Abstract
Only one prior study has examined why adolescent smoking cessation interventions are effective. To address this understudied and important issue, this study examined whether a large adolescent smoking cessation intervention trial’s outcomes were mediated by Social Cognitive Theory processes. In a randomized trial (N = 2,151), counselors proactively delivered a telephone intervention to senior year high school smokers. Mediators and smoking status were self-reported at 12 months post-intervention-eligibility (88.8% retention). At-least-6-months abstinence was the outcome. Among all enrolled smokers, increased self-efficacy to resist smoking in (a) social & (b) stressful situations together statistically mediated 55.6% of the intervention’s effect on smoking cessation (p <.0001). Among baseline daily smokers, increased self-efficacy to resist smoking in stressful situations statistically mediated 56.9% of the intervention’s effect (p < .001). Self-efficacy to resist smoking is a possible mediator of the intervention’s effect on smoking cessation.
Keywords: Social Cognitive Theory, mediators, intervention, adolescents, smoking cessation
Currently, 26.5% of US high school seniors smoke monthly (Centers for Disease Control and Prevention, 2008), which is disappointingly higher than the Healthy People 2010 goal of 16% (U.S. Department of Health and Human Services, 2000). Adolescent daily smokers are of great concern. There are additional health risks associated with daily smoking (Holmen, Barrett-Connor, Holmen, & Bjermer, 2000). Adolescent daily smokers tend to smoke into adulthood (Holmen et al., 2000) and have a higher risk of progressing to other drug dependencies (Henningfield, Clayton, & Pollin, 1990). Theoretically, daily smoking is a key indicator of the construct of nicotine dependence (Heatherton, Kozlowski, Frecker, Rickert, & Robinson, 1989).
Hutchinson Study of High School Smoking
To help address the serious problem of adolescent smoking, we conducted a group-randomized trial of adolescent cessation (N = 2,151): the Hutchinson Study of High School Smoking (HS Study). A key trial outcome, which the reader can find fully reported in Peterson et al. (2009), was a near doubling of at-least-6-months prolonged abstinence among baseline daily smokers (10.1% vs. 5.9%, p =.02). Additionally, there was a nearly conclusive increase in at-least-6-months prolonged abstinence among all baseline smokers (21.8% vs. 17.7%, p = .06). In a commentary on the findings, Leischow & Matthews (2009) stated that the results are “remarkable for multiple reasons, not least because it is the first to show substantial quit rates in adolescent smokers at 6 months after quitting.”
These main results are consistent with the overall treatment effects of other teen smoking cessation interventions, although the vast majority of these trials have been non-randomized, had low recruitment, poor retention, small sample sizes, short-duration cessation outcome measures, and short follow-up periods (Sussman, 2006). Whereas two prior trials proactively recruited adolescent smokers through participating pediatric or family practice clinics (Hollis et al., 2005; Pbert et al., 2008), the HS Study is the first adolescent smoking cessation trial to report increases in at-least-6-months prolonged abstinence, as measured 12-months-post-intervention-eligibilty, among a large proactively recruited population of adolescent smokers in a non-medical (i.e., community-based) setting.
This current study aims to help explain these results by examining the extent to which the intervention changed underlying processes (i.e., mediators) intended to be targeted by the intervention. Notably, while the HS intervention effect was nearly significant (p = .06) for all enrolled smokers, significant mediation may exist whether or not there is a statistically significant effect of the intervention on smoking behavior (MacKinnon, 2008; Mackinnon & Fairchild, 2009; MacKinnon, Fairchild, & Fritz, 2007). Overall, explaining these results is valuable for helping determine why the intervention worked for daily smokers and was almost effective for all smokers. Revealing what theoretical processes need to be targeted more effectively provides guidance on how to improve future interventions in adolescent smoking cessation.
Social Cognitive Theory: Conceptual basis of the HS Intervention
The HS smoking cessation intervention was based on Social Cognitive Theory (SCT; Bandura, 1986). Consistent with SCT, attitudes longitudinally predicting adolescent smoking cessation include the individual’s perceived importance of quitting (Branstetter, Horn, Dino, & Zhang, 2009), commitment to quitting smoking (McCuller, Sussman, Wapner, Dent, & Weiss, 2006), motives for smoking (Myers, McCarthy, MacPherson, & Brown, 2003) and motives for quitting (Solomon, Bunn, Pirie, Worden, & Flynn, 2006). To attempt to change these SCT-based processes in the appropriate direction, the HS intervention utilized Motivational Interviewing (MI; Miller & Rollnick, 2002).
Based on SCT, another attitude longitudinally predicting adolescent smoking cessation is an overall higher confidence (i.e., self-efficacy) in being able to quit smoking (Woodruff, Conway, & Edwards, 2008). The overall confidence to quit smoking is partly derived from two types of behavioral processes: the perceived abilities (i.e., self-efficacy) to resist smoking in the presence of (a) stressful situations and (b) social situations (Engels, Knibbe, de Vries, & Drop, 1998).
Environmental influences on smoking cessation include family members, peers, and the media who, through modeling, can shape an adolescent’s perception that smoking is normative (i.e., social norms for smoking; Fagan, Eisenberg, Stoddard, Frazier, & Sorensen, 2001). To attempt to change these SCT-based processes in the appropriate direction, the HS intervention utilized Cognitive Behavioral Skills Training (CBST; Baer, Kivlahan, & Donovan, 1999).
Prior research on mediation of adolescent smoking cessation interventions
Little is known about why adolescent smoking cessation interventions can be effective. Indeed, little is known about how psychological interventions work (Murphy, Cooper, Hollon, & Fairburn, 2009). To date, only one published study has reported on the extent to which adolescent smoking cessation trial outcomes could be explained by a given intervention’s effect on any (much less SCT-based) mediating processes (McCuller et al., 2006). The study found that 26% of Project EX’s effect on 30-day adolescent smoking abstinence was accounted for by increases in motivation to quit smoking.
This Study
The purpose of this study is to learn the extent to which the HS intervention cessation outcomes were mediated by SCT-based theoretical processes intended to be changed by the MI and CBST clinical processes. Specifically, this study determined the extent to which the HS intervention results for (a) all enrolled smokers and (b) daily smokers were statistically mediated by SCT-based theoretical processes of smoking cessation.
