Abstract
The posttraumatic diagnostic scale (PDS) is a self-report instrument for PTSD that is simple to administer and has demonstrated good psychometric properties. We compared the PDS with the gold standard clinician administered PTSD scale (CAPS) diagnostic interview for PTSD. We assessed 138 women who were victims of domestic violence using both the PDS and the CAPS. Findings confirmed that PTSD develops at a high base rate in this sample. The PDS generally performed well in relation to the CAPS although with a tendency to overdiagnose PTSD. The findings lend further support to the use of the PDS as a diagnostic tool for PTSD but indicate that it is better at identifying survivors with PTSD than those without the disorder.
Keywords: posttraumatic stress disorder, diagnosis, domestic violence
A number of good measures for posttraumatic stress disorder (PTSD) have been developed in the past 15 years including the Clinician Administered PTSD Scale (CAPS; Blake, Weathers, Nagy, & Kaloupek, 1995) and the Posttraumatic Diagnostic Scale (PDS; Foa, Cashman, Jaycox, & Perry, 1997). Both of these assessment instruments measure the same core set of PTSD symptoms as defined in the DSM-IV (American Psychiatric Association, 1994) and have demonstrated solid psychometric properties in trauma populations.
Administration of the CAPS should be done by a mental health professional or a paraprofessional with appropriate training (Blake et al., 1995) whereas the PDS on the other hand is a self-report instrument. The PDS has been compared to the Structured Clinical Interview for DSM-III-R (SCID; Spitzer, Williams, Gibbon, & First, 1990) in a general population of trauma victims and was found to perform quite well for the diagnosis of PTSD and to show good test–retest reliability and internal consistency (Foa et al., 1997). The PDS is a less costly alternative to the CAPS because administration does not require a trained professional.
Recently Sheeran and Zimmerman (2002) compared the performance of the PDS to the SCID PTSD module in a large psychiatric outpatient sample and found that it performed very well to identify PTSD positive participants using a simple cutoff score. Analysis of this psychiatric sample produced a prevalence rate of 11.2% for full PTSD based upon the SCID interview. Thus, this was a sample with a fairly low prevalence of PTSD compared to a traumatized sample. The optimal cutoff score for identifying PTSD cases with the PDS was 27 and produced a kappa of .50 and a sensitivity of .67 and specificity of .91.
The performance of the PDS has not been tested against the CAPS, the current gold-standard instrument for the diagnosis of PTSD (Weathers, Keane, & Davidson, 2001). In addition there is little information about how this instrument performs in the highly symptomatic and clinically complex trauma population of survivors of domestic violence (DV). Self-report instruments may not perform as well in situations where the trauma survivor has multiple similar traumatic events. The diagnosis of PTSD is designed to be derived from a single traumatic incident (American Psychiatric Association, 1994) with questions that pertain to symptoms that evolve from the traumatic event. However it is not clear how well the PDS would perform in comparison to the CAPS in more ambiguous situations such as when there are multiple traumatic events as in domestic violence (DV) situations. Survivors of domestic violence often report that they are the victims of repeated violent episodes that may occur over many years (Berliner, 1987; Walker, 1984). Assessment of PTSD symptoms in this kind of trauma population is more complex due to the ongoing nature of the traumatic experiences. The purpose of the present paper is to report on a sample of female survivors of domestic violence that were assessed with the PDS and the CAPS.
Methods
Participants
The participants were 138 female domestic violence survivors (mean age = 34.4 years, SD = 8.2, range = 18–59; race = 62% African American, 31% White, 7% other; mean education = 12.7 years, SD = 2.1, range = 8–19, education data missing for one participant). Examination of participant household income levels revealed that this was mostly a low-income sample with 28% earning less than $10,000 per year, 24% earning $10,000–20,000, 16% earning $20,000–30,000, 20% earning $30,000–50,000, and 12% earning more than $50,000. Income data were missing for one participant. In terms of family structure, 36% of the participants had no children, 23% had one child, 21% had two children, 12% had three children, and 8% had four or more children. Most of the women in the sample were in a violent relationship with a male partner (97%). Participants were recruited from established DV shelters (n = 69) or were nonshelter participants recruited from community agencies (n = 69). The average length of the relationship was 6.9 years (range = 3 months – 27 years) and the average length of the abuse was 4.5 years (range = 2.9 months – 24 years) in this sample.
