Abstract
Objective
This study sought to determine whether the family environment moderates psychosocial outcomes after traumatic brain injury (TBI) in young children.
Method
Participants were recruited prospectively from consecutive hospital admissions of 3-6 year old children, and included 19 with severe TBI, 56 with complicated mild/moderate TBI, and 99 with orthopedic injuries (OI). They completed four assessments across the first 18 months post-injury. The initial assessment included measures of parenting style, family functioning, and the quality of the home. Children’s behavioral adjustment, adaptive functioning, and social competence were assessed at each occasion. Mixed model analyses examined the relationship of the family environment to psychosocial outcomes across time.
Results
The OI and TBI groups differed significantly in social competence, but the family environment did not moderate the group difference, which was of medium magnitude. In contrast, group differences in behavioral adjustment became more pronounced across time at high levels of authoritarian and permissive parenting; among children with severe TBI, however, even those with low levels of permissive parenting showed increases in behavioral problems. For adaptive functioning, better home environments provided some protection following TBI, but not over time for the severe TBI group. These three-way interactions of group, family environment, and time post injury were all of medium magnitude.
Conclusions
The findings indicate that the family environment moderates the psychosocial outcomes of TBI in young children, but the moderating influence may wane with time among children with severe TBI.
Keywords: parenting, home, behavior, social competence, adaptive functioning
Traumatic brain injury (TBI) is one of the most common causes of death and long-term disability in children (Kraus, 1995). Nearly half a million children 0-14 years of age sustain TBI requiring medical care each year in the United States (Langlois et al., 2006). Among survivors, the consequences of TBI in children include physical disabilities, deficits in cognitive and academic skills, and problems in school performance, behavioral adjustment, adaptive functioning, and socialization (Anderson et al., 2006; Ewing-Cobbs et al., 2004a; Schwartz et al., 2003; Stancin et al., 2002; Yeates et al., 2004).
Research strongly suggests that the effects of pediatric TBI are age-dependent. Younger children are particularly vulnerable, with deficits most apparent when TBI are sustained prior to school age (Anderson et al., 2005; Ewing-Cobbs et al., 1997, 2006). Researchers have speculated that younger children display poorer outcomes because they are more susceptible to the diffuse brain insult that accompanies severe TBI and its effects on post-injury skill development (Ewing-Cobbs et al., 1997, 2004b; Taylor & Alden, 1997).
Although TBI appears to be associated with especially poor outcomes in young children at a group level, substantial variability in outcomes is evident across individual children (Anderson et al., 2005, 2006; Catroppa, Anderson, Morse, Haritou, & Rosenfeld, 2008). Research therefore has begun to focus on factors that predict individual differences in outcomes among young children with TBI. Injury severity is a consistent predictor, but does not account for most of the variance in outcomes (Anderson et al., 2005, 2006; Catroppa et al., 2008; Taylor et al, 2008).
In older children, pre-injury environmental factors have been shown to account for variability in outcomes following TBI, over and above injury severity. Indeed, the pre-injury family environment not only accounts for individual differences, but also is an important moderator of the outcomes of TBI in school-age children, such that the deleterious effects of TBI are buffered by better family environments and exacerbated by poorer family environments (Taylor et al., 2002; Yeates et al., 1997, 2002). However, research on the outcomes of TBI in young children has largely neglected to assess outcomes relative to the family and home environment, despite evidence from the study of normal development showing that the influence of parenting and the home environment is especially potent in younger children (Collins, Maccoby, Steinberg, Hetherington, & Bornstein, 2000).
The relative importance of injury severity and the home environment as predictors of outcomes following TBI in young children may depend on the type of outcome under consideration. In school-age children, injury severity often accounts for similar amounts of variance in both cognitive and behavioral outcomes. However, the two types of outcomes are not strongly correlated, suggesting that their remaining variance may not be accounted for by the same influences (Fletcher et al., 1990). In general, research in school-age children suggests that the family environment is more strongly related to behavioral than cognitive outcomes (Taylor et al., 2002; Yeates et al., 1997, 2002). This may not hold true for young children sustaining TBI, however, given the heightened importance of parenting and the home environment for cognitive development at younger as compared to older ages (Landry, Smith, & Swank, 2003).
We recently presented data on acute cognitive and school-readiness outcomes of TBI in young children based on a prospective, longitudinal study conducted at several hospitals in the midwest United States (Taylor et al., 2008). Participants included 3-6 year old children hospitalized for complicated mild to severe TBI, as well as a comparison group of children of like age hospitalized for orthopedic injuries (OI). Injury severity consistently predicted cognitive and school-readiness outcomes assessed 6 months post-injury, and environmental factors helped account for individual differences, but only limited evidence was found for environmental factors as moderators of cognitive or early academic outcomes relative to children with OI.
Young children with TBI are known to display psychosocial deficits, and their psychosocial functioning is also related to socioeconomic status and family functioning (Anderson et al., 2006; Catroppa et al., 2008), but we are not aware of any studies that have specifically examined the potential moderating influence of the home environment. Therefore, the primary goal of the current study was to extend our previous findings by examining psychosocial outcomes and the potential moderating influence of the pre- and early post-injury home environment in the same sample of participants. At an initial assessment shortly after injury, we obtained retrospective ratings of pre-injury parenting style and general family functioning, and also assessed the concurrent quality of the home environment. We also obtained retrospective ratings of children’s pre-injury behavioral adjustment, adaptive functioning, and social competence. Post-injury assessments of the latter psychosocial outcomes were then obtained every 6 months out to 18 months post injury. Unlike the previous cross-sectional analysis, therefore, we were able to use growth curve modeling or mixed model analyses to examine whether the home environment was a predictor of variations in children’s longitudinal trajectories of psychosocial outcomes following TBI.
We hypothesized that young children hospitalized for TBI would display deficits in behavioral adjustment, adaptive functioning, and social competence relative to children with OI only. The deficits were predicted to be most pervasive in children with severe TBI and to become more pronounced across assessments, based on previous research with both preschool and school-age children showing that psychosocial functioning following TBI tends to worsen over time (Anderson et al., 2006; Catroppa et al., 2008; Fay et al., 2009; Taylor et al., 2002). We also expected that psychosocial outcomes would be worse for children from environments characterized by less effective parenting, worse family functioning, and poorer quality homes (Anderson et al., 2006). Most importantly, we predicted that such environments would exacerbate the negative psychosocial consequences of TBI and, conversely, that environments characterized by more effective parenting, better family functioning, and higher quality home environments would be associated with less deleterious outcomes (Taylor et al., 1999, 2002; Yeates et al., 1997).
We also anticipated that the moderating influences of the pre-injury family environment might vary over time. If the effects of TBI on psychosocial outcomes worsened with time as expected, then the moderating influence of the family environment might become easier to detect at the later assessments, especially if the effects of the family environment on psychosocial functioning only manifest themselves gradually. On the other hand, the moderating influence might be strongest at the 6-month assessment, which was closest in time to the assessment of the family environment; this would be especially likely if the family environment itself actually changed in response to children’s injuries, because of potential bidirectional influences between psychosocial outcomes and parenting or family functioning (Taylor et al., 2001).
