INTRODUCTION
Research on whole systems of complementary and alternative medicine (WSCAM) [1–3] raises methodological questions concerning not only the use of individualized treatments with multiple components, but also the evaluation of patient-centered, whole person outcomes such as changes in a patient’s global status, and sense of wellness or well-being [4–7]. A key challenge is to design scientifically sound studies that have both internal and external validity from a WSCAM clinical perspective, including the assessment of positive outcomes, in addition to negative illness manifestations that are local and disease specific[8, 9].
WSCAM practices, such as traditional Chinese medicine, Ayurveda, homeopathy, and naturopathy (insert refs 10, 11), focus on the whole person indicators of health, including patients’ experienced global well-being [4, 10]. WSCAM clinicians assess the workings of multiple physiological subsystems concurrently and in relation to each other and rarely rely upon a single outcome (e.g., a single laboratory test biomarker) as evidence of “health” status. In contrast, most research designs emphasize evaluating static local outcomes for improvements in negatively-valenced symptoms and signs. Clinical studies that parse the person into separate local subsystems and investigate only disease- or lesion-specific outcomes and/or disease-related quality of life measures fail to capture evidence of actual clinical assessment practices of global outcomes and positive valences within a WSCAM framework.
Investigators have proposed using scientific concepts drawn from complex nonlinear dynamical systems theory towards improving the external validity of the clinical evidence base on WSCAM studies [8, 11, 12]. Several medical specialties are using methods of complex systems science to evaluate the functioning of body systems in an effort to increase diagnostic capability and assess patterns of disease [13–19]. Study designs such as these are well suited to non-reductive WSCAM studies that evaluate whole-person outcomes, because they attempt to quantify complex variables. In complexity theory the person is an indivisible complex adaptive system of interacting and interdependent parts, nested within and responsive/reactive to a complex environment. Synthesis of WSCAM with complexity theory suggests the need for characterizing WSCAM outcomes in terms of both (a) global and local outcomes and (b) positively and negatively valenced systemic behaviors (i.e., symptoms, signs) [8].
Psychologists have also utilized methods of complex systems science to investigate the concept of psychological flourishing. Flourishing is a “syndrome of positive feelings and positive functioning in life”[20], characterized by “goodness, generativity, growth, and resilience”[21], and is measured as self-reported well-being ratings. In a series of studies [21, 22], Losada, Heaphy, and Fredrickson have translated flourishing to a critical ratio of positive-to-negative affect (P:N), increasing accessibility of this concept as an objective marker of psychological health. Their body of work established the Losada line (P:N ≥ 2.9) as the key ratio where the nonlinear dynamics of human systems bifurcate into qualitatively opposite functional categories of optimal complexity (flourishing) versus less complexity (languishing).
How likely is it that an individual patient can change or increase their state of well-being? Patients commonly report “nonspecific effects” of treatment that are distinct from those relevant to their chief complaint, such as an increase in self-assessed positive affect and well-being following treatment by WSCAM [2, 10, 23–29]. Similarly, some patients report seeking WSCAM therapies in part to increase their sense of well-being [30]. Keyes [31] has shown important public health benefits of flourishing, extending his research to findings in the medical realm. Flourishing individuals have lower rates of cardiovascular and chronic disease, and decreased health care utilization, among other benefits, thus it is a worthwhile construct to explore.
Studies on non-clinical populations may provide estimates of the rates of optimal well-being to which clinical populations might aspire. An implicit assumption of a high level of global well-being is that the individual can not only overcome adversity, but also flourish in his or her life course [32]. Human beings commonly experience stress and environmental changes throughout their life cycle. Studies on the impact of adverse childhood experiences show that the number of such adverse experiences correlates with poorer mental, emotional, and physical health in adulthood [33–35]. Thus, an individual’s capacity to rebound from the impact of adverse events has major implications for long-term multidimensional well-being.
Resilience is the ability to bounce back or recover from stress [36, 37] and to show flexibility and adaptability to adverse life experiences [38, 39]. Previous research has demonstrated that resilient individuals use positive emotion to alleviate stress effects and show physiological differences in their ability to adapt to stress [32, 38]. Psychobiology research reveals that functional resilience differences among individuals stem from adaptive changes in neural circuitry in response to stress [39–41]. The more trait-like quality of resilience raises the question as to how much more of the variance in well-being it could explain. These studies suggest that there may be a global benefit to flourishing that merits evaluation as a marker of whole person health.