Compared to the only prior study on the topic of mediation of adolescent cessation interventions (McCuller et al., 2006), the current trial provided the following key advances: (1) large sample size (N = 1,911 vs. 172), (2) 12-month follow-up (vs. 3-month), (3) strong retention (88.8% vs. 51%), (4) examination of eight theory-based mediators (vs. one), (5) use of 6-months of prolonged abstinence (vs. 30-day point prevalence), (6) use of the higher-powered Sobel test (Sobel, 1986) of mediation [vs. the lower-powered Baron & Kenny (1986) method].
The HS trial’s randomized design also facilitated determining the extent to which the intervention impacted SCT-based processes. The trial measured SCT-based processes at baseline and at the same time as the smoking abstinence outcome measures, but not at an intermediate point (e.g., at end of treatment), in order to reduce participant burden and to efficiently deliver the intervention to a large number of participants. However, this data limitation raises the question of whether the SCT-based processes actually impacted the smoking cessation outcomes since it is possible that the SCT-based processes changed after (rather than before) the smoking outcomes (Kraemer, Wilson, Fairburn, & Agras, 2002; Murphy et al., 2009). A study design to address this critical issue is difficult to create because the effects of the mediator are often rapid (Murphy et al., 2009). Moreover, as discussed above, theory suggests and research shows that the SCT-based mediators longitudinally predict adolescent smoking cessation. Finally, a number of recent adult smoking cessation studies have conducted mediational analyses with a design similar to the current study (e.g., Stanton, Lloyd-Richardson, Papandonatos, de Dios, & Niaura, 2009).
Methods
Study sample
The HS trial was conducted in 50 public high schools located throughout Washington State (Peterson et al. 2009). To achieve the goal of 50 participating high schools, 59 high schools were randomly selected and contacted for recruitment, yielding a recruitment rate of 84.7%. Reasons for school declines were current involvement in other similar studies (3 schools), unwillingness to provide student and parent names and contact information (3 schools), and lack of time for extra activities (3 schools). The 50 participating schools had an average enrollment of 1,224 students (SD = 527.7). The average percentage of students eligible for free/reduced price school meals, an indication of a school’s socio-economic status, was 24.6% (SD: 13.7%). The communities in which the schools were located included both rural and urban populations, and were diverse in size, ranging in population from under 1,000 to nearly 600,000.
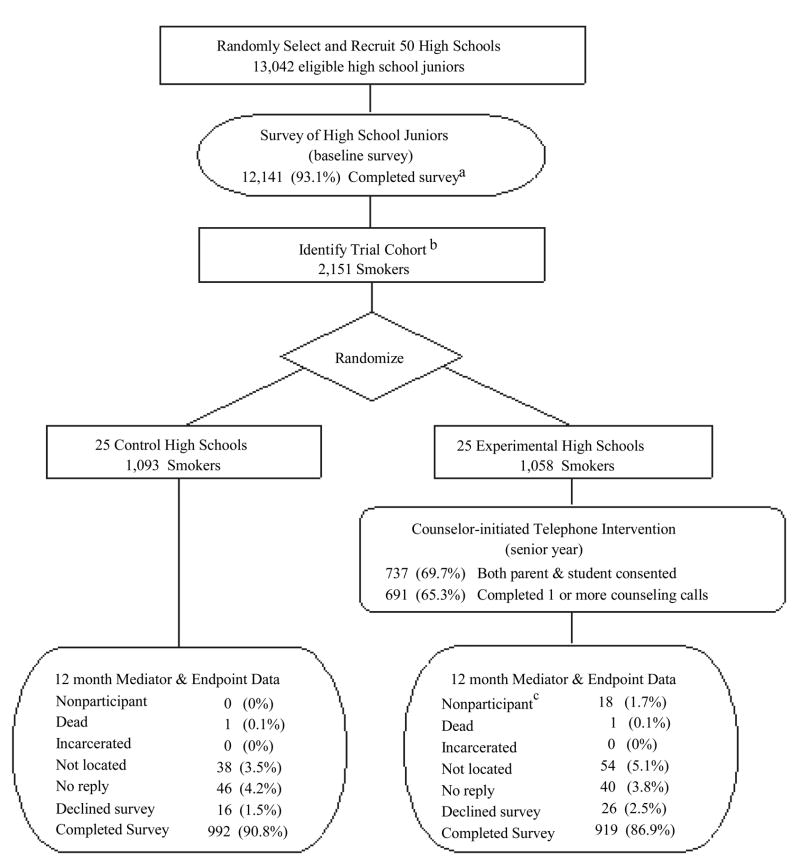
The trial cohort consisted of 2,151 smokers, identified via self-report, using the study-administered classroom survey designed both to identify smokers for recruitment and to provide baseline data (including mediator data) for the trial. In the 50 schools, 12,141 (93.1%) of 13,042 eligible juniors completed a baseline survey (Liu et al., 2007). (Of the 901who did not complete a survey, 524 (4.0%) did not reply to the follow-up telephone or mailed survey after being absent during the in-class surveys, and 377 (2.9%) actively declined via parent or teen decision.) A total of 2,175 smokers were identified; 24 (1.1%) declined contact for future activities, leaving 2,151 (98.9%) eligible for the trial. As shown in Figure 1, 1,911 (n = 992 in experimental; n = 919 in control) of the 2,151 (88.8%) eligible for the trial completed the 12-month mediator and outcome survey. These 1,911 individuals comprised the eligible population for this study. In addition, there was a small amount of missing data among the study population (N = 1,911), ranging from 1.67% (social norms) to 5.49% (confidence to quit smoking) with an average of 3.45%. Such a small amount of missing data has a negligible impact on study results (Lin, 2006; Rubin, 1987; Schafer, 1997; Zhang & Walker, 2008). Smoker participants, fully described in Liu et al. (2007), were 47% female and 25% non-White (7.2% Multiple races/ethnicity, 5.4% Hispanic, 4.9% Asian, 2.6% Native American, 2.5% African American, and & 1.4% Native Hawaiian or other Pacific Islander). Most were aged 16 (30.5%) or 17 (62%).
Figure 1.
HS Study experimental design.
Note. aOf the 901 (6.9%) who did not complete baseline survey: 524 (4.0%) absent/no reply, 377 (2.9%) declined. bTwenty-four smokers who declined further contact were excluded. cTrial participants who declined study participation post randomization.
