Abstract
Patients with Crohn's disease commonly undergo surgery during their lifetime. Indications for surgical intervention include obstruction, intra-abdominal or perianal abscess, enterocutaneous fistulas, and complex perianal disease. As medical therapies continue to improve, it is important that surgical therapies are chosen carefully. This is particularly important in the treatment of perianal fistulas; combined surgical and medical therapy offer the best chance for success. In the treatment of small-bowel disease, bowel preservation is key. For the repair of short strictures, endoscopic dilatation is the preferred method when accessible; strictureplasty has been shown to be safe and effective for increasingly longer segments of disease. Intra-abdominal abscesses should be drained percutaneously, if possible. In the presence of colonic disease, segmental resection is recommended. Unfortunately, refractory disease still frequently requires complete proctectomy and permanent diversion.
Keywords: Crohn's disease, fistula, surgery, stricture
Between 70% and 90% of patients with Crohn's disease will require surgery during their lifetime,1,2 even those who first present with a nonfistulizing, nonpenetrating phenotype,3 and as many as 39% will require repeated surgery.4 The percentages of patients with obstructing phenotypes and of penetrating phenotypes are approximately even,5 and no genotype has been reliably linked with phenotypic presentation or progression6 (including the CARD15 gene7). Indications for surgery include complications from strictures, intra-abdominal and perianal fistulas, intestinal perforation, intra-abdominal abscess, gastrointestinal bleeding, malignancy, and growth restriction in children.8
Estimates of the prevalence of perianal involvement in Crohn's disease have varied greatly, but the most recent population-based series demonstrate that anorectal involvement is seen in 14–38% of Crohn's disease patients,9–11 with isolated perianal disease seen in only 5%.12 In patients with ileocolonic Crohn's disease, only 15% will develop fistulas, though fistulas occur in 92% of patients with colonic Crohn's disease and rectal involvement.11 In most cases, bowel involvement antecedes perianal disease.13 There does not appear to be a predilection for age, with 13–62% of children and adolescents experiencing perianal manifestations.10,14,15 A study of 1,126 patients with Crohn's disease found that whites more commonly have proximal disease (odds ratio [OR], 1.8) and are less likely than Hispanics or African Americans to have perianal manifestations (OR, 0.58).16 The presence of anal disease is associated with a more disabling natural history,17 with more frequent extraintestinal manifestations18 and increased steroid resistance.19 The disease is recurrent, with 35–59% of patients relapsing within 2 years.20
Surgery for Crohn's disease is not curative. Although some debate exists as to whether early intervention may be beneficial in select cases, excess intervention can be harmful,4,21 making the timing of interventions require considerable judgment. As medical therapy continues to improve, this decision is increasingly shared between gastroenterologists and surgeons.
Intestinal Disease
Stricturing Disease
Patients with stricturing Crohn's disease are at risk for the development of intestinal obstruction. Acute obstruction is often due to a plug of indigestible fiber that is ingested or to inflammation at a site of active disease, and can be managed conservatively with a low residual diet and medical therapy in the majority of cases.22 Approximately 30% of Crohn's patients have disease limited to the ileum, and surgery can offer these patients durable remission. One half of Crohn's patients, however, will have multifocal ileocolonic disease, and these patients are almost 3 times as likely to require further surgery.23 It is, therefore, important to understand the patient's extent of disease at presentation and to rely upon methods increasingly focused on bowel preservation in patients with multiple strictures or recurrent disease. With evidence that extensive resection is potentially harmful,24 methods that preserve the bowel have become more popular, including strictureplasty techniques and endoscopic balloon dilatation.
Endoscopic dilatation may be an attractive nonoperative option in the treatment of Crohn's strictures. A recent quantitative review25 demonstrated that the endoscopic approach was technically successful in 86% of patients, with a major complication rate of 2–18%. In successful patients, only 42% required surgical intervention an average of 15 months after dilatation. Of note, although these results are promising, the majority of these reviewed series examined postoperative strictures, and short-segment disease (<4 cm) was the only predictor of long-term benefit. With a risk of perforated viscus, endoscopic dilatation should not be attempted without the availability of a surgical team.26
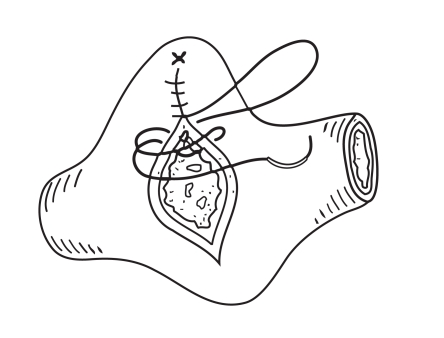
First described in the 1970s,27 strictureplasty is recommended in cases where bowel length preservation is critical (patients with recurrent disease after small-bowel resection), in cases where resection would be extensive (diffuse small-bowel involvement), or in cases with a single site of fibrotic, inactive disease.28 The recommended length of strictured intestine that can be repaired varies between 10 cm and 25 cm,26,29,30 though Michelassi and colleagues31 and Poggioli and coworkers32 have described successful strategies for segments up to 90 cm. The Heineke-Mikulicz strictureplasty is the most commonly performed technique and is useful in strictures under 10 cm33 (Figure 1). Strictureplasty should be avoided in colonic strictures secondary to Crohn's disease, though a study of 29 patients found colonic strictureplasty to be safe.34
Figure 1.
Heineke-Mikulicz strictureplasty.
Reproduced from Kumar D, Alexander-Williams J. Crohn's Disease and Ulcerative Colitis: Surgical Management. London, United Kingdom: Springer; 1993:89-101.
Yamamoto and associates35 pooled data on 1,112 patients who underwent 3,259 strictureplasties and found a morbidity rate of 13%, with fistula and abscess being the leading postoperative complications, followed by postoperative gastrointestinal bleeding and wound infection. Overall, 26% of patients experienced recrudescence of disease, usually within 5 years,30 and recurrence at another site in 25%.35
Small-bowel resection is the most commonly performed operation for Crohn's disease.36 For patients with limited disease, early resection may be the best option. In a study of 36 patients with ileal Crohn's disease diagnosed during appendectomy, Weston and associates37 found that 92% of patients who did not undergo ileocolectomy required additional surgery within 1 year, whereas only 50% of the patients who underwent immediate ileocolectomy required additional surgery, with a mean follow-up of 12 years.
Indications for a small-bowel resection include chronic obstructive symptoms, failure of medical therapy, perforation or abscess, and dysplasia or malignancy. Only the portion of small bowel grossly involved should be resected, with margins of 2 cm or less. A randomized controlled trial by Fazio and coworkers38 of 152 patients showed no benefit with margins between 2 cm and 12 cm, and leaving behind histologically active disease did not appear to effect recurrence.39
Minimally invasive techniques have recently been employed in the treatment of Crohn's disease. Investigators have examined whether a laparoscopic or open approach for performing an uncomplicated small-bowel resection is preferable. Two randomized controlled trials totaling 120 patients undergoing ileocolic resection for Crohn's disease have been conducted. The authors found laparoscopic surgery to be equivalent40 or superior41 to an open approach, measured by duration of hospital stay, morbidity, and (in Maartense and associates41) overall costs. Stocchi and colleagues42 recently found the results reported by Milsom and coworkers40 to be durable at 10 years, with no increased risk of recurrence or missed disease in the laparoscopic arm. Nearly all series describe an average of 30 minutes of additional operative time with a laparoscopic approach,43 and many have reported conversion rates of up to 40%.8 Conversion to an open approach, however, does not adversely affect final outcome,44 and the conversion rate may improve with surgeon experience.45 Recent series have shown laparoscopic surgery to be feasible and safe even for complex, recurrent cases of Crohn's disease.46
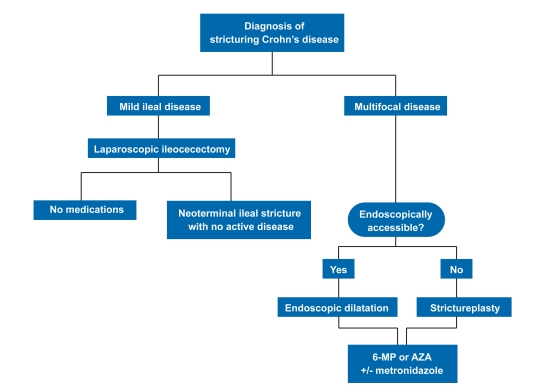
In summary, patients presenting with mild or moderate disease localized to the ileum may have a chance at durable remission and should be offered early surgical intervention with a small-bowel resection extirpating the diseased segment, preferably via a laparoscopic approach. Patients with strictures and no active disease at the site can be treated with either endoscopic dilatation or strictureplasty, once conservative management fails. Complex strictureplasty is best reserved for patients with multifocal recurrent ileocolic disease, and reasonable recurrence rates can safely be obtained with longer segments of diseased bowel as surgical technique continues to improve. A treatment algorithm for patients with stricturing Crohn's disease is outlined in Figure 2.47
Figure 2.