These participants were part of a larger study of domestic violence survivors (n = 413) and were included here because they had completed an assessment process that included the PDS and the CAPS interview. Twenty-four women were screened out of the study for the following reasons: two women were with their partners for less than 3 months; six women reported fewer than the required number of episodes of physical violence; 15 women reported abuse that occurred more than 6 months ago and one woman declined to participate after hearing more about the study. Participants who were ruled out of the study based on their telephone screening were given support, thanked for their time, and were provided with information about appropriate resources in the community.
Clinical Instruments
Posttraumatic Diagnostic Scale (PDS; Foa et al., 1997)
The PDS is a 17-item self-report instrument that can provide both a diagnosis of PTSD and measures of overall and subscale symptom severity. Respondents rate each item on a 4-point scale (0 = not at all to 3 = very much) over a period of the past month. A symptom is counted as present if a score of 1 or higher is selected. These frequency scores are summed to produce a severity score. A total score of 15 or higher along with the standard PTSD criteria of DSM-IV which includes exposure to an event that involved the threat of death or serious injury and elicits fear or helplessness and produces at least one reexperiencing symptom, three avoidance symptoms, and two arousal symptoms as well as clinically significant distress is considered a positive screen for PTSD (Sheeran & Zimmerman, 2002).
The PDS was normed on a diverse base of 248 men and women between the ages of 17 and 65 who had experienced or witnessed a wide variety of traumatic events (e.g. natural disaster, accident/fire, sexual and nonsexual assault, combat, life-threatening illness) at least one month before the PDS scale was administered (Foa et al., 1997). The scale’s performance was examined in relation to the PTSD module from the SCID. It was found to provide good diagnostic agreement with the SCID and to have good sensitivity and specificity. The PDS demonstrated high internal consistency (Cronbach’s α = .92) and test–retest reliability (κ = .74 for PTSD diagnosis; κ = .83 for total PDS score).
In this study, because of the chronic nature of domestic violence in which women typically report many incidents that might be legitimate Criterion A events, the responses on the PDS assessment were based upon the women’s self-reported most traumatic event.
Clinician Administered PTSD Scale (CAPS; Blake et al., 1995)
The CAPS is a 22-item scale with three associated features assessing validity. severity, and improvement. The CAPS contains separate 5-point frequency and intensity rating scales (0–4) for symptoms identified with PTSD in the DSM-IV. The CAPS also has items that rate social and occupational functioning, global PTSD symptom severity, and the validity of the participant’s responses. Interrater reliability on both frequency and severity ratings is reported to be better than .92 for each of the three symptom subscales. Internal consistency was also good for the three subscales with an alpha of .87 or greater for each of the symptom clusters. Convergent validity was reported for the following measures: Mississippi Scale for PTSD, .91, MMPI-2 PTSD scale, .77 and SCID PTSD, .89.
The CAPS gives both a continuous score of symptom frequency and intensity as well as the ability to make diagnostic determinations of PTSD status. In this study, for an item to meet diagnostic criterion a person had to receive a score of at least 1 on frequency and a 2 on intensity and ratings were made for the past month. The CAPS assessment was based upon the women’s self-reported most traumatic event (the same event used for the PDS). The CAPS was administered by master’s or doctoral level clinicians experienced in working with trauma survivors. In this study, the reliability of the CAPS interview was assessed for 40 randomly selected cases by having a second clinician listen to a tape recording of the original assessment and complete a second CAPS assessment. Inter-rater reliability for diagnostic agreement was found to be excellent with agreement on 39 out of 40 cases (κ = .93, p < .001).
Revised Conflict Tactics Scale-2 (CTS-2; Straus, Hamby, Boney-McCoy, & Sugarman, 1996)
In order to get an assessment of the level of violence in the relationship we used the CTS-2. This 33-item self-report scale has been widely used to measure the level of conflict among couples. Subscale scores provide information about physical aggression, psychological aggression, and injury. Internal consistency for these subscales is reported to be very good to excellent ranging from .86–.95.
