Abstract
Studies demonstrate that the apolipoprotein B/apolipoprotein A-I (ApoB/apoA-I) ratio predicts cardiovascular risk better than any of the cholesterol indexes. A number of factors that define the metabolic syndrome (MS) differ across African-American and European-American ethnicities. We assessed relationship of the apoB/apoA-I ratio to MS and coronary artery disease (CAD) in 224 African-Americans and 304 European-Americans. The MS was defined by the revised NCEP-ATP III criteria and CAD was assessed as ≥50% stenosis or a continuous cardiovascular score (0–75). European-Americans had higher apoB/apoA-I ratio compared with African-Americans (1.15 vs. 1.07, P=0.008). The apoB/apoA-I ratio was associated with presence of the MS in both European-Americans (OR=5.9; 95% confidence interval (CI), 2.53–13.57; P<0.001) and African-Americans (OR=8.3; 95% CI, 3.52–19.25; P<0.001), and was higher in subjects with MS compared to those without MS (1.21 vs. 1.04, P<0.001 for European-Americans and 1.20 vs. 0.94, P<0.001 for African-Americans). There was a stepwise increase in the prevalence of MS across apoB/apoA-I ratio tertiles in both ethnic groups (χ2=13.1, P<0.001 for European-Americans and χ2=19.6, P<0.001 for African-Americans). In multiple regression analyses, the apoB/apoA-I ratio independently predicted CAD in African-Americans (β=0.242, P=0.011). The cardiovascular score was significantly increased across apoB/apoA-I ratio tertiles in European-American subjects with MS (P=0.001), whereas this association was seen in African-American subjects without MS (P=0.023). In conclusion, the apoB/apoA-I ratio differed across ethnicities and was associated with presence of the MS in both groups. Among African-Americans, elevated apoB/apoA-I ratio independently predicted higher risk for CAD.
Keywords: apoB/apoA-I ratio, cardiovascular disease, ethnicity
A number of population based studies have suggested that the apolipoprotein B (apoB)/apolipoprotein A-I (apoA-I) ratio, an indicator of the balance between atherogenic and atheroprotective cholesterol transport, predicts cardiovascular risk more accurately and stronger than the use of either apoB or apoA-I alone, or any of the other cholesterol indexes.1–4 On the other hand, a cluster of metabolic abnormalities defined as metabolic syndrome (MS) has been associated with increased cardiovascular risk5–7, and we have previously reported on the differential distribution of MS components across African-American and European-American ethnicities with less frequent lipid abnormalities (hypertriglyceridemia and low high-density lipoprotein (HDL) cholesterol) among African-Americans.8 Furthermore, patients with atherogenic dyslipidemia such as MS most likely have an increased number of small, dense low-density lipoprotein (LDL) particles (which corresponds to higher apoB levels) at relatively modest LDL cholesterol levels.9 Thus, in the present study, we investigated whether the apoB/apoA-I ratio is related to the MS and its components and coronary artery disease (CAD) in the 2 ethnic groups with varying frequencies of MS components.
METHODS
Subjects were recruited from a patient population scheduled for diagnostic coronary angiography either at Harlem Hospital Center in New York City or at the Mary Imogene Bassett Hospital in Cooperstown, New York. The study design and inclusion and exclusion criteria have been described previously.8,10,11 Briefly, a total of 648 patients, self identified as European-American (n=344), African-American (n=232), or of other ethnicities (n=72), were enrolled. Of the 576 European-American and African-American subjects, 48 subjects were excluded as a result of incomplete data (16 subjects had missing coronary angiographic data, 17 subjects lacked information on waist circumference, HDL cholesterol levels were missing in 8 subjects, and information on hypertension was not available for 7 subjects). Exclusion criteria for this study included use of lipid-lowering drugs. The present report is therefore based on the findings in 528 subjects (304 European-Americans and 224 African-Americans). The study was approved by the institutional review boards at Harlem Hospital Center, Mary Imogene Bassett Hospital, Columbia University College of Physicians and Surgeons, and University of California Davis, and informed consent was obtained from all subjects.
