Abstract
PURPOSE
To describe the strategies and costs associated with recruiting African American and white adults into a randomized controlled pilot trial.
DESIGN
“Cryotherapy for Venous Disorders: A Pilot Study” is a randomized controlled trial designed to determine the effects of a cool gel wrap and leg elevation intervention versus a leg elevation alone intervention on skin temperature, skin microcirculation, quality of life, and pain in adults with stages 4 and 5 chronic venous disorders. We sought to recruit 60 participants (21 African Americans, 37 whites, and 2 Hispanic or Latino) to complete the study. These enrollment targets reflect the demographic distribution of the community in which the study was conducted (33% African American, 66% white, and 2% Latino). Proactive and reactive recruitment strategies were implemented to recruit subjects.
RESULTS
Seventy-three individuals (9 African American men, 29 African American women, 11 white men, 22 white women, 1 Asian woman, and 1 Hispanic woman) were screened, and of those, 67 were randomized (9 African American men, 25 African American women, 9 white men, 22 white women, 1 Asian woman, and 1 Hispanic women). Fifty-eight completed the study, yielding an overall 11% attrition rate. An additional 8 subjects canceled or did not show up for a first appointment. Reactive recruitment strategies were most successful for recruiting men, women, African American, and white participants. The 3 most successful reactive strategies were referrals from providers/clinics (34%), flyers posted in the hospital elevators (22%), and targeted mailings from a business (16%). Of the healthcare provider referrals (19), wound care nurses referred 12 completed participants. The amount budgeted for advertisement was $5,000 (2% of the total grant award). The amount spent on recruitment including labor was $5,978, which averaged $103 per participant who completed the study (N = 58). Reactive strategies per participant completer proved more cost-efficient than proactive strategies ($83 vs $215). However, the time spent by the principal investigator (approximately 100 hours or 2.5 hours per week × 40 weeks) on recruitment, particularly maintaining frequent face-to-face contact with providers, increased success in the area of healthcare provider referrals.
CONCLUSION
A variety of recruitment strategies are needed to ensure a diverse participant response to clinical research studies. As nurses become more involved in research activities, and particularly in recruitment, it is important to understand the most effective types of strategies and costs associated with these activities.
Introduction
The recruitment of participants for clinical trials can be a daunting task; no less important is the recruitment of participants for smaller pilot studies. Studies with sample sizes of 60 and less often require substantial resources, especially when the available participant pool is not at the fingertips of researchers. This was the case in a feasibility study to test a cryotherapy intervention on the microcirculation of skin affected by chronic venous disorders (CVDs). Although a number of strategies for recruiting participants for large clinical studies are well documented,1 this process evaluation report describes proactive and reactive recruitment strategies for a small clinical trial. The principal investigator (PI) did not have direct access to a clinical population from which to personally recruit participants. Thus, the recruitment plan required multiple recruitment strategies, sequenced over time, to advertise the study to a diverse participant pool. Several certified WOC nurses and certified wound care nurses were involved in the recruitment of patients. These referrals accounted for 20% of the total sample of completed participants.
Recruitment strategies for the study were developed from previous research experiences of the PI and review of the literature.2–7 Recruitment research questions and hypotheses were as follows: (1) What recruitment strategies (proactive and reactive) will be most successful in recruiting younger (<49 years), older (>=50 years), men, women, African American, and white participants with CVDs and at risk for developing venous leg ulcers (VLUs) for the cryotherapy study? (2) What recruitment strategies will be most successful in recruiting urban and rural patients for the study? (3) What recruitment strategies overall will be most successful in recruiting participants for the cryotherapy study?
Methods
Study Description
“Cryotherapy for Venous Disorder: A Pilot Study”8 is a randomized clinical trial funded by the National Institute for Nursing Research, National Institutes of Health (NIH), to determine the effects of 2 different 30-minute treatments on the lower leg microcirculation of skin affected by CVD. The long-term goal is to determine if cryotherapy, added to the standard of care for VLU prevention (compression and leg elevation), will improve skin microcirculation to reduce the number of new and recurring VLU in patients with CVD. Participants were randomized to receive 1 of 2 treatments: (1) a cool gel wrap and leg elevation or (2) leg elevation alone. Treatments lasted 30 minutes and were done at home by participants for 1 month. The study targeted African American and white men and women. The institutional review boards of the 2 participating study sites approved the study and recruitment materials. Based on sample size calculations, we sought to recruit 60 participants. To qualify, participants needed to be aged 21 years and older, have skin changes consistent with Clinical-Etiology-Anatomical-Pathological Classification Stage C4 (pigmentation, eczema, lipodermatosclerosis, and atrophie blanche) and Stage C5 (healed venous ulcer) CVDs,9 an ankle-brachial index of 0.80–1.3 mm Hg, intact skin sensation measured with a 10-g monofilament, intact thermal sensation measured with TipTherm, and venous refill time (VRT) of 25 seconds or less measured with a venous photoplethysmography in the affected leg. The participants agreed to wear compression stockings during waking hours. Exclusion criteria were having open ulcers, ankle-brachial index of less than 0.80 or more than 1.3 mm Hg, decreased skin and thermal sensation, VRT of more than 25 seconds, and unwillingness to obtain or wear compression stockings for 2 weeks prior to the start of the study and during waking hours while enrolled.
