Abstract
Objectives. We evaluated the effectiveness of the US Air Force Suicide Prevention Program (AFSPP) in reducing suicide, and we measured the extent to which air force installations implemented the program.
Methods. We determined the AFSPP's impact on suicide rates in the air force by applying an intervention regression model to data from 1981 through 2008, providing 16 years of data before the program's 1997 launch and 11 years of data after launch. Also, we measured implementation of program components at 2 points in time: during a 2004 increase in suicide rates, and 2 years afterward.
Results. Suicide rates in the air force were significantly lower after the AFSPP was launched than before, except during 2004. We also determined that the program was being implemented less rigorously in 2004.
Conclusions. The AFSPP effectively prevented suicides in the US Air Force. The long-term effectiveness of this program depends upon extensive implementation and effective monitoring of implementation. Suicides can be reduced through a multilayered, overlapping approach that encompasses key prevention domains and tracks implementation of program activities.
Although much is known about risk factors for suicide, there are few examples of multifaceted, sustainable programs for reducing morbidity and mortality attributable to suicide and suicidal behaviors. The Air Force Suicide Prevention Program (AFSPP) has been found to have achieved significant relative risk reductions of rates of suicide and other violence-related outcomes, including accidental death and domestic violence.1 The AFSPP, now in its 13th year, is an example of a sustained community-based effort that directly addresses suicide as a public health problem.
The AFSPP, launched in 1996 and fully implemented by 1997,1 emphasizes leadership involvement and a community approach to reducing deaths from suicide. The program is an integrated network of policy and education that focuses on reducing suicide through the early identification and treatment of those at risk. It uses leaders as role models and agents of change, establishes expectations for airman behavior regarding awareness of suicide risk (i.e., policymaking), develops population skills and knowledge (i.e., education and training), and investigates every suicide (i.e., outcomes measurement). The program represents the air force's fundamental shift from viewing suicide and mental illness solely as medical problems and instead seeing them as larger service-wide community problems (Gen T. S. Moorman Jr, US Air Force, personal communication, June 2001).
The program's approach is predicated on current knowledge that individuals at risk exhibit warning signs and that intervention at an early stage lowers risk and results in improved outcomes. Thus, the program aims to reduce stigma and encourage early help-seeking behavior by changing social norms through education and policy. This is achieved at the community level by changing the community's knowledge, values, beliefs, attitudes, and behaviors concerning distress, help-seeking, and suicide. The AFSPP affirms and encourages help-seeking behavior, normalizes the experience of distress, promotes the development of coping skills, fights the stigma associated with receiving mental health care, and educates the community about the absence of negative career consequences for seeking and receiving treatment. The program also seeks to improve outcomes in putative distal risk factors for suicide, including family violence, alcohol and substance use, diminishing work performance, and depression. The result over the years has been the creation of an atmosphere of responsibility and accountability for reducing deaths from suicide that includes new expectations for behavior at the community and individual levels.
With little theoretical guidance available in 1996 to shape the program, the air force developed an overlapping programmatic design, resulting in far-reaching enhanced capacity of organizational responsiveness in critical areas at multiple levels. These overlapping components became known formally as the 11 Initiatives of the Air Force Suicide Prevention Program, which are described briefly in the box on the next page and in detail online (AFPAM 44–160; available at http://afspp.afms.mil/idc/groups/public/documents/afms/ctb_056459.pdf).
We studied the effect of the AFSPP on air force suicide rates from 1997, when the program was fully implemented, through 2008. We examined rates in the context of a 27-year period, from 1981 through 2008, during which time there have been 3 military conflicts and a major downsizing of the air force during the early 1990s. This 27-year period provides an important historical perspective on suicide rates in an organization that underwent rapid, widespread change in force structure and that dealt with the onset and continuation of Operation Enduring Freedom in Afghanistan in 2001 and Operation Iraqi Freedom in 2003. We also conducted a naturalistic experiment from 2004 through 2006, when we measured the implementation of program components during and after a transient increase in suicide rates.
METHODS
An intervention regression model2 was applied to evaluate the influence of the AFSPP on quarterly suicide rates over time, and to create forecasts for future quarters. This type of time-series model has independent variables marking intervention periods and autoregressive errors that model the stochastic dependency of observations over time. All analyses were conducted using SAS software3 applied to data from air force administrative databases.
