Abstract
Compared to students attending regular high schools, alternative high schools (AHS) students are more likely to be racial/ethnic minorities, have higher levels of poverty, and higher rates of risky and poor health behaviors, including weight-related behaviors, such as limited fruit/vegetable intake. However, little is known about fruit/vegetable intake among AHS students. This study examined whether perceived barriers to healthy eating mediated association between self-efficacy to eat healthy foods and fruit/vegetable consumption among AHS students. The cross-sectional study population consisted of students (n=145) attending 6 alternative high schools in the St. Paul/Minneapolis, MN area who were participants in an obesity prevention pilot study and completed a baseline survey in Fall 2006. Mixed model linear regression, adjusting for sociodemographic characteristics was used to test a series of regression models performed according to mediation analysis procedures. Students' mean age was 17.3 years, 52% were male, 63% were low-income, and 61% were from racial/ethnic minorities. Students reported a mean fruit/vegetable intake of 3.6 servings per day, mean self-efficacy to eat healthy score of 22.2 (range 3-35), and mean barriers to eating healthy score of 6.9 (range 3-13). Perceived barriers to healthy eating fully mediated the relationship between self-efficacy and fruit/vegetable consumption (Sobel test statistic=2.7, p=0.007). Interventions targeting the dietary practices of AHS students should include components to decrease perceived barriers as a way to increase self-efficacy and ultimately fruit/vegetable intake.
Keywords: fruit and vegetable consumption, adolescents, alternative high schools, mediation analysis
Introduction
Increasing fruit and vegetable consumption has been identified as a major public health priority (1, 2). Among adolescents, most do not consume the recommended nine servings of fruit/vegetables per day (2, 3). Studies indicate that some groups of youth may be at greater risk for lower fruit/vegetable intake. For example, older youth report consuming fewer fruits/vegetables than younger youth (3, 4). Studies also support a positive association between income and fruit/vegetable intake with low-income youth consuming fewer fruit/vegetables than their higher income counterparts (5, 6). The association with race/ethnicity is less consistent (3-4, 7-8).
Reaching low-income, minority adolescents with positive nutrition messages is important as these young people are more at risk for obesity and related chronic disease (1). However, gaining access to this population of young people can be challenging (9). Alternative high schools are educational settings for students at risk for drop-out from traditional schools due to problems such as truancy, teen pregnancy, and behavioral problems (10, 11). Alternative schools provide access to youth who are more likely to be older, racial/ethnic minorities, have higher levels of poverty, and higher rates of risky health behaviors that include less healthy dietary practices (10-16). Yet little is known about factors that might contribute to improving the dietary behaviors of students.
The purpose of the current study was to enhance understanding of factors associated with fruit/vegetable consumption among adolescents attending alternative high schools. Guided by Social Cognitive Theory (17, 18), it was hypothesized that perceived barriers to healthy eating (socio-environmental factor) would mediate the association between self-efficacy (personal factor) and fruit/vegetable consumption (behavior). Several studies have assessed adolescents' food choices (7, 19), correlates to food selections, including self-efficacy (20, 21), and barriers to healthy eating (22, 23). However, few studies have assessed possible pathways that may contribute to behavior change (24). Mediation models can provide a means to improve understanding of behavioral pathways (25, 26).
Methods
Study design
The current study was a cross-sectional secondary analysis of baseline data obtained from the Team COOL (Controlling Overweight and Obesity for Life) pilot study. This group randomized school-based nutrition and physical activity intervention was conducted with a convenience sample of four urban and two suburban alternative high schools in Minneapolis-St. Paul, Minnesota (16). Across the six schools, the average enrollment was 102 students (range: 27-142 students), mean age was 17 years (range: 14-20 years), 52% were male, 64% racial/ethnic minorities (range 31-96%), and 60.5% qualified for free/reduced school meal programs (range: 40-96%).
