Abstract
Post-traumatic stress symptoms, depressive symptoms, and psychological dysregulation have been shown to mediate the relationship between child maltreatment and non-suicidal self-injury. However, these proposed mediators often co-occur and previous research has not tested mediation when all variables are assessed simultaneously. The current study sought to advance the literature on maltreatment and self-injury by estimating the mediational effects of post-traumatic stress symptoms, depressive symptoms, and psychological dysregulation in the same multiple mediator model. Both maltreated (n=129) and non-maltreated (n=82) adolescent females, consisting of Caucasian (55%), African-American (37%), and Bi-racial (8%) backgrounds, participated in the study. Results indicated that only post-traumatic stress symptoms mediated the relationship between maltreatment and self-injury when all variables were included in the model. Overall, post-traumatic symptoms represented a unique pathway from maltreatment to self-injury and warrant special attention when assessing and treating such behavior with adolescent females.
Keywords: child maltreatment, posttraumatic stress symptoms, non-suicidal self-injury, multiple mediation
The prevalence of self-injury is estimated to occur in approximately 13 – 46% of adolescents, with a disproportionately higher number of females represented in these samples (e.g., Lloyd-Richardson, Perrine, Dierker, & Kelley, 2007; Ross & Heath, 2002). Identifying factors that place adolescents on a pathway to self-injury is critical to understanding its place in adolescent development. The identification of these factors is also particularly important to advance clinical conceptualizations and treatments for adolescents engaging in such behavior.
Research on self-injury in adolescence suggests that adolescents engage in self-injury for individual as well as interpersonal reasons. Specifically, adolescents have reported getting a reaction from others, getting control over a particular situation, and regulating negative emotions and physiological states as the most common reasons for engaging in self-injury (Lloyd-Richardson, et al., 2007; Nock & Prinstein, 2004). Among these, the regulation of negative emotions or physiological states has garnered the most theoretical and empirical attention when attempting to identify proximal variables associated with self-injury. There appears to be a significant relationship between adolescents who have a limited skill set for regulating emotions, or emotion dysregulation, and an increased incidence of self-injury (Gratz & Roemer, 2008; Sim, Adrian, Zeman, Cassano, & Friedrich, 2009). This concept of emotion dysregulation is a part of developmental explanations that identify environmental, biological, and skill-based factors contributing to self-injury (Fruzzetti, Shenk, & Hoffman, 2005). Effective interventions for self-injury also emphasize the importance of emotion dysregulation in the treatment of such behavior with adolescents (Miller, Rathus, & Linehan, 2007).
Related studies have examined the function of engaging in self-injury for adolescents and report that adolescents engage in self-injury to reduce or escape negative emotions and aversive physiological states. For instance, in a community sample of young adolescent females, those experiencing higher levels of depressive symptoms were more likely to use self-injury as a way to regulate or escape those symptoms (Hilt, Cha, & Nolen-Hoeksema, 2008). Similarly, adolescents in a psychiatric inpatient setting experiencing symptoms of post-traumatic stress disorder (PTSD) and major depression, such as emotional numbing or blunted affect, were more like to use self-injury as a means of escaping these states (Nock & Prinstein, 2005). Thus, this growing body of research suggests an overlap in potential mechanistic processes in that adolescents who self-injure do so as a result of a limited skill set for coping with negative emotions (e.g., emotion dysregulation) and use self-injury as a drastic means of escaping or coping with negative emotions and physiological states.
