Abstract
Antibiotic-resistant Enterococcus faecalis and Clostridium difficile are responsible for nosocomial infections in humans, in which they inhabit the same niche. Here, we demonstrate transfer of the conjugative transposon Tn5397 from C. difficile 630 to E. faecalis JH2-2, the first reported gene transfer between these two bacteria. Furthermore, transfer from the E. faecalis EF20A transconjugant to the epidemic ribotype 027 C. difficile strain R20291 was also demonstrated. Tn5397 was shown to use a single specific target site in E. faecalis; it also has specific target sites in C. difficile. These experiments highlight the importance of continual monitoring for emerging resistances in these bacteria.
Clostridium difficile is an enteric pathogen and the leading cause of antibiotic-associated diseases ranging from self-limiting diarrhea to severe pseudomembranous colitis (7, 10, 19). Treatment is usually by oral metronidazole or vancomycin (4, 13, 15). Enterococcus spp. are opportunistic pathogens responsible for a wide variety of infections (2, 12, 24). Vancomycin resistance in enterococci is now widespread (3). In E. faecalis, the genes responsible have been shown to be carried on conjugative transposon Tn1549 (6, 20). C. difficile and Enterococcus spp. often coexist in patients, causing increased severity of illness and prolonged duration of hospitalization (1, 8, 5). Both bacteria can acquire resistance to multiple antibiotics via mobile elements (16).
Conjugative transposons (17) are capable of intracellular transposition and intercellular conjugation, often across large phylogenetic distances (16). Conjugative transposon Tn5397 confers resistance to tetracycline (Tc) and was originally identified in C. difficile strain 630 (14). This element contains tet(M) and has been shown to be transferable from C. difficile to Bacillus subtilis and vice versa and between C. difficile strains (14). In this study, we wanted to assess the potential for gene transfer of Tn5397 between C. difficile and E. faecalis.
All bacterial strains used in this study are shown in Table 1. C. difficile were grown anaerobically (80% N2, 10% CO2, and 10% H2) at 37°C on brain heart infusion (BHI) agar supplemented with 5% defibrinated horse blood (E & O Laboratories, United Kingdom) and C. difficile-selective supplement (Oxoid, United Kingdom) or in prereduced BHI broth. E. faecalis and Escherichia coli were grown aerobically on or in BHI or LB agar or broth at 37°C. Antibiotics were used at concentrations of 10 μg/ml (tetracycline and erythromycin [Erm]), 25 μg/ml (rifampin [Rif]), 5 μg/ml (fusidic acid [Fus]), and 100 μg/ml (ampicillin [Amp]) (Sigma). Filter mating was carried out as previously described (18). E. faecalis transconjugants were selected on tetracycline-, rifampin-, and fusidic acid-containing plates with aerobic growth. C. difficile R20291 transconjugants were selected on tetracycline- and erythromycin-containing plates with anaerobic growth. PCR was carried out with primers (Table 2) by using the GeneAmp 2400 PCR system (Perkin-Elmer Cetus) under the following conditions: 94°C for 4 min, followed by 30 cycles of 94°C for 1 min, 50 to 60°C for 1 min (dependent on primer annealing temperature), 72°C for 1 to 2 min (dependent on expected amplicon size), and 72°C for 4 min. Amplicons were sequenced at the Department of Biochemistry, University of Cambridge, United Kingdom. For Southern hybridization, genomic DNAs from the E. faecalis JH2-2 (recipient) and transconjugants were digested overnight with XmnI at 37°C, followed by separation on a 1% agarose gel. Fragments were then transferred to a Hybond N+ nylon membrane (Amersham Biosciences, United Kingdom) and hybridized to a 300-bp probe derived from the tndX gene. Analysis of the Southern blot was performed using ECL direct nucleic acid labeling and detection systems (Amersham Biosciences, United Kingdom) according to the manufacturer's instructions.
TABLE 1.