In Fall 2006, prior to randomization, all students enrolled in study schools were invited to complete a survey. Informed consent was obtained from participants 18 years and older, while those less than 18 years provided signed parental consent and individual assent. The self-administered 76-item survey was completed by 145 students and took approximately 30 to 40 minutes to complete. Details regarding survey measures have been previously published (16). Participants received a $5 gift card for completing the survey and height/weight measures. The University of Minnesota Institutional Review Board reviewed and approved the study.
Students attending alternative high schools have lower attendance rates than traditional school students (10-12). The study participation rate was therefore calculated by multiplying the school's 2006-2007 enrollment by the school's 2005-2006 attendance rate (15,16, 27). The adjusted participation rate across the six schools for the baseline survey was 36% (Range: 18%-100%).
Measures
Dependent variable
Fruit/vegetable consumption was assessed using a previously validated six-item fruit and vegetable screener (28), which assesses past-year consumption: Students were asked “Think about your usual eating habits over the past year. About how often do you eat each of the following foods and beverages?: (a) 100% Juice, (b) fruit (not including juice), (c) green salad (d) potatoes (not including French fries, fried potatoes, and potato chips), (e) carrots, (f) vegetables (not including carrots, potatoes or salad).” Response categories ranged from less than once a week to five or more times per day. Similar to other studies, data were recoded as daily servings of fruits/vegetables and summed (15, 29). Cronbach's α for the study sample was 0.85. Responses were considered outliers and excluded if they were greater than three standard deviations above the mean (n=2) (15).
Independent variables
Perceived barriers to healthy eating was assessed with a three-item scale used previously with adolescents and found to be reliable (30). Students responded to the question “How strongly do you agree with the following statements: (a) I am too busy to eat healthy foods, (b) Healthy foods cost too much, and (c) Eating healthy just takes too much time. Response categories ranged from strongly agree to strongly disagree on a five-point Likert scale. Responses were summed, with higher score indicating more barriers. Cronbach's α for the study sample was 0.82.
Self-efficacy to eat healthy was assessed with a seven-item scale (31). Participants were asked the following question: “How confident are you that you could change or maintain your eating patterns to: (a) Eat at least two servings of fruit, (b) Eat at least three servings of vegetables (not including fried potatoes), (c) Limit the soda pop you drink, (d) Limit how often you eat at fast food restaurants, (e) Limit between meal snacks, (f) Limit the portion sizes of the food you eat, and (g) Eat breakfast on most days.” Response categories ranged from not at all confident to very confident on a five-point Likert scale and were summed, with a higher score indicating greater confidence. This question has been shown to be reliable in other studies with adolescents (31). Cronbach's α for the study sample was 0.84.
Socio-demographic variables
Gender and age were determined using school records. Race/ethnicity was measured with the item “Do you think of yourself as American Indian/Alaskan; Asian; Black or African American; Hispanic/Latino; White; Other.” Due to small samples within several of the racial/ethnic groups, the “Other” category was recoded to include the following groups: American Indian/Alaskan (1%); Asian (6%); Hispanic/Latino (9%); multiethnic non-Hispanic (10%); other (3%). Socioeconomic status was assessed with the question: “Do you get free/low-cost lunches at school?” Students who reported having received free/reduced lunch were categorized as low income. If students did not respond to this question (n=8), but responded yes to participating in federal nutrition assistance programs, they were categorized as low-income.
Statistical analyses
Descriptive statistics were calculated for demographic and other key variables. A series of four regression models were performed according to mediation analysis procedures (25, 26). Each regression model was tested using mixed model multivariate linear regression, accounting for the study's nested design and intra class correlation. All regression models were adjusted for gender, race/ethnicity, age, and socio-economic status. All analyses were conducted using SAS statistical software (version 9.1, 2003, SAS Institute, Carey, NC). The Sobel Test, a statistic that verifies the results of a mediation model, was used to evaluate for statistical significance (32, 33).