Method
Study Design
The data for the current analyses were drawn from a larger parent study that used a concurrent cohort, prospective, and longitudinal design in which children ages 3 to 6 years of age hospitalized for either TBI or OI were followed for approximately 18 months post injury (Taylor et al., 2008). Following recruitment, which occurred shortly after injury when children were medically stable, children and caregivers completed an initial assessment, most often at the hospitals where the children received care for their injuries. Additionally, a home visit was conducted to assess the quality of the home environment. Three follow-up assessments were then conducted at 6, 12, and 18 months post-injury. At all occasions, child and caregiver assessments were conducted in tandem, and included parent interviews and ratings regarding child and family functioning, tests of children’s cognitive abilities, and video-taped parent-child interactions.
Participants
Participants were recruited from consecutive inpatient admissions to three tertiary care children’s hospitals and a general hospital in the Midwestern United States, all of which had Level 1 trauma centers. All children aged between 3 years and 6 years, 11 months and admitted for TBI or OI from 2003-2006 were considered for potential participation. Children were excluded from consideration if child abuse was documented as a cause of injury, the primary spoken language in the home was other than English, or if they had a previous history of autism, mental retardation, or neurological disorder.
Children were eligible for the TBI group if they sustained a blunt trauma to the head requiring overnight admission to the hospital and had either a Glasgow Coma Scale (GCS, Teasdale & Jennett, 1974) score < 15, suggesting altered neurological status, or evidence for TBI-related brain abnormalities from computed tomography (CT) or magnetic resonance imaging (MRI). Consistent with previous investigations (Anderson et al., 2006; Fletcher et al., 1990; Taylor et al., 1999), a GCS score of 8 or less defined a severe TBI. Complicated-mild to moderate TBI was defined as a GCS score of 9-12 with or without abnormal neuroimaging or a higher GCS score with abnormal neuroimaging. The GCS score assigned to the child was the lowest one recorded post-resuscitation. Because the focus of this study was on children with complicated-mild to severe TBI, a small group of children with uncomplicated mild TBI was excluded from analysis. Inclusion in the OI group required a documented bone fracture in an area of the body other than the head that required an overnight hospital stay, and the absence of any evidence of loss of consciousness or other findings suggestive of TBI.
The study was approved by the institutional review boards of all participating hospitals and informed consent was obtained from parents or legal guardians prior to participation. A total of 206 children (23 severe TBI, 64 complicated mild/moderate TBI, 119 OI) and their caregivers were enrolled in the study. Recruitment rates for families who were contacted were somewhat higher for the TBI group as a whole than for the OI group (53% vs. 35%). In both groups, the most common reasons for non-participation were a lack of interest or not having time for the study. Participants and non-participants did not differ on sex, race, age at injury, or census-based estimates of neighborhood income. For the purposes of this paper, children were included only if they had data for all relevant predictors and completed at least one of the 6, 12, or 18 month post-injury assessments. The final sample therefore included 174 children, with 19 severe TBI, 56 complicated mild/moderate TBI, and 99 OI. Children included in the analyses did not differ from those who were excluded in sex, race, age at injury, neighborhood income, or maternal education.
As shown in Table 1, the TBI and OI groups did not differ on a variety of demographic variables. The only exception was maternal education, which was lowest in the severe TBI group and highest in the OI group. The groups also did not differ on retrospective ratings of behavioral adjustment or social competence. Unexpectedly, the groups did differ significantly on retrospective ratings of adaptive functioning, with lower scores in the severe TBI group. However, data collected via parent interviews failed to suggest group differences in pre-injury developmental status as assessed by special education services or prior concerns about the child’s development, behavior, or learning.
Table 1.
Sample Demographic Characteristics.
| Group |
|||
|---|---|---|---|
| Severe TBI (n = 19) | Moderate TBI (n = 56) | OI (n = 99) | |
| Age at injury in years, M (SD) | 4.96 (1.00) | 5.04 (1.20) | 5.11 (1.07) |
| Males, n (%) | 13 (68%) | 33 (59%) | 53 (53%) |
| Non-white race, n (%) | 7 (37%) | 17 (30%) | 24 (24%) |
| Intimate partner in home, n (%) | 14 (74%) | 40 (71%) | 82 (83%) |
| Number of persons in household, M (SD) | 4.58 (1.50) | 4.43 (1.50) | 4.51 (1.18) |
| Attending daycare/preschool/kindergarten at time of injury, n (%) | 15 (79%) | 42 (75%) | 70 (71%) |
| Census tract median family income in dollars, M (SD) | 54,308 (15,823) | 57,051 (26,327) | 63,888 (23,410) |
| Maternal education, n (%):* | |||
| Less than high school | 6 (32%) | 8 (14%) | 6 (6%) |
| High school degree/GED | 8 (42%) | 21 (38%) | 37 (37%) |
| Partial college | 4 (21%) | 10 (18%) | 20 (20%) |
| College graduate or graduate degree | 1 (5%) | 17 (30%) | 36 (36%) |
| Pre-injury behavioral adjustment (CBCL total T score), M (SD) | 51.31 (16.09) | 47.93 (11.13) | 46.10 (10.88) |
| Pre-injury adaptive functioning (ABAS GAC standard score), M (SD)* | 79.50 (16.08) | 96.74 (19.21) | 93.30 (20.29) |
| Pre-injury social competence (PKBS/HCSBS z score), M (SD) | -0.19 (0.91) | 0.26 (0.81) | 0.37 (0.89) |
Note: TBI = traumatic brain injury; OI = orthopedic injury; SD = standard deviation; GED = General Education Diploma; CBCL = Child Behavior Checklist. ABAS = Adaptive Behavior Assessment System. GAC = General Adaptive Composite. PKBS = Preschool and Kindergarten Behavior Scales. HCSBS = Home and Community Social and Behavior Scales.
Group difference significant, p < .05.
Table 2 lists injury characteristics and acute cognitive ability for the groups. The time between injury and initial assessment was shorter for the OI group (range = 8 to 70 days) than for the TBI groups (range = 10 to 116 days across both groups). This difference likely reflected our willingness to extend recruitment somewhat beyond the desired window (i.e., 3 months post injury) so as to maximize enrollment of children with TBI. Most of the injuries in the TBI and OI group were due to transportation or falls, consistent with national trends for young children (Langlois et al., 2006). Transportation-related injuries were significantly more common in the TBI groups than in the OI group. The groups differed in their mean New Injury Severity Score (NISS, Osler et al., 1997), defined as the sum of the squares of the Abbreviated Injury Scale (AIS) scores for each child’s three most severely injured body regions. Post-hoc tests indicated higher NISS for the severe and complicated-mild/moderate TBI groups compared with the OI group. The groups also differed in mean “non-head-injury” NISS, computed as the NISS minus the AIS for the head region; the severity of injuries to regions other than the head was higher in the OI group than in the TBI groups. Finally, the groups differed in mean cognitive ability as measured on the Differential Abilities Scale (Elliott, 1990) at the initial assessment, with the severe TBI group showing the lowest functioning.
Table 2.
