Abstract
Aims
To determine, in the context of a trial in which counseling did not improve smoking cessation outcomes, whether this was due to a failure of the conceptual theory identifying treatment targets or the action theory specifying interventions.
Design
Data from a randomized clinical trial of smoking cessation counseling and bupropion SR were submitted to multilevel modeling to test whether counseling influenced real-time reports of cognitions, emotions, and behaviors, and whether these targets predicted abstinence.
Setting
Center for Tobacco Research and Intervention, Madison, WI.
Participants
403 adult, daily smokers without contraindications to bupropion SR use.
Intervention
Participants were randomly assigned to receive individual counseling or no counseling and a 9-week course of bupropion SR or placebo pill. Cessation counseling was delivered in eight 10-minute sessions focused on bolstering social support, motivation, problem-solving, and coping skills.
Measurements
Pre- and post-quit ecological momentary assessments of smoking behavior, smoking triggers, active prevention and coping strategies, motivation to quit, difficulty quitting, and reactions to initial lapses.
Findings
Counseling prompted avoidance of access to cigarettes, improved quitting self-efficacy, reduced perceived difficulty of quitting over time, and protected against guilt and demoralization following lapses. Results also supported the importance of limiting cigarette access, receiving social support, strong motivation and confidence, and easing withdrawal distress during cessation efforts. Quitting self-efficacy and perceived difficulty quitting may partially mediate counseling effects on abstinence.
Conclusions
Smoking cessation counseling may work by supporting confidence about quitting and reducing perceived difficulty quitting. Counseling did not affect other targets that protect against relapse.
Keywords: smoking cessation, tobacco dependence, brief counseling, mediation, randomized clinical trial, mechanisms of change
Introduction
Meta-analyses [1–4] suggest that smoking cessation counseling, offered in a variety of formats (e.g., individual, group, telephone), roughly doubles the odds of quitting successfully (odds ratios range from 1.3 to 3.2). Even relatively brief (e.g., 60 minutes) counseling can improve abstinence rates [1,5] and the cost-effectiveness of intensive group treatment for smoking cessation may compare favorably to prescription medication [6]. Negative findings have been reported, however, particularly for less intensive counseling [e.g., 7–10]. Effects also tend to be weaker for counseling offered with active medication rather than as a stand-alone treatment [1]. The magnitude of counseling effects appears to have dwindled over time [11], for reasons that are not yet clear [12–14]. The mixed evidence regarding counseling potency suggests that continued evaluation of counseling efficacy is important.
Formal tests of mediation have been rare in tobacco treatment research [15–18]. Mediation models simultaneously test conceptual theories about smoking relapse determinants and action theories about the effects of tobacco cessation treatments [19]. Mediation analyses examine relations among an initial variable (e.g., treatment), a putative mediator (e.g., coping), and an outcome (e.g., abstinence [19]). Statistically significant mediation requires (at minimum) that the treatment influences the mediator, and that the mediator and the outcome are related [19–21]. An important function of mediation analyses is to provide a post-mortem for treatments that do not work as intended. Such analyses may indicate whether null effects occur because the hypothesized mediator does not affect the outcome or because the treatment does not affect the mediator. Thus, post-mortem mediation analyses can reveal why treatments do not work.
The current study adopted a mediational framework to examine the effects of Public Health Service Guideline-based counseling [1] on intervening variables thought to predict abstinence and to examine the relations between putative mediators and cessation outcomes. Based upon meta-analyses and reviews citing key counseling ingredients [1, 2, 22–23] and previous cessation studies [24–33], we identified the following as potential mechanisms of counseling effects: 1) avoidance of common smoking triggers (e.g., places where smoking is permitted, cigarettes are easily accessible, or others are smoking); 2) increased anticipatory (pre-urge), immediate (mid-urge or mid-stress), or restorative (post-lapse) coping [34–35]; 3) increased social support; 4) enhanced motivation to quit and willingness to work at quitting [26–27, 29, 36]; 5) increased confidence [26, 28, 30, 32]; 6) reduced distress related to quitting [22]; and 7) adaptive responses to lapses (i.e., not giving up following a slip [31, 33–34, 37]). Counseling may induce these changes, which, in turn, may improve success in quitting.
Data for the current study came from a randomized controlled clinical trial comprising adult smokers interested in quitting. Participants were randomly assigned to receive eight 10-minute sessions of individual counseling or no additional clinical contact (there was no attentional control for nonspecific counseling effects). Meta-analyses suggest that even very brief counseling (i.e., 10 minutes total) can improve abstinence [1]. Participants were also randomly assigned to receive either active or placebo sustained-release bupropion (bupropion SR, GlaxoSmithKline, Inc., Research Triangle, NC). Results are collapsed across medication conditions, as counseling and medication condition did not interact for any mediator or abstinence outcome and bupropion SR results are reported elsewhere [17, 38].
Counseling did not significantly increase abstinence rates at any time point [38]. Thus, this trial presented an opportunity to explore why counseling did not improve cessation: i.e., we tested multilevel models of relations between counseling and candidate mediators (i.e., the “action model”), and logistic regression models of candidate mediator relations with 7-day point prevalence abstinence 56-days post-quit (i.e., the “conceptual model”) [39]. Mediators were assessed daily using ecological momentary assessment (EMA) [40–41].
Methods
Participants
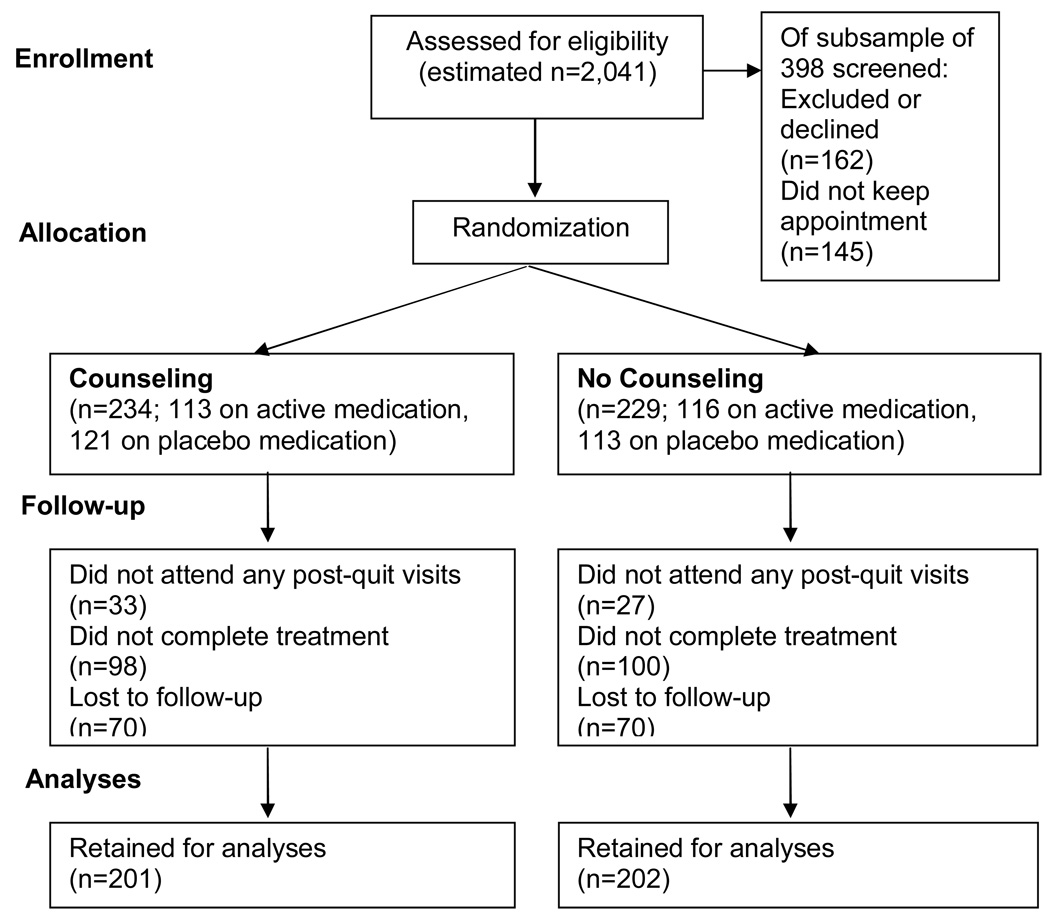
This sample is the same as that reported in [17] and [38]. Adult participants were recruited via mass media in the Madison, WI area from January 2001 to March 2003. Inclusion/exclusion criteria are shown in Table 1. Sixty (13.0%) of the 463 individuals enrolled withdrew before the quit date, leaving 403 for the current study requiring post-quit data (See Figure 1, also [38]). Demographic and baseline characteristics for the sample of 403 are summarized in Table 2. No significant differences in conditions were noted, except that those in the counseling condition were younger than control subjects (mean difference =2.824 years, 95% CI=.485–5.163, t=2.373, p=.018. Cohen’s d=.236). Age was entered as a covariate in analyses.