Treatment algorithm for stricturing Crohn's disease.
- 6-MP=
- 6-mercaptopurine
- AZA=
- azathioprine.
Modified from Cho SM, et al.47
Penetrating Disease
Penetrating disease can result in intra-abdominal fistulas between 2 intestinal sites involved with Crohn's disease, between involved sites and “innocent” organs, and between involved sites and the skin. Penetrating Crohn's disease can also result in intra-abdominal abscess and sepsis.
A fistula is the second most common primary indication for surgery, but it is almost always accompanied by another abnormality such as an intra-abdominal abscess or inflammatory mass.48 Fistulas are frequently found during operations for medically refractory Crohn's disease. In a series of 639 patients undergoing surgery, 222 (34.7%) had a total of 290 fistulas, 27% of which were diagnosed perioperatively.49
Small bowel to small bowel fistulas are often asymptomatic and do not typically require surgical intervention. Up to 40% of these patients, however, may progress to surgery within 1 year.50 In addition to causing abdominal abscess and pain, symptomatic fistulas between the proximal small bowel and colon can bypass a large portion of the bowel, resulting in malabsorption. These fistulas should be repaired as soon as the patient's nutritional status is stabilized. Surgical treatment involves resection of the involved small bowel and either repair of the fistula target (in the event of an enterovesicular or enterovaginal fistula) or wedge resection (if the target is the large bowel).51 Some physicians have found that repaired sigmoid sites were apt to leak and therefore recommend a limited sigmoid resection.52 Primary anastomosis is safe, and diversion is rarely required.
Enterocutaneous fistulas can be medically managed in as many as 30% of cases,53 but only if there is no associated intra-abdominal abscess.54 Nutritional support is critical; enteral feeding is preferred, though total parenteral nutrition has also been shown to be of benefit.55 Although the benefit of good nutrition and meticulous wound care are widely accepted, there is a lack of information regarding effective treatment with medications. Octreotide, a somatostatin analogue, has been shown to dramatically decrease the output of enterocutaneous fistulas,56 but it does not reduce the need for surgery in Crohn's patients.57 The ACCENT-158 and ACCENT-259 trials, which effectively used infliximab (Remicade, Centocor) for the treatment of penetrating Crohn's disease, did include 9 (of 94) and 39 (of 306) patients with abdominal enterocutaneous fistulas. As no subgroup analysis was performed on these patients alone, it is difficult to extrapolate the success seen with perianal disease to abdominal fistulas. Another series found that, while infliximab healed perianal fistulas, it did not result in the closure of enteroenteral or enterocutaneous fistulas, which still required surgery.60 Therefore, although infliximab therapy can be attempted, after a trial of at least 6 weeks, surgical intervention should be considered.61
Approximately 25% of Crohn's patients will develop an intra-abdominal abscess during their lifetime, often in association with a fistulous tract.62 In these cases, percutaneous drainage should be attempted whenever possible, as successful drainage can successfully avoid surgery in as many as two thirds of patients.63 Up to half of abscesses will recur, though this risk is less when surgically drained.64 In contrast, when an abscess is diagnosed intraoperatively (as occurs in 50% of cases),49 involved bowel should be resected. A stoma is often necessary to protect the anastomosis.65
Other Surgical Indications
Gastrointestinal hemorrhage is a rare complication of Crohn's disease and accounts for only 1% of operations. Given the desire to minimize resection of uninvolved small bowel, preoperative localization is of paramount importance. Angiography can be very helpful in preoperatively localizing the disease if the patient is actively bleeding.66
Although adenocarcinoma of the colon is slightly more common in patients with Crohn's disease than in the general population,67 the risk of small-bowel carcinoma is 60-fold higher.68 The risk is particularly high in patients with surgically bypassed segments,69 a practice that has fallen out of favor.70 Surgical resection of all involved segments and the nodal basin is recommended, but outcomes are usually poor, as the disease is often advanced at the time of diagnosis.69,71
Postoperative Recurrence
Endoscopic recurrence occurs in 70–90% of patients72 within as little as 1 week after surgery and becomes symptomatic in 60% of patients within 10 years.73 One third of patients will require repeat surgical intervention.69 Smokers have a 2.5-fold higher risk of requiring additional surgery74 and having a family history of Crohn's disease increases surgical recurrence 2-fold.75 The gold standard in surveillance is colonoscopy, which is recommended annually or biannually. The standard therapy to extend clinical remission has been treatment with immunomodulators, including 6-mercaptopurine and azathioprine,47 though recent data, including a randomized controlled trial in 24 patients,76 have shown a 90% reduction of endoscopic recurrence at 1 year in patients receiving infliximab therapy.
Perianal Disease
Perianal Fistula
Abscess and fistula are the most common presentations of anorectal Crohn's disease. Twenty-six percent of patients will present with an abscess, and an additional 29% will present with a fistula.77 A thorough examination must be performed before treatment is initiated, with special attention given to establishing the presence or absence of rectal inflammation. Any collection should be immediately drained. Beyond this point, treatment options for fistulas become extremely varied. Fistulas should be categorized as simple (defined as superficial, inter-, or trans-sphincteric fistulas below the dentate line, with a single opening and no anorectal stricture or abscess) or complex (defined as a trans-, supra-, or extrasphincteric fistula above the dentate line; a fistula with multiple external openings, an associated abscess, or stricture; or a rectovaginal fistula).10 Combined medical and surgical approaches offer the best chance for success.78–80
An examination under anesthesia (EUA) has traditionally been considered the gold standard for diagnosis of Crohn's-related fistula, but a prospective study by Schwartz and coworkers81 in 34 patients found that EUA had an accuracy of only 90%, based upon a composite gold standard derived from EUA, anal endoscopic ultrasound (EUS), and pelvic magnetic resonance imaging (MRI). This same study found that accuracy was 100% when any 2 of these 3 procedures were performed.
