Abstract
Objectives. We examined whether adding behavioral weight loss strategies could improve the outcomes of a community weight loss campaign.
Methods. Shape Up RI is a 12-week, online, team-based program for health improvement in Rhode Island. In study 1, we randomly assigned participants to the standard Shape Up RI program or to the program plus video lessons on weight loss. In study 2, we randomly assigned participants to the standard program or to the program plus video lessons; daily self-monitoring of weight, eating, and exercise; and computer-generated feedback.
Results. Adding video lessons alone (study 1) did not result in significantly improved weight loss (2.0 ±2.8 kg vs 1.4 ±2.9 kg; P = .15). However, when the video lessons were supplemented with self-monitoring and feedback (study 2), the average weight loss more than doubled (3.5 ±3.8 kg vs 1.4 ±2.7 kg; P < .01), and the proportion of individuals achieving a weight loss of 5% or more tripled (40.5% vs 13.2%; P < .01). Participants in study 2 submitted self-monitoring records on 78% of days, and adherence was significantly related to outcome.
Conclusions. Adding behavioral strategies to community campaigns may improve weight loss outcomes with minimal additional cost.
Given the increasing prevalence of overweight and obesity, it is critical to find cost-effective ways to provide assistance with weight loss to large numbers of individuals. Intensive lifestyle interventions that combine diet, exercise, and behavioral strategies typically produce average weight losses of 7% to 10% of initial body weight (7–10 kg) after approximately 6 to 12 months of treatment1,2 and markedly improve obesity-related comorbidities.3–5 However, intensive lifestyle programs are expensive to administer, are time-intensive, and are accessible to only a small minority of the overweight and obese population.
Community weight loss campaigns offer the opportunity to reach large numbers of overweight and obese individuals and engage them in weight loss efforts. Several studies done in the 1980s suggested the potential of team-based competitions for weight loss.6–9 Recently, there has been a resurgence of interest in such team-based approaches, which are now offered on a larger scale via the Internet. A recent example is Shape Up RI (available at www.shapeupri.org), a self-sustaining, annual community campaign designed to help Rhode Islanders lose weight and increase their physical activity through an online, team-based competition. Shape Up RI, like other similar campaigns, is impressive in its ability to reach and retain large numbers of overweight and obese individuals at minimal cost; however, the weight loss outcomes are modest compared with face-to-face programs1,2 and earlier worksite competitions.3–6 For example, in the 2007 Shape Up RI campaign the 4717 participants in the weight loss component averaged a 3.2 kg weight loss.10 The challenge moving forward is to maximize the weight losses achieved in this new generation of community-based campaigns without substantially increasing participant burden or delivery cost.
Intensive lifestyle programs are derived from social learning theory.11 These programs have been used in recent clinical trials including Look AHEAD and the Diabetes Prevention Program.1,2 A structured protocol of weekly lessons is available online.12 Typically, these programs are delivered face-to-face with weekly group or individual meetings for 6–12 months. Key components of these programs include clearly defined goals for weight loss, diet, and physical activity and self-monitoring of these parameters. In addition, social learning theory emphasizes the importance of changing physical, social, and emotional cues that may act as barriers to adopting new behaviors and developing positive reinforcers to sustain new behaviors.
In the present 2-part study, we tested the efficacy of incorporating key components of intensive lifestyle programs into the Shape Up RI program. In study 1, we tested the hypothesis that providing participants with the content of the Diabetes Prevention Program behavioral weight loss lessons delivered via the Internet would improve treatment outcomes. In study 2, we tested an enhanced intervention, involving not only Internet behavioral weight loss lessons but also regular self-monitoring of diet, activity, and body weight and automated feedback on this self-monitoring that recommended strategies for overcoming barriers and provided positive reinforcement for behavior change. Primary outcomes were weight loss at the end of the 12-week program and the proportion of participants losing at least 5% of their initial weight. Secondary outcomes were calories expended in physical activity, frequency of self-weighing, and adherence to other prescribed behavioral strategies.