Table 1.
Inclusion/exclusion criteria.
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| 18 years of age or greater | Current heavy drinking |
| Able to read and write English | Current illegal drug use |
| At least fairly motivated to quit smoking | Use of other tobacco products in last 7 days |
| Willing to fulfill study requirements | Current use of stop-smoking treatments |
| Smoking at least 10 cigarettes per day | Participation in a study in the past 30 days |
| Baseline CO level of at least 10 parts per million | Living with someone enrolled in the study |
| Current depression (CES-D score over 16)* History of bipolar disorder or psychosis Uncontrolled hypertension History of seizure Past negative reactions to bupropion Pregnancy Breast feeding |
Except when an interview with a licensed clinical psychologist suggested another cause for elevated scores.
Figure 1.
Enrollment and retention flow diagram, collapsed over medication conditions. Note that the number retained for analyses is the total pool of participants who completed the quit day visit and provided at least some post-quit data. The number of subjects included in specific multilevel models was sometimes smaller than this total sample size due to missing mediator data. Abstinence outcomes were not missing for any subject, as intent-to-treat analyses were conducted.
Table 2.
Characteristics of the sample included in mediation analyses (N=403).
| Variable | Value | No Counseling (n=202) n (%) |
Counseling (n=201) n (%) |
|---|---|---|---|
| Sex (N=403) | Female | 104 (51.5%) | 98 (48.8%) |
| Ethnicity (N=400) | Hispanic | 3 (1.5%) | 1 (0.5%) |
| Race | White | 181 (89.6%) | 176 (87.6%) |
| (N=400) | African-American | 12 (5.9%) | 13 (6.5%) |
| Other | 8 (4.0%) | 10 (5.0%) | |
| Marital Status | Married | 88 (43.6%) | 87 (43.3%) |
| (N=401) | Separated or Divorced | 50 (24.8%) | 32 (15.9%) |
| Never Married | 42 (20.8%) | 59 (29.4%) | |
| Cohabitating | 16 (7.9%) | 20 (10.0%) | |
| Widowed | 5 (2.5%) | 2 (1.0%) | |
| Education | Less than high school degree | 7 (3.5%) | 7 (3.5%) |
| (N=401) | High school | 48 (23.8%) | 38 (18.9%) |
| Some college | 94 (46.5%) | 101 (50.2%) | |
| College degree or greater | 53 (26.2%) | 53 (26.4%) | |
| Employment | Employed | 165 (81.7%) | 167 (83.1%) |
| Status | Unemployed | 10 (5.0%) | 9 (4.5%) |
| (N=397) | Homemaker | 7 (3.5%) | 10 (5.0%) |
| Student | 6 (4.0%) | 4 (2.0%) | |
| Retired | 6 (3.0%) | 6 (3.0%) | |
| Disabled | 3 (1.5%) | 4 (2.0%) | |
| Household Income (N=393) | < $25,000 | 55 (27.2%) | 60 (29.9%) |
| $25,00-$34,999 | 29 (14.4%) | 32 (15.9%) | |
| $35,000-$49,999 | 43 (21.3%) | 35 (17.4%) | |
| >$50,000 | 68 (33.7%) | 71 (35.3%) | |
| Time to First Cigarette | Within 5 minutes | 46 (22.8%) | 49 (24.4%) |
| (N=403) | 6–30 minutes | 103 (51.0%) | 80 (39.8%) |
| 31–60 minutes | 32 (15.8%) | 38 (18.9%) | |
| After 60 minutes | 21 (10.4%) | 34 (16.9%) | |
| Past Counseling (N=371) | Yes | 59 (29.2%) | 61 (30.3%) |
| M (SD) | M (SD) | ||
| Age (N=403) | 40.38 (11.73) | 37.56 (12.16) | |
| Cigarettes smoked per day (N=403) | 21.73 (8.93) | 21.59 (11.67) | |
| Baseline CO level (N=402) | 24.82 (11.41) | 23.85 (11.73) | |
| Baseline FTND Score (N=399) | 5.12 (2.14) | 4.92 (2.50) | |
Procedures
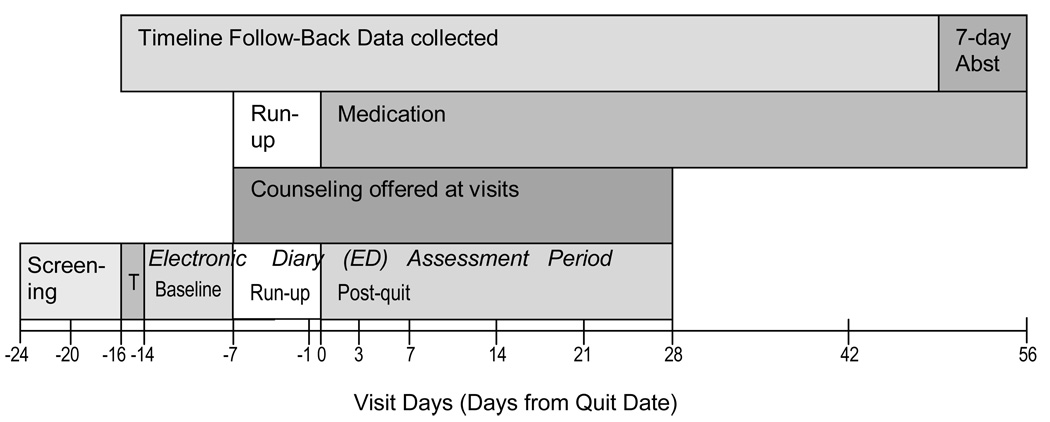
Study procedures are described in detail elsewhere [38]. Interested volunteers completed screening including a telephone interview, group orientation, and physical exam prior to randomization using a computer-generated list prepared by staff with no participant contact. Written informed consent was obtained from all subjects. Medication condition was double blinded, but counseling condition was not blinded. Participants attended a total of 13 office visits and carried an Electronic Diary for six weeks (Figure 2). Maximum remuneration for participation was $200. All study procedures were approved by the Institutional Review Board at the University of Wisconsin School of Medicine and Public Health.
Figure 2.
Study timeline. Target days of visits (relative to the day 0, the target quit day), are shown at bottom on the timeline. Intervals between visits varied slightly across subjects. Screening visits included a group orientation and an individual visit including a physical exam. Electronic Diary (ED) training was conducted at the next visit and the 2-day ED training period (noted as T) followed. The ED assessment period was parsed into a 1-week pre-treatment baseline period, a 1-week treatment run-up period, and a 4-week post-quit mediator assessment period, as shown in the lowest level of the figure. Counseling sessions began 1-week pre-treatment and were offered at this and the following 7 visits. Medication treatment began 1-week pre-quit (at 150 mg) per day, increased to 300 mg per day on day −4, and continued until day 56. The abstinence outcome used in analyses (noted as 7-day Abst in the figure) was intent-to-treat complete abstinence (not even a puff) in the week preceding the final visit confirmed by CO (collected at all visits) and not disconfirmed by serum cotinine testing.
