Abstract
Objective
Assess the impact of infusion pump technologies (traditional pump vs smart pump vs smart pump with barcode) on nurses' ability to safely administer intravenous medications.
Design
Experimental study with a repeated measures design.
Setting
High-fidelity simulated inpatient unit.
Results
The nurses remedied 60% of “wrong drug” errors. This rate did not vary as a function of pump type. The nurses remedied “wrong patient” errors more often when using the barcode pump (88%) than when using the traditional pump (46%) or the smart pump (58%) (Cochran Q=14.36; p<0.05). The number of nurses who remedied “wrong dose hard limit” errors was higher when using the smart pump (75%) and the barcode pump (79%) than when using the traditional pump (38%) (Cochran Q=12.13; p<0.003). Conversely, there was no difference in remediation of “wrong dose soft limit” errors across pump types. The nurses' pump programming was less accurate when mathematical conversions were required. Success rates on secondary infusions were low (55.6%) and did not vary as a function of pump type.
Conclusions
These findings indicate that soft (changeable) limits in smart infusion pumps had no significant effect in preventing dosing errors. Provided that smart pumps are programmed with hard (unchangeable) limits, they can prevent dosing errors, thereby increasing patient safety. Until barcode pumps are integrated with other systems within the medication administration process, their role in enhancing patient safety will be limited. Further improvements to pump technologies are needed to mitigate risks associated with intravenous infusions, particularly secondary infusions.
Keywords: Patient safety, medical error, infusion pumps, medication safety
Medication errors are the most significant cause of medical injuries, representing 19.4% of all adverse events.1 Intravenous (IV) infusions are frequent contributors to medication errors.2–4 General infusion pumps were designed to improve accuracy of IV infusions by allowing nurses to programme an hourly rate and volume. However, most adverse drug events (ADEs) associated with IV infusion devices result from nurses manually inputting incorrect settings into the pump.5–7 Common errors include unit errors, multiple-of-ten errors, miscalculations and push-button mistakes.8 Fatal errors have occurred as a result of decimal entry errors (eg, programming morphine at 90 mg/h instead of 9.0 mg/h9). Thus, although infusion pumps have revolutionised the way nurses deliver intravenous therapy, they have also led to ADEs.9
To address the high incidence of infusion errors, manufacturers have developed pumps that have dose error reduction systems (DERS), which include hospital-defined drug libraries with dosing limits and clinical advisories (ie, smart pumps). While traditional general-purpose infusion pumps have a wide range of acceptable programming parameters, smart pumps are designed with drug-specific safety software to help nurses remedy programming errors. Smart pumps provide either a “soft” limit warning (allows nurse to override the limit and continue infusing) or “hard” limit warning (requires nurse to reprogramme the pump within acceptable parameters). Although smart pumps contain safeguards against dosing errors, they do not prevent errors related to the remaining rights (ie, right drug, patient, route, time). Smart pumps with bar code readers (ie, barcode pumps) were designed to help prevent these remaining errors.
Researchers have explored the benefits of using smart pumps compared to traditional pumps. However, outcomes have been mixed. Although some studies2 8 12 13 found that smart pumps reduce errors compared to traditional pumps, others14 15 showed that smart pumps do not reduce the frequency of programming errors and can even introduce new errors. This past research, however, has important limitations. Several prospective studies14 16 17 assessed the potential impact of smart pumps on medication errors. These studies, however, did not explicitly evaluate whether error identification was due to smart pumps or whether errors may have been detected with traditional pumps, thus making it difficult to determine the value of smart pumps. Other researchers18–20 derived data from hospital incident reports to evaluate IV pump errors. These results, however, are not adequately quantifiable because of underreporting.
To our knowledge, there has been no study that has empirically tested the comparative effects of pump technology on safe medication administration. We, therefore, conducted an experimental study to directly compare pump type (ie, traditional vs smart vs barcode) and type of infusion task (with some planted errors) to investigate the impact of different infusion pumps on nurses' ability to safely deliver IV medications.
Methods
Participants
Nurses were recruited from the University Health Network, Toronto, Ontario, Canada. Participants signed up using sheets located in clinical care areas and were remunerated for their participation. Table 1 describes the nurses' characteristics.
Table 1.