Injury Characteristics and Acute Post Injury Cognitive Ability.
| Group |
|||
|---|---|---|---|
| Severe TBI (n = 19) | Moderate TBI (n = 56) | OI (n = 99) | |
| Time since injury to initial assessment in days, M (SD)* | 47.58 (23.42) | 46.48 (23.42) | 36.60 (15.01) |
| External cause of injury, n (%):*a | |||
| Transportation | 10 (52%) | 14 (25%) | 13 (13%) |
| Fall | 6 (32%) | 29 (52%) | 34 (34%) |
| Other | 3 (16%) | 13 (23%) | 52 (52%) |
| Length of hospital stay in days, M (SD)* | 9.91 (19.08) | 2.06 (1.91) | 0.79 (1.08) |
| NISS total, M (SD)* | 13.50 (8.62) | 15.07 (7.87) | 7.04 (2.66) |
| NISS non-head-related, M (SD)* | 1.38 (2.09) | 2.33 (5.20) | 7.04 (2.66) |
| Lowest GCS score, M (SD)* | 3.82 (1.70) | 13.44 (2.01) | NA |
| Differential Abilities Scale GCA, M (SD)b* | 83.82 (16.33) | 98.62 (15.98) | 102.34 (14.70) |
Note: TBI = traumatic brain injury; OI = orthopedic injury; SD = standard deviation; NISS = New Injury Severity Score; GCS = Glasgow Coma Scale; NA = Not applicable; GCA = General Cognitive Ability standard score.
Injuries due to “other” causes included those related to sports and recreation, rough-housing, and falling objects.
Administered at the initial assessment.
Group difference significant, p < .05.
Procedure and Measures
At the initial assessment, which typically took about 3 hours, the children’s primary caregivers completed retrospective ratings of pre-injury parenting style and general family functioning, as well as children’s pre-injury behavioral adjustment, adaptive functioning, and social competence. Caregivers also participated in a home visit during which a concurrent measure of the quality of the home environment was completed. The time between injury and home visit was shorter for the OI group (m = 38.69 days, sd = 19.16, range = 4 to 109 days) and complicated-mild/moderate TBI group (m = 41.60 days, sd = 19.40, range = 12 to 96 days) than for the severe TBI group (m = 60.61 days, sd = 43.29, range = 7 to 188 days). Post-injury ratings of the children’s psychosocial outcomes were then obtained from caregivers at 6, 12, and 18 months post-injury. For 96% of the participants, mothers were the informants at all assessment occasions; in only two cases did the informant change over time.
Family Environment
Three measures of the family environment were used as predictors of psychosocial outcomes. The measures were intended to assess parenting style, overall family functioning, and the quality of the home environment. Preliminary analyses revealed significant, but modest correlations among the variables (i.e., rs from .38 to -.43). The OI and TBI groups did not differ on any of the measures.
Parenting style was assessed using the Parenting Practices Questionnaire (Robinson, Mandleco, Olsen, & Hart, 1995). This 62-item rating scale assesses three dimensions of parenting style, consistent with Baumrind’s (1971) characterization of authoritarian, authoritative, and permissive parenting. The scales for each dimension represent composites of subscales derived through factor analysis. For the purposes of the current study, we used total scores for each dimension. The measure has shown satisfactory reliability and validity in previous research (Robinson et al., 2001).
The 12-item General Functioning subscale of the McMaster Family Assessment Device (FAD-GF, Byles, Byrne, Boyle, & Oxford, 1988; Miller, Bishop, Epstein, & Keitner, 1985) was used to assess family functioning. The measure has shown satisfactory reliability and validity in previous research (Byles et al., 1988; Miller et al., 1985) and is related to outcomes of TBI (Taylor, Yeates, Wade, Drotar, & Klein, 1999). For this study, the scores from the General Functioning Scale were standardized across the entire sample (m = 0, sd = 1). Consistent with the scaling of the original scores, high scores reflect worse family functioning.
The quality of the home environment was assessed using The Home Observation for Measures of the Environment (HOME, Bradley & Caldwell, 1984; Caldwell & Bradley, 1984), which was administered at children’s homes by trained research assistants. The HOME involves a combination of parent interview and direct observations of parent-child interactions and play or learning materials in the home to assess the extent to which the home environment is conducive to positive interactions with children and supportive of their development. The HOME has shown satisfactory reliability and validity in predicting children’s cognitive and social/emotional development (Bradley & Caldwell, 1984; Caldwell & Bradley, 1984). In this study, reliability was assessed by having two research assistants complete the HOME independently for approximately 5% of the home visits. Inter-rater agreement was satisfactory (r = .92). The total score from the HOME was used in the current study.
Psychosocial Outcomes
Psychosocial outcomes were assessed using measures designed to assess behavioral adjustment, adaptive functioning, and social competence. Behavioral adjustment was assessed using the preschool (for children < 6 years of age) and school-age (for children 6 or older) forms of the Child Behavior Checklist (CBCL; Achenbach & Rescorla, 2000; Achenbach & Rescorla, 2001). The CBCL is a well-known rating scale that was standardized on a large sample of community and clinic-referred children. It has demonstrated satisfactory reliability and validity in previous research, although it has not always been sensitive to the effects of childhood TBI (Fletcher et al., 1990, 1996). For the current study, behavioral adjustment was measured using the total T score from the CBCL (M = 50, SD = 10).
The infant/preschool (for children < 6 years of age) and school-age (for children 6 or older) versions of the Adaptive Behavior Assessment System-Second Edition (ABAS) were used to assess adaptive functioning (Harrison, & Oakland, 2003). The ABAS is a standardized questionnaire that assesses children’s ability to manage the demands of daily life in multiple settings (e.g., home and school). Overall adaptive functioning is summarized by the General Adaptive Composite, which is expressed as a standard score (M = 100, SD = 15). The ABAS demonstrates good reliability and has been shown to be sensitive to developmental differences and clinical disorders (Harrison, & Oakland, 2003; Oakland & Harrison, in press).
The Preschool and Kindergarten Behavior Scales-Second Edition (PKBS-2; Merrell, 2002) and the Home and Community Social and Behavior Scales (HCSBS; Merrell & Caldarella, 2002) were used to assess social competence. The PKBS and HCSBS are similar in structure and content, but are normed for younger (ages 3-6 years) and older (ages 5-18 years) children, respectively. For the purposes of this study, parents of children younger than 6 years of age completed the PKBS and those with children ages 6 or older completed the HCSBS. Both measures have demonstrated satisfactory reliability and validity (Lund & Merrell, 2001; Merrell, 1996; Merrell & Boelter, 2001; Merrell, Streeter, & Boetter, 2001). For this study, we used the social competence composite from each measure. To enable comparisons across measures, the corresponding summary scores from each measure were transformed to z scores with a M of 1 and SD of 0 (i.e., those from the PKBS-2 for children 3 to 5 years and those from the HCSBS for children 6 years and older). The two sets of z scores demonstrated substantial correlations across time, supporting the assumption that they provide equivalent measures of social competence.
Statistical Analysis
Raw group means and standard deviations for the three primary dependent variables (CBCL, PKBS/HCSBS, ABAS) at 6, 12, and 18 months post-injury are presented in Table 3. This data was subjected to general linear mixed model analyses to examine the prediction of psychosocial outcomes over time as a joint function of injury severity and the family environment. Three analyses were conducted, one for each of the three measures of psychosocial outcome that served as the dependent variables in the analyses (i.e., CBCL Total T score; ABAS General Adaptive Composite standard score; PKBS/HCSBS social competence composite z score). All analyses included the following covariates: retrospective ratings of pre-injury functioning on the dependent variable in question, obtained at the baseline assessment; child’s race (white vs. non-white); child’s sex; child’s age at injury; family socioeconomic status (SES); primary caregiver intimate relationship status (partner in the home vs. no partner in the home); and test version (all three measures of psychosocial outcomes had different versions for younger versus older children). SES was defined in terms of maternal education and median income for the census tract in which the family’s residence was located; a composite was computed by averaging the sample z scores for the two variables.
Table 3.