Bacterial strains
| Bacterium | Property(ies) | Reference or source |
|---|---|---|
| C. difficile 630 | Tcr, Ermr | 25 |
| C. difficile R20291a | Ermr | Anaerobe Reference Laboratory, Cardiff, UK |
| E. faecalis JH2-2 | Rifr, Fusr | 11 |
| E. faecalis EF20A | Tcr, Rifr, Fusr | This work |
| E. coli (α-select, bronze efficiency) competent cells | Ampr | Bioline, UK |
This strain was responsible for an epidemic outbreak at Stoke Mandeville Hospital, United Kingdom (9).
TABLE 2.
Primer and probe details
| Primer/probea | Sequence (5′-3′) | Amplicon and/or purposeb |
|---|---|---|
| Tndx (F30) | CTTACAATGTTAAAACAGCAAGC | 1.6-kb fragment of tndX |
| Tndx (R1612) | GAGAATGTATCAATGAGACACTG | 1.6-kb fragment of tndX 300-bp probe for Southern analysis |
| TndX probe | CTTTAGGGAAAATAACTGAT | 300-bp probe for Southern analysis |
| LEO | CCACTTGATATGAAAAATCAAATGGCTC | sspPCR, CI, left-end transposon-genome junction |
| REO | ACGTGTATCAAGCAGAGGGAATCGGTAAA | sspPCR, CI, right-end transposon-genome junction |
| PTS forward primer | GTGTCAATGACCGCAGAAGA | Chromosomal target site, left-end transposon-genome junction |
| PTS reverse primer | TCGCTAGAATGACCTGTAGAAGAA | Chromosomal target site, right-end transposon-genome junction |
| M13 forward primer | GTAAAACGACGGCCAGT | sspPCR |
| M13 reverse primer | CAGGAAACAGCTATGAC | sspPCR |
PTS, phosphotransferase system.
CI, circular intermediate.
To determine the insertion site in E. faecalis, single-specific-primer PCR (sspPCR) was used. Genomic DNAs (3 μg) of the E. faecalis EF20A transconjugant (Table 1) and pUC19 (0.1 μg) were digested with either EcoRI or BamHI. Digested pUC19 was dephosphorylated with calf intestine alkaline phosphatase (Sigma). Both digested DNAs were cleaned by using a Qiagen Miniprep column. Ligations were carried out overnight with T4 DNA ligase (Promega) at 4°C. One microliter of ligation mixture was used as a template in PCR. Amplification was carried out using the Tn5397-specific primers (LEO or REO) and either M13 forward or M13 reverse primer (Table 2). Sequenced PCR products were analyzed using NCBI tools (http://www.ncbi.nlm.nih.gov/) and the Expasy molecular biology server (http://www.expasy.ch/tools/). Multiple sequence alignments were carried out using ClustalW (http://www.ebi.ac.uk/clustalW).
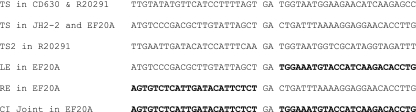
Tn5397 was transferred from C. difficile 630 to E. faecalis JH2-2 with a mean transfer frequency (± standard deviation [SD]) of 8.85 × 10−8 (± 2.14 × 10−7) transconjugants per recipient (average of 5 independent experiments). All 5 transconjugants analyzed were generated independently from different filter-mating experiments to exclude the possibility of analyzing siblings. All tetracycline-resistant transconjugants were positive for the tndX determinant of Tn5397 (22). The tndX gene is unique to Tn5397, the product of which is required and sufficient for its excision and insertion (22). Southern blot analysis showed that a single copy of Tn5397 had inserted in the same site in all E. faecalis transconjugants (results not shown). Determination of the insertion site of Tn5397 in E. faecalis, using sspPCR, showed that Tn5397 had inserted into a site within the JH2-2 chromosome which has identity to an open reading frame (ORF) from E. faecalis V583 encoding a IIA component of a mannose/sorbose-specific sugar phosphotransferase system (NCBI accession number NP_814245) involved in the uptake and phosphorylation of carbohydrates. The sequences of the target site and the joint of the circular form of Tn5397 in E. faecalis are shown in Fig. 1. PCR analysis for the transposon-genome junction for all 5 transconjugants confirmed that the element had entered this site in all transconjugants analyzed.
FIG. 1.
