Abstract
The purpose of this study was to compare cognitive-processing therapy (CPT) with prolonged exposure and a minimal attention condition (MA) for the treatment of posttraumatic stress disorder (PTSD) and depression. One hundred seventy-one female rape victims were randomized into 1 of the 3 conditions, and 121 completed treatment. Participants were assessed with the Clinician-Administered PTSD Scale, the PTSD Symptom Scale, the Structured Clinical Interview for DSM–IV, the Beck Depression Inventory, and the Trauma-Related Guilt Inventory. Independent assessments were made at pretreatment, posttreatment, and 3 and 9 months posttreatment. Analyses indicated that both treatments were highly efficacious and superior to MA. The 2 therapies had similar results except that CPT produced better scores on 2 of 4 guilt subscales.
Cognitive-processing therapy (CPT) was introduced as a possible treatment for posttraumatic stress disorder (PTSD) nearly a decade ago. CPT, specifically designed for the treatment of PTSD resulting from sexual assault, consists of two integrated components: cognitive therapy and exposure in the form of writing and reading about the traumatic event (Resick, 1992; Resick & Schnicke, 1992, 1993). The therapy focuses initially on assimilated–distorted beliefs such as denial and self-blame. Then the focus shifts to overgeneralized beliefs about oneself and the world. Beliefs and assumptions held before the trauma are also considered. Clients are taught to challenge their beliefs and assumptions through Socratic questioning and the use of daily worksheets. Once dysfunctional beliefs are deconstructed, more balanced self-statements are generated and practiced. The exposure component consists of having clients write detailed accounts of the most traumatic incident(s) that they read to themselves and to the therapists. Clients are encouraged to experience their emotions while writing and reading, and the accounts are then used to determine “stuck points”: areas of conflicting beliefs, leaps of logic, or blind assumptions.
In addition to a series of case study reports that indicated the therapy to be promising (Calhoun & Resick, 1993; Resick, 1992; Resick & Markway, 1991), Resick and Schnicke (1992) reported on CPT presented in a group-therapy format as compared with a naturally occurring wait-list condition. This 12-session therapy appeared to be effective for both PTSD and depressive symptoms in a first report in which 19 women treated with CPT were compared with 20 wait-list women. At 3- and 6-month follow-ups, none of the treated women met the criteria for PTSD (Resick & Schnicke, 1992). Although there was no specific bias in assignment to condition, there was not, unfortunately, random assignment to groups, nor was there independent assessment. Subsequently, the treatment manual was published with data reported on 36 women who were treated in a group format and 9 who completed individual treatment. The therapy package continued to be quite promising.
Clearly, the next step in examining CPT as a viable treatment for PTSD was to conduct a comparative outcome study. Aside from comparison with a waiting-list group, the therapy should also be compared against the best available treatment package (Kazdin, 1998). The therapy approaches that have received the most empirical support for treating PTSD among sexual assault survivors to this point are prolonged exposure (PE) and stress inoculation training (SIT; Foa et al., 1999; Foa, Rothbaum, Riggs, & Murdock, 1991). PE is a package that begins with education and breathing retraining and then introduces behavioral exposure to feared environmental reminders of the trauma and imaginal exposure to the trauma memory. SIT is a coping skills treatment protocol that includes education, skill building for relaxation, cognitive restructuring, and behavioral rehearsal (such as covert modeling, role-playing, and behavioral exposures) to reduce avoidance of feared stimuli (Kilpatrick, Veronen, & Resick, 1982; Resick, Jordan, Girelli, Hutter, & Marhoefer-Dvorak, 1988).
Foa et al. (1991) compared the efficacy of PE, SIT, supportive counseling, and a waiting-list control group for PTSD among raped or physically assaulted women. For their comparison studies, Foa and her colleagues eliminated the behavioral exposure component from SIT. At posttreatment, they found all four groups had improved significantly (including the waiting-list group), but the SIT group improved more than the supportive counseling and wait-list groups in terms of overall PTSD severity. The groups improved equally with regard to fear, anxiety, and depression. A second analysis comparing SIT, PE, and supportive counseling completers over time, including the follow-up, indicated no significant changes from post-therapy to a 3-month follow-up, although there was a trend for those receiving PE to improve after treatment on PTSD severity. There was no change from posttreatment to follow-up on any of the other measures in any of the groups. Neither SIT nor PE was superior to supportive counseling or a waiting list in terms of other measures of fear, anxiety, or depression.
In a second study, Foa et al. (1999) compared PE, SIT, and a combination of PE and SIT with a waiting-list control. The SIT–PE combination provided the same amount of therapy but divided the sessions into a shorter exposure component along with stress inoculation skills. Foa et al. found that all three therapies significantly reduced symptoms of PTSD and depression relative to the waiting list. PE appeared to improve general anxiety better than SIT or SIT–PE, whereas the results for PTSD and depression were similar for the three groups across a 1-year follow-up. Foa et al. developed an end-state index that combined measures of PTSD, depression, and anxiety. They found that 52% of PE, 31% of SIT, and 27% of PE–SIT participants had good end-state functioning. There was a significant difference between PE and PE–SIT. PE was chosen as the best comparison therapy for this study.
The purpose of the current study was to conduct a controlled trial with sufficient power to compare individually administered CPT with prolonged exposure and a minimal attention waiting-list condition (MA) among victims of rape with regard to symptoms of PTSD and depression. Both therapy packages were directly compared as developed, with no elements excluded in either protocol. However, there was an effort not to introduce “casual cognitive therapy” in the PE protocol or to conduct prolonged imaginal or behavioral exposures in the CPT protocol.
A secondary purpose was to examine the effects of both therapies on dysfunctional cognitions, specifically self-blame and guilt cognitions. If exposure therapy provides a corrective experience, then women who receive PE should exhibit changes in cognitions as well as symptoms. However, because cognitive therapy is specifically tailored to challenge dysfunctional cognitions, it was hypothesized that CPT would be more effective in altering guilt cognitions than PE. Indeed, Foa and McNally (1996) suggested that “therapeutic procedures effective for fear may be ineffective, or even harmful, for guilt and other negative emotions” (p. 340). They suggested that cognitive therapies may be more effective in addressing pathological guilt.
Method
Participants
Exclusion criteria included current psychosis, developmental disabilities, suicidal intent, current parasuicidal behavior, current dependence on drugs or alcohol, and illiteracy. In addition, participants could not currently be in an abusive relationship or being stalked. In the case of marital rape, the participant must have been out of the relationship for at least 6 months. Those with a history of incest were not excluded as long as there was another index rape that met the primary criterion for PTSD. Participants were included if they had experienced a discrete incident of completed rape (oral, anal, or vaginal) in childhood or adulthood, they were at least 3 months posttrauma (no upper limit), and, if on medication, they were stabilized. Women with a history of substance dependence were included if or when they had been off of the substance(s) for 6 months. Those with substance abuse histories were permitted to participate if they agreed and were deemed able to desist in usage during the period of treatment.
Two hundred sixty-seven women were assessed for possible participation. The most common reason for exclusion from the study (n = 74) was not meeting the criteria for PTSD (74%). Seven percent of the women were excluded because of ongoing domestic violence, 4% because of substance dependence, 4% because of current suicidal intent, and 9% as a result of other exclusion criteria. Twelve women failed to complete the initial assessment. Of 181 women randomized into the trial, 10 were terminated from the study as a result of meeting exclusion criteria subsequent to new violence (women had to be at least 3 months posttrauma), changes in medication, or substance dependence relapse. Therefore, the intent-to-treat (ITT) sample included 171 women, among whom 13 never returned for the first session. Thirty-seven women dropped out of treatment, and 121 women completed treatment along with at least the posttreatment assessment: 41 CPT clients, 40 PE clients, and 40 MA clients. Dropout rates for the two active treatment groups were similar: 26.8% for CPT and 27.3% for PE. In the MA condition, 14.9% did not return for the second assessment. There were no significant differences between women who dropped out of therapy and those who completed therapy with regard to their initial PTSD or depression scores.
In the ITT sample, there were no significant differences in demographic characteristics among the three groups. Overall, the average age of the women was 32 years (SD = 9.9), and they had a mean of 14.3 years of education (SD = 2.6). The majority of the women had never been married or were divorced or separated (75.7%). The sample was 71% White, 25% African American, and 4% of other racial backgrounds. Average length of time since the rape was 8.5 years (SD = 8.5 years), with a range of 3 months to 33 years. With regard to current medication, 30.7% of the sample was on psychotropic medication, and this rate did not differ across groups.
In an effort to represent typical clinical samples, we did not exclude women who had other traumas in addition to the index rape for which they sought treatment. In fact, 85.8% of the sample had experienced at least one other major crime victimization in addition to the index rape. Forty-eight percent had at least one additional rape; 13.6% reported serious physical assaults; 53.6% reported physical assaults with minor injuries; 21.9% reported being kidnapped as part of a crime; 17.8% had been robbery victims; 35.6% reported attempted rapes; 26.4% reported a criminal or vehicular homicide involving a friend or family member; and 14.3% reported being the victim of attempted murder. Forty-one percent of the sample had been sexually abused (genital contact) as children. The participants reported an average of 6.4 adult crime incidents (SD = 4.9) in addition to the index rape. The three groups did not differ with regard to their crime history.