Pelvic MRI is the preferred imaging modality in the classification of fistulizing perianal disease and has been shown to have an accuracy of 90%82,83 when classifying fistulas and 97% when delineating complex abscesses, though endoanal ultrasound is only slightly inferior.81,83,84 Surgical management can be altered in as many as 40% of Crohn's patients with the addition of MRI to EUA.85,86
Perianal abscess presents with pain, swelling, and fluctuation on rectal examination, and is thought to form by extension of a cryptoglandular infection or by obstruction of a perianal fistula. Abscesses can develop in any plane (superficial, intersphincteric, ischiorectal, or supralevator); however, regardless of location, they require prompt surgical incision and drainage and treatment of systemic symptoms with broad-spectrum antibiotics.10,87 Many physicians advocate placing a drain or partially dividing sphincters to facilitate drainage, but these devices have not been shown to improve outcomes.88,89 EUS has been used with success to guide the incision of deep or complex abscesses.90
In the presence of a fistula, a noncutting seton made of an inert material can be placed to prevent recurrence of abscess and to facilitate drainage, with healing or improvement seen in 79–100% of patients.91–96 Setons can be left in place long term without consequence; removal without definitive therapy results in recurrence in 20–80% of patients.94,97,98 In patients with persistent sepsis, a diverting stoma can be effective in up to 80% of patients, but it is rarely reversed—in only 4 of 18 (22%) patients in one study.99
Once a fistula is characterized and any concomitant abscess controlled, combined definitive medical and surgical therapy should be initiated. Antibiotics have been shown to be effective as a bridge to immunosuppressive therapy,100 with 70–95% of patients experiencing a positive clinical response within 6–8 weeks101,102 and a worsening of symptoms when the antibiotics are discontinued or decreased.103 Fewer than 50% of patients, however, experience healing of the fistula on antibiotic therapy alone, and the majority of cases will recur if antibiotics are withdrawn.104
More definitive medical therapy requires immunosuppression. A meta-analysis of 5 randomized controlled trials examined the efficacy of 6-mercaptopurine and azathioprine and showed that, in these 70 patients, 54% of treated patients experienced fistula healing versus only 21% of controls.105 Cyclosporine has excellent, rapid effect in up to 83% of patients when given intravenously,106,107 but the effect is not durable when patients are transitioned to oral medication or when therapy is discontinued.108 Tacrolimus has also shown efficacy in a randomized controlled trial, resulting in at least a 50% improvement in 43% of patients versus 8% in the placebo arm.109
Infliximab has proven to be particularly effective in the treatment of perianal fistulas in patients with Crohn's disease. The ACCENT-1 trial of 92 patients showed effi-cacy with induction therapy: 68% of patients treated with infliximab had at least a 50% improvement versus 26% with placebo.58 The ACCENT-2 trial documented longer time to recurrence of fistulas with infliximab maintenance therapy (40 weeks vs 14 weeks for placebo).59 In addition, treatment with infliximab resulted in less need for surgery and fewer hospitalizations.59 Interestingly, rectovaginal fistulas have a poorer response to infliximab therapy— only 14–30% heal compared to 46–78% of other perianal fistulas.58,110,111 The anti –tumor necrosis factor (TNF) antibody adalimumab (Humira, Abbott) has a similar safety profile to infliximab112 and had similar efficacy in a randomized controlled trial (the CHARM trial). Complete fistula closure at 1 year was seen in 39% of treated patients compared to 13% of the placebo arm.113 These results have been shown to be durable at 2 years.114
Fistulotomy, or the opening of the fistula tract via division of overlying tissues, offers the best chance for definitive treatment of perianal fistulas. Several series have examined the effect of fistulotomy in patients with low perianal fistula, with most reporting healing rates between 80% and 100%.10 When the investigators specifically noted the absence of rectal inflammation, results improved further, with healing achieved in 22 of 24 (92%) patients and recurrence in only 4 of 24 (17%) patients.89,115,116 Conversely, a study that specifically noted active proctocolitis at the time of surgery documented a healing rate of only 27% of fistulas.117
Much of the concern regarding operating on patients with anorectal Crohn's disease has been due to the possibility of repeat iatrogenic injury to the sphincter muscle.118 Newer therapies using fibrin glue and anal fistula plugs have been developed that do not require any division of muscle.119 Success using fibrin glue, however, has been mixed, with 60–78% of simple fistulas healed, but only 14–50% of complex fistulas healed in the general population120 and only 31–57% of fistulas in patients with Crohn's disease.121,122 In contrast, initial outcomes using the collagen anal fistula plug have been more promising: a prospective study of 20 patients found that the plug was able to close 80% of fistulas in patients with Crohn's disease123 and 85% of fistulas in the general population.124 Other researchers, however, have shown poor outcomes (20% long-term healing) in patients with Crohn's disease and complex fistulas.125
Once a simple fistula is diagnosed (and there is no rectal inflammation), it appears safe to perform either a fistulotomy or placement of an anal fistula plug while initiating medical therapy. In the setting of proctitis, outcomes are not as good, and medical therapy with the placement of a seton, anticipating possible fistulotomy should proctitis resolve in 6–8 weeks, may offer the best chance for success.
Complex fistulas are defined as high perianal fistulas or fistulas with branched tracts, associated abscess, or multiple external openings.10 First-line therapy is infliximab, which, as mentioned above, has had excellent results in this population in multiple randomized controlled trials,58,59 usually with the addition of immunosuppression. Adjunct surgical therapy, with temporary placement of a loose seton at the time of induction, can be helpful in 47–67% of cases.79,126
Fistulotomy is not recommended for complex fistulas, as previous series have found nonhealing and incontinence. As many as 40–60% of patients may eventually require proctectomy.117,127 In the absence of proctitis, however, a transanal advancement flap may be a good option. In this procedure, the internal fistula opening is excised and the mucosa, submucosa, and circular muscle are mobilized as an island and placed over the fistula tract. Investigators have demonstrated healing in as many as 89% of patients, but a disappointing rate of recurrence, up to 50%.128–130 A transanal sleeve advancement flap, in which the entire rectal mucosa is advanced over the internal fistula opening, is another alternative and has resulted in healing in 62% of cases, with a recurrence rate of 38%.131 Finally, a loose seton can be left indefinitely without significant effect on continence.132
Crohn's disease is the second most common cause of rectovaginal fistula.133 The initial treatment does not vary from that of other complicated fistulas, though, as noted above, infliximab does not have the same response rate in this population.134 Rectal advancement flaps are effective, with 54–71% healing,135,136 and similar results have been seen using rectal sleeve advancement flaps.135,137 Although most physicians advocate the use of rectal flaps, as the rectum is the high pressure side of the fistula, one series has demonstrated 92% healing in 14 patients treated with a vaginal advancement flap.138 In recurrent cases, repeating the flap can have some success (14% of cases in one series).135
Diversion and Proctectomy
A diverting ileostomy or, rarely, a colostomy can be helpful in severe perianal disease, with permanent stoma required in up to 37–49%. Risk factors include colon involvement, anal stricture, incontinence, and complex perianal fistulas.139,140
Temporary diversion is indicated when perianal disease is extremely extensive or progressive despite drainage of abscess and maximal medical therapy.141 Diversion may help to create a more favorable environment for complex perianal repairs. Yamamoto and associates142 found that although 25 of 31 (81%) patients experienced early remission, 17 (55%) relapsed, most required eventual proc-tectomy, and only 3 (10%) were able to have the stoma reversed. Permanent diversion, however, can improve quality of life; Kasparek and colleagues143 found that only 44% of diverted patients complained of Crohn's disease symptoms compared to 79% of undiverted patients.
Proctectomy may be indicated in patients who fail medical and surgical therapy, or in the presence of aggressive and unrelenting rectal disease. Resection of the rectum with permanent colostomy is required in 10–20% of cases.10 Unfortunately, proctectomy can be complicated by poor wound healing and perineal sinus formation in up to 25–50% of patients.144,145 A gracilis or rectus flap146 can be used to help combat these complications.
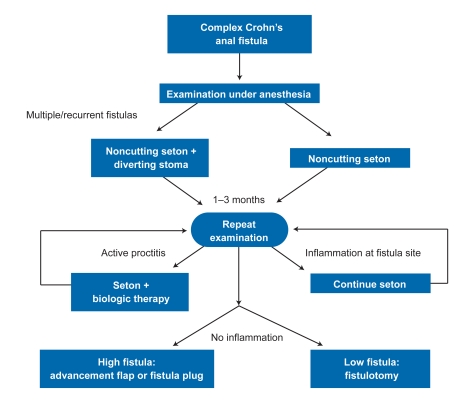
An algorithm for the approach to perianal disease management is shown in Figure 3.147
Figure 3.
Approach to management of Crohn's perianal fistula.
Reproduced from van der Hagen SJ, et al.147
Summary
Crohn's disease is a chronic incurable relapsing disease with a large variability in clinical presentation and is caused by idiopathic full thickness inflammation at any point in the gastrointestinal tract. Nearly all patients Reproduced from van der Hagen SJ, et al.147 require surgery during their lifetime for palliation of symptoms and complications of the illness. However, in the last 2 decades, medical treatments have advanced considerably, particularly with the development of anti-TNF therapeutics such as infliximab.
There is some evidence that mild ileal disease benefits from early excision, though recurrent or multifocal disease should be treated using techniques that preserve small-bowel length and function. Endoscopic dilatation of accessible lesions (<4 cm in length) or strictureplasty of lesions less than 25 cm in size (and, in rare situations, up to 90 cm) are increasingly safe and effective. Intra-abdominal abscesses should be drained percutaneously when possible. For perianal fistulas, combined medical therapy with a noncutting seton followed by judicious fistulotomy or (when fistulotomy is not possible) advancement flaps has been shown to be most effective in treatment of complex perianal disease. Despite all these advances, refractory cases, particularly with proctitis, often require proctectomy and permanent diversion.
Contributor Information
Robert T. Lewis, Dr. Lewis is a resident in the Department of Surgery in the University of Pennsylvania Health System in Philadelphia, Pennsylvania.
David J. Maron, Dr. Maron is a staff surgeon and Associate Director of the Colorectal Surgery Residency program at the Cleveland Clinic Florida in Weston, Florida.
