Abstract
We screened 194 Mycobacterium tuberculosis strains isolated from tuberculosis (TB) patients in Delhi and neighboring regions in India to identify the prevalence of extensive drug resistance (XDR) in clinical isolates. Among these, 104 isolates were found to be multidrug resistant (MDR), and 6 were identified as XDR isolates, which was later confirmed by antimicrobial susceptibility testing against the respective drug screening panel. Genotyping was carried out by amplifying and sequencing the following genes: rpoB (rifampin), katG (isoniazid), gyrA (fluoroquinolones), and rrs (amikacin, kanamycin, and capreomycin). Our analyses indicated that mutations at the hot spots of these genes were positively correlated with drug resistance in clinical isolates. The key mutation observed for rpoB was in the codon for amino acid position 531 (S531L), and other mutations were seen in the hot spot, including those encoding Q510P, L511H, D516V, and H526Y mutations. We identified S315T and R463L substitutions encoded in the katG locus. An S95T substitution encoded in the gyrA locus was the most common mutation observed in fluoroquinolone-resistant isolates. In addition, we saw D94G and D94N mutations encoded in the QRDR region. The 16S rRNA (rrs) gene encoded mainly the A1401G mutation and an additional mutation, G1484T, resulting in ribosomal modifications. Taken together, the data in this report clearly establish the presence of phenotypically distinct XDR strains in India by molecular profiling and further identify specific mutational hot spots within key genes of XDR-TB strains.
In recent years, the control of tuberculosis (TB) has become a global challenge due to the emergence of multidrug-resistant tuberculosis (MDR-TB) and extensively drug-resistant tuberculosis (XDR-TB). With 9.2 million new cases and 1.7 million deaths in 2006, TB remains one of the major life-threatening diseases worldwide (22). XDR-TB isolates are resistant to isoniazid and rifampin, to any fluoroquinolone (FQ), and to at least one of the three injectable second-line drugs (amikacin, kanamycin, and capreomycin) (6). As of June 2008, XDR-TB strains have been found in 49 countries, including the United States (6, 22). Furthermore, a recent report points to an alarming increase in the number of tuberculosis patients in the South Asian subcontinent, with India being singled out as having the greatest burden of XDR-TB, with a poor prognosis and high mortality among HIV-infected individuals (4). The risk of XDR-TB spread across country borders has heightened global concern over a potentially untreatable epidemic that may jeopardize recent advances made in global TB control.
The prevalence of XDR-TB in India was reported in 2007, but no further efforts have been made to identify its genotypes or geographical spread (9). The present study was undertaken to characterize mutations prevalent in clinical isolates from India with respect to various drug target loci. We examined the drug target genes for rifampin (rpoB), isoniazid (katG), fluoroquinolones (gyrA), and aminoglycosides (rrs), which are commonly prescribed for the treatment of tuberculosis in India. The loci studied were rpoB (RNA polymerase B subunit), katG (catalase-peroxidase), rrs (16S rRNA), and gyrA (DNA gyrase A). Here we report, for the first time, the molecular characterization of XDR-TB isolates from India. This study confirms the presence of XDR-TB in India and simultaneously raises an alarm about its prevalence among TB patients, as many of them may initially have MDR-TB that slowly progresses and mutates to XDR-TB. Furthermore, the fact that some of these patients have HIV infection or the possibility of later coinfection with HIV has the potential to make this global HIV-TB epidemic untreatable with current therapies.
MATERIALS AND METHODS
Mycobacterium tuberculosis clinical isolates.
Mycobacterium tuberculosis isolates were collected from patients reporting to the Super Religare Laboratories (SRL) Reference Center in Gurgaon, India, primarily from New Delhi and its neighboring regions. Most of these patients were referral cases and had been through various degrees of antitubercular drug therapy. Sputum and extrapulmonary specimens were collected from patients reporting with pulmonary or extrapulmonary tuberculosis to the SRL Reference Center. The specimens were processed by standard methods (N-acetyl-l-cysteine-NaOH), followed by culturing in a Bactec MGIT 960 nonradiometric automatic isolation system (BD). The isolates were characterized as belonging to the M. tuberculosis complex by use of p-nitrobenzoic acid (PNBA) in the Bactec MGIT 960 system (21).