Quarterly suicide rates were calculated per 100 000 for the active duty air force population from 1981 through 2007, and forecasted rates were calculated for each quarter of 2008. Each quarterly suicide rate was modeled as a regression with separate pre- and postintervention means and with first-order autoregressive errors (where the current error term is a fraction of the previous error term plus a random disturbance), using the ARIMA procedure.2 This model compares the preintervention quarterly mean suicide rate for all previous time periods to the postintervention mean quarterly suicide rate for all quarters following the start date of the intervention.
An autocorrelation plot and the white noise test were used to check for stationarity and autocorrelation. Both first-order autoregressive and first-order moving average models were estimated.2 The autoregressive model provided a better fit. The model was further examined for outliers, and its residuals were tested for any remaining autocorrelation. Six outliers were detected and entered into the model as points with different means.
The intervention regression model controlled for historical trends and seasonality, as well as for statistical white noise. The size of the air force population, which decreased over the study period, was confounded with time. To determine whether population size was correlated with suicide rates independently of the intervention, we modeled the annual suicide rate as a function of annual population size and an indicator of the start of the AFSPP in 1997, using a regression model weighted by the population size and with autocorrelated errors using SAS Proc Mixed.3 The model was repeated using the change in population size. Lastly, population risk indicators were established from historical patterns, to detect early triggers of changes in the pattern of suicide rates.
In 2002 we began discussing how the AFSPP was implemented across the many installations of the air force, and we sought to view it within a developing theoretical prevention framework.4 In 2004 we began using an implementation appraisal survey to measure implementation of AFSPP program activities associated with each of the 11 Initiatives (see the box on this page). In 2006 we further refined the survey into checklist form. The 11 Initiatives were purposely established to provide an overlapping organizational framework, but not necessarily a theoretical framework. Therefore, we clustered items on the implementation appraisal instruments into 7 prevention domains: (1) leadership involvement, (2) continuous professional military training, (3) development of guidelines for commanders, (4) ongoing community education, (5) development of integrated delivery system and community action information boards, (6) enhancement of community mental health services, and (7) instituting policies.
The 11 Initiatives of the US Air Force Suicide Prevention Program
Leadership involvement: Air force leaders actively support the entire spectrum of suicide prevention initiatives in the air force community. Regular messages from the chief of staff of the air force, other senior leaders, and base commanders motivate the air force community to fully engage in suicide prevention efforts.
Addressing suicide prevention through professional military education: Suicide prevention education is included in all formal military training.
Guidelines for commanders on use of mental health services: Commanders receive training on how and when to use mental health services, and their role in encouraging early help-seeking behavior.
Community preventive services: Community prevention efforts carry more impact than treating individual patients 1 at a time. The Medical Expense and Performance Reporting System was updated to effectively track and encourage prevention activities.
Community education and training: Annual suicide prevention training is provided for all military and civilian employees in the air force.
Investigative interview policy: The period following an arrest or investigative interview is a high-risk time for suicide. Following any investigative interview, the investigator is required to “hand off” the individual directly to the commander, first sergeant, or supervisor. The unit representative is then responsible for assessing the individual's emotional state and contacting a mental health provider if any question about the possibility of suicide exists.
Trauma stress response (originally critical incident stress management): Trauma stress response teams were established worldwide to respond to traumatic incidents such as terrorist attacks, serious accidents, or suicide. These teams help personnel deal with the emotions they experience in reaction to traumatic incidents.
Integrated Delivery System (IDS) and Community Action Information Board (CAIB): At the air force, major command, and base levels, the CAIB and IDS provide a forum for the cross-organizational review and resolution of individual, family, installation, and community issues that impact the readiness of the force and the quality of life for air force members and their families. The IDS and CAIB help coordinate the activities of the various base helping agencies to achieve a synergistic impact on community problems and reduce suicide risk.
Limited Privilege Suicide Prevention Program: Patients at risk for suicide are afforded increased confidentiality when seen by mental health providers (Limited Privilege Suicide Prevention Program). Additionally, Limited Patient-Psychotherapist Privilege was established in 1999, limiting the release of patient information to legal authorities during Uniform Code of Military Justice proceedings.