One area of research that has focused on potential mechanisms for self-injury is that of child maltreatment. A substantial amount of research has demonstrated that a history of child maltreatment is associated not only with higher rates of self-injury (Gratz, 2006; Noll, Horowitz, Bonanno, Trickett, & Putnam, 2003; Romans, Martin, Anderson, Herbison, & et al., 1995) but also with symptoms of post-traumatic stress disorder (PTSS) (Kendall-Tackett, Williams, & Finkelhor, 1993), depression (Cicchetti & Toth, 2005), and emotion dysregulation (Shipman, Zeman, Penza, & Champion, 2000). Moreover, recent data also suggest that these three variables have mediational properties in the relationship between child maltreatment and self-injury. Weierich & Nock (2008) found symptoms of post-traumatic stress disorder, specifically re-experiencing and avoidance symptoms, to mediate the relationship between childhood sexual abuse and self-injury while controlling for the presence of major depression. Similarly, Glassman, Weierich, Hooley, Deliberto, & Nock (2007) found self-criticism, potentially a form of cognitive dysregulation, mediated the relationship between emotional abuse and self-injury. Finally, emotion dysregulation partially mediated the effects of an invalidating family environment (a latent factor consisting of emotional abuse and neglect) and deliberate self-injury (Sim, et al., 2009). Thus, PTSS, depressive symptoms and emotion dysregulation may indeed be important factors explaining the pathway from child maltreatment to self-injury.
These studies offer an important area for continued research as they demonstrate that there may be more than one pathway to self-injury for those adolescents experiencing child maltreatment. However, while existing research has advanced our understanding of the mediational properties of PTSS, depressive symptoms and emotion dysregulation as individual mediators, to date there has not been a mediator test simultaneously assessing the unique effects of each of these mediators in a multivariate model. A multiple mediator test of these variables represents a methodological advancement in the literature on maltreatment and self-injury because: 1) proposed mediators often co-occur and 2) the unique effect of one mediator is estimated while controlling for the effects of all other mediators on self-injury. Thus, a more stringent test of which variables mediate the relationship between child maltreatment and self-injury is one where previously demonstrated variables are estimated simultaneously with other theoretically relevant mediators.
Hypotheses
The current study aimed to test the mediational properties of PTSS, depressive symptoms, and psychological dysregulation to identify pathways to self-injury and to develop relevant clinical targets when treating such behavior using a sample of maltreated and comparison females. We adopted a clear definition of non-suicidal self-injury (NSSI) as the deliberate destruction of one’s own body tissue without suicidal intent (Nock & Favazza, 2009). There were two main hypotheses examined in this study. First, PTSS, depressive symptoms, and psychological dysregulation, will mediate the relationship between child maltreatment and NSSI when estimated in individual mediator tests. Second, the total indirect effect for a multiple mediator model where PTSS, depressive symptoms, and psychological dysregulation are estimated simultaneously, will significantly explain the relationship between child maltreatment and NSSI. No specific hypothesis about which individual variable would significantly mediate the relationship between child maltreatment and NSSI when all variables are estimated simultaneously was made. However, each indirect path was estimated to determine which variable may be most useful in explaining the pathway to NSSI for maltreated females.
Method
Sample
129 maltreated and 82 non-maltreated, comparison female adolescents aged 14–18 participated in this study. Maltreated females were referred within the previous 12 months by area protective services and experienced substantiated maltreatment as determined by a Child Protective Service (CPS) agency investigation. We adopted a relatively stringent operational definition of childhood maltreatment that included cases of physical neglect and contact physical or sexual abuse. Physical neglect was defined as abandonment, lack of supervision, or failure to provide for a child’s basic need of nutrition, clothing, hygiene, and safety. Contact physical abuse was defined as physical acts by a caregiver (defined as an adult directly charged with the supervision of the victim) resulting in bodily markings or that required physician care. Contact sexual abuse was defined as sexual acts by a perpetrator at least four years older than the victim including genital contact (i.e., fondling of the victim or victim-forced genital fondling of the perpetrator), digital, vaginal, anal or oral penetration, or violent, forced attempted penetration. Of the 129 maltreated participants, 58% were referred for sexual abuse, 34% for physical abuse, and 15% for physical neglect. Of these maltreated participants, 7% were referred for multiple or co-occurring types of abuse.
Comparison females were recruited from a local teen health center and were individually matched to maltreated females on race, family income level, age and family constellation (one or two parent households). At the time of the lab session, comparison females were screened for, and excluded in light of, reported (via caregiver and self-reports) childhood maltreatment experiences. The mean age of the sample was 15.75 years (SD=1.11), the median family income level was in the $40,000 to $50,000 range, 51% of households were single-parent, and the sample was 55% Caucasian, 37% African-American, and 8% Bi-racial.