Raw Group Means and Standard Deviations for Psychosocial Outcomes
| Group |
|||||||
|---|---|---|---|---|---|---|---|
| Severe TBI | Moderate TBI | OI | |||||
| Outcome Measure | Months Post-Injury | M | SD | M | SD | M | SD |
| Child Behavior Checklist Total T score | 6 | 57.26 | 14.87 | 49.19 | 12.23 | 45.24 | 10.27 |
| 12 | 56.45 | 14.20 | 49.64 | 12.69 | 47.54 | 11.85 | |
| 18 | 55.81 | 12.25 | 47.54 | 11.85 | 44.87 | 10.44 | |
| ABAS GAC Standard score | 6 | 74.67 | 25.76 | 98.33 | 25.15 | 95.33 | 19.33 |
| 12 | 78.53 | 28.83 | 95.39 | 22.17 | 96.96 | 19.01 | |
| 18 | 77.20 | 30.10 | 94.66 | 23.38 | 97.54 | 18.51 | |
| PKBS/HCSBS Social Competence z score | 6 | -0.42 | 1.19 | 0.14 | 1.05 | 0.32 | 0.81 |
| 12 | -0.44 | 1.24 | 0.26 | 1.00 | 0.47 | 0.73 | |
| 18 | -0.52 | 1.16 | 0.31 | 1.04 | 0.48 | 0.77 | |
Note: TBI = traumatic brain injury; OI = orthopedic injury; SD = standard deviation; GED = General Education Diploma; CBCL = Child Behavior Checklist. ABAS = Adaptive Behavior Assessment System. GAC = General Adaptive Composite. PKBS = Preschool and Kindergarten Behavior Scales. HCSBS = Home and Community Social and Behavior Scales.
Given these covariates, we estimated the effects of the following predictors: injury severity (two dummy variables, one comparing the severe TBI and OI group and another comparing the complicated-mild/moderate TBI and OI group); FAD-GF scale; HOME total score; total scores for authoritarian, authoritative, and permissive parenting styles from the Parenting Practices Questionnaire; and a linear term for time post injury. Because data were available at only three time points (6, 12, and 18 months post-injury), the model did not include a parameter representing the quadratic rate of change (i.e., nonlinearity). The initial model also included all interactions involving group, time since injury, and each of the measures of the family environment. Subjects were considered a random effect, so that each subject was initially modeled with independent slopes and intercepts with respect to time. After fitting an initial model, we reduced model complexity to achieve the most parsimonious model. We followed an iterative process, eliminating predictors for which the F tests for fixed effects were not significant, starting with three-way interactions, and then re-estimating the model before examining lower-level interactions and, finally, main effects. For any significant interaction, all of the main effects and lower-level interactions upon which the significant interaction was based were retained in the model.
Effect sizes were computed by standardizing all continuous predictors (M = 0, SD = 1) other than time since injury, which was centered at 6 months, and obtaining parameter estimates based on the final mixed model for each dependent variable. The resulting coefficients are akin to standardized regression coefficients for continuous predictors and to standardized mean differences (e.g., d) for categorical variables. Because standardized regression coefficients can be scaled to correlations (Cohen, 1988), we used conventional definitions of effect size for correlations to characterize the magnitude of the standardized parameter estimates for continuous predictors and interactions involving only them (i.e., 0.1 is small, 0.3 is medium, and 0.5 is large). Likewise, we used conventional definitions of effect size for mean differences to characterize the magnitude of parameter estimates for categorical predictors and any interactions involving them (i.e., 0.2 is small, 0.5 is medium, 0.8 is large).
Results
Behavioral Adjustment
The analysis of the CBCL, summarized in Table 4, revealed significant three-way interactions between group membership, parenting style, and time post injury. Specifically, the interaction of group, permissive parenting, and time was significant, as was the interaction of group, authoritarian parenting, and time. The interaction involving authoritarian parenting was significant and medium in magnitude for both the severe TBI and moderate TBI groups (standardized estimates =.49 and .43, respectively). The interaction involving permissive parenting was medium in magnitude for the severe TBI group (standardized estimate = -.43) but small and not significant for the moderate TBI group (standardized estimate = .22). To illustrate the interactions, mean CBCL total scores were estimated for children with low and high levels of permissive (or authoritarian) parenting (i.e., those who were 1 or more standard deviations above or below the overall sample mean for the respective parenting measures). As Figure 1 shows, high levels of permissive parenting were associated with larger group differences in behavioral adjustment than lower levels; however, this did not hold true across time in the severe TBI group, which showed increases in behavioral problems even at lower levels of permissive parenting. The relationship of authoritarian parenting to behavioral adjustment was somewhat different. Figure 2 shows that high levels of authoritarian parenting were associated with less pronounced group differences initially, but with considerable worsening of behavioral adjustment among the TBI groups over time; in contrast, low levels of authoritarian parenting predicted a decline in group differences over time, especially for the complicated-mild/moderate TBI group.
Table 4.
Results of Mixed Models Analysis of Measures of Psychosocial Functioning
| Dependent Measure | Effect | Estimate | Standard Error | Df | F | p | |
|---|---|---|---|---|---|---|---|
| CBCL Total Score | Premorbid rating | 0.68 | 0.04 | 1, 164 | 288.59 | <.001 | * |
| Sex | -0.25 | 0.85 | 1, 149 | 0.09 | .76 | ||
| Race | 0.75 | 1.11 | 1, 156 | 0.46 | .50 | ||
| Intimate partner in home | -3.06 | 1.21 | 1, 166 | 6.46 | .01 | * | |
| CBCL version | -4.06 | 1.02 | 1, 310 | 15.76 | <.001 | * | |
| SES | -0.97 | 0.48 | 1, 152 | 4.16 | .04 | * | |
| Age at injury | -0.45 | 0.53 | 1, 357 | 0.73 | .39 | ||
| Time since injury | -1.68 | 0.88 | 1, 155 | 0.13 | .06 | ||
| Group | 2, 247 | 0.21 | .81 | ||||
| FAD z score | -1.28 | 0.67 | 1, 330 | 4.36 | .04 | * | |
| Authoritarian parenting | 1.14 | 1, 297 | 1.77 | .18 | |||
| Permissive parenting | 1.02 | 1.01 | 1, 274 | 8.53 | .01 | * | |
| FAD X time since injury | 1.41 | 0.68 | 1, 144 | 4.36 | .04 | * | |
| Authoritarian parenting X time since injury | -1.88 | 0.91 | 1, 211 | 4.32 | .04 | * | |
| Permissive parenting X time since injury | -0.31 | 0.98 | 1, 192 | 1.75 | .19 | ||
| Group X time since injury | 2, 148 | 1.08 | .34 | ||||
| Group X authoritarian parenting | 2, 294 | 8.00 | <.001 | * | |||
| Group X permissive parenting | 2, 278 | 4.11 | .02 | * | |||
| Group X authoritarian parenting X time since injury | 2, 192 | 8.18 | <.001 | * | |||
| Group X permissive parenting X time since injury | 2, 184 | 5.12 | .01 | * | |||
| ABAS GAC standard score | Premorbid rating | 0.64 | 0.06 | 1, 163 | 126.57 | <.001 | * |
| Sex | 0.82 | 2.17 | 1, 163 | 0.14 | .71 | ||
| Race | 2.27 | 2.72 | 1, 167 | 0.70 | .41 | ||
| Intimate partner in home | 0.29 | 2.96 | 1, 177 | 0.01 | .92 | ||
| ABAS version | 9.08 | 2.56 | 1, 342 | 12.63 | .001 | * | |
| SES | -2.72 | 1.26 | 1, 164 | 4.62 | .03 | * | |
| Age at injury | 1.02 | 1.32 | 1, 366 | 0.59 | .44 | ||
| Time since injury | 5.13 | 2.28 | 1, 180 | 1.99 | .16 | ||
| Group | 2, 312 | 3.88 | .02 | * | |||
| HOME score | 2.16 | 2.28 | 1, 318 | 5.40 | .02 | * | |
| Group X time since injury | 2, 160 | 0.77 | .47 | ||||
| HOME X time since injury | -1.15 | 2.22 | 1, 153 | 3.18 | .08 | ||
| Group X HOME | 2, 311 | 1.21 | .30 | ||||
| Group X HOME X time since injury | 2, 153 | 3.72 | .03 | * | |||
| PKBS/HCSBS Social Competence z score | Premorbid rating | 0.45 | 0.05 | 1, 186 | 69.88 | <.001 | |
| Sex | 0.18 | 0.09 | 1, 169 | 3.86 | .05 | ||
| Race | 0.02 | 0.12 | 1, 178 | 0.03 | .86 | ||
| Intimate partner in home | 0.27 | 0.13 | 1, 185 | 4.20 | .04 | * | |
| Test version | 0.24 | 0.10 | 1, 310 | 5.72 | .02 | * | |
| SES | 0.02 | 0.05 | 1, 173 | 0.21 | .65 | ||
| Age at injury | 0.04 | 0.05 | 1, 335 | 0.44 | .51 | ||
| Group | 2, 173 | 5.62 | .003 | * | |||
| Authoritative parenting | 0.16 | 0.04 | 1, 385 | 15.97 | <.001 | * | |
| Permissive parenting | -0.15 | 0.04 | 1, 420 | 14.67 | <.001 | * |
Significant effect, p < .05.