Treatment
Counseling
Counseling consisted of eight individual 10-minute sessions. The number of sessions and total contact time were selected based on meta-analyses of previous counseling trials that suggested that 31–90 minutes of counseling improve abstinence rates by a factor of 3.2 and that 4–8 sessions of counseling improve abstinence rates by a factor of 1.9, relative to no counseling [1]. Additional minutes of contact time (up to 300 minutes) and additional sessions (beyond eight) do not significantly increase abstinence rates [1].
Counseling focused on sustaining motivation to quit, problem solving related to quitting, coping with stress and urges to smoke, and fostering intra-treatment social support. Psychoeducation was provided (e.g., regarding tobacco dependence, withdrawal, and relapse). Counselors were undergraduate, bachelor’s level, or master’s level staff who achieved protocol mastery prior to working with participants and received ongoing weekly group supervision from a licensed clinical psychologist with extensive experience providing smoking cessation counseling. Treatment was manualized and a specific outline was provided for each counseling session (see supplementary material online). Fidelity to the treatment protocol was assessed by weekly session audiotape review and facilitated by weekly group supervision. Participants who did not receive counseling received general support and encouragement and completed the same study visits and assessments as did those in counseling, but had slightly shorter sessions.
Bupropion SR
Participants began taking 150-mg of bupropion SR or placebo in the morning one week before the quit day and increased to two 150-mg pills per day four days pre-quit. Participants were instructed to continue taking 300-mg per day for eight weeks post-quit.
Measures
At early office visits, participants provided demographic and smoking history information (see Table 2); completed the Fagerström Test of Nicotine Dependence (FTND [42]) and the Center for Epidemiologic Studies Depression Scale (CES-D [43]); and provided breath samples for carbon monoxide (CO) testing.
Daily smoking status (smoking vs. abstinent) was assessed through 52 weeks post-quit using EMA reporting of smoking behavior (up to day 28) or a time-line follow-back method (thereafter). All participants claiming seven-day point-prevalence abstinence at the end of medication treatment (56 days post-quit) were asked to provide a blood sample for cotinine (the major metabolite of nicotine) analysis. Participants were considered abstinent at the end of treatment if they reported no smoking in the last seven days, provided a breath sample containing less than 10 ppm CO at that visit, and had a serum cotinine level (if provided) below 15 ng/ml [44]. Claims of abstinence verified by CO were disconfirmed by cotinine in ten (9%) of 111 subjects. Forty more individuals (36.0%) failed to provide a blood sample for cotinine testing, which required a separate laboratory visit; these subjects were coded as abstinent.
Electronic Diaries (EDs, Palm Vx Palmtop Computer, Palm, Inc., Santa Clara, CA) were programmed by invivodata, Inc. (Pittsburgh, PA) to administer four to seven daily reports at random intervals of at least 30 minutes during the waking day and an evening report at bedtime. Random prompts assessed whether smoking was permitted (No/Yes), cigarettes were readily available (No/Yes), other smokers were present (No/Yes), attempts to prevent urges (No/Yes; post-quit only), temptations to smoke (number since last report), immediate coping with temptations (No/Yes; post-quit only); occurrence of stressful events (No/Yes), immediate coping with stress (No/Yes), receipt of social support (No/Yes), and number of cigarettes smoked.
A nightly report completed at bedtime assessed “motivation to quit/stay quit,” “willingness to work hard at quitting,” “confidence in ability to quit,” “difficulty quitting,” (post-quit only), and how “bothered by withdrawal” (post-quit only) subjects were over the preceding 24 hours on a scale from 0 (Low!!) to 10 (High!!).
Participants were also instructed to complete a brief “slip” report the first several times they smoked post-quit. Slip reports assessed the extent to which participants felt guilty, felt like giving up, and were confident in their ability to quit [45], on a scale ranging from 0 (Low!!) to 10 (High!!). Participants were also asked whether they “made plans to avoid further slips” (No/Yes) and whether they “tried to abstain” (No/Yes) in the hour before the slip.
