Abstract
Strains of Shiga toxin-producing Escherichia coli (STEC) are a heterogeneous E. coli group that may cause severe disease in humans. STEC have been categorized into seropathotypes (SPTs) based on their phenotypic and molecular characteristics and the clinical features of the associated diseases. SPTs range from A to E, according to a decreasing rank of pathogenicity. To define the virulence gene asset (“virulome”) characterizing the highly pathogenic SPTs, we used microarray hybridization to compare the whole genomes of STEC belonging to SPTs B, C, and D with that of STEC O157 (SPT A). The presence of the open reading frames (ORFs) associated with SPTs A and B was subsequently investigated by PCR in a larger panel of STEC and in other E. coli strains. A genomic island termed OI-57 was present in SPTs A and B but not in the other SPTs. OI-57 harbors the putative virulence gene adfO, encoding a factor enhancing the adhesivity of STEC O157, and ckf, encoding a putative killing factor for the bacterial cell. PCR analyses showed that OI-57 was present in its entirety in the majority of the STEC genomes examined, indicating that it represents a stable acquisition of the positive clonal lineages. OI-57 was also present in a high proportion of the human enteropathogenic E. coli genomes assayed, suggesting that it could be involved in the attaching-and-effacing colonization of the intestinal mucosa. In conclusion, OI-57 appears to be part of the virulome of pathogenic STEC and further studies are needed to elucidate its role in the pathogenesis of STEC infections.
Shiga toxin (Stx)-producing Escherichia coli (STEC) strains cause severe human diseases such as hemorrhagic colitis and the life-threatening hemolytic uremic syndrome (HUS) (20, 32). STEC strains are zoonotic pathogens, and ruminants, particularly cattle, are recognized as their main natural reservoir (3). STEC strains may belong to a large number of serotypes, but only some of them have been firmly associated with severe human infections (20, 36). E. coli O157:H7 causes most of the cases of severe disease worldwide, but infections sustained by STEC strains belonging to serogroups other than O157, such as O26, O111, O103, O145 and O121, have been increasingly reported (2, 3, 4, 26, 33, 36, 39).
The pathogenicity of STEC mainly relies on the presence of virulence genes located on mobile genetic elements (MGEs). These include the lambdoid bacteriophages transducing the Stx-coding genes (22) and the large virulence plasmid carrying the genes governing the production of enterohemolysin (28) and other putative virulence factors. In STEC O157, this plasmid also contains toxB, a gene that encodes a protein likely involved in the colonization of the gut mucosa (30, 34). Other important virulence properties are carried by pathogenicity islands (PAIs) such as the “locus of enterocyte effacement” (LEE) (16), which governs the capability of STEC to colonize the intestinal mucosa of the host with a peculiar mechanism known as attaching-and-effacing (A/E) (16, 20). Another PAI, termed O island 122 (OI-122) in the sequence of STEC O157 strain EDL933 (24), has been frequently found in STEC strains usually associated with severe human disease (9, 11, 19). This PAI carries the large virulence gene efa1-lifA, which appears to be involved in the colonization of the intestinal mucosa and in the inhibition of the host immune response (10, 21, 31). Beside these MGEs, many horizontally acquired DNA regions carrying genes encoding putative virulence factors or proteins of unknown function have been described in the genome of the STEC strains fully or partially sequenced so far. More than 170 of these regions have been annotated as genomic islands (GIs) in the sequences of the STEC O157 strains EDL933 and RIMD0509952/VT2 Sakai (7, 25).
Due to the high genomic plasticity of E. coli, MGEs can be easily exchanged among strains or lost, generating STEC clones with different genetic assets and, as a consequence, different degrees of virulence. Karmali et al. proposed to group STEC strains into five seropathotypes (SPTs), from A through E, according to their reported frequencies in human illness, their known association with outbreaks and severe disease, and the presence of MGEs such as the LEE and the OI-122 PAI (9). SPT A includes STEC strains of serotypes O157:H7 and O157:NM, associated with both outbreaks and sporadic cases of HUS. SPT B includes STEC strains that are capable of causing HUS and outbreaks but less commonly than STEC O157, such as those belonging to serotypes O26:H11, O103:H2, O111:NM, O121:H19, and O145:NM, whereas SPT C includes strains belonging to serotypes O91:H21 and O113:H21, which lack the LEE and have sometimes been associated with HUS (9). STEC serotypes associated with diarrhea but not with HUS, and STEC strains circulating only in animal reservoirs, have been included in SPTs D and E, respectively (9). This classification scheme takes into consideration the clinical aspects of the disease as well as the molecular features reported to play a role in STEC pathogenicity. However, the molecular bases of STEC infections have not been completely understood and the whole genetic asset conferring full virulence to SPTs A and B has not yet been completely identified.
In an attempt to clarify this issue, we compared the entire genome of STEC O157 with those of STEC strains belonging to SPTs B, C, and D. This approach allowed us to identify a putative PAI (termed OI-57) in the sequence of the STEC O157 EDL933 strain (25) that was consistently present in STEC strains belonging to SPTs A and B but not in the less pathogenic SPTs C and D. The association of OI-57 with SPTs A and B was confirmed by examining a panel of STEC strains that included isolates belonging to SPTs from type A to type E as well as nonpathogenic E. coli strains.
MATERIALS AND METHODS
Bacterial strains.
All the E. coli strains used in this study were part of the culture collection of the Istituto Superiore di Sanità and have been described in reports from previous studies (17, 18, 24, 37, 38). All the strains had been isolated in Italy between 1988 and 2008. STEC O157 reference strains EDL933 and RIMD0509952/VT2 Sakai, together with E. coli K-12 strain MG1655, were also included in the study. These strains were kindly provided by Roberto La Ragione, Veterinary Laboratories Agency, Weybridge, United Kingdom.
Eighteen STEC strains were used in the microarray experiments. They belonged to (i) serogroups O26 (five strains), O111 (four strains), O103 (two strains), and O145 (two strains), as representatives of seropathotype B; (ii) serogroups O113 (two strains) and O91 (two strains), as representatives of seropathotype C; and (iii) serogroup O45 (one strain), as a representative of seropathotype D.
The PCR analyses for the validation of the microarray results were performed using a panel of 61 additional STEC strains. SPT A included nine O157 strains. SPT B strains belonged to serogroups O26 (nine strains), O111 (ten), O145 (seven), O103 (four), and O121 (two); SPT C strains belonged to serogroups O113 (nine) and O91 (four). SPTs D and E were represented by seven strains of animal origin that were negative for the presence of the intimin-coding eae gene (23) and belonged to serogroups O23, O25, O8, O73, O109, and O nontypeable (ONT).