Participant characteristics
| Approximate size of eligible population from institution: 3000 | |
| Total no. nurse participants: 24 | |
| Sexes: 4 men and 20 women | |
| Characteristic | Frequency (n=24) |
| Age range | |
| 18–35 | 15 |
| 36–45 | 2 |
| 46–60 | 7 |
| Clinical care area | |
| Cardiac intensive care unit | 4 |
| Cardiovascular intensive care unit | 4 |
| Emergency | 3 |
| General surgery | 4 |
| General internal medicine | 2 |
| Post-anaesthesia care unit | 4 |
| Transplant unit | 3 |
| Role in hospital | |
| Full-time registered nurse | 22 |
| Part-time registered nurse | 1 |
| Casual registered nurse | 1 |
| Years of nursing experience | |
| 1–4 years | 12 |
| 5–15 years | 4 |
| >15 years | 8 |
| Current frequency of traditional infusion pump use* | |
| <once a day | 2 |
| 1–2 times a day | 2 |
| 3–5 times a day | 6 |
| >5 times a day | 14 |
No nurses had previous experience with smart infusion pumps including those used in this study.
Design
Participants delivered infusions with each of three pump types under seven task conditions, some of which contained planted errors. Thus, the design was a 3 (pump type)×7 (infusion task) repeated measures design. Four tasks required intermittent infusions and three required continuous infusions. The order of task conditions and pump types was counterbalanced to avoid carry-over effects.
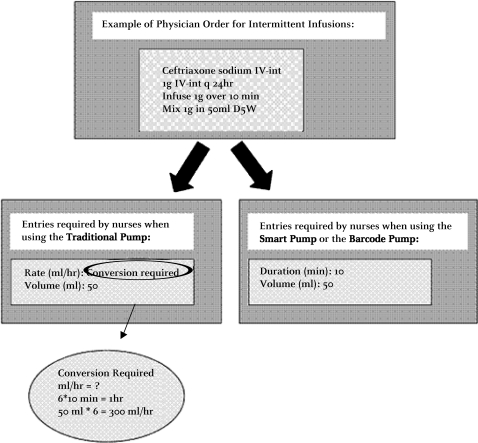
Another variable in this study was whether the nurses had to perform conversion calculations to programme the pumps from information provided in the order. Physician orders were presented in the exact manner the hospital presented orders at the time of the study. For continuous infusions, no conversions were required because the information provided on the order was consistent with the information required to programme the three pumps. For intermittent infusions, however, conversions were required when programming the traditional pump because the information provided on the order was not in accord with the parameters required by the pump (see figure 1 for an example).
Figure 1.
Example of programming an intermittent infusion.
Location and apparatus
Laboratory
The experiment was conducted in a laboratory that allowed high-fidelity simulation of an inpatient unit, including patient beds, furniture, Computerised Physician Order Entry (CPOE) system, IV infusion equipment, and paperwork. This laboratory had observational rooms with one-way glass, and each session was video and audio recorded. Mannequins were used instead of patients. Physician orders were presented on a CPOE system to reflect how nurses in this study currently view orders.
Pumps
Three pumps were selected from two different manufacturers. The traditional pump was from one manufacturer and the smart pump and barcode pump were both from another. The traditional pump was the device nurses currently use, and the smart pump and barcode pump consisted of devices that nurses had no previous experience using.
With the barcode pump, we replicated an environment where the pump scanner could be used to scan the barcode on the patient armband, nurse badge, and medication IV label. The barcode pump could detect if the infusion was being administered to the right patient. In a fully integrated system, the barcode pump server would communicate with the CPOE system and/or the pharmacy information system and consequently, would ensure compliance with other rights. Given that this fully integrated approach is rare, we opted to implement the barcode pump in the form that most hospitals can currently accommodate.
Tasks
Tasks and associated medication orders and drug labels were designed with the help of hospital pharmacists and nurses to ensure validity and nurse familiarity with the tasks. Table 2 describes the tasks.
Table 2.