To include a broad range of adolescent smoking patterns, all enrolled trial participant smokers were those who reported monthly or more smoking via a positive response to any of the following three baseline survey items: (a) How often do you currently smoke cigarettes? (responded “once a month or more, but less than once a week;” “once a week or more, but not daily;” or “at least daily”); (b) Have you smoked one or more cigarettes in the last 30 days? (responded “yes”); and (c) When was the last time you smoked, or even tried, a cigarette? (responded “8–30 days ago;” “1–7 days ago;” or “earlier today”). These definitions, and steps for identifying and recruiting smokers, were identical in the control and experimental conditions, thereby avoiding any selection bias in identifying the trial participants.
Experimental design
As shown in Figure 1, the HS trial used a two-arm, group-randomized design. The experimental unit was the high school, chosen to allow for supportive interaction among intervened smokers in the same high school, to capitalize on any associated synergism for smoking cessation, and to mimic one likely mode of disseminating the intervention (i.e., in schools) in the event it were proven effective. Of 50 participating high schools, 25 were randomly assigned to the HS cessation intervention condition and 25 were assigned to the (no-intervention) control condition.
For trial management reasons in this large study, the 50 participating high schools were recruited over a span of three years (“waves”), Fall (Sep–Nov) 2001 to 2003. All subsequent activities also occurred in waves: baseline data collection in Spring (Mar–May) 2002–2004, intervention implementation in (Sep–Jun) 2003–2005, and endpoint data collection in (Sep–Dec) 2004–2006. All participants in a Wave were assigned to one of six batches, comprised of both experimental and control participants, for follow-up to outcome. Each batch’s experimental cohort participants were assigned for intervention, one batch every four weeks, beginning at the start of the senior year. Once experimental participants in a batch became eligible for intervention, all participants in the batch, both experimental and control, were scheduled for outcome survey 12 months later.
Following the “intent-to-treat” tenet of good experimental design (Gail, 1985), all 2151 eligible teen smokers at baseline remained part of the trial and were tracked for follow-up, including those who dropped out. These analyses conservatively underestimated the smoking cessation effects of the HS intervention since the level of attrition in the experimental group was 3.9% higher than in the control group (13.14% vs. 9.24%, p <.01).
A matched-pair randomization was performed for each of the 25 pairs of high schools matched on prevalence of smoking, number of smokers, stage of readiness to quit, and percentage of students eligible for free/reduced-price school meals. Schools were randomly ordered within each matched pair, and then one school in each pair was randomly assigned to the experimental condition by a computerized coin flip that was performed openly, witnessed, and recorded. The HS trial experimental design, procedures, and intervention were reviewed and approved in advance and annually by the Hutchinson Center’s Institutional Review Board.
SCT-based intervention
The HS telephone counseling used MI and CBST guided by SCT (Bandura, 1986). Intervention delivery was guided by a documented intervention protocol (Kealey et al., 2009). Specific counseling content and number of calls were personalized to the participant’s readiness to quit and progress toward quitting—as opposed to a pre-set order of intervention delivery. As a personalized intervention, any given call to a study participant could vary from either providing MI to a combination of MI and CBST. The intervention was delivered in a non-linear and flexible manner in response to the needs of the individual at the time of the call, to accommodate the ebb and flow of the adolescent’s motivation to quit, and other individual circumstances. Smokers had an average of 2.83 calls (Median = 3).
We reported that the calls showed the following independently-rated MI-specific protocol adherence: for the two global scores, 96.2% of calls achieved or exceeded the proficiency benchmark for Empathy, and 99.1% achieved or exceeded the benchmark for MI spirit (Kealey et al., 2009). Ratings for Empathy and MI Spirit indicated advanced proficiency while 97.2% of calls achieved or exceeded the benchmark for ratio of reflections to questions, and 85.7% of calls achieved or exceeded benchmark for MI-adherence. With respect to independently-rated CBST-specific protocol adherence, counselors established that the participant was ready for the quit attempt in 100% of calls, helped smokers set goals and assessed abstinence challenges in 90% of calls, helped smokers develop action plans in 80% of calls, and helped smokers set a quit date in 60% of calls.
As we have reported in the past (Kealey et al., 2007), the HS trial was successful in proactively identifying, recruiting, and retaining a high percentage of eligible adolescent smokers to the smoking cessation telephone counseling intervention: (1) 85.9% (669/779) of parents of minor-age smokers provided parental consent, and as a result, 89.6% (948/1058) of proactively identified smokers in the experimental condition were intervention eligible (by consent or by age); (2) 72.9% (691/948) intervention-eligible smokers participated in telephone counseling; and (3) 72.2% (499/691) of participating smokers completed all their scheduled counseling calls. Overall, 65.3% of the 1,058 smokers proactively identified in 25 experimental condition high schools participated in the telephone counseling, and nearly half (47.2%) completed all of their counseling calls.
Endpoint data collection
When participants were age 19, which was 12-months post-intervention eligibility, we collected mediator and smoking data by mail. We followed up non-responders by mail and telephone. The overall follow-up rate was 88.8% (1,911/2,151) of all eligible smokers.
Measures of SCT-based mediators
The HS intervention utilized MI (Miller & Rollnick, 1991, 2002) to attempt to change four SCT-based processes in the appropriate direction. Measures of these four SCT-based processes, using items similar to those in research predicting adolescent smoking cessation, were (1) importance of quitting (Branstetter et al., 2009), (2) commitment to quitting smoking (Branstetter et al., 2009; McCuller et al., 2006), (3) smoking motives (Chassin, Presson, Pitts, & Sherman, 2000; Dalton, Sargent, Beach, Bernhardt, & Stevens, 1999; Myers et al., 2003) and (4) quitting motives (Solomon, et al., 2006). The HS intervention utilized Cognitive Behavioral Skills Training (CBST; Baer et al., 1999; Marlatt & Gordon, 1985) to attempt to change four other SCT-based processes in the appropriate direction. Measures of these four SCT-based processes, using items similar to those in research predicting adolescent smoking cessation, were (1) self-efficacy to quit smoking (Woodruff et al., 2008), (2) self-efficacy to resist smoking in stressful situations (Engels et al., 1998), (3) self-efficacy to resist smoking in social situations (Solomon et al., 2006), and (4) social norms for smoking (Fagan et al., 2001).
