Abstract
Although multifactorial fall prevention interventions have been shown to reduce falls and injurious falls, their translation into clinical settings has been limited. We describe a hospital-based, fall prevention clinic established to increase availability of preventive care for falls. Outcomes for forty-three adults aged 65+ seen during the clinic’s first six months of operation were compared to outcomes for 86 age-, gender-, and race-matched controls; all persons included in analyses received primary care at the hospital’s geriatrics clinic. Non-significant differences in falls, injurious falls, and fall-related healthcare use by study group in multivariate adjusted models were observed, likely due to the small, fixed sample size. The percent experiencing any injurious falls during the follow-up period was comparable for fall clinic visitors and controls (14% vs. 13%), despite a dramatic difference at baseline (42% of clinic visitors vs. 15% of controls). Fall-related healthcare use was higher for clinic visitors during the baseline period (21%, vs. 12% for controls) and decreased slightly (to 19%) during follow-up; differences in fall-related healthcare use by study group from baseline to follow-up were non-significant. These findings, although preliminary due both to the small sample size and the baseline difference between the groups in fall rates, suggest that being seen in a fall prevention clinic may reduce injurious falls. Additional studies will be necessary to conclusively determine the effects of multifactorial fall risk assessment and management delivered by mid-level providers working in real-world, clinical practice settings on key outcomes, including injurious falls, downstream fall-related healthcare use, and costs.
Keywords: fall prevention clinic, fall prevention, falls, injurious falls, emergency department, hospitalization, utilization
One-third of community dwelling adults aged 65 or older and one-half of adults over age 80 fall at least once each year.1,2 Falls are the most common cause of death due to unintentional injury among adults in this age category.3 Falls are associated with considerable morbidity, restricted activity, functional decline, and nursing home admission.3,4 Falls account for approximately 10% of visits to an emergency department and 6% of hospitalizations among Medicare beneficiaries.4
Research supports the effectiveness of multifactorial fall prevention programs: A multifactorial fall risk assessment and management program was consistently the most effective fall prevention strategy among community living elders, associated with an 18% reduction in falls and a 37% reduction in the rate of falls per person-month.5
However, most older adults who report having fallen do not receive a basic fall examination.6 Others have also observed that fall prevention is frequently not attended to in clinical practice,4 and locally collected data suggested that patients seeking medical attention after a fall received follow-up for the acute fall-related injury but no preventive care for falls.7
The Fall Prevention Clinic (FPC) at Harborview Medical Center (HMC) in Seattle, Washington began operation in June 2005 to address this issue. The primary aim of the clinic is to make evidence-based care for falls readily available. One of us (EAP) engaged in discussions with hospital leadership and in program planning over a one-year period prior to the clinic’s establishment; leadership was supportive of the idea from the outset.
This research is an evaluation of the clinic in terms of its impacts. We sought to determine whether those seen in FPC had reductions in falls, injurious falls, and fall-related healthcare use, compared to a control group. We hypothesized that fall-related healthcare use would be reduced after the FPC visit, and that this would occur via a reduction in injurious falls. The most common treatment recommendations given to patients evaluated in the FPC, their reported adherence to these recommendations at follow-up, and payments to the hospital for FPC visits were also investigated.
METHODS
Setting: Fall Prevention Clinic (FPC) at Harborview Medical Center (HMC)
The setting for this study was the FPC at HMC. HMC is a public hospital delivering comprehensive medical services to the residents of inner city Seattle. Owned by King County, governed by the HMC Board of Trustees, and managed under contract by the University of Washington (UW), it is part of the UW Academic Medical Center.
The FPC is staffed by a nurse practitioner (ARNP) and operates one half-day a week. The initial clinic visit is one hour long and consists of a comprehensive fall risk assessment, including: A structured algorithm, adapted from the ACOVE II intervention8,9 to identify risk factors for falls; a focused medical evaluation (vision, gait, balance, strength, postural vital signs, and cognitive and functional status); and recommendations for treatment of modifiable risk factors (e.g., physical therapy referral, environmental modifications, referral for eye exam).5 Each patient also receives education about fall prevention, physical activity, and home safety.