Instruments
Interviews
Clinician-Administered PTSD Scale (CAPS)
The CAPS (Blake et al., 1990) is an interviewer-administered diagnostic instrument that measures PTSD. It has been found to have excellent psychometric properties (Blake et al., 1995). For each symptom, a clinician rates two separate dimensions, frequency and intensity of symptoms, on a scale ranging from 0–4. For a symptom to be considered clinically significant, it must meet threshold criteria on both dimensions (i.e., at least a 1 on frequency and a 2 on intensity). The CAPS also includes items that rate social and occupational functioning, global PTSD symptom severity, and the validity of the participant’s responses.
Structured Interview for DSM–IV—Patient Version (SCID)
The SCID (First, Gibbon, Spitzer, & Williams, 1996) is a diagnostic interview based on criteria from the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM–IV; American Psychiatric Association, 1994). Two modules of the SCID were used to assess mood disorders and substance abuse–dependence. Each SCID interview was audiotaped, and 25% were scored by a second rater to assess reliability.
Standardized trauma interview
The standardized trauma interview was adapted from the Resick et al. (1988) treatment study. This structured interview covered the following topics: demographic information, information about the rape, within-crime reactions, trauma history, social support, and treatment history. Only the demographics and trauma history sections were included in the present analyses. In addition to questions about adult crimes and other traumas, child sexual abuse was assessed with the Sexual Abuse Exposure Questionnaire (Part I; SAEQ; Rowan, Foy, Rodriguez, & Ryan, 1994). The SAEQ is a 10-item self-report measure designed to assess sexual acts experienced before the age of 16 years. Individual items exhibit moderate to high test–retest reliability (range: .73–.94), with an overall kappa coefficient of .88 (Ryan, Rodriguez, Rowan, & Foy, 1992).
Interrater reliability on structured interviews
Interrater reliability was established with new diagnostic interviewers by using training tapes and having more experienced faculty interviewers supervise and rate initial live interviews. After reliability had been established (100% diagnostic reliability and high item reliability), all diagnostic interviewers had audiotapes reviewed by senior project staff on a random, ongoing basis to ensure that there was no drift in diagnostic decisions. Weekly individual and group meetings were held throughout the project to discuss diagnostic conceptualizations and to reconcile conflicting diagnostic decisions. Diagnostic rules were codified within a coding manual.
A random sample of 66 tapes was selected for evaluation of interrater reliability for the CAPS. Categorical diagnostic analyses revealed that the kappa coefficient for the overall PTSD diagnosis was .74, with 92% interrater agreement. When the total PTSD score was evaluated with continuous data (sum of the continuous scores for each of the diagnostic criteria), the correlation between interviewer and rater scores was .97. Kappa values and percentages of agreement for each of the three clusters of PTSD symptoms were as follows: reexperiencing, κ = .79, 98% agreement; avoidance, κ = .69, 92% agreement; and arousal, κ = .85, 98% agreement.
The SCID was administered to assess current and lifetime diagnoses of depression, alcohol dependence, and substance dependence. Initial reliability was established through the same procedures described earlier. A sample of 45 tapes was selected for diagnostic reliability. Kappa values for diagnoses ranged from .80 to 1.00, except for current alcohol dependence (κ = .66).
Self-Report Scales
PTSD Symptom Scale (PSS)
This 17-item scale (Foa, Riggs, Dancu, & Rothbaum, 1993) represents all DSM criteria for PTSD, including reexperiencing, avoidance and numbing, and high arousal. However, we used only the total frequency score. Foa et al. (1993) found the scale to have satisfactory internal consistency, high test–retest reliability, and good concurrent and convergent validity with rape victims. In the current study, the alpha coefficient was .84.
Beck Depression Inventory (BDI)
The BDI (Beck, Ward, Mendelsohn, Mock, & Erbaugh, 1961) is a 21-item self-report questionnaire widely used in research on depression (Beck, Steer, & Garbin, 1988). It has also been used to assess depression in rape victims (Atkeson, Calhoun, Resick, & Ellis, 1982; Foa et al., 1991; Resick & Schnicke, 1992). Beck et al. reported a split-half reliability of .93. In this study, the alpha coefficient was .92.
Trauma-Related Guilt Inventory (TRGI)
The TRGI (Kubany et al., 1996) is a 32-item Likert inventory with three scales and three subscales. The three scales are distress (6 items), global guilt (4 items), and guilt cognitions (22 items). The three subscales—hindsight bias (7 items), wrongdoing (5 items), and lack of justification (4 items)—compose the guilt cognitions scale. Test–retest correlations range from .73 to .86. The alpha coefficients for the scales are .73 to .91. Construct, criterion-related, and discriminant validities were established with samples of Vietnam combat veterans and battered women. In the current study, we included global guilt and the three subscales of the guilt cognitions scale. The alpha coefficients for this sample were as follows: global guilt, .92; hindsight bias, .92; lack of justification, .76; and wrongdoing, .73.
Expectancy of therapeutic outcome
This questionnaire (Foa et al., 1991) measured the perceived credibility of each active treatment. Four questions were asked at the first session, after the therapy had been explained: (a) How logical does this type of treatment seem to you? (b) How confident are you that this treatment will be successful in reducing your assault-related symptoms? (c) How confident are you that this treatment will be successful in reducing other personal problems? and (d) How confident would you be in recommending this treatment to a friend with similar problems? These questions were rated on a 9-point scale ranging from not at all (1) to extremely (9). At posttreatment, the questions were asked again. However, whereas the first and last questions stayed the same, the second and third questions were changed to “How successful was this treatment in reducing your assault-related symptoms?” and “How successful was this treatment in reducing other personal problems?”
Therapists and training
Therapists were eight women with doctorates in clinical or counseling psychology and a background in cognitive–behavioral therapy. Assignments were balanced so that each therapist handled an approximately equal number of therapy cases in each condition. After the therapists had read the manuals, there was a 2-day workshop for each therapy. They were trained in CPT by Patricia A. Resick and in PE by Edna Foa. The therapists watched training tapes of the therapy being conducted and then conducted therapy on two clients in each of the conditions as pilot participants. Throughout the study, all of the sessions were videotaped, and therapy was closely supervised by the principal investigator, with weekly peer-supervision sessions to ensure competence and adherence to the protocols.
Treatment adherence and competence
Independent raters who were not otherwise involved in the project conducted assessments of treatment adherence and therapist competence. All therapy sessions were videotaped and were available at random for rating. Ratings were made with rating forms developed for this project that included sections on unique and essential elements specific to each session, essential but not unique elements, acceptable but not necessary elements, and proscribed elements for each therapy (Nishith & Foa, 1994; Nishith & Resick, 1994). The number of items potentially rated for each session and across the two therapies varied depending on the goals and specifics of the protocol for each therapy. In the PE protocol, there were 8–15 unique and essential elements for each session (85 items in total). In the CPT protocol, there were 5–8 unique and essential items for each session (69 items in total). For adherence, the element was checked if it occurred; for competence, a rating was made on a 7-point scale (poor to excellent, with satisfactory at the midpoint). The two protocols had only 1 item in common, an overall rating of the therapist’s skill across the sessions for a given client; ratings ranged from 1 (poor) to 7 (excellent), with satisfactory at the midpoint.
The tapes were viewed by experts in each specific therapy who were not a part of the project and who were not affiliated with the university where the study was being conducted. Adherence and competence ratings were made for 23 CPT and 21 PE clients and for each, three randomly chosen sessions were rated.1 In other words, a rater viewed three randomly selected sessions for each of the clients who were chosen. All of the therapists were rated in proportion to the number of clients they treated. One of every three rated sets of tapes was sent to a second rater for a reliability check.
Regarding adherence, all unique and essential elements were included in all sessions, and there were no violations of the protocols in which proscribed elements were introduced in therapy. The competence of the therapists was rated on all of the unique and essential components for the session in question, and an overall therapist skill rating was made for the three sessions rated for each client. In the case of CPT, 99% of the therapy tapes were rated as satisfactory or better on unique and specific elements, and 100% were rated as satisfactory or better in terms of overall therapist skill. More specifically, of the 404 unique and essential ratings made, 1% were satisfactory, and 98% were good to excellent. Of the overall ratings for the 23 clients, 4% were satisfactory, and 96% were good to excellent. Reliability was conducted on 76 unique and essential items and 11 cases overall as to whether the therapy was or was not satisfactory. The two raters exhibited 100% agreement on the unique and essential items as well as on overall ratings.
The PE rater judged 92% of the tapes to be satisfactory or better on unique and specific elements and 95% to be satisfactory or better with regard to overall therapist skills. Of the 535 elements rated, 28% were satisfactory, and 64% were good to excellent. Of the 21 overall ratings, 14% were judged satisfactory and 81% good to excellent. The two raters evaluated 86 unique and essential items and 12 cases overall. The PE raters agreed on 84% of the unique and essential items and disagreed on 16% of items as to whether competence was satisfactory or not. Their overall ratings of therapist skill agreed in 92% of cases and disagreed in 8% of cases.