Task descriptions
| Task name | Description |
| Wrong drug | Label on the IV drug bag did not match the drug prescribed on the physician order. |
| Wrong patient | Patient identification armband on the mannequin did not correspond to the patient information (name, date of birth, and medication registration number) on the physician order. |
| Wrong dose hard limit | Dose provided on the physician order was outside of the allowable hard limit specified in the hospital's IV formulary; thus, the dose was clinically inappropriate. |
| Wrong dose soft limit | Dose provided on the physician order was outside of the allowable soft limit specified in the hospital's IV formulary; thus the dose was clinically inappropriate. |
| Drug not in library | Drug prescribed on the physician's order was not contained in the smart pump and bar code pump drug library. |
| Secondary infusion task (maintenance fluid and therapeutic drug) | Nurse participant was required to programme both a maintenance infusion and a secondary (ie, “piggyback”) infusion. Although no errors were planted in this condition, we assessed the prevalence and nature of errors associated with secondary intravenous infusions. |
Procedure
Each participant was provided with a 15-min training session on a given pump. The training covered the programming tasks required in the experiment and replicated typical vendor instruction. There were three patient mannequins in separate beds. Participants were briefed by a confederate nurse (ie, actor playing the role of a nurse) on the patients' medical history, given physician orders for IV infusions and asked to programme the pumps accordingly. The confederate nurse remained in the room, and participants were asked to communicate with her if they became confused. When prompted with a question, the confederate nurse asked the participant what they would do intuitively. If the participant remained confused, the confederate nurse provided up to three hints, after which she guided the participant through task completion. Once the participant completed all tasks, he or she received training on another pump and the procedure repeated itself until all pumps had been evaluated. Behind a one-way mirror, test facilitators recorded the number of remedied errors, pump programming accuracy and other observations.
Results
Each participant completed 21 infusions. Cochran's Q test was used to assess (a) error resolution, (b) pump programming accuracy and (c) success rate of secondary infusions, all as a function of pump type. Cochran Q tests were followed by pairwise comparisons (using Bonferroni correction) between different combinations of pump types using the McNemar χ2 test.
Error resolution
Wrong drug
Out of 72 infusions that contained planted drug errors (ie, three errors per participant), the participants remedied errors on 43 (60%) entries. Pump type did not significantly impact the ability to remedy “wrong drug” errors (p>0.1). Thus, none of these pumps helped the nurses remedy wrong drug errors.
Wrong patient
There was a significant difference in the resolution of patient ID errors across pumps [Cochran Q=14.36; df=2; p<0.05]. The number of nurses (out of 24) who remedied patient identification errors was significantly higher with the barcode pump (21 (88%)) than with the traditional pump (11 (46%)) or the smart pump (14 (58%)). The difference between the traditional pump and the smart pump, however, was not significant. Thus, the automatic patient identification verification on the barcode pump significantly increased the nurses' resolution of “wrong patient” errors.
Wrong dose hard limit
There was a significant difference in the number of wrong dose hard limit errors remedied across pumps (Cochran Q=12.13; df=2; p<0.003]. The number of nurses who remedied critical overdose errors was significantly higher with the smart pump (18 (75%)) and the barcode pump (19 (79%)) than with the traditional pump (9 (38%)). Thus, results suggest that when faced with hard limit alerts, nurses typically remedy the error. Participants who failed to remedy the error with the smart pump and the barcode pump opted out of the dose-checking technology after exceeding the hard limit and used the pump in its standard rate-based mode (ie, no-safeguard mode).
Wrong dose soft limit
There was no significant difference in the nurses' ability to remedy soft limit overdose errors across pumps (error remedied by 12 (50%) participants with the traditional pump vs 15 (63%) participants with the smart pump vs 18 (75%) participants with the barcode pump; p>0.1). Although the smart pump and barcode pump provide out-of-limit alerts, many nurses elected to override the alert. Thus, the results indicate that when provided with the flexibility to override limits, nurses often do so, even when clinically inappropriate.
Pump programming accuracy
-
Continuous Infusions (no conversion required across all pumps):
For tasks requiring continuous infusions, there was no difference in the number of accurate entries across pump types (p>0.1 for all tasks). Altogether, 216 infusions were performed, and participants were accurate on 203 (94%) entries. Thus, when the parameters included on the orders matched those required from the pump, participants' entries were overall accurate regardless of pump type. However, even a 94% accuracy rate might be considered inadequate.
-
Intermittent Infusions (conversion required for the traditional pump vs no conversion required for the smart pump and barcode pump):
For tasks requiring intermittent infusions, participants' entries were significantly more accurate with the smart pump and the barcode pump than with the traditional pump (p<0.01 for all tasks). Altogether, 72 infusions were performed with each pump. Participants were accurate on 42 (58%) infusions performed using the traditional pump, 67 (93%) using the smart pump, and 65 (90%) using the barcode pump. The magnitude of entry errors varied between 1.2 to 6 times higher than the correct parameter. Thus, the mismatch between physician order and the traditional pump menu forced users to perform conversions, resulting in incorrect entries. All errors were over-infusions; some appeared to be conversion errors while others appeared to be related to clinicians' reliance on their previous experience.