The ARNP usually recommends a follow-up visit to the FPC within a few months time. Typically 30 minutes in length, follow-ups focus on whether the patient has any questions about his/her treatment plan to prevent falls, is afraid of falling, and is adhering to treatment recommendations from the initial visit. Barriers to adherence are identified and addressed, and gait, balance, and strength are reassessed. All forms used in the FPC are available upon request.
Visits to the FPC are billed to the patient’s primary and (if available) secondary insurers. These insurers include Medicare and Medicaid as well as other commercial carriers. The initial visit is in nearly all instances billed as a comprehensive consultation.
Study Design
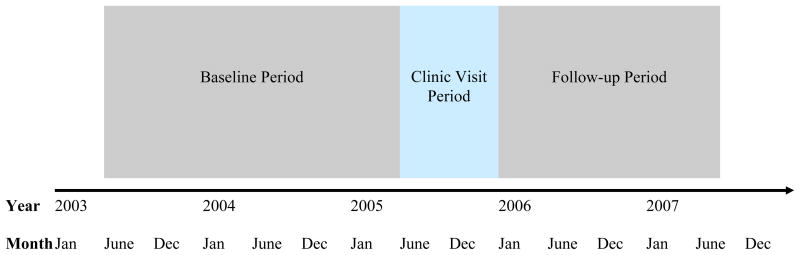
The analysis was designed along the lines of firm system research,10 wherein an outpatient clinic is subdivided into smaller units (firms), and changes are then introduced with one unit but not the other(s) and effects on outcomes are subsequently assessed. The time period of visits to the FPC (clinic visit period) was June 1, 2005 through December 31, 2005 (7 months). June 1, 2003 through May 31, 2005 (24 months) marked the baseline period, and January 1, 2006 through June 30, 2007 (18 months) comprised the follow-up period of observation (see Figure). We used a retrospective, comparison group design to answer our study questions.
Figure 1.
Study Timeline
Participants
Source of Study Participants
Study participants were primary care patients of the geriatric medicine clinic at HMC. The clinic has two sessions each week, one on Tuesday, the other on Thursday, wherein academic geriatricians see patients. All patients must be at least 65 years of age and community dwelling to receive primary care in this clinic. About two-thirds of the clinic’s patients are women, and one-third are non-white. Most have two or more chronic conditions (Phelan, unpublished data). The number of patients seen on a routine basis for primary care is approximately 650.
When the FPC began operating, geriatricians practicing in the Thursday clinic were asked to delay letting their patients know about the clinic for six months, so that a control group could be drawn from their practices, as those practices were comprised of patients that were comparable to intervention patients, insofar as intervention patients were to be drawn from the practices of academic geriatricians seeing patients on Tuesdays rather than Thursdays. Providers whose clinic was held on Tuesdays were asked to let their patients know of the clinic as soon as it opened and to encourage evaluation therein.
Fall Prevention Clinic Visitors
The FPC visitors (n=43) were patients referred by their Tuesday geriatrician provider to the FPC between June 1, 2005 and December 31, 2005. Providers were not asked to invite patients to be seen in the FPC based on any particular predisposition to fall, although many patients who ultimately elected to be seen did have a history of falls. A few patients were referred to the FPC from the HMC emergency department (ED). We elected to include these persons in our analysis, since most were primary care patients of HMC outpatient clinics and thus were from the same population base.
Controls
The control group (n=86) was comprised of patients who were explicitly not referred to the FPC between June 1, 2005 and December 31, 2005. Thursday providers were informed that they could begin referring their patients as of January 1, 2006. Controls were matched two to one to FPC patients on age, gender, and whenever possible, race.
Data Collection
Abstraction Methods
Data about demographic characteristics, health insurance, medications, comorbid conditions, fall history, and fall-related injury came from a thorough review of electronic medical records (EMR). Data on healthcare use were derived from automated databases of HMC’s quality improvement department. One of the authors (MM) abstracted all data. The abstraction process was monitored by one of us (EAP), who vetted abstraction questions from the abstractor whenever questions about interpretation of information contained within the medical record arose. As this was a quality improvement project, all authors, including the abstractor, were familiar with the FPC’s purpose; however, specific study hypotheses were known only to the senior author and not discussed with the abstractor.