METHODS
The Shape Up RI program delivered in 2008 and 2009 was a 12-week, statewide, Internet-based community program that used team-based competition to encourage increased physical activity and weight loss. Participants enrolled in teams of 5 to 11 individuals and had the opportunity to compete on steps walked, minutes of activity, and weight loss. Participants received a pedometer, a wristband to show their involvement, a paper logbook, and access to the Shape Up RI Web site, through which they submitted their data at the end of each round (every 2 weeks). Although Shape Up RI encouraged its participants to set goals and use their team for support, the program provided no training in behavioral strategies. Wing et al. provide additional details regarding the Shape Up RI program.10
Recruitment
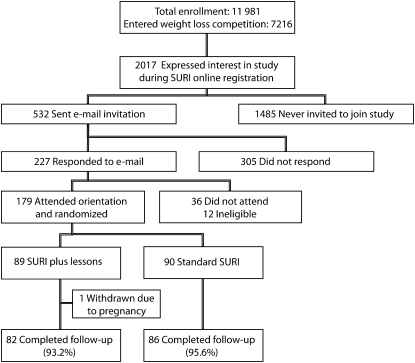
We recruited participants for study 1 and study 2 during online enrollment for the Shape Up RI 2008 and 2009 competitions, respectively. For study 1 registration process 7216 of the 11 981 participants chose the weight loss competition, and 2017 expressed interest in participating in a weight loss research study. In 2009, a total of 13 088 individuals enrolled in Shape Up RI, with 9211 entering the weight loss competition. Of these, 2141 expressed interest in our study. Because we were pilot-testing new procedures, we invited only the first 532 persons who expressed interest in 2008 and the first 702 persons in 2009 to attend the study orientation. Participant flow from this point on is depicted in Figure 1.
FIGURE 1.
Flow of participants in study 1: Shape Up RI (SURI), 2008–2009.
Participants
Participants were required to have enrolled in the Shape Up RI weight loss competition, to be older than 18 years, and to have a body mass index (BMI; weight in kilograms divided by height in meters squared) of 25 kg/m2 or greater. Participants in study 1 were strongly encouraged to recruit fellow team members to join the study, whereas in study 2, less emphasis was placed on enrolling with other teammates.
A total of 179 individuals (149 women and 30 men) from 70 teams participated in study 1. At baseline, the participants averaged 46.5 (SD = 10.1) years of age and had a BMI of 33.8 (SD = 6.3); their initial weight averaged 92.0 kg (SD = 19.2). The majority of participants (68.7%) held a college degree or higher, and 87.7% self-identified as White.
A total of 128 individuals (115 women and 13 men) from 97 teams participated in Study 2. At baseline, the average age of participants was 46.9 (SD = 9.7) years and their average BMI was 33.9 (SD = 5.6); their initial weight averaged 92.0 kg (SD = 17.8). Similar to study 1 participants, most study 2 participants (63.2%) held a college degree or higher, and 88.3% self-identified as White.
Design
The aim of study 1 was to determine whether providing weekly lessons teaching behavioral strategies for changing diet and exercise to Shape Up RI participants would improve their weight loss results. The study participants were randomly assigned with their teammates to 1 of 2 groups: Shape Up RI plus lessons (SURI+lessons; n = 89) or standard Shape Up RI (n = 90).