Results and Discussion
Among student participants, 52% were male; 63% were low income; and 61% were racial/ethnic minorities. For demographic and other key variables, there were no significant differences by gender. Participants reported a mean fruit/vegetable consumption of 3.6 servings per day (range: 0-24; Table 1).
Table 1. Key characteristics of alternative high school student participants (N=145), stratified by gender, residing in Minneapolis/St Paul, MN, 2006.
| Total sample N=145 |
Males n(%) 76 (52%) |
Females n(%) 69 (48%) |
p-value | |
|---|---|---|---|---|
| Age (years) | ||||
| Mean (SDa) | 17.3 (1.2) | 17.4 (1.2) | 17.1 (1.2) | 0.06 |
| Range | 14.1- 19.8 | 14.1-19.8 | 14.1-19.2 | |
| Socioeconomic status b | ||||
| Low: n(%) | 91 (63.6%) | 46 (62.2%) | 45 (65.2%) | 0.70 |
| Ethnic group | ||||
| White: n(%) | 57 (39.3%) | 28 (36.8%) | 29 (42.0%) | 0.76 |
| Black / African American:n(%) | 46 (31.7%) | 26 (34.2%) | 20 (29.0%) | |
| Other/Hispanic: n(%) | 42 (29.0%) | 22 (29.0%) | 20 (29.0%) | |
| Perceived barriers to healthy eating c | ||||
| Mean score (SD) | 6.9 (2.4) | 6.9 (2.5) | 6.8 (2.3) | 0.94 |
| Range | 3-13 | 3-13 | 3-13 | |
| Self-efficacy to eat healthy c | ||||
| Mean score (SD) | 22.2 (6.5) | 22.6 (6.7) | 21.8 (6.3) | 0.42 |
| Range | 7-35 | 7-35 | 7-35 | |
| Fruit and vegetable servings per dayd | ||||
| Mean (SD) | 3.6 (4.2) | 3.6 (4.3) | 3.6 (4.1) | 0.92 |
| Range | 0-24 | 0-19.5 | 0-24 | |
| Five or more fruit and vegetable servings per dayd | ||||
| n (%) | 33 (23.1) | 16 (21.3) | 17 (25) | 0.60 |
SD=Standard Deviation
Socioeconomic status was reported as high or low based on participation in free/reduced lunch program or other federal nutrition assistance programs. Students who reported having received free/reduced lunch were categorized as low income. If students did not respond to this question (n=8), but responded yes to participating in a federal nutrition assistance programs, they were categorized as low-income.
Total n varies due to missing data.
Two outliers were excluded from the analysis due to responses greater than three standard deviations from the median.
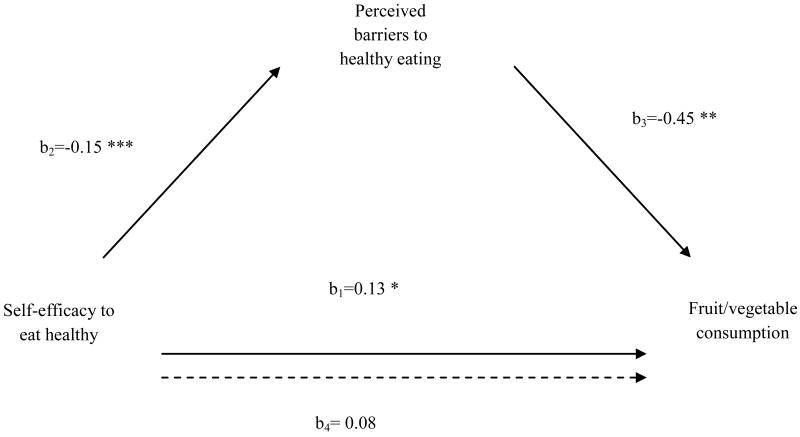
Figure 1 depicts results of the mediation analyses. In the first regression model, self-efficacy to eat healthy was found to be significantly and positively associated with fruit/vegetable consumption (b1=0.13 p=0.026). In regression model two, the association between self-efficacy to eat healthy and perceived barriers to healthy eating was found to be significantly and negatively associated (b2=-0.15 p<0.001). The third regression model found that perceived barriers to healthy eating and fruit/vegetable consumption were significantly and negatively associated (b3=-0.45 p=0.002). Finally, when self-efficacy to eat healthy and perceived barriers to healthy eating were included in the same model, the association between self-efficacy and fruit/vegetable consumption was no longer significant (b4= 0.08, p=0.15), fulfilling the requirements for full mediation. The Sobel Test confirmed that perceived barriers fully mediated the association between self-efficacy and fruit/vegetable consumption (Sobel test statistic =2.7, p=0.007). Students in the study sample reporting higher self-efficacy had fewer perceived barriers and higher fruit/vegetable intake.