Design and Treatment Overview
The design of the project involved random assignment of participants to CPT, PE, or MA. The two active treatments were completed within 6 weeks, the length of the MA condition. At the end of the second assessment, the MA participants were randomly assigned to either PE or CPT. CPT and PE were conducted twice weekly for a total of 13 hr of treatment. After the initial 60-min session of PE, sessions were 90 min long to enable adequate exposure levels. CPT, as originally developed, consisted of 12 hr of therapy. As a means of equating therapist contact time with PE, 1 hr was added to the CPT protocol. Thirty minutes were added to each of the two CPT writing exposure sessions (Sessions 4 and 5). CPT followed the format described by Resick and Schnicke (1993) with only a few minor modifications. The PE manual was similar to the protocol later published by Foa and Rothbaum (1997).
Although therapist contact time was equated, it was not possible to equate the homework assignments without violating the protocols. PE includes two major homework assignments each day that require 1.5–2 hr to complete. CPT also involves daily homework; however, excluding the two writing assignment sessions, this homework did not require extensive time allocations. An analysis of homework completed by participants showed that there were significant differences between the two treatments. In the ITT sample, the CPT group averaged 22.6 hr of homework (SD = 6.5), whereas the PE group averaged 44.8 hr (SD = 33.5), t(72.5) = —4.3, p < .001. In the completer sample, the CPT group averaged 26.6 hr of homework (SD = 15.9), and the PE group averaged 54.2 hr (SD = 31.0), t(57.8) = —5.0, p < .001. Although it was not possible to equate homework time assigned, the greater amount would favor PE (the comparison therapy in this study).
The study was originally designed to include only a 3-month follow-up. Women who were still positive for PTSD at the 3-month follow-up were offered the alternative treatment. Once the study started, a 9-month follow-up was added. However, the women who opted for the alternative treatment (4 in the original PE group and 1 in CPT) could not be included in the 9-month follow-up. Therefore, a caveat in interpretation is proffered for the treatment completer data at the 9-month follow-up, because 4 women in PE and 1 in CPT with higher PTSD scores were eliminated. In the ITT sample, these participants’ scores were carried forward from the 3-month assessment.
CPT
CPT followed the manual written by Resick and Schnicke (1993). Session 1 begins with education about PTSD, an overview of treatment, and an assignment to write an impact statement about the personal meaning of the event. After reading and discussing the meaning of the rape in Session 2, clients are introduced to the identification of and relationship among events, thoughts, and emotions. At the end of Session 3, clients are given the assignment of writing a detailed account of the trauma, including sensory details, thoughts, and emotions. They are encouraged to experience their emotions as they write their account and read it back to themselves. This account is read to the therapist in Session 4, and cognitive therapy begins with Socratic questions regarding self-blame and other distortions regarding the event. The account is written and processed a second time in Session 5. Writing about a second trauma may occur after Session 5, but the focus of the therapy shifts to teaching clients to challenge and change their beliefs about the meaning of the event and the implications of the trauma for their lives.
Clients are first taught to challenge a single thought by asking themselves a series of questions. They are then taught to identify problematic patterns of cognitions that have come to represent a style of responding. From that point, beginning with Session 7, clients use worksheets that incorporate the earlier ones and are asked to develop and practice alternative, more balanced self-statements. From Sessions 7–12, clients are asked to focus on one theme each week (safety, trust, power–control, esteem, or intimacy) and correct any overgeneralized beliefs related to that theme. At the 11th session, clients are also asked to rewrite their impact statements to reflect their current beliefs, and these revised statements are then used in the final session to evaluate gains made in treatment and areas in which clients wish to continue working.
PE
PE (Foa, Hearst, Dancu, Hembree, & Jaycox, 1994) includes four components, in the following order: education–rationale, breathing retraining, behavioral exposures, and imaginal exposures. During the first session, clients are educated about the symptoms of PTSD, and the therapist provides a rationale for in vivo and imaginal exposure in the context of avoidance reduction and habituation of conditioned negative emotional responses. Clients are also introduced to breathing retraining. In Session 2, rationale and education continue, subjective units of distress ratings are introduced, the therapist and client generate an in vivo exposure hierarchy, and the first in vivo exposure assignment is given. Sessions 3 to 9 begin by reviewing homework assignments, conducting imaginal exposure for 45–60 min of the 90-min session (depending on the length of the incident and the number of repetitions possible), and processing the exposure experience with nondirective statements (e.g., education about trauma reactions, paraphrasing, reiterating the treatment rationale, and normalizing reactions). Clients are instructed to listen to the tape of the imaginal exposure sessions each day and to engage in behavioral exposures with increasing difficulty for at least 45 min per day.
MA
The MA condition served as a waiting-list control. Women who were assigned to this condition were told that therapy would be provided in 6 weeks and that an interviewer would call them every 2 weeks to ensure that they did not need emergency services. They were also encouraged to call if they wished to talk to a therapist who could provide client-centered telephone counseling. If any participant were to have called more than once in the first 2 weeks regarding her reactions, called more than four times over the 6-week period, expressed increasing suicidal ideation or intent, or otherwise indicated that she did not feel she could wait for treatment, she would have been terminated from participation in the study and treated immediately by one of the project staff or referred for hospitalization. However, this never occurred. There were some dropouts from the MA condition, but they did not appear to be from emergent circumstances.
Results
Expectancy of Therapeutic Outcome
Because the expectancies were evaluated during the first and last therapy sessions, pretreatment data were not available for participants who never attended a session. These data were treated in two ways. First, the four expectancy questions at pretreatment were subjected to a multivariate analysis of variance (MANOVA) to determine whether the women who dropped out had different expectations from those who completed treatment. The MANOVA was nonsignificant. Next, we conducted a repeated measures MANOVA (pretreatment–posttreatment) with type of therapy (CPT or PE) as the independent variable. There was no interaction between groups and sessions. The group effect was nonsignificant; there were no differences between the two therapies on the therapeutic expectation questions at either pretreatment or posttreatment. The session effect was significant, F(4, 76) = 12.68, p < .001, and paired-sample t tests indicated that there were significant differences on each of the four questions: Question 1, t(80) = −3.93, p < .001; Question 2, t(80) = −5.29, p < .001; Question 3, t(79) = −2.88, p < .005; and Question 4, t(80) = −5.65, p < .001. Participants’ ratings increased from pretreatment to posttreatment on each of the questions for both therapies.
Analysis Plan
The results were analyzed in three different ways for comparison purposes. Unfortunately, this study was designed and conducted before ITT analysis became standard. Therefore, we did not continue to assess women who dropped out of treatment, and we administered only one scale, the PSS, during treatment. The PSS data were analyzed separately from the measures for which we had only pretreatment, posttreatment, and follow-up data. With only pretreatment data available for the treatment dropouts as well as those who never started, it was not possible for the main analyses involving the CAPS or BDI to determine whether partial therapy was at all beneficial for participants.
Initially, all of the participants who were accepted and randomized into the trial were analyzed with their last observations carried forward (LOCF). These ITT data allowed a more complete picture of the results regardless of whether the women completed the treatment or even began treatment. Another method of handling nonrandom missing data due to dropout is to use mixed-effects linear regression analysis or random regression. Random regression has several advantages over LOCF (Heyting, Tolboom, & Essers, 1992; Mazumdar, Liu, Houck, & Reynolds, 1999). Supplementing the use of LOCF data with random regression models as a converging test of our hypotheses allowed us added protection against misleading findings (Gibbons et al., 1993; Hedeker & Gibbons, 1996).
Finally, those women who completed treatment were analyzed separately. Although this might be viewed as a “censored” data set from a statistical standpoint, these results are very important from a clinical standpoint. The question addressed here is how effective these treatments are if someone completes the whole course of treatment. This might be particularly important for a therapy such as CPT in which the therapist is teaching new and different skills at each session and no two sessions are exactly alike. In the case of completer analyses, two different sets of analyses were conducted. First, a repeated measures pretreatment to posttreatment MANOVA was conducted for the three groups (CPT, PE, and MA). Second, a two-group (CPT and PE) analysis was conducted across the four assessment periods, including the 3- and 9-month follow-ups. Because there were two MANOVAs for the completer data set, Bonferroni corrections were calculated, and the p value was set at .025.