Study 2 examined the effects of the combination of multimedia lessons plus increased self-monitoring and automated computer feedback on behavior changes and weight loss in the Shape Up RI program. Because we previously reported that providing individualized feedback to participants on their self-monitoring record improved weight loss in an Internet-based program,13 we hypothesized that this enhanced program would improve adherence to behavioral strategies and weight loss outcomes in the Shape Up RI program. However, key questions were whether participants in a community-based intervention would be willing to complete intensive self-monitoring and whether the enhanced intervention could work in this setting. To test these questions, participants in study 2 were randomly assigned with their teammates to 1 of 2 groups: Shape Up RI enhanced (n = 82) or standard Shape Up RI (n = 46). A 2:1 randomization ratio was used to provide greater sample size in the experimental condition. To ensure that all participants could use the Shape Up RI Web site and complete a basic self-monitoring task, the participants were asked to keep a 4-day food diary and to answer simple questions via the Internet before qualifying for randomization.
Interventions
For both study 1 and study 2, the standard Shape Up RI groups had access to all of the components of the intervention. In addition, members of both standard groups received an e-mail with a directory of publicly available Web sites with information similar to the multimedia lessons that were used in the SURI+lessons group (study 1). No further contact took place until the follow-up assessment.
Members of the SURI+lessons group in study 1 were given access to weekly multimedia lessons that were based on the Diabetes Prevention Program.1 The lessons included information and instructions regarding nutrition, physical activity, and behavioral change. The lessons recommended a weight loss goal of 1 to 2 pounds per week, a calorie intake goal of 1200 to 1500 calories per day for those weighing less than 200 pounds and 1500 to 1800 calories per day for participants weighing more than 200 pounds, and a gradually increasing physical activity goal, with 100 minutes per week during the first 3 weeks, 150 minutes per week during weeks 4 to 7, and finally 200 minutes per week during weeks 8 to 12. Specific behavioral strategies such as self-monitoring of eating and physical activity, reducing dietary fat intake, problem solving, and stimulus control were taught and emphasized during the lessons.
The multimedia lessons contained an animated PowerPoint (Microsoft, Redmond, WA) presentation that was narrated by study staff members with expertise in the lesson's content. The presentations ranged from 10 to 20 minutes and included some opportunities for interaction (e.g., quizzes on lesson content). Links to supporting documents created by study staff and links to Web sites with related information were also provided. A new lesson was made available each week, and the participants were allowed unlimited viewing of previous lessons.
For the Shape Up RI enhanced program in study 2, the participants attended a group session held 1 to 2 weeks before the Shape Up RI competition that provided a brief introduction to the concept of energy balance and the importance of self-monitoring their diet and exercise. Participants were given printed food diaries and a calorie reference book to use for self-monitoring and were shown the procedures for submitting their self-monitoring data online. Program goals were presented, and the participants were informed that they would receive online feedback during the program.
A set of multimedia lessons similar to those used in study 1 (the SURI+lessons group) were used in study 2 (the Shape Up RI enhanced group). A few additional opportunities for interactivity were added, and the longer lessons were reduced to 15 minutes or less. Additionally, the participants were instructed to report their daily weight, calories and fat grams, steps, and exercise minutes via the Shape Up RI Web site (the data could be submitted daily or once per week but included daily information). Computer-automated feedback was provided weekly in response to these data. This feedback was based on that used in Tate et al.13 and was designed to be supportive to the participant. The feedback message commented on the participant's weight loss, calorie intake, and exercise minutes relative to the prescribed goals. If the participant was not meeting the suggested goals, the message included suggestions to help him or her reach that goal.
Assessments
Assessments were identical for studies 1 and 2 and took place at baseline and at the end of the 12-week Shape Up RI competition. The assessors were blind to treatment assignment. The participants were weighed on a digital scale at each assessment, and height was measured at baseline by use of a wall-mounted stadiometer. The participants also completed a demographic questionnaire (baseline only) and the Paffenbarger Physical Activity Questionnaire,14 which provides an estimate of calories expended per week in physical activity. An additional questionnaire assessed the use (yes or no) of 20 healthy-weight-control strategies over the past month for the purpose of weight control. The 20 strategies included dietary, physical activity, and behavioral strategies (e.g., decrease fat intake, increase exercise, and cut out between-meal snacking). The 20 items on this scale had high internal consistency (Chronbach α = 0.77). A total score was calculated to represent the total number of strategies used. A subset of 5 items was used to assess adherence to the core weight loss strategies described in the multimedia lessons used in both the SURI+lessons and Shape Up RI enhanced groups. The participants also completed a single item about their frequency of self-weighing, with response options ranging from “never” to “several times per day.” In addition, both the SURI+lessons and Shape Up RI enhanced groups were asked to indicate how many lessons they had viewed by using the following categories: 0, 1 to 3, 4 to 6, 7 to 9, or 10 to 12.