References
- 1.Canin-Endres J, Salky B, Gattorno F, Edye M. Laparoscopically assisted intestinal resection in 88 patients with Crohn's disease. Surg Endosc. 1999;13:595–599. doi: 10.1007/s004649901049. [DOI] [PubMed] [Google Scholar]
- 2.Mekhjian HS, Switz DM, Watts HD, Deren JJ, Katon RM, Beman FM. National cooperative Crohn's disease study: Factors determining recurrence of Crohn's disease after surgery. Gastroenterology. 1979;77(4 pt 2):907–913. [PubMed] [Google Scholar]
- 3.Louis E, Collard A, Oger AF, Degroote E, Aboul Nasr El Yafi FA, Belaiche J. Behaviour of Crohn's disease according to the Vienna classification: changing pattern over the course of the disease. Gut. 2001;49:777–782. doi: 10.1136/gut.49.6.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Chardavoyne R, Flint GW, Pollack S, Wise L. Factors affecting recurrence following resection for Crohn's disease. Dis Colon Rectum. 1986;29:495–502. doi: 10.1007/BF02562601. [DOI] [PubMed] [Google Scholar]
- 5.Van Assche G, Geboes K, Rutgeerts P. Medical therapy for Crohn's disease strictures. Inflamm Bowel Dis. 2004;10:55–60. doi: 10.1097/00054725-200401000-00009. [DOI] [PubMed] [Google Scholar]
- 6.Burke JP, Mulsow JJ, O'Keane C, Docherty NG, Watson RW, O'Connell PR. Fibrogenesis in Crohn's disease. Am J Gastroenterol. 2007;102:439–448. doi: 10.1111/j.1572-0241.2006.01010.x. [DOI] [PubMed] [Google Scholar]
- 7.Hugot JP, Laurent-Puig P, Gower-Rousseau C, et al. Mapping of a susceptibility locus for Crohn's disease on chromosome 16. Nature. 1996;379:821–823. doi: 10.1038/379821a0. [DOI] [PubMed] [Google Scholar]
- 8.Gardiner KR, Dasari BV. Operative management of small bowel Crohn's disease. Surg Clin North Am. 2007;87:587–610. doi: 10.1016/j.suc.2007.03.011. [DOI] [PubMed] [Google Scholar]
- 9.Hellers G, Bergstrand O, Ewerth S, Holmstrom B. Occurrence and outcome after primary treatment of anal fistulae in Crohn's disease. Gut. 1980;21:525–527. doi: 10.1136/gut.21.6.525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sandborn WJ, Fazio VW, Feagan BG, Hanauer SB, American Gastroenterological Association Clinical Practice Committee AGA technical review on perianal crohn's disease. Gastroenterology. 2003;125:1508–1530. doi: 10.1016/j.gastro.2003.08.025. [DOI] [PubMed] [Google Scholar]
- 11.Schwartz DA, Loftus EV, Jr, Tremaine WJ, et al. The natural history of fistulizing Crohn's disease in Olmsted county, Minnesota. Gastroenterology. 2002;122:875–880. doi: 10.1053/gast.2002.32362. [DOI] [PubMed] [Google Scholar]
- 12.Lockhart-Mummery HE. Symposium. Crohn's disease: Anal lesions. Dis Colon Rectum. 1975;18:200–202. doi: 10.1007/BF02587272. [DOI] [PubMed] [Google Scholar]
- 13.Williams DR, Coller JA, Corman ML, Nugent FW, Veidenheimer MC. Anal complications in Crohn's disease. Dis Colon Rectum. 1981;24:22–24. doi: 10.1007/BF02603444. [DOI] [PubMed] [Google Scholar]
- 14.Markowitz J, Daum F, Aiges H, Kahn E, Silverberg M, Fisher SE. Perianal disease in children and adolescents with Crohn's disease. Gastroenterology. 1984;86(5 pt 1):829–833. [PubMed] [Google Scholar]
- 15.Palder SB, Shandling B, Bilik R, Griffiths AM, Sherman P. Perianal complications of pediatric Crohn's disease. J Pediatr Surg. 1991;26:513–515. doi: 10.1016/0022-3468(91)90694-o. [DOI] [PubMed] [Google Scholar]
- 16.Nguyen GC, Torres EA, Regueiro M, et al. Inflammatory bowel disease characteristics among African Americans, Hispanics, and non-Hispanic whites: characterization of a large North American cohort. Am J Gastroenterol. 2006;101:1012–1023. doi: 10.1111/j.1572-0241.2006.00504.x. [DOI] [PubMed] [Google Scholar]
- 17.Beaugerie L, Seksik P, Nion-Larmurier I, Gendre JP, Cosnes J. Predictors of Crohn's disease. Gastroenterology. 2006;130:650–656. doi: 10.1053/j.gastro.2005.12.019. [DOI] [PubMed] [Google Scholar]
- 18.Rankin GB, Watts HD, Melnyk CS, Kelley ML., Jr National cooperative Crohn's disease study: extraintestinal manifestations and perianal complications. Gastroenterology. 1979;77(4 pt 2):914–920. [PubMed] [Google Scholar]
- 19.Gelbmann CM, Rogler G, Gross V, et al. Prior bowel resections, perianal disease, and a high initial Crohn's disease activity index are associated with corticosteroid resistance in active Crohn's disease. Am J Gastroenterol. 2002;97:1438–1445. doi: 10.1111/j.1572-0241.2002.05685.x. [DOI] [PubMed] [Google Scholar]
- 20.Makowiec F, Jehle EC, Starlinger M. Clinical course of perianal fistulas in Crohn's disease. Gut. 1995;37:696–701. doi: 10.1136/gut.37.5.696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Post S, Betzler M, von Ditfurth B, Schurmann G, Kuppers P, Herfarth C. Risks of intestinal anastomoses in Crohn's disease. Ann Surg. 1991;213:37–42. doi: 10.1097/00000658-199101000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Prantera C. Indications for surgery in Crohn's disease. Am J Gastroenterol. 1990;85:900–901. [PubMed] [Google Scholar]
- 23.Whelan G, Farmer RG, Fazio VW, Goormastic M. Recurrence after surgery in Crohn's disease. Relationship to location of disease (clinical pattern) and surgical indication. Gastroenterology. 1985;88:1826–1833. doi: 10.1016/0016-5085(85)90007-1. [DOI] [PubMed] [Google Scholar]
- 24.Heuman R, Boeryd B, Bolin T, Sjodahl R. The influence of disease atthe margin of resection on the outcome of Crohn's disease. Br J Surg. 1983;70:519–521. doi: 10.1002/bjs.1800700904. [DOI] [PubMed] [Google Scholar]
- 25.Hassan C, Zullo A, De Francesco V, et al. Systematic review: endoscopic dilatation in Crohn's disease. Aliment Pharmacol Ther. 2007;26:1457–1464. doi: 10.1111/j.1365-2036.2007.03532.x. [DOI] [PubMed] [Google Scholar]
- 26.Travis SP, Stange EF, Lemann M, et al. European Crohn's and Colitis Organisation. European evidence based consensus on the diagnosis and management of Crohn's disease: current management. Gut. 2006;55(suppl 1):i16–35. doi: 10.1136/gut.2005.081950b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Katariya RN, Sood S, Rao PG, Rao PL. Stricture-plasty for tubercular strictures of the gastro-intestinal tract. Br J Surg. 1977;64:496–498. doi: 10.1002/bjs.1800640713. [DOI] [PubMed] [Google Scholar]
- 28.Cima RR, Pemberton JH. Current Surgical Therapy. 9th ed. Philadelphia, PA: Mosby-Elsevier; 2008. Strictureplasty in Crohn's disease. In: Cameron JL, ed. [Google Scholar]
- 29.Fazio VW, Tjandra JJ. Strictureplasty for Crohn's disease with multiple long strictures. Dis Colon Rectum. 1993;36:71–72. doi: 10.1007/BF02050305. [DOI] [PubMed] [Google Scholar]
- 30.Roy P, Kumar D. Strictureplasty. Br J Surg. 2004;91:1428–1437. doi: 10.1002/bjs.4804. [DOI] [PubMed] [Google Scholar]
- 31.Michelassi F, Taschieri A, Tonelli F, et al. An international, multicenter, prospective, observational study of the side-to-side isoperistaltic strictureplasty in Crohn's disease. Dis Colon Rectum. 2007;50:277–284. doi: 10.1007/s10350-006-0804-y. [DOI] [PubMed] [Google Scholar]
