Abstract
BI 201335 is a hepatitis C virus (HCV) NS3-NS4A (NS3 coexpressed with NS4A) protease inhibitor that has been shown to have potent clinical antiviral activity. It is a highly optimized noncovalent competitive inhibitor of full-length NS3-NS4A proteases of HCV genotypes 1a and 1b with Ki values of 2.6 and 2.0 nM, respectively. Ki values of 2 to 230 nM were measured against the NS3-NS4A proteases of HCV genotypes 2 to 6, whereas it was a very weak inhibitor of cathepsin B and showed no measurable inhibition of human leukocyte elastase. BI 201335 was also shown to be a potent inhibitor of HCV RNA replication in vitro with 50% effective concentrations (EC50s) of 6.5 and 3.1 nM obtained in genotype 1a and 1b replicon assays. Combinations of BI 201335 with either interferon or ribavirin had additive effects in replicon assays. BI 201335 had good permeability in Caco-2 cell assays and high metabolic stability after incubation with human, rat, monkey, and dog liver microsomes. Its good absorption, distribution, metabolism, and excretion (ADME) profile in vitro, as well as in rat, monkey, and dog, predicted good pharmacokinetics (PK) in humans. Furthermore, drug levels were significantly higher in rat liver than in plasma, suggesting that distribution to the target organ may be especially favorable. BI 201335 is a highly potent and selective NS3-NS4A protease inhibitor with good in vitro and animal ADME properties, consistent with its good human PK profile, and shows great promise as a treatment for HCV infection.
Chronic hepatitis C virus (HCV) infection affects 130 to 170 million individuals worldwide (14). The etiologic agent is a small enveloped single-stranded RNA virus belonging to the Flaviviridae family, Hepacivirus genus (32). Although present in human populations for thousands of years, it was discovered only 20 years ago as the causative agent of non-A, non-B hepatitis (6). The HCV genome consists of approximately 9,600 bases, encoding a single polyprotein of approximately 3,000 amino acids, flanked by conserved 5′ and 3′ untranslated regions (UTRs). The viral polyprotein comprises four structural proteins followed by six nonstructural (NS) proteins that play essential roles in viral replication (25).
One of the best-studied nonstructural proteins is NS3, a bifunctional protein that consists of an N-terminal protease domain and a C-terminal helicase domain (9). The protease domain has a trypsin-like fold with a flat and solvent-exposed substrate binding site (11, 21). The central portion of the NS4A protein is integrated into the protein fold of the NS3 protease domain and is required for full activity (3). The NS3-NS4A (NS3 coexpressed with NS4A) protease plays a critical role in the maturation of the viral polyprotein precursor and was recognized early on as potential target for antiviral drugs (2). Indeed, the first direct acting antiviral agent to be studied in humans was the protease inhibitor BILN 2061, and two other protease inhibitors, telaprevir and boceprevir, are currently in phase III trials (10, 12, 13, 30).
The HCV protease inhibitors currently in clinical development may be divided into two classes depending on the nature of the active site binding group (40). Telaprevir (28) and boceprevir (22) both contain an α-ketoamide, which forms a covalent reversible interaction with the active site serine of the NS3-NS4A protease catalytic triad and contributes significantly to their potency. The other class of inhibitors contains functional groups that form ionic interactions with the residues of the catalytic triad and therefore makes exclusively noncovalent interactions with the protein.
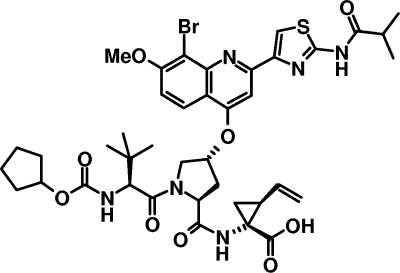
We and others have previously reported substrate-based noncovalent inhibitors containing a carboxylic acid at the C terminus (19, 33). We have shown that a carboxylic acid can establish crucial and unique interactions with the NS3 active site, imparting not only potency but also selectivity with respect to other serine proteases (18, 35). In contrast, inhibitors bearing reactive C-terminal functional groups can be potent inhibitors of other proteases (18). BI 201335 (Fig. 1) is a potent and selective inhibitor of the NS3-NS4A serine protease that derives significant potency both from the interaction of its C-terminal carboxylic acid with the active site, as well as from the aromatic proline substituent. The optimization of this series of inhibitors that resulted in the identification of BI 201335 took into account not only the potency of the compounds in biochemical and cellular assays but also their in vitro absorption, distribution, metabolism, and excretion (ADME) and animal pharmacokinetic properties (20). In this work we describe the preclinical profile of BI 201335, which led to its selection for preclinical development followed by clinical trials in HCV-infected patients.
FIG. 1.
Chemical structure of BI 201335. Me, methyl.
MATERIALS AND METHODS
Inhibitors.
The synthesis of BI 201335 has been reported (20). Telaprevir and boceprevir were synthesized at Boehringer Ingelheim according to published procedures (37, 41). Alpha interferon (IFN-α) from human leukocytes and ribavirin were obtained from Sigma-Aldrich.
NS3-NS4A proteins.
Details of the cloning, expression, and purification of full-length NS3-NS4A gene products used in this work have been published previously (24, 34). Briefly, the NS3-NS4A of genotypes 1a, 1b, and 2a were isolated from H77, Con1, and JFH1 clones, respectively. The corresponding proteins from genotypes 2b, 3a, 4a, 5a, and 6a were produced from in-house clones isolated directly from patient serum samples. All proteins were produced in Escherichia coli and autoprocessed at the NS3-NS4A junction prior to cell lysis. These N-terminally His-tagged proteins were then purified using nickel and poly(U) affinity resins. Proteins were eluted from the poly(U) resin in a buffer composed of 50 mM NaPO4 (pH 7.5), 10% glycerol, 1.0 M NaCl, and 0.05% n-dodecyl-β-d-maltoside and stored at −80°C prior to use.
Cells.
Human hepatoma Huh-7 cells were from Health Science Research Resources Bank, Osaka, Japan, and Huh-7.5 cells (4) were obtained under license from Apath, LLC. Huh-7 and Huh-7.5 cells and all replicon-containing Huh-7 cell lines used for the experiments were maintained in Dulbecco's modified Eagle's medium (DMEM) supplemented with 10% fetal bovine serum (FBS) at 37°C in an atmosphere of 5% CO2. Replicon-containing cells were maintained in medium supplemented with 0.5 mg/ml G418, unless indicated otherwise.
Biochemical assays.
Biochemical assays were performed at room temperature as described previously (24). Briefly, reaction mixtures comprised 0.5 nM NS3-NS4A enzyme (2.5 nM for genotype 1a), 5 μM fluorogenic depsipeptide substrate anthranilyl-DDIVPAbu[C(O)-O]AMY(3-NO2)TW-OH (Abu stands for aminobutyric acid) and inhibitor in a reaction buffer composed of 50 mM Tris-HCl (pH 8.0), 0.25 M sodium citrate, 0.01% n-dodecyl-β-d-maltoside, 1 mM tris(2-carboxyethyl)phosphine (TCEP) plus 5% dimethyl sulfoxide (DMSO). Telaprevir and boceprevir were preincubated with enzyme for 60 min prior to the addition of substrate. Reaction mixtures were incubated at 23°C for 60 to 70 min and terminated by the addition of 1 M morpholineethanesulfonic acid (MES) (pH 5.8). Fluorescence of the N-terminal product anthranilyl-DDIVP-Abu was measured using a POLARStar Galaxy plate reader (BMG). Calculated percent inhibition at each inhibitor concentration was then used to determine the median 50% inhibition concentration (IC50) (Assay Explorer v3.2; Symyx Technologies). IC50s obtained in these experiments were converted to apparent Ki values using the equation IC50 = Ki (1 + [S]/Km) for competitive inhibitors (5), where [S] is the concentration of substrate. Conversion to apparent Ki values corrected for differences in the ratio of [S] to Km for the different enzymes and thus allowed direct comparison of binding affinity across genotypes.