Statistical Analyses
Data analyses were conducted by using the Statistical Package for the Social Sciences, version 14.0 (SPSS for Windows, SPSS, Chicago, IL), and SAS, version 9.1 (SAS Institute Inc, Cary, NC). Primary outcome analyses tested the hypothesis that compared with the standard Shape Up RI group, the SURI+lessons group or the Shape Up RI enhanced group had (1) significantly greater weight losses and (2) a significantly greater proportion of individuals achieving a weight loss of at least 5% at the end of the competition. We used analysis of variance (ANOVA) and logistic regression, respectively. Separate analyses were conducted for completers only and for intent-to-treat with baseline values carried forward for dropouts. The results did not differ when the data were analyzed via linear mixed models that included the effect of team membership. The simpler ANOVA models are reported for ease of interpretation.
Secondary analyses used Pearson correlations to examine the association between measures of adherence and weight loss within the Shape Up RI enhanced group (study 2). Changes in the use of specific behavioral strategies (yes or no) from baseline to the end of treatment were analyzed within treatment group by using the χ2 test and between groups over time by using generalized estimating equations as implemented in SAS 9.1 PROC GENMOD. All tests were 2-tailed with α = .05. All variables were normally distributed, except for physical activity, which was log transformed for analysis.
RESULTS
At baseline in study 1, we found no significant differences between the treatment groups for any measured variable. A total of 168 participants (93.9%) returned for the postprogram assessment, with no significant difference in retention between the SURI+lessons group (93.2%) and the standard Shape Up RI group (95.6%; χ21, 179 = 0.91; P = .34).
Adherence to the Shape Up RI program, as indicated by submission of weight data at baseline and at the end of each of the 6 rounds (a total of 7 possible biweekly submissions), was excellent among both groups and did not differ significantly between them (participants in the SURI+lessons group reported their weights on 6.2 [SD = 1.6] rounds, and participants in the standard Shape Up RI group reported weights on 5.9 [SD = 2.0] rounds [t177 = 1.02; P = .31; d = 0.15]. In addition, 56.8% of participants in the SURI+lessons group reported watching more than half of the 12 lessons, and 32.1% watched at least 10 of the 12 videos.
Changes in the primary outcomes over the 12-week program are reported in Table 1. Weight losses and the proportion of participants losing at least 5% of their starting weight were both slightly greater among the SURI+lessons group than among the standard Shape Up RI group, but these differences were not significant in either the completers-only or intent-to-treat analyses. The changes in secondary outcome measures for the 2 groups are shown in Table 2. As shown, both groups reported increases in physical activity of approximately 800 kcal per week and increased use of many of the core behavioral strategies. However, there were no significant differences between the 2 groups for changes in use of specific behavioral strategies or the overall number of strategies used.
TABLE 1.