IDS Consultation Assessment Tool (originally the Behavioral Health Survey): The IDS Consultation Assessment Tool allows commanders to assess unit strengths and identify areas of vulnerability. Commanders can use this tool in collaboration with IDS consultants to design interventions to support the health and welfare of their personnel.
Suicide Event Surveillance System: Information on all air force active duty suicides and suicide attempts are entered into a central database that tracks suicide events and facilitates the analysis of potential risk factors for suicide in air force personnel.
The items in the domains are best described as “operational measurements,” after the work of Hand5; this kind of measure is also called an “indicator measure” by Fayers and Hand.6 As Fayers and Hand6 state, in contrast to psychometric measures, the goal of using indicator measures is to construct an index that consists of the combined values of the measured variables. We then used these indexes to calculate an implementation score for each of the 7 prevention domains. (To preserve the most information for analyses of implementation levels, data were analyzed at the installation level.) This permitted us to measure operationally whether an air force installation carried out the activities described in the box on the previous page, which are the direct result of complying with the 11 Initiatives. Each question was assigned a score of 1 if a respondent answered “yes” and 0 otherwise.
The data were weighted according to the number of implementation indicators from the 11 Initiatives that were grouped within each of the 7 prevention domains. Levels of implementation were then determined across all installations, and the scores were represented as the percentage of the maximum possible score for each of the 7 domains. Air force leaders and installation commanders completed the 11 Initiatives survey in 2004 and the 11 Initiatives checklist in 2006, using administrative records of activities monitored at each installation. Data were reported anonymously to minimize the potential for reporting bias and were compiled both at the base level and at the level of the 9 major commands, which are the operational units of the service.
RESULTS
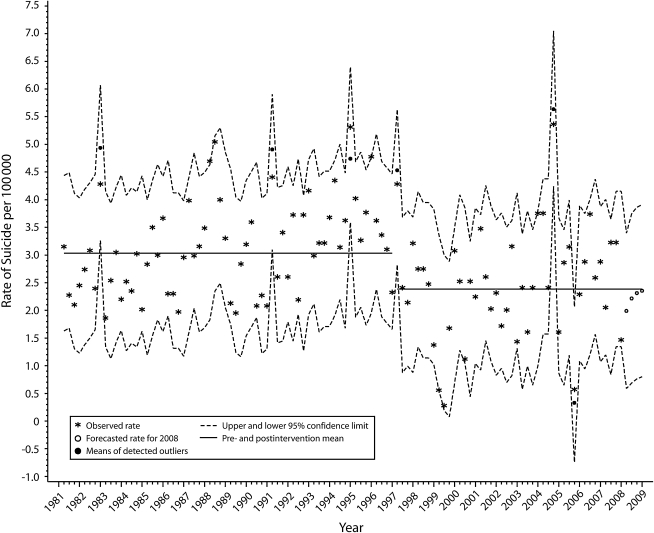
Figure 1 depicts the observed quarterly suicide rate from 1991 through 2008. The horizontal lines represent the mean pre- and postintervention quarterly suicide rates, and the deviations from this mean are depicted as outliers across the decades. The estimated mean suicide rate per quarter during the intervention period was 2.387 per 100 000, compared with 3.033 per 100 000 for the preintervention mean, for a change of 0.646 (P < .01). The estimated correlation coefficient between consecutive quarterly observations is 0.431 (P < .001), and the estimated variance of the disturbance term is 0.513. During the postintervention period, in the third quarter of 2004, there was a significant upward spike in suicide rates (P < .001); subsequently, suicide rates fell and have remained within the expected range of the low rates seen soon after initial implementation of the program.
FIGURE 1.
Quarterly suicide rates: US Air Force, 1981–2008.
Note. The US Air Force Suicide Prevention Program was implemented in 1997.
We observed an inverse relationship between population size and suicide rates in the preintervention period: a smaller population size tended to be associated with a higher suicide rate than that observed for a larger population size. All population sizes above 500 000 occurred during the period from 1981 through 1990, with the population declining during the remainder of the preintervention period. The regression model for the pre- and postintervention periods included an indicator of implementation of the AFSPP in 1997, in addition to population size. It showed a linear nonsignificant relationship between the rate and the population size, with a negative slope of −1.38 (P > .05). Because the population size and the intervention period are confounded, the regression intervention effect (–4.9; P < .05) is larger than in the bivariate analysis (–2.9; P < .05) unadjusted for population size. A similar trend was found when the relationship between the change in population size and suicide rate was investigated.