ITT Analyses With LOCF
ITT analyses with LOCF were conducted on 171 participants, including the 13 women who never attended a session but had been accepted into the study. A 3 (group: CPT, PE, or MA) × 4 (session: pretreatment, posttreatment, 3-month follow-up, or 9-month follow-up) repeated measures MANOVA using LOCF with CAPS and BDI scores as dependent variables produced a significant interaction, F(12, 320) = 4.1, Pillai’s trace = .27, p < .000; a significant session effect, F(6, 159) = 17.9, Pillai’s trace = .40, p < .001; and a significant group effect, F(4, 328) = 4.6, Pillai’s trace = .10, p < .001. Follow-up one-way analyses of variance (ANOVAs) indicated no pretreatment differences among any of the three groups on either measure. At the posttreatment assessment, there were significant differences between the groups on the CAPS, F(2, 168) = 15.5, p < .0001, and BDI, F(2, 167) = 12.1, p < .0001. A post hoc Tukey’s honestly significant difference (HSD) test indicated that the MA group had significantly higher symptom scores than either the CPT or PE group. At the 3-month and 9-month follow-ups, the results were the same: 3-month CAPS, F(2, 168) = 12.5, p < .0001; 3-month BDI, F(2, 167) = 10.1, p < .0001; 9-month CAPS, F(2, 168) = 12.1, p < .0001; and 9-month BDI, F(2, 167) = 8.4, p < .0001. In each case, the MA group had significantly higher scores than the treatment groups, which did not differ from each other. Means and standard deviations for each group at each session are listed in Table 1.
Table 1.
CPT, PE, and MA Mean Scores Over Time: Intent-to-Treat Sample
| Pretreatment |
Posttreatment |
3 months |
9 months |
||||||
|---|---|---|---|---|---|---|---|---|---|
| Measure and group | n | M | SD | M | SD | M | SD | M | SD |
| CAPS | |||||||||
| CPT | 62 | 74.76 | 18.77 | 39.08 | 31.12 | 42.21 | 30.13 | 42.87 | 31.06 |
| PE | 62 | 76.60 | 19.72 | 44.89 | 33.52 | 49.16 | 32.86 | 46.98 | 33.68 |
| MA | 47 | 69.85 | 19.57 | 69.26 | 18.55 | 69.26 | 18.55 | 69.26 | 18.55 |
| BDI | |||||||||
| CPT | 61 | 23.70 | 10.39 | 12.73 | 11.17 | 13.22 | 11.64 | 14.17 | 11.85 |
| PE | 61 | 24.03 | 8.88 | 16.00 | 11.06 | 16.49 | 11.62 | 16.41 | 11.37 |
| MA | 47 | 23.33 | 8.07 | 22.62 | 8.59 | 22.62 | 8.59 | 22.62 | 8.59 |
| PSS | |||||||||
| CPT | 62 | 29.55 | 8.62 | 13.66 | 11.05 | 14.67 | 11.79 | 15.13 | 12.03 |
| PE | 62 | 30.09 | 9.18 | 17.99 | 13.17 | 18.05 | 13.78 | 18.40 | 13.98 |
| MA | 47 | 28.70 | 7.33 | 27.77 | 8.12 | 27.77 | 8.12 | 27.77 | 8.12 |
| Global guilt | |||||||||
| CPT | 62 | 2.34 | 1.13 | 1.37 | 1.08 | 1.28 | 1.09 | ||
| PE | 61 | 2.53 | 1.11 | 1.73 | 1.20 | 1.69 | 1.25 | ||
| MA | 15/39a | 2.60 | 1.03 | 2.33 | 1.06 | 2.33 | 1.06 | ||
| Hindsight bias | |||||||||
| CPT | 62 | 1.88 | 1.08 | 0.99 | 1.14 | 0.93 | 1.05 | ||
| PE | 59 | 2.18 | 1.18 | 1.51 | 1.22 | 1.54 | 1.20 | ||
| MA | 15/39a | 1.97 | 1.05 | 1.98 | 1.08 | 1.98 | 1.08 | ||
| Lack of justification | |||||||||
| CPT | 62 | 2.55 | 1.05 | 1.71 | 1.20 | 1.79 | 1.16 | ||
| PE | 59 | 2.73 | 0.98 | 2.35 | 1.04 | 2.34 | 1.06 | ||
| MA | 14/36a | 2.80 | 0.57 | 2.69 | 0.98 | 2.69 | 0.98 | ||
| Wrongdoing | |||||||||
| CPT | 61 | 1.62 | 1.03 | 1.13 | 1.08 | 1.02 | 0.98 | ||
| PE | 58 | 2.00 | 0.89 | 1.54 | 1.03 | 1.44 | 1.06 | ||
| MA | 14/36a | 2.54 | 0.88 | 1.90 | 1.06 | 1.90 | 1.06 | ||
Note. CPT = cognitive-processing therapy; PE = prolonged exposure; MA = minimal attention; CAPS = Clinician-Administered PTSD Scale; BDI = Beck Depression Inventory; PSS = PTSD Symptom Scale; PTSD = posttraumatic stress disorder.
Pre-MA/post-MA assessments had different sample sizes as indicated.
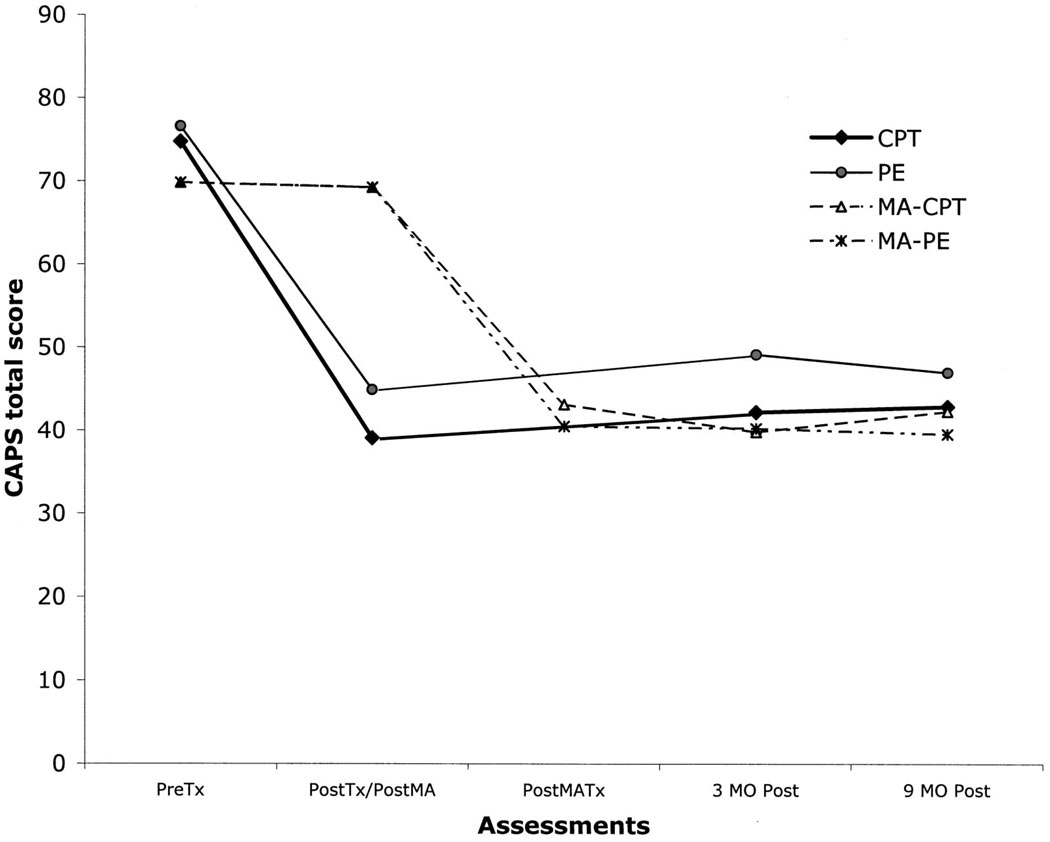
Simple repeated measures MANOVAs for each group across the four assessment sessions indicated that both the CPT, F(6, 55) = 12.6, Pillai’s trace = .58, p < .0001, and PE, F(6, 55) = 10.2, Pillai’s trace = .53, p < .001, groups changed significantly over time. The MA group did not change across the assessment periods. For the CPT and PE groups, the decreases in scores occurred from pretreatment to posttreatment. There were no significant changes from posttreatment to the 3-month or 9-month follow-up. CAPS scores for the ITT sample are depicted in Figure 1.
Figure 1.
Total CAPS scores in the CPT, PE, MA-CPT, and MA-PE conditions: intent-to-treat sample. CAPS = Clinician-Administered PTSD Scale; CPT = cognitive-processing therapy; PE = prolonged exposure; MA = minimal attention; Tx = treatment; Post = posttreatment; MO = month; PTSD = posttraumatic stress disorder.