Variable Definitions
Age on June 1, 2005, the first day of the clinic visit period, defined each patient’s age. Comorbid conditions and medications were those documented in the EMR at the time of the FPC visit (or at the first geriatric medicine clinic visit made during June-December 2005 for all control participants). All prescription medications, except for pro re nata (prn) medications, were counted; benzodiazepines were the only medication class specifically tracked, given their strong association with falls.11
Comorbid conditions identified in prior research as fall risk factors (e.g., arthritis, cognitive impairment) 12 and those common among the elderly (e.g., hypertension, diabetes) were abstracted from the EMR. Some comorbid conditions were grouped together for analysis purposes. For example, stroke included transient ischemic attack and cerebrovascular accident.
Fall-Related Outcome Measures
Classification of Outcome Occurrences into Baseline and Follow-Up Periods
Data on falls, fall-related injuries, and fall-related healthcare use occurring from June 2003 until the participant’s first FPC visit during the clinic visit period (June-December 2005) were included in the baseline period. The baseline period thus ranged from 24 to 30 months. We matched each control participant’s baseline period to that of the corresponding FPC participant. Follow-up data were derived from the time immediately following participants’ FPC visit during the clinic visit period to participants’ last recorded medical chart note, through June 30, 2007. Follow-up time averaged 1.6 years for the clinic group and 1.5 years for controls.
Falls
Falls were defined as “unintentionally coming to rest on the ground, floor, or other lower level from a standing, sitting, or horizontal position, not due to seizure, stroke, fainting, motor vehicle accident, or risky behavior (i.e. skiing, roof repair, drug overdose).”12 Any reference to falls in plural form (e.g., “fell multiple times”) was counted as two falls; in one case, a reference to “falls once per month” over a one year period was conservatively counted as six total fall events. Records were carefully screened to identify multiple reports of a single fall event.
Injurious falls
Fall-related injuries were divided into two categories, major and minor, and defined as any sequelae resulting from a fall. Major injuries included upper extremity, mid-body (pelvic, sacral, and multiple rib) and lower extremity fractures, and head injury. Minor injuries included soft tissue injury (abrasions, contusions, and lacerations), ligamentous injury, single rib fracture, broken tooth or teeth, and swollen body part. If more than one injury resulted from a fall, each injury was independently counted.
Fall-related healthcare use
The primary outcome was healthcare use (ED visit or hospitalization) resulting from a fall event. If a participant presented to an ED with a fall-related injury and was discharged, this was considered a fall-related ED visit. If a participant was admitted to a hospital on the same day as a reported fall, the hospital visit was considered fall-related.
Payments Received and ARNP Salary
Payments received by the hospital for FPC visits during the clinic visit period (June-December 2005) were determined from hospital administrative files. Salary paid to the ARNP by the hospital for staffing the clinic during the clinic visit period was also tracked. The ARNP salary was the amount of money paid to the ARNP for her work in the FPC only, and not the amount of her full-time salary.
Statistical Analyses
We calculated power for our fixed sample size. Estimating the annual incidence of falls to be 30–40% in the control group,1 and estimating that the Falls Clinic intervention would reduce the risk of falls among the clinic visitor group by 30% from baseline,5 with a fixed sample size of 43 FPC participants, and with a two-tailed significance level of 0.05, we estimated power to be ~80% for this outcome.
The data were analyzed using an intent-to-treat approach. Statistical analyses were performed using SPSS (version 13.0, SPSS Inc., Chicago, IL). FPC and control participants were compared on demographic and health characteristics, baseline fall-related characteristics, and fall-related healthcare use. Chi-square and t-tests were used to test for between-group differences on these variables. McNemar tests were used to assess the significance of differences in within-group proportions at baseline and follow-up for each fall-related outcome. Logistic regression models, one for each fall-related outcome measure (falls, injurious falls, and fall-related healthcare use, a composite outcome of ED visits and hospitalizations) as the dependent variable and study group (clinic visitor or control) as the primary independent variable were generated (hereinafter referred to as unadjusted models). Confounders adjusted for in each (adjusted) model for each outcome included age, gender, race, number of comorbidities (from 11, including hypertension, depression, arthritis, heart problems, vision problems, diabetes, dementia, anemia, stroke, syncope, and dizziness), number of medications, days of follow-up, and either a) one or more falls in the baseline period (yes/no) (for the falls and injurious falls regression models) or b) one or more ED visits or hospitalizations (yes/no) (for the fall-related healthcare use model). Depression was omitted as a covariate from adjusted models because it was highly correlated with comorbidity count. Results were considered statistically significant at p<0.05. This study was approved by the University of Washington’s Institutional Review Board.