Attrition
Of the 403 individuals retained through a target quit day, 265 (65.8%) attended all visits. Attrition rates did not differ by treatment condition at the quit date (no counseling: 11.8%; counseling: 14.1%; χ2(df=1, N=463)=.55, p=.46) or at the conclusion of treatment (no counseling: 28.2%; counseling: 29.4%; χ2(df=1, N=403)=.06, p=.80). Counseling conditions did not differ in terms of treatment visits attended (no counseling: M=7.19, Median=8, SD=1.59; counseling: M=7.33, Median=8, SD=1.45; t(401)=−.96, p=.34) or in ED adherence; participants completed random prompts on 75.5% of days prompted (t(401)=.65, p=.52) and 79.5% (t(401)=.50, p=.62) of evening reports prompted, on average.
Data Analysis
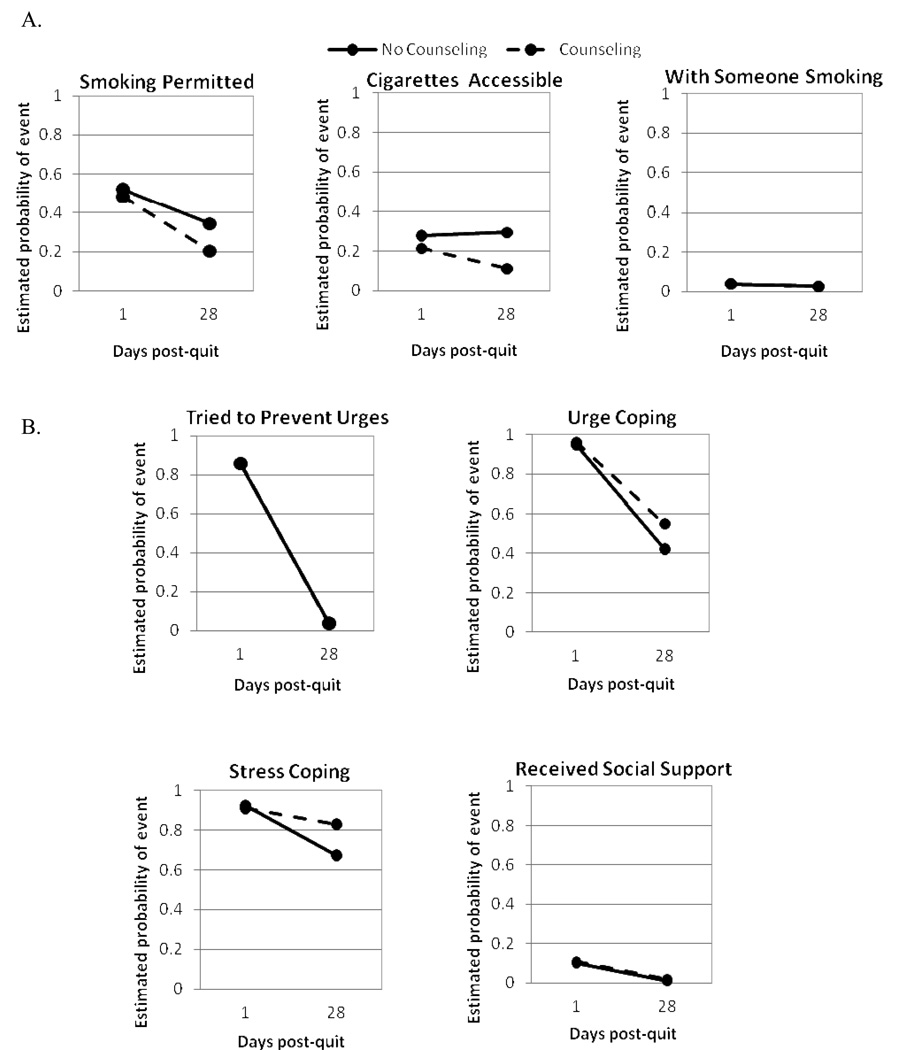
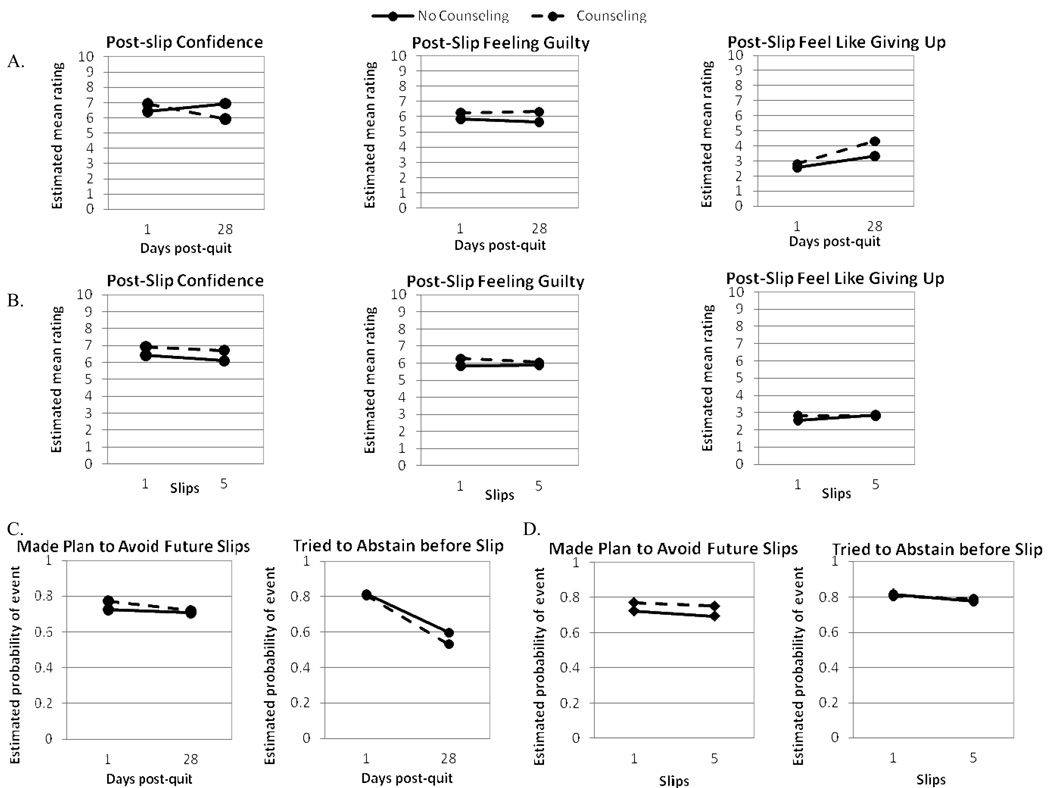
Estimates from multilevel models fit with HLM 6.0.4 software (Lincolnwood, IL: Scientific Software International [46]) are depicted in figures 3–5 (models are described in detail in the online supplementary material and results are shown in supplementary Tables S1–S3). Counseling effects on the average level and the linear slope for each random prompt and evening report mediator were estimated for four weeks post-quit by centering the time-since-quit-day variable around the mid-point (day 14) of the 28-day post-quit assessment period. Models controlled for pre-treatment and pre-quit levels of the mediators [47], recent smoking (within-subjects, coded as a binary variable due to skewness in smoking counts), and cessation failure (i.e., failing to quit on the target quit day, between subjects). Models were run without (see Tables S1–S3), and with, additional between-subject covariates: gender (0=male, 1=female), racial/ethnic status (0=Caucasian, 1=minority), education (0=some college or less education, 1=graduated from college or higher), years of age, baseline CES-D score, and baseline FTND score (the latter three variables were grand-centered). Coefficients were allowed to vary across subjects when variance estimates suggested that subjects significantly varied and when this did not interfere with model convergence. Thus, models generated covariate-adjusted estimates of an individuals’ average level of a mediator post-quit (controlling for pre-quit levels) and an estimate of the linear rate of change in the mediator in the post-quit period. The linear slope in mediators was estimated in order to identify systematic growth or declines in the mediator post-quit (which would change the interpretation of the estimated average level) and to explore whether these changes were related to treatment as hypothesized (e.g., we expected counseling to slow declines in motivation to quit).
Figure 3.
Estimated post-quit probabilities of behaviors reported in random prompts as a function of counseling condition (solid line indicates no counseling, dashed line indicates counseling). Panel A shows the probability of spending time where: smoking was permitted, cigarettes were easily accessible, and someone was smoking. Panel B shows the probabilities of: attempting to prevent urges to smoke, attempting to cope with urges, attempting to cope with stressful events, and receiving social support.
Figure 5.
Estimate means or probabilities of slip report responses as a function of counseling condition (no counseling shown by solid lines, counseling shown by dashed lines). Panels A and B depict mean ratings of confidence related to quitting, feelings of guilt about slipping, and feeling like giving up after a slip as a function of days from the quit day and the number of slips reported, respectively. Panels C and D depict the probability of attempting to abstain prior to a lapse and of making plans to avoid future slips following a lapse as a function of days post-quit and number of slips, respectively.
Results
Descriptive statistics regarding the candidate mediators are shown in Table 3. At the end of treatment, 29.4% of those who received counseling and 25.7% of those who did not receive counseling had confirmed 7-day point-prevalence abstinence. Counseling condition was not a significant predictor of abstinence in a logistic regression analysis (B=.181, SE=.223, Wald=.657, OR=1.199, 95% CI=.774–1.857, Number needed to treat to prevent one additional relapse=27).
Table 3.
Descriptive statistics for putative mediators post-quit, by counseling condition.