Figure 1. Mediation analysis assessing the relationship of self-efficacy to eat healthy and perceived barriers to health eating and fruit and vegetable consumption among participants.
b1= association between self-efficacy to eat healthy and fruit and vegetable consumption
b2= association between self-efficacy to eat healthy and perceived barriers to healthy eating
b3= association between perceived barriers to healthy eating and fruit and vegetable consumption
b4= (mediation test) association between self-efficacy to eat healthy and fruit and vegetable consumption, with barriers to healthy eating included in the model
Statistical significance is indicated by the following: *=p<0.05; **= p<0.01; ***=p<0.001
Other studies that have examined the association between self-efficacy and barriers to fruit/vegetable consumption have reported similar results (6, 34, 35). Previous studies have identified self-efficacy as a strong correlate of fruit/vegetable consumption across the lifespan (35, 36). In a recent review of the literature, Brug and colleagues found that positive self-efficacy to eat fruits/vegetables was significantly associated with daily fruit/vegetable intake among a sample of preadolescents (37). The current study investigated a more complex pathway via mediation as a means to explain the association between self-efficacy and fruit/vegetable intake.
Barriers to eating healthy as an important driver of adolescent fruit/vegetable consumption is supported by current literature. In a study of over 3800 adolescents, Lytle and colleagues reported that the greater the perceived barriers, the fewer fruits/vegetables consumed (38). Focus group research conducted among alternative high school students in Minnesota (39) found that perceived barriers, especially barriers related to access was an impediment to regular fruit/vegetable consumption. Adolescents felt that if fruits/vegetables were more readily available in their environment, such as in vending machines at school or on the table at home, they would be more likely to consume them. Other work conducted in alternative high schools highlighted that participation in school lunch programs was low due to “cold, unappealing meals.” At the same time, vending machines were well-stocked with salty, sugary snacks and beverages (40). Improving access to fruits/vegetables at school will be an important obesity prevention strategy. When environmental supports are in place, healthy choice becomes possible and self-efficacy has the opportunity to improve.
The majority of the study sample was low-income. Research also indicates that low-income students have greater barriers to fresh fruits/vegetables (41). Often, low-income families have to make the choice of spending their food dollar on inexpensive, calorie-dense foods rather than fruits/vegetables in order to make food stretch through the month (5, 22-24, 41). It has been demonstrated that if barriers such as price are removed, fruit/vegetable consumption increases (42, 43). For example, in a school-based intervention, it was found that pricing strategies to lower the cost of fruits and vegetables increased fruit/vegetable consumption for high school youth (43). The current findings suggest that the removal of price barriers may enhance students' self-efficacy to eat more healthfully and result in increase consumption of fruits/vegetables.