Procedure
Prior to starting the study, written informed consent was obtained from all participants. The PDS was administered first as part of a series of self-report questionnaires that were programmed into a laptop computer. Participant responses to each question automatically triggered the next question on the questionnaire. Participants could change responses if they wished and were instructed in how to go back to a previous question. Previous research suggests that this form of administration works well in trauma survivors (Griffin, Resick, Waldrop, & Mechanic, 2003). Following completion of the self-report measures a female clinician administered the CAPS. This order of administration was used to ensure that the responses on the PDS would not be contaminated by the diagnostic interview.
Women were eligible to participate in the study if they had been the victims of battering by an intimate partner and they had been in the intimate relationship for at least 3 months. In addition, the last episode of battering had to be within 6 months of the assessment.
Battering was defined by responses on the revised CTS-2 (Straus et al., 1996) as four or more incidents of minor violence (e.g., pushed, shoved, slapped, twisted arm, pulled hair, threw things at her), two or more severe incidents (e.g., punched with fist, choked, slammed into wall, thrown down stairs, kicked, threatened with or used a weapon, forced to have sex, caused them to fear for their life or the lives of a family member), or any combination of four or more minor and severe incidents during the past year of the relationship. Exclusionary criteria included apparent psychosis, intoxication, mental retardation, or illiteracy to ensure that informed consent could be given.
Analyses
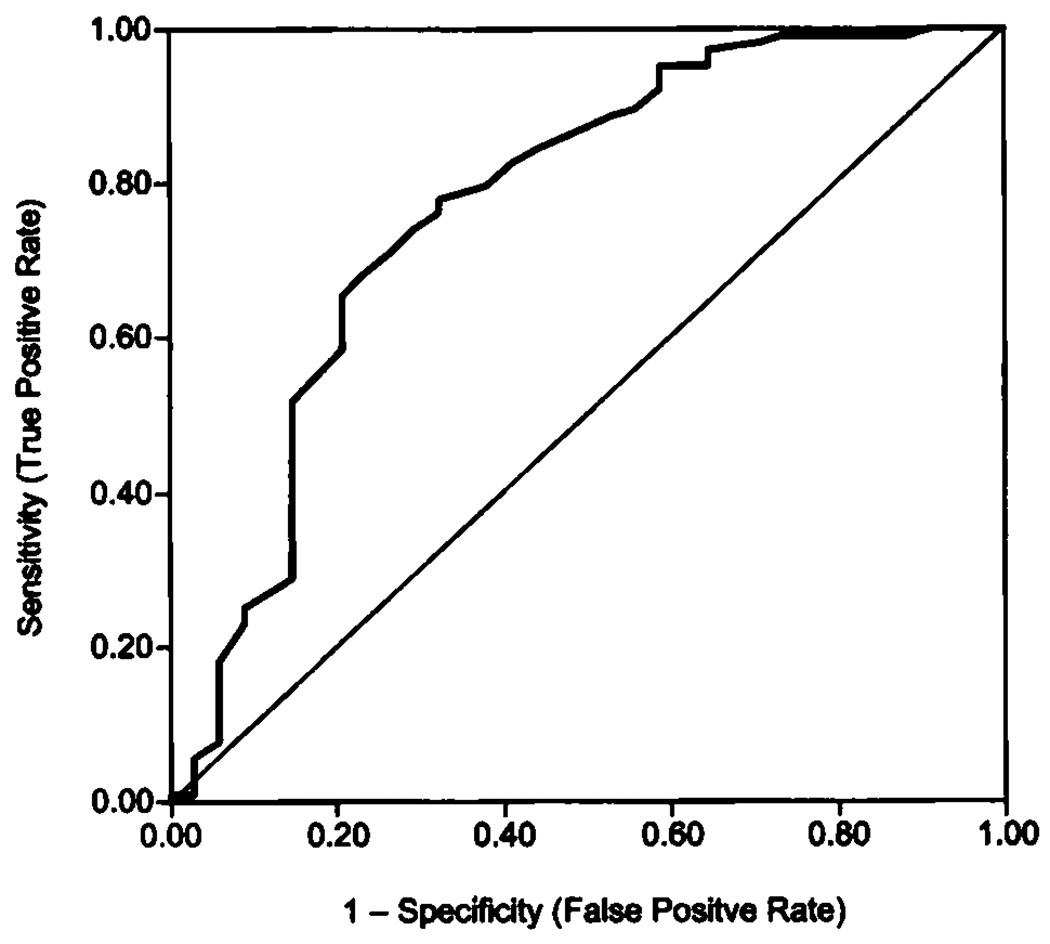
Receiver-operator curve (ROC) analysis was conducted to examine the utility of the PDS compared to the CAPS. On the basis of signal detection theory, ROC analysis provides quantitative information regarding the diagnostic utility of a measure compared to a “gold standard,” independent of the cut-score used for diagnostic decisions (McFall & Treat, 1999; Meehl & Rosen, 1995). The sensitivity (true positive rate) and false-alarm rates (1—specificity) associated with various cut-scores are plotted on a curve, providing a metric for comparing the incremental validity of an assessment method (Hsiao, Bartko, & Potter, 1989). The area under the curve (AUC) determines whether the diagnostic accuracy of the measure is better than chance (.50, represented by a diagonal line on the X–Y axis). A reasonable level of precision can be attained with as few as 100 observations using ROC analysis (Mossman & Somoza, 1989).