Secondary infusion errors
There was no significant difference in the nurses' ability to successfully programme secondary infusions across pump types (p>0.1). Altogether, 24 infusions were performed with each pump. Participants successfully programmed 12 (50%) secondary infusions with the traditional pump, 16 (67%) with the smart pump and 12 (50%) with the barcode pump. Thus, secondary infusion errors were high across all pumps. More details are provided in table 3.
Table 3.
Frequency, percentage and potential consequences of secondary infusion errors
| Error type | Frequency (n=32) | Percentage | Potential consequences |
| Bag mis-alignment (eg, positioning the therapeutic drug bag at or below the level of the maintenance fluid bag) | 12 | 37% | Mixing and concurrently delivering the therapeutic and maintenance fluids |
| Programming errors (eg, conversion calculation errors) | 9 | 28.13% | Delivering the maintenance fluid and/or the therapeutic drug at an incorrect rate |
| Confusion in the programming sequence (eg, programming the therapeutic drug at the rate of the maintenance fluid) | 6 | 18.75% | Infusing incorrect infusion rates of the therapeutic drug and/or maintenance fluid |
| Forgetting to open the clamp on the therapeutic tubing | 3 | 9.38% | Accidental administration of the maintenance fluid when intending to initiate the therapeutic drug infusion, and the maintenance fluid being infused at the rate of the therapeutic drug |
| Tubing arrangement errors (eg, connecting the infusion line from the therapeutic drug bag into the wrong port on the primary infusion line) | 2 | 6.25% | Free-flowing therapeutic drug into the patient |
Discussion
This study adds to the literature by explicitly comparing and quantifying the effects of pump types on the nurses' ability to safely administer IV medication and by identifying errors that are not addressed by current pumps. Certain errors that were potentially preventable by smart pumps or barcode pumps (eg, soft limit overdose errors) were due to deviations from policies.
Our findings are consistent with other studies,8 10 11 which showed that nurses often override soft limit alerts when clinically inappropriate. Furthermore, our findings suggest that when faced with hard limit warnings, nurses respond in a safe manner. However, many hospitals do not implement the hard limit feature. Other errors (eg, secondary infusion errors), were not preventable by smart or barcode technologies.
Our results are also consistent with other findings,21 indicating that errors related to setup and administration of secondary infusions have lead to adverse events. Furthermore, researchers18 22 23 have reported that confusion between dosing units and/or concentrations when using smart pumps lead to overdoses. Our findings concur and provide further evidence that variation in IV medication practices is associated with increased risks.
Finally, our results show that some errors (eg, undetected wrong drug errors) were due to a lack of integration between the pump and other components (eg, CPOE) of the medication delivery system. Thus, effective use of pump technology is dependent not only on the design of the pump itself but also on the way it is implemented. Institutions must promote a culture of safety that encourages nurses to think critically, evaluate pump warnings and limit overrides to circumstances that have been carefully assessed.
It has been estimated that approximately 44.0% of US hospitals use smart pumps.24 To optimise integration of smart pumps, healthcare institutions must dedicate a significant operational budget to cover costs including maintenance and licensing, drug library updating, continuous quality improvement analysis/reporting and costs related to training and maintaining nurse proficiency. Currently, hospitals may be investing three to four times more money into smart pumps compared to traditional pumps without realising noteworthy safety benefits.
While pumps with barcoding hold a lot of promise, smart pump and IT vendors have not yet fully established an integrated approach that ensures connectivity between medication management technologies. Our findings show that until hospitals can achieve full connectivity between technologies, barcode pumps will help prevent certain errors that earlier pump versions could not address (eg, wrong patient errors), but will continue to permit others (eg, wrong drug).