XDR characterization by phenotypic studies.
A total of 194 clinical M. tuberculosis isolates were used for antimicrobial testing with first- and second-line drugs in the MGIT 960 system per the manufacturer's protocol to identify the XDR-TB strains. The drug susceptibility profiles were tested at SRL, Gurgaon, India. The critical concentrations (μg/ml) of antitubercular drugs used in the MGIT 960 system were as follows: rifampin, 1.0; isoniazid, 0.1; ofloxacin, 2.0; levofloxacin, 2.0; moxifloxacin, 2.0; kanamycin, 4.0; capreomycin, 2.5; amikacin, 1.0; streptomycin, 1.0; ethambutol, 5.0; and pyrazinamide, 100.0. The MICs for the XDR strains were determined for phenotypic confirmation per the method of Sood et al. (16), and dilution of the compounds was performed per Clinical and Laboratory Standards Institute (CLSI; formerly NCCLS) guidelines (12).
Genomic DNA isolation, PCR, and DNA sequencing.
The isolates were cultured on Lowenstein-Jensen slants. The colonies were scraped from the slants and resuspended in 500 μl of Middlebrook 7H9 broth. Genomic DNAs were isolated by using a Qiagen DNeasy blood and tissue kit. The primers used in this study and their nucleotide positions in the corresponding genes are listed in Table 1. PCR amplification was done by using standardized protocols. The samples were resolved in a 1% agarose gel, and the specific bands were visualized in a Gel Doc system using Quantity One software. The PCR products were purified using a Qiagen PCR purification kit according to the manufacturer's instructions. The purified DNAs were eluted in sterile double-distilled water and used for the sequencing studies. Sequencing of the amplicons was carried out at Macrogen (outsourced to Biolinkk). The sequences generated with the program were compared to the respective wild-type sequences by using clone manager software.
TABLE 1.
Primers used for amplification of different loci of target genes for XDR-TB strain characterization
| Gene | Primer direction | Sequence (5′-3′) | Position (nt) | Amplicon size (bp) |
|---|---|---|---|---|
| katG1 | Forward | GTGCCCGAGCAACACCCACCCATTAC | 1-26 | 808 |
| Reverse | GGCGCCATGGGTCTTACCGAAAG | 812-834 | ||
| katG2 | Forward | CGGCGGTCACACTTTCGGTAAG | 801-822 | 759 |
| Reverse | CGGCGGTCACACTTTCGGTAAG | 1540-1560 | ||
| rpoB | Forward | CACCAGCCAGCTGAGCCAATTC | 1296-1317 | 442 |
| Reverse | CCATGTAGTCCACCTCAGACGAG | 1716-1738 | ||
| gyrA | Forward | GATGCAGCGCAGCTACATCGAC | 69-90 | 325 |
| Reverse | CTTCGGTGTACCTCATCGCCG | 374-394 | ||
| rrs | Forward | GAGATAGGCGTTCCCTTGTGGC | 995-1071 | 527 |
| Reverse | AAGGAGGTGATCCAGCCGCAC | 1502-1522 |
RESULTS
A total of 194 clinical isolates were screened for the identification of XDR in M. tuberculosis isolates by the Bactec MGIT 960 modified proportion method per the manufacturer's protocol. These isolates were from TB patients in Delhi and neighboring regions in India. Here we report the presence of XDR in clinical isolates from this region. Among the 194 M. tuberculosis isolates tested for susceptibility with the MGIT 960 system, 104 were found to be multidrug-resistant strains, and 6 were characterized as XDR-TB isolates and then cross-checked with the MICs of the respective drug screening panel of antitubercular drugs (Tables 2 and 3). These 6 XDR-TB clinical isolates were critically examined with the Bactec MGIT 960 system as well as by their MICs and were confirmed to be XDR-TB strains. The MICs of rifampin against the XDR-TB strains were >16 μg/ml, and the MICs of isoniazid against these isolates were in the range of 1 to >16 μg/ml. The MICs of fluoroquinolones against these XDR clinical isolates were in the range of 8 to >16 μg/ml, and the MICs of second-line drugs (kanamycin, amikacin, and capreomycin) were in the range of 4 to >16 μg/ml (Table 3). These MIC ranges indicate that these clinical isolates are resistant to first-line drugs (rifampin and isoniazid), to fluoroquinolones (ofloxacin), and to second-line injectable drugs (kanamycin, amikacin, and capreomycin), and therefore they are categorized as XDR-TB strains. These XDR isolates represent primarily those with acquired resistance, as either the patients had at some time been given antitubercular drug therapy or the XDR-TB isolates spread from one patient to another.