Blood pressure was measured using a random-zero mercury sphygmomanometer. The mean of 3 measurements of systolic and diastolic blood pressure was used. Waist circumference was calculated as the average of 2 measurements taken after inspiration and expiration at the midpoint between the lowest rib and iliac crest. Participants were asked to fast for 12 hours, and blood samples were drawn approximately 2 to 4 hours before the catheterization procedure. Serum and plasma samples were separated and stored at −80°C before analysis. Concentrations of triglycerides (Sigma Diagnostics, St. Louis, Missouri), total cholesterol and glucose (Roche, Somerville, New Jersey) were determined with standard enzymatic procedures.12,13 HDL cholesterol levels were measured after precipitation of apolipoprotein B–containing lipoproteins with dextran sulfate.14 Apolipoproteins B and A-I were measured by rate immunonephelometry (Array, Beckman, Brea, CA).15
We defined MS according to revised NCEP-ATP III criteria16 by the presence of ≥3 of the following: fasting plasma glucose level ≥100 mg/dl, serum triglyceride level ≥150 mg/dl, serum HDL cholesterol level <40 mg/dl for men and <50 mg/dl for women, blood pressure ≥130/85 mm Hg, hypertension treatment, and waist circumference >102 cm for men and >88 cm for women.
The coronary angiograms were read by 2 experienced readers blinded to patient identity, clinical diagnosis, and laboratory results. The readers recorded the location and extent of luminal narrowing for 15 segments of the major coronary arteries.17 A composite cardiovascular score (0 to 75) was calculated based on determination of presence of stenosis on a scale of 0 to 5 of the 15 predetermined coronary artery segments. Presence of CAD was defined as the presence of ≥50% stenosis in any 1 of 15 coronary artery segments.
Analyses of data were done with SPSS statistical analysis software (SPSS, Chicago, Illinois). Results were expressed as means ± SE and median with interquartile ranges for non-normally distributed values. Triglyceride, insulin levels and cardiovascular scores were logarithmically transformed to achieve normal distributions. Group means were compared using the Student t-test. Age and gender adjusted Pearson’s partial correlation coefficients were calculated for apoB/apoA-I ratio and MS components across ethnicity. Proportions were compared between groups using χ2 analysis and the Fisher exact test where appropriate. A logistic regression analysis was applied to assess the association between apoB/apoA-I ratio and the presence of MS. Multiple linear regression analyses were used to explore the independent association of the variables with the cardiovascular score. One-way ANOVA was used to compare mean levels of independent variables across apoB/apoA-I ratio tertiles, and post hoc analyses were performed by Tukey’ honestly significant difference test. Unless otherwise noted, a nominal 2-sided p value <0.05 was used to assess significance.
RESULTS
As expected, African-Americans had higher levels of HDL cholesterol (P<0.001) and apolipoprotein A-I (P<0.001), and lower levels of triglyceride (P<0.001) compared with European-Americans (Table 1). The levels of total cholesterol, LDL cholesterol, and apolipoprotein B were similar in the 2 ethnic groups. Notably, the apoB/apoA-I ratio was significantly higher in European-Americans compared with African-Americans (1.15 vs. 1.07, P=0.008) (Table 1).
Table 1.
Clinical characteristics of the study population
| Characteristics | European-Americans (n=304) | African-Americans (n=224) | P-value |
|---|---|---|---|
| Men/Women | 195/109 | 126/98 | NS |
| Metabolic syndrome (%) | 199 (65%) | 110 (49%) | <0.001 |
| Coronary artery disease (%) | 173 (57%) | 99 (44%) | 0.003 |
| Diabetes mellitus (%) | 63 (21%) | 66 (29%) | 0.018 |
| Age (years) | 56.6 ± 0.6 | 54.8 ± 0.6 | 0.023 |
| Systolic blood pressure (mm Hg) | 125 ± 1.0 | 129 ± 2.0 | NS |
| Diastolic blood pressure (mm Hg) | 75 ± 0.6 | 79 ± 1.4 | 0.005 |
| Waist circumference (cm) | 105 ± 1.0 | 96 ± 1.1 | <0.001 |
| Total cholesterol (mg/dl) | 197 ± 2.3 | 198 ± 3.0 | NS |
| LDL cholesterol (mg/dl) | 123 ± 2.0 | 126 ± 2.8 | NS |
| HDL cholesterol (mg/dl) | 41 ± 0.7 | 49 ± 1.1 | <0.001 |
| Triglyceride (mg/dl) | 151 (110–216) | 106 (80–144) | <0.001 |
| Glucose (mg/dl) | 132 ± 3.8 | 119 ± 3.3 | 0.013 |
| Insulin (μU/ml) | 15.1 (9.2–25.2) | 14.1 (8.7–21.7) | NS |
| Apolipoprotein B (mg/dl) | 136 ± 2.0 | 134 ± 2.7 | NS |
| Apolipoprotein A-I (mg/dl) | 122 ± 1.3 | 130 ± 1.9 | <0.001 |
| ApoB/apoA-I | 1.15 ± 0.33 | 1.07 ± 0.37 | 0.008 |
| Composite cardiovascular score | 12.9 (1.9–27.1) | 8.3 (1.5–24.9) | NS |
Values are expressed as mean ± SE and median (interquartile range) for non-normally distributed values. Group means were compared using Student’s t-tests and proportions were compared using χ2 analysis. Values for triglycerides and insulin were logarithmically transformed before analyses. Apo, apolipoprotein; HDL, high-density lipoprotein; LDL, low-density lipoprotein; NS, non significant.