The purpose of this paper is to present a large sample study on a non-clinical young adult population that investigates the interrelationships between some previously-validated measures of whole person outcomes. First, we examine the relationships and relative contributions of global physical health, positive and negative mood separately and as the P:N, and resilience to integrative well-being ratings on a previously-validated scale, the Arizona Integrative Outcomes Scale (AIOS)[42]. This will determine whether the ratio of positive to negatively valenced mood has a unique relationship to overall well-being different from its individual components.
Secondly, we divide the sample into flourishers versus languishers using the P:N, to examine differences between flourisher and languisher groups on trait resilience. Fredrickson and Losada [43] have postulated that flourishers exhibit relatively higher levels of systemic resilience across biopsychosocial levels of organization in the face of stressors and other environmental changes. The paper concludes with a discussion of how these types of measures may benefit future WSCAM outcome studies.
METHODS
Sample & Design
We used data collected during one semester of the University of Arizona’s introductory psychology course. College students voluntarily participate in this research project screening exercise at the beginning of the semester. Because multiple investigators participate in this exercise, each investigator is limited to a set number of items, thus only limited demographic information is collected and available for analysis. Approximately 1200 students completed questionnaires, but 856 provided complete data for this analysis. All study methods and questionnaires were reviewed and approved by the University of Arizona Human Subjects Protection Program.
Measures
Arizona Integrative Outcomes Scale (AIOS, a global well-being scale)[44]: a one-item, 100-mm visual analogue scale (range 0–100, with higher scores indicating greater sense of well-being). Subjects self-rate their combined physical, mental, emotional, social, and spiritual sense of well-being in the present moment. AIOS was specifically developed for use in complexity theory-driven research in WSCAM, and has demonstrated to distinguish healthy from unhealthy populations as measured by physical health, and is inversely related to psychological distress.
Global Physical Health [45, 46] (GPH, the single item from the widely-used SF-36 medical outcomes scale [47]): a one-item, five-point Likert scale (range 1–5; higher scores indicate better perceived physical health) in which subjects rate their perceived level of physical health at the present time, ranging from “poor” to “excellent.” Prospective studies have shown that poorer global physical health ratings predict subsequent increases in mortality rates and health services utilization in elderly populations [46]. Self-rated global health is a better predictor of clinical outcomes than clinician assessments [48].
Positive and Negative Affect Schedule (PANAS)[49]: a 20-item, 5-point Likert rating of 10 positive and 10 negative state emotions, ranging from “very slightly” to “extremely” (score range, for both positive and negative valenced scales 10 to 50). The scale asks subjects to rate their feelings at the moment of survey completion. In this study, positive to negative affect ratio (P:N) is our main measure of flourishing [21].
Marlowe-Crowne Social Desirability Scale Short Form (MCSD-SF) [50]: a 13-item, true/false trait questionnaire for repressive defensiveness, i.e. the tendency to deny negative information about oneself (range 0–13, where 13=extremely defensive).
The Connor-Davidson Resilience Scale [51] is a validated 25-item scale (possible range 0–100) wherein subjects rate their degree of agreement with statements such as “I am able to adapt when changes occur” and “I believe I can achieve my goals, even if there are obstacles” referencing their feelings over the past month. Responses are graded on a 5-point scale ranging from “not true at all” to “true nearly all the time.”
Analysis
In addition to descriptive statistics, we ran Pearson correlations and performed a stepwise multiple linear regression analysis of the data. The stepwise regression analysis used the AIOS score as the dependent variable and, in order, entered the following variables as independent variables: demographics (age, sex), MCSD-SF, negative affect, positive affect, GPH, and resilience. Then, we examined the regression analysis using positive/negative ratio (P:N) instead of the separate positive and negative PANAS scores in the list of independent variables.
To further evaluate the categorical division of participants into flourishers versus languishers by the 2.9 Losada line bifurcation point, we divided the sample into two groups on the basis of their P:N score (10). That is, individuals with a P:N ≥ 2.9 were designated as “flourishers,” and persons with scores <2.9 were designated as “languishers.” We then used general linear model statistics controlling for age, sex, and MCSD-SF to compare the two groups on the AIOS and resilience measures.
RESULTS
Mean scores for all measures are represented in Table 1 (N=856). The average age of 19 years fell into the young adult range, and the sex distribution was 64% female. AIOS correlated significantly with MCSD-SF (r=0.22, p<0.001), positive PANAS score (r=0.37, p<0.001), negative PANAS score (r= −0.30, p<0.001), GPH (r=0.37, p<0.001), and resilience (r=0.49, p<0.001), as well as with the P:N (r=0.49, p<0.001). Resilience itself also correlated significantly with MCSD-SF (r=0.23, p<0.001), negative PANAS (r= −0.24, p<0.001), positive PANAS (r=0.38, p<0.001), GPH (r=0.29, p<0.001), and the P:N score (r=0.45, p<0.001).