To demonstrate its mechanism of inhibition, steady-state velocities were measured at various concentrations of BI 201335 (0 to 24 nM) and fluorogenic depsipeptide substrate Ac-DED(EDANS)EEAbu[C(O)-O]ASK(DABCYL)-NH2 {Ac stands for acetyl, EDANS stands for 5-[(aminoethyl)amino]naphthalene-1-sulfonic acid, and DABCYL stands for 4-(dimethylaminoazo)benzene-4-carboxylic acid} (0.25 to 4.0 μM). Initial rate data were fit to the equation for competitive inhibition, using the GraFit software (version 3.0; Erithacus Software Ltd., Staines, United Kingdom).
Selectivity assays.
NS3 protease inhibitor selectivity was determined against human leukocyte elastase (HLE) and human liver cathepsin B (CatB). Both enzymes were obtained from Calbiochem. The colorimetric substrate Succ-Ala-Ala-Val-pNA (Succ stands for succinate and pNA stands for para-nitroaniline) and the fluorogenic substrate Z-Phe-Arg-AMC (AMC stands for 7-amino-4-methylcoumarin) were used for the HLE and CatB assays, respectively, and were purchased from Bachem. Assays were performed in 96-well plates. The HLE assay was performed with 130 μM Succ-Ala-Ala-Ala-pNA and 8 nM HLE in 50 mM Tris-HCl (pH 8.0), 250 mM sodium citrate, 0.01% n-dodecyl-β-d-maltoside, 5% DMSO, whereas the CatB assay was performed with 4 μM Z-Phe-Arg-AMC and 0.5 nM cathepsin B in 100 mM sodium phosphate (pH 6.0), 1 mM EDTA, 0.01% Tween 20, 1 mM TCEP, 5% DMSO (the CatB stock solution was activated in buffer containing 400 mM NaCl, 20 mM TCEP, and no DMSO prior to use). Enzyme and inhibitor were incubated for 60 min at room temperature followed by the addition of substrate solution to a final volume of 100 μl. After 60 min, absorbance at 405 nm was measured (Thermomax plate reader) for the HLE assay, and fluorescence was measured (BMG POLARstar Galaxy plate reader with a 355-nm excitation filter and 485-nm emission filter) for the CatB assay.
Replicon assays.
The HCV genotype 1a and 1b replicon-containing cell lines carry adapted self-replicating bicistronic replicons encoding an HCV internal ribosome entry site (IRES)-neomycin phosphotransferase gene fusion in the first cistron and an encephalomyocarditis virus (EMCV) IRES-HCV NS2-NS5B-3′UTR from the HCV genotype 1a H77 (adaptive mutations encoding amino acid changes T1280A, S1358P, D1431N, F1809L, and I1839V) and 1b Con1 sequence (adaptive mutations encoding amino acid changes R1135K, S1560G, K1691R, T1993A, G2042C, L2155P, and P2166L) in the second cistron, respectively (13, 36). The genotype 2a replicon cell line is a Huh-7-derived cell line also carrying a bicistronic replicon encoding the unadapted subgenomic NS3-NS5B-3′UTR fragment from HCV JFH-1 isolate (36).
The cells were maintained in medium supplemented with 10% FBS and 0.25 mg/ml G418. Prior to the assay, the cells were plated in medium without G418 at a density of 10,000 cells per well in a 96-well plate and incubated at 37°C. The following day, the medium was removed and replaced by the same volume of DMEM containing 10% FBS, 0.5% DMSO, and serial dilutions of the test compound and then incubated for 72 h, after which replicon RNA levels were determined by TaqMan quantitative real-time reverse transcription-PCR (RT-PCR). Briefly, total RNA was extracted from the replicon cells using the RNeasy 96 kit (Qiagen) and quantified using RiboGreen (Molecular Probes). Real-time RT-PCR was performed on an ABI Prism 7700 sequence detection system using the TaqMan EZ RT-PCR (Applied Biosystems) (27). Reference standards containing known quantities of in vitro-transcribed, highly purified HCV replicon RNA were included in each RT-PCR assay plate for a standard curve to determine the HCV RNA copy number in each sample. The RNA copy number was normalized by RiboGreen RNA quantification of the total RNA extracted from the cell culture well and expressed as the number of genome equivalents per microgram of total RNA.
HCV virus replication assay.
Portions of the assay that required handling infectious virus were performed in a biosafety level 3 containment laboratory. A full-length HCV JFH1 molecular clone obtained under license from Toray (Japan) was used to transcribe HCV RNA in vitro using T7 RNA polymerase. Transfection of the in vitro-transcribed RNAs into human hepatoma replicon-cured Huh-7.5 cells was used to produce infectious virus as previously described (39, 42). Virus that had adapted to cell culture and that carried a gene encoding the K74T substitution in the core protein and a gene encoding the C2441S substitution in the C terminus of NS5A was used for the virus replication assay. Huh-7.5 cells were seeded in a 96-well plate at a density of 1 × 104 cells/well in cell culture medium and incubated for 24 h at 37°C and 5% CO2. The day of the assay, the medium was removed, and 100 μl of virus diluted in fresh medium was added with or without compounds. The test compound in 100% DMSO was first diluted in assay medium to a final DMSO concentration of 0.5% following the procedure described for subgenomic replicon testing with nine concentration curves. After 72 h of incubation, the medium was removed, and total RNA was extracted using the Qiagen RNeasy 96 kit according to the manufacturer's instructions. HCV RNA was quantified by real-time RT-PCR as described above for the HCV replicon assays.
Cell toxicity assay.
The cytotoxicity of BI 201335 was measured using a spectrophotometric assay that measures conversion of 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide (MTT) to purple formazan. Cells were exposed to serial dilutions of the inhibitor for 72 h after which cell viability was determined by adding MTT reagent (Sigma) and measuring the formazan product at 570 nm. The calculated percent inhibition was used to determine the cytotoxic concentration of drug that reduced the viable cell number by 50% (CC50) value.
Combination effects with IFN-α and ribavirin.
Huh-7 cells harboring adapted genotype 1b HCV subgenomic bicistronic replicon that carried an HCV-IRES-firefly luciferase-FMDV 2A-neomycin phosphotransferase fusion gene (FMDV stands for foot-and-mouth disease virus)in the first cistron, and an EMCV IRES-HCV NS2-NS5B-3′UTR in the second cistron (36) were used for these experiments. Inhibition of HCV RNA replication was determined by measuring luciferase levels (Promega Bright-Glo). Two experimental approaches were used to investigate potential drug interaction between BI 201335 and IFN-α or ribavirin. For the combination index model, the cells were incubated for 3 days in 96-well plates with serial dilutions of either IFN-α or ribavirin and BI 201335 and a fixed ratio combination of inhibitors below their cytotoxic concentration. The degree of synergy was evaluated by the median-effect principle with the combination index (CI) calculation and the mutually exclusive model of drug interaction (8). A program based on the median effect plot and the CI equation was used for data analysis (CalcuSyn v1; Biosoft). The lower and upper bounds of 95% confidence intervals were determined from the dose-response measurements (GraphPad; Prism) and then inserted into the combination index calculation to obtain confidence intervals for the CI values in each individual experiment. The interpretation of the CI values was based on the recommendations of Chou (7) but with fewer descriptive levels in order to be consistent with the observed intrinsic variability of the cell-based assay. Thus, a CI value of 0.80 to 1.25 indicates an additive effect and the absence of drug interaction. CI values incrementally larger than 1.25 suggest an increasing level of antagonism, whereas CI values incrementally smaller than 0.80 suggest an increasing level of synergy.
The combination of BI 201335 with IFN-α was also analyzed according to the Bliss independence model. For this analysis, each combination experiment included 6 to 9 doses of each drug alone and 54 different combinations of the two drugs. BI 201335 and IFN-α were serially diluted in cell culture medium spanning the range of dose response for inhibition of HCV RNA replication. Compound combinations were prepared in a matrix format using the same range of concentrations and tested in the HCV replicon assay. Results were subsequently transformed using the MacSynergy II software (29). All data points generated from the matrix of drug concentrations were used in this analysis. Triplicate data sets were used to perform statistical analysis and determine the volume of synergy or antagonism at 95% confidence for the interpretation of the results, where volumes of synergy and antagonism between −25 and 25% indicate no interaction. The cytotoxicity of each combination was evaluated by the MTT assay described above.