A total of $5,000 was budgeted for advertising materials to be used for recruitment or 2% of the total grant award. The study was conducted at 2 hospitals, 1 at a large metropolitan southeastern academic medical center and 1 at a rural community hospital 75 miles away. The first subject was enrolled in February 2008 and the last in November 2008. Participants were paid $25 for the screen, $25 more if enrolled, and $50 after completion for a total of $100. Checks were mailed 2 to 4 weeks after each visit. Parking was free and conveniently located near the study sites. The PI was blinded to the treatment assignments.
Recruitment
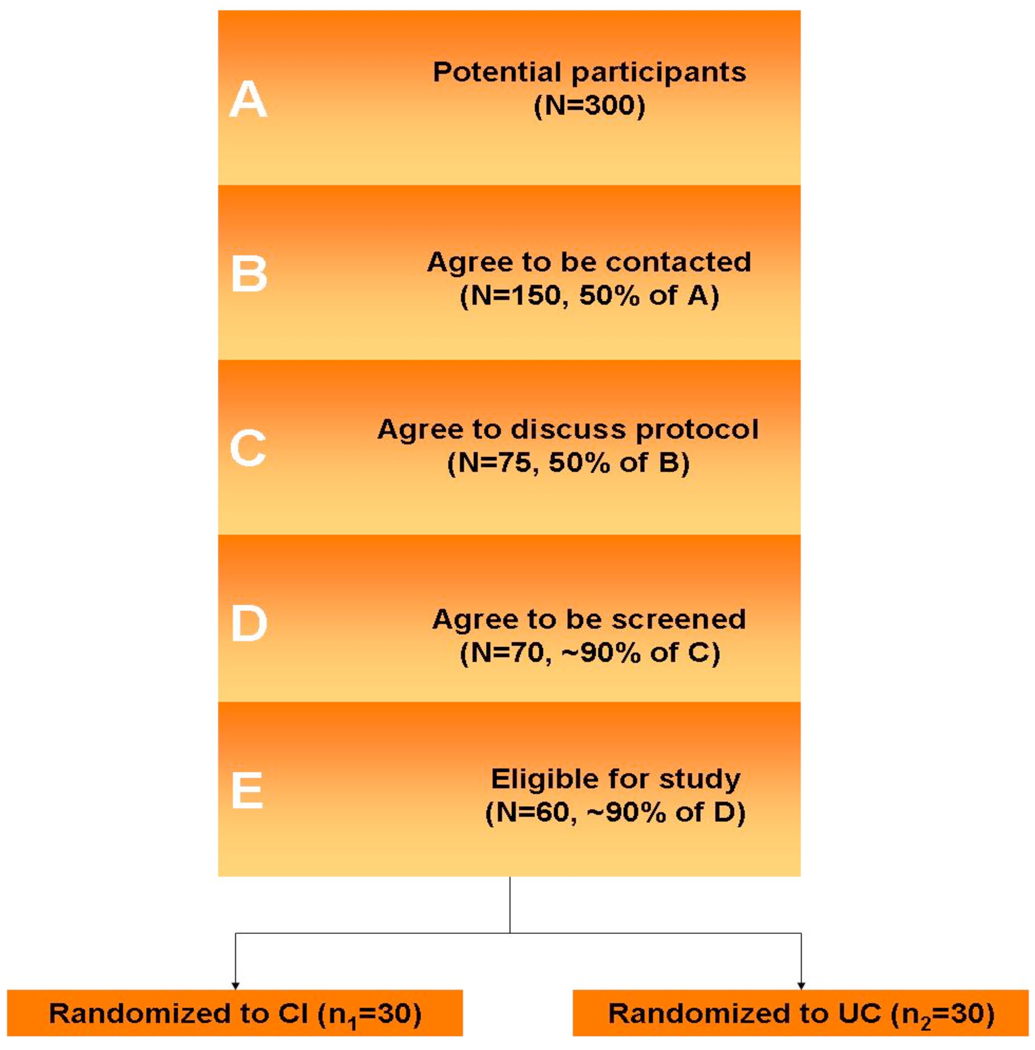
A targeted enrollment table is required of all NIH-funded studies (Table 1). Our enrollment target reflected the demographic distribution of the southeastern metropolitan communities in which the study was conducted (33% African American, 66% white, and 2% Latino). Because of the multiplicity of clinics affiliated with the academic medical center, it was difficult to estimate how many adults living in the metropolitan area could be targeted for the study through these hospital sources alone. However, given the population of the metropolitan (603,178) and rural (95,945) areas,10 together with the PI's preestablished contacts with non-academic-affiliated wound centers, community health centers, residential facilities, and businesses that provide services such as compression therapy, it was anticipated that the recruitment goals could be achieved within the allotted period (Table 2). Statistically, it was determined that 300 individuals needed to be approached to successfully recruit 30 participants per group (Figure 1), or 8 per week, to enroll 2 to 3 per week. These projections accounted for periods of low enrollment during holidays, vacations, rescheduled visits, and an anticipated 20% to 25% attrition rate.