Table 1.
Means and Standard Deviations for Study Variables (n=856)
| Mean ± SD | |
|---|---|
| Age | 18.9 ± 1.3 |
| Sex (% Female) | 64% |
| MCSD | 6.2 ± 2.7 |
| AIOS | 64.02 ± 18.3 |
| GPH | 3.57 ± 0.91 |
| PANAS Negative Affect | 17.03±6.4 |
| PANAS Positive Affect | 29.56±8.83 |
| P:N | 1.93 ± 0.82 |
| Resilience | 72.86±13.5 |
AIOS= Arizona Integrative Outcomes Scale; MCSD = Marlowe Crowne Social Desirability; GPH= Global Physical Health; P:N = Positive to Negative Affect ratio.
In the stepwise regression analysis the respective contributions of each independent variable to the variance of the AIOS value were: age 0%, sex 0.8%, MCSD-SF 5%, negative PANAS score 8.2%, positive PANAS score 12.9%, GPH 6.1%, and resilience 2.3%. In the regression analysis using P:N rather than the separate positive and negative mood scores, the respective contributions of each independent variable to the variance of the AIOS value were: 0% for age, 0.8% for sex, 5% for MCSD-SF, 18.9% for P:N, 6.3% for GPH, and 2.8% for resilience. Table 2 shows the standardized regression coefficients and their respective R2 values.
Table 2.
Regression Findings Predicting AIOS ratings
| β | Std. Error | t | R2 | ||
|---|---|---|---|---|---|
| Model with separate affect | |||||
| Constant | 31.92 | 8.694 | |||
| Age | −.41 | .42 | −.96 | .000 | |
| Sex | 1.62 | 1.16 | 1.40 | .008 | |
| MCSD | .396 | .22 | 1.85 | .050 | |
| PANAS Negative Affect | −.78 | .09 | −8.63** | .082 | |
| PANAS Positive Affect | .51 | .07 | 7.22** | .129 | |
| GPH | 4.82 | .65 | 7.45** | .061 | |
| Resilience | .24 | .05 | 5.21** | .023 | |
| Model with affect ratio | |||||
| Constant | 21.24 | 8.61 | |||
| Age | −.54 | .43 | −1.27 | .000 | |
| Sex | 1.32 | 1.17 | 1.13 | .008 | |
| MCSD | .36 | .22 | 1.63 | .050 | |
| P:N | 7.14 | .79 | 9.10** | .189 | |
| GPH | 4.79 | .65 | 7.36** | .063 | |
| Resilience | .27 | .05 | 5.73** | .028 | |
P<0.05,
P<0.001.
AIOS= Arizona Integrative Outcomes Scale; MCSD = Marlowe Crowne Social Desirability; GPH= Global Physical Health; P:N = Positive to Negative Affect ratio.
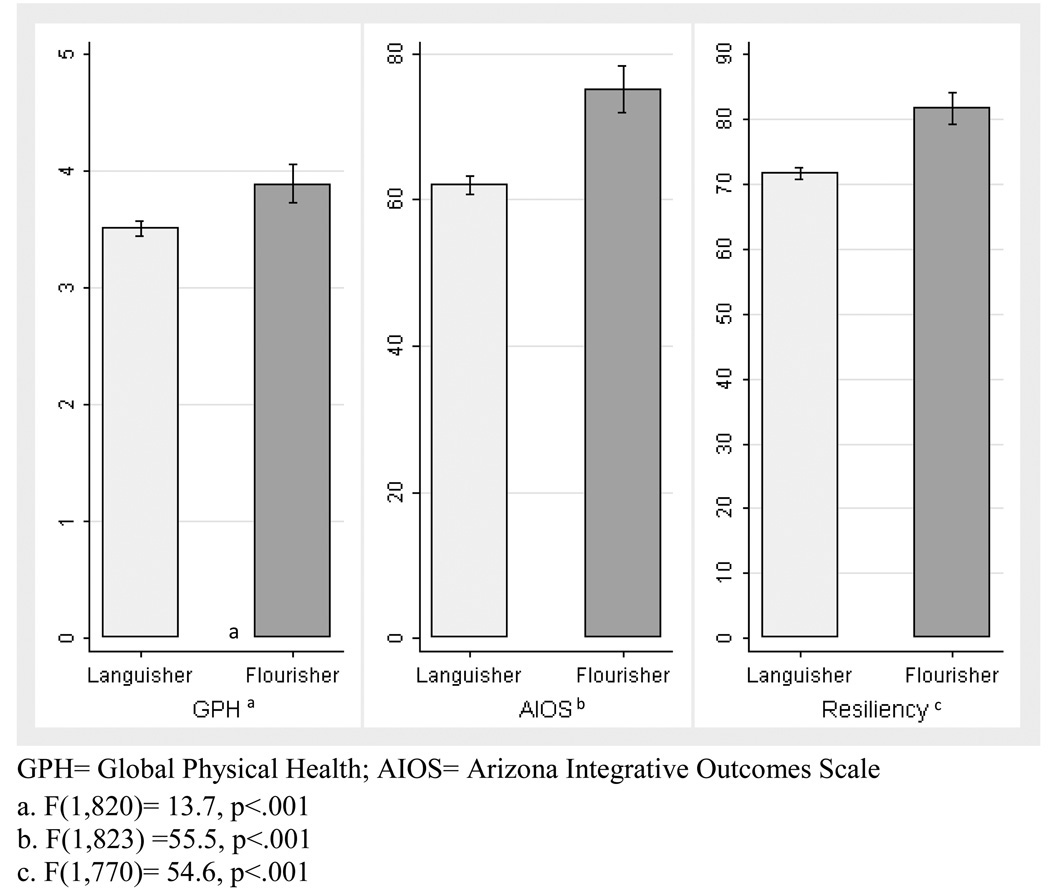
Flourishers defined as above by a P:N ≥2.9 represented 14.5% of the sample. There were significant differences between flourishers and languishers for P:N and defensiveness (MCSD). The mean P:N was 3.39 (SD 0.45) for flourishers versus 1.69 (SD 0.59) for the languishers, and the mean MCSD score was 7.7 (SD 2.6) for flourishers versus 5.9 (SD 2.6) for the languishers. After controlling for age, sex, and MCSD, the flourishers were still significantly higher than the languishers for AIOS, GPH, and resilience. Figure 1 shows the adjusted mean values for AIOS, GPH and resilience scores.
Figure 1.
Comparison of Flourishers to Languishers on GPH, AIOS and Resiliency.
DISCUSSION