The effect sizes for the two active treatments at posttreatment (relative to the MA condition) with the LOCF data set are presented in Table 2. Hedges g effect sizes (Hedges, 1982) were computed so that the results would be directly comparable to the effect sizes calculated in the International Society for Traumatic Stress Studies (ISTSS) treatment guidelines for PTSD (Foa, Keane, & Friedman, 2000). Basic Hedges’ g values are part of the Cohen d effect- size family. Effect sizes were calculated as the mean difference between the experimental (CPT and PE) and comparison (MA) groups divided by the pooled standard deviation within each of the samples. When the CPT and PE groups were compared directly, the experimental group was CPT, and PE was used as the comparison group. Effect sizes were then converted to unbiased Hedges’ g values to correct for variations due to small sample sizes (Hedges, 1982; Rosenthal, 1991). To assist with interpretation, Cohen (1988) proposed a set of qualitative descriptors to accompany individual effect sizes. Demarcations between descriptors are meant to be approximate rather than absolute in nature. Small effect sizes are operationally defined as 0.2; medium effect sizes, as 0.5; and large effect sizes, as 0.8 (Cohen, 1988). The CPT and PE groups showed large effects for symptoms (relative to the MA group) in the ITT sample. When we compared the CPT and PE groups directly (rather than the MA condition), CPT resulted in small but positive effect-size differences for PTSD, depression, and guilt measures at posttreatment, 3 months, and 9 months, indicating modestly greater symptomatic improvement relative to the participants in the PE condition.
Table 2.
Unbiased Hedges g Effect Sizes: Cognitive-Processing Therapy (CPT), Prolonged Exposure (PE), and Minimal Attention (MA)
| CPT vs. PEc |
|||||
|---|---|---|---|---|---|
| Measure | CPT vs. MAa (posttreatment) |
PE vs. MAb (posttreatment) |
Posttreatment | 3 months | 9 months |
| Intent-to-treat sample | |||||
| CAPS | 0.97 | 0.74 | 0.14 | 0.18 | 0.10 |
| PSS | 1.22 | 0.74 | 0.29 | 0.21 | 0.20 |
| BDI | 0.84 | 0.57 | 0.24 | 0.22 | 0.16 |
| Global guiltd | 0.79 | 0.47 | 0.25 | 0.28 | |
| Hindsight bias | 0.79 | 0.37 | 0.36 | 0.44 | |
| Lack of justification | 0.78 | 0.31 | 0.46 | 0.40 | |
| Wrongdoing | 0.64 | 0.31 | 0.32 | 0.34 | |
| Completer sample | |||||
| CAPS | 2.78 | 2.05 | 0.24 | 0.33 | –0.30 |
| PSS | 2.70 | 1.76 | 0.43 | 0.31 | 0.10 |
| BDI | 2.09 | 1.18 | 0.51 | 0.59 | 0.06 |
| Global guilt | 1.90 | 1.32 | 0.47 | 0.56 | |
| Hindsight bias | 2.02 | 1.04 | 1.00 | 1.03 | |
| Lack of justification | 1.79 | 0.73 | 1.06 | 0.69 | |
| Wrongdoing | 1.30 | 0.77 | 0.59 | 0.48 | |
Note. CAPS = Clinician-Administered PTSD Scale; PSS = PTSD Symptom Scale; BDI = Beck Depression Inventory; PTSD = posttraumatic stress disorder.
Positive effect sizes indicate that participants in the CPT condition evidenced greater symptomatic improvement than participants in the MA condition.
Positive effect sizes indicate that participants in the PE condition evidenced greater symptomatic improvement than participants in the MA condition.
Positive effect sizes indicate that participants in the CPT condition evidenced greater symptomatic improvement than participants in the PE condition. Negative effect sizes indicate that participants in the PE condition evidenced greater symptomatic improvement than participants in the CPT condition.
Measures of guilt were not assessed at 3 months posttreatment.
Random Effects Regression Analyses
Pretreatment–Posttreatment Effects: CAPS and BDI
We tested the accuracy of the major analyses conducted with LOCF data by running analyses testing the same hypotheses using the random regression method (or mixed-effects regression). Given that MA participants received pretreatment and posttreatment MA assessments and then were moved into one of the two active treatments, only two time points were assessed in these three-group random regression analyses. Random regression models handle nonrandom missing data due to dropout by estimating time trend lines for each individual based on available data for that individual as well as information about the parameters of the entire sample. The MIXREG (Hedeker & Gibbons, 1996) program for random effects regression was used to compare the three treatment groups on the CAPS and then on the BDI. It was necessary to run two separate analyses for each dependent variable (CAPS and BDI) to compare changes over time across three groups using MIXREG (R. Gibbons, personal communication, April 2000). As a means of guarding against increased experimentwise error rates, results were only considered significant at the .0125 level.
The results of these analyses were consistent with the main findings of the LOCF analyses. The CPT group showed significantly more change in CAPS scores than the MA group (estimated improvement difference: −53.87, SE = 4.51, z = −11.96, p < .0001). The PE group also showed significantly greater change in CAPS score over time than the MA group (estimated improvement difference: −50.51, SE = 4.57, z = −11.06, p < .0001), but the CPT and PE groups were not significantly different from each other.
A second set of random effects regression analyses examined differences in BDI score change over time among the CPT, PE, and MA groups. As in the CAPS analyses, there was no indication of significant serial error correlations. CPT participants showed significantly greater changes in BDI scores over time than MA participants (estimated improvement difference: −15.93, SE = 2.09, z = −7.61, p < .0001). PE participants showed similarly significant decreases in BDI scores relative to the MA group (estimated improvement difference: −11.72, SE = 2.11, z = −5.55, p < .0001). There was no significant difference in BDI score change over time between the PE and CPT groups (estimated improvement difference: 4.21, SE = 2.03, z = 2.07, p < .04).
Random Effects Regression on PSS Change
Participants were given the PSS at the initial assessment, at the beginning of every other session, and at the posttherapy assessments. The two therapies were equal in terms of overall number of hours but differed in number and length of sessions. Mixed-effects linear regression analysis (MIXREG) was used to assess group differences in PSS score change over the course of therapy. The PSS was given to the CPT and PE groups on a regular basis, but the MA participants were not attending sessions. Therefore, only the CPT and PE groups were included in this analysis. A MIXREG run not allowing for serial correlation of errors showed a trend toward a significant difference between the CPT and PE groups on PSS score over time. The trend suggested a larger decrease in PSS scores over the course of CPT than over the course of PE. However, it was found that there was substantial serial correlation of errors (r = .68, p < .0001), best described by a first-order nonstationary autoregressive error pattern. In this pattern, any given PSS score is predicted to a much greater degree by the score at the previous time point than by the score at the time point before that. A MIXREG analysis accounting for serially correlated errors showed no trend toward significant treatment group differences on the PSS. There were no significant differences in PSS scores between the two conditions at baseline or over time in therapy.
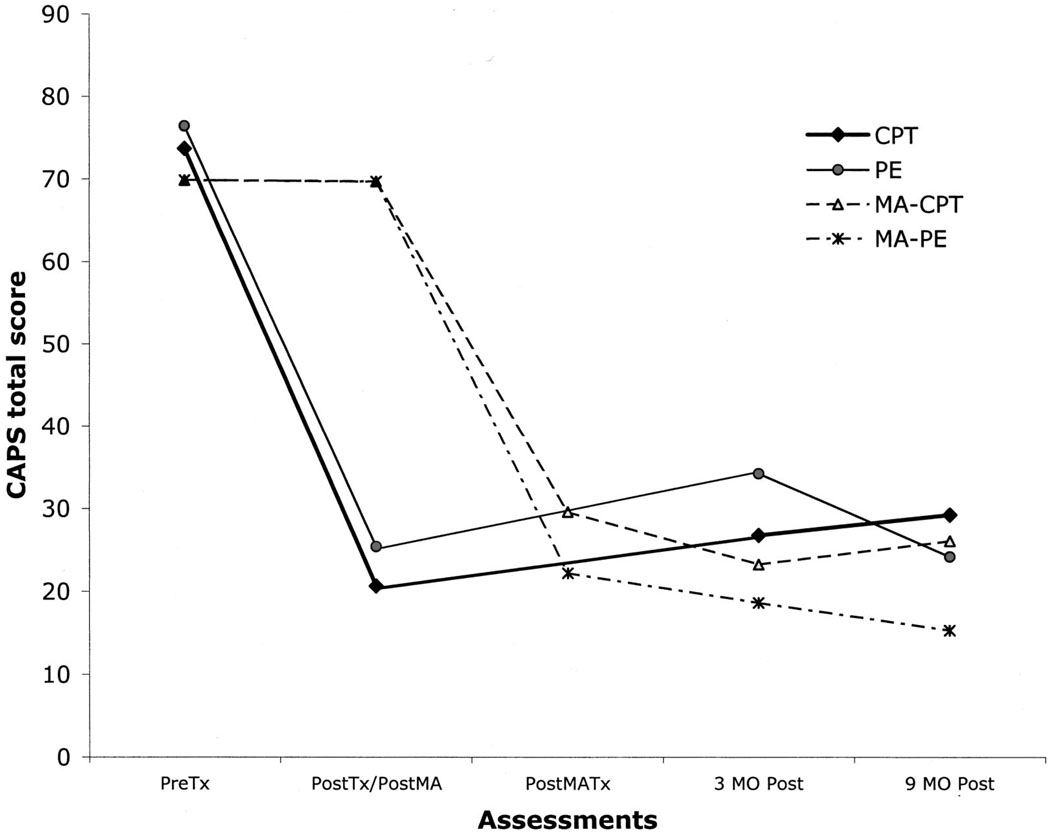
Analyses of Treatment Completers
Means and standard deviations for the completer sample are shown in Table 3, and CAPS scores are plotted in Figure 2. In the first analysis, the three groups were compared in a repeated measures MANOVA from pretreatment to posttreatment with CAPS total score and BDI score as dependent variables. The MANOVA resulted in a significant interaction, F(4, 214) = 23.7, Pillai’s trace = .61, p < .0001, and significant treatment group, F(4, 214) = 9.4, Pillai’s trace = .30, p < .001, and session, F(2, 106) = 141.1, Pillai’s trace = .73, p < .0001, effects. Univariate repeated measures ANOVAs indicated that both the CAPS, F(2, 118) = 79.2, p < .0001, and the BDI, F(2, 107) = 26.0, p < .0001, resulted in significant interactions. Follow-up one-way ANOVAs indicated no pretreatment session differences but significant posttreatment effects on the CAPS, F(2, 118) = 76.1, p < .0001, and BDI, F(2, 110) = 32.8, p < .0001. Post hoc Tukey’s HSD tests indicated that the group differences on both the CAPS and BDI were between the MA group and the two treatment groups. A second analysis was conducted between the two treatment groups over the four assessment sessions. This repeated measures MANOVA resulted in significant session effects, F(6, 38) = 55.6, Pillai’s trace = .90, p < .0001, but no treatment type effect or interaction. On the CAPS, both groups exhibited a strong decrease in scores from pretreatment to posttreatment, F(1, 80) = 407.4, p < .0001; some increase from posttreatment to the 3-month follow-up, F(1, 73) = 8.5, p < .005; and no change from 3 months to 9 months. On the BDI, the groups improved significantly from pretreatment to posttreatment, F(1, 75) = 142.5, p < .0001. From posttreatment to 3 months, there were no significant changes, nor were there significant changes from 3 months to 9 months posttreatment.