Procedures
Adolescent participants resided in the catchment area of a Children’s Hospital located in the Mid-west region of the US. Caregivers accompanied adolescents to the lab session to provide informed consent. Participants eighteen years of age provided their own consent. After the consenting procedures, adolescents completed computerized questionnaires via multimedia computer assessment where participants responded to a host of questions regarding depressive symptoms and psychological dysregulation. In addition, all participants were interviewed to assess the presence of posttraumatic stress symptoms and deliberate self-injury. The study received approval from the hospital’s Institutional Review Board and was awarded a Federal Certificate of Confidentiality.
Measures
Posttraumatic Stress Symptoms (PTSS)
The Comprehensive Trauma Interview (CTI; Barnes, Noll, Putnam, & Trickett, 2009; Horowitz, 1998) is a semi-structured interview assessing symptomatic responses associated with exposure to traumatic or distressing life events with established inter-rater reliability. The CTI has a specific section devoted to the assessment of PTSS following exposure to a traumatic or distressing event using the PTSD Symptoms Scale derived from Davidson, Kudler, and Smith (1989). Questions in the PTSD Symptoms Scale were modified to comply with Clusters B (Reexperiencing), C (Avoidance), and D (Hyperarousal) of the Diagnostic and Statistical Manual of Mental Disorders – IV (American Psychiatric Association, 1994) for PTSD. Example of questions asked of each participant are: “Have you ever had painful images, memories or thoughts of what happened?”, “Have you ever avoided doing things or getting into situations that reminded you of what happened?”, and “Have you ever been jumpy, on edge, or easily startled because of what happened?” Responses to all questions are coded (0= No, 1=Yes) and a summary score of all responses is then calculated to reflect cumulative levels of PTSS. Because there were high correlations observed among the three cluster types (r’s = .61 – .71), a summary score of all endorsed symptoms was created and used in subsequent analyses. Reliability of the summary score of the PTSS symptoms in the current sample was excellent, α = .88.
Depressive Symptoms
The ten-item version of Center for Epidemiologic Studies-Depression (CES-D-10) scale was used to assess current depressive symptoms. The CES-D-10 is a shortened form of the CES-D with established levels of reliability and validity (Andresen, Malmgren, Carter, & Patrick, 1994). Reliability in the current sample was acceptable (α = .74).
Psychological Dysregulation
The Dysregulation Inventory (DI; Mezzich, Tarter, Giancola, & Kirisci, 2001) was administered to assess the presence of difficulties in the modulation of problematic cognitions, affect and behaviors. The DI is a 92-item self-report measure using a four-point weighted response scale from “0 = Never True” to “3 = Always True”. There are three subscales of the DI: affective, cognitive and behavioral dysregulation. Previous research has demonstrated acceptable levels of reliability (α’s = .89, .84, .93 respectively) for these three subscales with female adolescents. The total scale score of the DI was used in the current analyses because of high correlations among the DI’s subscales, r’s =.73–.81. Reliability for the total scale score of the DI in this sample was α = .96. We use the term ‘psychological dysregulation’ to refer to total levels of the presence of difficulties modulating problematic cognitions, affect and behaviors.
Non-suicidal Self-injury (NSSI)
NSSI was assessed in the CTI by a single question determining whether the adolescent had ever tried to intentionally hurt themselves by damaging the physical integrity of their body (0= No, 1=Yes). Because this item could elicit a ‘Yes’ response from those participants who engaged in NSSI, as well as those who previously attempted suicide, additional data on previous suicide attempts was available and obtained from another section of the CTI. Twenty-eight participants reported making a previous suicide attempt. Since our focus for the current study was on NSSI as opposed to suicidal self-injury, these twenty-eight participants were removed, reducing our total sample size to 183 for all remaining analyses.