In vitro metabolic clearance was determined in 96-well format with three time points of incubation at 0, 10, and 20 min at 37°C. Male human liver microsomes (LM) and rhesus monkey LM were obtained from Gentest (Woburn, MA). Male Sprague-Dawley rat LM were prepared in-house. Male beagle dog liver microsomes were obtained from In Vitro Technologies (Baltimore, MD). Initial compound concentration was 2 μM. The incubation medium contained 1 mg of microsomal protein, 2.5 mM NADPH in a total volume of 1 ml of 0.066 M Tris buffer, pH 7.4. Reactions were initiated by the addition of NADPH and terminated at the appropriate time points by quenching with an equal volume of a 1:1 mixture of acetonitrile-methanol. Samples were centrifuged at 2,000 × g at 4°C for 10 min, and the resulting supernatants were analyzed by high-performance liquid chromatography (HPLC) (Waters Limited, Mississauga, Ontario, Canada). Intrinsic metabolic clearance and liver microsome metabolic clearance were calculated by the methods of Obach et al. (26).
Caco-2 cell permeability.
Caco-2 cells obtained from ATCC were seeded at a density of 125,000 cells per 0.5 ml in Costar 12-well plate inserts and allowed to grow and differentiate for 23 to 25 days with medium changes every second day. Prior to the assay, culture medium (DMEM supplemented with 10% FBS, 1% nonessential amino acids, and penicillin-streptomycin) was removed from both sides of the Transwell insert, and the cells were rinsed twice with warm Hanks balanced salt solution (HBSS). At the last rinse step, the chambers were filled with warm transport buffer (the apical side was filled with HBSS, 25 mM MES, and 0.25% bovine serum albumin [BSA] [pH 6.0]; the basolateral side was filled with HBSS, 25 mM HEPES, and 0.25% BSA [pH 7.4]). The plates were incubated at 37°C for 30 min after which the donor fluid (apical side for apical-to-basolateral [A-to-B] assay, basolateral side for B-to-A assay) was removed and replaced with the working solution. At designated time points (0, 1, 2, and 3 h), fluid from the receiver chamber was removed and replaced with appropriate fresh transport buffer. The samples were quenched with cold acetonitrile and centrifuged to pellet protein, and the supernatant was analyzed by HPLC (Waters Limited, Mississauga, Ontario, Canada). Apparent permeability was calculated as described by Artursson (1).
Protein binding.
The human plasma protein binding of BI 201335 was determined by equilibrium dialysis using rotating chambers as previously described (38). The plasma chamber containing BI 201335 (1 mg/ml) was separated by a cellulose dialysis membrane (molecular size cutoff, 12 to 14 kDa) from the chamber containing only 100 mM phosphate (pH 7.4) buffer. The chambers were incubated for 6 h at 37°C with a rotation rate of 25 rpm. Plasma protein binding (as a percentage) was calculated as previously described (38).
Pharmacokinetics and liver distribution.
All protocols involving animal experimentation were reviewed and approved by the respective Animal Care and Use Committee of each test facility. In-life procedures were in compliance with the Guide for the Care and Use of Laboratory Animals from the Canadian Council of Animal Care. All rat pharmocokinetics (PK) and distribution studies were performed at Boehringer Ingelheim (Canada) Ltd. PK studies in dogs and monkeys were performed at LAB Pre-Clinical Research International Inc., Laval, Quebec, Canada. All chemicals used were reagent grade or better. Plasma samples and tissue samples awaiting analysis were stored frozen at −20°C.
Rat pharmacokinetic studies were performed in male Sprague-Dawley rats (275 to 300 g) (Charles River, St.-Constant, Quebec, Canada). Animals were forced to fast overnight with access to 10% dextrose in water and dosed at 5 mg/kg of body weight in a dosing volume of 10 ml/kg of a vehicle consisting of 0.5% Methocel and 0.3% Tween 80. Blood samples were collected from the cannulated right carotid at 0, 0.25, 0.5, 1, 1.5, 2, 3, 4, 6, and 8 h postdosing, and plasma samples from 3 rats were pooled at each time point. For comparative plasma and liver study in rats, systemic blood samples were collected from each anesthetized rats via cardiac puncture at 0, 1, 2, 4, 6, 8, and 12 h postdosing using heparinized syringe. The liver was perfused with 25 ml ice-cold saline for 1 min prior to collection of the right lateral lobe. All collected organs were frozen in 10 ml 0.32 M sucrose at −20°C. Oral PK studies in fasted male rhesus monkeys (3.0 to 4.8 kg) and beagle dogs (9.8 to 13.8 kg) were performed using the same dose of 5 mg/kg and the same oral formulation.
Plasma samples (200 μl) were mixed with 800 μl Milli-Q water, treated with 5 μl of phosphoric acid, and loaded onto the Oasis HLB 30 mg/cm3 solid-phase extraction 96-well plate (Waters Limited, Mississauga, Ontario, Canada). Extractions were performed with a Gilson 215 system (Gilson, Inc., Middleton, WI). The cartridges were first preconditioned with 1 ml of 5% ammonium hydroxide (vol/vol) in acetonitrile, followed by 1 ml acetonitrile and then with 1 ml Milli-Q water. After the samples were loaded, the cartridges were washed with 1 ml Milli-Q water, followed by 1 ml of 5% methanol (vol/vol) in water, and finally by 1 ml of 2% acetic acid (vol/vol) in methanol-acetonitrile-water (1:1:8). BI 201335 was eluted with 2 volumes of 500 μl of 5% ammonium hydroxide (vol/vol) in acetonitrile. The organic phase was evaporated under a nitrogen stream using Turbo Vap 96 (Zymark, Hopkinton, MA) at 60°C. The residue was reconstituted in 200 to 400 μl of 2% ammonium hydroxide in acetonitrile-Milli-Q water (1:1). Two to five microliters was injected for liquid chromatography-mass spectrometry (LC-MS) analysis.
To extract BI 201335 from the liver, 0.6-g rat liver tissue samples were homogenized with 7 ml of 1 M Tris. Each homogenate was mixed with 0.7 mg of subtilisin. Samples were incubated in a water bath at 55°C for 1 h and then precipitated with 1.5 ml trichloroacetic acid. The supernatant was collected after centrifugation at 1,100 × g for 15 min at 4°C and then extracted using the same procedure as described above for plasma extraction.
Pharmacokinetic samples were analyzed individually for BI 201335 by liquid chromatography-tandem mass spectrometry (ZQ-LCMS system; Waters Limited, Mississauga, Ontario, Canada) at a m/z of 869.3. The lower limits of quantification (LOQ) were 10, 10, and 50 nM for rat, monkey, and dog plasma, respectively. The LOQ was 100 nM for rat liver. Mean ± standard error (n = 3 when applicable) concentrations of BI 201335 were calculated per species, tissue, and sampling time. The temporal profiles of drug concentrations in plasma were analyzed by noncompartmental methods using WinNonlin (version 3.1; Scientific Consulting, Inc., Cary, NC).
RESULTS
Activity in biochemical assays.
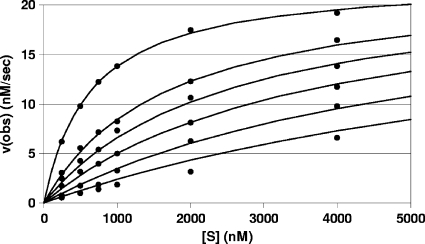
Inhibition of protease activity by BI 201335 was evaluated using the full-length NS3 protein coexpressed with the 54-amino-acid cofactor NS4A (NS3-NS4A). Apparent Ki values of less than 3 nM were obtained for HCV genotype 1a and 1b enzymes (Table 1). Figure 2 displays genotype 1a NS3 or NS4A (NS3/4A) enzyme steady-state kinetics at increasing concentrations of BI 201335 which were most consistent with a competitive mechanism of inhibition, as expected for an inhibitor originally derived from the protease substrate.