There are limitations to our study. The small sample size and the simulation of a real inpatient unit limit the generalisability of the results. However, significant differences were detected nonetheless. The large number of planted errors might have influenced participants to behave differently (eg, be more alert to errors) than they would under clinical circumstances where these errors occur less frequently. Participants had no previous experience with smart pumps. Therefore, results are representative of nurses who receive vendor training but have little experience using the technology. Although our results can be generalised to a novice smart pump user population, they are consistent with findings from studies where nurses had experience with smart pumps. For example, our results are coincident with researchers who found that nurses often override smart pump safety limits.8 10 11 It is possible that nurses in this study overrode limits to please the researcher and carry out instructions as indicated. This is unlikely, however, given that participants were explicitly asked to underscore problematic drug orders. Researchers have found that safety overrides are frequently due to alert fatigue, a mental state resulting from many alerts consuming time and mental energy.25–29 Other researchers attribute overrides to alerts being lengthy, difficult to interpret and lacking clarity as to clinical consequences.29 30 A deeper understanding of how to design effective alerts could be developed by assessing the following: (a) how cognitive processes contribute to clinicians' response to alerts; (b) clinicians' reasons for overriding alerts (eg, ignore, misinterpret, incorrect selection); (c) how to incorporate effective handling of safety alerts without interrupting workflow and (d) how to increase clinician trust and responsiveness to smart pump alerts. Future work should also focus on achieving safer systems by integrating components at various stages (eg, ordering, prescribing, administering) of the medication delivery process.
Acknowledgments
The authors gratefully acknowledge the Ministry of Health and Long-Term Care of Ontario (MoHLTC), particularly Dr Leslie Levin and Dr Birthe Jorgensen of the Medical Advisory Secretariat (MAS) for supporting this work. We also acknowledge the involvement of the hospital staff at the University Health Network (UHN). The authors thank Ms. Eliza To for her help with the pharmacy requirements of this project and for her valuable insights. We would also like to thank Jennifer Jeon, Mark Fan and Sarah Rothwell for their help in the execution of the experiment.
Footnotes
Funding: This research was funded by the Ministry of Health and Long-Term Care (MoHLTC grant no. 06431, Toronto, Ontario, Canada) and conducted at the request of the Ontario Health Technology Assessment Committee (OHTAC, Toronto, Ontario, Canada). The opinions in the present paper are those of the authors and do not necessarily reflect the sponsor's official position.
Competing interests: None.
Ethics approval: Research Ethics Board (REB) approval was obtained. REB reference number: 08-0161-AE.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Leape LL, Brennan TA, Laird NM, et al. The nature of adverse events in hospitalized patients: results from the Harvard Medical Practice Study II. N Engl J Med 1991;324:377–84 [DOI] [PubMed] [Google Scholar]
- 2.Kinnealey E, Fishman G, Sims N, et al. Infusion pumps with “drug libraries” at the point of care—a common solution for safer drug delivery 2003. http://www.npsf.org/download/Kinnealy.pdf (accessed 22 Dec 2008).
- 3.Ross LM, Wallace J, Paton JY. Medication errors in a paediatric teaching hospital in the UK: five years operational experience. Arch Dis Child 2001;83:492–7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kaushal R, Bates DW, Landrigan C, et al. Medication errors and adverse drug events in pediatric inpatients. JAMA 2001;285:2114–20 [DOI] [PubMed] [Google Scholar]
- 5.Tourville J. Automation and error reduction: how technology is helping Children's Medical Center of Dallas reach zero-error tolerance. US Pharmacist 2003;28:80–6 [Google Scholar]
- 6.Eskew JA, Jacobi J, Buss WE, et al. Using innovative technologies to set new safety standards for the infusion of intravenous medications. Hospital Pharmacy 2002;37:1179–89 [Google Scholar]
- 7.Adachi W, Lodolce AE. Failure mode and effects analysis to improve the process of intravenous drug administration. Am J Health Syst Pharm 2005;62:917–20 [DOI] [PubMed] [Google Scholar]