Table 3.
Mean Scores for Treatment Completers: Cognitive-Processing Therapy (CPT), Prolonged Exposure (PE), and Minimal Attention (MA) Groups
| Pretreatment |
Posttreatment |
3 months |
9 months |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Measure and group | n | M | SD | n | M | SD | n | M | SD | n | M | SD |
| CAPS | ||||||||||||
| CPT | 41 | 73.71 | 18.47 | 41 | 20.66 | 15.60 | 37 | 26.78 | 20.03 | 26 | 29.27 | 23.56 |
| PE | 40 | 76.43 | 19.11 | 40 | 25.40 | 23.54 | 37 | 34.27 | 26.89 | 26 | 24.12 | 18.78 |
| MA | 40 | 69.88 | 19.91 | 40 | 69.73 | 19.19 | ||||||
| BDI | ||||||||||||
| CPT | 40 | 23.43 | 10.30 | 39 | 6.82 | 5.68 | 37 | 7.86 | 7.77 | 23 | 9.57 | 8.75 |
| PE | 40 | 23.90 | 9.15 | 38 | 11.42 | 9.90 | 34 | 13.23 | 11.36 | 24 | 9.21 | 6.32 |
| MA | 38 | 23.50 | 8.31 | 37 | 22.30 | 9.09 | ||||||
| PSS | ||||||||||||
| CPT | 41 | 29.22 | 8.72 | 40 | 8.30 | 6.00 | 36 | 9.75 | 9.04 | 24 | 9.53 | 9.28 |
| PE | 40 | 29.93 | 8.84 | 40 | 11.80 | 9.87 | 34 | 12.72 | 10.98 | 26 | 10.23 | 9.12 |
| MA | 39 | 28.94 | 7.47 | 39 | 27.95 | 8.41 | ||||||
| Global guilt | ||||||||||||
| CPT | 41 | 2.37 | 1.16 | 36 | 0.85 | 0.68 | 24 | 0.66 | 0.63 | |||
| PE | 40 | 2.52 | 1.11 | 37 | 1.20 | 0.84 | 26 | 1.06 | 0.89 | |||
| MA | 13 | 2.69 | 0.72 | 37 | 2.35 | 0.97 | ||||||
| Hindsight bias | ||||||||||||
| CPT | 40 | 1.88 | 1.10 | 35 | 0.34 | 0.57 | 23 | 0.39 | 0.43 | |||
| PE | 38 | 2.12 | 1.18 | 35 | 1.02 | 0.85 | 25 | 0.90 | 0.78 | |||
| MA | 13 | 2.03 | 0.99 | 36 | 1.95 | 1.04 | ||||||
| Lack of justification | ||||||||||||
| CPT | 39 | 2.56 | 1.07 | 35 | 1.08 | 0.91 | 25 | 1.40 | 1.05 | |||
| PE | 39 | 2.61 | 1.04 | 34 | 2.01 | 0.98 | 25 | 1.98 | 1.07 | |||
| MA | 12 | 2.79 | 0.62 | 34 | 2.68 | 1.01 | ||||||
| Wrongdoing | ||||||||||||
| CPT | 40 | 1.55 | 1.04 | 35 | 0.70 | 0.84 | 25 | 0.56 | 0.68 | |||
| PE | 38 | 1.89 | 0.82 | 35 | 1.17 | 0.84 | 25 | 0.82 | 0.67 | |||
| MA | 12 | 2.55 | 0.92 | 34 | 1.86 | 1.07 | ||||||
Note. CAPS = Clinician-Administered PTSD Scale; BDI = Beck Depression Inventory; PSS = PTSD Symptom Scale; PTSD = posttraumatic stress disorder.
Figure 2.
Total CAPS scores in the CPT, PE, MA-CPT, and MA-PE conditions: treatment completers. CAPS = Clinician-Administered PTSD Scale; CPT = cognitive-processing therapy; PE = prolonged exposure; MA = minimal attention; Tx = treatment; Post = posttreatment; MO = month; PTSD = posttraumatic stress disorder.
The effect sizes for the completer sample are shown in Table 2. Both therapies had large effects relative to MA at posttreatment on PTSD, depression, and guilt scores. Effect sizes were also calculated for CPT relative to PE at posttreatment and the 3- and 9-month follow-ups. At posttreatment and the 3-month follow-up, there were small CAPS effect-size differences for CPT as compared with PE. For the BDI, there were moderate effect-size differences between the two active treatments favoring CPT at posttreatment and the 3-month follow-up. Contrary to the ITT analyses, at the 9-month follow-up, PE showed a small effect-size difference relative to CPT for the CAPS; there were no differences for the PSS and BDI.
Diagnosis and Treatment Outcome
Finally, diagnoses were examined in the three groups at posttreatment using the symptom but not time criteria. First, in the ITT sample, only 1 MA client of 45 (2.2%) was PTSD negative at the post-MA assessment. In comparison with the MA group, 33 of the 62 women randomized into CPT (53%) and 33 of the 62 PE clients (53%) were negative for PTSD at posttreatment, χ2(2) = 35.9 < .0001. In comparisons of those who received CPT versus PE over time, there were no significant differences in diagnosis at any of the time points. At the 3-month follow-up, 42% of CPT and 53% of PE clients still met criteria for PTSD. At the 9-month follow-up, 45% of CPT and 50% of PE clients were PTSD positive.
There were also no significant differences between the two active treatments for the SCID (major depression) in the ITT sample. The SCID module for major depressive disorder (MDD) was not readministered until the 3-month follow-up because at posttreatment the assessment would have had to involve the last third of the treatment (2 weeks). At pretreatment, 43.5% of the CPT and 47.5% of the PE clients met criteria for MDD. At the 3-month follow-up, 30.6% of CPT and 29.5% of PE clients still met criteria for MDD. At the 9-month follow-up, 22.6% of the CPT clients and 29.5% of the PE clients continued to meet criteria for MDD.
Completing the treatments as designed, of course, yielded a very different picture. Of those who completed treatment, only 19.5% of CPT and 17.5% of PE clients still met criteria for PTSD. At the 3-month follow-up, 16.2% of CPT and 29.7% of PE clients were PTSD positive. At the 9-month follow-up, 19.2% of CPT and 15.4% of PE clients were still PTSD positive. There were no significant differences in PTSD diagnostic status between the CPT and PE groups at any time point.
With regard to depression comorbidity among treatment completers, 46.3% of CPT and 52.6% of PE participants also met criteria for current MDD at pretreatment. At the 3-month follow-up, 17.6% of CPT and 22.2% of PE participants still met criteria for MDD. At the 9-month follow-up, 3.8% of CPT and 15.4% of PE clients continued to meet criteria for MDD. All of the chisquare analyses were nonsignificant.
End-State Functioning
To determine the percentage of participants who achieved good end-state functioning, we computed an index that combined scores from the PSS and BDI using the same cutoffs as Foa et al. (1999). Good end-state functioning was defined as at or below a cutoff of 20 on the PSS and at or below 10 on the BDI. In the ITT sample at posttreatment, 53% of the CPT and 37% of the PE participants had good end-state functioning, and there was a trend for CPT participants to have better functioning than PE participants, χ2(1) = 3.3, p < .08. At 3 months posttreatment, there was also a trend, χ2(1) = 2.7, p < .11, with 50% of the CPT and 36% of the PE participants reporting good end-state functioning. At 9 months posttreatment, there was no difference between groups, with 45% of the CPT and 40% of the PE participants reporting good end-state functioning.