To give air force leadership tools for early detection of future increases in suicide rates, we developed risk indicators on the basis of the forecasted suicide rate for 2008 (9.3 per 100 000). Rates less than or equal to 1 standard deviation from the forecast rate (< 12.1 per 100 000) were identified as indicators of concern. Rates greater than 1 standard deviation from the forecast rate (12.1–14.8 per 100 000) were defined as indicators of warning, and rates greater than 2 standard deviations from the forecast rate (> 14.8 per 100 000) were identified as critical indicators of a change in the pattern of suicide rates.
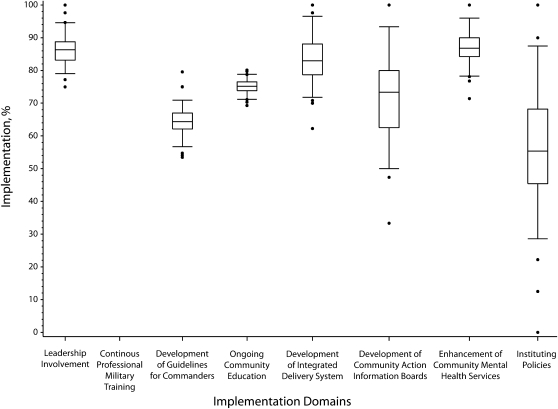
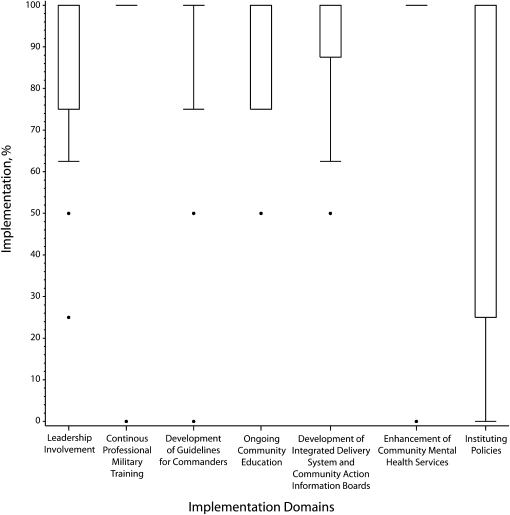
Installations reported variation in the extent to which they implemented the AFSPP's suicide prevention activities as specified by the 11 Initiatives. Figures 2 and 3 show the levels of implementation across the 7 prevention domains in 2004 and 2006, respectively. These results suggest an overall higher level of AFSPP implementation in 2006 than in 2004. Median implementations for the 7 prevention domains in 2004 were all below 90%, and the lowest was 56% (Figure 2). In comparison, during 2006 the overall implementation values for 2 of the 7 prevention domains (continuous professional military training and enhancement of community mental health services) were 100% for 95% of all bases. For prevention activities in the 5 other prevention domains in 2006, at least half of the bases were found to have high levels of implementation (Figure 3).
FIGURE 2.
Levels of US Air Force Suicide Prevention Program (AFSPP) implementation, distributed across installations, in 2004.
Note. Horizontal lines represent the 5th, 25th, 50th, 75th, and 95th percentiles. Dots represent points beyond the 95th percentile.
FIGURE 3.
Levels of the US Air Force Suicide Prevention Program (AFSPP) implementation, distributed across installations, in 2006.
Note. Horizontal lines represent the 5th, 25th, 50th, 75th, and 95th percentiles. Dots represent points beyond the 95th percentile.
DISCUSSION
In recent years there has been a marked increase in research on translating the findings of efficacy and effectiveness studies into actual health practices.7,8 The AFSPP provides an opportunity to study the implementation of public health practices intended to reduce deaths from suicide. This opportunity is unique in 3 ways. First, the AFSPP was developed well before implementation science was acknowledged as a field of study. Second, the current operational structure of the AFSPP evolved over time, even though its principal initiatives were described at the outset; thus, attention to sustained implementation of its core components emerged iteratively. Third, this public health prevention program was not originally developed on a theoretical basis, which is now recommended as the best way to strengthen the credibility of measured outcomes.7 In spite of this latter shortcoming, the subsequent identification of theoretical prevention domains for the AFSPP proved to be relatively straightforward.