- 32.Poggioli G, Laureti S, Pierangeli F, Ugolini F. A new model of strictureplasty for multiple and long stenoses in Crohn's ileitis: side-to-side diseased to disease-free anastomosis. Dis Colon Rectum. 2003;46:127–130. doi: 10.1007/s10350-004-6508-2. [DOI] [PubMed] [Google Scholar]
- 33.Tichansky D, Cagir B, Yoo E, Marcus SM, Fry RD. Strictureplasty for Crohn's disease: meta-analysis. Dis Colon Rectum. 2000;43:911–919. doi: 10.1007/BF02237350. [DOI] [PubMed] [Google Scholar]
- 34.Broering DC, Eisenberger CF, Koch A, et al. Strictureplasty for large bowel stenosis in Crohn's disease: Quality of life after surgical therapy. Int J Colorectal Dis. 2001;16:81–87. doi: 10.1007/s003840000278. [DOI] [PubMed] [Google Scholar]
- 35.Yamamoto T, Fazio VW, Tekkis PP. Safety and efficacy of strictureplastyfor Crohn's disease: a systematic review and meta-analysis. Dis Colon Rectum. 2007;50:1968–1986. doi: 10.1007/s10350-007-0279-5. [DOI] [PubMed] [Google Scholar]
- 36.Mintz Y, Talamini MA. Crohn's disease of the small bowel. In: Cameron JL, editor. Current Surgical Therapy. 9th ed. Philadelphia, PA: Mosby-Elsevier; 2008. [Google Scholar]
- 37.Weston LA, Roberts PL, Schoetz DJ, Jr, Coller JA, Murray JJ, Rusin LC. Ileocolic resection for acute presentation of Crohn's disease of the ileum. Dis Colon Rectum. 1996;39:841–846. doi: 10.1007/BF02053980. [DOI] [PubMed] [Google Scholar]
- 38.Fazio VW, Marchetti F, Church M, et al. Effect of resection margins on the recurrence of Crohn's disease in the small bowel. A randomized controlled trial. Ann Surg. 1996;224:563–571. doi: 10.1097/00000658-199610000-00014. discussion 571-573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hamilton SR, Reese J, Pennington L, Boitnott JK, Bayless TM, Cameron JL. The role of resection margin frozen section in the surgical management of Crohn's disease. Surg Gynecol Obstet. 1985;160:57–62. [PubMed] [Google Scholar]
- 40.Milsom JW, Hammerhofer KA, Bohm B, Marcello P, Elson P, FazioV W. Prospective, randomized trial comparing laparoscopic vs. conventionalsurgery for refractory ileocolic Crohn's disease. Dis Colon Rectum. 2001;44:1–8. doi: 10.1007/BF02234810. discussion 8-9. [DOI] [PubMed] [Google Scholar]
- 41.Maartense S, Dunker MS, Slors JF, et al. Laparoscopic-assisted versus open ileocolic resection for Crohn's disease: a randomized trial. Ann Surg. 2006;243:143–149. doi: 10.1097/01.sla.0000197318.37459.ec. discussion 150-153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stocchi L, Milsom JW, Fazio VW.Long-term outcomes of laparoscopic versus open ileocolic resection for Crohn's disease: follow-up of a prospective randomized trial Surgery 2008144622–627.discussion 627-628 92 [DOI] [PubMed] [Google Scholar]
- 43.Tan JJ, Tjandra JJ. Laparoscopic surgery for Crohn's disease: a meta-analysis. Dis Colon Rectum. 2007;50:576–585. doi: 10.1007/s10350-006-0855-0. [DOI] [PubMed] [Google Scholar]
- 44.Casillas S, Delaney CP, Senagore AJ, Brady K, Fazio VW. Does conversion of a laparoscopic colectomy adversely affect patient outcome? Dis Colon Rectum. 2004;47:1680–1685. doi: 10.1007/s10350-004-0692-4. [DOI] [PubMed] [Google Scholar]
- 45.Evans J, Poritz L, MacRae H. Influence of experience on laparoscopic ileocolic resection for Crohn's disease. Dis Colon Rectum. 2002;45:1595–1600. doi: 10.1007/s10350-004-7245-2. [DOI] [PubMed] [Google Scholar]
- 46.Goyer P, Alves A, Bretagnol F, Bouhnik Y, Valleur P, Panis Y. Impact of complex Crohn's disease on the outcome of laparoscopic ileocecal resection: a comparative clinical study in 124 patients. Dis Colon Rectum. 2009;52:205–210. doi: 10.1007/DCR.0b013e31819c9c08. [DOI] [PubMed] [Google Scholar]
- 47.Cho SM, Cho SW, Regueiro M. Postoperative management of Crohn's disease. Med Clin North Am. 2010;94:179–188. doi: 10.1016/j.mcna.2009.08.019. [DOI] [PubMed] [Google Scholar]
- 48.Michelassi F, Balestracci T, Chappell R, Block GE. Primary and recurrent Crohn's disease. Experience with 1379 patients. Ann Surg. 1991;214:230–238. doi: 10.1097/00000658-199109000-00006. discussion 238-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Michelassi F, Stella M, Balestracci T, Giuliante F, Marogna P, Block GE. Incidence, diagnosis, and treatment of enteric and colorectal fistulae in patients with Crohn's disease. Ann Surg. 1993;218:660–666. doi: 10.1097/00000658-199321850-00012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Broe PJ, Bayless TM, Cameron JL. Crohn's disease: are enteroenteral fistulas an indication for surgery? Surgery. 1982;91:249–253. [PubMed] [Google Scholar]
- 51.Hwang JM, Varma MG. Surgery for inflammatory bowel disease. World J Gastroenterol. 2008;14:2678–2690. doi: 10.3748/wjg.14.2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Fazio VW, Wilk P, Turnbull RB, Jr, Jagelman DG. The dilemma of Crohn's disease: ileosigmoidal fistula complicating Crohn's disease. Dis Colon Rectum. 1977;20:381–386. doi: 10.1007/BF02587365. [DOI] [PubMed] [Google Scholar]
- 53.Schein M. What's new in postoperative enterocutaneous fistulas? World J Surg. 2008;32:336–338. doi: 10.1007/s00268-007-9411-x. [DOI] [PubMed] [Google Scholar]
- 54.McIntyre PB, Ritchie JK, Hawley PR, Bartram CI, Lennard-Jones JE. Management of enterocutaneous fistulas: a review of 132 cases. Br J Surg. 1984;71:293–296. doi: 10.1002/bjs.1800710416. [DOI] [PubMed] [Google Scholar]
- 55.Lloyd DA, Gabe SM, Windsor AC. Nutrition and management of enterocutaneous fistula. Br J Surg. 2006;93:1045–1055. doi: 10.1002/bjs.5396. [DOI] [PubMed] [Google Scholar]
- 56.Nubiola P, Badia JM, Martinez-Rodenas F, et al. Treatment of 27 postoperative enterocutaneous fistulas with the long half-life somatostatin analogue SMS 201-995. Ann Surg. 1989;210:56–58. doi: 10.1097/00000658-198907000-00009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Draus JM, Jr, Huss SA, Harty NJ, Cheadle WG, Larson GM. Enterocutaneous fistula: Are treatments improving? Surgery. 2006;140:570–576. doi: 10.1016/j.surg.2006.07.003. discussion 576-578. [DOI] [PubMed] [Google Scholar]
- 58.Present DH, Rutgeerts P, Targan S, et al. Infliximab for the treatment of fistulas in patients with Crohn's disease. N Engl J Med. 1999;340:1398–1405. doi: 10.1056/NEJM199905063401804. [DOI] [PubMed] [Google Scholar]
- 59.Sands BE, Anderson FH, Bernstein CN, et al. Infliximab maintenance therapy for fistulizing Crohn's disease. N Engl J Med. 2004;350:876–885. doi: 10.1056/NEJMoa030815. [DOI] [PubMed] [Google Scholar]
- 60.Miehsler W, Reinisch W, Kazemi-Shirazi L, et al. Infliximab: lack of effi-cacy on perforating complications in Crohn's disease. Inflamm Bowel Dis. 2004;10:36–40. doi: 10.1097/00054725-200401000-00006. [DOI] [PubMed] [Google Scholar]