RESULTS
Participant Flow
During the 7-month (from June 1, 2005 through December 31, 2005) clinic visit period, 43 patients were seen in the FPC, 35 (81%) of whom were referred by providers of the geriatric medicine clinic; the remainder were referred from the hospital’s ED. Of the 43 patients, 36 (84%) remained active in the hospital system and had medical chart notes available through the end of the follow-up period. Of the 7 lost to follow-up, 1 died and 1 discontinued care at HMC during the clinic visit period, and 2 died and 3 had no chart activity during the follow-up period.
Of the 86 controls, 64 (74%) remained active in the HMC system with chart notes updated through the follow-up period. Of the 22 lost to follow-up, 1 died and 4 had no medical chart activity during the clinic visit period, and 1 died, 3 discontinued care at HMC, and 13 had no medical chart activity during the follow-up period.
Participant Characteristics
Table 1 shows baseline demographic, health-related, and fall-related characteristics of participants. Cases and controls were balanced on age, gender, and race, as expected due to matching on those variables. FPC participants had a greater mean number of comorbidities (3.21 vs. 2.43, p=0.003) and a higher proportion experienced depression (48.8% vs. 23.3%, p=0.003) compared to controls. Nearly all those seen in the FPC had fallen at least once. The mean number of injurious falls was low in both groups, but significantly higher for the FPC group. Major and minor injuries were both more common among the FPC group, and for minor injuries, significantly so. A larger proportion of the FPC group had experienced one or more falls. The percent with any fall-related ED visits and hospitalizations during the baseline period was higher for the FPC group for both measures, though not significantly so.
Table 1.
Baseline Demographic, Health, and Fall-Related Characteristics of Study Participants, by Study Group
| Characteristic | FPC Group (N=43) | Control Group (N=86) | P-Value |
|---|---|---|---|
| Age, years, mean (± SD) | 78.5 (± 7.4) | 78.7 (± 7.5) | 0.90 |
| Female, % | 69.8 | 69.8 | 1.00 |
| Non-white race, % | 32.6 | 37.2 | 0.61 |
| Insurance, primary, %* | 0.46 | ||
| Medicare | 90.7 | 91.9 | |
| Medicaid | 4.7 | 4.7 | |
| Other | 4.6 | 3.5 | |
| Medications, number, mean (± SD) | 7.0 (± 3.1) | 5.9 (± 3.2) | 0.07 |
| Benzodiazepine use, % | 2.3 | 0 | 0.32 |
| Comorbidity, number, mean (± SD) | 3.21 (± 1.54) | 2.43 (± 1.31) | 0.003 |
| Comorbidity, % | |||
| Hypertension | 81.4 | 73.3 | 0.31 |
| Depression | 48.8 | 23.3 | 0.003 |
| Arthritis | 44.2 | 32.6 | 0.20 |
| Heart Problems† | 32.6 | 27.9 | 0.59 |
| Vision Problems‡ | 23.3 | 12.8 | 0.13 |
| Diabetes Mellitus | 20.9 | 11.6 | 0.16 |
| Dementia§ | 16.3 | 12.8 | 0.59 |
| Stroke|| | 4.7 | 12.8 | 0.15 |
| Falls, number, mean (± SD) | 1.58 (± 1.20) | 1.02 (± 1.94) | 0.09 |
| Injurious falls, number, mean (± SD) | 0.6 (± 0.8) | 0.2 (± 0.4) | 0.003 |
| Major injury, % | 18.6 | 8.1 | 0.08 |
| Minor injury, % | 23.3 | 8.1 | 0.017 |
| Fall frequency, % | <0.001 | ||
| 0 | 2.3 | 61.6 | |
| 1 | 65.1 | 17.4 | |
| ≥2 | 32.6 | 20.9 | |
| ED visit, fall-related, % | 20.9 | 11.6 | 0.16 |
| Hospitalization, fall-related, % | 7.0 | 2.3 | 0.20 |
Percentage totals may exceed 100 due to rounding.