TABLE 1.
Potency of BI 201335, telaprevir, and boceprevir against NS3-NS4A proteins of different HCV genotypes
| Inhibitor |
Ki(app)a (nM) against NS3-NS4A protein of HCV genotype: |
|||||||
|---|---|---|---|---|---|---|---|---|
| 1a | 1b | 2a | 2b | 3a | 4a | 5a | 6a | |
| BI 201335 | 1.2 ± 0.2 | 2.8 ± 0.5 | 21 ± 4 | 64 ± 12 | 230 ± 30 | 1.8 ± 0.5 | 5.8 ± 1.0 | 6.1 ± 0.9 |
| Telaprevir | 3.2 ± 1.1 | 4.4 ± 1.1 | 15 ± 6 | 73 ± 11 | 160 ± 20 | 50 ± 18 | 110 ± 20 | 4.5 ± 1.2 |
| Boceprevir | 1.1 ± 0.3 | 2.0 ± 0.4 | 7.3 ± 3.7 | 28 ± 11 | 23 ± 6 | 8.6 ± 0.6 | 18 ± 4 | 2.3 ± 0.1 |
Ki(app), apparent Ki determined from IC50 and the ratio of substrate concentration to Km as described in Materials and Methods. Values shown are means ± standard deviations from at least three independent experiments.
FIG. 2.
Steady-state kinetic data for inhibition of NCV genotype 1a NS3-NS4A protease by BI 201335. The concentration of substrate is shown on the x axis, and the observed maximum rate of metabolism [v(obs)] is shown on the y axis. The points shown correspond to experimental values at inhibitor concentrations of 0, 3.2, 5.5, 8.9, 15, and 24 nM. The lines show the best fit of the data to a competitive mechanism. The experiment was repeated twice, giving Ki values of 2.0 ± 0.1 and 3.3 ± 0.2 nM. Data from the first experiment are shown.
BI 201335 showed a similar level of inhibitory potency against the NS3-NS4A proteases of HCV genotypes 4a, 5a, and 6a as it did against the two genotype 1 enzymes (≤5-fold difference), but it was somewhat less potent against enzymes from HCV genotypes 2a, 2b, and 3a (20, 50, and 190-fold, relative to genotype 1a). Apparent Ki values are given in Table 1 to allow better comparison of activity against different genotypes, because substrate Km values varied slightly (see Materials and Methods). The genotype 2 and 3 NS3 protease active sites contain a small number of amino acid differences that we previously showed account for the reduced affinity for the carboxylic acid inhibitor BILN 2061 (34).
IC50s for the α-ketoamide-containing inhibitors telaprevir and boceprevir were determined in parallel as reported in Table 1. Both compounds were previously shown to inhibit HCV genotype 1a and 1b enzymes with low-nanomolar potency (22, 28). Telaprevir had similar activity against genotype 2a and 6a NS3/4A protease but shifted 23-, 50-, 16-, and 34-fold with genotype 2b, 3a, 4a, and 5a enzyme, respectively, compared to genotype 1a. Boceprevir had a similar cross-genotype profile to telaprevir, though increases in apparent Ki were slightly smaller. As previously reported (22, 28), we observed a time-dependent increase in inhibition with the two α-ketoamide inhibitors, so values for telaprevir and boceprevir were obtained with a 60-min preincubation of enzyme and inhibitor prior to the addition of substrate, whereas those for BI 201335 were obtained without preincubation. This difference between BI 201335 and telaprevir or boceprevir is consistent with the mechanism of binding for each inhibitor. The binding of telaprevir or boceprevir is slow, because a covalent complex must form after initial weak association (22, 28).
As previously shown for other carboxylic acid-containing inhibitors, BI 201335 had no significant activity against the human serine and cysteine proteases elastase and cathepsin B (CatB) (Table 2) (13, 18). We tested inhibition of elastase, in particular, since this protease has a substrate specificity similar to that of NS3. Telaprevir was a fairly good inhibitor of both of these enzymes (IC50 < 2.5 μM) whereas boceprevir had weaker but measurable activity (Table 2). To probe more widely for possible BI 201335 off-target pharmacological activity, we submitted it to an extended panel of enzymatic and receptor binding assays, including 39 proteases, six other enzymes, 32 receptors, and 12 ion channels and transporters (see Table S1 in the supplemental material). BI 201335 had little or no activity against any of the proteases in the panel (<50% at 10 μM). The only off-target IC50s below 10 μM were obtained against the phosphatase calcineurin (9 and 19 μM in two different assays) and acyl coenzyme A (acyl-CoA)-cholesterol acyltransferase (2.4 μM). These micromolar activities may not be physiologically relevant, given the high level of plasma protein binding observed for this compound (see below).
TABLE 2.
Activity of BI 201335, telaprevir, and boceprevir against representative serine and cysteine proteases
| Inhibitor | IC50 (nM) against the following proteasea: |
|
|---|---|---|
| HLE | CatB | |
| BI 201335 | >30,000 | 26,000 ± 1,900 |
| Telaprevir | 680 ± 10 | 2,300 ± 900 |
| Boceprevir | 17,000 ± 1,000 | 6,200 ± 1,000 |
Fifty percent concentrations (IC50s) shown are means ± standard deviations from three separate experiments. HLE, human leukocyte elastase; CatB, cathepsin B.
Activity in cellular assays.
Activity in cell culture is one of the most important indicators of potential for in vivo efficacy and was a focus of our lead optimization program (20). In replicon assays, BI 201335 had low-nanomolar activity similar to that observed in enzymatic assays against genotypes 1a, 1b, and 2a (clone JFH1) (Table 3). BI 201335 was also tested in the genotype 2a JFH1 viral replication system, giving a similar 50% effective concentration (EC50) to that obtained in the replicon (Table 3). The shift in genotype 2a replicon potency relative to genotype 1 is similar to what was observed in enzyme assays. Despite their excellent enzymatic activity, telaprevir and boceprevir inhibited RNA replication of HCV genotype 1 replicons more weakly than they inhibited enzymatic activity. Similar EC50s for telaprevir and boceprevir against genotype 1b replicons have been reported previously (15, 22). Under our assay conditions, the observed reductions in replicon RNA were time dependent, plateauing for higher concentrations of all inhibitors at approximately 3 log units after a 72-h incubation (L. Lagacé, unpublished data). We and others have demonstrated previously that longer-term treatment with protease inhibitors in the absence of antibiotic selection can result in further reduction of RNA copy number and eventual cure of the Huh7 cells (27).
TABLE 3.
Activity of BI 201335, telaprevir, and boceprevir in subgenomic replicon, JFH1 viral replication, and cytotoxicity assays in Huh-7 cells
| Inhibitor | EC50 (nM) against HCV genotypea: |
CC50 (nM)b | |||
|---|---|---|---|---|---|
| 1a | 1b | 2a replicon | 2a virus | ||
| BI 201335 | 6.5 ± 0.9 | 3.1 ± 1.2 | 50 ± 7 | 43 ± 27 | 30,000 |
| Telaprevir | 700 ± 50 | 540 ± 30 | ND | ND | 37,000 |
| Boceprevir | 550 ± 210 | 520 ± 220 | ND | ND | >70,000 |
Fifty percent effective concentrations (EC50) values shown are means ± standard deviations from at least three independent experiments. ND, not determined.
The cytotoxic concentration of drug that reduced the viable cell number by 50% (CC50) was determined by adding MTT reagent (see Materials and Methods.