- 61.Schecter WP, Hirshberg A, Chang DS, et al. Enteric fistulas: principles of management. J Am Coll Surg. 2009;209:484–491. doi: 10.1016/j.jamcollsurg.2009.05.025. [DOI] [PubMed] [Google Scholar]
- 62.Ribeiro MB, Greenstein AJ, Yamazaki Y, Aufses AH., Jr Intra-abdominal abscess in regional enteritis. Ann Surg. 1991;213:32–36. doi: 10.1097/00000658-199101000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Gutierrez A, Lee H, Sands BE. Outcome of surgical versus percutaneous drainage of abdominal and pelvic abscesses in Crohn's disease. Am J Gastroenterol. 2006;101:2283–2289. doi: 10.1111/j.1572-0241.2006.00757.x. [DOI] [PubMed] [Google Scholar]
- 64.Garcia JC, Persky SE, Bonis PA, Topazian M. Abscesses in Crohn's disease: outcome of medical versus surgical treatment. J Clin Gastroenterol. 2001;32:409–412. doi: 10.1097/00004836-200105000-00010. [DOI] [PubMed] [Google Scholar]
- 65.Jawhari A, Kamm MA, Ong C, Forbes A, Bartram CI, Hawley PR. Intra-abdominal and pelvic abscess in Crohn's disease: results of noninvasive and surgical management. Br J Surg. 1998;85:367–371. doi: 10.1046/j.1365-2168.1998.00575.x. [DOI] [PubMed] [Google Scholar]
- 66.Cirocco WC, Reilly JC, Rusin LC. Life-threatening hemorrhage and exsan guination from Crohn's disease. Report of four cases. Dis Colon Rectum. 1995;38:85–95. doi: 10.1007/BF02053865. [DOI] [PubMed] [Google Scholar]
- 67.Mahmoud N, Rombeau JL, Ross HM, Fry RD. Colon and rectum. In: Townsend CM, Beauchamp RD, Evers BM, Mattox KL, editors. Sabiston Textbook of Surgery. 17th ed. Philadelphia, PA: Saunders; 2004. [Google Scholar]
- 68.Kronberger IE, Graziadei IW, Vogel W. Small bowel adenocarcinoma in Crohn's disease: a case report and review of literature. World J Gastroenterol. 2006;12:1317–1320. doi: 10.3748/wjg.v12.i8.1317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Michelassi F, Testa G, Pomidor WJ, Lashner BA, Block GE. Adenocarcinoma complicating Crohn's disease. Dis Colon Rectum. 1993;36:654–661. doi: 10.1007/BF02238592. [DOI] [PubMed] [Google Scholar]
- 70.Poylin VY, Fischer JE. Small bowel tumors. In: Cameron JL, editor. Current Surgical Therapy. 9th ed. Philadelphia, PA: Mosby-Elsevier; 2008. [Google Scholar]
- 71.Solem CA, Harmsen WS, Zinsmeister AR, Loftus EV., Jr Small intestinal adenocarcinoma in Crohn's disease: a case-control study. Inflamm Bowel Dis. 2004;10:32–35. doi: 10.1097/00054725-200401000-00005. [DOI] [PubMed] [Google Scholar]
- 72.Olaison G, Smedh K, Sjodahl R. Natural course of Crohn's disease after ileo-colic resection: endoscopically visualised ileal ulcers preceding symptoms. Gut. 1992;33:331–335. doi: 10.1136/gut.33.3.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Sachar DB. The problem of postoperative recurrence of Crohn's disease. Med Clin North Am. 1990;74:183–188. doi: 10.1016/s0025-7125(16)30594-6. [DOI] [PubMed] [Google Scholar]
- 74.Reese GE, Nanidis T, Borysiewicz C, Yamamoto T, Orchard T, Tekkis PP. The effect of smoking after surgery for Crohn's disease: a meta-analysis of observational studies. Int J Colorectal Dis. 2008;23:1213–1221. doi: 10.1007/s00384-008-0542-9. [DOI] [PubMed] [Google Scholar]
- 75.Renda MC, Orlando A, Civitavecchia G, et al. The role of CARD15 mutations and smoking in the course of Crohn's disease in a Mediterranean area. Am J Gastroenterol. 2008;103:649–655. doi: 10.1111/j.1572-0241.2007.01589.x. [DOI] [PubMed] [Google Scholar]
- 76.Regueiro M, Schraut W, Baidoo L, et al. Infliximab prevents Crohn's disease recurrence after ileal resection. Gastroenterology. 2009;136:441–450.e1. doi: 10.1053/j.gastro.2008.10.051. quiz 716. [DOI] [PubMed] [Google Scholar]
- 77.Keighley MR, Allan RN. Current status and influence of operation on perianal Crohn's disease. Int J Colorectal Dis. 1986;1:104–107. doi: 10.1007/BF01648416. [DOI] [PubMed] [Google Scholar]
- 78.Regueiro M, Mardini H. Treatment of perianal fistulizing Crohn's disease with infliximab alone or as an adjunct to exam under anesthesia with seton placement. Inflamm Bowel Dis. 2003;9:98–103. doi: 10.1097/00054725-200303000-00003. [DOI] [PubMed] [Google Scholar]
- 79.Topstad DR, Panaccione R, Heine JA, Johnson DR, MacLean AR, Buie WD. Combined seton placement, infliximab infusion, and maintenance immunosuppressives improve healing rate in fistulizing anorectal Crohn's disease: a single center experience. Dis Colon Rectum. 2003;46:577–583. doi: 10.1007/s10350-004-6611-4. [DOI] [PubMed] [Google Scholar]
- 80.Schwartz DA, White CM, Wise PE, Herline AJ. Use of endoscopic ultrasound to guide combination medical and surgical therapy for patients with Crohn's perianal fistulas. Inflamm Bowel Dis. 2005;11:727–732. doi: 10.1097/01.mib.0000172811.57242.18. [DOI] [PubMed] [Google Scholar]
- 81.Schwartz DA, Wiersema MJ, Dudiak KM, et al. A comparison of endoscopic ultrasound, magnetic resonance imaging, and exam under anesthesia for evaluation of Crohn's perianal fistulas. Gastroenterology. 2001;121:1064–1072. doi: 10.1053/gast.2001.28676. [DOI] [PubMed] [Google Scholar]
- 82.Schaefer O, Lohrmann C, Langer M. Assessment of anal fistulas with high-resolution subtraction MR-fstulography: comparison with surgical findings. J Magn Reson Imaging. 2004;19:91–98. doi: 10.1002/jmri.10436. [DOI] [PubMed] [Google Scholar]
- 83.Buchanan GN, Halligan S, Bartram CI, Williams AB, Tarroni D, Cohen CR. Clinical examination, endosonography, and MR imaging in preoperative assessment of fistula in ano: comparison with outcome-based reference standard. Radiology. 2004;233:674–681. doi: 10.1148/radiol.2333031724. [DOI] [PubMed] [Google Scholar]
- 84.Lunniss PJ, Barker PG, Sultan AH, et al. Magnetic resonance imaging of fistula-in-ano. Dis Colon Rectum. 1994;37:708–718. doi: 10.1007/BF02054416. [DOI] [PubMed] [Google Scholar]
- 85.Beets-Tan RG, Beets GL, van der Hoop AG, et al. Preoperative MR imaging of anal fistulas: does it really help the surgeon? Radiology. 2001;218:75–84. doi: 10.1148/radiology.218.1.r01dc0575. [DOI] [PubMed] [Google Scholar]
- 86.Buchanan GN, Halligan S, Williams AB, et al. Magnetic resonance imaging for primary fistula in ano. Br J Surg. 2003;90:877–881. doi: 10.1002/bjs.4125. [DOI] [PubMed] [Google Scholar]
- 87.Singh B, McC Mortensen NJ, Jewell DP, George B. Perianal Crohn's disease. Br J Surg. 2004;91:801–814. doi: 10.1002/bjs.4613. [DOI] [PubMed] [Google Scholar]
- 88.Pritchard TJ, Schoetz DJ, Jr, Roberts PL, Murray JJ, Coller JA, Veidenheimer MC. Perirectal abscess in Crohn's disease. Drainage and outcome. Dis Colon Rectum. 1990;33:933–937. doi: 10.1007/BF02139102. [DOI] [PubMed] [Google Scholar]
- 89.Sohn N, Korelitz BI, Weinstein MA. Anorectal Crohn's disease: definitive surgery for fistulas and recurrent abscesses. Am J Surg. 1980;139:394–397. doi: 10.1016/0002-9610(80)90301-3. [DOI] [PubMed] [Google Scholar]