The presence of the putative virulence gene in OI-57 was also assessed in a panel of Stx-negative E. coli isolates belonging to other pathogroups. These included 42 enteropathogenic E. coli (EPEC) isolates, nine enterotoxigenic E. coli (ETEC) isolates, eight enteroaggregative E. coli (EAEC) isolates, and eight cytotoxic necrotizing factor 1 (CNF1)-producing E. coli (NTEC) isolates. The EPEC strains were characterized as typical or atypical on the basis of the presence or the absence of the EPEC adherence factor (EAF) plasmid as described by Franke et al. (6). The ETEC strains belonged to serogroups O6, O64, and O147; the EAEC strains belonged to serogroups O86, O111, O126, and O128; and the NTEC strains belonged to serogroups O2, O6, O75, and O83.
Twenty-seven nonpathogenic E. coli isolates from the Escherichia coli Reference (ECOR) collection (23) and the K-12 LE 392 strain were also examined.
Microarray hybridizations.
The microarray slides used in this study were purchased from Ocimum Biosolutions Ltd. (Hyderabad, India). They were composed of 6,176 oligonucleotides (50-mer) representing almost all the coding genes of the three control strains. In particular, the slides were spotted with oligonucleotides specific for 4,288 open reading frames (ORFs) of E. coli K-12 strain MG1655, 5,358 ORFs of E. coli O157:H7 strain RIMD0509952, and 5,336 ORFs of E. coli O157:H7 strain EDL933.
Total DNA of the test strains was purified from overnight bacterial cultures by using a genomic DNA extraction kit (Gentra Systems) according to the manufacturer's instructions. DNA was labeled with a BioPrime DNA labeling system (InVitrogen Life Technologies, Carlsbad, CA). For a 50-μl reaction mixture, 2.5 μg of DNA was combined with 15 μg of random octamers, heated to 95°C for 5 min, and chilled in ice. The remaining components were added to achieve the final concentration as follows: 0.12 mM dATP-dGTP-dCTP, 0.06 mM dTTP, 0.02 mM Cy3 or Cy5-dUTP (Amersham Pharmacia Biotech, Little Chalfont, United Kingdom), and 40 units of the Klenow fragment of E. coli DNA polymerase. The reaction mixture was incubated at 37°C for 3 h, and the labeled DNA was purified by using a QIAquick PCR purification kit (Qiagen, Chatsworth, CA) according to the manufacturer's instructions. The DNA probe, composed of one of the test DNAs labeled with Cy3 (15 μl) and a mixture of DNA from the three control strains labeled with Cy5 (15 μl), was mixed with 15 μl of hybridization buffer (Ocimum Biosolutions Ltd., Hyderabad, India), heated to 95°C for 5 min, and chilled on ice before hybridization on the slide. The mixture of the three control DNAs was used to check the efficiency of hybridization on the whole slide surface.
Hybridizations were carried out overnight under glass coverslips in a sealed wet box at 42°C. Following hybridization, slides were washed for 2 min in 1× SSC (1× SSC is 0.15 M NaCl plus 0.015 M sodium citrate)-0.05% sodium dodecyl sulfate (SDS) at 42°C and two times for 2 min in 0.06× SSC at room temperature. Following washes, the slides were dried by centrifugation in conical 50-ml tubes.
Hybridized slides were analyzed by using a ProScanArray microarray scanner (Perkin Elmer, Downers Grove, IL). Computer analysis of images was conducted by using ScanArray software (Perkin Elmer, Downers Grove, IL) and MeV software (27). An ORF was considered present in the test DNA when the corresponding spot in the hybridized slide showed a mean fluorescence value higher than that of the background plus 2 standard deviations.
PCR validation of the microarray results.
The major differences identified by the microarray analyses were further characterized by developing PCR assays aimed at assessing the presence of the ORFs that had been detected in SPTs A and B but not in SPTs C and D. PCR primers were deployed by using the primer-BLAST tool available at NCBI website (http://www.ncbi.nlm.nih.gov/tools/primer-blast/index.cgi?LINK_LOC=BlastHome) and are listed in Table 1 .
TABLE 1.
PCR primers used in this studya
| Primer name | ORF name | ORF product | Primer sequence | Primer location (nt position) |
|---|---|---|---|---|
| Z0953 Fwd | Z0953 | Hypothetical protein | GGCTTTAACGTGCGCTAACT | 897927-897946 |
| Z0953 Rev | TCATCTTTTTCCTCGTGCATC | 898046-898026 | ||
| Z0958 Fwd | Z0958 | Unknown protein encoded by CP-933K | ATGGATTTCACCAGCAGGAT | 902731-902750 |
| Z0958 Rev | ATTCATTCTGTTCTTTCATCATCG | 902830-902807 | ||
| Z0989 Fwd | Z0989 | Unknown protein encoded by prophage CP-933K | AGAAACCTGACTTCGCCTGA | 929184-929203 |
| Z0989 Rev | CTTTTGTTGCATCCTCAGCA | 929601-929582 | ||
| Z1142 Fwd | Z1142 | Urease-associated protein UreD | TGTCGGTCTGCTCACTGTTC | 1078712-1078731 |
| Z1142 Rev | TCTCCAGACGGTTAGCGAGT | 1079115-1079096 | ||
| Z1154 Fwd | Z1154 | Putative colicin immunity protein | TCCAGTTTCTGGTGATGTTTTG | 1085954-1085975 |
| Z1154 Rev | TGGCCCTTCCTTGTTCAATA | 1086158-1086139 | ||
| Z1174 Fwd | Z1174 | Putative tellurium resistance protein TerC | TAATGTTCGCGTTTGACTCG | 1103602-1103621 |