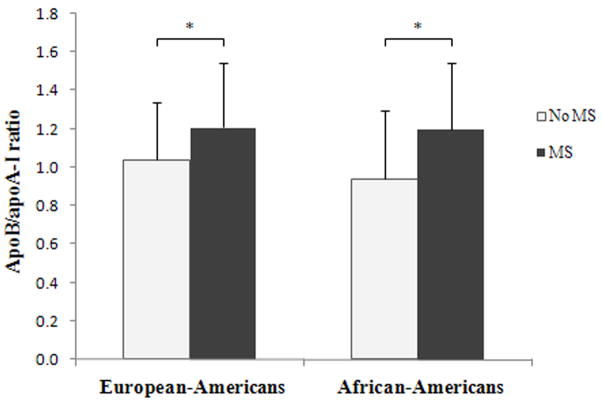
The apoB/apoA-I ratio was significantly associated with presence of the MS in both European-Americans (OR=5.9; 95% confidence interval (CI), 2.53–13.57; P<0.001) and African-Americans (OR=8.3; 95% CI, 3.52–19.25; P<0.001), As seen in Figure 1, the apoB/apoA-I ratio was significantly higher in subjects with MS compared to those without MS in both ethnic groups (1.21 vs. 1.04, P<0.001 for European-Americans and 1.20 vs. 0.94, P<0.001 for African-Americans). To explore the association between apoB/apoA-I ratio and MS in more detail, we dichotomized the study subjects into 3 groups according to their apoB/apoA-I levels. There was a stepwise increase in the prevalence of MS across apoB/apoA-I ratio tertiles in both ethnic groups (χ2=13.1, P<0.001 for European-Americans and χ2=19.6, P<0.001 for African-Americans, Figure 2). Further, as seen in the figure, European-Americans had higher prevalence of MS compared to African-Americans for all apoB/apoA-I ratio tertiles. Irrespective of ethnicity, the apoB/apoA-I ratio was significantly and positively correlated with systolic blood pressure and triglyceride levels, and negatively with HDL cholesterol levels (Table 2). In addition, among European-Americans, the apoB/apoA-I ratio was significantly correlated with waist circumference (P=0.008). The apoB/apoA-I ratio was significantly increased with increasing number of MS components in both European-Americans (P<0.001) and African-Americans (P<0.001) (Supplemental Figure 1).
Figure 1.
ApoB/apoA-I ratio in subjects with and without MS across ethnic groups. *: P<0.001
Figure 2.
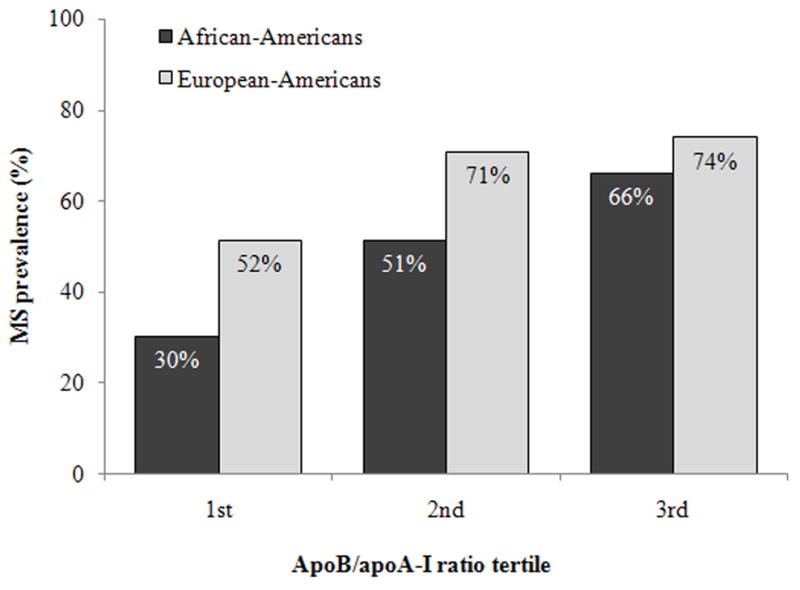
Prevalence of MS across apoB/apoA-I ratio tertiles among European-Americans and African-Americans. The cut-off points for tertiles were ≤0.98, 0.98–1.26, ≥1.26 for European-Americans and ≤0.88, 0.88–1.20, ≥1.20 for African-Americans, respectively. The results are based on n=99 for 1st, n=103 for 2nd and n=100 for 3rd tertiles in European-Americans and n=76 for 1st, n=74 for 2nd and n=74 for 3rd tertiles in African-Americans. Two European-American subjects (1 with and 1 without MS) were excluded from the analyses due to missing data.