| Variable | Value | No Counseling | Counseling |
|---|---|---|---|
|
Random Prompt JUST BEFORE PROMPT |
(n=16,886) n (%) |
(n=17,860) n (%) |
|
| Was smoking permitted? | Yes | 7,401 (43.8%) | 7,444 (41.7%) |
| Were cigarettes available? | Yes, easily | 5,024 (29.8%) | 4,265 (23.9%) |
| Was anyone smoking? | Yes | 1,465 (8.7%) | 1,329 (7.4%) |
| SINCE LAST PROMPT | |||
| Tried to prevent temptations/urges? | Yes | 6,100 (36.1%) | 6,470 (36.2%) |
| How many strong temptations/urges? | >0 | 7,281 (43.1%) | 7,368 (41.3%) |
| Tried to cope with temptations/urges? | Yes | 5,670 (33.6%) | 6,097 (36.2%) |
| Upsetting stressful situation ? | Yes | 1,321 (7.8%) | 1,269 (7.1%) |
| Tried to cope with stress? | Yes | 1,003 (5.9%) | 1,064 (6.0%) |
| Received social support? | Yes | 2,048 (12.1%) | 2,482 (13.9%) |
| Cigarettes smoked? | >0 | 2,295 (13.6%) | 1,744 (9.8%) |
| Evening Report | (n=4,095) | (n=4,278) | |
| SINCE LAST EVENING REPORT ON AVERAGE | Mean (SD) | Mean (SD) | |
| Confidence in ability to quit? | 0–10 | 7.57 (2.51) | 8.06 (2.31) |
| Motivation to quit? | 0–10 | 7.77 (2.43) | 8.22 (2.19) |
| Willing to work hard at quitting? | 0–10 | 7.91 (2.31) | 8.32 (2.10) |
| Difficulty quitting? | 0–10 | 5.72 (3.06) | 5.09 (3.24) |
| Bothered by withdrawal? | 0–10 | 4.93 (3.06) | 4.32 (3.19) |
| Cigarettes smoked? | 0–99 | 2.35 (6.74) | 1.58 (4.78) |
| Slip Report | (n=1,313) | (n=947) | |
| RIGHT NOW | Mean (SD) | Mean (SD) | |
| Confidence in ability to quit? | 0–10 | 5.98 (2.99) | 6.00 (2.84) |
| Feeling guilty? | 0–10 | 6.10 (3.18) | 6.39 (3.16) |
| Feel like giving up? | 0–10 | 3.43 (3.25) | 3.95 (3.37) |
| n (%) | n (%) | ||
| Made plan to avoid future lapses? | Yes | 841 (64.1%) | 649 (68.5%) |
| HOUR BEFORE SMOKED | |||
| Tried to abstain? | Yes | 821 (62.7%) | 632 (66.9%) |
Counseling Effect on Mediators
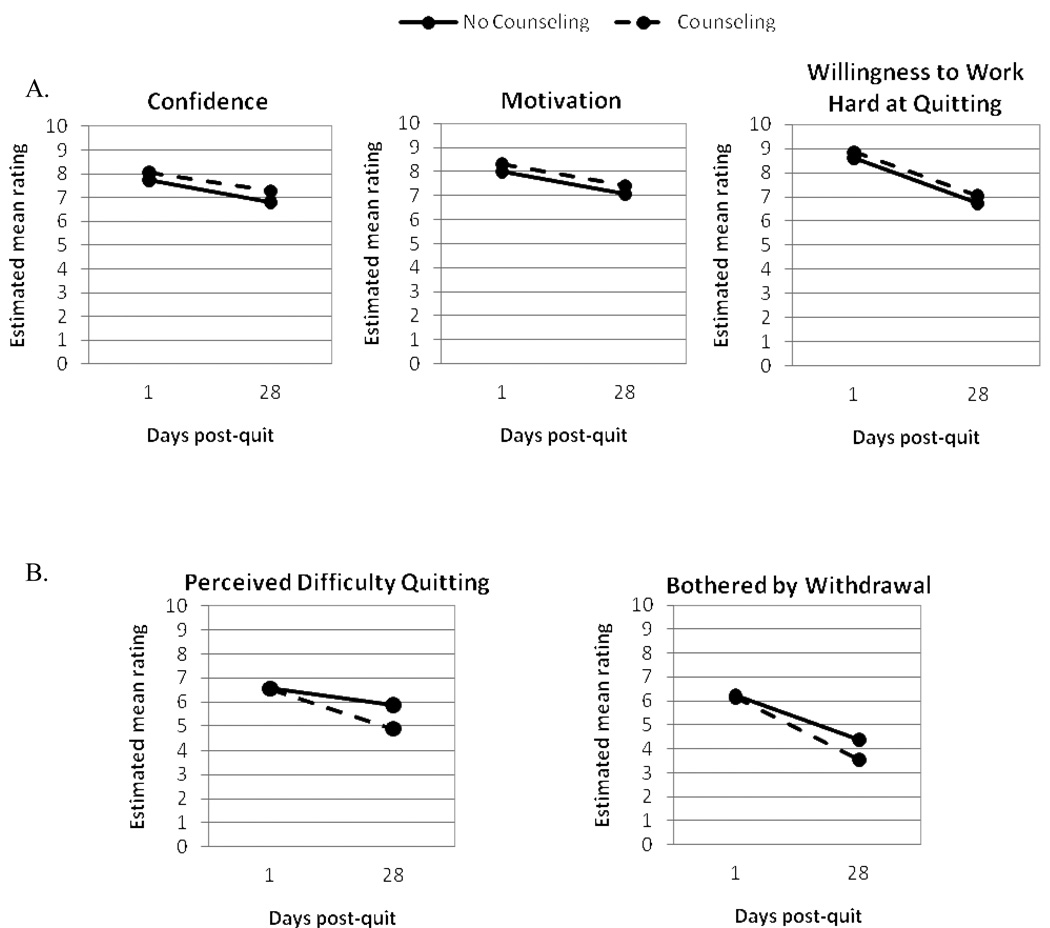
Counseling was associated with some reductions in smoking trigger exposure (Figure 3). Those who received counseling were less likely, on average, to spend time where cigarettes were easily accessible post-quit and reported steeper declines in spending time where cigarettes were accessible or smoking was permitted than did control subjects. Spending time with others who were smoking was rare and did not differ as a function of counseling. Counseling was not associated with greater urge prevention (anticipatory coping), but did increase the probability that subjects would report coping with urges or stress post-quit (only when covariates were included in the model; See Figure 3). In addition, those in the counseling condition reported significantly higher nightly levels of confidence related to quitting, on average, than did control subjects (Figure 4, Panel A). Counseling effects on motivation to quit and willingness to work at quitting were not significant after controlling for baseline covariates and cessation failure. Perceived difficulty quitting declined faster among those who received counseling than those in the control condition (Figure 4, Panel B). Feeling bothered by withdrawal was not significantly affected by counseling. Slip report data, however, indicated that those in the counseling condition showed greater declines in post-slip quitting confidence over time (Figure 5, Panel A). Counseling recipients also showed declines in feelings of guilt and slower increases in feeling like giving up after additional slips (Figure 5, Panel B) than did controls. Reports of proactive attempts to avoid lapses before they happened or to plan to avoid future lapses were not significantly influenced by counseling (Figure 5, Panels C and D).
Figure 4.
Estimated post-quit evening report ratings as a function of counseling condition (solid line indicates no counseling, dashed line indicates counseling). Panel A shows ratings of confidence related to quitting, motivation to quit, and willingness to work hard at quitting. Panel B shows perceived difficulty quitting and being bothered by withdrawal.
Mediator Relations with Abstinence
Empirical Bayes estimates of post-quit individual growth curve coefficients (average levels and linear slopes) derived from HLM models were used as predictors of biochemically verified 7-day point-prevalence abstinence at the end of treatment in logistic regression models (Table 4). Including both the mediator average and slope in models allowed us to determine whether overall levels of the mediator were important in abstinence, or whether change in the mediator was important. Models included counseling condition as a predictor and controlled for cessation failure and baseline covariates (gender, minority status, education, age, dependence, depressive symptoms). Several candidate mediators were significantly related to subsequent abstinence. Specifically, easy access to cigarettes was negatively related to abstinence. Increasing use of urge prevention was also associated with reduced abstinence probability, but this relation became non-significant when individuals’ average probability and slope of temptations to smoke (derived from a separate HLM model of temptation occurrence) were included in the model to rule out the possibility that urge prevention increased because urges more frequently beset subjects. Receiving social support and maintaining a higher average level of confidence, motivation, and willingness to quit were all predictive of abstinence. Higher average levels of and increases in difficulty quitting or being bothered by withdrawal were predictive of relapse. Feeling more like giving up after additional lapses was also significantly predictive of relapse.
Table 4.