A 50% cytotoxic concentration (CC50 value) of 30 μM was obtained for BI 201335 in proliferating Huh-7 cells (Table 3), yielding a selectivity index of 4,600 relative to the genotype 1a EC50 of 6.5 nM. Similar CC50 values were obtained in stationary or proliferating Huh-7 replicon cells (25 and 23 μM, respectively). Under the same conditions, the CC50 values for telaprevir and boceprevir in proliferating Huh-7 cells (Table 3) were similar or higher, but these drugs exhibit selectivity indices of only 67 and >130, respectively, relative to their less potent activity against the genotype 1a replicon.
In vitro combination studies with interferon and ribavirin.
The inhibitory activity of pair-wise combinations of IFN-α or ribavirin with BI 201335 were evaluated using a genotype 1b replicon encoding a luciferase reporter gene. In this system, the BI 201335 EC50 was 5.4 ± 0.1 nM, whereas IFN-α and ribavirin had EC50s of 0.32 ± 0.07 IU/ml and 11 ± 5 μM, respectively. BI 201335 was mixed with IFN-α or ribavirin at different ratios, and serial dilutions of each mixture were tested. Results of two independent experiments are shown in Table 4 and in Table S2 in the supplemental material. The concentration ratios were chosen to cover a 10-fold range on either side of the ratio where both drugs would contribute equally to inhibition if their effects were purely additive. The degree of inhibition for each drug combination was evaluated according to the median effect principle using the combination index calculation (8). The effect of interferon in combination with BI 201335 was also assessed using the Bliss independence model (29). The cytotoxicity of the mixtures was also evaluated.
TABLE 4.
Combination indices for BI 201335-IFN-α and BI 201335-ribavirin drug combinations
| Drug combination and ratio | Combination index (95% confidence interval) |
||
|---|---|---|---|
| 50% inhibition | 75% inhibition | 90% inhibition | |
| BI 201335/IFN-α ratioa | |||
| 1:6 | 1.00 (0.68-1.30) | 1.09 (0.74-1.41) | 1.21 (0.82-1.57) |
| 1:12 | 0.99 (0.83-1.10) | 0.95 (0.80-1.05) | 0.94 (0.79-1.05) |
| 1:60 | 1.38 (1.22-1.54) | 1.00 (0.89-1.12) | 0.81 (0.72-0.90) |
| 1:300 | 1.53 (0.98-2.44) | 1.13 (0.72-1.80) | 0.94 (0.60-1.49) |
| 1:600 | 1.34 (1.14-1.67) | 0.95 (0.81-1.18) | 0.73 (0.62-0.91) |
| BI 201335/ribavirin ratiob | |||
| 1:220 | 0.99 (0.77-1.29) | 1.11 (0.86-1.44) | NDc |
| 1:440 | 1.14 (0.88-1.53) | 1.09 (0.84-1.46) | ND |
| 1:2,200 | 1.21 (0.99-1.52) | 0.98 (0.80-1.23) | ND |
| 1:11,000 | 0.93 (0.73-1.14) | 0.90 (0.70-1.10) | ND |
| 1:22,000 | 0.83 (0.58-1.07) | 0.97 (0.68-1.25) | ND |
The BI 201335/IFN-α ratio shows the ratio of BI 201335 concentration (micromolar) to alpha interferon (IFN-α) (in international units per millililiter). The 1:60 ratio corresponds to equipotent concentrations of the two drugs.
The BI 201335/ribavirin ratio is a molar ratio. The 1:2,200 ratio corresponds to equipotent concentrations of the two drugs.
ND, not determined due to cytotoxicity observed at the required concentrations of ribavirin.
No cytotoxicity was observed for BI 201335 or IFN-α at the concentrations used in these experiments. Ribavirin has a very low selectivity index in the cells carrying HCV replicon that were derived from Huh-7 cells, and the cytotoxicity observed with ribavirin-BI 201335 combinations was similar to that observed with the corresponding concentrations of ribavirin alone. Combination index values were calculated at the 50%, 75%, and 90% inhibition levels for the combination with IFN-α and at 50% and 75% inhibition for the ribavirin combination. Results from one experiment are shown in Table 4, and the results for two other independent experiments are shown in Table S3 in the supplemental material. Due to ribavirin cytotoxicity, the combination index values for ribavirin and BI 201335 could not be evaluated at the 90% inhibition level (8). Combinations of BI 201335 with either IFN-α or ribavirin were predominantly additive, giving combination index values between 0.8 and 1.25, with the exception of two BI 201335/IFN-α ratios evaluated at the 50% inhibition level. The 75% and 90% inhibition levels are considered to more closely reflect the clinical antiviral effect.
Analysis of data from the inhibition of HCV replicon RNA replication by combinations of BI 201335 and IFN-α according to the Bliss independence model is shown in Fig. 3 (29). This three-dimensional (3-D) plot represents deviations from expected interactions at 95% confidence and gives a horizontal plane at 0% if the interaction is purely additive, a peak above the plane for synergistic interaction, and a pit with negative value for antagonistic interaction. The residual plots illustrating the statistically significant volumes of inhibition of HCV RNA replication at 95% confidence show that only minor regions of synergy and antagonism were observed for combinations of BI 201335 and IFN-α. Thus, the interaction between BI 201335 and IFN-α did not deviate significantly from additivity as defined by this model.
FIG. 3.
3-D analysis of the inhibition of the HCV replicon RNA replication by combinations of BI 201335 and IFN-α using the MacSynergy II program. The volume of synergy and antagonism at 95% confidence were 3.9 and −0.29 nM2%. The data are indicative of additive inhibition by the combination of BI 201335 and IFN-α. Similar results were obtained in three independent experiments.
In vitro ADME.
BI 201335 demonstrated a good apparent A-to-B permeability in Caco-2 cells (Table 5), similar to its permeability in the B-to-A direction, with an efflux ratio of ∼1. In vitro liver microsome stability studies revealed low metabolic clearance of <19% of hepatic blood flow (Qh) in all species tested, including humans, with the ranking order monkey > human > dog ≈ rat (Table 5). BI 201335 was highly bound to human plasma proteins (99.6%), as determined by equilibrium dialysis.
TABLE 5.
In vitro permeability and metabolism results for BI 201335, telaprevir, and boceprevir
| Inhibitor | Caco-2 cell permeabilitya (106 cm/s) |
LM metabolic CL (% Qh) in the following animalb: |
||||
|---|---|---|---|---|---|---|
| A-to-B permeability | B-to-A permeability | Human | Rat | Monkey | Dog | |
| BI 201335 | 8.7 | 8.1 | 16.5 | <5.6 | 18.6 | <10.9 |
| Telaprevir | 4.1 | 23 | 64 | 41 | ND | ND |
| Boceprevir | 0.6 | 23 | 56 | ND | ND | ND |
A-to-B permeability, apical-to-basolateral permeability; B-to-A permeability, basolateral-to-apical permeability.
LM metabolic CL, liver microsome (LM) metabolic clearance (CL) as a percentage of hepatic blood flow (% Qh). ND, not determined.
Pharmacokinetics in animals.
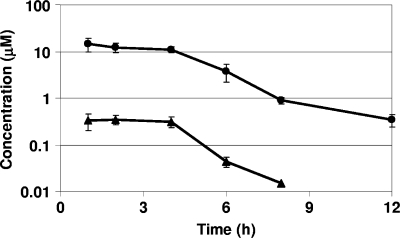
Pharmacokinetic parameters played an important role in the final stages of the lead optimization project from which BI 201335 was selected (20). BI 201335 was absorbed rapidly following a single oral dose of 5 mg/kg in rats, monkeys, and particularly in dogs, with time to maximum concentration of drug in serum (Tmax) values of 1 to 2 h (Table 6). The 0.41 μM oral maximum concentration of drug in serum (Cmax) and 1.6 μM·h area under the concentration-time curve (AUC) in rats increased to 3.8 μM and 14 μM·h, respectively, in dogs, whereas the corresponding values from monkeys were intermediate and consistent with in vivo allometry rather than the in vitro metabolic half-life trend. After oral administration to rats, BI 201335 rapidly distributed to the liver, reached a mean liver/plasma ratio of 42 within 1 h, and maintained a similar ratio over the whole sampling time of 8 h, with comparable mean retention time (MRT) values in both liver and plasma (Fig. 4).