Comparisons of the performance of the PDS to the CAPS also took the form of cross-tabulations comparing PTSD case identification. Based upon these calculations a number of subsequent statistics were derived including: sensitivity (ability to correctly identify individuals with PTSD), specificity (ability to correctly identify individuals without PTSD), false-positive rate, false-negative rate, positive predictive power (agreement in the presence of PTSD), negative predictive power (agreement in the absence of PTSD), overall diagnostic power, kappa (intertest agreement), prevalence (percent of the sample with a PTSD diagnosis), and “well” rate (percent of the sample without a PTSD diagnosis). These calculations were performed for the recommended cutoff score of 15 (D. F. Tolin, personal communication, October, 2000, as cited in Sheeran & Zimmerman, 2002) and for the cutoff score that maximized kappa as well as the PDS PTSD criteria.
Pearson correlations were calculated between the total scale scores and each subscale score for all participants. Finally, means and standard deviations were calculated for each scale total score and subscale scores, grouped by CAPS PTSD diagnosis, and compared via analysis of variance. Z-scores were also calculated so that each scale score could be compared on a common metric.
Results
Analysis of the CAPS interview revealed that this was a highly symptomatic sample with 104 (75%) of the 138 women diagnosed with PTSD. The ability of the PDS to approximate the results of the CAPS is presented in Table 1. The table presents indices for the PDS using the standard DSM-IV PTSD criteria, and the recommended cut score of 15 and the empirically derived cut score of 17 that maximized the kappa statistic. In addition, each of these cut scores is also paired with the standard PTSD criteria.
Table 1.
Performance Measures of the PDS to Detect PTSD Status Relative to the CAPS Diagnosis of PTSD
| PDS cut score = 15 | PDS cut score = 17 | ||||
|---|---|---|---|---|---|
| Statistic | PDS PTSD criteria only |
Cut score only |
Cut score+ PTSD criteria |
cut score only |
Cut score + PTSD criteria |
| Sensitivity | .94 | .97 | .92 | .95 | .90 |
| Specificity | .53 | .35 | .56 | .41 | .59 |
| False-positive rate | .47 | .65 | .44 | .59 | .41 |
| False-negative rate | .06 | .03 | .08 | .05 | .10 |
| Positive predictive power | .86 | .82 | .86 | .83 | .87 |
| Negative predictive power | .75 | .80 | .70 | .74 | .67 |
| Overall diagnostic power | .84 | .82 | .83 | .82 | .83 |
| Kappa | .52 | .40 | .52 | .43 | .51 |
| Prevalence | .83 | .89 | .80 | .86 | .78 |
| “Well” rate | .17 | .11 | .20 | .14 | .22 |
Note. Data are presented for the recommended PDS cutoff score and the empirically derived score as well as only using the PTSD criteria (note that the CAPS prevalence was .75).
Using the recommended PDS cut-score of 15, 123 participants met criteria for PTSD (89%). Using an empirically derived cut-score of 17 for this sample, the cut-score with maximum intertest agreement (kappa) with the CAPS interview, 119 participants met PTSD criteria (86%). The addition of the PTSD criteria to the cut scores improved the agreement with the CAPS with the best performance observed using a combination of a cut score of 17 and the PTSD criteria producing a close match to the CAPS with a 78% prevalence rate. Using only the PDS PTSD criteria there were 114 women (83%) diagnosed with PTSD, an increase of 8% over the CAPS.