Target sites of Tn5397 within C. difficile 630 (CD630), C. difficile R20291, and E. faecalis JH2-2. Tn5397 sequence is shown in boldface. TS, target site in the genome; LE, left end of Tn5397; RE, right end of Tn5397; CI, circular intermediate of Tn5397; TS2, the second target site in C. difficile R20291. All sequences are derived from PCR amplicons.
One transconjugant, EF20A, was used as a donor with C. difficile R20291 as the recipient. Tn5397 transferred at a frequency of 6.15 × 10−8 transconjugants per donor or 4.44 × 10−6 transconjugants per recipient. Tn5397 usually occupies a single specific site in the C. difficile 630 genome, whereas in R20291, there are two specific sites (Fig. 1). We confirmed by PCR that Tn5397 insertion in C. difficile R20291 transconjugants had occurred at one of these sites (results not shown).
This is the first study to demonstrate reciprocal genetic exchange between E. faecalis and C. difficile. The fact that Tn5397 has a single preferred target site is similar to the situation in C. difficile 630 but different from that in B. subtilis, in which insertion occurs at multiple sites (21, 23). Demonstration of two-way genetic transfer between E. faecalis and C. difficile in the laboratory environment represents an ideal situation for gene transfer, and this setting is different from the usual environment of the bacteria; however, these results highlight the need for continual monitoring of emerging resistances in both C. difficile and E. faecalis, specifically for resistance to clinically important vancomycin, clindamycin, and fluoroquinolones.
Acknowledgments
A.S.J. is funded by the Malaysian Government. The research leading to these results has received funding from the European Community's Seventh Framework Programme (FP7/2007-2013) under grant agreement no. 223585 and the Medical Research Council (grant no. G0601176).
Footnotes
Published ahead of print on 16 August 2010.
REFERENCES
- 1.Al-Nassir, W. N., A. K. Sethi, Y. Li, M. J. Pultz, M. M. Riggs, and C. J. Donskey. 2008. Both oral metronidazole and oral vancomycin promote persistent overgrowth of vancomycin-resistant enterococci during treatment of Clostridium difficile-associated disease. Antimicrob. Agents Chemother. 52:2403-2406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amyes, S. G. B. 2007. Enterococci and streptococci. Int. J. Antimicrob. Agents 29:43-52. [DOI] [PubMed] [Google Scholar]
- 3.Arias, C. A., G. A. Contreras, and B. E. Murray. 2010. Management of multi-drug resistant enterococcal infections. Clin. Infect. Dis. 16:556-562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baines, S. D., R. O'Connor, K. Saxton, J. Freeman, and M. H. Wilcox. 2009. Activity of vancomycin against epidemic Clostridium difficile strains in a human gut model. J. Antimicrob. Chemother. 663:520-525. [DOI] [PubMed] [Google Scholar]
- 5.Donskey, C. J., A. J. Ray, C. K. Hoyen, P. D. Fuldauer, D. C. Aron, and R. A. Bonomo. 2003. Cocolonization and infection with multiple nosocomial pathogens in patients colonized with vancomycin-resistant enterococci. Infect. Control Hosp. Epidemiol. 24:242-245. [DOI] [PubMed] [Google Scholar]
- 6.Garnier, F., S. Taourit, P. Glaser, P. Courvalin, and M. Galimand. 2000. Characterization of transposon Tn1549, comferring VanB-type resistance in Enterococcus spp. Microbiology 146:1481-1489. [DOI] [PubMed] [Google Scholar]
- 7.Gerding, D. N. 1997. Is there a relationship between vancomycin-resistant enterococcal infection and Clostridium difficile infection? Clin. Infect. Dis. 25(Suppl. 2):S206-S210. [DOI] [PubMed] [Google Scholar]
- 8.Gerding, D. N., S. Johnson, L. R. Peterson, M. E. Mulligan, and J. Silva, Jr. 1995. Clostridium difficile-associated diarrhea and colitis. Infect. Control Hosp. Epidemiol. 16:459-477. [DOI] [PubMed] [Google Scholar]
- 9.Healthcare Commission. 2006. Investigation into outbreaks of Clostridium difficile at Stoke Mandeville Hospital, Buckinghamshire Hospitals NHS Trust. Healthcare Commission, London, United Kingdom. http://www.cqc.org.uk/_db/_documents/Stoke_Mandeville.pdf.