The present study examined the relative contributions of psychological (trait and state) and physical health to an integrative measure of overall or global well-being in a sample of young adults early in their college careers. Previous studies have used well-being and methods of complex dynamical systems to establish the concept of psychological flourishing, which has been linked to better health outcomes. Because whole systems of complementary and alternative medicine include the assessment of symptom patterns and the dynamics of symptom and illness changes, complex systems methods may be applied to evaluate treatment outcomes.
We found that P:N had the strongest correlation with and accounted for the greatest amount of variance in global well-being ratings. The contribution of P:N was greater than that of positive and negative mood separately, and a physical health measure. Dividing the sample by the Losada line into flourishers and languishers showed that flourishers were significantly higher than languishers on well-being, global physical health, and resilience ratings. These observations are consistent with the characteristics of flourishers predicted by Fredrickson and Losada’s model [43]. They proposed four features of flourishing individuals, including goodness (happiness, satisfaction, superior functioning); generativity (behavioral flexibility and creativity); growth (gains in personal and social resources); and resilience (survival and growth after adversity).
In this study, 14.5% of the young adults fell into the flourisher category. This is lower than we might expect in a young, presumably healthy population. Young adult students at the beginning of their college career may experience significant stress levels, in part due to the psychosocial adjustments of being away from home and entering a new phase in life [52]. However, the high proportion of languishers in this sample of young adult college students brings into question the status of the general public outside of the clinical context.
Interestingly, the percentage of individuals who fit P:N criteria for flourishing in our study was lower than the 17.2% percentage found in a previous epidemiological study by Keyes of over 3000 adults in midlife (ages 25–74) [20]. Results of this study by age cohort suggest that individuals exhibit higher levels of flourishing later in life, with highest percentages occurring in the 45–65 age range (20.8–21.4%) and lowest percentages from ages 25–44 (14.7%) [20]. In this study, age 25 represents the youngest age included in the sample and therefore no direct comparison with our data can be made. Nonetheless, the evidence indicates that flourishing itself may have a curvilinear relationship with age.
Most patients seen by WSCAM providers are already older than the college students in this sample, with 50–60 years olds representing the highest percentage of adults seen[53], and many begin treatment with a substantial illness burden. As Lipsitz and Goldberger [54] have observed, aging itself leads to a loss of dynamical complexity, and multiple investigators have shown a loss of systemic complexity with a wide variety of mental, emotional, and physical disorders.