Data Analytic Strategy
Mediational tests were conducted in two stages to comprehensively assess the role of each mediator in explaining the effect between maltreatment and NSSI. First, each proposed mediator was analyzed using individual mediator analyses (e.g., Baron & Kenny, 1986). Sobel tests were conducted to determine whether the indirect effect for each proposed mediator was significant, an indication of mediation. Second, each variable demonstrating mediation in individual mediator analyses was then included in a multiple mediator model (Preacher & Hayes, 2008) to: (1) assess whether the specified set of variables mediated the relationship between maltreatment and NSSI, and (2) whether the unique indirect effect of any one variable mediated the relationship above and beyond the other variables estimated in the model.
Results
There were no demographic differences observed between the maltreated and comparison groups on age, race, family income or family composition. A multivariate analysis of variance (MANOVA) was conducted to assess for differences between maltreatment and comparison samples on each of the proposed mediational variables. The MANOVA revealed a significant overall effect for the specified model, F(3, 179) = 12.83, p < .001. Post-hoc comparisons indicated that maltreated females were significantly more likely to have higher PTSS, F(1, 181) = 34.45, p < .001, CES-D-10, F(1, 181) = 8.34, p < .01, and DI, F(1, 181) = 12.86, p < .001 scores. Significant relationships between types of maltreatment and NSSI were also observed. Phi correlation coefficients indicated that sexual abuse (φ = .21, p <.01), neglect (φ = .15, p <.05), and multiple abuses (φ = .26, p <.001) were significantly related to NSSI. Table 1 presents the correlation matrix for all variables included in the mediational tests.
Table 1.
Inter-correlations among variables included in mediational analyses.
| Variable | 1 | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| 1. Maltreatment | - | ||||
| 2. CES-D-10 | .21* | - | |||
| 3. PTSS | .40** | .40** | - | ||
| 4. DI | .26** | .52** | .34** | - | |
| 5. NSSI | .26** | .28** | .38** | .23* | - |
Note:
= p ≤ .01;
= p ≤ .001. CES-D-10 = Center for Epidemiologic Studies-Depression-10; PTSS = Posttraumatic Stress Symptoms; DI = Dysregulation Inventory; NSSI = Non-suicidal Self-injury. Pearson’s, Phi, and Point-biserial correlations are presented for respective comparisons.
Individual Mediator Tests
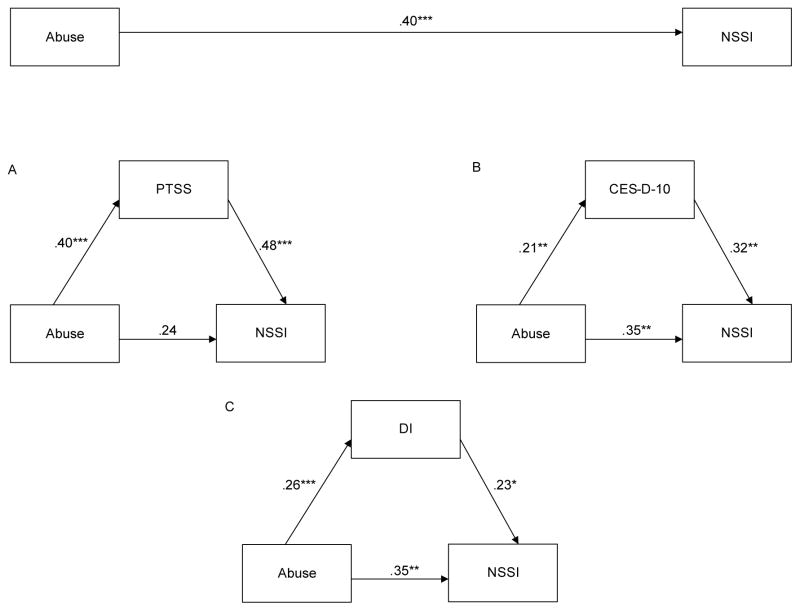
Three individual tests of mediation were conducted with maltreatment status as the predictor variable, PTSS, CES-D-10, or DI as a mediator, and NSSI as the criterion variable. Maltreatment status was included as a predictor in each model testing the relationship between a respective mediator and NSSI. Direct paths with continuous outcomes were assessed using linear regression. Paths with dichotomous outcomes were assessed using logistic regression. Because linear and logistic regressions use different scaling procedures to derive respective parameter estimates, each estimate was standardized in order to make comparisons across results from the differing regression equations (see MacKinnon & Dwyer, 1993). As a result, Sobel tests were then obtained and were used to determine mediation in these analyses. As hypothesized, all three variables demonstrated mediation of the relationship between maltreatment and NSSI. Sobel tests assessing the significance of the indirect path for PTSS, 3.30, p < .001, CES-D-10, 2.09, p < .05, and DI were all significant, 2.05, p < .05. As such, each variable was retained in the multiple mediator model that simultaneously estimated the indirect pathways for each mediator. See Figure 1 for standardized estimates of the direct paths in each of the individual mediator tests.