Table 2.
Pearson’s partial correlation coefficients between apolipoprotein B/apolipoprotein A-I ratio and metabolic syndrome components across ethnicity (adjusted for age and gender)
| Variable | European-Americans | P-value | African-Americans | P-value |
|---|---|---|---|---|
| Waist circumference (cm) | 0.154 | 0.008 | 0.170 | NS |
| Systolic blood pressure (mm Hg) | 0.144 | 0.013 | 0.304 | 0.005 |
| Diastolic blood pressure (mm Hg) | 0.059 | NS | 0.156 | NS |
| HDL cholesterol (mg/dl) | − 0.454 | <0.0001 | − 0.579 | <0.0001 |
| Triglyceride (mg/dl) | 0.415 | <0.0001 | 0.406 | <0.0001 |
| Glucose (mg/dl) | 0.080 | NS | 0.190 | NS |
Values for triglycerides were logarithmically transformed before analyses. HDL, high-density lipoprotein; NS, non significant.
Further analysis using multiple linear regression models was carried out to explore whether the apoB/apoA-I ratio predicts CAD (as measured by the composite cardiovascular score) and whether this association would be independent of other established CVD risk factors and/or presence of MS (Table 3). When apoB/apoA-I ratio and other major CVD risk factors were considered (i.e., model 1), age (β=0.375, P<0.001), gender (β=−0.237, P<0.001), hypertension (β=0.168, P=0.002) and smoking (β=0.158, P=0.002) were key determinants explaining 30% of the cardiovascular score in European-Americans. Notably, no significant association was found between the apoB/apoA-I ratio and CAD in this particular ethnic group. In contrast, for African-Americans, the apoB/apoA-I ratio (β=0.335, P=0.014) and age (β=0.395, P<0.001) were independently and strongly associated with the cardiovascular score. When MS was included in the model (i.e., model 2), in European-Americans, the independent association of age (β=0.395, P<0.001), gender (β=−0.249, P<0.001) and smoking (β=0.156, P=0.003) with CAD remained all significant, with an addition of MS (β=0.114, P=0.037). For African-Americans, the association of apoB/apoA-I ratio (β=0.242, P=0.011) and age (β=0.383, P<0.001) with CAD both remained significant, but there was no association with the MS.
Table 3.
Multiple regression analyses of apolipoprotein B/apolipoprotein A-I ratio, metabolic syndrome and other established cardiovascular risk factors with cardiovascular score in European-Americans and African Americans.
| Model | Independent variables | R2 | F | β | P-value |
|---|---|---|---|---|---|
| Ethnicity | |||||
| Model 1 | |||||
| European-Americans | 0.301 | 13.0 | <0.001 | ||
| Age (years) | 0.375 | <0.001 | |||
| Gender (m/f) | − 0.237 | <0.001 | |||
| LDL cholesterol (mg/dl) | 0.012 | NS | |||
| HDL cholesterol (mg/dl) | − 0.035 | NS | |||
| Triglyceride (mg/dl) | 0.002 | NS | |||
| Waist circumference (cm) | − 0.001 | NS | |||
| Hypertension (y/n) | 0.168 | 0.002 | |||
| Smoking (y/n) | 0.158 | 0.002 | |||
| ApoB/apoA-I | 0.112 | NS | |||
| African-Americans | 0.225 | 6.8 | <0.001 | ||
| Age (years) | 0.395 | <0.001 | |||
| Gender (m/f) | − 0.042 | NS | |||
| LDL cholesterol (mg/dl) | − 0.044 | NS | |||
| HDL cholesterol (mg/dl) | 0.116 | NS | |||
| Triglyceride (mg/dl) | 0.106 | NS | |||
| Waist circumference (cm) | − 0.044 | NS | |||
| Hypertension (y/n) | − 0.039 | NS | |||
| Smoking (y/n) | 0.085 | NS | |||
| ApoB/apoA-I | 0.335 | 0.014 | |||
| Model 2 | |||||
| European-Americans | 0.287 | 18.9 | <0.001 | ||
| Age (years) | 0.395 | <0.001 | |||
| Gender (m/f) | − 0.249 | <0.001 | |||
| LDL cholesterol (mg/dl) | 0.014 | NS | |||
| Smoking (y/n) | 0.156 | 0.003 | |||
| Metabolic syndrome (y/n) | 0.114 | 0.037 | |||
| ApoB/apoA-I | 0.126 | NS | |||
| African-Americans | 0.209 | 9.5 | <0.001 | ||
| Age (years) | 0.383 | <0.001 | |||
| Gender (m/f) | − 0.049 | NS | |||
| LDL cholesterol (mg/dl) | 0.014 | NS | |||
| Smoking (y/n) | 0.097 | NS | |||
| Metabolic syndrome (y/n) | 0.046 | NS | |||
| ApoB/apoA-I | 0.242 | 0.011 | |||
Model 1; adjusted for age, gender, LDL and HDL cholesterol, triglycerides, waist circumference, hypertension, smoking and apoB/apoA-I ratio for both ethnic groups. Model 2; adjusted for Model 1 with an addition of metabolic syndrome for both ethnic groups. Apo, apolipoprotein; LDL, low-density lipoprotein; NS, non significant.