Note: Model estimates are based on raw scores for all measures. Model estimates are not given for effects involving group membership, which combines separate contrasts comparing (1) severe TBI and OI groups and (2) complicated mild/moderate TBI and OI groups. Df = degrees of freedom. SES = Socioeconomic status. CBCL = Child Behavior Checklist. ABAS = Adaptive Behavior Assessment System. GAC = General Adaptive Composite. PKBS = Preschool and Kindergarten Behavior Scales. HCSBS = Home and Community Social and Behavior Scales. HOME = Home Observation for Measures of the Environment.
Figure 1.

Mean CBCL Total Problem Scores at 6, 12, and 18 months Post-Injury as a Function of Group Membership and Permissive Parenting Style (low vs. high).
Figure 2.
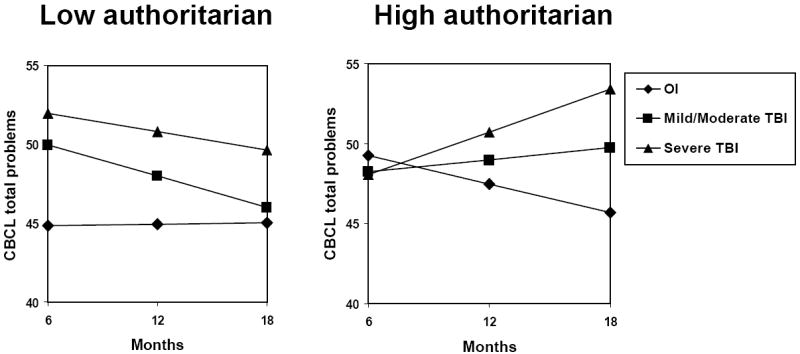
Mean CBCL Total Scores at 6, 12, and 18 months Post-Injury as a Function of Group Membership and Authoritarian Parenting Style (low vs. high).
Neither of the other aspects of the family environment (i.e., HOME, FAD-GF) interacted with group membership to predict behavioral adjustment. Better family functioning as measured by the FAD-GF was associated with better behavioral adjustment, but primarily at the final assessment 18 months post-injury, as reflected in a small but significant FAD-GF X time interaction (standardized estimate = .11). The HOME was not a significant predictor of behavioral adjustment.
Several covariates were significant predictors of behavioral adjustment, all with relationships that were small in magnitude. Children with more premorbid behavioral problems had higher post-injury ratings on the CBCL (standardized estimate = .69), as did those whose parents were of lower socioeconomic status (standardized estimate = - .08) or did not have intimate partners in the home (standardized estimate = -.25). Parent ratings were also higher on the preschool version of the CBCL than on the school-age version (standardized estimate = -.16).
Adaptive Functioning
In the analysis of the ABAS General Adaptive Composite (see Table 4), the interaction of group membership, the HOME, and time post injury was significant. The interaction was medium in magnitude for the severe TBI group (standardized estimate = -.52) but not significant for the moderate TBI group (standardized estimate = .18). We estimated mean ABAS General Adaptive Composite scores for children into those with low and high scores on the HOME to illustrate the interaction. Figure 3 shows that lower quality home environments were associated with increases in group differences in adaptive functioning over time for those with complicated-mild/moderate TBI; for the severe TBI group, differences were initially more pronounced for children from lower quality homes, but this did not hold true over time. Neither parenting style nor family functioning were predictors of children’s adaptive functioning, either as main effects or in interaction with group membership or time post injury.
Figure 3.
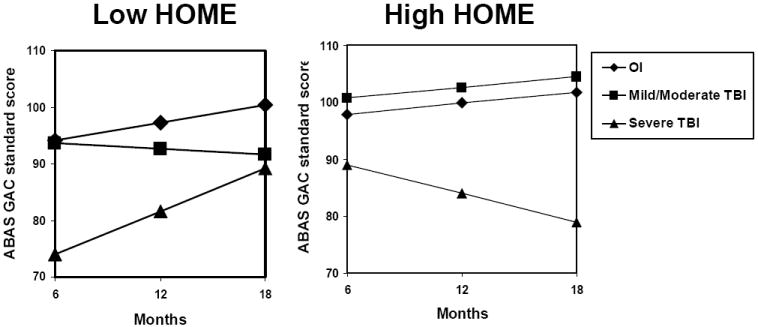
Mean ABAS General Adaptive Composite (GAC) Standard Score at 6, 12, and 18 months Post-Injury as a Function of Group Membership and Total HOME Score (low vs. high).
Several covariates predicted adaptive functioning, with effects that were small to large in magnitude. Children with better premorbid adaptive functioning had higher post-injury ratings on the ABAS (standardized estimate = .59), as did those whose parents had lower socioeconomic status (standardized estimate = -.13). Parent ratings were also higher on the school-age version of the ABAS than on the preschool version (standardized estimate = .41).
Social Competence
Social competence as measured by the PKBS/HCSBS composites was not moderated by the family environment (see Table 4). The group main effect was significant, largely because the severe TBI group displayed lower social competence than the OI group. The difference was of medium magnitude (standardized estimate = -.53). However, the group difference was not moderated by any of the measures of the family environment. Social competence was predicted by higher levels of authoritative parenting (standardized estimate = .16) and lower levels of permissive parenting (standardized estimate = -.15), but these small to medium relationships did not vary across groups or time. Neither family functioning nor the quality of the home environment was associated with social competence.
Social competence was also related to several covariates, with small to large effect sizes. Post-injury ratings on the PKBS/HCSBS were higher in children with better premorbid social competence (standardized estimate = .44) and among those whose caregivers had intimate partners in the home (standardized estimate = .28). Parent ratings were also higher on the HCSBS than on the PKBS (standardized estimate = .24), and increased with time post-injury (standardized estimate = .19).