- 10.Huang, H., A. Weintraub, H. Fang, and C. E. Nord. 2009. Antimicrobial resistance in Clostridium difficile. Int. J. Antimicrob. Agents 34:516-522. [DOI] [PubMed] [Google Scholar]
- 11.Jacob, A. E., and S. J. Hobbs. 1974. Conjugal transfer of plasmid-borne multiple antibiotic resistance in Streptococcus faecalis var. zymogenes. J. Bacteriol. 117:360-372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Leclercq, R. 2009. Epidemiological and resistance issues in multidrug-resistant staphylococci and enterococci. Clin. Microbiol. Infect. 15:224-231. [DOI] [PubMed] [Google Scholar]
- 13.Leffler, D. A., and J. T. Lamont. 2009. Treatment of Clostridium difficile-associated disease. Gastroenterology 136:1899-1912. [DOI] [PubMed] [Google Scholar]
- 14.Mullany, P., M. Wilks, L. Lamb, C. Clayton, B. Wren, and S. Tabaqchali. 1990. Genetic analysis of a tetracycline resistance element from Clostridium difficile and its conjugal transfer to and from Bacillus subtilis. J. Gen. Microbiol. 136:1343-1349. [DOI] [PubMed] [Google Scholar]
- 15.Pepin, J. 2008. Vancomycin for the treatment of Clostridium difficile infection: for whom is this expensive bullet really magic? Clin. Infect. Dis. 46:1493-1498. [DOI] [PubMed] [Google Scholar]
- 16.Roberts, A. P., and P. Mullany. 2009. A modular master on the move: the Tn916 family of mobile genetic elements. Trends Microbiol. 17:251-258. [DOI] [PubMed] [Google Scholar]
- 17.Roberts, A. P., M. Chandler, P. Courvalin, G. Guédon, P. Mullany, T. Pembroke, J. I. Rood, C. J. Smith, A. O. Summers, M. Tsuda, and D. E. Berg. 2008. Revised nomenclature for transposable genetic elements. Plasmid 60:167-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roberts, A. P., P. Mullany, and M. Wilson. 2001. Gene transfer in bacterial biofilms. Methods Enzymol. 336:60-65. [DOI] [PubMed] [Google Scholar]
- 19.Rupnik, M., M. H. Wilcox, and D. N. Gerding. 2009. Clostridium difficile infection: new developments in epidemiology and pathogenesis. Nat. Rev. Microbiol. 7:526-536. [DOI] [PubMed] [Google Scholar]
- 20.Tsvetkova, K., J.-C. Marvaud, and T. Lambert. 2010. Analysis of the mobilization functions of the vancomycin resistance transposon Tn1549, a member of a new family of conjugative elements. J. Bacteriol. 192:702-713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wang, H., A. P. Roberts, D. Lyras, J. I. Rood, M. Wilks, and P. Mullany. 2000. Characterization of the ends and target sites of the novel conjugative transposon Tn5397 from Clostridium difficile: excision and circularization is mediated by the large resolvase, TndX. J. Bacteriol. 182:3775-3783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang, H., and P. Mullany. 2000. The large resolvase TndX is required and sufficient for integration and excision of derivatives of the novel conjugative transposon Tn5397. J. Bacteriol. 182:6577-6583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang, H., M. C. M. Smith, and P. Mullany. 2006. The conjugative transposon Tn5397 has a strong preference for integration into its Clostridium difficile target site. J. Bacteriol. 188:4871-4878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Woodford, N., and D. M. Livermore. 2009. Infections caused by Gram-positive bacteria: a review of the global challenge. J. Infect. 59(Suppl. 1):S4-S16. [DOI] [PubMed] [Google Scholar]
- 25.Wüst, J. N., and U. Hardegger. 1983. Transferable resistance to clindamycin, erythromycin and tetracycline in Clostridium difficile. Antimicrob. Agents Chemother. 23:784-786. [DOI] [PMC free article] [PubMed] [Google Scholar]