TABLE 6.
Oral pharmacokinetic parameters for BI 201335
| Pharmacokinetic parametera | Valueb for pharmacokinetic parameter in the following animal: |
||
|---|---|---|---|
| Rat | Monkey | Dog | |
| Cmax (μM) | 0.41 | 2.0 ± 0.3 | 3.8 ± 0.3 |
| Tmax (h) | 1.5 | 2.0 ± 0.0 | 0.83 ± 0.17 |
| AUC (μM·h) | 1.55 | 8.3 ± 0.9 | 13 ± 3 |
| AUC0-∞ (μM·h) | 1.63 | 8.3 ± 0.9 | 14 ± 3 |
| MRT p.o. (h) | 3.18 | 3.7 ± 0.1 | 2.6 ± 0.3 |
Abbreviations: Cmax, maximum concentration of drug in serum; Tmax, maximum concentration of drug in serum; AUC, area under the concentration-time curve; AUC0-∞, area under the concentration-time curve from 0 h to infinity; MRT, mean retention time; p.o., per os (oral).
Values are arithmetic means ± standard errors for three males, except for rats, for which samples from three animals were pooled for analysis.
FIG. 4.
Comparative liver and plasma distribution of BI 201335 following a single oral dose of 5 mg/kg in male Sprague-Dawley rats. Liver BI 201335 levels (circles) and plasma BI 201335 levels (triangles) are shown. Values are averages based on samples from three animals analyzed separately. The error bars indicate the standard errors of the means. The lines are drawn only to aid visualization.
DISCUSSION
BI 201335 is a linear tripeptide that potently inhibits the HCV NS3-NS4A protease in enzymatic and cell-based assays. Its binding affinity is derived from highly optimized noncovalent interactions with the enzyme, rather than the covalent interaction required by inhibitors bearing α-ketoamides that react reversibly with the active site serine. In contrast with such inhibitors, which generally have a low level of selectivity for the inhibition of the NS3-NS4A protease relative to some other human proteases, the presence of a carboxylic acid as the active site binding group contributes to its good selectivity and clean off-target pharmacological profile. Unlike some other protease inhibitors, BI 201335 and other linear carboxylic acid inhibitors have very similar activities in enzymatic and cellular assays, suggesting that they efficiently enter cells to interact with the HCV replication complex (20). Although BI 201335 was optimized for activity against wild-type (WT) HCV genotype 1 enzymes, it has similarly high levels of potency against enzymes from HCV genotypes 4a, 5a, and 6a and only moderately reduced activity against proteases from HCV genotypes 2a and 3a.
We found the combination of BI 201335 with IFN-α to be additive in replicon assays. IFN-α combination studies have been published previously for telaprevir, boceprevir, and other NS3-NS4A protease inhibitors. Surprisingly, although all these drugs inhibit the replicon by the same mechanism, reported results have ranged from additive to strongly synergistic (15-17, 28, 31). The results of combination experiments are dependent on the specific drug concentrations tested and the criteria used to evaluate the results, and we believe that the different conclusions reached in these studies result in part simply from differences in experimental design. As for other HCV protease inhibitors, it will necessary to use BI 201335 in combination with IFN-α and ribavirin or with another antiviral agent to minimize emergence of resistance. We have selected BI 201335-resistant variants using the replicon system but have found that emergence of resistance is suppressed by treatment with BI 201335 in combination with IFN-α (L. Lagacé and G. Kukolj, unpublished data).
In studies performed with Caco-2 cells, BI 201335 has a good in vitro permeability in the A-to-B direction, with an apparent permeability (Papp) value similar to that observed in the B-to-A direction. This suggests that it is not subject to extensive efflux. Cross-species metabolic studies in rat, dog, monkey, and human liver microsomes demonstrated that the intrinsic clearance of BI 201335 is less than 19% Qh in all species tested. It is interesting to note that the oral Cmax and AUC following a single oral dose in animals showed a ranking order of dog> monkey > rat, which is different from the ranking order based on liver microsome metabolic clearance, but consistent with general allometry trends of metabolic organ weight and blood perfusion rates. This probably reflects the characteristics of a compound with low intrinsic clearance such that the predominant factors contributing to oral plasma exposure are absorption, distribution and/or excretion, rather than metabolism.
The target organ for inhibitors of HCV replication is the liver, and we have demonstrated that BI 201335 rapidly partitions into rat liver, reaching an equilibrium liver/plasma ratio (Kp) of 42. This high liver distribution, if maintained across species, together with the plasma drug levels observed in multiple species, suggests that it should be possible to achieve very high liver exposures in humans relative to the EC50s in HCV genotype 1a or 1b replicon assays.
New drugs for treatment of hepatitis C are eagerly awaited because they have the potential to significantly improve the clinical efficacy of the current therapy, pegylated IFN-α plus ribavirin. Very potent inhibitors that could significantly improve rates of sustained viral response (SVR) while not adding to the significant side effects of interferon and ribavirin are especially desirable. The preclinical antiviral and pharmacokinetic properties of BI 201335, coupled with appropriate evaluations in safety pharmacology and toxicology studies, were consistent with this target profile and suggested that BI 201335 represented a strong candidate for clinical trials in patients with HCV. Initial clinical trials have shown that BI 201335 monotherapy effectively reduced viral loads in HCV patients, with a median maximum viral load reduction of 4.0 log units observed at a dose of 240 mg once daily (23). In the same initial trial, a group of treatment-experienced patients (four prior partial responders and two relapsers) received 240 mg BI 201335 once daily in combination with pegylated interferon and ribavirin, and in this difficult-to-treat group, a median maximal viral load reduction of 5.3 log units was achieved, with no breakthrough resistance observed during treatment (23). These early results highlight the potential for combination therapy with BI 201335 to be highly effective in the treatment of chronic hepatitis C virus infection.
Supplementary Material
Acknowledgments
We thank C. Bousquet, M. Cartier, N. Dansereau, J. De Marte, V. Gorys, M. Jutras, D. Lamarre, N. Lapeyre, C. Lawetz, M. Marquis, R. Maurice, H. Montpetit, F. Otis, C. Pellerin, L. Pilote, M. Rhéaume, C. Spickler, and S. Zhao for their contributions to the work described in the manuscript.
Footnotes
Published ahead of print on 7 September 2010.
Supplemental material for this article may be found at http://aac.asm.org/.