- 90.Giovannini M, Bories E, Moutardier V, et al. Drainage of deep pelvic abscesses using therapeutic echo endoscopy. Endoscopy. 2003;35:511–514. doi: 10.1055/s-2003-39673. [DOI] [PubMed] [Google Scholar]
- 91.Williams JG, Rothenberger DA, Nemer FD, Goldberg SM. Fistula-in-ano in Crohn's disease. Results of aggressive surgical treatment. Dis Colon Rectum. 1991;34:378–384. doi: 10.1007/BF02053687. [DOI] [PubMed] [Google Scholar]
- 92.Halme L, Sainio AP. Factors related to frequency, type, and outcome of anal fistulas in Crohn's disease. Dis Colon Rectum. 1995;38:55–59. doi: 10.1007/BF02053858. [DOI] [PubMed] [Google Scholar]
- 93.Sangwan YP, Schoetz DJ, Jr, Murray JJ, Roberts PL, Coller JA. Perianal Crohn's disease. Results of local surgical treatment. Dis Colon Rectum. 1996;39:529–535. doi: 10.1007/BF02058706. [DOI] [PubMed] [Google Scholar]
- 94.Faucheron JL, Saint-Marc O, Guibert L, Parc R. Long-term seton drainage for high anal fistulas in Cohn's disease—a sphincter-saving operation? Dis Colon Rectum. 1996;39:208–211. doi: 10.1007/BF02068077. [DOI] [PubMed] [Google Scholar]
- 95.Pearl RK, Andrews JR, Orsay C P, et al. Role of the seton in the management of anorectal fistulas. Dis Colon Rectum. 1993;36:573–577. doi: 10.1007/BF02049864. discussion 577-579. [DOI] [PubMed] [Google Scholar]
- 96.Thornton M, Solomon MJ. Long-term indwelling seton for complex anal fistulas in Crohn's disease. Dis Colon Rectum. 2005;48:459–463. doi: 10.1007/s10350-004-0830-6. [DOI] [PubMed] [Google Scholar]
- 97.Buchanan GN, Owen HA, Torkington J, Lunniss PJ, Nicholls RJ, Cohen CR. Long-term outcome following loose-seton technique for external sphincter preservation in complex anal fistula. Br J Surg. 2004;91:476–480. doi: 10.1002/bjs.4466. [DOI] [PubMed] [Google Scholar]
- 98.Eitan A, Koliada M, Bickel A. The use of the loose seton technique as a definitive treatment for recurrent and persistent high trans-sphincteric anal fistulas: a long-term outcome. J Gastrointest Surg. 2009;13:1116–1119. doi: 10.1007/s11605-009-0826-6. [DOI] [PubMed] [Google Scholar]
- 99.Edwards CM, George BD, Jewell DP, Warren BF, Mortensen NJ, Kettlewell MG. Role of a defunctioning stoma in the management of large bowel Crohn's disease. Br J Surg. 2000;87:1063–1066. doi: 10.1046/j.1365-2168.2000.01467.x. [DOI] [PubMed] [Google Scholar]
- 100.Dejaco C, Harrer M, Waldhoer T, Miehsler W, Vogelsang H, Reinisch W. Antibiotics and azathioprine for the treatment of perianal fistulas in Crohn's disease. Aliment Pharmacol Ther. 2003;18:1113–1120. doi: 10.1046/j.1365-2036.2003.01793.x. [DOI] [PubMed] [Google Scholar]
- 101.Bernstein LH, Frank MS, Brandt LJ, Boley SJ. Healing of perineal Crohn's disease with metronidazole. Gastroenterology. 1980;79:599. [PubMed] [Google Scholar]
- 102.Turunen UM, Farkkila MA, Hakala K, et al. Long-term treatment of ulcerative colitis with ciprofoxacin: a prospective, double-blind, placebo-controlled study. Gastroenterology. 1998;115:1072–1078. doi: 10.1016/s0016-5085(98)70076-9. [DOI] [PubMed] [Google Scholar]
- 103.Brandt LJ, Bernstein LH, Boley SJ, Frank MS. Metronidazole therapy for perineal Crohn's disease: a follow-up study. Gastroenterology. 1982;83:383–387. [PubMed] [Google Scholar]
- 104.Jakobovits J, Schuster MM. Metronidazole therapy for Crohn's disease and associated fistulae. Am J Gastroenterol. 1984;79:533–540. [PubMed] [Google Scholar]
- 105.Pearson DC, May GR, Fick GH, Sutherland LR. Azathioprine and 6-mercaptopurine in crohn disease. A meta-analysis. Ann Intern Med. 1995;123:132–142. doi: 10.7326/0003-4819-123-2-199507150-00009. [DOI] [PubMed] [Google Scholar]
- 106.Hinterleitner TA, Petritsch W, Aichbichler B, Fickert P, Ranner G, Krejs GJ. Combination of cyclosporine, azathioprine and prednisolone for perianal fistulas in Crohn's disease. Z Gastroenterol. 1997;35:603–608. [PubMed] [Google Scholar]
- 107.Egan LJ, Sandborn WJ, Tremaine WJ. Clinical outcome following treatment of refractory inflammatory and fistulizing Crohn's disease with intravenous cyclo-sporine. Am J Gastroenterol. 1998;93:442–448. doi: 10.1111/j.1572-0241.1998.00442.x. [DOI] [PubMed] [Google Scholar]
- 108.Gurudu SR, Griffel LH, Gialanella RJ, Das KM. Cyclosporine therapy in inflammatory bowel disease: short-term and long-term results. J Clin Gastroenterol. 1999;29:151–154. doi: 10.1097/00004836-199909000-00009. [DOI] [PubMed] [Google Scholar]
- 109.Sandborn WJ, Present DH, Isaacs KL, et al. Tacrolimus for the treatment of fistulas in patients with Crohn's disease: a randomized, placebo-controlled trial. Gastroenterology. 2003;125:380–388. doi: 10.1016/s0016-5085(03)00877-1. [DOI] [PubMed] [Google Scholar]
- 110.Parsi MA, Lashner BA, Achkar JP, Connor JT, Brzezinski A. Type of fistula determines response to infliximab in patients with fstulous Crohn's disease. Am J Gastroenterol. 2004;99:445–449. doi: 10.1111/j.1572-0241.2004.04083.x. [DOI] [PubMed] [Google Scholar]
- 111.Ricart E, Panaccione R, Loftus EV, Tremaine WJ, Sandborn WJ. Infliximab for Crohn's disease in clinical practice at the Mayo Clinic: the first 100 patients. Am J Gastroenterol. 2001;96:722–729. doi: 10.1111/j.1572-0241.2001.03612.x. [DOI] [PubMed] [Google Scholar]
- 112.Schiff MH, Burmester GR, Kent JD, et al. Safety analyses of adalimumab (HUMIRA) in global clinical trials and US postmarketing surveillance of patients with rheumatoid arthritis. Ann Rheum Dis. 2006;65:889–894. doi: 10.1136/ard.2005.043166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Colombel JF, Sandborn WJ, Rutgeerts P, et al. Adalimumab for maintenance of clinical response and remission in patients with Crohn's disease: the CHARM trial. Gastroenterology. 2007;132:52–65. doi: 10.1053/j.gastro.2006.11.041. [DOI] [PubMed] [Google Scholar]
- 114.Colombel JF, Schwartz DA, Sandborn WJ, et al. Adalimumab for the treatment of fistulas in patients with Crohn's disease. Gut. 2009;58:940–948. doi: 10.1136/gut.2008.159251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Hobbiss JH, Schofield PF. Management of perianal Crohn's disease. J R Soc Med. 1982;75:414–417. doi: 10.1177/014107688207500609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Morrison JG, Gathright JB, Jr, Ray JE, Ferrari BT, Hicks TC, Timmcke AE. Surgical management of anorectal fistulas in Crohn's disease. Dis Colon Rectum. 1989;32:492–496. doi: 10.1007/BF02554504. [DOI] [PubMed] [Google Scholar]
- 117.Nordgren S, Fasth S, Hulten L. Anal fistulas in Crohn's disease: incidence and outcome of surgical treatment. Int J Colorectal Dis. 1992;7:214–218. doi: 10.1007/BF00341224. [DOI] [PubMed] [Google Scholar]
- 118.Alexander-Williams J, Steinberg DM, Fielding JS, Tompson H, Cooke WT. Proceedings: perianal Crohn's disease. Gut. 1974;15:822–823. [PubMed] [Google Scholar]