Weight Loss Outcomes of Participants in Studies 1 and 2: Shape Up RI (SURI), 2008–2009
| Study 1 |
Study 2 |
|||||
| Standard SURI, No., Mean ±SD, or % | SURI Plus Lessons, No., Mean ±SD, or % | P | Standard SURI, No., Mean ±SD, or % | SURI Enhanced, No., Mean ±SD, or % | P | |
| Completers only | ||||||
| No. | 86 | 82 | 38 | 74 | ||
| Weight loss, kg | 1.4 ±2.9 | 2.0 ±2.8 | .15 | 1.4 ±2.7 | 3.5 ±3.8 | < .01 |
| Weight loss, % of initial weight | 1.6 ±3.3 | 2.2 ±3.1 | .17 | 1.6 ±3.2 | 4.0 ±4.4 | < .01 |
| Participants losing > 5% of initial weight, % | 11.6 | 18.3 | .23 | 13.2 | 40.5 | < .01 |
| Intent-to-treat analysis | ||||||
| No. | 90 | 89 | 46 | 82 | ||
| Weight loss, kg | 1.3 ±2.9 | 1.9 ±2.8 | .20 | 1.2 ±2.5 | 3.1 ±3.7 | < .01 |
| Weight loss, % of initial weight | 1.5 ±3.2 | 2.1 ±3.0 | .22 | 1.4 ±3.0 | 3.6 ±4.4 | < .01 |
| Participants losing > 5% of initial weight, % | 11.1 | 16.9 | .27 | 11.1 | 36.6 | < .01 |
Note. Standard SURI is the standard SURI program; SURI plus lessons is the standard SURI program plus video lessons; SURI enhanced is the standard SURI program plus video lessons and daily self-monitoring of behaviors with automated feedback.
TABLE 2.
Use of Behavioral Strategies by Participants Before and After the Program for Studies 1 and 2 (Completers Only): Shape Up RI (SURI), 2008–2009
| Standard SURI |
SURI Plus Lessons (Study 1) or SURI Enhanced (Study 2) |
||||
| Before, Mean ±SD or % | After, Mean ±SD or % | Before, Mean ±SD or % | After, Mean ±SD or % | Time x Group, P | |
| Study 1 | |||||
| Exercise,a kcal/wk | 984 ±1077 | 1718 ±1762 | 1258 ±1437 | 2009 ±1949 | .74 |
| Total no. of strategies | 5.9 ±3.6 | 8.6 ±3.8 | 6.3 ±3.5 | 9.5 ±3.7 | .39 |
| Self-weighing daily | 18.6 | 21.2 | 23.2 | 30.4 | .66 |
| Use of specific strategies | |||||
| Graph weight | 5.8 | 15.3 | 12.2 | 23.2 | .90 |
| Reduce calorie intake | 57.0 | 71.8 | 61.0 | 81.7 | .28 |
| Record intake daily | 18.6 | 25.9 | 23.2 | 36.6 | .46 |
| Count calories | 17.4 | 32.9 | 23.2 | 47.6 | .61 |
| Record exercise daily | 14.0 | 51.8 | 17.1 | 47.6 | .44 |
| Study 2 | |||||
| Exercise,a kcal/wk | 1071 ±931 | 1565 ±1206 | 1435 ±1771 | 2769 ±2506 | .08 |
| Total no. of strategies | 5.0 ±4.5 | 8.3 ±3.3 | 6.8 ±3.6 | 12.0 ±4.2 | .03 |
| Self-weighing daily | 20.0 | 28.9 | 12.2 | 67.6 | < .01 |
| Use of specific strategies | |||||
| Graph weight | 17.8 | 23.7 | 7.3 | 44.6 | < .01 |
| Reduce calorie intake | 53.3 | 68.4 | 68.3 | 87.8 | .35 |
| Record intake daily | 22.2 | 26.3 | 18.3 | 75.7 | < .01 |
| Count calories | 15.6 | 26.3 | 15.9 | 79.7 | < .01 |
| Record exercise daily | 8.9 | 47.4 | 7.3 | 68.9 | .19 |
Note. Standard SURI is the standard SURI program; SURI plus lessons (study 1 only) is the standard SURI program plus video lessons; SURI enhanced (study 2 only) is the standard SURI program plus video lessons and daily self-monitoring of behaviors with automated feedback.
Because of positive skew, analysis was performed on log-transformed values.