Figure 1.
Individual mediator analyses. A = Post-traumatic stress symptoms (PTSS), B = Center for Epidemiologic Studies-Depression-10 (CES-D-10), and C = Dysregulation Inventory (DI). NSSI = Non-suicidal self-injury. * = p < .05; ** = p < .01; *** = p < .001.
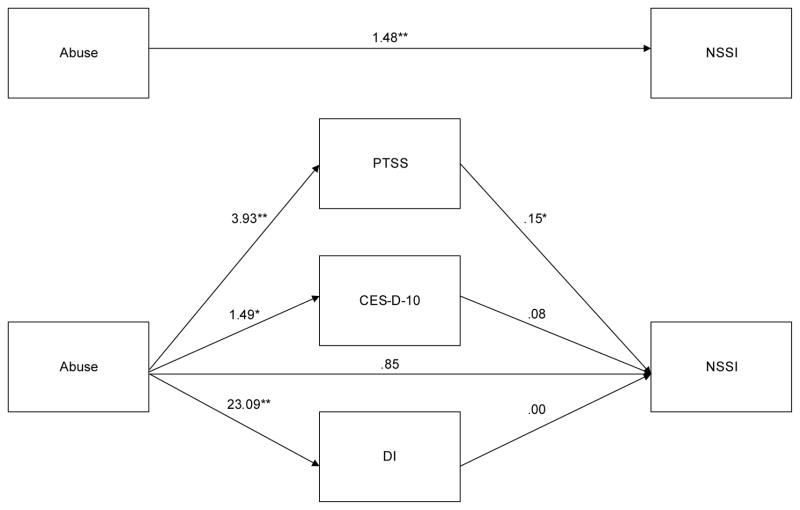
Multiple Mediator Test
Tests of multiple mediation with PTSS, CES-D-10, and DI assessed simultaneously were estimated utilizing PASW v.17 and a supplemental macro script for testing multiple mediator models (see Preacher & Hayes, 2008). The total indirect effect for the set of PTSS, CES-D-10, and DI scores was significant, Z = 3.21, p < .001, indicating that the set of mediators explained the relationship between maltreatment status and NSSI. As can be seen in Figure 2, the direction of estimates in each pathway indicates that being maltreated was associated with greater PTSS, CES-D-10, and DI scores which were associated with an increased risk for NSSI. The specific indirect effect of each mediator was then examined to determine whether any individual variable significantly mediated the effect of maltreatment status on NSSI while also assessing the other two mediators. As can be seen in Table 2, PTSS was the only unique indirect pathway mediating the relationship between maltreatment and self-injury, Z = 2.71, p < .01. CES-D-10 and DI did not significantly contribute to the total indirect effect above and beyond PTSS. See Figure 2 for the unstandardized estimates of each direct pathway.
Figure 2.
Multiple mediator analysis. PTSS = Post-traumatic stress symptoms; CES-D-10 = Center for Epidemiologic Studies-Depression-10; DI = Dysregulation Inventory; NSSI = Non-suicidal self-injury. * = p ≤ .01; ** = p ≤ .001.
Table 2.