The means and standard deviations for these mediator scales (and pertinent subscales) at baseline are shown along the diagonal in the table of correlations (See Table 1). As shown in Table 1, with the exception of importance of quitting and commitment to quitting (r =.67; p <.01), the measures had small to moderate correlations with each other, with a mean (and standard deviation) of the absolute values of the correlations of .18 (.15). The signs of these correlations were in the expected directions. These correlations suggested they were related but distinct measures. Supporting this descriptive evidence of discriminant validity, the oblimin rotation principal components factor analysis, yielding twelve factors explaining 97.69% of the variance, indicated the mediator variables had high loadings (range: .885 to 1.000) on their corresponding factors and low cross loadings (range: .001 to .047). The exception was that importance of quitting and commitment to quitting both loaded on the same factor (.889 for importance and .885 for commitment) but we elected to keep them separate since SCT and MI views these as separate yet related constructs.
Table 1.
Correlations between and individual means (standard deviations) of SCT-based mediators at baseline
| SCT-based Mediator | 1. | 2. | 3a. | 3b. | 3c. | 3d. | 4a. | 4b. | 4c. | 5. | 6. | 7. | 8. |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Importance of quitting a | 3.10 (.97) | ||||||||||||
| 2. Commitment to quittinga | .67** | 3.31 (.87) | |||||||||||
| 3. Smoking motives b | |||||||||||||
| 3a. Identity as a smokerc | −.02 | −.09** | 1.16 (.80) | ||||||||||
| 3b. Social acceptabilityd | .006 | −.10** | −.001 | 1.23 (1.13) | |||||||||
| 3c. Exercising choicee | −.18** | −.13** | .16* | .29** | .69 (.80) | ||||||||
| 3d. Feelings/pleasuresf | −.08** | −.06* | .36** | .33** | .35** | 1.17 (.95) | |||||||
| 4. Quitting motivesb | |||||||||||||
| 4a. Self-controlg | .26** | .20** | −.19** | −.22** | .26** | −.30** | 1.43 (1.47) | ||||||
| 4b. Healthh | .29** | .26** | −.13** | −.21** | .13** | −.22** | .50** | 1.65 (1.08) | |||||
| 4c. Relief of social pressurei | .17** | .15** | −.05* | −.17** | .14** | −.19** | .40** | .32** | .97 (1.11) | ||||
| 5. Confidence to quita | .21** | .34** | −.44** | .04 | −.05* | −.19** | .12** | .08** | −.04 | 3.20 (.90) | |||
| 6. Self-efficacy to resist: sociala | .23** | .21** | −.38** | −.06* | .05 | −.18** | .03 | .04 | .02 | .44** | 2.31 (1.21) | ||
| 7. Self efficacy to resist: stressfula | .17** | .21* | −.44** | −.05 | .09** | −.25** | .11** | .07** | .03 | .51** | .54** | 1.99 (1.13) | |
| 8. Social normsj | −.03 | .02 | .10** | .04 | −.04 | .00 | −.10** | .03 | .04 | −.09** | −.06* | −.11** | 3.17 (1.12) |
Note. Sample sizes for correlations ranged from 1806 to 1879.
Responses: “not at all” (coded “1”), “only a little” (coded “2”), “fairly” (coded “3”), and “very” (coded “4”).
Responses checked off were coded as “1” and those not checked off were coded “0”. All responses to each subscale were scored by summation.
(two-item scale; KR-20 reliability = .57).
(four-item scale; KR-20 reliability = .56).
(two-item scale; KR-20 reliability = .62).
(three-item scale; KR-20 reliability = .51).
(four-item scale; KR-20 reliability = .79).
(three-item scale; KR-20 reliability = .63).
(four-item scale; KR-20 reliability = .58).
Responses: “strongly agree” (coded “1”), “agree” (coded “2”), “don’t know” (coded “3”), “disagree” (coded “4”), and “strongly disagree” (coded “5”).
p < .05.
p < .01.
Endpoint measure of six-month prolonged smoking abstinence
The main abstinence endpoint was 6-month prolonged abstinence, which captures the period of highest risk of relapse (Hughes et al., 2003). Three items measured this abstinence outcome: (1) When was the last time you smoked, or even tried, a cigarette? (response choices: “I have never smoked, or even tried, a cigarette,” “Earlier today,” “1–7 days ago,” “8–30 days ago,” “Between 1 month and 3 months ago,” “Between 3 months and 6 months ago,” “Over 6 months ago”); (2) How often do you currently smoke cigarettes? (response choices: “Not at all,” “Less than once a month,” “Once a month of more, but less than once a week,” “At least daily”); (3) Think about the last 30 days. On how many of the last 30 days have you smoked one or more cigarettes? (response choices: “Every day,” “20–29 days,” “10–19 days,” “5–9 days,” “2–4 days,” “1 day,” “0 days”). In accordance with recommendations that the endpoint measure be taken at least 6 months after the start of intervention (Mermelstein et al., 2002), the HS endpoints were collected 1 year after a participant became eligible for intervention. This was done to allow up to six months for the participants to receive the intervention. The adoption of this definition provides a common ground for comparisons of results across studies. In order to be classified as abstinent, a participant had to respond “over 6 months ago” to the first item and “not at all” to the second item and “0 days” to the third item.
Mediation Analysis
To examine the extent to which the HS intervention outcomes were mediated by the hypothesized SCT-based processes, we used the Sobel test of mediation (MacKinnon, Lockwood, Hoffman, West, & Sheets, 2002; Sobel, 1982, 1986). Specifically, the first regression model examined the effect of the independent variable X (HS intervention group vs. control group) on smoking cessation [Model 1: E(Y)= λ1+τX]. The second regression model examined the effect of the independent variable X on the mediator M [Model 2: E(M)= λ2+αX]. Because there were no baseline imbalances between the experimental and control groups on the SCT-based measures of mediators targeted by this MI and CBST intervention (all p >.05), only the mediators at endpoint were used in the analysis. The third regression model examined the simultaneous impact of the independent variable X and mediator M on the smoking cessation endpoint Y [Model 3: E(Y)= λ3+τ′ X+βM]. Finally, the mediation effect is described as the change in the magnitude of the intervention effect after the mediator is added into the model (τ – τ′), which is algebraically equivalent to α · β for ordinary least-squares regression (Mackinnon, Warsi, & Dwyer, 1995). Each of the mediator analyses were performed for the following a priori-defined groups: (1) all enrolled smokers and (2) daily smokers. Note that daily smokers contribute to the model involving all enrolled smokers. All the mediation analyses of the eight hypothesized mediators were planned analyses performed both separately and again together for all individual mediators that were significant (MacKinnon, 2000).