Conceptual model results: Logistic regression predicting 7-day point-prevalence abstinence 56 days post-quit from HLM empirical Bayes estimates.
| Post-quit Intercept EB Estimate | Post-quit Day EB Estimate (Slope) | |||||||
|---|---|---|---|---|---|---|---|---|
| Empirical Bayes (EB) Predictor | B (SE) | Wald | OR | 95% CI | B (SE) | Wald | OR | 95% CI |
| Random prompt report | ||||||||
| Where smoking permitted (n=398) | .094 (.121) | .604 | 1.099 | .867–1.392 | -2.548 (2.661) | .917 | .078 | .000–14.412 |
| Cigarettes easily accessible (n=398) | −.232 (.082) | 7.921 | .793* | .675–.932 | −1.584 (1.530) | 1.072 | .205 | .010–4.118 |
| With someone smoking (n=398) | .113 (.218) | .269 | 1.120 | .731–1.715 | - | |||
| Tried to prevent urges (n=385) | −.031 (.064) | .232 | .969 | .854–1.100 | −2.460 (1.081) | 5.183 | .085*† | .010–.710 |
| Tried to cope with urges (n=383) | .027 (.076) | .128 | 1.027 | .886–1.192 | -1.337 (1.782) | .563 | .263 | .008–8.625 |
| Stress coping (n=370) | .178 (.111) | 2.558 | 1.194 | .961–1.484 | -- | |||
| Received Social Support (n=398) | .505 (.237) | 4.562 | 1.658* | 1.043–2.636 | -6.027 (4.141) | 2.118 | .002 | .000–8.086 |
| Evening report | ||||||||
| Confidence in ability to quit (n=400) | .934 (.146) | 40.648 | 2.544* | 1.909–3.389 | - | |||
| Motivation to quit (n=400) | .903 (.155) | 33.937 | 2.466* | 1.820–3.341 | - | |||
| Willingness to work at quitting (n=400) | .831 (.145) | 32.792 | 2.295* | 1.727–3.050 | - | |||
| Difficulty quitting (n=373) | −.177 (.064) | 7.635 | .838* | .740–.950 | −8.251 (1.762) | 21.938 | .000* | .000–.008 |
| Bothered by withdrawal (n=373) | −.155 (.061) | 6.355 | .857* | .759–.966 | −5.307 (1.546) | 11.792 | .005* | .000–.102 |
| Slip report | ||||||||
| Confidence in ability to quit (n=247) | .129 (.104) | 1.533 | 1.137 | .928–1.394 | -- | |||
| Feeling guilty (n=247) | −.104 (.072) | 2.071 | .901 | .782–1.038 | -- | |||
| Feel like giving up (n=247) | −.155 (.107) | 2.107 | .856 | .695–1.056 | −11.717 (4.453) | 6.923 | .000* | .000–.050 |
| Made plan to avoid future slips (n=245) | −.017 (.162) | .011 | .983 | .716–1.351 | -- | |||
| Tried to abstain before slip (n=242) | −.079 (.161) | .239 | .924 | .674–1.267 | -- | |||
p<.05;
- Predictor dropped from model due to very large SE and confidence intervals (e.g., .312-6386.599 for the post-quit slope in being with a smoker);
-- Not estimated because coefficient fixed to facilitate convergence or due to lack of variability in HLM model;
Effect reduced to non-significance when empirical Bayes estimates of average probability and slope of strong temptations to smoke were entered in the model
Mediation Summary
In this study, the only candidate mediators that were significantly influenced by treatment and significantly related to later abstinence were: easy access to cigarettes, quitting confidence, and the post-quit slope in perceived difficulty quitting. To assess whether statistically significant mediation of counseling effects by these variables occurred, the ProdClin program (Tempe, AZ [48]) was used to estimate the asymmetric confidence intervals for the mediated effects. Cigarette access was not a significant mediator, as the confidence interval for the estimated mediated effect (ab) of.007 (SE=.005) comprised zero (95% CI=.000–.018). The estimated mediated effect for confidence was significant, in contrast (ab=.357, SE=.169, 95% CI=.046–.711). The mediated effect for the rate of decline in self-reported difficulty quitting was also significant at .305 (SE=.126, 95% CI=.088–.578).
Discussion
The current study examined whether brief smoking cessation counseling affected the behavioral, cognitive, and affective targets it was designed to alter and whether these targets were related to abstinence as expected. This analytic strategy may enhance our understanding of why treatments fail to promote desired change by simultaneously testing both action theories about treatment and conceptual theories about abstinence determinants. In this way, examining relations among treatment, treatment targets, and outcomes may help explain treatment failures and suggest avenues for treatment refinement.
Treatment Models
The current study provided mixed support for the counseling action model. Subjects in counseling spent less time where smoking was permitted and where cigarettes were available than did controls, which suggests that counseling may be effective in helping smokers reduce exposure to some smoking triggers. Counseling was not associated with a decrease in exposure to others smoking, but floor effects may have made it difficult to detect counseling effects on this relatively rare form of exposure. Counseling had mixed benefits in terms of coping; counseling did not increase urge prevention, but did promote active stress and urge coping (after controlling for covariates). Counseling did not significantly boost perceived social support.
Counseling had some notable effects on cognitive constructs as well. Counseling appeared to elevate quitting self-efficacy and helped subjects perceive quitting as less difficult over time. Counseling did not significantly boost or maintain motivation or willingness to work at quitting, which tended to decline over the post-quit period in both the counseling and control conditions. Counseling had only marginal effects on withdrawal distress, but reduced the toll of multiple slips on feelings of guilt and demoralization, as intended. Unexpectedly, those receiving counseling who lapsed also reported a steeper decline in post-slip confidence over the first 28 days of the quit attempt than did those in the control condition. This effect may reflect a response to psychoeducation in the counseling sessions regarding the importance of limiting lapses and the danger of relapsing following any smoking. The importance of maintaining complete abstinence (i.e., “not even a puff”) was emphasized and this may have prompted those who received counseling to be more shaken by a slip than those in the control group. Behaviors and cognitions related to sustained commitment to quitting (attempting to abstain and planning to avoid future slips) were not significantly improved by counseling.
These results show that PHS Guideline based counseling affects some targets more than others. For example, smokers may be more likely to apply counseling recommendations that they get rid of cigarettes and avoid places where smoking is permitted than they are to develop or adopt new cognitive or behavioral plans to prevent urges or lapses. The treatment offered in this study was consistent with treatment guidelines, yet still failed to increase abstinence rates, perhaps in part because it failed to improve some of the behaviors (e.g., eliciting social support) and beliefs (e.g., willingness to work at quitting) that were most strongly predictive of abstinence. The current study had adequate power (.79) to detect a difference in abstinence rates as small as 6% (at alpha .05), a small effect size (Number needed to treat=17, Cohen’s d=.1–.2). Thus, large or medium effects would have been detected, and only small effects would have escaped detection.
Abstinence Predictors
The current study adds to literature on actions and beliefs that facilitate abstinence. This is the first study to assess the benefits of avoiding triggers (e.g., cigarette access), perceived social support, and maintaining confidence and willingness to work hard at quitting in an ongoing way through the quit process. Previous research has suggested such benefits [28, 32, 49–52], but not documented them in real-time. Urge prevention appeared to be associated with reduced likelihood of abstinence, but this relation was not significant when temptation frequency was controlled in logistic regression models. Those most likely to use urge prevention strategies may be those most beset by strong temptations to smoke. Perceived difficulty quitting and withdrawal distress were associated with decreased abstinence likelihood, in support of negative reinforcement models of drug motivation [23]. These relations persisted even with the inclusion of time-varying smoking and cessation failure covariates, and, thus, are not simply artifacts of earlier smoking.
Mediational Analyses
Only two variables met criteria for mediation: i.e., evidence of a significant relation between treatment and the mediator, a significant relation between the mediator and abstinence (controlling for treatment), and a statistically significant estimated mediated effect (as indicated by asymmetric confidence intervals that do not comprise zero [21]). Cessation self-efficacy was higher amongst those receiving counseling than amongst control participants, and was predictive of abstinence at the end of treatment. Declines in perceived difficulty quitting were also greater in those receiving counseling than in those in the control group, and this was predictive of later abstinence. Although reduced access to cigarettes was significantly related to both counseling and abstinence, the estimate of the mediated effect was not statistically significant. Other targets effectively improved by counseling were not predictive of abstinence, and other predictors of abstinence were not significantly affected by treatment.
The most parsimonious conclusion from these analyses is that counseling was ineffective because it failed to have meaningful effects on many of the target behaviors and beliefs that were most important in determining abstinence, such as motivation and willingness to work at quitting, social support, or withdrawal distress. This raises broader questions about the impact of behavioral counseling in general, specifically about the translation from treatment content to actual patient behavior. Little is known about the processes that are important for effectively making this transition, and this suggests the importance of testing the effect of treatment on target behaviors.