TABLE 2.
XDR-TB clinical isolate susceptibilities to antimycobacterial drugs
| Isolate | Origin | Source specimen | Age of patient (yr) | Gender of patient | Susceptibility to druga |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| INH | RIF | OFLOX | LEVO | MOXI | KANA | CAPREO | AMIK | STREPTO | ETHAMB | PZA | |||||
| 625 | Agra | Sputum | 32 | F | R | R | R | TN | R | R | R | TN | TN | TN | R |
| 761 | New Delhi | Pus | 22 | M | R | R | R | R | R | R | R | R | S | S | S |
| 2403 | Moradabad | Sputum | 45 | M | R | R | R | R | R | R | R | R | R | R | R |
| 2301 | Agra | Sputum | 34 | M | R | R | R | R | R | R | R | R | R | R | R |
| 2911 | New Delhi | Sputum | 16 | F | R | R | R | R | R | R | R | R | R | R | S |
| 2474 | New Delhi | Sputum | 48 | M | R | R | R | TN | TN | S | S | R | R | R | R |
Resistance (R) or sensitivity (S) of strains to the corresponding anti-TB drugs. TN, test not requested and therefore not performed. INH, isoniazid; RIF, rifampin; OFLOX, ofloxacin; LEVO, levofloxacin; MOXI, moxifloxacin; CAPREO, capreomycin; AMIK, amikacin; STREPTO, streptomycin; ETHAMB, ethambutol; PZA, pyrazinimide.
TABLE 3.
MICs of antitubercular drugs against XDR-TB clinical isolatesa
| Drug | MIC (μg/ml) for strain |
|||||
|---|---|---|---|---|---|---|
| 2911 | 625 | 2474 | 761 | 2301 | H37Rv | |
| Rifampin | 16 | >16 | >16 | >16 | >16 | 0.25 |
| Isoniazid | 4 | >16 | 1 | 4 | 0.5 | 0.25 |
| Ethambutol | 4 | 4 | 4 | 8 | 4 | 1 |
| Moxifloxacin | 1 | 1 | 1 | 1 | 2 | 0.125 |
| Ofloxacin | 8 | 16 | 8 | 16 | 8 | 0.5 |
| Amikacin | >16 | >16 | >16 | 16 | >16 | 0.5 |
| Kanamycin | >16 | >16 | >16 | >16 | >16 | 2 |
| Streptomycin | >16 | 16 | >16 | 0.125 | 0.5 | 1 |
| Cycloserine | >16 | 16 | 16 | 16 | 16 | 8 |
| Capreomycin | 16 | 16 | 4 | >16 | 4 | 2 |
| Ethionamide | 4 | 4 | >16 | 1 | 2 | 0.5 |
| Sparfloxacin | >16 | 8 | 16 | 16 | 16 | 0.5 |
Isolate 2403 was not able to grow in synthetic media, so the MICs of all these drugs with this isolate could not be studied.
The 6 phenotypically confirmed XDR-TB isolates were further analyzed for mutations in the hot spot regions of various gene loci. The results are summarized in Table 4. On the basis of the drug susceptibility profile of each isolate, the relevant drug target genes were PCR amplified and sequenced. The corresponding genes were sequenced from all XDR-TB isolates and the standard laboratory reference strain H37Rv (ATCC 27294). Reported sequences of the genes were taken as templates for sequence analysis. No mutations were observed in the rpoB, katG, gyrA, and rrs genes of H37Rv. Sequencing results for H37Rv exactly matched the wild-type sequences of the respective genes.
TABLE 4.