There are strengths and limitations to this study. To our knowledge, this is the first study to examine perceived barriers to healthy eating as a mediator of the association between self-efficacy to eat healthy and fruit/vegetable consumption, providing important information on the health behaviors of alternative high school students. Reliable measures were used to assess variables of interest. Given the nature of self-reported data, there was also potential for social desirability bias, such as overestimating fruit/vegetable intake (44, 45). Although the response rate is considered low, the study sample was representative of students attending the study schools, and similar to data describing students attending alternative high schools nationwide (11-14). Because only schools in the Minneapolis-St Paul area were included, the generalizability of study findings may be limited. Further, the small sample size may have limited the ability to detect significant differences in certain variables, such as race/ethnicity. As a cross-sectional study, the findings described are preliminary and cannot address causality. However, the mediation analysis did produce expected results, which supports further testing of the hypothesis in longitudinal and intervention studies.
Conclusions
There is an ongoing need for dietitians and other health professionals to promote increased consumption of fruits/vegetables among school-aged youth. Data indicate that students attending alternative high schools, a population of older youth, who are disproportionately low-income, minority and at an increased risk for overweight/obesity, may require additional support. The current study suggests that by addressing perceived barriers to healthy eating among students, self-efficacy to choose healthy foods may improve and fruit/vegetable consumption may increase. Further study is needed in alternative high schools in order to improve our understanding of the dietary behaviors of diverse youth and to help guide interventions that aim to meet the needs of this population.
Acknowledgments
The authors thank the school staff and students who participated in the Team COOL pilot study.
This research was supported by a grant from the National Institutes of Health/National Institute of Diabetes and Digestive and Kidney Diseases no. R21DK072948.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Meg Bruening, Nutrition PhD Student, Maternal Child Health Nutrition Trainee, Division of Epidemiology and Community Health, University of Minnesota, 1300 South Second Street, Suite 300, Minneapolis, MN 55454, Tel: 612.626.8984, Fax: 612.624.0315.
Martha Y. Kubik, Email: kubik002@umn.edu, Associate Professor School of Nursing, University of Minnesota, 6101 Weaver Densford Hall, 308 Harvard St SE, Minneapolis, MN 55455, Tel: 612.625.0606, Fax: 612.625.7091.
DenYelle Kenyon, Email: kenyond@sanfordhealth.org, Assistant Scientist, Health Disparities Research Center, Sanford Research/USD, 900 W. Delaware St., Sioux Falls, SD 57104, Tel: 605-328-0408, Fax: 605-328-0401.
Cynthia Davey, Email: davey002@umn.edu, Senior Research Fellow, Biostatistical Design and Analysis Center, Clinical and Translational Science Institute, Academic Health Center, University of Minnesota, 717 Delaware St. SE, 223-21, Minneapolis, MN 55414, Tel: 612.624.7656, Fax: 612.625.2695.
Mary Story, Email: story001@umn.edu, Professor, Division of Epidemiology and Community Health, University of Minnesota, 1300 South Second Street, Suite 300, Minneapolis, MN 55454, Tel: 612.626.8801, Fax: 612.624.0315.