Table 1.
TARGETED/PLANNED ENROLLMENT: Number of Subjects 60 (58)
| Ethnic Category | Sex/Gender | ||
|---|---|---|---|
| Females | Males | Total | |
| Hispanic or Latino | 1 (1) | 1 (0) | 2 (1) |
| Not Hispanic or Latino | 0 (1) | 0 0 | (1) |
| Ethnic Category: Total of All Subjects * | 2 (2) | ||
| Racial Categories | |||
| American Indian/Alaska Native | |||
| Asian | |||
| Native Hawaiian or Other Pacific Islander | |||
| Black or African American | 16 (21) | 4 (8) | 20 (29) |
| White | 31(18) | 7 (9) | 38 (27) |
| Racial Categories: Total of All Subjects * | 48 (41) | 12 (17) | 60 (58) |
(Actual completed are in parentheses)
TABLE 2.
Anticipated subject recruitment pool
| Collaborating Sites | Location | Adult Population |
Anticipated # Eligible |
Actual # Completed |
Primary recruitment strategy |
|---|---|---|---|---|---|
| Medical center adult ambulatory care clinics, outpatient physical therapy |
Urban | 3,500 | 30–40 | 17 | R |
| Local wound clinics | Urban | 450 | 20–30 | 12 | R |
| Faith-based and senior residential apartments |
Urban | 700 | 5–10 | 6 | R |
| Businesses selling compression | Urban | 150 visits/month |
10–20 | 10 | R |
| Community outreach centers, primary care practices |
Rural | 12,000 African- Americans |
30–50 | 8 | P |
| Rural hospital wound clinic | Rural | 2,000 | 20–30 | 5 | R |
Figure 1.
Patient enrollment and expected sample size
Recruitment Strategies
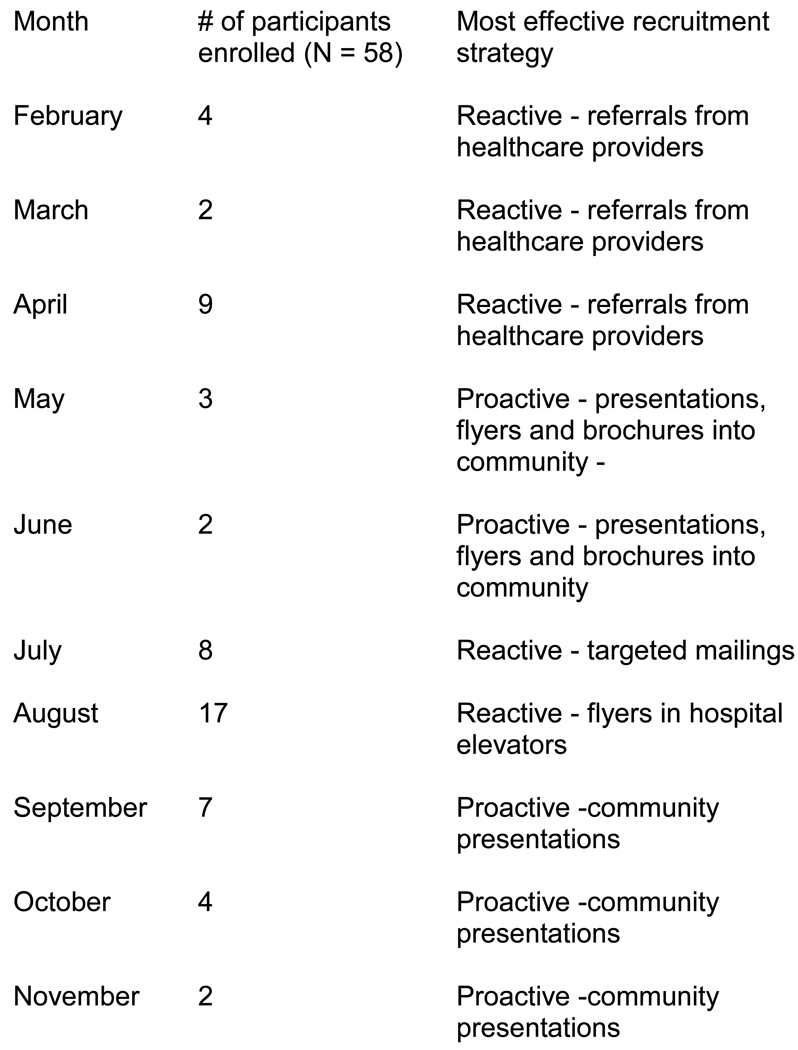
The PI was solely responsible for championing recruitment efforts. Proactive strategies 4 involve personal contact with participants through venues such as health fairs, presentations, and street outreach (approaching individuals in grocery stories, shopping centers, etc). Examples of reactive strategies,5 where there is no direct personal contact includes public information, flyers, brochures, targeted mailings, and visits to healthcare providers who were asked to make referrals. In Table 2, the column to the far right reflects the type of strategy most effect for recruitment in the collaborating sites. The recruitment plan was frequently evaluated to determine the best way to sequence or stage recruitment strategies. Reactive strategies were predominantly used during the first 1 to 3 months of the study. The PI contacted wound care nurses and physicians to arrange and meet with them face-to-face. Presentations to staffs of several outpatient clinics such as bariatrics, internal medicine, vascular, and at independent physical therapy clinics were also given. During months 4 to 5 and 8 to 9, the PI manned booths at health fairs and gave presentations to support groups, church groups, neighborhood soup kitchens, senior citizen and other community centers, residential living facilities, and senior apartment complexes where individuals could sign up for the study. Street outreach was also used during these times. These activities provided a steady “trickle” of interest throughout the 10-month recruitment period and reached individuals who might not have considered participation otherwise.