Characterization of XDR-TB isolates through identification of mutations in drug target genes
| Strain | Mutation(s) in drug target gene |
|||
|---|---|---|---|---|
| rpoB (rifampin) | katG (isoniazid) | gyrA (FQ) | rrs (kanamycin, capreomycin, amikacin) | |
| 625 | S531L, G566R, I569L | S315T, R463L | A90V, S95T | A1401G |
| 761 | S531L, Q510P | S315T, R463L | D94N, S95T | G1484T |
| 2301 | S531L | R463L, E217G | D94G, S95T | A1401G |
| 2403 | Q510P, L511V, S531L | S315T, R463L | A90V, S95T | A1401G |
| 2474 | H526Y | D329A, R463L | D94G, S95T | A1401G |
| 2911 | D516V | S315T, R463L | D94G, S95T, R128S, Y129C | A1401G |
| H37Rv | No mutation | No mutation | No mutation | No mutation |
A stretch of 30 amino acids at the center of the amplicon for the rpoB locus was studied. Amino acids 507 to 533 comprised the hot spot region for mutations. In all 6 XDR isolates, we observed mutations in the hot spot region. We identified previously reported mutations as well as certain novel mutations. The mutations observed in the hot spot region were Q510P, L511V, D516V, H526Y, and S531L (Tables 4 and 5). Amino acid 531 seemed to be the most vulnerable to mutation, as most rifampin-resistant isolates had the TCG→TTG mutation. The mutations in the hot spot region correlated well with the MICs of rifampin against XDR strains.
TABLE 5.
XDR-TB isolates with point mutations in the rpoB gene
| XDR strain | Rifampin MIC (μg/ml) | Mutation | Nucleotide change | Amino acid change | Mutation type |
|---|---|---|---|---|---|
| 625 | >16 | S531L | C→T | Ser→Leu | Previously reported |
| 761 | >16 | Q510P | A→C | Gln→Pro | This study |
| S531L | C→T | Ser→Leu | Previously reported | ||
| 2301 | >16 | S531L | C→T | Ser→Leu | Previously reported |
| 2403 | Q510P | A→C | Gln→Pro | This study | |
| L511H | T→A | Leu→His | Previously reported | ||
| S531L | C→T | Ser→Leu | Previously reported | ||
| 2474 | >16 | H526Y | C→T | His→Tyr | Previously reported |
| 2911 | 16 | D516V | A→T | Asp→Val | This study |
In the present study, we looked for mutations in the 5′ region (nucleotides [nt] 1 to 834; referred to as katG1) and the mid-region (nt 801 to 1560; referred to as katG2) of katG, corresponding to amino acid positions 1 to 278 and 267 to 520, respectively (Table 1). The mutations observed in the katG gene are summarized in Table 4. In the 5′ region, the E217G mutation was observed in XDR isolate 2301. The other strains did not show any mutations in this region, but in the mid-region of the katG gene, 3 mutations, S315T, D329A, and R463L, were identified; among these, the 2 key mutations were S315T and R463L. In addition to the R463L mutation, common in Indian MDR-TB isolates, four of six isolates had the S315T mutation. In one of the isolates (XDR 2474), the D329A mutation was also observed.
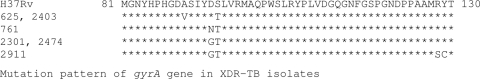
The QRDR region of the gyrA gene was sequenced to identify mutations (Fig. 1 and Table 4). The isolates showed a common mutation corresponding to the amino acid change S95T (Table 4). The second most common mutation, observed in four isolates, was D94G or D94N. Three isolates had an A90V substitution, while one isolate (XDR 2911) had two additional mutations, R128S and Y129C. All six isolates had the common mutation S95T, and 4 isolates had mutations at position 94 as well as position 95. One isolate (XDR 2911) had 4 mutations, S95T, D94G, R128S, and Y129C.
FIG. 1.
Mutation pattern of gyrA gene in XDR-TB isolates.
XDR-TB isolates resistant to amikacin, kanamycin, and streptomycin were tested for mutations in the rrs locus. The results showed two mutations, A1401T and G1484T. The A1401T mutation was a common mutation observed in 5 isolates. In XDR 761, the G1484T mutation was seen. This mutation in the rrs gene is the cause for the emergence of resistance to kanamycin and amikacin.