Study 2
At baseline in study 2, there were no significant differences between the treatment groups for any measured variable. Of the 128 participants randomly assigned at baseline, 112 (87.5%) returned for the postprogram follow-up assessment, with no significant difference in retention between the Shape Up RI enhanced group (90.2%) and the standard Shape Up RI group (84.4%; χ21,127 = 0.94; P = .33).
Adherence to the program was excellent. Participants in the Shape Up RI enhanced and standard Shape Up RI groups reported their weights on an average of 5.9 (SD = 1.8) and 5.6 (SD = 2.0) of the 7 rounds, respectively. In addition, participants in the Shape Up RI enhanced group reported their weights on 65.1 (SD = 28.4) of the 84 days (or 78% of days) and reported their calorie intake on 62.2 (SD = 29.9) of the 84 days (or 74%). It is striking that 48% of the participants in the Shape Up RI enhanced group reported their intake and 59% reported their weight every single day for 84 days. We also found that 65% of participants watched 7 or more of the 12 multimedia lessons and 50% reported viewing at least 10 lessons.
As shown in Table 1, weight losses for participants in Shape Up RI enhanced participants were significantly greater than for standard Shape Up RI participants over the 12-week program (3.5 ±3.8 kg vs 1.4 ±2.7 kg; t110 = 3.082; P < .01; d = 0.62), and a greater proportion of Shape Up RI enhanced participants lost at least 5% of their starting weight (40.5% vs 13.2%; b = 1.50; SE = 0.54; OR = 4.50; P < .01). Similar results were obtained in intent-to-treat analyses. In addition, participants in the Shape Up RI enhanced group reported greater increases in physical activity, daily self-weighing, and other healthy-weight-control strategies (Table 2).
Weight loss among the Shape Up RI enhanced group was related to the number of days of calorie and weight reporting and the number of lessons viewed (r values 0.43, 0.42, and 0.47, respectively; all P < .01) and to posttreatment levels of physical activity (r = 0.26; P < .05), number of weight control strategies used (r = 0.35; P < .01), and frequency of self-weighing (r = 0.55; P < .01). Weight loss among the standard Shape Up RI group was not significantly related to any of these behavior changes.
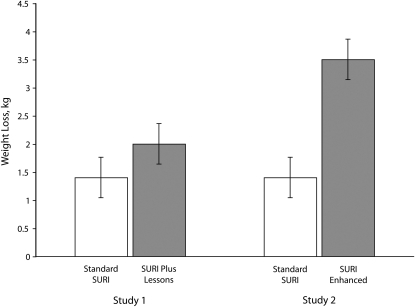
Study Comparison
The weight losses observed in study 1 and study 2 are depicted together in Figure 2. The addition of video lessons in study 1 resulted in a minor nonsignificant increase in weight loss, whereas the addition of video lessons and self-monitoring with automated feedback resulted in a large significant increase in weight loss compared with that of the standard Shape Up RI program.
FIGURE 2.
Weight loss of participants in study 1 and study 2: Shape Up RI (SURI), 2008–2009.
Note. Study 1 compares the standard SURI program with the SURI program plus video lessons. Study 2 compares the standard SURI program with the SURI program plus video lessons, daily self-monitoring of behaviors, and automated feedback.
DISCUSSION
The primary finding from these studies is that adding multimedia lessons, self-monitoring, and automated feedback to the Shape Up RI program significantly increased the average weight losses achieved and the percentage of participants losing 5% or more of their starting weight in this community-based intervention. The Shape Up RI enhanced intervention that included these 3 components produced an average weight loss of 3.5 kg compared with 1.4 kg for those in the standard Shape Up RI group and tripled the percentage of participants who lost at least 5% of their body weight (40.5% vs 13.2%). Notably, adding lessons alone did not appear to sufficiently improve outcomes.