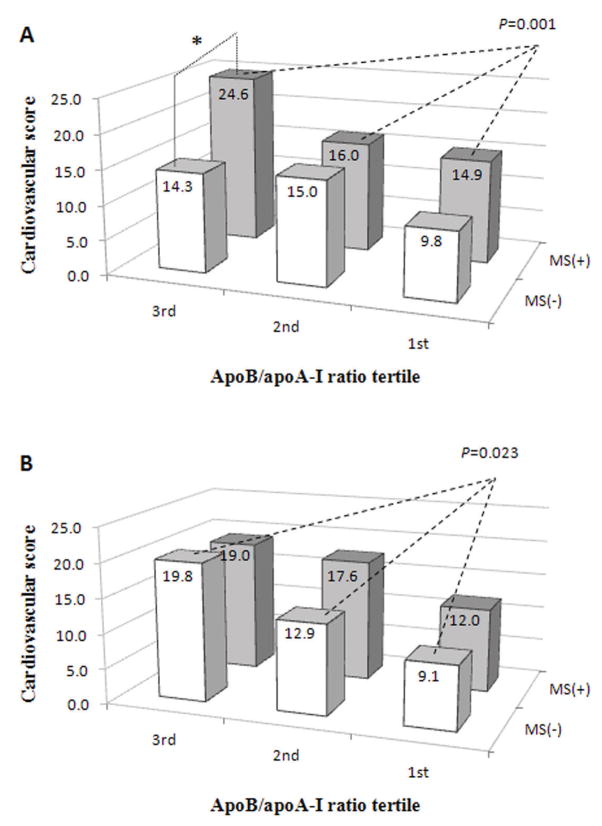
Finally, we investigated the combined effect of the apoB/apoA-I ratio and presence of the MS on the magnitude of CAD in the 2 ethnic groups (Figure 3). Among European-Americans, subjects with MS and a high apoB/apoA-I ratio had a significant increase of the composite cardiovascular score compared to subjects with MS and a low ratio (P=0.001), whereas no such difference was seen among subjects without MS (Figure 3A). A somewhat different picture was seen among African-Americans, where a significant increase in the composite cardiovascular score was seen among subjects without MS and with a high apoB/apoA-I ratio compared with those without MS and a low ratio (P=0.023, Figure 3B). Notably, no such difference was seen among African-American subjects with MS. Further, we observed a clear difference in the composite cardiovascular score among subjects in the highest apoB/apoA-I ratio tertile across ethnicity and MS status. For European-Americans in the highest apoB/apoA-I ratio tertile, the composite cardiovascular score was significantly elevated in subjects with MS compared to those without MS (24.6 vs. 14.3, P=0.001, Figure 3A). In contrast, for African-Americans in the highest apoB/apoA-I ratio tertile, the composite cardiovascular score was similar in subjects with and without MS (19.0 vs. 19.8, Figure 3B).
Figure 3.
Composite cardiovascular scores across apoB/apoA-I ratio tertiles among European-Americans (A) and African-Americans (B) with and without MS. ApoB/apoA-I tertiles were based on all subjects within each ethnic group and the numbers were (A) n=51 for 1st, n=73 for 2nd and n=74 for 3rd tertiles for subjects with MS and n=48 for 1st, n=30 for 2nd and n=26 for 3rd tertiles for subjects without MS among European-Americans; (B) n=23 for 1st, n=38 for 2nd and n=49 for 3rd tertiles for subjects with MS and n=53 for 1st, n=36 for 2nd and n=25 for 3rd tertiles for subjects without MS among African-Americans. Two European-American subjects (1 with and 1 without MS) were excluded from the analyses due to missing data. *: P=0.001.