Prior research indicates that a P:N around 2.5 represents “normal” functioning in a system, whereas optimal functioning requires values over 4.0 [55, 56]. In the present studies, people who are flourishers appear to exhibit a somewhat higher but not extreme level of denial of negativity (higher MCSD-SF), a finding that suggests that some degree of denial of negativity may benefit people, allowing them to perceive themselves as doing better in their lives. Nonetheless, the “languishers” in the present study fell considerably below 2.5 in their P:N, with mean values of 1.69. A P:N of 1.8 leads to poor resilience under stress in Losada’s original research.
We raise the question of how these measures may be used to evaluate health care outcomes in future studies, viewing the patient as a dynamical system undergoing change. P:N and integrative well-being ratings may be important variables to include in prospective studies that track clinical progress and development of illness or recovery from illness with treatment. Including these variables in evaluation may be especially enlightening in outcomes studies of treatments that aim to treat individuals on physical and psychological levels, and address systems concurrently.
Limitations inherent to the study population are that the individuals sampled represent a predominantly young (mean age 19) presumably healthy population, the results of which may not generalize to the greater adult population.
Additionally, the data presented in this study is cross-sectional, represents one time point, measuring subjects’ experience at the time of survey completion. It therefore does not represent normal fluctuations in mood and sense of well-being that occur over time and vary situationally. Data collected over a span of time at multiple time points would be more reflective of overall, as opposed to momentary, health and well-being status and may yield more dramatic results. The study uses brief, versus more comprehensive measures to assess self-assessed health and well-being status. Whether these brief surveys are the most accurate proxy measures of psychological and health status remains the subject of further research. However, the aims in this study were exploratory, and it is encouraging that group differences emerged, even within this limitation.
The current correlational data offer no evidence of causality. Owens et al’s findings from their earlier cross-sectional clinical study showing that higher positive PANAS mood scale scores correlated with higher CAM effectiveness ratings are also intriguing, but provide no indication of causality [57]. Further prospective studies should address whether higher P:N at the beginning of treatment is necessary for truly optimal recovery, whether P:N changes with treatment and clinical outcomes, and whether P:N has any causal relationship to WSCAM effects.
Another limitation is the reliance on brief self-ratings rather than comprehensive questionnaires and complete clinical evaluations. Previous evidence that self-rated global health is a better predictor of subsequent outcomes than are clinician evaluations strengthens the case for the present global measures[58, 59], given their relatively low subject burden. However, additional assessments such as measures of stress, energy (e.g., vigor, fatigue from the Profile of Mood States Scale), positive states of mind [60], specific local symptom patterns, and biomarkers at rest and under controlled stressors would provide a more complete picture of individual status at baseline and over time. Additionally, further research on clinically meaningful differences on scores over time would help interpret these findings and apply in practice.
Further studies are needed to determine the utility of these measures in clinical settings, across broad populations of different demographics. Additionally, studies assessing mean P:N and AIOS scores by age cohort will aid the interpretation of ratings in clinical situations.
Future studies could also improve understanding of the possible interactions between baseline individual differences in P:N and the individualized treatment package in generating the heterogeneous outcomes seen in clinical care. The four measures used in this study correlated positively, with the strongest associations being between P:N with AIOS and resilience, and between AIOS and resilience. It is possible that AIOS (state measure) and resilience measure (trait measure) similar individual characteristics, and that the constructs of well-being and resilience show some overlap. Further studies with other populations that show greater score variation will be instructive.
The Fredrickson and Losada model implies that the P:N may be predictive of outcomes in a complex system such as a human being. They note that the P:N relates mathematically to the control parameter for the nonlinear attractor dynamics of a system. Knowing the P:N thus helps predict whether the system (e.g., person, dyad, or social group) will develop, under adversity, the complex dynamics of flourishing or the more rigid dynamics of languishing.