Our findings suggest that the success of the Shape Up RI enhanced group was at least partially attributable to the superior adherence to the healthy-weight-control behaviors recommended in the multimedia lessons. The present study could not identify which component of the Shape Up RI enhanced strategy was most important, but it is likely that each component of the strategy exerted an effect on the others, such that the automated feedback in study 2 appeared to have increased the number of lessons viewed and the use of strategies recommended in these lessons. We also assume that the provision of feedback increased the likelihood that the participants would self-monitor their behaviors. Moreover, each of these behaviors was related to improved weight losses.
Our study may provide a model for a cost-effective community approach to weight control. Although the weight losses achieved in these studies were much smaller than those typically seen in face-to-face clinic-based programs, the advantage of programs such as Shape Up RI is their ability to attract large numbers of participants. Many of the Shape Up RI participants expressed interest in joining our study and receiving the additional assistance with weight loss, and those who joined our program were similar to the Shape Up RI cohort as a whole (data not shown). The multimedia lessons and automated feedback that were added in the enhanced program can be added to Internet-based community programs with little additional cost and can be offered to large numbers of participants. Although previous studies have shown that regular self-monitoring is a critical element for weight loss success,15,16 we were concerned about adherence in a community-based program. Thus, our finding that 58% of the participants sent in their weight and 49% sent in their caloric intake every day for 84 days was encouraging. Retention of this cohort in these studies was also excellent.
Although our results suggest that the Shape Up RI enhanced intervention was superior to the SURI+lessons program, we note that the 2 interventions were not directly compared in a single randomized trial. However, the comparison between these 2 interventions was facilitated by the fact that the standard Shape Up RI program remained quite similar from 2008 to 2009, and the outcomes for the standard group were almost identical across the 2 pilots (mean weight loss of 1.4 kg and 11.1% achieving the 5% weight loss goal in both study 1 and study 2). The findings reported here were also limited by the small number of study participants; by the mostly female, college-educated, and White sample; and by the lack of data on whether such participants are particularly responsive to Internet interventions.17 Finally, this study evaluated only the short-term effects of the intervention; future studies are needed to determine whether adding these components would also improve longer-term results.
As noted above, behavioral weight loss programs are typically presented in a face-to-face format, with weekly lessons, following a structured protocol. There have been efforts to disseminate these behavioral weight loss approaches through community settings, such as the YMCA18 and through the Internet.19,20 However, such studies have typically been focused on the individual participant, not on broader communities of overweight and obese participants. Alternatively, a few community-based weight loss programs have delivered basic educational material about diet and exercise via the Internet,21 but the educational materials were not based on structured behavioral programs. We are not aware of any previous studies that have systematically examined the effects of adding specific behavioral weight loss components such as lessons and feedback to community-based weight loss programs.
In conclusion, community-based programs such as Shape Up RI are an effective approach to reaching large numbers of participants who are attempting to lose weight and to providing them with social support and an organized program. However, our studies suggest that weight losses in such programs could be significantly improved by incorporating training in behavioral skills, through multimedia lessons, and by providing automated feedback in response to participants' self-monitoring. Such additional components can be offered to large numbers of participants without increasing the cost of the intervention and can result in almost a 3-fold greater weight loss.
Human Participant Protection
All procedures were approved by The Miriam Hospital institutional review board and all participants provided written informed consent.