Mediation of the relationship between child maltreatment and non-suicidal self-injury.
| Point Estimate | SE | Z | BCa 95% CI |
||
|---|---|---|---|---|---|
| Lower | Upper | ||||
| Total | .82 | .25 | 3.21** | .35 | 1.32 |
| PTSS | .62 | .23 | 2.71* | .21 | 1.09 |
| CES-D-10 | .13 | .11 | 1.17 | −.04 | .42 |
| DI | .07 | .14 | 0.48 | −.22 | .36 |
Note:
= p < .01;
= p < .001. BCa = bias corrected and accelerated; CES-D-10 = Center for Epidemiologic Studies-Depression-10; PTSS = Posttraumatic Stress Symptoms; DI = Dysregulation Inventory. Estimates based on 5000 bootstrap samples.
Discussion
The goal of the present study was to evaluate the total and unique contributions of several proposed mediators of the relationship between child maltreatment and self-injury. To do so, variables that have previously been shown to mediate this relationship were selected to stringently test which mediator has the strongest relationship with self-injury when estimated simultaneously. Results from the present study add to a growing body of literature identifying pathways from maltreatment to self-injury while offering important insight into the clinical implications of such results.
Consistent with previous research, there was a significant relationship between child maltreatment and self-injury. However, this relationship was mediated by a set of variables related to both maltreatment and self-injury, including PTSS, depressive symptoms, and psychological dysregulation. Within this set of variables, PTSS was the only variable to mediate the relationship between maltreatment and self-injury. This suggests that the experience of PTSS, including clusters of avoidant, hyperarousal, and re-experiencing symptoms, adds considerable and unique risk for maltreated adolescents to engage in self-injury above and beyond the effects of depressive symptoms and psychological dysregulation. Although previous research has found that the re-experiencing and avoidance clusters of PTSD mediate the relationship between maltreatment and self-injury (Weierich & Nock, 2008), the high correlations among these symptom clusters in the current sample precluded any attempt to illustrate unique effects for any cluster type given the high potential for multicollinearity. Nevertheless, this study highlights that the pathway from maltreatment to PTSS to self-injury is particularly influential for adolescent females and that PTSS are among the most clinically relevant targets with this population.
A functional perspective of self-injury (Nock & Prinstein, 2004) suggests that it is the context in which adolescents respond to or cope with negative emotional states, especially PTSS, that seems to be most relevant in explaining self-injurious behavior as well as how to treat it. Our conclusion is that these results support previous research and theory that conceptualize self-injury as an effort to cope with certain negative experiences or states (Nock & Prinstein, 2005). To do so is to view self-injury in response to prior events and serving an important purpose or function within this context. Thus, self-injury is viewed not as an isolated, static symptom of any one particular psychiatric disorder but as an active attempt at coping with and relating to an aversive situation or context. This interpretation is especially useful as it allows for clinical targets to be shaped toward process-oriented targets, such as coping skills for affect-related situations, as opposed to content oriented targets that focus primarily on symptoms of specific disorders (Barlow, Allen, & Choate, 2004).
It was surprising that psychological dysregulation did not mediate the relationship between maltreatment and self-injury in the multiple mediator test. Although difficult to interpret null findings, we believe that there could be several explanations for this. First, Sim et al (2009) showed emotion dysregulation to be a partial mediator of self-injury but relied on a sample of adolescent emotional abuse where our focus was on other types of maltreatment. Upon examination of the relationship between types of maltreatment and self-injury in the current study, child sexual abuse, neglect, and exposure to multiple types of maltreatment were significant correlates of self-injury and appear to contribute most to the relationship between maltreatment and self-injury. Hence, the discrepancy between our study and the Sim et al. (2009) study could be attributable to the examination of emotional abuse in particular. Second, the current study performed a test of several potential mediators of self-injury including psychological dysregulation and depressive symptoms. Thus, after accounting for the unique effects of PTSS, there may not have been a significant amount of variation left for psychological dysregulation and depressive symptoms to explain. This is not to say that these variables should be discounted as important processes involved in the study of self-injury. Instead, there may be additional components in PTSS that are more salient.