References
- 1.The US Department of Health and Human Services. Healthy People 2010. second. II. Washington: US Government Printing Office; 2005. Nutrition and overweight. [Google Scholar]
- 2.The US Department of Health and Human Services and US Department of Agriculture. Dietary Guidelines for Americans 2005. 6th. Washington: US Government Printing Office; 2005. [Google Scholar]
- 3.Centers for Disease Control and Prevention. Youth risk behavior surveillance —United States, 2007. MMWR CDC Surveill Summ. 2008;57(SS-4) [Google Scholar]
- 4.Larson NI, Neumark-Sztainer DR, Harnack LJ, Wall MM, Story MT, Eisenberg ME. Fruit and vegetable intake correlates during the transition to young adulthood. Am J Prev Med. 2008;35(1):33–37. doi: 10.1016/j.amepre.2008.03.019. [DOI] [PubMed] [Google Scholar]
- 5.Drewnowski A, Specter SE. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79(1):6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- 6.Zabinski MF, Daly T, Norman GJ, Rupp JW, Calfas KJ, Sallis JF, Patrick K. Psychosocial correlates of fruit, vegetable, and dietary fat intake among adolescent boys and girls. J Am Diet Assoc. 2006;106(6):814–21. doi: 10.1016/j.jada.2006.03.014. [DOI] [PubMed] [Google Scholar]
- 7.Langevin DD, Kwiatkowski C, McKay MG, Maillet JO, Touger-Decker R, Smith JK, Perlman A. Evaluation of diet quality and weight status of children from a low socioeconomic urban environment supports “at risk” classification. J Am Diet Assoc. 2007;107(11):1973–7. doi: 10.1016/j.jada.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 8.Striegel-Moore RH, Thompson DR, Affenito SG, Franko DL, Barton BA, Schreiber GB, Daniels SR, Schmidt M, Crawford PB. Fruit and vegetable intake: Few adolescent girls meet national guidelines. Prev Med. 2006;42(3):223–8. doi: 10.1016/j.ypmed.2005.11.018. [DOI] [PubMed] [Google Scholar]
- 9.Gryder SD. Reaching out: what's blocking the way? School Foodservice & Nutrition. 1999;53(6):58–59. 62, 64. [Google Scholar]
- 10.Kleiner B, Porch R, Farris E. Public alternative schools and programs for students at risk of education failure: 2000-01. Ed Stat Quarterly. 2002 [Google Scholar]
- 11.National Center for Education Statistics. Numbers and Types of Public Elementary and Secondary Schools from the Common Core of Data: School Year 2006–07. [May 13, 2009]; Available at: http://www.eric.ed.gov/ERICWebPortal/custom/portlets/recordDetails/detailmini.jsp?_nfpb=true&_&ERICExtSearch_SearchValue_0=ED503068&ERICExtSearch_SearchType_0=no&accno=ED503068. Published October, 2008. Updated May 13, 2009.
- 12.Lehr CA, Moreau RA, Lange CM, Lanners EJ. Minneapolis, MN: University of Minnesota, Institute on Community Integration; [May 13, 2009]. Alternative Schools, Findings from a National Survey of the States. Available at: http://ici.umn.edu/alternativeschools/publications/. Published October, 2004. Updated September 25, 2007. [Google Scholar]
- 13.Grunbaum JA, Lowry R, Kann L. Prevalence of health-related behaviors among alternative high school students as compared with students attending regular high schools. J Adolesc Health. 2001;29(5):337–43. doi: 10.1016/s1054-139x(01)00304-4. [DOI] [PubMed] [Google Scholar]
- 14.Grunbaum JA, Kann L, Kinchen SA, Ross JG, Gowda VR, Collins JL, Kolbe LJ. Youth Risk Behavior Surveillance--National Alternative High School Youth Risk Behavior Survey, United States, 1998. MMWR CDC Surveill Summ. 1999;48(7):4. 1–44. [PubMed] [Google Scholar]
- 15.Arcan C, Kubik MY, Fulkerson JA, Story M. Sociodemographic differences in selected eating practices among alternative high school students. J Am Diet Assoc. 2009;109(5):823–9. doi: 10.1016/j.jada.2009.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kubik MY, Davey C, Fulkerson JA, Sirard J, Story M, Arcan C. Alternative high school students: prevalence and correlates of overweight. Am J Health Behav. 2009;33(5):600–9. doi: 10.5993/ajhb.33.5.13. [DOI] [PubMed] [Google Scholar]
- 17.Bandura A. Social cognitive theory. In: Vasta R, editor. Annals of child development. Vol. 6. 1989. pp. 1–60. [Google Scholar]