In the completer sample, 76% of the CPT and 58% of the PE participants reported good end-state functioning, resulting in a trend, χ2(1) = 2.9, p < .09. At the 3-month follow-up, 72% of CPT and 50% of PE participants reported good end-state functioning, again a trend favoring CPT, χ2(1) = 3.6, p < .06. At 9 months, there was no significant difference between the two treatments, with 64% of CPT and 68% of PE participants reporting good end-state functioning.
Supplementary Analyses
Length of Time Since Index Rape
Because the length of time since the index rape varied from 3 months to 33 years, it is possible that treatment outcome was affected by chronicity. The distribution of years since rape was somewhat skewed toward more recent index traumas (within the previous 2 years). Therefore, instead of using years since index rape as a continuous variable, we divided the ITT and completer samples into three relatively equal groups based on percentile: 3 months to 2.25 years (n = 56), 2.3 to 10 years (n = 54), and more than 10 years (n = 58). There was no significant difference in the distribution of the chronicity groups across the three therapy conditions. The data were analyzed by means of 3 × 3 (Treatment Group × Time Group) ANOVAs at posttreatment with pretreatment CAPS, BDI, and PSS scores as covariates. There were no interactions or main effects for length of time since index rape for either the ITT sample or the completer sample.
Effect of Treatment on Guilt
One of the aims of the study was also to examine the effect of treatment on cognitions. After the study was under way, a decision was made to administer some of the measures to the MA participants only at the second assessment session to reduce the size of the assessment battery. However, we did administer these measures at both time periods initially, so the MA sample size was sufficient to compare the MA condition with the other two treatments. Also, we administered a reduced battery at the 3-month follow-up once we decided to implement a 9-month follow-up. We did not administer the TRGI at the 3-month follow-up. Therefore, in the case of these analyses, treatments were compared at pretreatment, posttreatment, and the 9-month follow-up.
First, using the ITT data, we conducted a repeated measures MANOVA comparing the groups over the three assessments. There were four dependent variables: global guilt, hindsight bias– responsibility, lack of justification, and wrongdoing. The MANOVA resulted in significant group, F(8, 244) = 2.3, Pillai’s trace = .14, p < .02, and session, F(4,117) = 4.4, Pillai’s trace = .23, p < .001, effects. The interaction term was not significant. As with the symptom measures, there were no significant pretreatment differences between groups. However, at posttreatment, the groups were different on all four subscales: global guilt, F(3, 159) = 8.8, p < .0001; hindsight bias, F(2, 157) = 9.1, p < .0001; lack of justification, F(2, 154) = 10.6, p < .0001; and wrongdoing, F(2,153) = 6.3, p < .005. Post hoc Tukey’s HSD tests indicated that both the CPT and PE groups had significantly lower global guilt and wrongdoing scores than the MA group. However, the CPT group had significantly lower hindsight bias and lack of justification scores than either the PE group or the MA group, which did not differ from each other.
At the 9-month assessment, with MA posttreatment scores carried forward, there were also significant differences on all four measures: global guilt, F(2, 159) = 10.1, p < .0001; hindsight bias, F(2, 157) = 11.3, p < .0001; lack of justification, F(2,154) = 8.8, p < .001; and wrongdoing, F(2, 153) = 8.5, p < .001. The Tukey’s HSD test revealed the same pattern as the posttreatment assessment, with the CPT group having lower hindsight bias and lack of justification scores than the PE and MA groups and both active treatments resulting in lower scores than MA on global guilt and wrongdoing. Repeated measures MANOVAs for each group individually indicated that the MA group did not improve over time, whereas both the CPT and PE groups improved significantly over time: CPT, F(8, 49) = 5.0, p < .001, and PE, F(8, 48) = 4.8, p < .001. There were no significant changes from posttreatment to the 9-month follow-up for either active treatment.
The analyses for treatment completers replicated those for the ITT sample (and are available from Patricia A. Resick on request). Effect sizes for guilt cognitions are listed in Table 2 for the ITT and completer samples. In the ITT sample, CPT showed a large effect size for guilt cognitions, whereas PE showed a medium effect size. In the completer sample, both groups exhibited very large effects; however, there were moderate-to-large effect sizes for CPT relative to PE at posttreatment and 9 months posttreatment.
Delayed Treatment Results
Finally, on completion of the MA condition, interested participants were randomly assigned to one of the two active treatments. The treatment results in these delayed condition groups replicated those for the participants who were assigned directly to treatment. Figures 1 and 2 depict total CAPS scores in the ITT and completer samples for all four groups (the initial findings for the three groups [CPT, PE, and MA] and the delayed treatment results for the women who were subsequently assigned to CPT or PE on completion of the MA condition).
Discussion
A consistent picture emerged through the use of different types of statistical analyses with ITT and completer samples. Both CPT and PE were highly successful in treating PTSD in this sample of chronically distressed rape victims, most of whom had histories of other serious traumas. In contrast, the MA condition did not result in improvements. Both active therapies exceeded the clients’ expectations, even though their expectations were moderately high to begin with. The results for PE were quite similar to the results reported by Foa et al. (1999). CPT was as successful in treating PTSD as PE, even though participants did only half as much homework and had only two sessions (along with homework) directly recounting the trauma memory with writing and reading. Both therapies were also successful in treating depressive symptoms. However, CPT was superior to PE in remediating guilt cognitions on two of the four TRGI subscales.
Treatment outcome was not affected by the chronicity of the trauma. Therapy was equally effective for more recent and more chronic PTSD and depression, and there was no interaction between time since rape and either type of therapy. These results should not be surprising when one considers the predominance of avoidance in PTSD. Given that people with PTSD attempt to avoid thinking about and being reminded of the trauma, the trauma memory may become rather static once they have developed chronic PTSD. The number of years that pass may not actually change one’s thinking or emotions about the event if any reminders stimulate escape and avoidance behavior. Fortunately, both types of treatment appear to be as effective for someone traumatized 30 years ago as for someone traumatized 3 months ago.
The results of this study should have good generalizability to trauma populations generally. We attempted to restrict the exclusion criteria to those factors that would typically mitigate against focusing on trauma work in clinical settings (e.g., suicidality or substance dependence) or for experimental control purposes (e.g., less than 3 months postrape and medication changes). There was no exclusion for trauma history or personality disorders, so this sample was quite typical of clinical samples seeking treatment for PTSD.
The therapists had an equal amount of training and supervision in both types of therapy, and we found no differences in learning or implementing either therapy. Before participating in the research, the therapists had varied training with trauma clients, although they all had training in cognitive–behavioral therapy. Unusual to this study was the attempt to assess therapist competence as well as adherence to the protocols by outside evaluators who were experts with the particular therapies being studied. The fidelity of the treatments was excellent, and the competence of the therapists was evaluated as satisfactory or better in the sample that was rated.
In comparison with other treatments cited in the ISTSS treatment guidelines for PTSD (Foa et al., 2000), CPT compared very favorably. The effect sizes for CPT were as large as or larger than those for any other treatment study reported thus far. Among those who completed the treatments as designed, the effect sizes for both treatments were quite large. There was a slight advantage in effect sizes and end-state functioning favoring CPT over PE through the 3-month follow-up (and the 9-month follow-up for ITT sample effect sizes). Furthermore, the large majority of participants were no longer diagnosed with PTSD, and their improvement was maintained over a 9-month follow-up. This study included sufficient methodological rigor and a large enough sample size to provide reasonable support for the strength of the findings. Also, the delayed treatment groups provided a replication of the initial findings.
Along with decreases in symptoms after treatment, both types of treatment resulted in changes in cognitions. Given that we were quite vigilant in refraining from conducting cognitive therapy in PE, these findings demonstrate that exposure alone results in shifts in guilt cognitions. However, CPT was superior to PE with regard to guilt on two of the four TRGI scales. In reviewing exposurebased treatments, Foa and McNally (1996) suggested that exposure may be ineffective in terms of guilt. However, this may depend on the type of guilt reported by clients. Global guilt is highly correlated with general distress, and wrongdoing assesses characterological self-blame. As general global statements of guilt, global guilt and wrongdoing may be more easily dispelled with exposure to the trauma memory and simple statements regarding lack of blame (e.g., “It wasn’t your fault, you were not to blame”). However, hindsight bias and lack of justification are guilt cognitions that focus on interpretation of behaviors engaged in during the trauma and whether the event was foreseeable or preventable (E. S. Kubany, personal communication, September 2000). Such cognitions may require more focused and intense attention, as provided by CPT. CPT resulted in greater decreases in hindsight bias and lack of justification, which may require more active and sustained cognitive intervention than global guilt or a general sense of wrongdoing.