The ROC curve analysis presented in Fig. 1 indicates that the diagnostic utility of the PDS was significantly better than chance, with the area under the curve equal to .77 (p < .001). The PDS showed extremely high sensitivity at both cut-scores, but specificity increased with the sample-derived cut-score (.35–.41). Overall, PDS specificity was poor in this sample, showing a high false-positive rate (ranging from 65−41%). Additional measures of diagnostic confidence, or the chances of accurately predicting the presence or absence of PTSD by PDS score, include the predictive power statistics (Baldessari, Finklestein, & Arana, 1983). Positive predictive power was good ranging from .82–.87, and negative predictive power was somewhat lower ranging from .67–.80.
Fig. 1.
Receiver operating characteristic (ROC) curve of PDS cut-scores. Area under the curve = 0.77, SE = 0.052, p < .001. The diagonal line represents chance performance.
The overall means, standard deviations, and Pearson correlations are reported in Table 2 for the PDS subscales and total score and the CAPS subscales and total score. For the CAPS, scores have been calculated as a frequency score only and as a score derived from summing the frequency and the intensity ratings. The means and standard deviations for both the CAPS and the PDS grouped by PTSD diagnosis as determined on the CAPS are reported in Table 3. Z-scores are also reported because the PDS and CAPS response are different (0–3 and 0–4 respectively). The Z-scores provide a convenient way to compare changes on these scales across conditions on a common metric. The results indicate that the scores on the PDS tended to be comparable for each Of the subscales and for the total scores.
Table 2.
Correlations Between the PDS and the CAPS Subscale Scores (n = 138)
| Variable | M | SD | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | PDS reexperiencing | 8.0 | 3.8 | .64 | .64 | .85 | .66 | .40 | .55 | .61 | .68 | .38 | .56 | .60 |
| 2. | PDS avoidance | 11.8 | 5.0 | .70 | .91 | .47 | .62 | .53 | .64 | .51 | .61 | .55 | .65 | |
| 3. | PDS arousal | 9.3 | 3.8 | .88 | .50 | .47 | .66 | .63 | .55 | .45 | .67 | .63 | ||
| 4. | PDS total | 29.1 | 11.1 | .61 | .58 | .65 | .71 | .65 | .56 | .67 | .71 | |||
| 5. | CAPS reexperiencing (frq only) | 9.0 | 4.5 | .52 | .64 | .82 | .94 | .51 | .65 | .79 | ||||
| 6. | CAPS avoidance (frq only) | 14.2 | 6.1 | .63 | .87 | .56 | .98 | .66 | .87 | |||||
| 7. | CAPS arousal (frq only) | 10.9 | 4.8 | .88 | .64 | .61 | .97 | .84 | ||||||
| 8. | CAPS total (frq only) | 34.0 | 13.3 | .81 | .85 | .88 | .98 | |||||||
| 9. | CAPS reexperiencing (frq + int) | 17.9 | 8.6 | .55 | .67 | .83 | ||||||||
| 10. | CAPS avoidance (frq + int) | 26.2 | 11.5 | .65 | .88 | |||||||||
| 11. | CAPS arousal (frq + int) | 20.7 | 8.7 | .88 | ||||||||||
| 12. | CAPS total (frq + int) | 64.8 | 25.0 |
Note. Frq = Frequency; Int = Intensity. For all correlation coefficients: p < .01.
Table 3.