DISCUSSION
The main novel finding in our study was a differential role of the apoB/apoA-I ratio and MS as CAD risk factors across African-American and European-American ethnicities. When the apoB/apoA-I ratio and MS were considered along with other established CVD risk factors (age, gender, LDL cholesterol and smoking), the apoB/apoA-I ratio was independently associated with a higher degree of CAD in African-Americans, but not in European-Americans. On the contrary, the MS was a major determinant of the cardiovascular score in European-Americans, but not in African-Americans. Furthermore, European-Americans with MS in the highest apoB/apoA-I ratio tertile had substantially higher cardiovascular score compared with those in subjects without MS. Thus, in European-Americans, the apoB/apoA-I ratio may provide additional prognostic information beyond MS with regard to CAD risk. These findings also support prior data representing a synergistic effect of the MS and a high apoB/apoA-I ratio on the magnitude of CAD.18,19
The apoB/apoA-I ratio was lower in African-Americans than in European-Americans. African-American subjects had higher levels of HDL cholesterol and apoA-I at comparable levels of total and LDL cholesterol and apoB compared with European-Americans. This differential lipid and lipoprotein pattern correlates with the observed difference in the apoB/apoA-I ratio between these 2 ethnic groups. In principle, subjects with a low apoB/apoA-I ratio have less apoB and more apoA-I particles. Therefore, it is tempting to speculate that the high apoA-I and the comparable apoB levels in African-Americans generated a lower apoB/apoA-I ratio in this particular ethnic group. In a large case-control study4 conducted in 52 countries, the apoB/apoA-I ratio was shown to be variable across ethnicities with high mean values in south Asians, Arabs, Persians and Latin Americans and with low mean values in Chinese and African-Americans. For European-Americans, the ratio was recorded between the 2 values. Thus, our results, that show apoB/apoA-I ratio was lower in African-Americans than in European-Americans, are consistent with the findings of the former study.4
Previously, we reported that the prevalence of the MS, as assessed by the revised criteria proposed by NCEP-ATP III16, was lower in African-Americans than in European-Americans (49% vs. 65%), and the abnormal lipid components of the MS were less frequent among the former ethnical group.8 On a population level, African-American subjects generally have lower triglyceride and higher HDL cholesterol levels than European-American subjects20–22, which may in turn explain some of the frequency difference in prevalence of the MS components between these 2 groups. In European-Americans, the higher prevalence and more common lipid abnormalities may have made the MS as a strong and independent predictor of CAD. Conversely, in African-Americans, the lower prevalence and less common lipid abnormalities have made it difficult to identify the independent role of the MS, suggesting that the apoB/apoA-I ratio may be an important independent predictor of cardiovascular risk in this ethnic group.
In agreement with previous studies18,19,23 the apoB/apoA-I ratio was associated with MS and its major components such as systolic blood pressure, HDL cholesterol and triglyceride levels, regardless of ethnicity. Moreover, subjects with increasing number of MS components had a parallel increase in the apoB/apoA-I ratio in both ethnic groups. In line with others20,24 and with our previous study8, prevalence of MS was higher among European-Americans compared with African-Americans for all apoB/apoA-I ratio tertiles and was gradually increased with an increasing ratio of apoB/apoA-I in the 2 ethnic groups.
Among European-Americans, our findings reinforce the concept that presence of MS combined with a high apoB/apoA-I ratio synergistically increases the risk for CAD. However, among African-Americans, a high apoB/apoA-I ratio independently and strongly predicted increased risk for CAD regardless of the MS status. Taken together, our data has several clinically important implications. First, the predictive value of the apoB/apoA-I ratio for CAD risk differed across African-American and European-American subjects with and without MS. Particularly, in European-Americans, the ratio may provide additional prognostic information beyond MS. Second, a high apoB/apoA-I ratio predicted increased coronary risk in African-American subjects even without MS. Therefore, in African-Americans, the apoB/apoA-I ratio may have the potential to yield additional important information and be used as a CAD risk assessment tool. Third, since the apoB/apoA-I ratio is a risk factor for CAD, therapeutic targeting of a high apoB/apoA-I ratio (reducing the number of apoB-containing atherogenic lipoprotein particles e.g. LDL cholesterol and raising the number of apoA-I containing anti-atherogenic lipoprotein particles e.g. HDL cholesterol) might be important for CAD risk reduction in both European-Americans and African-Americans regardless of their MS status.