- 8.Murdoch LJ, Cameron V. Smart infusion technology: a minimum safety standard for intensive care? Br J Nurs 2008;17:630–6 [DOI] [PubMed] [Google Scholar]
- 9.Reeves J. “Smart Pump” technology reduces errors. Anesthesia Patient Safety Foundation 2003;18:1–16 [Google Scholar]
- 10.Institute for Safe Medical Practices Smart pumps are not smart on their own. Horsham (PA): ISMP, 2007. http://www.ismp.org/newsletters/acutecare/archives/Apr07.asp#19 (accessed 22 Dec 2008). [Google Scholar]
- 11.Pratt N. Intravenous medication safety wireless data system. In: Schneider PJ, ed. Measuring medication safety with smart IV systems. San Diego, (CA): Health Leaders, 2004;vol. 7(12 Suppl):39–44 [Google Scholar]
- 12.Larsen GY, Parker HB, Cash J, et al. Standard drug concentrations and smart-pump technology reduce continuous-medication-infusion errors in pediatric patients. Pediatrics 2005;116:e21–5 [DOI] [PubMed] [Google Scholar]
- 13.Maddox RR. ICU sedation—an analysis of intravenous dose limit overrides. In: Schneider PJ, ed. Measuring medication safety with smart iv systems: proceedings from the fourth conference. San Diego (CA): Cardinal Health Centre for Medication Safety and Clinical Improvement, 2004:37–40 [Google Scholar]
- 14.Husch M, Sullivan C, Rooney D, et al. Insights from the sharp end of intravenous medication errors: implications for infusion pump technology. Qual Saf Health Care 2005;14:80–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rothschild JM, Keohane CA, Cook EF, et al. A controlled trial of smart infusion pumps to improve medication safety in critically ill patients. Crit Care Med 2005;33:533–40 [DOI] [PubMed] [Google Scholar]
- 16.Malashock CM, Shull S, Gould A. Effect of smart infusion pumps on medication errors related to infusion device programming. Hospital Pharmacy 2004;39:460–9 [Google Scholar]
- 17.Wilson K, Sullivan M. Preventing medication errors with smart infusion technology. Am J Health Syst Pharm 2004;61:177–83 [DOI] [PubMed] [Google Scholar]
- 18.Bates DW, Vanderveen T, Seger D, et al. Variability in intravenous medication practices: implications for medication safety. Jt Comm J Qual Patient Saf 2005;31:203–10 [DOI] [PubMed] [Google Scholar]
- 19.O'Neil AC, Peterson LA, Cook EF, et al. Physician reporting compared with medical record review to identify adverse medical events. Ann Intern Med 1993;119:370–6 [DOI] [PubMed] [Google Scholar]
- 20.Stanhope N, Crowley-Murphy M, Vincent C, et al. An evaluation of adverse incident reporting. J Eval Clin Pract 1999;5:5–12 [DOI] [PubMed] [Google Scholar]
- 21.Nunnally ME, Bitan Y. Time to get off this pig's back? The human factors aspects of the mismatch between device and real-world knowledge in the health care environment. J Patient Saf 2006;2:124–31 [Google Scholar]
- 22.Institute for Safe Medications Canada High alert drugs and infusion pumps: extra precautions required. ISMP Canada Safety Journal 2004;4:1–2 [Google Scholar]
- 23.Institute for Safe Medication Practices “Smart” infusion pumps join CPOE and bar coding as important ways to prevent medication errors 2005. http://www.ismp.org/msaarticles/smartprint.htm (accessed 5 Feb 2005).
- 24.Pedersen CA, Gumpper KF. ASHP national survey on informatics: assessment of the adoption and use of pharmacy informatics in U.S. hospitals 2007. Am J Health Syst Pharm 2008;65:2244–64 [DOI] [PubMed] [Google Scholar]
- 25.Peterson JF, Bates DW. Preventable medication errors: identifying and eliminating serious drug interactions. J Am Pharm Assoc 2001;41:159–60 [DOI] [PubMed] [Google Scholar]
- 26.Glassman PA, Simon B, Belperio P, et al. Improving recognition of drug interactions. Benefits and barriers to using automated drug alerts. Med Care 2002;40:1161–71 [DOI] [PubMed] [Google Scholar]
- 27.Taylor L, Tamblyn R. Reasons for physician non-adherence to electronic drug alerts. Medinfo 2004;11:1101–5 [PubMed] [Google Scholar]
- 28.Magnus D, Rodgers S, Avery AJ. GPs' views on computerized drug interaction alerts: questionnaire survey. J Clin Pharm Ther 2002;27:377–82 [DOI] [PubMed] [Google Scholar]
- 29.Feldstein A, Simon SR, Schneider J, et al. How to design computerized alerts to ensure safe prescribing practices. Jt Comm J Qual Saf 2004;30:602–13 [DOI] [PubMed] [Google Scholar]
- 30.Ashworth M. GPs' views on computerized drug interaction alerts. J Clin Pharm Ther 2002;27:311–2 [DOI] [PubMed] [Google Scholar]