Discussion
The findings indicate that the family environment accounts for significant variance in psychosocial outcomes following TBI in young children. The family environment was an independent predictor of behavioral adjustment and social competence across groups, but not of adaptive functioning (i.e., CBCL and PKBS/HCSBS, but not ABAS). More specifically, better family functioning predicted better behavioral adjustment at 18 months post-injury, authoritative parenting predicted better social competence across time, and permissive parenting predicted worse social competence across time; and these relationships held true for both children with TBI and those with OI. Consistent with previous research (Anderson et al., 2006; Catroppa et al., 2008), the results provide support for the notion that the family environment is an important predictor of young children’s functioning after TBI, and must be considered along with injury-related variables in predicting psychosocial outcomes.
Even more critically, the findings are consistent with our hypothesis that the family environment is a significant moderator of the impact of TBI. The family environment moderated group differences in behavioral adjustment and adaptive functioning, but not in social competence (i.e., CBCL and ABAS, but not PKBS/HCSBS). More specifically, parenting style moderated behavioral adjustment, with more pronounced effects of TBI seen among children whose parents reported higher levels of permissive and authoritarian parenting; and the quality of the home environment moderated adaptive functioning, with more pronounced group differences tending to be seen among children from lower quality homes. These findings extend existing research, which has not specifically examined the moderating influence of the family environment on the outcomes of young children with TBI. Given the low probability of detecting interactions in non-experimental research designs (McClelland & Judd, 1993), the presence of multiple significant interactions, all of which were of a similar nature, argues strongly for the existence of a complex interplay between the damaged brain and its environmental context during recovery from TBI in young children.
Notably, the moderating effect of the family environment varied as a function of multiple factors, including injury severity, time post injury, the specific dimension of the environment under consideration, and the type of outcome assessed (Taylor & Alden, 1997). With regard to injury severity, the moderating effects of the family environment were most consistent for children with complicated mild to moderate TBI, whose psychosocial function worsened over time in the context of more permissive and authoritarian parenting and lower quality home environments. In contrast, the moderating role of the family environment actually appeared to wane across time for children with severe TBI, who consistently showed deficits in psychosocial functioning by 18 months post-injury regardless of the family environment, despite early variability in outcomes attributable to the family environment. In a previous study of children sustaining TBI in later childhood, the moderating effects of the family environment were most apparent for those with severe TBI (Taylor et al., 2002; Yeates et al., 1997, 2002). The contrast between these findings suggest that children who sustain severe TBI at a young age may be less able to overcome the deleterious effects of those injuries than older children, even in the context of a supportive family environment. In contrast, young children with less severe TBI may be more likely to offset the effects of their injuries in a supportive environment, but are vulnerable to deleterious effects in less positive environments.
The moderating role of the family environment also varied as a function of time since injury. For instance, high levels of authoritarian parenting were associated with better behavioral adjustment at 6 months post injury, but with worse adjustment at 18 months. This result suggests that authoritarian parenting may suppress behavior problems initially following TBI in young children, but is not effective and may actually exacerbate problems over the longer term. More broadly, the finding suggests that the moderating influence of the family environment can change over time, presumably depending on the status of children’s recovery from TBI and corresponding changes in how environmental contingencies help shape their behavior.
The role of the family environment also may vary according to the specific dimension of the environment being considered. In the current study, parenting and the quality of the home environment were more consistently related to psychosocial outcomes than was global family functioning. This may reflect a stronger influence of parenting style and the quality of the home environment than of family functioning on children’s psychosocial development (Gottfried & Gottfried, 1984). Another possibility is that the influence of family functioning is largely indirect, and actually mediated by its impact on parenting and the stimulation offered by the home environment. Statistical analyses of complex causal models would be needed to differentiate among these competing explanations.
With regard to outcome measures, injury severity helps account for both cognitive and behavioral outcomes in this sample, but the family environment is more closely related to the behavioral outcomes assessed in this study than to the cognitive outcomes reported previously (Taylor et al., 2008). Family risk factors also have been found to exacerbate the psychosocial outcomes associated with prematurity and very low birth weight (Breslau, 1995), but are less predictive of other developmental outcomes (Bendersky & Lewis, 1994; Hack et al., 1992). A possible explanation for these related findings is that cognitive functioning in young children depends primarily upon the integrity of the central nervous system following a neurological insult like TBI, and hence is less affected by the family environment. In contrast, psychosocial outcomes are likely to depend not only on the integrity of the central nervous system, but also on the many environmental influences on behavior. Future research is needed that expands on the current findings by investigating more discrete psychosocial outcomes than the broad-based measures examined in this study.
Although the focus of this study was the moderating influence of the family environment on psychosocial outcomes following TBI in young children, we should acknowledge that children who suffer traumatic injuries not involving the brain may also be vulnerable to psychosocial difficulties. Moreover, the degree to which they are at risk may be related to the severity or nature of their injuries (Stancin et al., 2001). In the current study, very few of the children with orthopedic injuries suffered severe injuries requiring multiple surgeries or resulting in disfigurement or significant physical disability. However, such children are probably at more risk of psychosocial difficulties, and their outcomes may also be moderated by the family environment in a manner akin to that shown in the current study to characterize children with TBI.
The current study is characterized by several shortcomings. First, analyses were constrained to an examination of linear change post-injury because of the limited number of time points at which outcome data were collected. Future studies should involve data collection at more than three time points, to increase the reliability with which linear change is estimated as well as to permit modeling of non-linear change. Measurement issues are also a potential concern in the current study. The ratings of parenting style and family functioning were provided by parents, who also completed ratings of psychosocial outcomes. Thus, shared rater variance may have inflated the correlations found between those predictors and outcomes; however, this should not have confounded the assessment of the moderating effects of the family environment, as long as the inflation due to shared rater variance was similar for both the TBI and OI groups. Another measurement limitation was the use of different test versions for children of different ages. On all three measures of psychosocial functioning, some children were rated using the preschool version of the test while others were rated using the school-aged version. Test version was included as a covariate in data analyses, thereby controlling for consistently higher ratings on the preschool version of all three measures. However, we cannot be certain whether differences in test versions had inadvertent effects on group comparisons.
Another weakness is that the family environment was only measured once, shortly after the injury. An alternative explanation for the apparent decline in the moderating influence of the family environment among the severe TBI group is that the family environments of children with severe TBI may be more subject to change as a consequence of the injury, and thus the early post-injury family environment may become less predictive with time for those children. Future studies are needed to explore the potentially bidirectional relationships over time between the family environment and children’s psychosocial outcomes (Taylor et al., 2001). A related concern is that the study also did not take into account the potential influences of educational, rehabilitative, and other treatment services. A significant proportion of children with TBI received services outside the home, and such services could have influenced both family functioning and children’s psychosocial outcomes, potentially reducing the impact of the pre-and early post-injury family environment, perhaps especially in the severe TBI group. Attempting to assess the impact of these services is fraught with difficulty, because their provision is inevitably confounded with injury severity in the context of a naturalistic study. However, we acknowledge that they could affect the relationship between the pre- and early post-injury family environment and children’s subsequent psychosocial outcomes.