There are several overall strengths of this study. First, the sample consisted of a relatively large number of female adolescents within a racially diverse demography. Second, a multi-method assessment of data collection was used via state of the art methodologies including: (1) CPS substantiated cases to determine child maltreatment, (2) a comparison group that was demographically matched to the maltreated sample on income, race, age, and family constellation to control these potential confounds, (3) a thorough, semi-structured interview to assess current levels of PTSS and NSSI, and (4) well-established self-report measures to assess current levels of depressive symptoms and psychological dysregulation. Third, data obtained from these methodologies were used in a unique, multivariate test of several known mediators of the relationship between child maltreatment and self-injury. To our knowledge, this is the first multiple mediator test of the relationship between child maltreatment and NSSI. These findings represent an original contribution to the literature while strengthening conclusions made about the pathways to NSSI for maltreated female adolescents as well as the relevant targets for clinical intervention with this population.
In light of these strengths, there are several limitations to consider. First, although we found mediation for PTSS, this is a cross-sectional study and in the absence of longitudinal data and analyses, it remains unclear whether this mediational effect would be upheld in a longitudinal design. Second, our sample, though rich in size and diversity, consists only of females and conclusions about whether this same pathway to self-injury holds for adolescent males remains unclear. Despite these limitations, the results from this study highlight the importance of assessing PTSS in maltreated female adolescents engaging in self-injury.
One way to understand the place of self-injury in adolescence is to examine the developmental pathways of those adolescents engaging in self-injury. The value of such an approach allows for the identification of risk factors that explain how an adolescent comes to engage in such behavior. As a major impetus in this direction, a history of child maltreatment appears to lead adolescents down a path to self-injury that is explained in large part by the presence of post-traumatic symptoms. Self-injury can be viewed, then, as an active response to coping with maltreatment and post-traumatic symptoms which leads to the identification of functionally relevant therapeutic targets, such as the escape functions of self-injury and the need for more flexible behaviors that successfully address the aversive negative consequences of maltreatment.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4. Washington, D.C.: American Psychiatric Press; 1994. [Google Scholar]
- Andresen EM, Malmgren JA, Carter WB, Patrick DL. Screening for depression in well older adults: evaluation of a short form of the CES-D (Center for Epidemiologic Studies Depression Scale) Am J Prev Med. 1994;10(2):77–84. [PubMed] [Google Scholar]
- Barlow DH, Allen LB, Choate ML. Toward a Unified Treatment for Emotional Disorders. Behavior Therapy. 2004;35(2):205–230. doi: 10.1016/j.beth.2016.11.005. [DOI] [PubMed] [Google Scholar]
- Barnes JE, Noll JG, Putnam FW, Trickett PK. Sexual and physical revictimization among victims of severe childhood sexual abuse. Child Abuse & Neglect. 2009;33(7):412–420. doi: 10.1016/j.chiabu.2008.09.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality & Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Cicchetti D, Toth SL. Child maltreatment. Annual Review of Clinical Psychology. 2005;1(1):409–438. doi: 10.1146/annurev.clinpsy.1.102803.144029. [DOI] [PubMed] [Google Scholar]
- Davdison J, Kudler HS, Smith R. Validity and reliability of the DSM-III criteria for posttraumatic stress disorder. Journal of Nervous and Mental Disease. 1989;177:336–341. doi: 10.1097/00005053-198906000-00003. [DOI] [PubMed] [Google Scholar]
- Fruzzetti AE, Shenk C, Hoffman PD. Family interaction and the development of borderline personality disorder: A transactional model. Development & Psychopathology. 2005;17(4):1007–1030. doi: 10.1017/s0954579405050479. [DOI] [PubMed] [Google Scholar]