| Z1174 Rev | CGATGCTGTAACCATGATGC | 1103838-1103819 | ||
| Z1214 Fwd | Z1214 | Hypothetical protein | CCAGTGAACATATTTCCGGC | 1139766-113978 |
| Z1214 Rev | TGGGTGAAATGAATGAGGTTT | 1139897-1139877 | ||
| Z1348 Fwd | Z1348 | Hypothetical protein | TAAAACTGCGTCTGGCTGTG | 1267374-1267393 |
| Z1348 Rev | TTCTTTTTATCACCGGCCAC | 1267514-1267495 | ||
| Z1368 Fwd | Z1368 | Hypothetical protein | AGAAGAAGTGGTGTCACGGG | 1282029-1282048 |
| Z1368 Rev | GTTATCCGCCTTCATGGTGT | 1282191-1282172 | ||
| Z1385 Fwd | Z1385 | Putative secreted protein encoded by cryptic prophage CP-933 M | TTAGGTGCCGGAGGAATATG | 1294045-1294064 |
| Z1385 Rev | AAGACCTTTGCCTGATGTGG | 1294428-1294409 | ||
| Z1611 Fwd | Z1611 | putative phage inhibition, colicin resistance and tellurite resistance protein | TGGTGTTTTATGGTCAGCCA | 1496984-1497003 |
| Z1611 Rev | TATGCTTCCATTCACGTCCA | 1497736-1497717 | ||
| Z1780 Fwd | Z1780 | Hypothetical protein | CGTGAGGCAGCACAAAACTA | 1634608-1634627 |
| Z1780 Rev | GACGCGTAATGCGTGTTCTA | 1634991-1634972 | ||
| Z1914 Fwd | Z1914 | Putative minor tail fiber protein CP-933X | TTTTGAGATGAACGGGAAGG | 1736664-1736683 |
| Z1914 Rev | TAATCTTTGTCTGTCCCCGC | 1736906-1736887 | ||
| Z2053 Fwd | adfO | Putative intestinal colonization factor | TGG TGG CCC GCA TAC AGC | 1860232-1860249 |
| Z2053 Rev | TGC CCA GTC AGC CCA GGT TA | 1860733-1860714 | ||
| Z2054 Fwd | ckf | Putative killer protein | ATG CTC GTC ACA TAT AGA TTG | 1861195-1861215 |
| Z2054 Rev | GTT CGT AAG CTG TGA AGA CA | 1861396-1861377 | ||
| Z2066 Fwd | Z2066 | Unknown protein encoded by prophage CP-933O | TAAGGCACCGGAAATCAAAC | 1867809-1867828 |
| Z2066 Rev | TGCATCAGATTCACTCTGCC | 1868228-1868209 | ||
| Z2096 Fwd | Z2096 | Unknown protein encoded within prophage CP-933O | TTCTTTGCATGCCTCTCTGA | 1886847-1886828 |
| Z2096 Rev | CGGGAACGATGAAGGTAAAA | 1886665-1886684 | ||
| Z2097 Fwd | Z2097 | Unknown protein encoded within prophage CP-933O | TTCTTTGCATGCCTCTCTGA | 1886847-1886828 |
| Z2097 Rev | CGGGAACGATGAAGGTAAAA | 1886665-1886684 | ||
| Z2098 Fwd | Z2098 | Unknown protein encoded within prophage CP-933O | GCTGAATGATTCCCATGTCA | 1887762-1887743 |
| Z2098 Rev | ACCCACGAAAGAGCAGAACA | 1887608-1887627 | ||
| Z2104 Fwd | Z2104 | Putative ARAC-type regulatory protein | CATGGTTTGCTCCCCAATTA | 1892233-1892252 |
| Z2104 Rev | CGGAATGTCAGTCAGACGAG | 1892440-1892421 | ||
| Z2105 Fwd | Z2105 | Unknown protein encoded within prophage CP-933O | CTTCAAAAAGAAAACCCGCA | 1893385-1893404 |
| Z2105 Rev | GATCTTCGCTTTCTCGGATG | 1893523-1893504 | ||
| Z2121 Fwd | Z2121 | Unknown protein encoded within prophage CP-933O | CAAGCAGCATTCTTGCAGAC | 1904821-1904840 |
| Z2121 Rev | GCTGACATGCGTAACGAGAA | 1904991-1904972 | ||
| Z2148 Fwd | Z2148 | Unknown protein encoded within prophage CP-933O | AATATTTTCCCACGTCCCGT | 1927623-1927604 |
| Z2148 Rev | GACAGGGTAATCACGCAGGT | 1927516-1927535 | ||
| Z2149 Fwd | Z2149 | Hypothetical protein | CTTTCGGACTCAGGTGAAGC | 1927995-1928014 |
| Z2149 Rev | GGTAAGCCTTCACCAACCAA | 1928224-1928205 | ||
| Z2150 Fwd | Z2150 | Unknown protein encoded by prophage CP-933R | ACCCCAGTCTCAGGTGTGTC | 2117258-2117277 |
| Z2150 Rev | CGGTGAGAGGAGGCTTACTG | 2117540-2117521 | ||
| Z2366 Fwd | Z2366 | Unknown protein encoded within prophage CP-933R | GAAGAACAGAACCCGCAGAA | 2138525-2138544 |
| Z2366 Rev | TGTCTGAACAGGTGCTCTGG | 2138730-2138711 | ||
| Z2979 Fwd | Z2979 | Putative stability/partitioning protein encoded within prophage CP-933T | CACACCACAGGAAGTGGATG | 2677781-2677800 |
| Z2979 Rev | TCCTTTTCACGAATAACCGC | 2678275-2678256 | ||
| Z3931 Fwd | Z3931 | Unknown protein encoded by prophage CP-933Y | CCGGCACAAACAATAATTCC | 3554499-3554518 |
| Z3931 Rev | AGGTGTTGATGATGTTGCCA | 3554671-3554652 | ||
| Z3933 Fwd | Z3933 | Serine/threonine protein phosphatase | GGCAAGAGCTTTAGCCAGAA | 3556023-3556042 |
| Z3933 Rev | AATCACATTCCCCTGGTTCA | 3556182-3556163 | ||
| Z4315 Fwd | Z4315 | Hypothetical protein | TGCTTCCGTTCTTATTTGCC | 3921831-3921850 |
| Z4315 Rev | GCATAAAGGATGGCGTCAAG | 3922024-3922005 | ||
| Z4325 Fwd | Z4325 | Putative enterotoxin | TATCAGGCCCTTCAAAATGG | 3929618-3929637 |
| Z4325 Rev | TATTGCCAAGTACGCCACAA | 3929831-3929812 | ||
| Z6020 Fwd | Z6020 | Hypothetical protein | CTTCCACGAGGCATTTCATT | 2281021-2281040 |
| Z6020 Rev | ACTGATGAGGTTGTCGGAGC | 2281237-228121 | ||
| Z6021 Fwd | Z6021 | Putative flagellar L-ring protein precursor | AGAAACCTGACTTCGCCTGA | 2282433-2282414 |
| Z6021 Rev | CCAGCTTTCCTCCGTGATAA | 2281605-2281624 | ||
| Z6044 Fwd | Z6044 | Putative major head protein/prohead proteinase | CTTCGCATGACTGAAGGTGA | 2304946-2304965 |
| Z6044 Rev | CTGGGAACTGATGGAGGTGT | 2305822-2305803 |
Primer locations and nomenclature of the ORFs refer to nucleotides in the sequence of STEC O157 strain EDL933 (GenBank accession no. AE005174); nt, nucleotide.
All the PCRs were performed using 50 ng of total DNA as the template, 1.5 mM MgCl2, 200 μM deoxynucleoside triphosphate, 1 μM each primer, and 1 U of Taq polymerase.
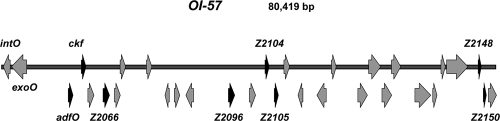
PCR detection and analysis of the OI-57 genomic island.