Includes coronary heart disease, coronary artery disease, congestive heart failure, atrial fibrillation, aortic stenosis, murmur of aortic stenosis, aortic insufficiency, tachycardia syndrome, bradycardia syndrome, arrhythmia, idiopathic cardiomyopathy, restrictive cardiomyopathy, pacemaker, cardiac ischemia.
Includes cataracts, glaucoma, diplopia, diabetic retinopathy, retinal detachment, macular degeneration.
Includes Alzheimer’s disease, memory problems.
Includes TIA, CVA.
Program Implementation
Treatment Recommendations
Treatments recommended most frequently by the ARNP for FPC participants at their initial clinic visit were physical activity (100%), physical or occupational therapy (67%), an eye exam (67%), a change in medication (26%), a change in footwear or a podiatry evaluation (19%), hip protectors (14%), and a home safety assessment (9%).
Frequency of Follow-up Visits and Adherence to Treatment Recommendations
Among FPC visitors, 37% completed a follow-up visit, and 81% of those who completed a follow-up visit were working on at least one aspect of their treatment plan at follow-up.
Outcomes
Falls, Injurious Falls, and Fall-Related HealthCare Use by Study Group
Table 2 shows the percent of patients in each group in the baseline and follow-up periods for each fall-related outcome. Adjusted odds ratios (OR) and the 95% confidence intervals (CI) for the odds of patients in the FPC experiencing each outcome compared to controls is also given. The adjusted odds of each outcome were reduced for FPC participants, although confidence intervals crossed one in each case. Major injuries comprised 5% in each group at follow-up (P=1.00). Minor injuries occurred in 12% of the FPC group and 8% of controls at follow-up (P=0.52). The within-group differences in proportions between baseline and follow-up for the outcomes of falls (McNemar P<0.001) and injurious falls (McNemar P=0.004) were significant only for the FPC group.
Table 2.
Fall-Related Outcome Measures (Any Falls, Any Injurious Falls, Any Fall-Related Healthcare use), at Baseline and Follow-up, by Study Group (FPC N=43; Control N=86)
| -------------UNADJUSTED------------------ | -----ADJUSTED*----- | |||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | Unadjusted Odds Ratio | 95%CI | Adjusted Odds Ratio | 95%CI | |
| Any falls, % | 2.25 | 1.1, 4.8 | 0.83 | 0.3, 2.4 | ||
| FPC | 98 | 47 | ||||
| Controls | 38 | 28 | ||||
| Any injurious falls, % | 1.10 | 0.4, 3.2 | 0.57 | 0.2, 2.1 | ||
| FPC | 42 | 14 | ||||
| Controls | 15 | 13 | ||||
| Any healthcare use, %† | 1.56 | 0.6, 4.2 | 0.77 | 0.2, 2.5 | ||
| FPC | 21 | 19 | ||||
| Controls | 12 | 13 | ||||
Adjusted odds ratios represent the multivariate adjusted odds of the outcome measure in the FPC vs. the control group, obtained from logistic regression models of each follow-up outcome measure as the dependent variable and adjusting for age, sex, race, comorbidity count, medication count, days of follow-up, and the baseline value of the outcome measure.
Healthcare use defined as any fall-related ED visit or hospitalization.
Payments Received and ARNP Salary
Payments received by the hospital for FPC visits during the clinic visit period totaled $7,756. Salary for the ARNP to provide these services totaled $3,761.
DISCUSSION
Others have called for further work to confirm that the reductions in falls achieved in clinical trials are also being found in routine clinical practice.13 The results of this study showed that a FPC visit operating outside the context of a rigorously designed research study may have important effects on reducing falls, including injurious falls, among older adults with a history of falls. We observed a substantial reduction in the percents with falls (98%–47%=50% — Table 2) and injurious falls (42%–14%=28% — Table 2) among those older adults who had been seen in the FPC. During the follow-up period, the proportion with injurious falls in the FPC group was comparable to controls (14% vs. 13% — Table 2), whereas it had been substantially higher in the FPC group during the baseline period (42% vs. 15% — Table 2). The proportion of FPC participants sustaining major injuries (10%) in our study is consistent with published reports.4 Multivariate analyses were suggestive of reductions in falls and injurious falls related to the clinic intervention, although the small sample size limits the interpretability of these models. Additionally, the FPC was modestly income-generating for the hospital.