The mediation analysis accommodated three special design and data features of the HS study. (1) Baseline imbalance in smoking frequency: There were no baseline differences (all p >.05) between the intervention and control groups on any of the SCT-based mediators, achievement motivation, social support, perceived stress and many other factors known to predict adolescent smoking (for further information, see Liu, et al., 2007). While the intervention and control groups were comparable, the experimental arm included a higher percentage of baseline daily smokers than the control arm (39.9% vs. 34.5%, p < .05; Liu, et al., 2007). We adjusted for the difference in the level of baseline daily smokers by including baseline smoking frequency as a covariate in all of the regression models. (2) Binary outcome: The parameter a in the second regression model was estimated via linear regression model and the parameter b in the third regression model was estimated via logistic regression model, resulting in regression coefficients with different scales. To create estimates with the same scale, the scaling method suggested by MacKinnon & Dwyer (1993) was used to standardize the two regression coefficients and to obtain the unbiased estimate of mediation before applying the Sobel test. (3) Intraclass correlation: Due to the group nature of the random assignment, the intraclass correlation among smokers within the same school was accommodated in the regressions with an intraclass correlation using the GEE estimation method. Due to the negligible impact of the small levels of missing data on study results (Lin, 2006; Rubin, 1987; Schafer, 1997; Zhang & Walker, 2008), all missing data were handled through pairwise deletion.
Results
SCT mediation of HS intervention for all enrolled smokers
As shown in Table 2, the intervention had a significant effect on increasing two processes targeted by CBST: (1) self-efficacy to resist smoking in social situations (α̂ = 0.119, p < .01) and (2) self-efficacy to resist smoking in stressful situations (α̂ = 0.119, p < .05). In addition, there was a strongly suggestive effect on increasing one process targeted by MI: commitment to quitting smoking (β̂ = 0.085, p = .06). The following mediators were significantly associated with higher levels of smoking cessation: (1) importance of quitting smoking (β̂ = 1.382, p < .0001), (2) commitment to quitting smoking (β̂ = 1.160, p < .0001), (3) three smoking motives subscales (identity as a smoker, β̂ = −0.927, p < .0001; social acceptability of smoking, β̂= − 0.211, p < .01; feelings/pleasure from smoking, β̂ = −0.582, p < .0001), (4) confidence to quit smoking (β̂ = 1.168, p < .0001), (5) self-efficacy to resist smoking in social situations (β̂ = 1.171, p < .0001), and (6) self-efficacy to resist smoking in stressful situations (β̂ = 1.124, p < .0001). The CBST-targeted processes of self-efficacy to resist smoking in social situations and self-efficacy to resist smoking in stressful situations mediated 49% ( , SE = 0.022, p < .05) and 31% ( , SE = 0.024, p < .05), respectively, of the intervention’s effect on smoking cessation. These two variables together mediated 55.6% ( , SE = 0.020, p < .0001) of the intervention’s effect on smoking cessation. [There was also a suggestive mediation effect of the MI-targeted process of commitment to quitting ( , SE = 0.024, p = .06, results not shown in table)].
Table 2.
Among all enrolled smokers, effect of HS Intervention on SCT-based mediators, association between mediators and smoking cessation, and mediation effects of the HS intervention (N=1911).
| SCT-based mediators | Mediation path | Mediation effect ( c) | ||
|---|---|---|---|---|
| α̂a | β̂b | Estimate | Standard errord | |
| SCT-based mediators primarily targeted by Motivational Interviewing | ||||
| Importance of quitting smoking | 0.068 | 1.382*** | 0.039 | 0.030 |
| Commitment to quitting smoking | 0.085† | 1.160*** | 0.044 | 0.024 |
| Smoking motives | ||||
| Identity as a smoker | 0.005 | −0.927*** | −0.002 | 0.003 |
| Social acceptability | 0.061 | −0.211** | −0.007 | 0.010 |
| Exercising choice | −0.006 | −0.129 | 0.000 | 0.003 |
| Feelings/pleasures | 0.022 | −0.582*** | −0.007 | 0.016 |
| Quitting motives | ||||
| Self-control | −0.003 | 0.044 | −0.000 | 0.002 |
| Health | 0.011 | 0.204 | 0.001 | 0.003 |
| Relief of social pressure to quit | −0.084 | 0.176 | −0.008 | 0.007 |
| SCT-based mediators primarily targeted by Cognitive Behavioral Skills Training | ||||
| Confidence to quit smoking | 0.023 | 1.168*** | 0.012 | 0.023 |
| Self efficacy to resist in social situations | 0.119** | 1.171*** | 0.057* | 0.022 |
| Self-efficacy to resist in stressful situations | 0.119* | 1.124*** | 0.057* | 0.024 |
| Social norms for smoking | 0.007 | 0.016 | 0.000 | 0.001 |
| Total effect of all significant mediators | 55.6% | |||
Standardized regression coefficient for intervention effect on mediator.
Standardized coefficient for association between mediator and cessation outcome controlling for HS intervention.
Product of standardized α and β coefficients.
Standard error of the mediation effect.
p < .05.
p < .01.
p < .001.
p < .0001.
p = .06.
SCT mediation of HS intervention for all baseline daily smokers
As shown in Table 3, the intervention had a significant effect on increasing one process targeted by CBST: (1) self-efficacy to resist smoking in stressful situations (α̂ = 0.200, p < .01). The following mediators were significantly associated with higher levels of smoking cessation: (1) importance of quitting smoking (β̂ = 1.279, p < .0001), (2) commitment to quitting smoking (β̂ = 1.472, p < .0001), (3) two smoking motives subscales (identity as a smoker, β̂ = −0.811, p < .01; feelings/pleasure from smoking, β̂ = −0.580, p < .05), (4) confidence to quit smoking (β̂ = 1.295, p < .0001), (5) self-efficacy to resist smoking in social situations (β̂ = 1.154, p < .0001), and (6) self-efficacy to resist smoking in stressful situations (β̂ = 1.560, p < .0001). The CBST-targeted process of self-efficacy to resist smoking in stressful situations mediated 56.9% ( , SE = 0.044, p < .01) of the intervention’s effect on smoking cessation.
Table 3.