The presence of the OI-57 GI was investigated using primer pairs (Table 1) corresponding to the ORFs whose products were annotated with a putative function, namely, the putative virulence factor adfO and ORF Z2054, encoding a putative bacterial cell killing factor, according to the EDL933 strain sequence (GenBank accession no. AE005174). Six additional primer pairs, corresponding to as many ORFs (Z2066, Z2096, Z2104, Z2105, Z2148, and Z2150), were used to assess the integrity of the OI-57 GI (Table 1 and Fig. 1).
FIG. 1.
Map of OI-57. The ORFs investigated in this study (Table 3) are indicated. The intO gene indicates the beginning of the genomic island. The island architecture and the nomenclature of the ORFs refer to the STEC O157:H7 strain EDL933 sequence (GenBank accession no. AE005174).
RESULTS
Whole-genome comparison between STEC O157 and STEC strains belonging to SPTs B, C, and D.
Microarrays were used to compare the whole genomes of STEC strains belonging to SPTs B (13 strains), C (four strains), and D (one strain) with that of STEC O157 (SPT A). Total DNA from each of the selected 18 strains was hybridized onto commercial microarray slides containing the complete gene set of the E. coli O157:H7 strains EDL933 and RIMD0509952/VT2 Sakai and E. coli K-12 strain MG1655.
The analysis of the microarray profiles identified 87 ORFs absent in the strains belonging to SPTs C and D but giving strong hybridization signals with the SPT B strains (not shown). These ORFs represented the most evident difference between the groups studied and were selected for further investigation.
Sequence and functional analyses conducted in silico showed that some (61 out of 87) of the ORFs identified were part of E. coli metabolic pathways, part of the Stx1- or Stx2-converting phages, or part of the K-12-related Rac phage; other ORFs were part of GIs that have also been found in strains belonging to SPTs C and D. None of these ORFs were further investigated, since they were not considered potential markers of the presence of GIs specifically associated with the most pathogenic SPTs, types A and B. The remaining 26 ORFs (Table 2), located in 12 different GIs according to the sequence of the STEC O157 strain EDL933 (25), were considered genes apparently specific for SPTs A and B. To verify this possible association, their presence was further investigated in a larger panel of STEC strains belonging to different SPTs by using specific PCR assays.
TABLE 2.
PCR detection of the 26 ORFs identified by microarray analysis in STEC strains belonging to seropathotypes (SPTs) A, B, C and D/E and in nonpathogenic E. coli strains from the ECOR collectiona
| Target gene | Genomic island | No. of PCR-positive strains among seropathotype(s)/serogroup(s) (total no. tested): |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| SPT A (O157) (9) | SPT B |
SPT C |
SPT D/E (various O groups) (7) | ECOR (27) | |||||||
| O26 (9) | O111 (10) | O145 (7) | O103 (4) | O121 (2) | O113 (9) | O91 (4) | |||||
| Z0953 | OI-36 | 9 | 8 | 10 | 7 | 4 | 2 | 1 | 1 | 5 | 5 |
| Z0958 | OI-36 | 9 | 9 | 10 | 7 | 4 | 2 | 0 | 0 | 5 | 0 |
| Z0989 | OI-36 | 9 | 9 | 10 | 7 | 4 | 0 | 0 | 0 | 5 | 0 |
| Z1142 | OI-43 | 9 | 9 | 10 | 7 | 2 | 2 | 0 | 0 | 0 | 0 |
| Z1154 | OI-43 | 9 | 9 | 10 | 7 | 2 | 2 | 0 | 1 | 0 | 4 |
| Z1174 | OI-43 | 9 | 9 | 10 | 7 | 2 | 2 | 1 | 0 | 1 | 0 |
| Z1214 | OI-43 | 9 | 9 | 10 | 7 | 2 | 0 | 0 | 0 | 6 | 15 |
| Z1348 | OI-44 | 9 | 9 | 10 | 7 | 4 | 2 | 0 | 0 | 5 | 0 |
| Z1368 | OI-44 | 9 | 9 | 10 | 7 | 4 | 2 | 2 | 4 | 0 | 9 |
| Z1385 | OI-44 | 9 | 8 | 10 | 7 | 4 | 2 | 0 | 0 | 4 | 0 |
| Z1611 | OI-48 | 9 | 9 | 10 | 7 | 2 | 2 | 1 | 0 | 1 | 0 |
| Z1780 | OI-50 | 9 | 9 | 10 | 7 | 2 | 2 | 1 | 1 | 0 | 2 |
| Z1914 | OI-52 | 9 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Z2097 | OI-57 | 7 | 9 | 10 | 7 | 4 | 2 | 0 | 0 | 0 | 0 |
| Z2098 | OI-57 | 7 | 9 | 10 | 7 | 2 | 2 | 0 | 0 | 0 | 0 |
| Z2121 | OI-57 | 9 | 9 | 10 | 7 | 4 | 2 | 0 | 0 | 0 | 0 |
| Z2149 | OI-57 | 9 | 8 | 9 | 2 | 2 | 0 | 0 | 0 | 0 | 0 |
| Z2366 | OI-36 | 9 | 9 | 10 | 7 | 4 | 2 | 0 | 0 | 5 | 0 |
| Z2979 | OI-76 | 9 | 9 | 10 | 4 | 4 | 2 | 0 | 1 | 4 | 2 |
| Z3931 | OI-108 | 9 | 9 | 10 | 7 | 4 | 2 | 0 | 0 | 5 | 0 |
| Z3933 | OI-108 | 9 | 9 | 10 | 7 | 4 | 2 | 0 | 0 | 5 | 0 |
| Z4315 | OI-122 | 9 | 6 | 10 | 6 | 2 | 2 | 5 | 0 | 1 | 2 |
| Z4325 | OI-122 | 9 | 9 | 10 | 7 | 4 | 2 | 0 | 0 | 0 | 0 |
| Z6021 | OI-71 | 9 | 9 | 10 | 6 | 4 | 2 | 0 | 0 | 3 | 0 |
| Z6020 | OI-71 | 9 | 7 | 2 | 7 | 4 | 2 | 0 | 0 | 0 | 0 |
| Z6044 | OI-71 | 9 | 9 | 10 | 7 | 4 | 2 | 2 | 4 | 0 | 9 |
The number of strains tested is reported in parentheses at the corresponding serogroup heading. The nomenclature of the target genes and genomic islands refers to the sequence of STEC O157 strain EDL933 (GenBank accession no. AE005174).
PCR validation of the microarray results.
The panel included STEC strains belonging to SPTs from A to D and E and also E. coli strains from healthy human subjects included in the ECOR collection (23). The PCR primers specific for the 26 ORFs apparently associated with SPTs A and B are shown in Table 1. The results of the PCR analyses (Table 2) showed that eight ORFs, located in five different GIs according to the EDL933 strain sequence (25), were present only in strains belonging to SPTs A and B.