We identified a few studies of fall prevention clinics.14–16 One was a randomized trial in which participants were selected from a health insurance company database, aged ≥75 years, non-blind, free of Parkinson’s disease, and cognitively intact.15 The intervention, individually tailored, emphasized exercise, vision, and counseling. Rates of falls and injurious falls were assessed for one year using monthly fall calendars and telephone interviews. While the intervention reduced some fall risk factors, a decrease in fall-related outcomes (falls, injurious falls) was not observed. This may have been due to the fact that study participants were at a lower level of fall risk than those in our study.
A recently published, uncontrolled evaluation of outcomes for 13 Australian falls clinics and 454 elders represents the largest study of fall prevention clinics to date.14 Participants were similar to ours (i.e., mostly female, mean age ~78 years, at high fall risk [i.e., with a history of falls]). The intervention consisted of a multidisciplinary assessment and multifactorial intervention. Outcomes, assessed by self-report, included falls, injurious falls, and falls for which medical attention was sought. Each outcome was reduced >50% at follow-up compared to baseline, resembling our 51% reduction in falls and nearly 28% reduction in injurious falls at follow-up. Of note, our clinic is parsimonious in that a single interventionist (i.e., ARNP), as opposed to a multidisciplinary team, conducts assessments. Our approach may be more feasibly implemented in primary care settings.
A third study of falls clinics in the Veterans Administration in Florida and Puerto Rico is to our knowledge the only published study of falls clinics in the United States.16 This was an uncontrolled evaluation of an interdisciplinary team that assessed and managed 313 veterans (average age 73.5 years, 91% male) referred due to high fall risk. Assessments were lengthy (2 hours); treatment plans consisted of recommendations (usually related to medication adjustment) to the primary care provider and interventions implemented directly by the team. A significant, three-fold reduction in the mean number of falls at the 3-month follow-up was observed. Injurious falls and fall-related healthcare use were not assessed.
Findings from the above studies, taken together with our own, suggest that the protective effects of a falls clinic’s multifactorial intervention on falls and injurious falls may be limited to older adults with a history of falls. The full effects of such programs on downstream healthcare use and costs are as yet largely undetermined, although our results suggest a possible benefit on controlling fall-related healthcare use.
Strengths of our study include its evaluation of a real-world intervention, operating within the context of usual care and involving a heterogeneous group of elders, in contrast to randomized trials that apply strict eligibility criteria and generally have excluded elders with dementia. As such, our results help inform the question of whether multifactorial fall risk reduction efforts will benefit a broader segment of the community dwelling, elderly population at high risk of falls and injury. We were also able to identify a control group of age-, gender-, and race-matched older adults drawn from the same clinic as FPC visitors, which permitted us to conduct a controlled evaluation of key outcomes. Our design was conservative, in that controls could have been referred to the FPC during the follow-up period, which would tend to bias results towards the null. Finally, our study examined the effects of the FPC intervention over a fairly lengthy (18-month) follow-up period. While fall risk reduction was attained in other studies during shorter follow-up periods of observation,16 it is possible that these short-term benefits could diminish by the second year of follow-up, as has been seen in randomized trials of fall prevention interventions.17 A longer follow-up period is important, as it demonstrates that the effects of a multifactorial fall risk assessment with follow-up persist beyond the initial time period following the intervention.