This line of reasoning suggests that the ratio of positive to negative mood or positive to negative behaviors under external stressors or demands could determine whether or not a system can ultimately undergo optimal outcomes and express full well-being. Thus, applying complex systems theory and science to additional studies of the non-clinical population across various age groups could improve our understanding of the general nature of well-being and human flourishing. Can interventions targeting P:N and flourishing improve well-being? Complex systems theory-driven studies in patients on the process of whole person healing could open an important new direction for patient-centered research on individual differences in WSCAM outcomes. The present studies provide an initial step toward this goal.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Ritenbaugh C, Verhoef M, Fleishman S, Boon H, Leis A. Whole systems research: a discipline for studying complementary and alternative medicine. Altern Ther Health Med. 2003;9(4):32–36. [PubMed] [Google Scholar]
- 2.Verhoef M, Lewith G, Ritenbaugh C, Thomas K, Boon H, Fonnebo V. Whole systems research: moving forward. Focus on Alternative and Complementary Therapies. 2004;9(2):87–90. [Google Scholar]
- 3.Verhoef MJ, Lewith G, Ritenbaugh C, Boon H, Fleishman S, Leis A. Complementary and alternative medicine whole systems research: Beyond identification of inadequacies of the RCT. Complement Ther Med. 2005;13(3):206–212. doi: 10.1016/j.ctim.2005.05.001. [DOI] [PubMed] [Google Scholar]
- 4.Gould A, MacPherson H. Patient perspectives on outcomes after treatment with acupuncture. Journal of Alternative and Complementary Medicine. 2001;7:261–268. doi: 10.1089/107555301300328133. [DOI] [PubMed] [Google Scholar]
- 5.Koithan M, Verhoef M, Bell IR, Ritenbaugh C, White M, Mulkins A. The process of whole person healing: "unstuckness" and beyond. J Altern Complement Med. 2007;13(6):659–668. doi: 10.1089/acm.2007.7090. [DOI] [PubMed] [Google Scholar]
- 6.Jonas WB, Chez RA. Toward optimal healing environments in health care. J Altern Complement Med. 2004;10 Suppl 1:S1–S6. doi: 10.1089/1075553042245818. [DOI] [PubMed] [Google Scholar]
- 7.Beck DM, Dossey BM, Kines W. Local action and global networking: the Nightingale Initiative for Global Health. Explore (NY) 2007;3(1):64–69. doi: 10.1016/j.explore.2006.10.011. [DOI] [PubMed] [Google Scholar]
- 8.Bell IR, Koithan M. Models for the study of whole systems. Integrative Cancer Therapies. 2006;5(4):293–307. doi: 10.1177/1534735406295293. [DOI] [PubMed] [Google Scholar]
- 9.Ritenbaugh C, Hammerschlag R, Calabrese C, Mist S, Aickin M, Sutherland E, Leben J, Debar L, Elder C, Dworkin SF. A pilot whole systems clinical trial of traditional Chinese medicine and naturopathic medicine for the treatment of temporomandibular disorders. J Altern Complement Med. 2008;14(5):475–487. doi: 10.1089/acm.2007.0738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bell IR, Koithan M, Gorman MM, Baldwin CM. Homeopathic practitioner views of changes in patients undergoing constitutional treatment for chronic disease. Journal of Alternative & Complementary Medicine. 2003;9(1):39–50. doi: 10.1089/107555303321222937. [DOI] [PubMed] [Google Scholar]
- 11.Bell I, Koithan M. Patient-Centered Research on Whole Systems of Complementary and Alternative Medicine: A Complex Systems Science Perspective (Part I: Concepts) 2009 doi: 10.1159/000335181. Submitted for publication. [DOI] [PubMed] [Google Scholar]
- 12.Bell I, Koithan M. Patient-Centered Research on Whole Systems of Complementary and Alternative Medicine: A Complex Systems Science Perspective (Part II: Applications) 2009 doi: 10.1159/000335181. Submitted for publication. [DOI] [PubMed] [Google Scholar]
- 13.Bell IR, Caspi O, Schwartz GE, Grant KL, Gaudet TW, Rychener D, Maizes V, Weil A. Integrative medicine and systemic outcomes research: issues in the emergence of a new model for primary health care. Arch Intern Med. 2002;162(2):133–140. doi: 10.1001/archinte.162.2.133. [DOI] [PubMed] [Google Scholar]
- 14.Costa M, Ghiran I, Peng CK, Nicholson-Weller A, Goldberger AL. Complex dynamics of human red blood cell flickering: alterations with in vivo aging. Phys Rev E Stat Nonlin Soft Matter Phys. 2008;78(2 Pt 1) doi: 10.1103/PhysRevE.78.020901. 020901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Goldberger AL, Peng CK, Lipsitz LA. What is physiologic complexity and how does it change with aging and disease? Neurobiol Aging. 2002;23(1):23–26. doi: 10.1016/s0197-4580(01)00266-4. [DOI] [PubMed] [Google Scholar]