One of these ORFs (Z4325) was part of the OI-122 PAI, which has already been shown to be associated with SPTs A and B (9, 19). ORF Z1142 was part of the operon encoding the components of the urea metabolic pathway and related to the ureD gene from Klebsiella aerogenes. A similar operon is located on a large GI that is present in two copies (OI-43 and OI-48) in the EDL933 strain (24). OI-43 and OI-48 also contain other 4 of the 26 investigated ORFs (Z1154, Z1174, Z1214, and Z1611), which were also present in strains belonging to SPT C and SPTs D and E and in strains from the ECOR collection (Table 2).
ORF Z6020 was specific to SPTs A and B. However, it was located in OI-71 (25), which also contained the ORFs Z6044 and Z6021, frequently observed among strains belonging to SPT C and SPTs D and E, and Z6044, found in 9 of 27 ECOR collection isolates.
The remaining ORFs exclusively present in SPTs A and B were located in OI-57 (Z2097, Z2098, Z2121, and Z2149) and in OI-52 (Z1914). These GIs appeared to be specific to SPT A (OI-52) and SPTs A and B (OI-57), and in silico sequence analyses showed that both carry putative virulence genes. In particular, OI-52 harbors the genes conferring resistance to the herbicide methylviologen (Z1870) and encoding the RUS endodeoxyribonuclease (Z1873) (25). OI-57 carries adfO, a gene coding for a factor that has been shown to promote the adherence of STEC O157 to in vitro-cultured cells (8). OI-57 also carries a gene, hereby termed ckf, encoding a putative phage-associated killer protein. Paralogues of this protein have been reported to disrupt the bacterial host membranes when produced in excess (25).
Analysis of OI-57 in STEC strains.
The apparent association of OI-57 with both SPTs A and B prompted us to investigate its structure in the positive strains. These were analyzed by PCR for the presence of the above-mentioned virulence gene adfO as well as for the presence ckf and of six additional ORFs scattered along the entire GI and selected for their positions (Table 3). The presence of these eight ORFs was also investigated in STEC strains belonging to SPT C and SPTs D and E and in the ECOR strains, which had been negative for the OI-57 ORFs previously investigated. The results of the PCR assays (Table 3) indicated a strong association of the entire OI-57 with SPTs A and B. In particular, the virulence gene adfO was present, always together with ckf, in 92.7% of the strains belonging to these SPTs, while both genes were absent from STEC strains belonging to SPT C and SPTs D and E and from the nonpathogenic strains from the ECOR collection. As for the other OI-57 ORFs investigated (Fig. 1), most of them were present in the majority of the SPT A and B strains, suggesting the presence of an entire OI-57. Conversely, these ORFs were rarely observed among the SPT C strains and in ECOR collection isolates (Table 3).
TABLE 3.
PCR analysis of OI-57 in STEC strains belonging to seropathotypes (SPT) A and Ba
| ORF | Gene product | No. of positive strains (total no. tested) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| SPT A (O157) (9) | SPT B |
SPT C |
SPT D/E (various O groups) (7) | ECOR (27) | |||||||
| O26 (9) | O111 (10) | O145 (7) | O103 (4) | O121 (2) | O113 (9) | O91 (4) | |||||
| Z2053 | AdfO | 9 | 9 | 9 | 7 | 2 | 2 | 0 | 0 | 0 | 0 |
| Z2054 | Ckf | 9 | 9 | 9 | 7 | 2 | 2 | 0 | 0 | 0 | 0 |
| Z2066 | Hypothetical protein | 9 | 9 | 10 | 7 | 4 | 2 | 0 | 0 | 0 | 7 |
| Z2096 | Hypothetical protein | 7 | 9 | 10 | 7 | 4 | 2 | 0 | 0 | 0 | 0 |
| Z2104 | Putative ARAC-type regulatory protein | 9 | 9 | 10 | 7 | 4 | 2 | 0 | 0 | 0 | 2 |
| Z2105 | Hypothetical protein | 7 | 9 | 10 | 7 | 4 | 2 | 2 | 0 | 0 | 2 |
| Z2148 | Hypothetical protein | 9 | 9 | 10 | 7 | 4 | 2 | 0 | 0 | 0 | 0 |
| Z2150 | Hypothetical protein | 9 | 9 | 8 | 1 | 3 | 2 | 0 | 0 | 0 | 0 |
The target genes represented eight ORFs scattered along the entire OI-57 genomic island. STEC strains belonging to SPTs C and D/E and nonpathogenic E. coli strains from the ECOR collection were also examined. The number of strains tested is reported in parentheses at the corresponding serogroup. The nomenclature of the ORFs refers to the sequence of STEC O157 strain EDL933 (GenBank accession no. AE005174).
Presence of OI-57 in other E. coli pathogroups.
In order to verify the specificity of the association of OI-57 with STEC SPTs A and B, we investigated its presence in a set of E. coli strains belonging to other pathogroups. The E. coli isolates included 42 EPEC, 9 ETEC, 8 EAEC, and 8 NTEC strains, which were tested by PCR using primers specific for adfO and ckf (Table 1). The results of the PCR experiments (Table 4) showed that both genes were present in 71% of EPEC strains, while they could not be detected in the other E. coli pathogroups, with the exception of one EAEC strain. In particular, OI-57 was present in three of the eight typical EPEC strains and in 27 of the 34 atypical EPEC strains (Table 5).
TABLE 4.
PCR detection of OI-57 adfO and ckf genes in E. coli strains belonging to different pathogroupsa
| E. coli pathogroup (no. of strains) | No. of strains with the PCR profile | PCR amplification ofb: |
|
|---|---|---|---|
| ORF Z2053c | ORF Z2054d | ||
| EPEC (42) | 30 | + | + |
| 12 | − | − | |
| EAEC (8) | 7 | − | − |
| 1 | + | + | |
| ETEC (9) | 9 | − | − |
| NTEC (8) | 8 | − | − |
| ECOR (27) | 27 | − | − |
The nomenclature of the ORFs refers to the sequence of STEC O157 strain EDL933 (GenBank accession no. AE005174).
+, amplified; −, not amplified.
adfO, encoding the intestinal colonization factor.
ckf, encoding the cell killing factor.
TABLE 5.