We acknowledge some limitations of this study. The study design was cross-sectional in nature and the sample size was relatively small. Subjects in our study were recruited from patients scheduled for coronary angiography and were likely more typical of a high-risk patient group than the healthy population at large. This may explain the relatively higher levels of apoB and apoB/apoA-I ratios in our subjects. However, none of the patients had histories of acute coronary symptoms or surgical intervention within 6 months, arguing against any secondary increase in inflammatory parameters due to an acute CAD. Furthermore, clinical and laboratory parameters were in agreement with differences generally observed between healthy African-American and European-American populations in other studies. Although our findings need to be confirmed in larger population-based studies, they suggest that targeted, individualized prevention strategies might be of value in the treatment of heterogeneous patient populations.
Supplementary Material
Association between apoB/apoA-I ratio and number of components in the MS among European-Americans and African-Americans, (P<0.001 for both ethnic groups).
Acknowledgments
Dr. Pearson was supported by Grant HL 49735 from National Heart, Lung and Blood Institute, Bethesda, Maryland. Dr. Berglund was supported by Grant HL 62705 from National Heart, Lung and Blood Institute, Davis, CA. This work was supported in part by the University of California Davis Clinical and Translational Science Center (RR 024146).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Yusuf S, Hawken S, Ounpuu S, Dans T, Avezum A, Lanas F, McQueen M, Budaj A, Pais P, Varigos J, Lisheng L. Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control study. Lancet. 2004;364:937–952. doi: 10.1016/S0140-6736(04)17018-9. [DOI] [PubMed] [Google Scholar]
- 2.Gotto AM, Jr, Whitney E, Stein EA, Shapiro DR, Clearfield M, Weis S, Jou JY, Langendorfer A, Beere PA, Watson DJ, Downs JR, de Cani JS. Relation between baseline and on-treatment lipid parameters and first acute major coronary events in the Air Force/Texas Coronary Atherosclerosis Prevention Study (AFCAPS/TexCAPS) Circulation. 2000;101:477–484. doi: 10.1161/01.cir.101.5.477. [DOI] [PubMed] [Google Scholar]
- 3.Kastelein JJ, van der Steeg WA, Holme I, Gaffney M, Cater NB, Barter P, Deedwania P, Olsson AG, Boekholdt SM, Demicco DA, Szarek M, LaRosa JC, Pedersen TR, Grundy SM. Lipids, apolipoproteins, and their ratios in relation to cardiovascular events with statin treatment. Circulation. 2008;117:3002–3009. doi: 10.1161/CIRCULATIONAHA.107.713438. [DOI] [PubMed] [Google Scholar]
- 4.McQueen MJ, Hawken S, Wang X, Ounpuu S, Sniderman A, Probstfield J, Steyn K, Sanderson JE, Hasani M, Volkova E, Kazmi K, Yusuf S. Lipids, lipoproteins, and apolipoproteins as risk markers of myocardial infarction in 52 countries (the INTERHEART study): a case-control study. Lancet. 2008;372:224–233. doi: 10.1016/S0140-6736(08)61076-4. [DOI] [PubMed] [Google Scholar]
- 5.Reaven GM. Banting lecture 1988. Role of insulin resistance in human disease. Diabetes. 1988;37:1595–1607. doi: 10.2337/diab.37.12.1595. [DOI] [PubMed] [Google Scholar]
- 6.Grundy SM. Does a diagnosis of metabolic syndrome have value in clinical practice? Am J Clin Nutr. 2006;83:1248–1251. doi: 10.1093/ajcn/83.6.1248. [DOI] [PubMed] [Google Scholar]
- 7.Reaven GM. The metabolic syndrome: is this diagnosis necessary? Am J Clin Nutr. 2006;83:1237–1247. doi: 10.1093/ajcn/83.6.1237. [DOI] [PubMed] [Google Scholar]
- 8.Anuurad E, Chiem A, Pearson TA, Berglund L. Metabolic syndrome components in African-Americans and European-American patients and its relation to coronary artery disease. Am J Cardiol. 2007;100:830–834. doi: 10.1016/j.amjcard.2007.04.025. [DOI] [PubMed] [Google Scholar]
- 9.Kathiresan S, Otvos JD, Sullivan LM, Keyes MJ, Schaefer EJ, Wilson PW, D’Agostino RB, Vasan RS, Robins SJ. Increased small low-density lipoprotein particle number: a prominent feature of the metabolic syndrome in the Framingham Heart Study. Circulation. 2006;113:20–29. doi: 10.1161/CIRCULATIONAHA.105.567107. [DOI] [PubMed] [Google Scholar]