Limitations
The failure to detect predicted relations may reflect problems in assessment or delivery of the counseling intervention. For example, assessment reactivity may have contributed to downward trends in almost all the ratings and behaviors tracked post-quit. We consider this unlikely, however, as assessment began weeks before quitting and many targets showed initial increases in endorsement in the first week of assessment followed by later declines and the rate of decline varied markedly across variables. Endorsement rates of quitting-related behaviors and beliefs may decline over the first few weeks of a quit attempt as subjects re-establish stability in their smoking behavior (whether the outcome is abstinence or smoking) and, therefore, devote less effort to smoking or abstaining. In addition, the generalizability of the current results to the broader population of smokers may be limited, particularly in light of the racial homogeneity of the sample and the remuneration offered to participants. Attrition and the number of tests conducted may also render results less replicable, as might the fact that the intervening variables were not manipulated directly (which limits the inferences that can be drawn based on significant mediator-outcome relations). Finally, the linear modeling strategy and timeframes adopted may not be optimal [17]. Inclusion of moderators and examination of moderated mediation may also have yielded different results.
Conclusions
Results from this randomized clinical trial provide limited support for prevailing models of smoking cessation counseling and abstinence determinants. Results suggested that the processes targeted in Guidelines-based treatment are indeed important in predicting abstinence, but that brief smoking cessation counseling may affect few of these targets as intended. As such, current treatment efforts could be enhanced to better address potent predictors of abstinence.
Supplementary Material
Acknowledgments
This work was supported by Transdisciplinary Tobacco Use Research Center grant P50CA084724 from the National Cancer Institute and P50DA19706 from the National Institute of Drug Abuse. We thank the staff of the Center for Tobacco Research and Intervention at the University of Wisconsin School of Medicine and Public Health.
Douglas E. Jorenby has received research support from Nabi Biopharmaceutical and Pfizer, Inc. and consulting fees from Nabi Biopharmaceutical. Saul Shiffman serves as consultant to GlaxoSmithKline Consumer Healthcare on an exclusive basis regarding OTC smoking cessation products and is also a partner in a company that is developing a new nicotine medication. He is a co-founder of invivodata, inc., which provides electronic diary services for clinical research. Timothy B. Baker has conducted research sponsored by GlaxoSmithKline, Nabi Biopharmaceuticals, Pfizer, and Sanofi-Synthelabo.
GlaxoSmithKline provided complementary active and placebo medication used in this study. GlaxoSmithKline was not involved in the design, data collection, analysis or reporting of this study.
References
- 1.Fiore MC, Jaén CR, Baker TB, et al. Rockville, MD: U.S. Department of Health and Human Services, Public Health Service; Treating Tobacco Use and Dependence: 2008 Update. Clinical Practice Guideline. 2008 May;
- 2.Lancaster T, Stead LF. Individual behavioural counselling for smoking cessation. The Cochrane Database of Systematic Reviews. 2005;(Issue 2) doi: 10.1002/14651858.CD001292.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Stead LF, Lancaster T. Group behaviour therapy programmes for smoking cessation. Cochrane Database of Systematic Reviews. 2005;(Issue 1) doi: 10.1002/14651858.CD001007.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Stead LF, Perera R, Lancaster T. Telephone counseling for smoking cessation. Cochrane Database of Systematic Reviews. 2006;(Issue 1) doi: 10.1002/14651858.CD002850.pub2. [DOI] [PubMed] [Google Scholar]
- 5.MacLeod ZR, Charles MA, Arnaldi VC, Adams IM. Telephone counseling as an adjunct to nicotine patches in smoking cessation: a randomized controlled trial. Med J Australia. 2003;179:349–352. doi: 10.5694/j.1326-5377.2003.tb05590.x. [DOI] [PubMed] [Google Scholar]
- 6.Hall SM, Lightwood JM, Humfleet GL, Bostrom A, Reus VI, Munoz R. Cost-effectiveness of bupropion, nortriptyline, and psychological intervention in smoking cessation. J Behav Health Ser R. 2005;32:381–392. doi: 10.1007/BF02384199. [DOI] [PubMed] [Google Scholar]
- 7.Bronson DL, Flynn BS, Solomon LJ, Vacek PM, Secker-Walker RH. Smoking cessation counselling during periodic health examinations. Arch Intern Med. 1989;149:1653–1656. [PubMed] [Google Scholar]
- 8.Burling TA, Marshall GD, Seidner AL. Smoking cessation for substance abuse inpatients. J Subst Abuse. 1991;3:269–276. doi: 10.1016/s0899-3289(10)80011-2. [DOI] [PubMed] [Google Scholar]
- 9.Fiore MC, McCarthy DE, Jackson TC, Zehner ME, Jorenby DE, Mielke M, Smith SS, Guiliani TA, Baker TB. Integrating smoking cessation treatment into primary care: An effectiveness study. Prev Med. 2004;38:412–420. doi: 10.1016/j.ypmed.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 10.Jorenby DE, Smith SS, Fiore MC, Hurt RD, Offord KP, Croghan IT, et al. Varying nicotine patch dose and type of smoking cessation counseling. JAMA. 1995;274:1347–1352. [PubMed] [Google Scholar]
- 11.Irvin JE, Brandon TH. The increasing recalcitrance of smokers in clinical trials. Nicotine Tob Res. 2000;2:79–84. doi: 10.1080/14622200050011330. [DOI] [PubMed] [Google Scholar]
- 12.Hughes JR, Brandon TH. A softer view of hardening. Nicotine Tob Res. 2003;5:961–962. doi: 10.1080/14622200310001615330. [DOI] [PubMed] [Google Scholar]
- 13.U.S. Department of Health and Human Services. Bethesda, MD: U.S. Department of Health and Human Services, National Institutes of Health, National Cancer Institute; Those Who Continue to Smoke: Is Achieving Abstinence Harder and Do We Need to Change Our Interventions? Smoking and Tobacco Control Monograph No. 15. 2003 [NIH Publication No. 3260].