- 18.Baranowski T, Perry C, Parcel GS. How individuals, environments, and health behavior interact: Social Cognitive Theory. In: Glanz K, Rimer BK, Lewis FM, editors. Health Behavior and Health Education: Theory, Research, and Practice. 3rd. San Francisco, CA: Jossey-Bass; 2002. pp. 165–184. [Google Scholar]
- 19.Contento IR, Williams SS, Michela JL, Franklin AB. Understanding the food choice process of adolescents in the context of family and friends. J Adolesc Health. 2006;38(5):575–82. doi: 10.1016/j.jadohealth.2005.05.025. [DOI] [PubMed] [Google Scholar]
- 20.Neumark-Sztainer D, Story M, Resnick MD, Blum RW. Correlates of inadequate fruit and vegetable consumption among adolescents. Prev Med. 1996;25(5):497–505. doi: 10.1006/pmed.1996.0082. [DOI] [PubMed] [Google Scholar]
- 21.Baranowski T, Watson K, Missaghian M, Broadfoot A, Cullen K, Nicklas T, Fisher J, Baranowski J, O'Donnell S. Social support is a primary influence on home fruit, 100% juice, and vegetable availability. J Am Diet Assoc. 2008;108(7):1231–5. doi: 10.1016/j.jada.2008.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stevenson C, Doherty G, Barnett J, Muldoon OT, Trew K. Adolescents' views of food and eating: identifying barriers to healthy eating. J Adolesc. 2007;30(3):417–34. doi: 10.1016/j.adolescence.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 23.Evans AE, Wilson DK, Buck J, Torbett H, Williams J. Outcome expectations, barriers, and strategies for healthful eating: a perspective from adolescents from low-income families. Fam Community Health. 2006;29(1):17–27. doi: 10.1097/00003727-200601000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Yeh MC, Ickes SB, Lowenstein LM, Shuval K, Ammerman AS, Farris R, Katz DL. Understanding barriers and facilitators of fruit and vegetable consumption among a diverse multi-ethnic population in the USA. Health Promot Int. 2008;23(1):42–51. doi: 10.1093/heapro/dam044. [DOI] [PubMed] [Google Scholar]
- 25.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J of Person and Soc Psych. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 26.MacKinnon DP, Krull JL, Lockwood CM. Equivalence of the mediation, confounding and suppression effect. Prev Sci. 2000;1(4):173–81. doi: 10.1023/a:1026595011371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Minnesota Department of Education. 2005-2006 attendance rates by school. [March 20, 2009]; Minnesota Department of Education Web site. http://education.state.mn.us/MDE/Data/Data_Downloads/Student/Attendance/index.html.
- 28.Field AE, Colditz GA, Fox MK, Byers T, Serdula M, Bosch RJ, Peterson KE. Comparison of 4 questionnaires for assessment of fruit and vegetable intake. Am J Public Health. 1998;88:1216–1218. doi: 10.2105/ajph.88.8.1216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thompson FE, Kipnis V, Subar AF, Krebs-Smith SM, Kahle LL, Midthune D, Potischman N, Schatzkin A. Evaluation of 2 brief instruments and a food-frequency questionnaire to estimate daily number of servings of fruit and vegetables. Am J Clin Nutr. 2000;71(6):1503–10. doi: 10.1093/ajcn/71.6.1503. [DOI] [PubMed] [Google Scholar]
- 30.French SA, Story M, Neumark-Stzainer D, Fulkerson JA, Hannan P. Fast food restaurant use among adolescents: associations with nutrient intake, food choice and behavioral and psychosocial variables. Int J Obes Relat Metab Disord. 2001;25(12):1823–1833. doi: 10.1038/sj.ijo.0801820. [DOI] [PubMed] [Google Scholar]
- 31.Custasis DC, Shannon BM. Influences on adolescent eating behavior. J Adolesc Health. 1996;18(1):27–34. doi: 10.1016/1054-139X(95)00125-C. [DOI] [PubMed] [Google Scholar]
- 32.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociological Methodology. 1982:290–312. [Google Scholar]
- 33.Preacher KJ, Leonardelli Gl. Calculation for the Sobel Test. [April 18, 2008]; University of Kansas Interactive Mediation Website. Available at: http://people.ku.edu/∼preacher/sobel/sobel.htm. Published March, 2003. Updated August 10, 2006.