The dropout rates for this study were typical of PTSD rape treatment samples and similar to other studies (Foa et al., 1991, 1999; Krakow et al., 2001) with sexual assault survivors. This sample was suffering from severe and chronic PTSD, and most of the participants had been multiply traumatized. However, there were no differences in pretreatment PTSD or depression between those who dropped out and those who completed treatment. Although it was beyond the scope of this study to examine the full range of variables that might have affected treatment completion, this would be an important topic for future research.
In previous research, CPT was conducted in the context of group therapy (Resick & Schnicke, 1992). This study demonstrates that CPT is also quite efficacious as an individual treatment. Although CPT has been tested only with rape victims thus far, there is no reason to think that CPT would not be successful for other types of trauma. There are no treatment components that would be unique to the issues of rape victims. However, CPT needs to be tested with other populations to ensure generalization. Along the same lines, the therapy also will need to be evaluated among men with PTSD. Effectiveness studies of both CPT and PE will be necessary to determine the generalizability of the therapy outside of research settings. Furthermore, dismantling studies are needed to determine whether the exposure component, the cognitive therapy component, or both components are necessary and sufficient for remediating PTSD symptoms. Finally, as we find different types of therapy to be effective, we need to begin matching clients with therapies for optimal outcomes. Clients with PTSD in combination with comorbid guilt may benefit more from CPT than PE. There may be other factors, unknown at this time, that differentially favor one treatment or the other for particular clients.
Acknowledgments
This work was supported by Grant NIH-1 R01-MH51509 from the National Institute of Mental Health, awarded to Patricia A. Resick. We thank Linda Sharpe-Taylor, Amy Williams, Kathleen Chard, and Janine Broudeur for their assistance in conducting therapy with the clients seen through the study. We also express our appreciation to Edna Foa for consulting and training in prolonged exposure and Barbara Rothbaum, Lee Fitz Gibbons, Laurie Zoelner, Sherry Falsetti, and Monica Schnicke for assisting with adherence and competence ratings. Finally, we thank Robert Gibbons for his generous consultation on data analysis.
Footnotes
This number also includes clients who received CPT or PE after completing the MA condition and being randomly assigned to one of the two active treatments. Although the treatment outcome data for these groups are not presented in depth in this article, the protocols for treatment were followed, and participants were assessed on the same schedule.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Atkeson BM, Calhoun KS, Resick PA, Ellis EM. Victims of rape: Repeated assessment of depressive symptoms. Journal of Consulting and Clinical Psychology. 1982;50:96–102. doi: 10.1037//0022-006x.50.1.96. [DOI] [PubMed] [Google Scholar]
- Beck AT, Steer RA, Garbin MG. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clinical Psychology Review. 1988;8:77–100. [Google Scholar]
- Beck AT, Ward CH, Mendelsohn M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Klauminzer G, Charney DS, Keane TM. A clinician rating scale for assessing current and lifetime PTSD: The CAPS-1. Behavior Therapist. 1990;18:187–188. [Google Scholar]
- Calhoun KS, Resick PA. PTSD. In: Barlow DH, editor. Clinical handbook of psychological disorders. New York: Guilford Press; 1993. pp. 48–98. [Google Scholar]
- Cohen J. Statistical power analyses for the behavioral sciences. 2nd ed. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- First M, Gibbon M, Spitzer RL, Williams JBW. Structured Clinical Interview for DSM–IV (SCID) New York: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, Street GP. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology. 1999;67:194–200. doi: 10.1037//0022-006x.67.2.194. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hearst DE, Dancu CV, Hembree E, Jaycox LH. Prolonged exposure (PE) manual. Medical College of Pennsylvania, Eastern Pennsylvania Psychiatric Institute; 1994. Unpublished manuscript. [Google Scholar]
- Foa EB, Keane TM, Friedman MJ, editors. Effective treatments for PTSD: Practice guidelines from the International Society for Traumatic Stress Studies. New York: Guilford Press; 2000. [Google Scholar]
- Foa EB, McNally RJ. Mechanics of change in exposure therapy. In: Rapee RM, editor. Current controversies in the anxiety disorders. New York: Guilford Press; 1996. pp. 329–343. [Google Scholar]
- Foa EB, Riggs DS, Dancu CV, Rothbaum BO. Reliability and validity of a brief instrument for assessing posttraumatic stress disorder. Journal of Traumatic Stress. 1993;6:459–473. [Google Scholar]
- Foa EB, Rothbaum BO. Treating the trauma of rape. New York: Guilford Press; 1997. [Google Scholar]
- Foa EB, Rothbaum BO, Riggs DS, Murdock TB. Treatment of post-traumatic stress disorder in rape victims: A comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology. 1991;59:715–723. doi: 10.1037//0022-006x.59.5.715. [DOI] [PubMed] [Google Scholar]
- Gibbons R, Hedeker D, Elkin I, Waternaux C, Kraemer H, Greenhouse J, et al. Some conceptual and statistical issues in analysis of longitudinal psychiatric data. Archives of General Psychiatry. 1993;50:739–750. doi: 10.1001/archpsyc.1993.01820210073009. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Gibbons R. MIXREG: A computer program for mixed-effects regression analysis with autocorrelated errors. Computer Methods and Programs in Biomedicine. 1996;49:229–252. doi: 10.1016/0169-2607(96)01723-3. [DOI] [PubMed] [Google Scholar]
- Hedges LV. Estimation of effect size from a series of independent experiments. Psychological Bulletin. 1982;97:490–499. [Google Scholar]
- Heyting A, Tolboom JTBM, Essers JGA. Statistical handling of dropouts in longitudinal clinical trials. Statistics in Medicine. 1992;11:2043–2061. doi: 10.1002/sim.4780111603. [DOI] [PubMed] [Google Scholar]
- Kazdin AE. Research design in clinical psychology. 3rd ed. Boston: Allyn & Bacon; 1998. [Google Scholar]
- Kilpatrick DG, Veronen LJ, Resick PA. Psychological sequelae to rape: Assessment and treatment strategies. In: Doleys DM, Meredith RL, Ciminero AR, editors. Behavioral medicine: Assessment and treatment strategies. New York: Plenum; 1982. pp. 473–497. [Google Scholar]
- Krakow B, Hollifield M, Johnston L, Koss M, Schrader R, Warner TD, et al. Imagery rehearsal therapy for chronic nightmares in sexual assault survivors with posttraumatic stress disorder. Journal of the American Medical Association. 2001;286:537–545. doi: 10.1001/jama.286.5.537. [DOI] [PubMed] [Google Scholar]
- Kubany ES, Haynes SN, Abueg FR, Manke FP, Brennan JM, Stahura C. Development and validation of the Trauma-Related Guilt Inventory (TRGI) Psychological Assessment. 1996;8:428–444. [Google Scholar]
- Mazumdar S, Liu K, Houck P, Reynolds C. Intent-to-treat analysis for longitudinal clinical trials: Coping with the challenge of missing values. Journal of Psychiatric Research. 1999;33:87–95. doi: 10.1016/s0022-3956(98)00058-2. [DOI] [PubMed] [Google Scholar]
- Nishith P, Foa EB. Prolonged exposure therapy (PE): Therapist adherence and competence protocol. University of Missouri—St. Louis; 1994. Unpublished manuscript. [Google Scholar]
- Nishith P, Resick PA. Cognitive processing therapy (CPT): Therapist adherence and competence protocol. University of Missouri—St. Louis; 1994. Unpublished manuscript. [Google Scholar]
- Resick PA. Cognitive treatment of a crime-related PTSD. In: Peters RD, McMahon RJ, Quinsey VL, editors. Aggression and violence throughout the life span. Newbury Park, CA: Sage; 1992. pp. 171–191. [Google Scholar]
- Resick PA, Jordan CG, Girelli SA, Hutter CK, Marhoefer-Dvorak S. A comparative outcome study of group behavior therapy for sexual assault victims. Behavior Therapy. 1988;19:385–401. [Google Scholar]
- Resick PA, Markway BG. Clinical treatment of adult female victims of sexual assault. In: Hollin C, Howells K, editors. Clinical approaches to sex offenders and their victims. London: Wiley; 1991. pp. 261–284. [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. Journal of Consulting and Clinical Psychology. 1992;60:748–756. doi: 10.1037//0022-006x.60.5.748. [DOI] [PubMed] [Google Scholar]
- Resick PA, Schnicke MK. Cognitive processing therapy for rape victims: A treatment manual. Newbury Park, CA: Sage; 1993. [Google Scholar]
- Rosenthal R. Meta-analytic procedures for social research. Newbury Park, CA: Sage; 1991. Rev. ed. [Google Scholar]
- Rowan AB, Foy DW, Rodriguez N, Ryan S. Posttraumatic stress disorder in a clinical sample of adults sexually abused as children. Child Abuse and Neglect. 1994;18:51–61. doi: 10.1016/0145-2134(94)90095-7. [DOI] [PubMed] [Google Scholar]
- Ryan SW, Rodriguez N, Rowan A, Foy DW. Psychometric analysis of the Sexual Abuse Exposure Questionnaire (SAEQ); Paper presented at the 100th Annual Convention of the American Psychological Association; Washington, DC. 1992. Aug, [Google Scholar]