DISCUSSION
The ever-increasing burden of drug resistance is a serious concern in developing countries, particularly for patients with M. tuberculosis infection. This mycobacterium uses various mechanisms to evade killing by therapeutic drugs, including mutations in genes that code for drug target proteins (3, 10, 11, 13). The objective of the present study was to identify mutations in drug target genes in strains of M. tuberculosis prevalent among the Indian population. The findings of our study showed that many mutations in the rpoB, katG, and gyrA genes are similar to those reported from other parts of the world (13, 18, 19), and these common mutations might have global ramifications. In addition, a few mutations in our report clearly reflect the uniqueness of XDR-TB strains from the Delhi region. The modified proportion method (MGIT 960) as well as the MIC method revealed the existence of XDR strains in the Delhi region. Since no proper phenotypic and genotypic study is available from other parts of India, we cannot rule out the possibility of the existence of similar XDR strains throughout India. Since India remains a hot spot for TB (1), it is important to have a molecular profile for these XDR-TB strains.
We undertook the present study to characterize the mutations prevalent in clinical isolates of M. tuberculosis from India with respect to the drug target genes rpoB, katG, gyrA, and rrs. Most of the mutations were common in reported XDR strains, thus confirming the existence of XDR-TB in India. In addition, our study identified a few novel mutations in the XDR-TB clinical isolates from the Delhi region.
The existence of common mutations in the rpoB gene, at codons 526 and 531, in Indian isolates and those reported previously (5, 15, 18, 20) indicates that these mutations are common for many drug-resistant strains around the globe, with the possibility of further spread. We found mutations in the hot spot region of the rpoB gene, encoding the residues at positions 510, 511, and 516, that correlate with those in previous studies (15, 18). Additional mutations outside the hot spot region were observed in rpoB, encoding the residues at positions 566 and 569. The latter mutations were detected in a significant number of drug-resistant isolates, a fact that needs to be kept in mind while designing diagnostic kits for the detection of XDR-TB. We found a definite correlation between the MIC and the type of mutation for many isolates. As reported by previous investigators (7, 8, 19), mutations at positions 526 and 531 are important in the development of high-level resistance, as isolates with these mutations frequently exhibit high MICs.
We observed that many isolates carried the R463L and S315T substitutions. The R463L mutation correlates with a study by Siddiqi et al. (15), and the S315T mutation corroborates the findings of Sun et al. very well (18). Earlier, Sreevatsan et al. (17) reported that the R463L polymorphism does not contribute to resistance per se but is an important marker for evolutionary genetics. The E217G mutation encoded in the 5′ region of the katG gene was quite uncommon and has not been reported by any other group. The MIC of isoniazid against isolates XDR 2301 and XDR 2474 was 1 μg/ml, and the mutation at position 315 was not observed. In other isolates, the mutation at position 315 was observed, and the MIC was 4 to >16 μg/ml. There appears to be a strong correlation between high-level resistance to isoniazid and mutation at position 315 in the katG gene product.
FQs comprise the secondary line of treatment for drug-resistant tuberculosis. One of the reasons that all of our XDR isolates were resistant to FQ may be due to its overuse in the community. In addition, FQ-resistant strains may be spreading in hospitals as well as in community settings. The most common mutation in FQ-resistant isolates in the present study was the S95T mutation, which seems to have no direct role in the development of drug resistance, as it also occurs in drug-sensitive strains (17). In reports by Siddiqi et al. (14, 15), the majority of ofloxacin-resistant MDR strains showed the S95T mutation, very few isolates showed mutations at positions 90 and 94, and they did not observe any mutation in some of the FQ-resistant isolates. Codons 89, 90, 91, 94, and 95 in the gyrA gene have been shown to be polymorphic (13, 23). Recently, the molecular characterization of XDR isolates in China revealed mutations at position 94 (D94N, D94G, D94A, D94H, and D94Y) and position 90 (A90V) (18). The Indian MDR isolates revealed mutations mainly at position 95 (S95T) (14, 18). The XDR isolates from our study revealed mutations at position 94 as well as position 95, which appear to have characteristic features. We also observed mutations common for the XDR isolates reported in earlier studies (15, 18, 23).