The PI met with an African American community research recruiter with prior involvement in several large clinical trials. He arranged for multiple community talks to predominantly African American audiences. During these proactive efforts, the PI discussed venous disorders, presented figures depicting vein and skin pathology, explained the study purpose and procedures, gave a demonstration of the treatment, and did VRT measurements of leg skin of individuals who thought they might have a problem.11–13 The anticipated outcomes were also described. Those who were interested were given a study “business” card or brochure with the PI's contact information, while the PI wrote down their phone number, address, or e-mail address. About half of the individuals who expressed interest gave the PI their contact information, while the other half preferred to call the PI. Within 24 hours, the PI made contact by phone to further describe the study details, conduct the study prescreen, and schedule the first appointment.
During months 6 to 7, numerous reactive strategies were used. Reactive strategies provided a “bolus” of referrals, especially during June and July. A local nurse who is a lymphedema specialist and who owns a compression therapy business agreed to send out letters and brochures to her clients. She was also advertising a special on compression stockings. Other reactive activities included posting inexpensive flyers in 8 elevators in the main academic medical center hospital. At each of the 8 elevators, there were approximately 1.3 elevator riders per minute (counted during 15-minute increments at the 8 elevators during different periods throughout the day) between the hours of 8 AM and 5 PM. This strategy provided exposure to approximately 5,616 passengers per day. The flyers were left up for 2 to 3 weeks based on hospital policy, during which time the chance of repeat passengers was high. The goal of this strategy was to post flyers in high-traffic areas where people have to stand still for several moments and are likely to see the flyer several times.
The study logo, color of print, and font were kept consistent across all promotional media. Printed materials indicated that participation was free and compensation was available. Brochures and flyers were developed by a graphic designer and were distributed to local businesses, medical offices, grocery stores, and churches. Other written media included letters and brochures from the PI sent to community physicians, public service announcements distributed via the hospital marketing department to local media, and news stories appearing in hospital and local newspapers. One African American participant placed brochures in her beauty shop; participants were also encouraged to tell friends and family about the study and were given study flyers to pass out. By month 10, recruitment activities were limited because 95% of the targeted enrollment had been met.