Presence or absence of OI-57 in typical (EAF plasmid-positive) and atypical (EAF plasmid-negative) EPEC by serogroup
| Serogroup | No. of strains with the PCR profile/total no. of strains tested | PCR amplification ofa: |
|
|---|---|---|---|
| OI-57b | EAF | ||
| O125 | 2/3 | + | − |
| O125 | 1/3 | − | − |
| O26 | 12/12 | + | − |
| O45 | 1/1 | + | − |
| O55 | 3/4 | + | − |
| O55 | 1/4 | − | + |
| O86 | 2/2 | − | + |
| O103 | 2/2 | + | − |
| O111 | 2/4 | + | + |
| O111 | 1/4 | + | − |
| O111 | 1/4 | − | − |
| O114 | 1/1 | + | + |
| O127 | 2/5 | − | + |
| O127 | 3/5 | − | − |
| O128 | 4/6 | + | − |
| O128 | 2/6 | − | − |
| O NDc | 2/2 | + | − |
+, amplified; −, not amplified.
Positivity with respect to OI-57 implies the presence of both the adfO and ckf genes.
O ND, not determined.
Analysis of OI-57 in EPEC strains.
The structure of OI-57 in the positive EPEC strains was investigated by assessing the presence of the additional six OI-57-associated ORFs (Fig. 1). Variability higher than that observed in STEC was detected, with only 7 of the 30 OI-57-positive EPEC strains harboring the complete set of ORFs. Among the remaining strains, 10 were positive for five of the ORFs (9 for Z2066, Z2104, Z2105, Z2148, and Z2150 and 1 with ORF Z2096 instead of ORF Z2105), 7 were positive for four ORFs (4 strains possessed ORFs Z2066, Z2104, Z2148, and Z2150 and 3 strains had ORF Z2105 instead of ORF Z2150), 4 possessed ORFs Z2066, Z2104, and Z2148, and 2 strains were positive for ORF Z2148 only.
DISCUSSION
The pathogenicity of STEC represents a complex phenomenon that has not yet been fully elucidated. Human beings are exposed to a wide variety of STEC strains, which can be frequently found in animal reservoirs, in foodstuffs of animal origin, and in the environment. However, most of these strains, albeit able to produce Stx, are rarely associated with severe human disease (3), probably because they lack other virulence factors needed for full pathogenicity. Therefore, the strains pathogenic to humans appear to be a subpopulation of STEC and have been categorized into four seropathotypes (from A to D), according to serotype, relative frequencies in human disease, association with outbreaks and HUS, and other genomic features (9, 11, 12). An additional seropathotype (SPT E) includes STEC strains that seem to be confined to animal hosts (9, 11).
The introduction of the pathogenomic approach, based on the use of whole-genome high-throughput technologies, led to a deeper knowledge of the virulence characteristics of STEC strains and showed that their full pathogenicity may result from the activation of complex pathways involving the action of several virulence factors encoded by MGEs. These include the PAIs LEE (16) and OI-122 (9, 19) and the large virulence plasmids carrying the operon encoding the enterohemolysin (28). These MGEs are consistently present in STEC strains belonging to the serogroups most frequently associated with HUS and included in SPTs A and B and can undoubtedly be considered part of the genomic asset that composes the STEC “virulome.” Other factors that have been believed to play a role in STEC virulence and pathogenicity include fimbriae (29) and effectors translocated via the LEE-encoded type 3 secretion system (15, 16) or the plasmid-borne type 2 secretion system (8). However, although the data provided were in most cases conclusive, the presence of these factors has not been investigated in a large number of strains belonging to the different SPTs.
In recent years, genome sequencing projects have provided an important contribution to the characterization of the genomic arrays needed for the virulence of bacterial pathogens. Sequencing of the STEC O157 chromosome showed the presence of 177 GIs that are absent in E. coli K-12 and that, in many cases, possess the characteristics of putative PAIs (7, 25), even though their actual roles in virulence are often still unknown.
To define the genomic map of the traits characterizing the pathogenic STEC SPTs, we used microarray hybridization to compare the whole genome of STEC O157 with the genomes of a panel of STEC strains encompassing SPTs B, C, and D. The comparison identified some ORFs, located on GIs, that appeared to be associated with SPTs A and B; these were further investigated using PCR amplification and a larger panel of E. coli strains.
This approach led us to identify a GI termed OI-57 in the EDL933 strain chromosome (25) that was consistently present in STEC strains belonging to the highly pathogenic SPTs A and B but not in the less pathogenic strains of SPT C and SPTs D and E. OI-57 harbors two adjacent genes whose products are annotated with a putative function: adfO, encoding a putative virulence factor promoting the adherence of STEC O157 to HeLa cells (8), and ckf, encoding a phage-associated putative bacterial cell-killing factor (25). The latter has a paralogous protein that acts by disrupting the bacterial host membranes when produced in excess, as reported in GenBank (accession no. AE005174).
The analysis of E. coli isolates belonging to other pathogroups showed that OI-57 was also present in a high proportion of human EPEC strains belonging to the most common serogroups. EPEC strains can be classified into two subtypes (typical or atypical) according to the presence or absence of bundle-forming pili (35), which are fimbrial adhesins that represent a marker of the EAF plasmid (6). We could observe a higher rate of the presence of OI-57 in atypical EPEC (Table 5). However, due to the conflicting reports on the pathogenicity of atypical EPEC (35) and to the low number of typical EPEC strains examined, associations of OI-57 with the EPEC clones cannot be inferred.
The presence of OI-57 in EPEC strains is still interesting, since they share with STEC strains belonging to SPTs A and B an important pathogenetic mechanism: the capability to colonize the host intestinal mucosa, inducing the peculiar lesion known as “attaching and effacing” (20). This mechanism is governed by the presence of the LEE (16, 20), and the strong association of OI-57 with LEE-positive strains suggests its possible involvement in the gut colonization processes. This hypothesis is supported by experimental observations showing that the adfO gene enhanced the adhesivity of STEC O157 to in vitro-cultured cells (8) and was upregulated in STEC O157 lineages characterized by a high attack rate in outbreaks (1).
Despite the strong association of OI-57 with the most pathogenic STEC seropathotypes, we could not observe any association with a particular lineage of LEE-positive E. coli (35). This finding may reflect a general synergism between the products of the genes harbored by these two mobile genetic elements in the colonization of the host gut.
According to the hypotheses of dynamic modeling of the genomes of the pathogens (5, 14), PAIs usually assemble genes derived from plasmids and phages in cointegrated structures that are then stabilized by selective pressure through the inactivation of the mobility and recombination genes or are removed by loss of genetic material by recombination events (13). To evaluate whether OI-57 can be considered a stable acquisition of the STEC genome, we investigated its integrity by PCR amplification of eight ORFs, encompassing the length of the whole island. Our PCR analyses showed that a presumably entire OI-57 was present in the majority of the positive STEC strains examined (Table 3), thus indicating that the island represents a stable acquisition in these clonal lineages. The analysis of OI-57 integrity in EPEC, the only other E. coli pathogroup that appears to have acquired the island, showed a higher degree of variability than in STEC, with less than one-fourth of the strains showing a complete collection of the ORFs tested.