We observed two mutations (A1401G and G1484T) in the rrs locus, and they were associated with resistance to aminoglycosides. Earlier low-level resistance was observed due to mutations associated with the rrs locus, as reported by Bottger in 1994 (2). Another study by Siddiqi et al. did not find any of these mutations in 14 streptomycin-resistant isolates (15).
The emergence of XDR-TB in India is a concern, as it remains one of the major killer diseases (1). Due to inadequate monitoring and a lack of proper treatment regimens, MDR-TB and XDR-TB remain major threats to the Indian population, particularly for individuals on the lower threshold of the socioeconomic ladder. Our study provides additional information about the mutations that are common in XDR isolates from India and other parts of the world (18). To the best of our knowledge, this is the first report on XDR-TB in India with molecular characterization of target genes. Our data will be helpful in designing new molecular biology-based techniques for the diagnosis of XDR-TB. Further molecular characterization of XDR-TB strains throughout India, along with our data, will help in the design and execution of proper therapeutic interventions for patients infected with these strains.
Acknowledgments
We thank Kedar Padmakar Purnapatre for a critical reading of the manuscript.
We acknowledge financial support for research from Ranbaxy Laboratories Limited.
Footnotes
Published ahead of print on 16 August 2010.
REFERENCES
- 1.Balaji, V., P. Daley, A. A. Anand, T. Sudarsanam, J. S. Michael, R. D. Sahni, P. Chordia, I. A. George, et al. 2010. Risk factors for MDR and XDR-TB in a tertiary referral hospital in India. PLoS One 5:9527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bottger, E. C. 1994. Resistance to drug targeting protein synthesis in mycobactera. Trends Microbiol. 2:416-421. [DOI] [PubMed] [Google Scholar]
- 3.Cole, S. T., R. Brosch, J. Parkhill, T. Garnier, C. Churcher, D. Harris, et al. 1998. Deciphering the biology of Mycobacterium tuberculosis from the complete genome sequence. Nature 393:537-544. (Erratum, 396:190.) [DOI] [PubMed] [Google Scholar]
- 4.Gandhi, N. R., A. Moll, A. W. Sturm, R. Pawinski, T. Govender, U. Lalloo, K. Zeller, J. Andrews, and G. Friedland. 2006. Extensively drug-resistant tuberculosis as a cause of death in patients co-infected with tuberculosis and HIV in a rural area of South Africa. Lancet 368:1575-1580. [DOI] [PubMed] [Google Scholar]
- 5.Hasnain, S. E., A. Amin, N. Siddiqi, M. Shamim, N. K. Jain, A. Rattan, V. M. Katoch, and S. K. Sharma. 1998. Molecular genetics of multiple drug resistance (MDR) in Mycobacterium tuberculosis, p. 35-40. In R. L. Singhal and O. P. Sood (ed.), Drug resistance: mechanism and management. Proceedings of the Fourth Annual Ranbaxy Science Foundation Symposium. Ranbaxy Science Foundation, New Delhi, India.