Results
The gender and age of the participants and the type of recruitment strategies for men and women are presented in Tables 3 and 4. As noted in research question 1, we hypothesized that proactive strategies would result in recruiting older subjects, African Americans and women, whereas reactive strategies are more likely to recruit younger subjects, whites, and men. All categories of subjects responded best to reactive strategies: older subjects >=50 years (n = 48), African Americans (n = 29), men (n = 17), and women (n = 41). Proactive strategies were less based on age, ethnicity, and gender. Reactive strategies were also more effective for recruiting both urban and rural dwellers.
Table 3.
Recruitment strategies for males
| Strategy | AA Male < 50 yo |
AA Male ≥ 50 yo |
C Male < 50 yo |
C Male ≥ 50 yo |
Totals | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| U | R | U | R | U | R | U | R | U | R | ||
| Proactive | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 2 | 1 | 3 |
| Reactive | 2 | 1 | 0 | 3 | 0 | 0 | 8 | 0 | 10 | 4 | 14 |
| Totals | 2 | 1 | 1 | 4 | 0 | 0 | 9 | 0 | 12 | 5 | 17 |
| 3 | 5 | 0 | 9 | 17 | |||||||
AA = African American; C = Caucasian; yo = years of age; U = Urban; R = Rural
Table 4.
Recruitment strategies for females
| Strategy | AA Female < 50 yo |
AA Female ≥ 50 yo |
C Female < 50 yo |
C Female ≥ 50 yo |
Totals | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| U | R | U | R | U | R | U | R | R | U | ||
| Proactive | 0 | 0 | 1 | 3 | 0 | 0 | 4 | 0 | 5 | 3 | 8 |
| Reactive | 5 | 0 | 8 | 4 | 2 | 0 | 10* | 4 | 25 | 8 | 33 |
| 5 | 0 | 9 | 7 | 2 | 0 | 14 | 4 | 30 | 11 | 41 | |
| 5 | 16 | 2 | 18 | 41 | |||||||
AA = African American; C = Caucasian; yo = years of age; U = Urban; R = Rural;
includes one Asian and one Hispanic participant
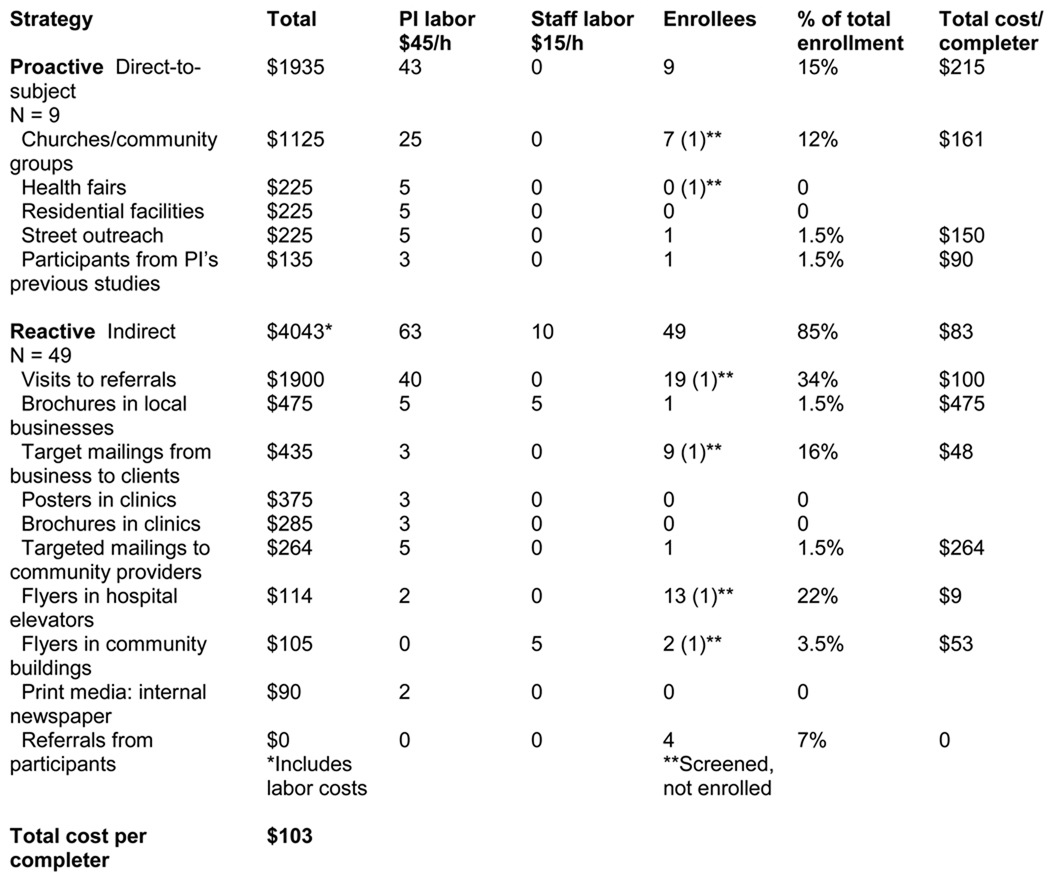
Proactive strategies cost $215 per participant, as compared to reactive strategies that cost $83 per participant. The difference was chiefly due to personnel costs; proactive strategies recruited fewer individuals (9 vs 49). Overall, proactive strategies were the least effective of the 2 recruitment methods (Tables 5 and 6).