Among daily smokers at baseline, effect of HS Intervention on SCT-based mediators, association between mediators and smoking cessation, and mediation effects of the HS intervention (N=695)
| SCT-based mediators | Mediation path | Mediation effect ( c) | ||
|---|---|---|---|---|
| α̂a | β̂b | Estimate | Standard errord | |
| SCT-based mediators primarily targeted by Motivational Interviewing | ||||
| Importance of quitting smoking | 0.013 | 1.279*** | 0.007 | 0.051 |
| Commitment to quitting smoking | 0.098 | 1.472*** | 0.063 | 0.060 |
| Smoking motives | ||||
| Identity as a smoker | 0.029 | −0.811** | −0.012 | 0.023 |
| Social acceptability | 0.059 | −0.114 | −0.004 | 0.009 |
| Exercising choice | 0.102 | −0.436 | −0.024 | 0.020 |
| Feelings/pleasures | 0.041 | −0.580* | −0.012 | 0.024 |
| Quitting motives | ||||
| Self-control | −0.035 | 0.130 | 0.002 | 0.009 |
| Health | 0.019 | 0.165 | −0.002 | 0.008 |
| Relief of social pressure to quit | −0.073 | 0.154 | −0.006 | 0.010 |
| SCT-based mediators primarily targeted by Cognitive Behavioral Skills Training | ||||
| Confidence to quit smoking | 0.040 | 1.295*** | 0.023 | 0.046 |
| Self efficacy to resist in social situations | 0.153 | 1.154*** | 0.077 | 0.049 |
| Self-efficacy to resist in stressful situations | 0.200** | 1.560*** | 0.121** | 0.044 |
| Social norms for smoking | 0.026 | 0.143 | 0.002 | 0.007 |
| Total effect of all significant mediators | 56.9% | |||
Standardized regression coefficient for intervention effect on mediator.
Standardized coefficient for association between mediator and cessation outcome controlling for HS intervention.
Product of standardized α and β coefficients.
Standard error of the mediation effect.
p < .05.
p < .01.
p < .0001.
Discussion
This paper aimed to help explain the results of HS intervention through examining mediation by eight SCT processes among all enrolled smokers and among daily smokers. Regarding all enrolled smokers, (1) the intervention significantly increased the CBST-targeted theoretical processes of self-efficacy to resist smoking in social situations and self-efficacy to resist smoking in stressful situations, which along with six other SCT-based processes, were significantly associated with adolescent smoking cessation, and (2) these two SCT-based processes together statistically mediated 55.6% of the intervention’s effect on smoking cessation. Regarding baseline daily smokers, (1) the intervention significantly increased the CBST-targeted theoretical process of self-efficacy to resist smoking in stressful situations, which along with six other SCT-based processes, were significantly associated with adolescent smoking cessation, and (2) this self-efficacy statistically mediated 56.9% of the intervention’s effect on smoking cessation. The magnitudes of the combined statistical mediation effects (55.6% to 56.9%) suggest that the SCT-based process of resistance self-efficacy accounted for substantial fractions of the HS intervention impact on smoking cessation.
While the study has important methodological limitations (see Limitations section below), the results suggest a number of interpretations. On a theoretical level, these main results suggest that smoking resistance self-efficacy is an important SCT-based process underlying the effect of the HS intervention on adolescent smoking cessation. Consistent with this conclusion, two recent adult smoking cessation trials both found that baseline-to-follow-up-endpoint changes in smoking resistance self-efficacy substantially mediated the impact of the interventions on smoking cessation at the follow-up endpoint (Stanton, et al., 2009; Vidrine, Arduino, & Gritz, 2006). Interestingly, self-efficacy to resist smoking in stressful situations was a strong (i.e., 56.9% of effect) and was the only significant mediator of the intervention among the baseline daily smokers. In contrast, self-efficacy to resist smoking in social situations was a significant mediator of the intervention among all enrolled smokers but not among daily smokers. Compared to daily smokers, it may be that the counselors placed more emphasis on helping the occasional smokers learn skills to resist smoking in social situations (e.g., parties) since these are common situations in which these adolescents smoke. In contrast, compared to occasional smokers, it may be that the counselors placed more emphasis on helping the daily smokers learn skills to resist smoking in stressful situations since stress was a more common reason given for smoking by these adolescents who smoke. It is also possible that some subgroups of smokers have an easier time changing specific SCT-based processes than other subgroups of smokers. Future analysis of the clinical content of the intervention can test these possibilities. Clinical content analysis could provide for a more nuanced mediational model: MI clinical content leads to changes in the MI-targeted SCT-based theoretical mediators while CBST clinical content leads to changes in CBST-targeted SCT-based theoretical mediators, which in turn lead to cessation. The fact that some participants did not receive CBST would be a limitation of such an analysis.
The current study provides a key methodological advance over McCuller et al. (2006)—the only prior study of mediation of an adolescent smoking cessation intervention. They found that 26% of Project EX’s effect on 30-day adolescent smoking abstinence was accounted for by increases in motivation to quit smoking. The current study’s results complement these findings by suggesting that 56% to 57% of the HS Study’s effect on 6-month adolescent prolonged abstinence was accounted for by increases in self-efficacy to resist smoking.
Intervention implications
The results suggest that interventions to increase resistance self-efficacy might increase the chances of successful adolescent smoking cessation outcomes. During intervention implementation, it might be important to closely monitor (1) the intervention to ensure that it focuses on resistance self-efficacy, and (2) the participants for the impact of the intervention on this theoretical process. Such monitoring could provide ongoing feedback on what components need adjusting during intervention implementation. Future research could test methods for how to achieve these goals.
Limitations that can be addressed in future research
Most importantly, while there were no group differences in the mediators at baseline, the simultaneous assessment of the mediators and cessation outcome is a serious limitation of this study. Increases in resistance self-efficacy (and the other significant SCT-based processes) may be a cause of the HS intervention or merely a consequence of smoking cessation. And the strong associations between resistance self-efficacy (and other key SCT-based processes) and smoking cessation may mean that smoking cessation increases resistance self-efficacy rather than vice-versa. A more rigorous design would have measured the mediators and smoking cessation outcomes at frequent intervals (e.g., during and at end of intervention) in order to provide a stronger inference that the changes in these mediators predicted smoking cessation (Murphy et al., 2009). Second, the SCT-based processes were measured with only one to a few items per process, thereby contributing to their unknown (due to one item) or low reliability. (To survey this large number of adolescents with high retention such brevity was essential.) Their unknown or low reliability may also explain why some of these measures were not predictive of smoking cessation. The fact that certain measures mediated adolescent smoking cessation with unknown or low reliability emphasizes the strength of these findings, which may have been even stronger using measures with higher reliability. Third, although the self-reported abstinence outcome was conservatively defined, biochemical verification of adolescent smoking cessation would have been ideal. Finally, despite efforts to increase the study’s racial/ethnic minority enrollment, the trial’s racial/ethnic minority population size, although reflective of the community populations in the 50 participating schools, was underpowered to allow for minority-specific investigations.