- Glassman LH, Weierich MR, Hooley JM, Deliberto TL, Nock MK. Child maltreatment, non-suicidal self-injury, and the mediating role of self-criticism. Behaviour Research and Therapy. 2007;45(10):2483–2490. doi: 10.1016/j.brat.2007.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gratz KL. Risk factors for deliberate self-harm among female college students: The role and interaction of childhood maltreatment, emotional inexpressivity, and affect intensity/reactivity. American Journal of Orthopsychiatry. 2006;76(2):238–250. doi: 10.1037/0002-9432.76.2.238. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. The relationship between emotion dysregulation and deliberate self-harm among female undergraduate students at an urban commuter university. Cognitive Behaviour Therapy. 2008;37(1):14–25. doi: 10.1080/16506070701819524. [DOI] [PubMed] [Google Scholar]
- Hilt LM, Cha CB, Nolen-Hoeksema S. Nonsuicidal self-injury in young adolescent girls: Moderators of the distress-function relationship. Journal of Consulting and Clinical Psychology. 2008;76(1):63–71. doi: 10.1037/0022-006X.76.1.63. [DOI] [PubMed] [Google Scholar]
- Horowitz L. The relationship of child sexual abuse to revictimization: Mediating variables and developmental processes. Catholic University of America; 1998. [Google Scholar]
- Kendall-Tackett KA, Williams LM, Finkelhor D. Impact of sexual abuse on children: A review and synthesis of recent empirical studies. Psychological Bulletin. 1993;113(1):164–180. doi: 10.1037/0033-2909.113.1.164. [DOI] [PubMed] [Google Scholar]
- Lloyd-Richardson EE, Perrine N, Dierker L, Kelley ML. Characteristic and functions on non-suicidal self-injury in a community sample of adolescents. Psychological Medicine. 2007;37(8):1183–1192. doi: 10.1017/S003329170700027X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Evaluation Review. 1993;17(2):144–158. [Google Scholar]
- Mezzich AC, Tarter RE, Giancola PR, Kirisci L. The dysregulation inventory: A new scale to assess the risk for substance use disorder. Journal of Child & Adolescent Substance Abuse. 2001;10(4):35–43. [Google Scholar]
- Miller AL, Rathus JH, Linehan MM. Dialectical Behavior Therapy with Suicidal Adolescents. New York, NY: Guilford; 2007. [Google Scholar]
- Nock MK, Favazza AR. Nonsuicidal self-injury: Definition and classification. In: Nock MK, editor. Understanding nonsuicidal self-injury: Origins, assessment, and treatment. 2009. pp. 9–18. [Google Scholar]
- Nock MK, Prinstein MJ. A Functional Approach to the Assessment of Self-Mutilative Behavior. Journal of Consulting and Clinical Psychology. 2004;72(5):885–890. doi: 10.1037/0022-006X.72.5.885. [DOI] [PubMed] [Google Scholar]
- Nock MK, Prinstein MJ. Contextual features and behavioral functions of self-mutilation among adolescents. J Abnorm Psychol. 2005;114(1):140–146. doi: 10.1037/0021-843X.114.1.140. [DOI] [PubMed] [Google Scholar]
- Noll JG, Horowitz LA, Bonanno GA, Trickett PK, Putnam FW. Revictimization and self-harm in females who experienced childhood sexual abuse: results from a prospective study. J Interpers Violence. 2003;18(12):1452–1471. doi: 10.1177/0886260503258035. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40(3):879–891. doi: 10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Romans SE, Martin JL, Anderson JC, Herbison GP, et al. Sexual abuse in childhood and deliberate self-harm. American Journal of Psychiatry. 1995;152(9):1336–1342. doi: 10.1176/ajp.152.9.1336. [DOI] [PubMed] [Google Scholar]
- Ross S, Heath N. A study of the frequency of self-mutilation in a community sample of adolescents. Journal of Youth and Adolescence. 2002;31(1):67–77. [Google Scholar]
- Shipman K, Zeman J, Penza S, Champion K. Emotion management skills in sexually maltreated and nonmaltreated girls: a developmental psychopathology perspective. Dev Psychopathol. 2000;12(1):47–62. doi: 10.1017/s0954579400001036. [DOI] [PubMed] [Google Scholar]
- Sim L, Adrian M, Zeman J, Cassano M, Friedrich WN. Adolescent deliberate self-harm: linkages to emotion regulation and family emotional climate. Journal of Research on Adolescence. 2009;19(1):75–91. [Google Scholar]
- Weierich MR, Nock MK. Posttraumatic stress symptoms mediate the relation between childhood sexual abuse and nonsuicidal self-injury. J Consult Clin Psychol. 2008;76(1):39–44. doi: 10.1037/0022-006X.76.1.39. [DOI] [PubMed] [Google Scholar]