Limitations to this study include that it was observational, without randomization of participants, with measured differences between the groups at baseline. Specifically, an important imbalance was the higher rate of falls in the FPC visitor group at baseline. We attempted to handle this imbalance in our analysis, by controlling for the presence of one or more falls in the baseline period (yes/no) in multivariate models. However, this analytic approach may not have fully accounted for the baseline differences between the groups on this measure. A second limitation is the possibility of incomplete data collection. While we carefully extracted data from medical records, we may have missed some reports of falls and fall-related healthcare use, particularly if care were received outside the health care system under study. More likely is the probability that some participants’ full fall history was not reflected in their medical records, as it may have gone unreported to health care providers. Only 41% of fallers reported their fall to their primary care provider in the veterans’ falls clinic study.16 In light of this, information on the specific number of falls, mean number of falls, and fall frequency may be underestimates. While medical records may under-capture events such as falls and fall-related injury, we have no reason to suspect differential rates of under-documentation by study group on our primary outcome of fall-related healthcare use, since these data were derived from administrative files. Some of our participants also had ambiguous reports of fall history (i.e., “fell several times”), which required us to estimate the actual number of falls; our estimates in these instances were conservative, again potentially creating an underestimate of actual fall events. A third limitation was our fixed sample size, which limited our power to detect significant differences between the study groups in multivariate analyses. Fourth, although our study included patients with dementia, due to small numbers (7 in the FPC group, 11 in the control group), we were unable to determine the effect of our intervention for this subgroup. Lastly, we did not control for some factors, such as activity restriction due to fear of falling, that may have affected the outcomes of falls and injurious falls; consideration should be given to adjusting for variables such as fear of falling in future studies examining these outcomes.
This study adds to the evidence supporting multifactorial risk assessment and extends that evidence by demonstrating that comprehensive fall risk assessment with follow-up provided by an ARNP in a real-world clinic setting may reduce falls and injurious falls among community-living elders with a history of falls. Such preventive care is likely to improve quality of life by averting the loss of independence that frequently follows an injurious fall. In addition, the opportunity for cost avoidance related to reductions in ED use and hospitalizations is substantial: Data from others suggest that incurring one or more injurious falls is associated with an increase in annual hospital costs of $11,042 and emergency department costs of $253.18 Thus, substantial health care savings to both fee-for-service and managed care Medicare could be realized if this form of preventive care for falls were made more widely available to large numbers of older persons. With larger evaluations of such programs, it is anticipated that best practices for reducing fall-related injuries and fall-related healthcare use will be definitively confirmed.
Acknowledgments
We would like to thank Susan Onstad from the Department of Decision Support, Harborview Medical Center, Seattle, Washington for her assistance in identifying the control group and providing healthcare utilization and income data for study participants.
This research was conducted while Dr. Phelan was a Paul Beeson Physician Faculty Scholars in Aging Research Program awardee. This research was also supported by Grant K23 AG20982 from the National Institute on Aging.
Footnotes
Conflict of Interest: The editor in chief has reviewed the conflict of interest checklist provided by the authors and has determined that the authors have no financial or any other kind of personal conflicts with this paper.
Sponsor’s Role: The sponsor had no role in the design, methods, data collection, or analysis of the study, nor any role in the preparation of the manuscript.
Author Contributions:
Meghann Moore contributed to design of the study, led data collection, performed data analyses, and contributed to preparation of the manuscript.
Barbara Williams provided input into and performed data analyses.
Sally Ragsdale was responsible for delivery of the fall prevention clinic intervention to FPC participants.
James P. LoGerfo supported the establishment of the clinic and provided critical review of the manuscript.
Richard Goss provided input into study design and data collection methods and provided critical review of the manuscript.
Astrid B. Schreuder provided input into study design and data collection methods, contributed to the IRB application, and provided critical review of the manuscript with a focus on statistical methods.
Elizabeth A. Phelan provided funding for the study, developed study concept, oversaw study design, data collection, and data analyses, and edited and approved the final manuscript.
References
- 1.Tinetti ME, Speechley M, Ginter SF. Risk factors for falls among elderly persons living in the community. N Engl J Med. 1988;319:1701–1707. doi: 10.1056/NEJM198812293192604. [DOI] [PubMed] [Google Scholar]
- 2.Hill K, Schwarz J, Flicker L, et al. Falls among healthy, community-dwelling, older women: A prospective study of frequency, circumstances, consequences and prediction accuracy. Aust N Z J Public Health. 1999;23:41–48. doi: 10.1111/j.1467-842x.1999.tb01203.x. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC) [Accessed October 10, 2007.];Falls among older adults: An overview. Available at: www.cdc.gov/ncipc/factsheets/adultfalls.html.