Conclusions
Compared to the only prior study on this topic (McCuller et al., 2006), this study provides key advances toward understanding why adolescent smoking cessation interventions are effective. Self-efficacy to resist smoking may be an important mediator of the HS intervention’s effect on smoking cessation—although this conclusion should be considered within the context of this study’s limitations. Targeting theory-based mediators, especially self-efficacy to resist smoking, may be important for effecting adolescent quit rates.
Acknowledgments
The authors thank David P. MacKinnon for his sage advice on the meditational analyses. The data for this paper were provided by the Hutchinson Study of High School Smoking, a project funded by National Cancer Institute grant CA-8259. The data were collected with the approval of the Fred Hutchinson Cancer Research Center’s Institutional Review Board and with informed consent of the respondents. We thank the participants in the study who provided their survey data. Portions of this paper were presented at the Society for Behavioral Medicine Annual Meeting & Scientific Sessions, Seattle, Washington, April 2010.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/adb
Contributor Information
Jonathan B. Bricker, Fred Hutchinson Cancer Research Center & Department of Psychology, University of Washington, Seattle, Washington
Jingmin Liu, Fred Hutchinson Cancer Research Center, Seattle, Washington.
Bryan A. Comstock, Center for Biomedical Statistics, University of Washington
Arthur V. Peterson, Fred Hutchinson Cancer Research Center and Department of Biostatistics, University of Washington
Kathleen A. Kealey, Fred Hutchinson Cancer Research Center
Patrick M. Marek, Fred Hutchinson Cancer Research Center
References
- Baer JS, Kivlahan DR, Donovan DM. Integrating skills training and motivational therapies. Implications for the treatment of substance dependence. Journal of Substance Abuse Treatment. 1999;17(1–2):15–23. doi: 10.1016/s0740-5472(98)00072-5. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Branstetter SA, Horn K, Dino G, Zhang J. Beyond quitting: predictors of teen smoking cessation, reduction and acceleration following a school-based intervention. Drug and Alcohol Dependence. 2009;99(1–3):160–168. doi: 10.1016/j.drugalcdep.2008.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Youth risk behavior surveillance-United States, 2007. MMWR Morbidity &Mortality Weekly Report. 2008;57(SS-4):11–14. 37–38, 61–66. [PubMed] [Google Scholar]
- Chassin L, Presson CC, Pitts SC, Sherman SJ. The natural history of cigarette smoking from adolescence to adulthood in a midwestern community sample: multiple trajectories and their psychosocial correlates. Health Psychology. 2000;19(3):223–231. [PubMed] [Google Scholar]
- Dalton MA, Sargent JD, Beach ML, Bernhardt AM, Stevens M. Positive and negative outcome expectations of smoking: implications for prevention. Preventive Medicine. 1999;29(6 Pt 1):460–465. doi: 10.1006/pmed.1999.0582. [DOI] [PubMed] [Google Scholar]
- Engels RC, Knibbe RA, de Vries H, Drop MJ. Antecedents of smoking cessation among adolescents: who is motivated to change? Preventive Medicine. 1998;27(3):348–357. doi: 10.1006/pmed.1998.0304. [DOI] [PubMed] [Google Scholar]
- Fagan P, Eisenberg M, Stoddard AM, Frazier L, Sorensen G. Social influences, social norms, social support, and smoking behavior among adolescent workers. American Journal of Health Promotion. 2001;15(6):414–421. doi: 10.4278/0890-1171-15.6.414. [DOI] [PubMed] [Google Scholar]
- Gail MH. Eligibility exclusions, losses to follow-up, removal of randomized patients, and uncounted events in cancer clinical trials. Cancer Treatment Report. 1985;69(10):1107–1113. [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Rickert W, Robinson J. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. British Journal of Addiction. 1989;84(7):791–799. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- Henningfield JE, Clayton R, Pollin W. Involvement of tobacco in alcoholism and illicit drug use. British Journal of Addiction. 1990;85(2):279–291. doi: 10.1111/j.1360-0443.1990.tb03084.x. [DOI] [PubMed] [Google Scholar]
- Hollis JF, Polen MR, Whitlock EP, Lichtenstein E, Mullooly JP, Velicer WF, et al. Teen reach: outcomes from a randomized, controlled trial of a tobacco reduction program for teens seen in primary medical care. Pediatrics. 2005;115(4):981–989. doi: 10.1542/peds.2004-0981. [DOI] [PubMed] [Google Scholar]
- Holmen TL, Barrett-Connor E, Holmen J, Bjermer L. Adolescent occasional smokers, a target group for smoking cessation? the Nord-Trondelag Health Study, Norway, 1995–1997. Preventive Medicine. 2000;31(6):682–690. doi: 10.1006/pmed.2000.0750. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: issues and recommendations. Nicotine & Tobacco Research. 2003;5(1):13–25. [PubMed] [Google Scholar]
- Kealey KA, Ludman EJ, Mann SL, Marek PM, Phares MM, Riggs KR, et al. Overcoming barriers to recruitment and retention in adolescent smoking cessation. Nicotine & Tobacco Research. 2007;9(2):257–270. doi: 10.1080/14622200601080315. [DOI] [PubMed] [Google Scholar]
- Kealey KA, Ludman EJ, Marek PM, Mann SL, Bricker JB, Peterson AV. Design and implementation of an effective telephone counseling intervention for adolescent smoking cessation. Journal of the National Cancer Institute. 2009;101(20):1393–1405. doi: 10.1093/jnci/djp318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Wilson GT, Fairburn CG, Agras WS. Mediators and moderators of treatment effects in randomized clinical trials. Archives of General Psychiatry. 2002;59(10):877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- Leischow SJ, Matthews E. Helping adolescent smokers quit: can telephone quitlines lead the way? Journal of the National Cancer Institute. 2009;101(20):1367–1368. doi: 10.1093/jnci/djp333. [DOI] [PubMed] [Google Scholar]