Despite these weaknesses, the results of the current study have important clinical implications. They suggest that rehabilitation programs should devote resources not only to the child who has suffered a TBI, but also to the child’s family. To the extent that the family environment is related to psychosocial outcomes, and actually moderate the effects of TBI, rehabilitative interventions should involve efforts to assess parenting skills and home environments, identify families that are at risk, and foster more effective parenting and the provision of developmentally-appropriate stimulation at home. We have previously shown in this sample that TBI results in a disruption of reciprocity in parent-child interactions, so that the usual positive benefits of warm, responsive parenting are less apparent for young children with TBI (Wade et al., 2008). Recent studies with parents of children with very low birth weight have shown that these parenting behaviors can be increased through intervention resulting in improved cognitive development (Smith, Landry, & Swank, 2005). These findings suggest that parenting interventions could be adapted to improve developmental outcomes following TBI in young children (Wade, Oberjohn, Burkhardt, & Greenberg, in press).
Acknowledgments
The research reported here was supported by grant R01 HD42729 to Dr. Wade from NICHD, in part by USPHS NIH Grant M01 RR 08084, and by Trauma Research grants from the State of Ohio Emergency Medical Services. Dr. Yeates received support from career development grant K02 HD44099 from NICHD during the conduct of the research. The authors wish to acknowledge the contributions of Christine Abraham, Andrea Beebe, Lori Bernard, Anne Birnbaum, Beth Bishop, Tammy Matecun, Karen Oberjohn, Elizabeth Roth, and Elizabeth Shaver in data collection and coding. We also thank Nori Minich for her assistance in data analysis. The Cincinnati Children’s Medical Center Trauma Registry, Rainbow Pediatric Trauma Center, Rainbow Babies & Children’s Hospital, Nationwide Children’s Hospital Trauma Program, and MetroHealth Center Department of Pediatrics and Trauma Registry provided assistance with recruitment.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/neu
References
- Achenbach TM, Rescorla LA. Manual for ASEBA Preschool Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2000. [Google Scholar]
- Achenbach TM, Rescorla LA. Manual for ASEBA School-Aged Forms & Profiles. Burlington, VT: University of Vermont, Research Center for Children, Youth, & Families; 2001. [Google Scholar]
- Anderson VA, Catroppa C, Dudgeon P, Morse SA, Haritou F, Rosenfeld JV. Understanding predictors of functional recovery and outcome 30 months following early childhood head injury. Neuropsychology. 2006;20:42–57. doi: 10.1037/0894-4105.20.1.42. [DOI] [PubMed] [Google Scholar]
- Anderson VA, Catroppa C, Morse S, Haritou F, Rosenfeld J. Functional plasticity or vulnerability after early brain injury? Pediatrics. 2005;116:1374–1382. doi: 10.1542/peds.2004-1728. [DOI] [PubMed] [Google Scholar]
- Baumrind D. Current patterns of parental authority. Developmental Psychology Monographs. 1971;4:1–103. [Google Scholar]
- Bendersky M, Lewis M. Environmental risk, biological risk, and developmental outcome. Developmental Psychology. 1994;30:184–194. [Google Scholar]
- Bradley RH, Caldwell BM. The HOME Inventory and family demographics. Developmental Psychology. 1984;20:315–320. [Google Scholar]
- Breslau N. Psychiatric sequelae of low birth weight. Epidemiologic Reviews. 1995;17:96–106. doi: 10.1093/oxfordjournals.epirev.a036191. [DOI] [PubMed] [Google Scholar]
- Byles J, Byrne C, Boyle MH, Oxford OR. Ontario Child Health Study: Reliability and validity of the General Functioning Scale of the McMaster Family Assessment Device. Family Process. 1988;27:97–104. doi: 10.1111/j.1545-5300.1988.00097.x. [DOI] [PubMed] [Google Scholar]
- Caldwell B, Bradley R. Home Observation for Measurement of the Environment. Little Rock: University of Arkansas at Little Rock; 1984. [Google Scholar]
- Catroppa C, Anderson VA, Morse SA, Haritou F, Rosenfeld JV. Outcome and predictors of functional recovery 5 years following pediatric traumatic brain injury. Journal of Pediatric Psychology. 2008;33:707–718. doi: 10.1093/jpepsy/jsn006. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Collins WA, Maccoby EE, Steinberg L, Hetherington EM, Bornstein MH. Contemporary research on parenting: The case for nature and nurture. American Psychologist. 2000;55:218–232. [PubMed] [Google Scholar]
- Elliott C. Differential Ability Scales: Introductory and technical handbook. San Antonio, TX: Psychological Corporation; 1990. [Google Scholar]
- Ewing-Cobbs L, Barnes M, Fletcher JM, Levin HS, Swank PR, Song J. Modeling of longitudinal academic achievement scores after pediatric traumatic brain injury. Developmental Neuropsychology. 2004a;25:107–133. doi: 10.1080/87565641.2004.9651924. [DOI] [PubMed] [Google Scholar]
- Ewing-Cobbs L, Fletcher JM, Levin HS, Francis DJ, Davidson K, Miner ME. Longitudinal neuropsychological outcome in infants and preschoolers with TBI. Journal of the International Neuropsychological Society. 1997;3:581–591. [PubMed] [Google Scholar]
- Ewing-Cobbs L, Prasad MR, Kramer L, Cox CS, Jr, Baumgartner J, Fletcher S, Mendez D, Barnes M, Zhang X, Swank P. Late intellectual and academic outcomes following traumatic brain injury sustained during early childhood. Journal of Neurosurgery. 2006;105:2887–2896. doi: 10.3171/ped.2006.105.4.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewing-Cobbs L, Prasad MR, Landry SH, Kramer L, DeLeon R. Executive functions following traumatic brain injury in young children: A preliminary analysis. Developmental Neuropsychology. 2004b;26:487–512. doi: 10.1207/s15326942dn2601_7. [DOI] [PubMed] [Google Scholar]
- Fay TB, Yeates KO, Wade SL, Drotar D, Stancin T, Taylor HG. Predicting longitudinal patterns of functional deficits in children with traumatic brain injury. Neuropsychology. 2009;23:271–282. doi: 10.1037/a0014936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fletcher JM, Ewing-Cobbs L, Miner M, Levin H, Eisenberg H. Behavioral changes after closed head injury in children. Journal of Consulting and Clinical Psychology. 1990;58:93–98. doi: 10.1037//0022-006x.58.1.93. [DOI] [PubMed] [Google Scholar]
- Fletcher JM, Levin HS, Lachar D, Kusnerik L, Harward H, Mendelsohn D, Lilly MA. Behavioral outcomes after pediatric closed head injury: Relationships with age, severity, and lesion size. Journal of Child Neurology. 1996;11:283–290. doi: 10.1177/088307389601100404. [DOI] [PubMed] [Google Scholar]
- Gottfried AW, Gottfried AE. Home environment and cognitive development in young children of middle socioeconomic status families. In: Gottfried AW, editor. Home environment and early cognitive development: Longitudinal research. New York: Academic Press; 1984. pp. 57–112. [Google Scholar]
- Hack M, Breslau N, Aram B, Weissman B, Klein N, Borawski-Clark E. The effect of very low birth weight and social risk on neurocognitive abilities at school age. Developmental and Behavioral Pediatrics. 1992;13:412–420. [PubMed] [Google Scholar]