- 4.Tinetti ME, Gordon C, Sogolow E, et al. Fall-risk evaluation and management: Challenges in adopting geriatric care practices. Gerontologist. 2006;46:717–725. doi: 10.1093/geront/46.6.717. [DOI] [PubMed] [Google Scholar]
- 5.Chang JT, Morton SC, Rubenstein LZ, et al. Interventions for the prevention of falls in older adults: Systematic review and meta-analysis of randomised clinical trials. BMJ. 2004;328:680–687. doi: 10.1136/bmj.328.7441.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wenger NS, Solomon DH, Roth CP, et al. The quality of medical care provided to vulnerable community-dwelling older patients. Ann Intern Med. 2003;139:740–747. doi: 10.7326/0003-4819-139-9-200311040-00008. [DOI] [PubMed] [Google Scholar]
- 7.Paniagua MA, Malphurs JE, Phelan EA. Older patients presenting to a county hospital ED after a fall: Missed opportunities for prevention. Am J Emerg Med. 2006;24:413–417. doi: 10.1016/j.ajem.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 8.Reuben DB, Roth C, Kamberg C, et al. Restructuring primary care practices to manage geriatric syndromes: The ACOVE-2 intervention. J Am Geriatr Soc. 2003;51:1787–1793. doi: 10.1046/j.1532-5415.2003.51565.x. [DOI] [PubMed] [Google Scholar]
- 9.Wenger NS, Roth CP, Shekelle PG, et al. A Practice-Based Intervention to Improve Primary Care for Falls, Urinary Incontinence, and Dementia. J Am Geriatr Soc. 2009;57:547–555. doi: 10.1111/j.1532-5415.2008.02128.x. [DOI] [PubMed] [Google Scholar]
- 10.Goldberg HI, Neighbor WE, Cheadle AD, et al. A controlled time-series trial of clinical reminders: Using computerized firm systems to make quality improvement research a routine part of mainstream practice. Health Serv Res. 2000;34:1519–1534. [PMC free article] [PubMed] [Google Scholar]
- 11.Landi F, Onder G, Cesari M, et al. Psychotropic medications and risk for falls among community-dwelling frail older people: An observational study. J Gerontol A Biol Sci Med Sci. 2005;60:622–626. doi: 10.1093/gerona/60.5.622. [DOI] [PubMed] [Google Scholar]
- 12.Guideline for the prevention of falls in older persons. American Geriatrics Society, British Geriatrics Society, and American Academy of Orthopaedic Surgeons Panel on Falls Prevention. J Am Geriatr Soc. 2001;49:664–672. [PubMed] [Google Scholar]
- 13.Beer C. Attitudes of GPs to medical management in a falls clinic service. Aust Fam Phys. 2006;35:1008–1010. [PubMed] [Google Scholar]
- 14.Hill KD, Moore KJ, Dorevitch MI, et al. Effectiveness of falls clinics: An evaluation of outcomes and client adherence to recommended interventions. J Am Geriatr Soc. 2008;56:600–608. doi: 10.1111/j.1532-5415.2007.01626.x. [DOI] [PubMed] [Google Scholar]
- 15.Lord SR, Tiedemann A, Chapman K, et al. The effect of an individualized fall prevention program on fall risk and falls in older people: A randomized, controlled trial. J Am Geriatr Soc. 2005;53:1296–1304. doi: 10.1111/j.1532-5415.2005.53425.x. [DOI] [PubMed] [Google Scholar]
- 16.Hart-Hughes S, Palacious P, Quigley P, et al. An interdisciplinary approach to reducing fall risks and falls. J Rehabil. 2004;70:46–51. [Google Scholar]
- 17.Wagner EH, LaCroix AZ, Grothaus L, et al. Preventing disability and falls in older adults: A population-based randomized trial. Am J Public Health. 1994;84:1800–1806. doi: 10.2105/ajph.84.11.1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rizzo JA, Friedkin R, Williams CS, et al. Health care utilization and costs in a Medicare population by fall status. Med Care. 1998;36:1174–1188. doi: 10.1097/00005650-199808000-00006. [DOI] [PubMed] [Google Scholar]