Discussion
The total cost per participant completing the study was $103. Proactive strategies were more costly and less effective than reactive strategies, resulting in 9 participants at a cost of $215 each. Surprisingly, 2 of the most effective strategies—posting flyers in 8 hospital elevators ($9 per participant; n = 13 [22%]), and targeted mailings sent from a business owner to clients ($48 per participant; n = 9 [16%])—were the least expensive. Although the most effective method was healthcare provider referral ($100; n = 19 [34%]), it was double the cost of the targeted mailings.
Placing brochures in local businesses that sold compression stockings proved the most expensive reactive strategy, costing $475 for one participant completer. Direct costs included graphic design ($125), print expenses for 250 brochures ($240), and brochure holders ($55); indirect costs included PI time to develop the copy, check it for readability, and take pictures to put in the brochure and staff time to deliver. On the other hand, brochures that were sent out with a targeted mailing from a local business owner were highly effective in our study. Targeted mailings were also a successful reactive recruitment strategy in a study of 192 postmenopausal women recruited for the Beneficial Effects of Soy Trial (BEST).14 Although highly effective, the cost of mailings was the highest of all recruitment strategies used in that study; it cost $21,109 for a return on investment of $267.20 per completed participant.
In contrast to the high cost in the BEST study, direct mailing costs were found to be much lower in a study of women's preferences regarding tamoxifen use for primary prevention of breast cancer.15 The mailing yielded 312 women from the total sample of 771 at a cost of $773 or $2.48 per screened participant. Total recruitment cost per screened participant was $113. Costs were not reported in a study of a 12-month clinical trial of a telemedicine-based diabetes self-management intervention.16 The study, conducted in a rural community health center, used direct mailing followed by a phone call as the initial primary and highly successful recruitment modality to recruit 869 minorities from a pool of 1,984 who met inclusion criteria for the study. The recruitment strategy was conceptually based on a collaborative relationship model with the community health center that emphasized a multilevel, multistaged recruitment process.
Similar to the findings of other researchers, provider referral proved the most effective reactive recruitment strategy at a cost of $100 per participant completer. In a study of 180 older, rural African American women with type 2 diabetes, 25% of the sample was recruited via healthcare provider referrals.17 The researchers emphasized the need to develop trusting and collaborative relationships with healthcare providers. Although costs were not reported, expenses associated with healthcare referrals have been reported in other studies of large clinical trials. In a heart failure trial of 744 participants receiving a disease management intervention, $2,800 was spent on healthcare provider referrals, which resulted in 210 completers (19.7% of total sample) at a cost of $94.07 per subject.2 A dramatic difference in healthcare provider costs was noted in a sister study of 570 individuals with asthma who received a disease management intervention.2 This study was conducted by the same research team that conducted the heart failure study, but healthcare provider referral in the asthma study cost much less at $19.44 per 144 participant completer.2 Although the disparity in costs was not explained by the researchers, it seems plausible that because the identified participant pool was much lower for the asthma study (4,451) than for the heart failure study (49,934), fewer physician ($100/hour) and staff ($10/hour) labor hours were required for recruitment. In the BEST study, recruitment costs were $38.30 per completer.14 These findings reveal a wide range of costs associated with healthcare provider referral.