- Harrison PL, Oakland T. Adaptive Behavior Assessment System Second Edition Manual. San Antonio: Psychological Corporation; 2003. [Google Scholar]
- Kraus JF. Epidemiological features of brain injury in children: Occurrence, children at risk, causes and manner of injury, severity, and outcomes. In: Broman SH, Michel ME, editors. Traumatic head injury in children. New York: Oxford University Press; 1995. pp. 22–39. [Google Scholar]
- Landry SH, Smith KE, Swank PR. The importance of parenting during early childhood for school-age development. Developmental Neuropsychology. 2003;24:559–592. doi: 10.1080/87565641.2003.9651911. [DOI] [PubMed] [Google Scholar]
- Langlois JA, Rutland-Brown W, Thomas KE. Traumatic brain injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2006. [Google Scholar]
- Lund J, Merrell KW. Social and antisocial behavior of children with learning and behavioral disorders: Construct validity of the Home and Community Social Behavior Scales. Journal of Psychoeducational Assessment. 2001;19:112–122. [Google Scholar]
- McClelland GH, Judd CM. Statistical difficulties of detecting interactions and moderator effects. Psychological Bulletin. 1993;114:376–390. doi: 10.1037/0033-2909.114.2.376. [DOI] [PubMed] [Google Scholar]
- Merrell KW. Social-emotional assessment in early childhood: The Preschool and Kindergarten Behavior Scales. Journal of Early Intervention. 1996;20:132–145. [Google Scholar]
- Merrell K. Preschool and Kindergarten Behavior Scales. second edition. Austin: PRO-ED, Inc; 2002. [Google Scholar]
- Merrell KW, Boelter E. An investigation of the relationships between social behavior and ADHD in children and youth: Construct validity of the Home and Community Behavior Scales. Journal of Emotional and Behavioral Disorders. 2001;9:260–269. [Google Scholar]
- Merrell KW, Caldarella P. Home & Community Social Behavior Scales. Eugene, OR: Assessment Intervention Resources; 2002. [Google Scholar]
- Merrell KW, Streeter AL, Boelter EW. Validity of the Home and Community Social Behavior Scales: Comparisons with five behavior-rating scales. Psychology in the Schools. 2001;38:313–325. [Google Scholar]
- Miller IW, Bishop DS, Epstein NB, Keitner GI. The McMaster Family Assessment Device: Reliability and validity. Journal of Marital and Family Therapy. 1985;11:345–356. [Google Scholar]
- Oakland T, Harrison P. Adaptive behaviors and skills: An introduction. In: Oakland T, Harrison P, editors. Adaptive Behavior Assessment System-II: Clinical uses and interpretations. New York: Elsevier; in press. [Google Scholar]
- Osler T, Bakker SP, Long WA. A modification of the injury severity score that both improves accuracy and simplifies scoring. Journal of Trauma. 1997;43:922–925. doi: 10.1097/00005373-199712000-00009. [DOI] [PubMed] [Google Scholar]
- Robinson CC, Mandleco B, Olsen SF, Hart CH. Authoritative, authoritarian, and permissive parenting practices: Development of a new measure. Psychological Reports. 1995;77:819–830. [Google Scholar]
- Robinson CC, Mandleco B, Olsen SF, Hart CH. The parenting styles and dimensions questionnaire. In: Perlmutter BF, Touliatos J, Holden GW, editors. Handbook of family measurement techniques: Vol 3 Instruments and Index. Thousand Oaks, CA: Sage; 2001. pp. 319–321. [Google Scholar]
- Schwartz L, Taylor HG, Drotar D, Yeates KO, Wade SL, Stancin T. Long-term behavior problems after pediatric traumatic brain injury: Prevalence, predictors, and correlates. Journal of Pediatric Psychology. 2003;28:251–264. doi: 10.1093/jpepsy/jsg013. [DOI] [PubMed] [Google Scholar]
- Smith KE, Landry SH, Swank PR. The influence of decreased parental resources on the efficacy of a responsive parenting intervention. Journal of Consulting and Clinical Psychology. 2005;73:711–720. doi: 10.1037/0022-006X.73.4.711. [DOI] [PubMed] [Google Scholar]
- Stancin T, Drotar D, Taylor HG, Yeates KO, Wade SL, Minich NM. Health-related quality of life of children and adolescents after traumatic brain injury. Pediatrics. 2002;109 doi: 10.1542/peds.109.2.e34. URL: http://www.pediatrics.org/cgi/content/full/109/2/e34. [DOI] [PubMed]
- Stancin T, Kaugars AS, Thompson GH, Taylor HG, Yeates KO, Wade S, Drotar D. Child and family functioning 6 and 12 months after a serious pediatric fracture. Journal of Trauma: Injury, Infection, and Critical Care. 2001;51:69–76. doi: 10.1097/00005373-200107000-00011. [DOI] [PubMed] [Google Scholar]
- Taylor HG, Alden J. Age-related differences in outcome following childhood brain injury: An introduction and overview. Journal of the International Neuropsychological Society. 1997;3:555–567. [PubMed] [Google Scholar]
- Taylor HG, Swartwout MD, Yeates KO, Walz NC, Stancin T, Wade SL. Traumatic brain injury in young children: Post-acute effects on cognitive and school readiness skills. Journal of the International Neuropsychological Society. 2008;14:734–745. doi: 10.1017/S1355617708081150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor HG, Yeates KO, Wade SL, Drotar D, Klein SK, Stancin T. Influences on first-year recovery from traumatic brain injury in children. Neuropsychology. 1999;13:76–89. doi: 10.1037//0894-4105.13.1.76. [DOI] [PubMed] [Google Scholar]
- Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Burant C. Bidirectional child-family influences on outcomes of traumatic brain injury in children. Journal of the International Neuropsychological Society. 2001;7:755–767. doi: 10.1017/s1355617701766118. [DOI] [PubMed] [Google Scholar]
- Taylor HG, Yeates KO, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of long- and short-term outcomes after traumatic brain injury in children: Behavior and achievement. Neuropsychology. 2002;16:15–27. doi: 10.1037//0894-4105.16.1.15. [DOI] [PubMed] [Google Scholar]
- Wade SL, Oberjohn K, Burkhardt A, Greenberg I. Feasibility and preliminary efficacy of a web-based parenting skills program for young children with traumatic brain injury. Journal of Head Trauma Rehabilitation. doi: 10.1097/HTR.0b013e3181ad6680. in press. [DOI] [PubMed] [Google Scholar]
- Wade SL, Taylor HG, Walz NC, Salisbury S, Stancin T, Bernard LA, Oberjohn K, Yeates KO. Parent-child interactions during the initial weeks following brain injury in young children. Rehabilitation Psychology. 2008;53:180–190. doi: 10.1037/0090-5550.53.2.180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yeates KO, Swift E, Taylor HG, Wade SL, Drotar D, Stancin T, Minich N. Short- and long-term social outcomes following pediatric traumatic brain injury. Journal of the International Neuropsychological Society. 2004;10:412–426. doi: 10.1017/S1355617704103093. [DOI] [PubMed] [Google Scholar]
- Yeates KO, Taylor HG, Drotar D, Wade S, Klein S, Stancin T. Premorbid family environment as a predictor of neurobehavioral outcomes following pediatric TBI. Journal of the International Neuropsychological Society. 1997;3:617–630. [PubMed] [Google Scholar]
- Yeates KO, Taylor HG, Wade SL, Drotar D, Stancin T, Minich N. A prospective study of short- and long-term neuropsychological outcomes after traumatic brain injury in children. Neuropsychology. 2002;16:514–523. doi: 10.1037//0894-4105.16.4.514. [DOI] [PubMed] [Google Scholar]