- 14.Warner KE, Burns DM. Hardening and the hard-core smoker: concepts, evidence, and implications. Nicotine Tob Res. 2003;5:37–48. doi: 10.1080/1462220021000060428. [DOI] [PubMed] [Google Scholar]
- 15.Ferguson SG, Shiffman S, Gwaltney CJ. Does reducing withdrawal severity mediate nicotine patch efficacy? A randomized clinical trial. J Consult Clin Psych. 2006;74:1153–1161. doi: 10.1037/0022-006X.74.6.1153. [DOI] [PubMed] [Google Scholar]
- 16.Lerman C, Roth D, Kaufmann V, Audrain J, Hawk L, Liu W, et al. Mediating mechanisms for the impact of bupropion in smoking cessation treatment. Drug Alcohol Depen. 2002;67:219–223. doi: 10.1016/s0376-8716(02)00067-4. [DOI] [PubMed] [Google Scholar]
- 17.McCarthy DE, Piasecki TM, Lawrence DL, Jorenby DE, Shiffman S, Baker TB. Psychological mediators of bupropion SR treatment for smoking cessation. Addiction. 2008;103:1521–1533. doi: 10.1111/j.1360-0443.2008.02275.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Piper ME, Federman EB, McCarthy DE, Bolt DM, Smith SS, Fiore MC, Baker TB. Using mediational models to explore the nature of tobacco motivation. J Abnorm Psychol. 2008;117:94–105. doi: 10.1037/0021-843X.117.1.94. [DOI] [PubMed] [Google Scholar]
- 19.Kenny DA, Kashy DA, Bolger N. Data analysis in social psychology. In: Gilbert D, Fiske ST, Lindzey G, editors. Handbook of Social Psychology. 4th edn. vol. 1. New York: McGraw Hill; 1998. pp. 233–265. [Google Scholar]
- 20.Kraemer HC, Wilson GT, Fairburn GC, Agras WS. Mediators and moderators of treatment effects in randomized controlled trials. Arch Gen & Psychiat. 2002;59:877–883. doi: 10.1001/archpsyc.59.10.877. [DOI] [PubMed] [Google Scholar]
- 21.MacKinnon DP. Introduction to statistical mediation analysis. New York: Lawrence Earlbaum Associates; 2008. [Google Scholar]
- 22.Piasecki TM. Relapse to smoking. Clin Psychol Rev. 2006;26:196–215. doi: 10.1016/j.cpr.2005.11.007. [DOI] [PubMed] [Google Scholar]
- 23.Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychol Rev. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- 24.Shiffman S, Paty JA, Gnys M, Kassel JD, Hickcox M. First lapses to smoking: Within-subjects analysis of real-time reports. J Consult Clin Psych. 1996;64:366–379. doi: 10.1037//0022-006x.64.2.366. [DOI] [PubMed] [Google Scholar]
- 25.Shiffman S, Paty J A, Rohay JM, Di Marino ME, Gitchell JG. The efficacy of computer-tailored smoking cessation material as a supplement to nicotine polacrilex gum therapy. Arch Intern Med. 2000;160:1675–1681. doi: 10.1001/archinte.160.11.1675. [DOI] [PubMed] [Google Scholar]
- 26.Boardman T, Catley D, Mayo MS, Ahluwalia JS. Self-efficacy and motivation to quit during participation in a smoking cessation program. Int J Behav Med. 2005;12:266–272. doi: 10.1207/s15327558ijbm1204_7. [DOI] [PubMed] [Google Scholar]
- 27.Brandon TH, Herzog TA, Juliano LM, Irvin JE, Lazev AB, Simmons VN. Pretreatment task persistence predicts smoking cessation outcome. J Abnorm Psychol. 2003;112:448–456. doi: 10.1037/0021-843x.112.3.448. [DOI] [PubMed] [Google Scholar]
- 28.Condiotte MM, Lichtenstein E. Self-efficacy and relapse in smoking cessation programs. J Consult Clin Psych. 1981;49:648–658. doi: 10.1037//0022-006x.49.5.648. [DOI] [PubMed] [Google Scholar]
- 29.Curry SJ, Grothaus L, McBride C. Reasons for quitting: Intrinsic and extrinsic motivation for smoking cessation in a population-based sample of smokers. Addict Behav. 1997;22:727–739. doi: 10.1016/s0306-4603(97)00059-2. [DOI] [PubMed] [Google Scholar]
- 30.Hyland A, Li Q, Bauer JE, Giovino GA, Steger C, Cummings KM. Predictors of cessation in a cohort of current and former smokers followed over 13 years. Nicotine Tob Res. 2004;6:363–369. doi: 10.1080/14622200412331320761. [DOI] [PubMed] [Google Scholar]
- 31.Marlatt GA, Gordon JR. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. New York: Guilford Press; 1985. [Google Scholar]
- 32.Shiffman S, Balabanis MH, Paty JA, Engberg J, Gwaltney CJ, Liu KS, et al. Dynamic effects of self-efficacy on smoking lapse and relapse. Health Psychol. 2000;19:315–323. doi: 10.1037//0278-6133.19.4.315. [DOI] [PubMed] [Google Scholar]
- 33.Shiffman S, Hickcox M, Paty JA, Gnys M, Kassel JD, Richards TJ. Progression from a smoking lapse to relapse: Prediction from abstinence violation effects, nicotine dependence, and lapse characteristics. J Consult Clin Psychol. 1996;64:993–1002. doi: 10.1037//0022-006x.64.5.993. [DOI] [PubMed] [Google Scholar]
- 34.Shiffman S. Conceptual issues in the study of relapse. In: Gossop M, editor. Relapse and addictive behaviour. Kent, England: Croom Helm Ltd; 1989. [Google Scholar]
- 35.Wills TA, Shiffman S. Coping behavior and its relation to substance use: A conceptual framework. In: Shiffman S, Wills TA, editors. Coping and Substance Use. New York: Academic Press; 1985. [Google Scholar]
- 36.U.S. Department of Health and Human Services. Rockville, MD: U.S. Public Health Service. Agency for Healthcare Research and Quality; You Can Quit Smoking. Support and Advice from Your Prenatal Care Provider. Consumer Tear Sheet, September 2008. http://www.ahrq.gov/clinic/tobacco/prenatal.htm.
- 37.Curry S, Marlatt GA, Gordon JR. Abstinence violation effect: Validation of an attributional construct with smoking cessation. J Consult Clin Psychol. 1987;55:145–149. doi: 10.1037//0022-006x.55.2.145. [DOI] [PubMed] [Google Scholar]
- 38.McCarthy DE, Piasecki TM, Lawrence DL, Jorenby DE, Shiffman S, Fiore M, et al. A randomized, controlled clinical trial of bupropion SR and individual smoking cessation counseling. Nicotine Tob Res. 2008;10:717–729. doi: 10.1080/14622200801968343. [DOI] [PubMed] [Google Scholar]
- 39.Collins LM, Graham JW, Flaherty BP. An alternative framework for defining mediation. Multivar Behav Res. 1998;33:295–312. doi: 10.1207/s15327906mbr3302_5. [DOI] [PubMed] [Google Scholar]
- 40.Stone AA, Shiffman S. Ecological momentary assessment (EMA) in behavioral medicine. Annals of Behavioral Medicine. 1994;16:199–202. [Google Scholar]
- 41.Shiffman S, Stone AA, Hufford M. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32. doi: 10.1146/annurev.clinpsy.3.022806.091415. [DOI] [PubMed] [Google Scholar]
- 42.Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. Brit J Addict. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- 43.Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 44.SRNT Subcommittee on Biochemical Verification. Biochemical verification of tobacco use and cessation. Nicotine Tob Res. 2002;4:149–159. doi: 10.1080/14622200210123581. [DOI] [PubMed] [Google Scholar]
- 45.Shiffman S, Hickcox M, Paty JA, Gnys M, Kassel JD, Richards T. The Abstinence Violation Effect following smoking lapses and temptations. Cognitive Ther Res. 1997;21:497–523. [Google Scholar]
- 46.Raudenbush S, Bryk A, Cheong YF, Congdon R, du Toit M. HLM 6: Hierarchical linear and nonlinear modeling. Lincolnwood, IL: Scientific Software International; 2004. [Google Scholar]
- 47.Cole DA, Maxwell SE. Testing mediational models with longitudinal data: Questions and tips in the use of structural equation modeling. J Abnorm Psychol. 2003;112:558–577. doi: 10.1037/0021-843X.112.4.558. [DOI] [PubMed] [Google Scholar]
- 48.MacKinnon DP, Fritz MS, Williams J, Lockwood CM. Distribution of the product confidence limits for the indirect effect: Program PRODCLIN. Behav Res Methods. 2005;39:384–389. doi: 10.3758/bf03193007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.O’Connell KA, Gerkovich MM, Bott MJ, Cook MR, Shiffman S. The effect of anticipatory strategies on the first day of smoking cessation. Psychol Addict Behav. 2002;16:150–156. [PubMed] [Google Scholar]
- 50.Shiffman S. A cluster-analytic classification of smoking relapse episodes. Addict Behav. 1986;11:295–307. doi: 10.1016/0306-4603(86)90057-2. [DOI] [PubMed] [Google Scholar]
- 51.Horwitz MB, Hindi-Alexander M, Wagner TJ. Psychosocial mediators of abstinence, relapse, and continued smoking: a one-year follow-up of a minimal intervention. Addict Behav. 1985;10:29–39. doi: 10.1016/0306-4603(85)90050-4. [DOI] [PubMed] [Google Scholar]
- 52.Gwaltney CJ, Shiffman S, Balabanis MH, Paty JA. Dynamic self-efficacy and outcome expectancies: prediction of smoking lapse and relapse. J Abnorm Psychol. 2005;114:661–675. doi: 10.1037/0021-843X.114.4.661. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.