- 16.Goldberger AL. Giles f. Filley lecture. Complex systems. Proc Am Thorac Soc. 2006;3(6):467–471. doi: 10.1513/pats.200603-028MS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goldberger AL. Heartbeats, hormones, and health: is variability the spice of life? Am J Respir Crit Care Med. 2001;163(6):1289–1290. doi: 10.1164/ajrccm.163.6.ed1801a. [DOI] [PubMed] [Google Scholar]
- 18.Higgins JP. Nonlinear systems in medicine. Yale J Biol Med. 2002;75(5–6):247–260. [PMC free article] [PubMed] [Google Scholar]
- 19.Costa M, Goldberger AL, Peng CK. Broken asymmetry of the human heartbeat: loss of time irreversibility in aging and disease. Phys Rev Lett. 2005;95(19) doi: 10.1103/PhysRevLett.95.198102. 198102. [DOI] [PubMed] [Google Scholar]
- 20.Keyes CL. The mental health continuum: from languishing to flourishing in life. J Health Soc Behav. 2002;43(2):207–222. [PubMed] [Google Scholar]
- 21.Fredrickson BL, Losada MF. Positive affect and the complex dynamics of human flourishing. Am Psychol. 2005;60(7):678–686. doi: 10.1037/0003-066X.60.7.678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Losada M. The Complex Dynamics of High Performance Teams. Mathematical and Computer Modeling. 1999;30:179–192. [Google Scholar]
- 23.Paterson C, Britten N. Acupuncture for people with chronic illness: combining qualitative and quantitative outcome assessment. Journal of Alternative & Complementary Medicine. 2003;9(5):671–681. doi: 10.1089/107555303322524526. [DOI] [PubMed] [Google Scholar]
- 24.Paterson C, Dieppe P. Characteristic and incidental (placebo) effects in complex interventions such as acupuncture. BMJ. 2005;330(7501):1202–1205. doi: 10.1136/bmj.330.7501.1202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Paterson C. Measuring changes in self-concept: a qualitative evaluation of outcome questionnaires in people having acupuncture for their chronic health problems. BMC Complement Altern Med. 2006;6(1):7. doi: 10.1186/1472-6882-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Verhoef MJ, Casebeer AL, Hilsden RJ. Assessing efficacy of complementary medicine: adding qualitative research methods to the "Gold Standard". J Altern Complement Med. 2002;8(3):275–281. doi: 10.1089/10755530260127961. [DOI] [PubMed] [Google Scholar]
- 27.Paterson C, Baarts C, Launsø L, Verhoef MJ. Evaluating complex health interventions: a critical analysis of the 'outcomes' concept. BMC Complement Altern Med. 2009;9:18. doi: 10.1186/1472-6882-9-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bell IR, Caspi O, Schwartz GE, Grant KL, Gaudet TW, Rychener D, Maizes V, Weil A. Integrative medicine and systemic outcomes research: issues in the emergence of a new model for primary health care. Archives of Internal Medicine. 2002;162(2):133–140. doi: 10.1001/archinte.162.2.133. [DOI] [PubMed] [Google Scholar]
- 29.Verhoef MJ, Vanderheyden LC, Dryden T, Mallory D, Ware MA. Evaluating complementary and alternative medicine interventions: in search of appropriate patient-centered outcome measures. BMC Complement Altern Med. 2006;6:6–38. doi: 10.1186/1472-6882-6-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Caspi O, Koithan M, Criddle MW. Alternative medicine or "alternative" patients: a qualitative study of patient-oriented decision-making processes with respect to complementary and alternative medicine. Medical Decision Making. 2004;24(1):64–79. doi: 10.1177/0272989X03261567. [DOI] [PubMed] [Google Scholar]
- 31.Keyes CL. Promoting and protecting mental health as flourishing: a complementary strategy for improving national mental health. Am Psychol. 2007;62(2):95–108. doi: 10.1037/0003-066X.62.2.95. [DOI] [PubMed] [Google Scholar]
- 32.Fredrickson BL, Tugade MM, Waugh CE, Larkin GR. What good are positive emotions in crises? A prospective study of resilience and emotions following the terrorist attacks on the United States on September 11th, 2001. J Pers Soc Psychol. 2003;84(2):365–376. doi: 10.1037//0022-3514.84.2.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, Koss MP, Marks JS. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine. 1998;14(4):245–258. doi: 10.1016/s0749-3797(98)00017-8. [comment]. [DOI] [PubMed] [Google Scholar]
- 34.Dong M, Giles WH, Felitti VJ, Dube SR, Williams JE, Chapman DP, Anda RF. Insights into causal pathways for ischemic heart disease: adverse childhood experiences study. Circulation. 2004;110(13):1761–1766. doi: 10.1161/01.CIR.0000143074.54995.7F. [DOI] [PubMed] [Google Scholar]
- 35.Dube SR, Felitti VJ, Dong M, Giles WH, Anda RF. The impact of adverse childhood experiences on health problems: evidence from four birth cohorts dating back to 1900. Prev Med. 2003;37(3):268–277. doi: 10.1016/s0091-7435(03)00123-3. [DOI] [PubMed] [Google Scholar]