- 10.Anuurad E, Tracy RP, Pearson TA, Beckett L, Berglund L. Comparison of C-reactive protein and metabolic syndrome as cardiovascular risk factors in African-Americans and European-Americans. Am J Cardiol. 2009;103:523–527. doi: 10.1016/j.amjcard.2008.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Philbin EF, Weil HF, Francis CA, Marx HJ, Jenkins PL, Pearson TA, Reed RG. Race-related differences among patients with left ventricular dysfunction: observations from a biracial angiographic cohort. Harlem-Bassett LP(A) Investigators. J Card Fail. 2000;6:187–193. doi: 10.1054/jcaf.2000.9677. [DOI] [PubMed] [Google Scholar]
- 12.McGowan MW, Artiss JD, Strandbergh DR, Zak B. A peroxidase-coupled method for the colorimetric determination of serum triglycerides. Clin Chem. 1983;29:538–542. [PubMed] [Google Scholar]
- 13.Allain CC, Poon LS, Chan CS, Richmond W, Fu PC. Enzymatic determination of total serum cholesterol. Clin Chem. 1974;20:470–475. [PubMed] [Google Scholar]
- 14.Warnick GR, Benderson J, Albers JJ. Dextran sulfate-Mg2+ precipitation procedure for quantitation of high-density-lipoprotein cholesterol. Clin Chem. 1982;28:1379–1388. [PubMed] [Google Scholar]
- 15.Maciejko JJ, Levinson SS, Markyvech L, Smith MP, Blevins RD. New assay of apolipoproteins A-I and B by rate nephelometry evaluated. Clin Chem. 1987;33:2065–2069. [PubMed] [Google Scholar]
- 16.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC, Jr, Spertus JA, Costa F. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 17.Miller M, Mead LA, Kwiterovich PO, Jr, Pearson TA. Dyslipidemias with desirable plasma total cholesterol levels and angiographically demonstrated coronary artery disease. Am J Cardiol. 1990;65:1–5. doi: 10.1016/0002-9149(90)90017-u. [DOI] [PubMed] [Google Scholar]
- 18.Wallenfeldt K, Bokemark L, Wikstrand J, Hulthe J, Fagerberg B. Apolipoprotein B/apolipoprotein A-I in relation to the metabolic syndrome and change in carotid artery intima-media thickness during 3 years in middle-aged men. Stroke. 2004;35:2248–2252. doi: 10.1161/01.STR.0000140629.65145.3c. [DOI] [PubMed] [Google Scholar]
- 19.Lind L, Vessby B, Sundstrom J. The apolipoprotein B/AI ratio and the metabolic syndrome independently predict risk for myocardial infarction in middle-aged men. Arterioscler Thromb Vasc Biol. 2006;26:406–410. doi: 10.1161/01.ATV.0000197827.12431.d0. [DOI] [PubMed] [Google Scholar]
- 20.Park YW, Zhu S, Palaniappan L, Heshka S, Carnethon MR, Heymsfield SB. The metabolic syndrome: prevalence and associated risk factor findings in the US population from the Third National Health and Nutrition Examination Survey, 1988–1994. Arch Intern Med. 2003;163:427–436. doi: 10.1001/archinte.163.4.427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Howard BV, Criqui MH, Curb JD, Rodabough R, Safford MM, Santoro N, Wilson AC, Wylie-Rosett J. Risk factor clustering in the insulin resistance syndrome and its relationship to cardiovascular disease in postmenopausal white, black, hispanic, and Asian/Pacific Islander women. Metabolism. 2003;52:362–371. doi: 10.1053/meta.2003.50057. [DOI] [PubMed] [Google Scholar]
- 22.Appel SJ, Floyd NA, Giger JN, Weaver MT, Luo H, Hannah T, Ovalle F. African American women, metabolic syndrome, and national cholesterol education program criteria: a pilot study. Nurs Res. 2005;54:339–346. doi: 10.1097/00006199-200509000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Sierra-Johnson J, Somers VK, Kuniyoshi FH, Garza CA, Isley WL, Gami AS, Lopez-Jimenez F. Comparison of apolipoprotein-B/apolipoprotein-AI in subjects with versus without the metabolic syndrome. Am J Cardiol. 2006;98:1369–1373. doi: 10.1016/j.amjcard.2006.06.029. [DOI] [PubMed] [Google Scholar]
- 24.Ford ES, Giles WH, Dietz WH. Prevalence of the metabolic syndrome among US adults: findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–359. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Association between apoB/apoA-I ratio and number of components in the MS among European-Americans and African-Americans, (P<0.001 for both ethnic groups).