References
- 1.Diabetes Prevention Program Research Group Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346(6):393–403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Look AHEAD Research Group Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the look AHEAD trial. Diabetes Care. 2007;30(6):1374–1383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldstein DJ. Beneficial health effects of modest weight loss. Int J Obes Relat Metab Disord. 1992;16(6):397–415 [PubMed] [Google Scholar]
- 4.Pi-Sunyer FX. A review of long-term studies evaluating the efficacy of weight loss in ameliorating disorders associated with obesity. Clin Ther. 1996;18(6):1006–1035 [DOI] [PubMed] [Google Scholar]
- 5.National Task Force on the Prevention and Treatment of Obesity Overweight, obesity and health risk. Arch Intern Med. 2000;160(7):898–904 [DOI] [PubMed] [Google Scholar]
- 6.Wing RR, Epstein LH. A community approach to weight control: The American Cancer Society Weight-A-Thon. Prev Med. 1982;11(2):245–250 [DOI] [PubMed] [Google Scholar]
- 7.Cohen RY, Stunkard AJ, Felix MRJ. Comparison of three worksite weight-loss competitions. J Behav Med. 1987;10(5):467–479 [DOI] [PubMed] [Google Scholar]
- 8.Brownell KD, Cohen RY, Stunkard AJ, Felix MRJ, Cooley NB. Weight loss competitions at the work site: impact on weight, morale and cost-effectiveness. Am J Public Health. 1984;74(11):1283–1285 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stunkard AJ, Cohen RY, Felix MR. Weight loss competitions at the worksite: how they work and how well. Prev Med. 1989;18(4):460–474 [DOI] [PubMed] [Google Scholar]
- 10.Wing RR, Pinto AM, Crane MM, Kumar R, Weinberg BM, Gorin AA. A statewide intervention reduces BMI in adults: Shape Up Rhode Island results. Obesity (Silver Spring). 2009;17(5):991–995 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bandura A. Social learning theory. Englewood Cliffs, NJ: Prentice-Hall; 1977 [Google Scholar]
- 12.Diabetes Prevention Program Diabetes Prevention Program lifestyle materials for sessions 1-16: lifestyle coach materials and optional participant handouts. Available at: http://www.bsc.gwu.edu/dpp/lifestyle/dpp_dcor.html. Accessed August 13, 2010
- 13.Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an Internet weight loss program. Arch Intern Med. 2006;166(15):1620–1625 [DOI] [PubMed] [Google Scholar]
- 14.Paffenbarger RS, Wing AL, Hyde RT. Physical activity as an index of heart attack risk in college alumni. Am J Epidemiol. 1978;108(3):161–175 [DOI] [PubMed] [Google Scholar]
- 15.Guare JC, Wing RR, Marcus MD, Epstein LH, Burton LR, Gooding WE. Analysis of changes in eating behavior and weight loss in type II diabetic patients. Diabetes Care. 1989;12(7):500–503 [DOI] [PubMed] [Google Scholar]
- 16.Baker RC, Kirschenbaum DS. Weight control during the holidays: highly consistent self-monitoring as a potentially useful coping mechanism. Health Psychol. 1998;17(4):367–370 [DOI] [PubMed] [Google Scholar]
- 17.Wantland DJ, Portillo CJ, Holzemer WL, Slaughter R, McGhee EM. The effectiveness of Web-based vs. non-Web-based interventions: a meta-analysis of behavioral change outcomes. J Med Internet Res. 2004;6(4):e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Finch EA, Kelly MS, Marrero DG, Ackermann RT. Training YMCA wellness instructors to deliver an adapted version of the Diabetes Prevention Program lifestyle intervention. Diabetes Educ. 2009;35(2):224–228, 232 [DOI] [PubMed] [Google Scholar]
- 19.Tate DF, Wing RR, Winett RA. Using internet technology to deliver a behavioral weight loss program. JAMA. 2001;285(9):1172–1177 [DOI] [PubMed] [Google Scholar]
- 20.Gold BC, Burke S, Pintauro S, Buzzell P, Harvey-Berino J. Weight loss on the web: a pilot study comparing a structured behavioral intervention to a commercial program. Obesity (Silver Spring). 2007;15(1):155–164 [DOI] [PubMed] [Google Scholar]
- 21.Carter-Edwards L, Bastian LA, Schultz M, Amamoo MA, Ostbye T. An internet-based weight loss intervention initiated by a newspaper. Prev Chronic Dis. 2009;6(3):A101. [PMC free article] [PubMed] [Google Scholar]