- 6.Jassal, M., and W. R. Bishai. 2009. Extensively drug-resistant tuberculosis. Lancet Infect. Dis. 9:19-30. [DOI] [PubMed] [Google Scholar]
- 7.Kapur, V., L. L. Li, S. Iordanescu, M. C. Hamrick, A. Wanger, B. N. Kreiswirth, and J. M. Musser. 1994. Characterization by automated DNA sequencing of mutations in the gene (rpoB) encoding the RNA polymerase beta subunit in rifampin-resistant Mycobacterium tuberculosis strains from New York City and Texas. J. Clin. Microbiol. 32:1095-1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Miller, L. P., J. T. Crawford, and T. M. Shinnick. 1994. The rpoB gene of Mycobacterium tuberculosis. Antimicrob. Agents Chemother. 38:805-811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mondal, R., and A. Jain. 2007. Extensively drug resistant Mycobacterium tuberculosis, India. Emerg. Infect. Dis. 13:1429-1431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Morris, S., G. Han Bai, P. Suffys, L. P. Gomez, M. Fairchok, and D. Rouse. 1995. Molecular mechanisms of multiple drug resistance in clinical isolates of Mycobacterium tuberculosis. J. Infect. Dis. 171:954-960. [DOI] [PubMed] [Google Scholar]
- 11.Musser, J. M. 1995. Antimicrobial agent resistance in mycobacteria: molecular genetic insights. Clin. Microbiol. Rev. 8:496-514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.NCCLS. 2000. Susceptibility testing of mycobacteria, nocardia, and other aerobic actinomycetes: tentative standard M24-T2, vol. 20, no. 26. NCCLS, Wayne, PA. [PubMed]
- 13.Ramaswamy, S., and J. M. Musser. 1998. Molecular genetic bases of antimicrobial agent resistance in Mycobacterium tuberculosis: 1998 update. Tuber. Lung Dis. 79:3-29. [DOI] [PubMed] [Google Scholar]
- 14.Siddiqi, N., M. Shamim, N. K. Jain, A. Rattan, A. Amin, V. M. Katoch, S. K. Sharma, and S. E. Hasnain. 1998. Molecular genetic analysis of multidrug resistance in Indian isolates of Mycobacterium tuberculosis. Mem. Inst. Oswaldo Cruz 93:589-594. [DOI] [PubMed] [Google Scholar]
- 15.Siddiqi, N., M. Shamim, S. Hussain, R. K. Choudhary, N. Ahmed, Prachee, S. Banerjee, G. R. Savithri, M. Alam, N. Pathak, A. Amin, M. Hanief, V. M. Katoch, S. K. Sharma, and S. E. Hasnain. 2002. Molecular characterization of multidrug-resistant isolates of Mycobacterium tuberculosis from patients in North India. Antimicrob. Agents Chemother. 46:443-450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sood, R., M. Rao, S. Singhal, and A. Rattan. 2005. Activity of RBx 7644 and RBx 8700, new investigational oxazolidinones, against Mycobacterium tuberculosis infected murine macrophages. Int. J. Antimicrob. Agents 25:464-468. [DOI] [PubMed] [Google Scholar]
- 17.Sreevatsan, S., X. Pan, K. E. Stockbauer, N. Connell, B. N. Kreiswirth, T. S. Whittam, and J. M. Musser. 1997. Restricted structural gene polymorphism in the Mycobacterium tuberculosis complex indicates evolutionary recent global dissemination. Proc. Natl. Acad. Sci. U. S. A. 94:9869-9874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sun, Z., Y. Chao, X. Zhang, J. Zhang, Y. Li, Y. Qiu, Y. Liu, L. Nie, A. Guo, and C. Li. 2008. Characterization of extensively drug-resistant Mycobacterium tuberculosis clinical isolates in China. J. Clin. Microbiol. 46:4075-4077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taniguchi, H., H. Aramaki, Y. Nikaido, Y. Mizuguchi, M. Nakamura, T. Koga, and S. Yoshida. 1996. Rifampicin resistance and mutations of the rpoB gene in Mycobacterium tuberculosis. FEMS Microbiol. Lett. 144:103-108. [DOI] [PubMed] [Google Scholar]
- 20.Telenti, A., P. Imboden, F. Marchesi, D. Lowrie, S. T. Cole, M. J. Colston, L. Matter, K. Schopfer, and T. Bodmer. 1993. Detection of rifampicin-resistance mutations in Mycobacterium tuberculosis. Lancet 341:647-650. [DOI] [PubMed] [Google Scholar]
- 21.Tortoli, E., M. Benedetti, A. Fontanelli, and M. T. Simonetti. 2002. Evaluation of automated BACTEC MGIT 960 system for testing susceptibility of Mycobacterium tuberculosis to four major antituberculous drugs: comparison with the radiometric BACTEC 460TB method and the agar plate method of proportion. J. Clin. Microbiol. 40:607-610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.World Health Organization. 2008. Tuberculosis facts. World Health Organization, Geneva, Switzerland. www.who.int/tb.
- 23.Xu, C., B. N. Kreiswirth, S. Sreevatsan, J. M. Musser, and K. Drlica. 1996. Fluoroquinolone resistance associated with specific gyrase mutations in clinical isolates of multidrug-resistant Mycobacterium tuberculosis. J. Infect. Dis. 174:1127-1130. [DOI] [PubMed] [Google Scholar]