneru B, Wang CP, et al. Cyclosporine and its metabolites in mother and baby. Transplantation. 1988;46:468. doi: 10.1097/00007890-198809000-00032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bourget P, Fernandez H, Bismuth H, et al. Transplacental passage of cyclosporine after liver transplantation. Transplantation. 1990;49:662. [PubMed] [Google Scholar]
- 18.Bourget P, Fernandez H, Delouis C. Accumulation of cyclosporine in the conceptus during the first trimester of pregnancy after liver transplantation. Transplantation. 1991;51:1306. doi: 10.1097/00007890-199106000-00033. [DOI] [PubMed] [Google Scholar]
- 19.Shaheen FAM, Al-Sulaiman MH, Al-Khader JA. Long-term nephrotoxicity after exposure to cyclosporine in utero. Transplantation. 1993;56(1):224. doi: 10.1097/00007890-199307000-00044. [DOI] [PubMed] [Google Scholar]
- 20.Klintmalm G, Althoff P, Appleby G, Segerbrandt E. Renal function in a newborn baby delivered of a renal transplant patient taking cyclosporine. Transplantation. 1984;38(2):198. [PubMed] [Google Scholar]
- 21.Metha KP, Karnik SR, Sathe A, Pant R, Khatwani R, Bhise A. Renal parameters during infancy. Indian Pediatr. 1992;29(11):1385. [PubMed] [Google Scholar]
- 22.Guignard JP. Renal function in a newborn infant. Pediatr Clin North Am. 1982;29:777. doi: 10.1016/s0031-3955(16)34211-0. [DOI] [PubMed] [Google Scholar]
- 23.Satlin LM. Maturation of renal potassium transport. Pediatr Nephrol. 1991;5:260. doi: 10.1007/BF01095968. [DOI] [PubMed] [Google Scholar]
- 24.McCauley J, Takaya S, Fung JJ, et al. The question of FK506 nephrotoxicity. Transplant Proc. 1991;23:1444. [PMC free article] [PubMed] [Google Scholar]
- 25.Fung JJ, Todo S, Jain A, et al. The Pittsburgh trial of tacrolimus versus cyclosporine for liver transplantation. J Am Coll Surg. 1996;183:117. [PMC free article] [PubMed] [Google Scholar]
- 26.Todo S, Fung JJ, Starzl TE, et al. Single center experience with primary orthotopic liver transplantation under FK506 immunosuppression. Ann Surg. 1994;220:297. doi: 10.1097/00000658-199409000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.The European FK506 Multicentre Liver Study Group (Writing Committee: : Neuhaus P, Pichlmayr R, William R) Randomized trial comparing tacrolimus (FK506) and cyclosporin in prevention of liver allograft rejection. Lancet. 1994;344:423. [PubMed] [Google Scholar]
- 28.The U.S. Multicenter FK506 Liver Study Group. A comparison of tacrolimus (FK506) and cyclosporine for immunosuppression in liver transplantation. N Engl J Med. 1994;331:1110. doi: 10.1056/NEJM199410273311702. [DOI] [PubMed] [Google Scholar]
- 29.Starzl TE, Donner A, Eliasziw M, et al. Randomized trialomania?: the multicenter liver transplant trials. Lancet. 1995;346:1346. doi: 10.1016/s0140-6736(95)92349-7. [DOI] [PMC free article] [PubMed] [Google Scholar]