Means, Standard Deviations, and Z-scores for the PDS and the CAPS Grouped by PTSD Diagnosis as Determined by the CAPS Interview
| PTSD (n = 104) | Non-PTSD (n = 34) | ||||
|---|---|---|---|---|---|
| Measure | M | SD | M | SD | F value |
| PDS | |||||
| Total score | |||||
| Raw score | 31.9 | 9.2 | 20.6 | 12.3 | |
| Z-Score | 0.25 | 0.83 | −0.76 | 1.1 | 32.1*** |
| Reexperiencing | |||||
| Raw score | 8.7 | 3.3 | 5.7 | 4.3 | |
| Z-Score | 0.19 | 0.88 | −0.58 | 1.14 | 17. 1*** |
| Avoidance | |||||
| Raw score | 13.1 | 4.1 | 7.7 | 5.3 | |
| Z-Score | 0.27 | 0.82 | −0.81 | 1.10 | 37.6*** |
| Arousal | |||||
| Raw score | 10.0 | 3.4 | 7.1 | 4.2 | |
| Z-Score | 0.19 | 0.89 | −0.58 | 1.10 | 16.7*** |
| CAPS | |||||
| Total freq. score | |||||
| Raw score | 39. 1 | 9.6 | 18.4 | 10.2 | |
| Z-score | 0.39 | 0.73 | −1.18 | 0.77 | 114.7*** |
| Reexperiencing | |||||
| Raw score | 10.0 | 4.2 | 5.7 | 3.9 | |
| Z-Score | 0.23 | 0.93 | −0.71 | 0.86 | 27.5*** |
| Avoidance | |||||
| Raw score | 16.7 | 4.3 | 6.6 | 4.2 | |
| Z-Score | 0.41 | 0.70 | −1.30 | 0.69 | 145.9*** |
| Arousal | |||||
| Raw score | 12.4 | 3.7 | 6.2 | 4.9 | |
| Z-Score | 0.32 | 0.76 | −0.98 | 1.01 | 62.1*** |
| CTS | |||||
| Physical aggression | 82.1 | 69.3 | 47.9 | 45.4 | 7.2.** |
| Psychological aggression | 109.1 | 46.8 | 80.6 | 40.2 | 10.1** |
| Injury | 25.9 | 24.5 | 16.9 | 19.4 | 3.9* |
Note:
P < .05,
P < .01,
P < .001.
Discussion
The findings suggest that in this clinical sample of battered women, the self-report measure of PTSD derived from the PDS performed well as a proxy for the full CAPS interview. However the PDS tended to produce an overestimate of the prevalence of PTSD compared to the CAPS in this domestic violence sample (ranging from 78–89% depending on criterion score vs. 75%, respectively). This is not surprising because the CAPS is based upon indices of the frequency and the intensity of symptoms and the PDS diagnosis is based upon a simple endorsement of the symptoms being present. In addition, the CAPS score also relies upon the clinical judgment of a trained interviewer. We observed generally better performance by the PDS at identifying individuals with PTSD as diagnosed on the CAPS (sensitivity—true positive rate of the disorder) than at identifying individuals who did not have the disorder (specificity—true negative rate of the disorder). The high base rate of PTSD (75%) observed in this sample of DV survivors is notable and was likely the result of the relatively stringent abuse criteria as defined by responses on the CTS that we used for inclusion in the study, but also reflects the chronic and traumatic nature of domestic violence (Astin, Lawrence, & Foy, 1993; Houskamp & Foy, 1991).
The high base rate of PTSD observed here is significant in terms of the implications for assessment and treatment of domestic violence survivors who may suffer PTSD at extremely high rates. This domestic violence sample also provides a useful comparison for the assessment of the functioning of the PDS instrument in a highly symptomatic sample that has experienced multiple traumas over an extended of time. The chronic nature of domestic violence which provokes a large amount of PTSD symptomatology may be a partial explanation for the tendency of the PDS to overestimate PTSD in this type of sample.
The findings from this study were similar to those reported by Foa et al. (1997) in a general trauma sample. However, our findings of agreement between the CAPS and the PDS were not as strong as the earlier findings using the SCID as the gold standard. In particular, Foa, et al. reported a kappa of .65 between the PDS and the SCID PTSD module and sensitivity of .89 and specificity of .75. Comparing the best results from our study, using the sample derived cutoff of 17 plus the standard PTSD symptom criteria, indicated approximately the same degree of sensitivity (.90) but lesser specificity (.59). This also was reflected in our finding of a relatively high false positive rate (.41) and lower kappa (.51).
Our findings are also generally in agreement with the work of Sheeran and Zimmerman (2002). However they found that a simple cutoff score on the PDS of 27 was optimal for agreement with the SCID diagnosis of PTSD. Our sample-derived best cutoff was considerably lower at 17. This is likely the result of the much lower base rate of PTSD in their community sample (11.2% vs. 75% in the current study).