In conclusion, our results indicate that the STEC strains causing severe disease in humans and belonging to SPTs A and B possess OI-57 as part of their virulome. OI-57 could be involved in the attaching-and-effacing colonization of the intestinal mucosa and appears to be present in its entirety in the majority of the STEC strains investigated.
Further studies are needed to elucidate the roles of the putative virulence gene adfO and of ckf in the pathogenesis of STEC infections. These genes could also represent candidate targets for the development of diagnostic tools aimed at the identification of the STEC strains constituting a threat to human health among the wealth of Stx-producing strains present in animal reservoirs and in vehicles of infections.
Acknowledgments
This work was supported by European Union grant SANCO 2005/FOOD SAFETY/031 Public Health-E. coli from the EU Commission, by grant RFPS-2007-7-638803.P1 from the Italian Ministry of Health, and by grant FPI 20060054361 from Spanish Ministry of Education and Science.
We are solely responsible for the work described in this paper, and our opinions are not necessarily those of the E.U.
Editor: B. A. McCormick
Footnotes
Published ahead of print on 7 September 2010.
REFERENCES
- 1.Abu-Ali, G. S., L. M. Ouellette, S. T. Henderson, T. S. Whittam, and S. D. Manning. 2010. Differences in adherence and virulence gene expression between two outbreak strains of enterohaemorrhagic Escherichia coli O157:H7. Microbiology 156:408-419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brooks, J. T., E. G. Sowers, J. G. Wells, K. D. Greene, P. M. Griffin, R. M. Hoekstra, and N. A. Strockbine. 2005. Non-O157 Shiga toxin-producing Escherichia coli infections in the United States, 1983-2002. J. Infect. Dis. 192:1422-1429. [DOI] [PubMed] [Google Scholar]
- 3.Caprioli, A., S. Morabito, H. Brugère, and E. Oswald. 2005. Enterohaemorrhagic Escherichia coli: emerging issues on virulence and modes of transmission. Vet. Res. 36:289-311. [DOI] [PubMed] [Google Scholar]
- 4.Caprioli, A., A. E. Tozzi, G. Rizzoni, and H. Karch. 1997. Non-O157 Shiga toxin-producing Escherichia coli infections in Europe. Emerg. Infect. Dis. 3:578-579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.de la Cruz, F., and J. Davies. 2000. Horizontal gene transfer and the origin of species: lessons from bacteria. Trends Microbiol. 8:128-133. [DOI] [PubMed] [Google Scholar]
- 6.Franke, J., S. Franke, H. Schmidt, A. Schwarzkopf, L. H. Wieler, G. Baljer, L. Beutin, and H. Karch. 1994. Nucleotide sequence analysis of enteropathogenic Escherichia coli (EPEC) adherence factor probe and development of PCR for rapid detection of EPEC harbouring virulence plasmids. J. Clin. Microbiol. 32:2460-2463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hayashi, T., K. Makino, M. Ohnishi, K. Kurokawa, K. Ishii, K. Yokoyama, C. G. Han, E. Ohtsubo, K. Nakayama, T. Murata, M. Tanaka, T. Tobe, T. Iida, H. Takami, T. Honda, C. Sasakawa, N. Ogasawara, T. Yasunaga, S. Kuhara, T. Shiba, M. Hattori, and H. Shinagawa. 2001. Complete genome sequence of enterohemorrhagic Escherichia coli O157:H7 and genomic comparison with a laboratory strain K-12. DNA Res. 8:11-22. [DOI] [PubMed] [Google Scholar]
- 8.Ho, T. D., B. M. Davis, J. M. Ritchie, and M. K. Waldor. 2008. Type 2 secretion promotes enterohemorrhagic Escherichia coli adherence and intestinal colonization. Infect. Immun. 76:1858-1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karmali, M. A., M. Mascarenhas, S. Shen, K. Ziebell, S. Johnson, R. Reid-Smith, J. Isaac-Renton, C. Clark, K. Rahn, and J. B. Kaper. 2003. Association of genomic O island 122 of Escherichia coli EDL 933 with verocytotoxin-producing Escherichia coli seropathotypes that are linked to epidemic and/or serious disease. J. Clin. Microbiol. 41:4930-4940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Klapproth, J. M., I. C. Scaletsky, B. P. McNamara, L. C. Lai, C. Malstrom, S. P. James, and M. S. Donnenberg. 2000. A large toxin from pathogenic Escherichia coli strains that inhibits lymphocyte activation. Infect. Immun. 68:2148-2155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Konczy, P., K. Ziebell, M. Mascarenhas, A. Choi, C. Michaud, A. M. Kropinski, T. S. Whittam, M. Wickham, B. Finlay, and M. A. Karmali. 2008. Genomic O island 122, locus for enterocyte effacement, and the evolution of virulent verocytotoxin-producing Escherichia coli. J. Bacteriol. 190:5832-5840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kresse, A. U., I. Rienacker, A. M. Valle, H. Steinruck, H. Claus, S. M. Payne, H. Tschape, P. H. Williams, and R. Reissbrodt. 2007. Enterohaemorrhagic Escherichia coli O157 and non-O157 serovars differ in their mechanisms for iron supply. Int. J. Med. Microbiol. 297:9-15. [DOI] [PubMed] [Google Scholar]
- 13.Lawrence, J. G., and H. Ochman. 1998. Molecular archaeology of the Escherichia coli genome. Proc. Natl. Acad. Sci. U. S. A. 95:9413-9417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lederberg, J. 1997. Infectious disease as an evolutionary paradigm. Emerg. Infect. Dis. 3:417-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Loukiadis, E., R. Nobe, S. Herold, C. Tramuta, Y. Ogura, T. Ooka, S. Morabito, M. Kerouredan, H. Brugere, H. Schmidt, T. Hayashi, and E. Oswald. 2008. Distribution, functional expression, and genetic organization of Cif, a phage-encoded type III-secreted effector from enteropathogenic and enterohemorrhagic Escherichia coli. J. Bacteriol. 190:275- 285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McDaniel, T. K., and J. B. Kaper. 1997. A cloned pathogenicity island from enteropathogenic Escherichia coli confers the attaching and effacing phenotype on E. coli K-12. Mol. Microbiol. 23:399-407. [DOI] [PubMed] [Google Scholar]
- 17.Morabito, S., H. Karch, H. Schmidt, F. Minelli, P. Mariani-Kurkdjian, F. Allerberger, K. A. Bettelheim, and A. Caprioli. 1999. Molecular characterisation of verocytotoxin-producing Escherichia coli of serogroup O111 from different countries. J. Med. Microbiol. 48:891-896. [DOI] [PubMed] [Google Scholar]