REFERENCES
- 1.Artursson, P. 1990. Epithelial transport of drugs in cell culture. I. A model for studying the passive diffusion of drugs over intestinal absorptive (Caco-2) cells. J. Pharm. Sci. 79:476-482. [DOI] [PubMed] [Google Scholar]
- 2.Bartenschlager, R., L. Ahlborn-Laake, J. Mous, and H. Jacobsen. 1993. Nonstructural protein 3 of the hepatitis C virus encodes a serine-type proteinase required for cleavage at the NS3/4 and NS4/5 junctions. J. Virol. 67:3835-3844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bartenschlager, R., V. Lohmann, T. Wilkinson, and J. O. Koch. 1995. Complex formation between the NS3 serine-type proteinase of the hepatitis C virus and NS4A and its importance for polyprotein maturation. J. Virol. 69:7519-7528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blight, K. J., J. A. McKeating, and C. M. Rice. 2002. Highly permissive cell lines for subgenomic and genomic hepatitis C virus RNA replication. J. Virol. 76:13001-13014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cheng, Y., and W. H. Prusoff. 1973. Relationship between the inhibition constant (K1) and the concentration of inhibitor which causes 50 per cent inhibition (I50) of an enzymatic reaction. Biochem. Pharmacol. 22:3099-3108. [DOI] [PubMed] [Google Scholar]
- 6.Choo, Q. L., G. Kuo, A. J. Weiner, L. R. Overby, D. W. Bradley, and M. Houghton. 1989. Isolation of a cDNA clone derived from a blood-borne non-A, non-B viral hepatitis genome. Science 244:359-362. [DOI] [PubMed] [Google Scholar]
- 7.Chou, T. C. 2006. Theoretical basis, experimental design, and computerized simulation of synergism and antagonism in drug combination studies. Pharmacol. Rev. 58:621-681. [DOI] [PubMed] [Google Scholar]
- 8.Chou, T. C., and P. Talalay. 1984. Quantitative analysis of dose-effect relationships: the combined effects of multiple drugs or enzyme inhibitors. Adv. Enzyme Regul. 22:27-55. [DOI] [PubMed] [Google Scholar]
- 9.Gallinari, P., D. Brennan, C. Nardi, M. Brunetti, L. Tomei, C. Steinkuhler, and R. De Francesco. 1998. Multiple enzymatic activities associated with recombinant NS3 protein of hepatitis C virus. J. Virol. 72:6758-6769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hinrichsen, H., Y. Benhamou, H. Wedemeyer, M. Reiser, R. E. Sentjens, J. L. Calleja, X. Forns, A. Erhardt, J. Cronlein, R. L. Chaves, C. L. Yong, G. Nehmiz, and G. G. Steinmann. 2004. Short-term antiviral efficacy of BILN 2061, a hepatitis C virus serine protease inhibitor, in hepatitis C genotype 1 patients. Gastroenterology 127:1347-1355. [DOI] [PubMed] [Google Scholar]
- 11.Kim, J. L., K. A. Morgenstern, C. Lin, T. Fox, M. D. Dwyer, J. A. Landro, S. P. Chambers, W. Markland, C. A. Lepre, E. T. O'Malley, S. L. Harbeson, C. M. Rice, M. A. Murcko, P. R. Caron, and J. A. Thomson. 1996. Crystal structure of the hepatitis C virus NS3 protease domain complexed with a synthetic NS4A cofactor peptide. Cell 87:343-355. [DOI] [PubMed] [Google Scholar]
- 12.Kronenberger, B., and S. Zeuzem. 2009. Current and future treatment options for HCV. Ann. Hepatol. 8:103-112. [PubMed] [Google Scholar]
- 13.Lamarre, D., P. C. Anderson, M. Bailey, P. Beaulieu, G. Bolger, P. Bonneau, M. Bos, D. R. Cameron, M. Cartier, M. G. Cordingley, A. M. Faucher, N. Goudreau, S. H. Kawai, G. Kukolj, L. Lagacé, S. R. LaPlante, H. Narjes, M. A. Poupart, J. Rancourt, R. E. Sentjens, R. St. George, B. Simoneau, G. Steinmann, D. Thibeault, Y. S. Tsantrizos, S. M. Weldon, C. L. Yong, and M. Llinàs-Brunet. 2003. An NS3 protease inhibitor with antiviral effects in humans infected with hepatitis C virus. Nature 426:186-189. [DOI] [PubMed] [Google Scholar]
- 14.Lavanchy, D. 2009. The global burden of hepatitis C. Liver Int. 29(Suppl. 1):74-81. [DOI] [PubMed] [Google Scholar]
- 15.Lin, K., R. B. Perni, A. D. Kwong, and C. Lin. 2006. VX-950, a novel hepatitis C virus (HCV) NS3-4A protease inhibitor, exhibits potent antiviral activities in HCV replicon cells. Antimicrob. Agents Chemother. 50:1813-1822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lin, T. I., O. Lenz, G. Fanning, T. Verbinnen, F. Delouvroy, A. Scholliers, K. Vermeiren, A. Rosenquist, M. Edlund, B. Samuelsson, L. Vrang, H. de Kock, P. Wigerinck, P. Raboisson, and K. Simmen. 2009. In vitro activity and preclinical profile of TMC435350, a potent hepatitis C virus protease inhibitor. Antimicrob. Agents Chemother. 53:1377-1385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liverton, N. J., S. S. Carroll, J. DiMuzio, C. Fandozzi, D. J. Graham, D. Hazuda, M. K. Holloway, S. W. Ludmerer, J. A. McCauley, C. J. McIntyre, D. B. Olsen, M. T. Rudd, M. Stahlhut, and J. P. Vacca. 2010. MK-7009, a potent and selective inhibitor of hepatitis C virus NS3/4A protease. Antimicrob. Agents Chemother. 54:305-311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Llinàs-Brunet, M., M. Bailey, R. Deziel, G. Fazal, V. Gorys, S. Goulet, T. Halmos, R. Maurice, M. Poirier, M. A. Poupart, J. Rancourt, D. Thibeault, D. Wernic, and D. Lamarre. 1998. Studies on the C-terminal of hexapeptide inhibitors of the hepatitis C virus serine protease. Bioorg. Med. Chem. Lett. 8:2719-2724. [DOI] [PubMed] [Google Scholar]
- 19.Llinàs-Brunet, M., M. Bailey, G. Fazal, S. Goulet, T. Halmos, S. Laplante, R. Maurice, M. Poirier, M. A. Poupart, D. Thibeault, D. Wernic, and D. Lamarre. 1998. Peptide-based inhibitors of the hepatitis C virus serine protease. Bioorg. Med. Chem. Lett. 8:1713-1718. [DOI] [PubMed] [Google Scholar]
- 20.Llinàs-Brunet, M., M. D. Bailey, N. Goudreau, P. K. Bhardwaj, J. Bordeleau, M. Bos, Y. Bousquet, M. G. Cordingley, J. Duan, P. Forgione, M. Garneau, E. Ghiro, V. Gorys, S. Goulet, T. Halmos, S. H. Kawai, J. Naud, M. A. Poupart, and P. W. White. 2010. Discovery of a potent and selective noncovalent linear inhibitor of the hepatitis C virus NS3 protease (BI 201335). J. Med. Chem. 53:6466-6476. [DOI] [PubMed] [Google Scholar]
- 21.Love, R. A., H. E. Parge, J. A. Wickersham, Z. Hostomsky, N. Habuka, E. W. Moomaw, T. Adachi, and Z. Hostomska. 1996. The crystal structure of hepatitis C virus NS3 proteinase reveals a trypsin-like fold and a structural zinc binding site. Cell 87:331-342. [DOI] [PubMed] [Google Scholar]
- 22.Malcolm, B. A., R. Liu, F. Lahser, S. Agrawal, B. Belanger, N. Butkiewicz, R. Chase, F. Gheyas, A. Hart, D. Hesk, P. Ingravallo, C. Jiang, R. Kong, J. Lu, J. Pichardo, A. Prongay, A. Skelton, X. Tong, S. Venkatraman, E. Xia, V. Girijavallabhan, and F. G. Njoroge. 2006. SCH 503034, a mechanism-based inhibitor of hepatitis C virus NS3 protease, suppresses polyprotein maturation and enhances the antiviral activity of alpha interferon in replicon cells. Antimicrob. Agents Chemother. 50:1013-1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Manns, M. P., M. Bourlière, Y. Benhamou, S. Pol, M. Bonacini, C. Trepo, D. Wright, T. Berg, J. L. Calleja, P. W. White, J. O. Stern, G. Steinmann, C. L. Yong, G. Kukolj, J. Scherer, and W. O. Boecher. Potency, safety and pharmacokinetics of the NS3/4A protease inhibitor BI201335 in patients with chronic HCV genotype-1 infection. J. Hepatol., in press. [DOI] [PubMed]