The effects of the AFSPP are inevitably confounded with the activation of the air force for warfare, beginning immediately after the attacks of September 11, 2001, and accelerating into the wars in Afghanistan and Iraq. The possibility that these conflicts had an effect on suicide rates, regardless of any changes in program content or implementation, cannot be ruled out. Military morale is expected to be higher at the start of a conflict, particularly after a domestic attack, but as these 2 conflicts continued, morale may have suffered from a variety of factors, including stop-loss measures that barred service personnel from leaving the military at the end of their enlistments early in the war, the absence of any new attacks in the United States, and the cumulative effects of repeated deployments on military personnel and family members in areas such as relationships and finances. It is beyond the scope of this study to elucidate any contributions from these factors.
The upward spike in suicide rates observed during 2004 (Figure 1) raised important questions about whether the 2 ongoing wars, a decreasing force size, or diminished implementation of the AFSPP had taken its toll upon the program's presumed effectiveness. Our data did not allow us to estimate exactly when implementation efforts diminished; rather, they only gave us a snapshot at the end of 2004, a time when implementation likely had been diminishing for several years in the face of heavy demands from both the Afghanistan and Iraq wars. Regardless, air force leadership felt it was imperative to address the possibility that diminished implementation of the program played a role in the increase in suicide rates and initiated actions to ensure community-wide compliance with all of the components of the program. In 2006, levels of implementation were again measured. When suicide levels in 2004 and 2006 were compared with levels of implementation in 2004 and 2006, it appeared that diminished implementation of the AFSPP may have played a role in the reversal of the program's apparent effectiveness.
The air force now measures compliance with established AFSPP procedures on an annual basis. Organizational capacity for monitoring compliance with the program is now coupled with development of population risk indicators that are used to monitor suicide rates for identification of early shifts in patterns of suicide rates. There are limitations to this approach, but it reflects the importance of close tracking of programmatic activities for reducing deaths from suicide and the critical need to move beyond descriptive, epidemiologic studies of suicide risk.
The AFSPP has been continuously and incrementally improved since its launch, including the adoption of formalized prevention domains in 2004. The measures of implementation that were introduced in 2004 and refined for 2006 represent ongoing continuous quality improvement efforts. Given this drive to enhance effectiveness as rapidly as possible, the 2004 and 2006 measures evaluated the same key implementation prevention domains but were obtained somewhat differently. Although studies have demonstrated that this approach is appropriate when effecting changes in large organizations, it results in incrementally different measures being taken at each time point.6 This is a limitation of the current study when viewed from the perspective of prevention science or therapeutic trials. This limitation is addressed to some degree through the development of theoretical prevention domains that remained constant over time under which the measures were grouped and compared. To date, however, there has been no external validation of these domains and measures. These data are being used as early-generation studies of implementation of a multicomponent suicide prevention program to inform the next generation of implementation studies, which should include such external validation measures.
If the relationship between suicide rates and population size in the air force were linear, as it appears to be when corrected for the intervention effect of the AFSPP, a higher suicide rate would have been expected during the postintervention years (1997–2008), when the air force population was declining. However, we are mindful of the nonsignificant inverse relationship between population size and suicide rate when left uncorrected for the intervention effect, rendering this inference somewhat tentative. We also recognize that a reduction in the number of service members with mental health problems could limit any conclusion regarding a sustainable programmatic impact over time. However, air force–specific data from the Department of Defense Survey of Health Related Behaviors found that, in 1998, 9.5% of air force personnel received mental health care; in 2002, 13.5% received mental health care; and in 2005, 13.3% received mental health care, suggesting that the air force is not decreasing its population of personnel with mental health problems.9–11 It also is worth noting in this regard that the air force encourages early help-seeking behavior for a mental health problem, and 97% of air force personnel who seek mental health care do not experience any negative consequences to their military careers as a result.12
Knowledge about risk factors for suicide includes evidence that aggression, impulsivity, risk-taking, acute and chronic stresses (often including interpersonal or occupational related stress13–18), and alcohol or substance use19,20 are powerfully associated with suicidal behaviors, which are moderated in their expression by gender and age. Despite these compelling data, there has been no reduction in overall suicide rates in the US civilian population since the 1940s, when national rates fell after the Great Depression and during the nation's involvement in World War II. Thus, many policymakers and clinicians remain uncertain whether systematic approaches to reducing deaths from suicide are feasible and effective. The AFSPP is the first long-term sustained effort of its kind to serve as an example of what communities can accomplish in reducing morbidity and mortality attributable to suicidal behaviors if there is ongoing commitment to do so.