- Lin TH. Missing data imputation in quality-of-life assessment: imputation for WHOQOL-BREF. Pharmacoeconomics. 2006;24(9):917–925. doi: 10.2165/00019053-200624090-00008. [DOI] [PubMed] [Google Scholar]
- Liu J, Peterson AV, Jr, Kealey KA, Mann SL, Bricker JB, Marek PM. Addressing challenges in adolescent smoking cessation: design and baseline characteristics of the HS Group-Randomized trial. Preventive Medicine. 2007;45(2–3):215–225. doi: 10.1016/j.ypmed.2007.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP. Contrasts in multiple mediator models. In: Rose JS, Chassin L, Presson CC, Sherman SJ, editors. Multivariate applications in substance use research: New methods for new questions. Mahwah, NJ: Erlbaum; 2000. pp. 141–160. [Google Scholar]
- MacKinnon DP. Introduction to Statistical Mediation Analysis. Mahwah, NJ: Erlbaum; 2008. [Google Scholar]
- MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Evaluation Review. 1993;17:144–158. [Google Scholar]
- Mackinnon DP, Fairchild AJ. Current Directions in Mediation Analysis. Current Directions of Psychological Science. 2009;18(1):16–20. doi: 10.1111/j.1467-8721.2009.01598.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Fairchild AJ, Fritz MS. Mediation analysis. Annual Review of Psychology. 2007;58:593–614. doi: 10.1146/annurev.psych.58.110405.085542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychological Methods. 2002;7(1):83–104. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackinnon DP, Warsi G, Dwyer JH. A Simulation Study of Mediated Effect Measures. Multivariate Behavioral Research. 1995;30(1):41. doi: 10.1207/s15327906mbr3001_3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Gordon JR. Relapse Prevention: Maintenance Strategies in the Treatment of Addictive Behaviors. New York: The Guilford Press; 1985. [Google Scholar]
- McCuller WJ, Sussman S, Wapner M, Dent C, Weiss DJ. Motivation to quit as a mediator of tobacco cessation among at-risk youth. Addictive Behaviors. 2006;31(5):880–888. doi: 10.1016/j.addbeh.2005.07.019. [DOI] [PubMed] [Google Scholar]
- Mermelstein R, Colby SM, Patten C, Prokhorov A, Brown R, Myers M, et al. Methodological issues in measuring treatment outcome in adolescent smoking cessation studies. Nicotine & Tobacco Research. 2002;4(4):395–403. doi: 10.1080/1462220021000018470. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People To Change Addictive Behavior. New York: The Guilford Press; 1991. [Google Scholar]
- Miller WR, Rollnick S. Motivational Interviewing: Preparing People for Change. 2. New York: The Guilford Press; 2002. [Google Scholar]
- Murphy R, Cooper Z, Hollon SD, Fairburn CG. How do psychological treatments work? Investigating mediators of change. Behavioral Research & Therapy. 2009;47(1):1–5. doi: 10.1016/j.brat.2008.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers MG, McCarthy DM, MacPherson L, Brown SA. Constructing a short form of the Smoking Consequences Questionnaire with adolescents and young adults. Psychological Assessment. 2003;15(2):163–172. doi: 10.1037/1040-3590.15.2.163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pbert L, Flint AJ, Fletcher KE, Young MH, Druker S, DiFranza JR. Effect of a pediatric practice-based smoking prevention and cessation intervention for adolescents: a randomized, controlled trial. Pediatrics. 2008;121(4):e738–747. doi: 10.1542/peds.2007-1029. 710.1542/peds.2007-1029. [DOI] [PubMed] [Google Scholar]
- Peterson AV, Jr, Kealey KA, Mann SL, Marek PM, Ludman EJ, Liu J, et al. Group-randomized trial of a proactive, personalized telephone counseling intervention for adolescent smoking cessation. Journal of the National Cancer Institute. 2009;101(20):1378–1392. doi: 10.1093/jnci/djp317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DB. Multiple imputation for nonresponse in surveys. New York: John Wiley & Sons; 1987. [Google Scholar]
- Schafer JL. Analysis of incomplete multivariate data. New York: Chapman and Hall; 1997. [Google Scholar]
- Sobel . Asymptotic confidence intervals for indirect effects in structural equation models. In: Leinhardt S, editor. Sociological Methodology. Washington, DC: American Sociological Association; 1982. pp. 290–293. [Google Scholar]
- Sobel . Some new results on indirect effects and their standard errors in covariance structure models. In: Tuma N, editor. Sociological Methodology. Washington, DC: American Sociological Association; 1986. pp. 159–186. [Google Scholar]
- Solomon LJ, Bunn JY, Pirie PL, Worden JK, Flynn BS. Self-efficacy and outcome expectations for quitting among adolescent smokers. Addictive Behaviors. 2006;31(7):1122–1132. doi: 10.1016/j.addbeh.2005.08.001. [DOI] [PubMed] [Google Scholar]
- Sussman S, Sun P, Dent CW. A meta-analysis of teen cigarette smoking cessation. Health Psychology. 2006;25(5):549–557. doi: 10.1037/0278-6133.25.5.549. [DOI] [PubMed] [Google Scholar]
- Stanton CA, Lloyd-Richardson EE, Papandonatos GD, de Dios MA, Niaura R. Mediators of the relationship between nicotine replacement therapy and smoking abstinence among people living with HIV/AIDS. AIDS Education &Prevention. 2009;21(3 Suppl):65–80. doi: 10.1521/aeap.2009.21.3_supp.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. With Understanding and Improving Health and Objectives for Improving Health. 2. 2B. Washington, DC: U.S. Government Printing Office; 2000. Healthy People, 2010; pp. 3–40. [Google Scholar]
- Vidrine DJ, Arduino RC, Gritz ER. Impact of a cell phone intervention on mediating mechanisms of smoking cessation in individuals living with HIV/AIDS. Nicotine & Tobacco Research. 2006;8(Suppl 1):S103–108. doi: 10.1080/14622200601039451. [DOI] [PubMed] [Google Scholar]
- Woodruff SI, Conway TL, Edwards CC. Sociodemographic and smoking-related psychosocial predictors of smoking behavior change among high school smokers. Addictive Behaviors. 2008;33(2):354–358. doi: 10.1016/j.addbeh.2007.09.012. [DOI] [PubMed] [Google Scholar]
- Zhang B, Walker CM. Impact of missing data on person-model fit and person trait estimation. Applied Psychological Measurement. 2008;32:466–479. [Google Scholar]