- 24.Massariol, M. J., S. Zhao, M. Marquis, D. Thibeault, and P. W. White. 2010. Protease and helicase activities of hepatitis C virus genotype 4, 5, and 6 NS3-NS4A proteins. Biochem. Biophys. Res. Commun. 391:692-697. [DOI] [PubMed] [Google Scholar]
- 25.Moradpour, D., F. Penin, and C. M. Rice. 2007. Replication of hepatitis C virus. Nat. Rev. Microbiol. 5:453-463. [DOI] [PubMed] [Google Scholar]
- 26.Obach, R. S., J. G. Baxter, T. E. Liston, B. M. Silber, B. C. Jones, F. MacIntyre, D. J. Rance, and P. Wastall. 1997. The prediction of human pharmacokinetic parameters from preclinical and in vitro metabolism data. J. Pharmacol. Exp. Ther. 283:46-58. [PubMed] [Google Scholar]
- 27.Pause, A., G. Kukolj, M. Bailey, M. Brault, F. Do, T. Halmos, L. Lagacé, R. Maurice, M. Marquis, G. McKercher, C. Pellerin, L. Pilote, D. Thibeault, and D. Lamarre. 2003. An NS3 serine protease inhibitor abrogates replication of subgenomic hepatitis C virus RNA. J. Biol. Chem. 278:20374-20380. [DOI] [PubMed] [Google Scholar]
- 28.Perni, R. B., S. J. Almquist, R. A. Byrn, G. Chandorkar, P. R. Chaturvedi, L. F. Courtney, C. J. Decker, K. Dinehart, C. A. Gates, S. L. Harbeson, A. Heiser, G. Kalkeri, E. Kolaczkowski, K. Lin, Y. P. Luong, B. G. Rao, W. P. Taylor, J. A. Thomson, R. D. Tung, Y. Wei, A. D. Kwong, and C. Lin. 2006. Preclinical profile of VX-950, a potent, selective, and orally bioavailable inhibitor of hepatitis C virus NS3-4A serine protease. Antimicrob. Agents Chemother. 50:899-909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prichard, M. N., and C. Shipman, Jr. 1990. A three-dimensional model to analyze drug-drug interactions. Antiviral Res. 14:181-205. [DOI] [PubMed] [Google Scholar]
- 30.Reiser, M., H. Hinrichsen, Y. Benhamou, H. W. Reesink, H. Wedemeyer, C. Avendano, N. Riba, C. L. Yong, G. Nehmiz, and G. G. Steinmann. 2005. Antiviral efficacy of NS3-serine protease inhibitor BILN-2061 in patients with chronic genotype 2 and 3 hepatitis C. Hepatology 41:832-835. [DOI] [PubMed] [Google Scholar]
- 31.Seiwert, S. D., S. W. Andrews, Y. Jiang, V. Serebryany, H. Tan, K. Kossen, P. T. Rajagopalan, S. Misialek, S. K. Stevens, A. Stoycheva, J. Hong, S. R. Lim, X. Qin, R. Rieger, K. R. Condroski, H. Zhang, M. G. Do, C. Lemieux, G. P. Hingorani, D. P. Hartley, J. A. Josey, L. Pan, L. Beigelman, and L. M. Blatt. 2008. Preclinical characteristics of the hepatitis C virus NS3/4A protease inhibitor ITMN-191 (R7227). Antimicrob. Agents Chemother. 52:4432-4441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Simmonds, P., J. Bukh, C. Combet, G. Deleage, N. Enomoto, S. Feinstone, P. Halfon, G. Inchauspe, C. Kuiken, G. Maertens, M. Mizokami, D. G. Murphy, H. Okamoto, J. M. Pawlotsky, F. Penin, E. Sablon, I. Shin, L. J. Stuyver, H. J. Thiel, S. Viazov, A. J. Weiner, and A. Widell. 2005. Consensus proposals for a unified system of nomenclature of hepatitis C virus genotypes. Hepatology 42:962-973. [DOI] [PubMed] [Google Scholar]
- 33.Steinkuhler, C., G. Biasiol, M. Brunetti, A. Urbani, U. Koch, R. Cortese, A. Pessi, and R. De Francesco. 1998. Product inhibition of the hepatitis C virus NS3 protease. Biochemistry 37:8899-8905. [DOI] [PubMed] [Google Scholar]
- 34.Thibeault, D., C. Bousquet, R. Gingras, L. Lagacé, R. Maurice, P. W. White, and D. Lamarre. 2004. Sensitivity of NS3 serine proteases from hepatitis C virus genotypes 2 and 3 to the inhibitor BILN 2061. J. Virol. 78:7352-7359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tsantrizos, Y. S., G. Bolger, P. Bonneau, D. R. Cameron, N. Goudreau, G. Kukolj, S. R. LaPlante, M. Llinàs-Brunet, H. Nar, and D. Lamarre. 2003. Macrocyclic inhibitors of the NS3 protease as potential therapeutic agents of hepatitis C virus infection. Angew. Chem. Int. Ed. Engl. 42:1356-1360. [DOI] [PubMed] [Google Scholar]
- 36.Vaillancourt, F. H., L. Pilote, M. Cartier, J. Lippens, M. Liuzzi, R. C. Bethell, M. G. Cordingley, and G. Kukolj. 2009. Identification of a lipid kinase as a host factor involved in hepatitis C virus RNA replication. Virology 387:5-10. [DOI] [PubMed] [Google Scholar]
- 37.Venkatraman, S., S. L. Bogen, A. Arasappan, F. Bennett, K. Chen, E. Jao, Y. T. Liu, R. Lovey, S. Hendrata, Y. Huang, W. Pan, T. Parekh, P. Pinto, V. Popov, R. Pike, S. Ruan, B. Santhanam, B. Vibulbhan, W. Wu, W. Yang, J. Kong, X. Liang, J. Wong, R. Liu, N. Butkiewicz, R. Chase, A. Hart, S. Agrawal, P. Ingravallo, J. Pichardo, R. Kong, B. Baroudy, B. Malcolm, Z. Guo, A. Prongay, V. Madison, L. Broske, X. Cui, K. C. Cheng, Y. Hsieh, J. M. Brisson, D. Prelusky, W. Korfmacher, R. White, S. Bogdanowich-Knipp, A. Pavlovsky, P. Bradley, A. K. Saksena, A. Ganguly, J. Piwinski, V. Girijavallabhan, and F. G. Njoroge. 2006. Discovery of (1R,5S)-N-[3-amino-1-(cyclobutylmethyl)-2,3-dioxopropyl]-3-[2(S)-[[[(1,1-dimethylethyl)amino]carbonyl]amino]-3,3-dimethyl-1-oxobutyl]-6,6-dimethyl-3-azabicyclo[3.1.0]hexan-2(S)-carboxamide (SCH 503034), a selective, potent, orally bioavailable hepatitis C virus NS3 protease inhibitor: a potential therapeutic agent for the treatment of hepatitis C infection. J. Med. Chem. 49:6074-6086. [DOI] [PubMed] [Google Scholar]
- 38.Vita, M., M. Abdel-Rehim, C. Nilsson, Z. Hassan, P. Skansen, H. Wan, L. Meurling, and M. Hassan. 2005. Stability, pKa and plasma protein binding of roscovitine. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 821:75-80. [DOI] [PubMed] [Google Scholar]
- 39.Wakita, T., T. Pietschmann, T. Kato, T. Date, M. Miyamoto, Z. Zhao, K. Murthy, A. Habermann, H. G. Krausslich, M. Mizokami, R. Bartenschlager, and T. J. Liang. 2005. Production of infectious hepatitis C virus in tissue culture from a cloned viral genome. Nat. Med. 11:791-796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.White, P. W., M. Llinàs-Brunet, and M. Bös. 2006. Blunting the Swiss army knife of hepatitis C virus: inhibitors of NS3/4A protease. Prog. Med. Chem. 44:65-107. [DOI] [PubMed] [Google Scholar]
- 41.Yip, Y., F. Victor, J. Lamar, R. Johnson, Q. M. Wang, J. I. Glass, N. Yumibe, M. Wakulchik, J. Munroe, and S.-H. Chen. 2004. P4 and P1′ optimization of bicycloproline P2 bearing tetrapeptidyl α-ketoamides as HCV protease inhibitors. Bioorg. Med. Chem. Lett. 14:5007-5011. [DOI] [PubMed] [Google Scholar]
- 42.Zhong, J., P. Gastaminza, G. Cheng, S. Kapadia, T. Kato, D. R. Burton, S. F. Wieland, S. L. Uprichard, T. Wakita, and F. V. Chisari. 2005. Robust hepatitis C virus infection in vitro. Proc. Natl. Acad. Sci. U. S. A. 102:9294-9299. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.