- 36.Smith B, Dalen J, Wiggins K, Tolley E, Christopher P, Bernard J. The Brief Resilience Scale: Assessing the Ability to Bounce Back. International Journal of Behavioral Medicine. 2008;15:194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- 37.Agnes ME. Webster's New College Dictionary. Cleveland, OH: Wiley; 2005. [Google Scholar]
- 38.Tugade MM, Fredrickson BL. Resilient individuals use positive emotions to bounce back from negative emotional experiences. J Pers Soc Psychol. 2004;86(2):320–333. doi: 10.1037/0022-3514.86.2.320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Feder A, Nestler EJ, Charney DS. Psychobiology and molecular genetics of resilience. Nat Rev Neurosci. 2009;10(6):446–457. doi: 10.1038/nrn2649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Charney DS. Psychobiological mechanisms of resilience and vulnerability: implications for successful adaptation to extreme stress. Am J Psychiatry. 2004;161(2):195–216. doi: 10.1176/appi.ajp.161.2.195. [DOI] [PubMed] [Google Scholar]
- 41.Stein DJ. The psychobiology of resilience. CNS Spectr. 2009;14(2) Suppl 3:41–47. doi: 10.1017/s1092852900027280. [DOI] [PubMed] [Google Scholar]
- 42.Bell IR, Cunningham V, Caspi O, Meek P, Ferro L. Development and validation of a new global well-being outcomes rating scale for integrative medicine research. BMC Complement Altern Med. 2004;4:1. doi: 10.1186/1472-6882-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Fredrickson BL, Losada MF. Positive affect and the complex dynamics of human flourishing. American Psychologist. 2005;60(7):678–686. doi: 10.1037/0003-066X.60.7.678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Bell IR, Cunningham V, Caspi O, Meek P, Ferro L. Development and validation of a new global well-being outcomes rating scale for integrative medicine research. BMC Complementary & Alternative Medicine. 2004;4(1):15. doi: 10.1186/1472-6882-4-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Idler EL, Kasl S. Health perceptions and survival: do global evaluations of health status really predict mortality? Journal of Gerontology. 1991;46(2):S55–S65. doi: 10.1093/geronj/46.2.s55. [DOI] [PubMed] [Google Scholar]
- 46.Idler E, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–36. [PubMed] [Google Scholar]
- 47.Ware JE, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Medical Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 48.Mossey JM, Shapiro E. Self-rated health: a predictor of mortality among the elderly. American Journal of Public Health. 1982;72(8):800–808. doi: 10.2105/ajph.72.8.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: the PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- 50.Reynolds WM. Development of reliable and valid short forms of the Marlowe-Crowne Social Desirability Scale. Journal of Clinical Psychology. 1982;38:119–125. [Google Scholar]
- 51.Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depression & Anxiety. 2003;18(2):76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 52.Kennedy C, Kassab O, Gilkey D, Linnel S, Morris D. Psychosocial factors and low back pain among college students. J Am Coll Health. 2008;57(2):191–195. doi: 10.3200/JACH.57.2.191-196. [DOI] [PubMed] [Google Scholar]
- 53.Barnes PM, Powell-Griner E, McFann K, Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004;(343):1–19. [PubMed] [Google Scholar]
- 54.Lipsitz LA, Goldberger AL. Loss of 'complexity' and aging. Potential applications of fractals and chaos theory to senescence. JAMA. 1992;267:1806–1809. [PubMed] [Google Scholar]
- 55.Schwartz RM, Reynolds CF, III, Thase ME, Frank E, Fasiczka AL. Optimal and Normal Affect Balance in Psychotherapy of Major Depression: Evaluation of the Balanced States of Mind Model. Behavioural and Cognitive Psychotherapy. 2002;30(30):439–450. [Google Scholar]
- 56.Gottman JM, Levenson RW. The Timing of Divorce: Predicting When a Couple Will Divorce over a 14-year Period. Journal of Marriage and the Family. 2000;62(3):737–745. [Google Scholar]
- 57.Owens JE, Taylor AG, Degood D. Complementary and alternative medicine and psychologic factors: toward an individual differences model of complementary and alternative medicine use and outcomes. Journal of Alternative & Complementary Medicine. 1999;5(6):529–541. doi: 10.1089/acm.1999.5.529. [DOI] [PubMed] [Google Scholar]
- 58.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. [PubMed] [Google Scholar]
- 59.Mossey JM, Shapiro E. Self-rated health: a predictor of mortality among the elderly. Am J Public Health. 1982;72(8):800–808. doi: 10.2105/ajph.72.8.800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Horowitz M, Adler N, Kegeles S. A scale for measuring the occurrence of positive states of mind: a preliminary report. Psychosomatic Medicine. 1988;50:477–483. doi: 10.1097/00006842-198809000-00004. [DOI] [PubMed] [Google Scholar]