One limitation of the this study is that the order of presentation of the instruments was always done with the PDS presented first and then followed by the CAPS interview. It is unclear what, if any, effect this may have had on the participant’s responses to the symptom items. Our reasoning for this order was that the extra probes that are done by the interviewers during the CAPS assessment would likely have changed the response to the PDS in potentially significant ways.
The findings provide support for the use of the PDS in a research setting for the assessment of PTSD. The PDS tended to provide close agreement with the CAPS diagnosis of PTSD and our findings suggest the PDS is a reasonable proxy for the full CAPS interview albeit with a tendency to overdiagnose the disorder. This issue may be exacerbated when the PDS is used in a highly traumatized and symptomatic sample.
Acknowledgment
This work was supported by NIMH grant MH55542.
Footnotes
Copyright of Journal of Traumatic Stress is the property of John Wiley & Sons, Inc.. The copyright in an individual article may be maintained by the author in certain cases. Content may not be copied or emailed to multiple sites or posted to a listserv without the copyright holder's express written permission. However, users may print, download, or email articles for individual use.
References
- American Psychiatric Association. Diagnostic and statisitical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Astin MC, Lawrence KJ, Foy DW. Posttraumtic stress disorder among battered women: Risk and resiliency factors. Violence and Victims. 1993;8:17–28. [PubMed] [Google Scholar]
- Baldessari RJ, Finklestein S, Arana GW. The predictive power of diagnostic tests and the effect of prevalence of illness. Archives of General Psychiatry. 1983;40:569–573. doi: 10.1001/archpsyc.1983.01790050095011. [DOI] [PubMed] [Google Scholar]
- Berliner L. The frequency of interpersonal violence: What do the studies tell us? Journal of Interpersonal Violence. 1987;2:223–224. [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG. The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Foa EB, Cashman L, Jaycox L, Perry K. The validation of a self-report measure of posttraumatic stress disorder: The Posttraumatic Diagnostic Scale. Psychological Assessment. 1997;9(4):445–451. [Google Scholar]
- Griffin MG, Resick PA, Waldrop AE, Mechanic MB. Participation in trauma research: Is there evidence of harm? Journal of Traumatic Stess. 2003;16:221–227. doi: 10.1023/A:1023735821900. [DOI] [PubMed] [Google Scholar]
- Houskamp BM, Foy DW. The assessment of posttraumatic stress disorder in battered women. Journal of Interpersonal Violence. 1991;6:367–375. [Google Scholar]
- Hsiao JK, Bartko JJ, Potter WZ. Diagnosing diagnoses. Archives of General Psychiatry. 1989;46:664–667. doi: 10.1001/archpsyc.1989.01810070090014. [DOI] [PubMed] [Google Scholar]
- McFall RM, Treat TA. Quantifying the information value of clinical assessments with signal detection theory. Annual Review of Psychology. 1999;50:215–241. doi: 10.1146/annurev.psych.50.1.215. [DOI] [PubMed] [Google Scholar]
- Meehl PE, Rosen A. Antecedent probability and the efficiency of psychometric signs, patterns, or cutting scores. Psychology Bulletin. 1995;52:194–216. doi: 10.1037/h0048070. [DOI] [PubMed] [Google Scholar]
- Mossman D, Somoza E. Maximizing diagnostic information from the dexamethasone suppression test. Archives of General Psychiatry. 1989;46:653–660. doi: 10.1001/archpsyc.1989.01810070079013. [DOI] [PubMed] [Google Scholar]
- Sheeran T, Zimmerman M. Screening for posttraumatic stress disorder in a general psychiatric outpatient setting. Journal of Consulting and Clinical Psychology. 2002;70:961–966. doi: 10.1037//0022-006x.70.4.961. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Williams JBW, Gibbon M, First MB. Structured Clinical Interview for DSM-III-R-Patient edition (with Psychotic Screen; SCID-P) Washington, DC: American Psychiatric Press; 1990. [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, Sugarman DB. The revised Conflict Tactics Scale (CTS2) Journal of Family Issues. 1996;17:283–316. [Google Scholar]
- Walker LA. Battered women, psychology, and public policy. American Psychologist. 1984;39:1178–1182. doi: 10.1037//0003-066x.39.10.1178. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JRT. Clinician-Administered PTSD scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]