In our study, the cost of $100 per participant included PI time spent visiting healthcare providers who were and were not affiliated with the academic medical center. This time also took into account sending thank you notes after meetings, dropping off a steady stream of brochures to their clinics, and e-mailing the regular reminders to refer patients. WOC and wound care nurses referred the most participant completers (12); physicians referred 3; and physical therapists referred 4. Of the physician referrals, 2 were from the research team physician and 1 was from a community physician. The PI worked for almost 20 years with a larger internal medicine ambulatory care practice where she managed a wound and foot clinic, but received no referrals despite several presentations, having study brochures in waiting rooms and posting flyers around the clinic. The rationale for not having a referral can be expressed as “out of sight, out of mind.”
During the study, recruitment activities were slowly rolled out in the first few months to evaluate each recruitment strategy, make needed changes, and provide a steady stream of potential study subjects. The staging technique was similar to a community-based recruitment approach used for the Fiber Fermentation on Fecal Incontinence study of adults living in the community with fecal incontinence.18 Three primary recruitment strategies were staged to address the normal ebb and flow of participant accrual and resulted in a steady, yet manageable flow of participants. The most effective strategy, direct-to-subject recruitment, resulted in 80% of the initial 310 cases identified for the study with only 6.5% identified through a healthcare provider. It was concluded that proactive strategies were better suited for studies of a sensitive nature, in this case, fecal incontinence.
Overall, the targeted enrollment for minorities and men was exceeded in our study, but not for white women (Table 1). We did not turn away eligible participants based on ethnicity or gender, even when the category targets were met. The large response from African American women and men in general was unanticipated. We believe that the interest of younger African American women who encouraged older family members to enroll favored robust enrollment. About half of the men in the study were encouraged by their wives to contact the PI about participation in the study. Family members, no matter what age, are very important recruitment targets to consider for recruitment planning. Furthermore, it is imperative that recruitment materials include pictures of men and women representative of the ethnic backgrounds of the target population. Our recruitment materials were designed with diverse ethnicities, genders, ages, and reading levels and similar to those described by others. Reactive culturally specific recruitment strategies were designed for the target population and yielded the greatest proportion of participants (n = 107) in a study of an 8-month recruitment campaign for which 249 (target goal 240) African American smokers tested the efficacy of culturally specific self-help materials for smoking cessation.19 Although a discussion of culturally specific or culturally relevant advertising medium is not within the scope of this discussion, we believe careful consideration of these factors is paramount for creating a successful recruitment process.
Conclusion
The results of this process evaluation provide valuable insights to guide researchers, certified WOC nurses, and certified wound care nurses in identifying recruitment approaches for small clinical trials. The most successful strategies were referrals from healthcare providers, particularly wound care nurses, targeted mailings, and flyers. Nevertheless, the effectiveness of these approaches depends on the population being recruited. Careful consideration of age, gender, and ethnicity are required to optimally define the best recruitment strategy, even for small clinical trials. Reactive strategies appear to enhance recruitment rates over a shorter period of time, but proactive recruitment, although more expensive, may entice participation from individuals who are not reached by healthcare providers, flyers, or targeted mailings. Thus, a combination of staged approaches is recommended.
KEY POINTS.
[check mark] Recruitment for smaller clinical trials and pilot studies requires proactive and reactive recruitment strategies.
[check mark] Human labor costs associated with recruitment should be factored in to the recruitment plan.
[check mark] Staggering recruitment strategies ensure a manageable flow of participants.
FIGURE 2.
Recruitment strategies and costs
Figure 3.
Recruitment strategy by month
ACKNOWLEDGMENTS
The project described was supported by grant number 1 R21 NR010604-01 from the National Institutes of Health, National Institute of Nursing Research (NINR). Supplemental support was provided by the General Clinical Research Center #RR01070 of the Medical University of South Carolina.
Footnotes
Accession: 00152192-201001000-00007
Contributor Information
Teresa J. Kelechi, Medical University of South Carolina, College of Nursing, Charleston..
Ashlee Watts, SCTR Research Support Services, SUCCESS Center, Charleston, South Carolina..
Jan Wiseman, Medical University of South Carolina, College of Nursing, Charleston..