Because of the wars in Afghanistan and Iraq, we can expect a large population of combat veterans to experience mental health disorders, and many of these individuals may not seek care. Stigma attached to mental health issues is a pervasive cultural phenomenon in the general US population, and it is even more pronounced in the military. The potential reluctance of military personnel to seek help because of stigma may become particularly significant in light of a recent report based on a prospective study of a US military cohort of 77 047 military active duty, reserve, and National Guard personnel by Smith et al.21 These investigators found that deployed individuals who experienced combat exposure had a 3-fold increase in new onset of self-reported posttraumatic stress disorder. In a study by Boscarino,22 veterans with posttraumatic stress disorder continued to be at heightened risk for suicide 30 years after separation from the service.
These findings highlight the importance of the role of specific combat exposures. It will be critical for clinicians who encounter returning military personnel to be trained to recognize the early risk factors and warning signs of suicidal behaviors, and specifically those associated with combat exposures. Although an earlier study23 carried out among combat-exposed Vietnam veterans found a significant dose–response effect related to being wounded, it is unlikely that many physicians and clinicians are aware of the importance of assessing trauma exposure among those who have served. The larger challenge for communities worldwide is whether the pervasive stigma associated with mental health disorders and psychosocial problems will be overcome as a result of acceptance that these significant, adverse mental health outcomes are a normal human response to the exposures associated with serving in the military.
In conclusion, the US Air Force showed, through its efforts to reduce deaths from suicide, that (1) it is possible to reduce the rate of suicide across a period of years using a multifaceted, overlapping, community-based approach, and (2) reductions in suicide rates cannot be simply maintained by virtue of a program's inherent momentum. Programmatic efforts must be continuously supported and monitored to ensure sustained effects. This may mean that many communities and organizations will not easily be able to launch large-scale suicide prevention efforts on a scale comparable to the AFSPP, especially in developing countries.24 We suspect that there may be real limitations on the feasibility of an exact replication of the AFSPP to other settings. Nevertheless, the enduring public health message from 12 years of this program is that suicide rates can be reduced, and that program success requires interventions to be consistently supported, maintained, and monitored for compliance. This is a message that all communities and organizations worldwide can embrace while considering how to appropriately structure programs and interventions at a local level.
Acknowledgments
This project was supported by National Institute of Mental Health (grants K01 MH055317, R01 MH075017-01A1, and P20 MH071897).
Note. The funding agency was not involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the article.
Human Participant Protection
This study received approval from the institutional review board at the University of Rochester and the Wilford Hall institutional review board for the US Air Force.