- 34.Rasmussen M, Krølner R, Klepp KI, Lytle L, Brug J, Bere E, Due P. Determinants of fruit and vegetable consumption among children and adolescents: a review of the literature. Part I: Quantitative studies. Int J Behav Nutr Phys Act. 2006;11:3–22. doi: 10.1186/1479-5868-3-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gallaway MS, Jago R, Baranowski T, Baranowski JC, Diamond PM. Psychosocial and demographic predictors of fruit, juice and vegetable consumption among 11-14-year-old Boy Scouts. Public Health Nutr. 2007;10(12):1508–14. doi: 10.1017/S1368980007000742. [DOI] [PubMed] [Google Scholar]
- 36.Granner ML, Sargent RG, Calderon KS, Hussey JR, Evans AE, Watkins KW. Factors of fruit and vegetable intake by race, gender, and age among young adolescents. J Nutr Educ Behav. 2004;36(4):173–80. doi: 10.1016/s1499-4046(06)60231-5. [DOI] [PubMed] [Google Scholar]
- 37.Brug J. Determinants of healthy eating: motivation, abilities and environmental opportunities. Fam Pract. 2008;25(1):i50–5. doi: 10.1093/fampra/cmn063. [DOI] [PubMed] [Google Scholar]
- 38.Lytle LA, Varnell S, Murray DM, Story M, Perry C, Birnbaum AS, Kubik MY. Predicting adolescents' intake of fruits and vegetables. J Nutr Educ Behav. 2003;35(4):170–5. doi: 10.1016/s1499-4046(06)60331-x. [DOI] [PubMed] [Google Scholar]
- 39.Kubik MY, Lytle L, Fulkerson JA. Physical activity, dietary practices, and other health behaviors of at-risk youth attending alternative high schools. J Sch Health. 2004;74(4):119–24. doi: 10.1111/j.1746-1561.2004.tb06613.x. [DOI] [PubMed] [Google Scholar]
- 40.Kubik MY, Lytle L, Fulkerson JA. Fruits, vegetables, and football: findings from focus groups with alternative high school students regarding eating and physical activity. J Adolesc Health. 2005;36(6):494–500. doi: 10.1016/j.jadohealth.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 41.Neumark-Sztainer D, Wall M, Perry C, Story M. Correlates of fruit and vegetable intake among adolescents. Findings from Project EAT. Prev Med. 2003;37(3):198–208. doi: 10.1016/s0091-7435(03)00114-2. [DOI] [PubMed] [Google Scholar]
- 42.Cullen KW, Watson KB. The impact of the Texas public school nutrition policy on student food selection and sales in Texas. Am J Public Health. 2009;99(4):706–12. doi: 10.2105/AJPH.2007.129387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.French SA, Story M, Jeffery RW, Snyder P, Eisenberg M, Sidebottom A, Murray D. Pricing strategy to promote fruit and vegetable purchase in high school cafeterias. J Am Diet Assoc. 1997;97(9):1008–10. doi: 10.1016/S0002-8223(97)00242-3. [DOI] [PubMed] [Google Scholar]
- 44.Cullen KW, Baranowski T, Baranowski J, Hebert D, de Moor C. Pilot study of the validity and reliability of brief fruit, juice and vegetable screeners among inner city African-American boys and 17 to 20 year old adults. J Am Coll Nutr. 1999;18(5):442–50. doi: 10.1080/07315724.1999.10718882. [DOI] [PubMed] [Google Scholar]
- 45.Prochaska JJ, Sallis JF. Reliability and validity of a fruit and vegetable screening measure for adolescents. J Adolesc Health. 2004;34(3):163–5. doi: 10.1016/j.jadohealth.2003.07.001. [DOI] [PubMed] [Google Scholar]