References
- 1.Mapstone J, Elbourne D, Roberts IG. Strategies to improve recruitment to research studies. Cochrane Database Syst Rev. 2007;(2):MR000013. doi: 10.1002/14651858.MR000013.pub3. [DOI] [PubMed] [Google Scholar]
- 2.Galbreath AD, Smith B, Wood P, Forkner E, Peters JI. Cumulative recruitment experience in two large single-center randomized, controlled clinical trials. Contemp Clin Trials. 2008;29(3):335–342. doi: 10.1016/j.cct.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 3.Aitken LM, Pelter MM, Carlson B, et al. Effective strategies for implementing a multicenter international clinical trial. J Nurs Scholarsh. 2008;40(2):101–108. doi: 10.1111/j.1547-5069.2008.00213.x. [DOI] [PubMed] [Google Scholar]
- 4.McDonald PW. Population-based recruitment for quit-smoking programs: an analytic review of communication variables. Prev Med. 1999;28(6):545–557. doi: 10.1006/pmed.1998.0479. [DOI] [PubMed] [Google Scholar]
- 5.Harris KJ, Ahluwalia JS, Catley D, Okuyemi KS, Mayo MS, Resnicow K. Successful recruitment of minorities into clinical trials: the Kick It at Swope project. Nicotine Tob Res. 2003;5(4):575–584. doi: 10.1080/1462220031000118540. [DOI] [PubMed] [Google Scholar]
- 6.Jeffries SK, Choi W, Butler J, Harris KJ, Ahluwalia JS. Strategies for recruiting African-American residents of public housing developments into randomized controlled trial. Ethn Dis. 2005;15(4):773–778. [PubMed] [Google Scholar]
- 7.Staffileno BA, Coke LA. Recruiting and retaining young, sedentary, hypertension-prone African American women in a physical activity intervention study. J Cardiovasc Nurs. 2006;21(3):208–216. doi: 10.1097/00005082-200605000-00009. [DOI] [PubMed] [Google Scholar]
- 8.Kelechi TJ. Cryotherapy for Venous Disorders: A Pilot. Bethesda, MD: National Institute of Nursing Research; 2007–2009. NIH 1R21NR010604-01. [Google Scholar]
- 9.Padberg FT. CEAP classification for chronic venous disease. Dis Mon. 2005;51(2/3):176–182. doi: 10.1016/j.disamonth.2005.03.013. [DOI] [PubMed] [Google Scholar]
- 10.US Census Bureau. [Retrieved January 20, 2009];State and county quick facts. 2008 from http://quickfacts.census.gov/qfd/states/45/45019.html.
- 11.Kelechi TJ, McNeil RB. A prospective, descriptive study of hour-to-hour and day-to-day temperature variability of skin affected by chronic venous disorders. Ostomy Wound Manage. 2008;54(4):18–34. [PubMed] [Google Scholar]
- 12.Kelechi TJ, Michel Y. A descriptive study of skin temperature, tissue perfusion, and tissue oxygen in patients with chronic venous disease. Biol Res Nurs. 2007;9(1):70–80. doi: 10.1177/1099800407299424. [DOI] [PubMed] [Google Scholar]
- 13.Kelechi TJ, Haight BK, Herman J, Michel Y, Brothers T, Edlund B. Skin temperature in chronic venous insufficiency. J Wound Ostomy Continence Nurs. 2003;13(1):17–24. doi: 10.1067/mjw.2003.10. [DOI] [PubMed] [Google Scholar]
- 14.Lindenstruth KA, Curtis CB, Allen JK. Recruitment of African American and White postmenopausal women into clinical trials: the Beneficial Effects of Soy Trial experiences. Ethn Dis. 2006;16(4):938–942. [PMC free article] [PubMed] [Google Scholar]
- 15.Keyzer JF, Melnikow J, Kuppermann M, et al. Recruitment strategies for minority participation: challenges and cost lessons from the POWER interview. Ethn Dis. 2005;15:395–406. [PubMed] [Google Scholar]
- 16.Davis RM, Hitch AD, Nichols M, Rizvi A, Salaam M, Mayer-Davis EJ. A collaborative approach to the recruitment and retention of minority patients with diabetes in rural community health centers. Contemp Clin Trials. 2009;30(1):63–70. doi: 10.1016/j.cct.2008.09.007. [DOI] [PubMed] [Google Scholar]
- 17.Burns D, Soward ACM, Skelly AH, Leeman J, Carlson J. Effective recruitment and retention strategies for older members of rural minorities. Diabetes Educ. 2008;34(6):1045–1052. doi: 10.1177/0145721708325764. [DOI] [PubMed] [Google Scholar]
- 18.Whitebird RR, Bliss DZ, Hase KA, Savik K. Community-based recruitment and enrollment for a clinical trial on the sensitive issue of fecal incontinence: the FIBER study. Res Nurs Health. 2006;29(3):233–243. doi: 10.1002/nur.20131. [DOI] [PubMed] [Google Scholar]
- 19.Webb MS, Seigers D, Wood EA. Recruiting African American smokers into intervention research: relationships between recruitment strategies and participant characteristics. Res Nurs Health. 2009;32:86–95. doi: 10.1002/nur.20299. [DOI] [PubMed] [Google Scholar]