- 119.Lindsey I, Smilgin-Humphreys MM, Cunningham C, Mortensen NJ, George BD. A randomized, controlled trial of fibrin glue vs. conventional treatment for anal fistula. Dis Colon Rectum. 2002;45:1608–1615. doi: 10.1007/s10350-004-7247-0. [DOI] [PubMed] [Google Scholar]
- 120.Swinscoe MT, Ventakasubramaniam AK, Jayne DG. Fibrin glue for fistula-in-ano: the evidence reviewed. Tech Coloproctol. 2005;9:89–94. doi: 10.1007/s10151-005-0204-7. [DOI] [PubMed] [Google Scholar]
- 121.Vitton V, Gasmi M, Barthet M, Desjeux A, Orsoni P, Grimaud JC. Long-term healing of Crohn's anal fistulas with fbrin glue injection. Aliment Pharmacol Ther. 2005;21:1453–1457. doi: 10.1111/j.1365-2036.2005.02456.x. [DOI] [PubMed] [Google Scholar]
- 122.Loungnarath R, Dietz DW, Mutch MG, Birnbaum EH, Kodner IJ, Fleshman JW. Fibrin glue treatment of complex anal fistulas has low success rate. Dis Colon Rectum. 2004;47:432–436. doi: 10.1007/s10350-003-0076-8. [DOI] [PubMed] [Google Scholar]
- 123.O'Connor L, Champagne BJ, Ferguson MA, Orangio GR, Schertzer ME, Armstrong DN. Efficacy of anal fistula plug in closure of Crohn's anorectal fistulas. Dis Colon Rectum. 2006;49:1569–1573. doi: 10.1007/s10350-006-0695-y. [DOI] [PubMed] [Google Scholar]
- 124.Champagne BJ, O'Connor LM, Ferguson M, Orangio GR, Schertzer ME, Armstrong DN. Efficacy of anal fistula plug in closure of cryptoglandular fistulas: long-term follow-up. Dis Colon Rectum. 2006;49:1817–1821. doi: 10.1007/s10350-006-0755-3. [DOI] [PubMed] [Google Scholar]
- 125.Ky AJ, Sylla P, Steinhagen R, Steinhagen E, Khaitov S, Ly EK. Collagen fistula plug for the treatment of anal fistulas. Dis Colon Rectum. 2008;51:838–843. doi: 10.1007/s10350-007-9191-2. [DOI] [PubMed] [Google Scholar]
- 126.Talbot C, Sagar PM, Johnston MJ, Finan PJ, Burke D. Infliximab in the surgical management of complex fistulating anal Crohn's disease. Colorectal Dis. 2005;7:164–168. doi: 10.1111/j.1463-1318.2004.00749.x. [DOI] [PubMed] [Google Scholar]
- 127.Matos D, Lunniss PJ, Phillips RK. Total sphincter conservation in high fistula in ano: results of a new approach. Br J Surg. 1993;80:802–804. doi: 10.1002/bjs.1800800651. [DOI] [PubMed] [Google Scholar]
- 128.Makowiec F, Jehle EC, Becker HD, Starlinger M. Clinical course after transanal advancement flap repair of perianal fistula in patients with Crohn's disease. Br J Surg. 1995;82:603–606. doi: 10.1002/bjs.1800820509. [DOI] [PubMed] [Google Scholar]
- 129.Joo JS, Weiss EG, Nogueras JJ, Wexner SD. Endorectal advancement fap in perianal Crohn's disease. Am Surg. 1998;64:147–150. [PubMed] [Google Scholar]
- 130.Robertson WG, Mangione JS. Cutaneous advancement fap closure: alternative method for treatment of complicated anal fistulas. Dis Colon Rectum. 1998;41:884–886. doi: 10.1007/BF02235371. discussion 886-887. [DOI] [PubMed] [Google Scholar]
- 131.Marchesa P, Hull TL, Fazio VW. Advancement sleeve faps for treatment of severe perianal Crohn's disease. Br J Surg. 1998;85:1695–1698. doi: 10.1046/j.1365-2168.1998.00959.x. [DOI] [PubMed] [Google Scholar]
- 132.Galis-Rozen E, Tulchinsky H, Rosen A, et al. Long-term outcome of loose seton for complex anal fistula: a two-centre study of patients with and without Crohn's disease. Colorectal Dis. 2010;12:358–362. doi: 10.1111/j.1463-1318.2009.01796.x. [DOI] [PubMed] [Google Scholar]
- 133.Andreani SM, Dang HH, Grondona P, Khan AZ, Edwards DP. Rectovaginal fistula in Crohn's disease. Dis Colon Rectum. 2007;50:2215–2222. doi: 10.1007/s10350-007-9057-7. [DOI] [PubMed] [Google Scholar]
- 134.Sands BE, Blank MA, Patel K, van Deventer SJ, ACCENT II Study Long-term treatment of rectovaginal fistulas in Crohn's disease: response to infliximab in the ACCENT II study. Clin Gastroenterol Hepatol. 2004;2:912–920. doi: 10.1016/s1542-3565(04)00414-8. [DOI] [PubMed] [Google Scholar]
- 135.Hull TL, Fazio VW. Surgical approaches to low anovaginal fistula in Crohn's disease. Am J Surg. 1997;173:95–98. doi: 10.1016/S0002-9610(96)00420-5. [DOI] [PubMed] [Google Scholar]
- 136.Kodner IJ, Mazor A, Shemesh EI, Fry RD, Fleshman JW, Birnbaum EH. Endorectal advancement fap repair of rectovaginal and other complicated anorectal fistulas. Surgery. 1993;114:682–689. discussion 689-690. [PubMed] [Google Scholar]
- 137.Berman IR. Sleeve advancement anorectoplasty for complicated anorectal/ vaginal fistula. Dis Colon Rectum. 1991;34:1032–1037. doi: 10.1007/BF02049972. [DOI] [PubMed] [Google Scholar]
- 138.Sher ME, Bauer JJ, Gelernt I. Surgical repair of rectovaginal fistulas in patients with Crohn's disease: transvaginal approach. Dis Colon Rectum. 1991;34:641–648. doi: 10.1007/BF02050343. [DOI] [PubMed] [Google Scholar]
- 139.Galandiuk S, Kimberling J, Al-Mishlab TG, Stromberg AJ. Perianal Crohn's disease: predictors of need for permanent diversion. Ann Surg. 2005;241:796–801. doi: 10.1097/01.sla.0000161030.25860.c1. discussion 801-802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Mueller MH, Geis M, Glatzle J, et al. Risk of fecal diversion in complicated perianal Crohn's disease. J Gastrointest Surg. 2007;11:529–537. doi: 10.1007/s11605-006-0029-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Singh B, George BD, Mortensen NJ. Surgical therapy of perianal Crohn's disease. Dig Liver Dis. 2007;39:988–992. doi: 10.1016/j.dld.2007.07.157. [DOI] [PubMed] [Google Scholar]
- 142.Yamamoto T, Allan RN, Keighley MR. Effect of fecal diversion alone on peri-anal Crohn's disease. World J Surg. 2000;24:1258–1262. doi: 10.1007/s002680010250. discussion 1262-1263. [DOI] [PubMed] [Google Scholar]
- 143.Kasparek MS, Glatzle J, Temeltcheva T, Mueller MH, Koenigsrainer A, Kreis ME. Long-term quality of life in patients with Crohn's disease and perianal fistulas: influence of fecal diversion. Dis Colon Rectum. 2007;50:2067–2074. doi: 10.1007/s10350-007-9006-5. [DOI] [PubMed] [Google Scholar]
- 144.Cohen JL, Stricker JW, Schoetz DJ, Jr, Coller JA, Veidenheimer MC. Recto-vaginal fistula in Crohn's disease. Dis Colon Rectum. 1989;32:825–828. doi: 10.1007/BF02554548. [DOI] [PubMed] [Google Scholar]
- 145.Yamamoto T, Bain IM, Allan RN, Keighley MR. Persistent perineal sinus after proctocolectomy for Crohn's disease. Dis Colon Rectum. 1999;42:96–101. doi: 10.1007/BF02235190. [DOI] [PubMed] [Google Scholar]
- 146.Rius J, Nessim A, Nogueras JJ, Wexner SD. Gracilis transposition in complicated perianal fistula and unhealed perineal wounds in Crohn's disease. Eur J Surg. 2000;166:218–222. doi: 10.1080/110241500750009311. [DOI] [PubMed] [Google Scholar]
- 147.van der Hagen SJ, Baeten CG, Soeters PB, Russel MG, Beets-Tan RG, van Gemert WG. Anti-TNF-alpha (infliximab) used as induction treatment incase of active proctitis in a multistep strategy followed by definitive surgery of complex anal fistulas in Crohn's disease: a preliminary report. Dis Colon Rectum. 2005;48:758–767. doi: 10.1007/s10350-004-0828-0. [DOI] [PubMed] [Google Scholar]