- 18.Morabito, S., R. Tozzoli, A. Caprioli, H. Karch, and A. Carattoli. 2002. Detection and characterization of class 1 integrons in enterohemorrhagic Escherichia coli. Microb. Drug Resist. 8:85-91. [DOI] [PubMed] [Google Scholar]
- 19.Morabito, S., R. Tozzoli, E. Oswald, and A. Caprioli. 2003. A mosaic pathogenicity island made up of the locus of enterocyte effacement and a pathogenicity island of Escherichia coli O157:H7 is frequently present in attaching and effacing E. coli. Infect. Immun. 71:3343-3348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Nataro, J. P., and J. B. Kaper. 1998. Diarrheagenic Escherichia coli. Clin. Microbiol. Rev. 11:142-201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nicholls, L., T. H. Grant, and R. M. Robins-Browne. 2000. Identification of a novel genetic locus that is required for in vitro adhesion of a clinical isolate of enterohaemorrhagic Escherichia coli to epithelial cells. Mol. Microbiol. 35:275-288. [DOI] [PubMed] [Google Scholar]
- 22.O'Brien, A. D., J. W. Newland, S. F. Miller, R. K. Holmes, H. W. Smith, and S. B. Formal. 1984. Shiga-like toxin-converting phages from Escherichia coli strains that cause hemorrhagic colitis or infantile diarrhea. Science 226:694-696. [DOI] [PubMed] [Google Scholar]
- 23.Ochman, H., and R. K. Selander. 1984. Standard reference strains of Escherichia coli from natural populations. J. Bacteriol. 157:690-693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Oswald, E., H. Schmidt, S. Morabito, H. Karch, O. Marches, and A. Caprioli. 2000. Typing of intimin genes in human and animal enterohemorrhagic and enteropathogenic Escherichia coli: characterization of a new intimin variant. Infect. Immun. 68:64-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Perna, N. T., G. Plunkett III, V. Burland, B. Mau, J. D. Glasner, D. J. Rose, G. F. Mayhew, P. S. Evans, J. Gregor, H. A. Kirkpatrick, G. Posfai, J. Hackett, S. Klink, A. Boutin, Y. Shao, L. Miller, E. J. Grotbeck, N. W. Davis, A. Lim, E. T. Dimalanta, K. D. Potamousis, J. Apodaca, T. S. Anantharaman, J. Lin, G. Yen, D. C. Schwartz, R. A. Welch, and F. R. Blattner. 2001. Genome sequence of enterohaemorrhagic Escherichia coli O157:H7. Nature 409:529-533. [DOI] [PubMed] [Google Scholar]
- 26.Robins-Browne, R. M., and E. L. Hartland. 2002. Escherichia coli as a cause of diarrhea. J. Gastroenterol. Hepatol. 17:467-475. [DOI] [PubMed] [Google Scholar]
- 27.Saeed, A. I., V. Sharov, J. White, J. Li, W. Liang, N. Bhagabati, J. Braisted, M. Klapa, T. Currier, M. Thiagarajan, A. Sturn, M. Snuffin, A. Rezantsev, D. Popov, A. Ryltsov, E. Kostukovich, I. Borisovsky, Z. Liu, A. Vinsavich, V. Trush, and J. Quackenbush. 2003. TM4: a free, open-source system for microarray data management and analysis. Biotechniques 34:374-378. [DOI] [PubMed] [Google Scholar]
- 28.Schmidt, H., L. Beutin, and H. Karch. 1995. Molecular analysis of the plasmid-encoded hemolysin of Escherichia coli O157:H7 strain EDL 933. Infect. Immun. 63:1055-1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shen, S., M. Mascarenhas, R. Morgan, K. Rahn, and M. A. Karmali. 2005. Identification of four fimbria-encoding genomic islands that are highly specific for verocytotoxin-producing Escherichia coli serotype O157 strains. J. Clin. Microbiol. 43:3840-3850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stevens, M. P., A. J. Roe, I. Vlisidou, P. M. van Diemen, R. M. La Ragione, A. Best, M. J. Woodward, D. L. Gally, and T. S. Wallis. 2004. Mutation of toxB and a truncated version of the efa-1 gene in Escherichia coli O157:H7 influences the expression and secretion of locus of enterocyte effacement-encoded proteins but not intestinal colonization in calves or sheep. Infect. Immun. 72:5402-5411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stevens, M. P., P. M. van Diemen, G. Frankel, A. D. Phillips, and T. S. Wallis. 2002. Efa1 influences colonization of the bovine intestine by Shiga toxin-producing Escherichia coli serotypes O5 and O111. Infect. Immun. 70:5158-5166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tarr, P. I., C. A. Gordon, and W. L. Chandler. 2005. Shiga-toxin-producing Escherichia coli and haemolytic uraemic syndrome. Lancet 365:1073-1086. [DOI] [PubMed] [Google Scholar]
- 33.Tarr, C. L., T. M. Large, C. L. Moeller, D. W. Lacher, P. I. Tarr, D. W. Acheson, and T. S. Whittam. 2002. Molecular characterization of a serotype O121:H19 clone, a distinct Shiga toxin-producing clone of pathogenic Escherichia coli. Infect. Immun. 70:6853-6859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tatsuno, I., M. Horie, H. Abe, T. Miki, K. Makino, H. Shinagawa, H. Taguchi, S. Kamiya, T. Hayashi, and C. Sasakawa. 2001. toxB gene on pO157 of enterohemorrhagic Escherichia coli O157:H7 is required for full epithelial cell adherence phenotype. Infect. Immun. 69:6660-6669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tennant, S. M., M. Tauschek, K. Azzopardi, A. Bigham, V. Bennett-Wood, E. L. Hartland, W. Qi, T. S. Whittam, and R. M. Robins-Browne. 2009. Characterisation of atypical enteropathogenic E. coli strains of clinical origin. BMC Microbiol. 9:117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tozzi, A. E., A. Caprioli, F. Minelli, A. Gianviti, L. De Petris, A. Edefonti, G. Montini, A. Ferretti, T. De Palo, M. Gaido, and G. Rizzoni. 2003. Shiga toxin-producing Escherichia coli infections associated with hemolytic uremic syndrome, Italy, 1988-2000. Emerg. Infect. Dis. 9:106-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Tozzoli, R., A. Caprioli, S. Cappannella, V. Michelacci, M. L. Marziano, and S. Morabito. 2010. Production of the subtilase AB5 cytotoxin by Shiga toxin-negative Escherichia coli. J. Clin. Microbiol. 48:178-183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Tozzoli, R., A. Caprioli, and S. Morabito. 2005. Detection of toxB, a plasmid virulence gene of Escherichia coli O157, in enterohemorrhagic and enteropathogenic E. coli. J. Clin. Microbiol. 43:4052-4056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.World Health Organization. 1999. Zoonotic non-O157 Shiga toxin-producing Escherichia coli (STEC). Report of a WHO scientific working group meeting. World Health Organization, Geneva, Switzerland.