References
- 1.Knox KL, Litts DA, Talcott GW, Feig JC, Caine ED. Risk of suicide and related adverse outcomes after exposure to a suicide prevention program in the US Air Force: cohort study. BMJ. 2003;327(7428):1376–1380 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Box GEP, Jenkins GM, Reinsel GC. Time Series Analysis: Forecasting and Control. Hoboken, NJ: John Wiley & Sons; 2008 [Google Scholar]
- 3.SAS Institute SAS/STAT 9.1 User's Guide. Cary, NC: SAS Institute; 2004 [Google Scholar]
- 4.Knox KL, Conwell Y, Caine ED. If suicide is a public health problem, what are we doing to prevent it? Am J Public Health. 2004;94(1):37–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hand DJ. Statistics and the theory of measurement. J R Stat Soc Ser A Stat Soc. 1996;159(3):445–492 [Google Scholar]
- 6.Fayers PM, Hand DJ. Causal variables, indicator variables and measurement scales: an example from quality of life. J R Stat Soc Ser A Stat Soc. 2002;165(2):233–261 [Google Scholar]
- 7.Rychetnik L, Frommer M, Hawe P, Shiell A. Criteria for evaluating evidence on public health interventions. J Epidemiol Community Health. 2002;56(2):119–127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang S, Moss JR, Hiller JE. Applicability and transferability of interventions in evidence-based public health. Health Promot Int. 2005;21(1):76–83 [DOI] [PubMed] [Google Scholar]
- 9.Bray RM, Sanchez RP, Ornstein ML, et al. Department of Defense Survey of Health Related Behaviors Among Active Duty Military Personnel: 1998. Washington, DC: US Dept of Defense; 1999 [Google Scholar]
- 10.Bray RM, Hourani LL, Rae KL, et al. Department of Defense Survey of Health Related Behaviors Among Active Duty Military Personnel: 2002. Washington, DC: US Dept of Defense; 2003 [Google Scholar]
- 11.Bray RM, Hourani LL, Olmsted KL, et al. Department of Defense Survey of Health Related Behaviors Among Active Duty Military Personnel: 2005. Washington, DC: US Dept of Defense; 2006 [Google Scholar]
- 12.Campise RL, Rowan Anderson B. A multisite study of Air Force outpatient behavioral health treatment-seeking patterns and career impact. Mil Med. 2006;171(11):1123–1127 [DOI] [PubMed] [Google Scholar]
- 13.Conner KR, Cox C, Duberstein PR, Tian L, Nisbet PA, Conwell Y. Violence, alcohol, and completed suicide: a case-control study. Am J Psychiatry. 2001;158(10):1701–1705 [DOI] [PubMed] [Google Scholar]
- 14.Beautrais AL, Joyce PR, Mulder RT. Precipitating factors and life events in serious suicide attempts among youths aged 13 through 24 years. J Am Acad Child Adolesc Psychiatry. 1997;36(11):1543–1551 [DOI] [PubMed] [Google Scholar]
- 15.Duberstein PR, Conwell Y, Caine ED. Interpersonal stressors, substance abuse, and suicide. J Nerv Ment Dis. 1993;181(2):80–85 [DOI] [PubMed] [Google Scholar]
- 16.Mahon MJ, Tobin JP, Cusack DA, et al. Suicide among regular-duty military personnel: a retrospective case-control study of occupation-specific risk factors for workplace suicide. Am J Psychiatry. 2005;162(9):1688–1696 [DOI] [PubMed] [Google Scholar]
- 17.Helmkamp JC. Occupation and suicide among males in the US Armed Forces. Ann Epidemiol. 1996;6(1):83–88 [DOI] [PubMed] [Google Scholar]
- 18.Marzuk PM, Nock MK, Leon AC, et al. Suicide among New York City police officers, 1977–1996. Am J Psychiatry. 2002;159(12):2069–2071 [DOI] [PubMed] [Google Scholar]
- 19.Conner KR, Duberstein PR, Conwell Y. Age-related patterns of factors associated with completed suicide in men with alcohol dependence. Am J Addict. 1999;8(4):312–318 [DOI] [PubMed] [Google Scholar]
- 20.Ilgen MA, Harris A, Moos RH, Tiet QQ. Predictors of a suicide attempt one year after entry into substance use disorder treatment. Alcohol Clin Exp Res. 2007;31(4):635–642 [DOI] [PubMed] [Google Scholar]
- 21.Smith TC, Wingard DL, Ryan MA, Kritz-Silverstein D, Slymen DJ, Sallis JF; Millennium Cohort Study Team. Prior assault and posttraumatic stress disorder after combat deployment. Epidemiology. 2008;19(3):505–512 [DOI] [PubMed] [Google Scholar]
- 22.Boscarino JA. Postraumatic stress disorder and mortality among US Army veterans 30 years after military service. Ann Epidemiol. 2006;16(4):248–256 [DOI] [PubMed] [Google Scholar]
- 23.Bullman TA, Kang HK. The risk of suicide among wounded Vietnam veterans. Am J Public Health. 1996;86(5):662–667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hawton K, van Heeringen K. Suicide. Lancet. 2009;373(9672):1372–1381 [DOI] [PubMed] [Google Scholar]