Abstract
Objectives. We aimed to determine the percentage of suicide attempts attributable to individual Axis I and Axis II mental disorders by studying population-attributable fractions (PAFs) in a nationally representative sample.
Methods. Data were from the National Epidemiologic Survey on Alcohol and Related Conditions Wave 2 (NESARC; 2004–2005), a large (N = 34 653) survey of mental illness in the United States. We used multivariate logistic regression to compare individuals with and without a history of suicide attempt across Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, Axis I disorders (anxiety, mood, psychotic, alcohol, and drug disorders) and all 10 Axis II personality disorders. PAFs were calculated for each disorder.
Results. Of the 25 disorders we examined in the model, 4 disorders had notably high PAF values: major depressive disorder (PAF = 26.6%; 95% confidence interval [CI] = 20.1, 33.2), borderline personality disorder (PAF = 18.1%; 95% CI = 13.4, 23.5), nicotine dependence (PAF = 8.4%; 95% CI = 3.4, 13.7), and posttraumatic stress disorder (PAF = 6.3%; 95% CI = 3.2, 10.0).
Conclusions. Our results provide new insight into the relationships between mental disorders and suicide attempts in the general population. Although many mental illnesses were associated with an increased likelihood of suicide attempt, elevated rates of suicide attempts were mostly attributed to the presence of 4 disorders.
With almost 1 million deaths worldwide every year and a rate increase of 60% over the past 45 years, suicide is clearly a major public health problem.1 Although the US Surgeon General has prioritized suicide prevention,2 suicidal behavior has not significantly decreased in the United States.3 Suicide attempts are strong risk factors for eventual suicide completion4–6; therefore, understanding and modifying risk factors for suicide attempts remain a promising approach to reducing suicide rates.
Unfortunately, our understanding of the risk factors for suicide attempts is plagued by poor specificity. Vigorous study efforts have identified multiple risk factors, including several sociodemographic factors and mental disorders.3,7–10 However, significant associations between candidate risk factors and suicide attempts are tempered by low positive predictive values.11 The population-attributable fraction (PAF; also known as the population-attributable risk) has emerged as a promising statistical tool to better quantify the effect of risk factors on a given outcome at the population level. The PAF describes the reduction in incidence of a particular outcome if the entire population was not exposed to the examined risk factor.12
The PAF has been underused in the study of suicide risk factors.13,14 A recent review of the PAF in suicide research15 showed that existing studies examining the PAFs of risk factors for suicide attempts have focused primarily on depression and mood disorders, with PAFs ranging from 28% to 74%.14,16–21 A small number of studies have investigated the PAFs of substance use disorders and anxiety disorders for suicide attempts, also with mixed findings.14,18,22 Other findings suggest that the risk of suicide attempts attributable to mental disorders is largely explained by the association between mental disorders and suicidal ideation.9 A major limitation in the literature is that relatively few mental disorders have been examined by using PAFs for suicide attempts. Despite substantial evidence for the causative role of personality disorders in suicidal behavior,23–25 the PAF of personality disorders has been examined in only 1 study to date, and that study was unable to examine the effects of individual personality disorders.18 Borderline personality disorder is a strong risk factor for suicide attempts,25 yet the PAF of borderline personality disorder for suicide attempts is unknown. Posttraumatic stress disorder (PTSD) is another disorder associated with suicide attempts,26,27 yet the proportion of suicide attempts attributable to PTSD has not been examined. Furthermore, many previous studies included limited adjustment for confounding factors. Even though several mental disorders have been labeled as risk factors for suicidal behavior,7 many studies using the PAF do not adjust for mental disorders other than the disorder of interest. The PAF is based on the assumption that the examined risk factor is causally related to the outcome,12 and given the high rates of comorbidity of mental disorders,28 multivariate models examining a comprehensive range of mental disorders are needed to provide a more realistic assessment of the PAF for a specific mental illness.
Our primary objective was to examine the proportion of suicide attempts attributable to specific mental disorders. To address the limitations of the existing literature, we used the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC),29 wave 2, as the data set. This data set features a very large sample size (N = 34 653), includes a comprehensive assessment of Axis I disorders and all 10 Axis II personality disorders, and is representative of the US population. On the basis of existing literature showing high PAF values for major depressive disorder and other mood disorders, we hypothesized that whereas several mental disorders would be independently associated with suicide attempts, major depressive disorder and other mood disorders would account for the highest proportion of suicide attempts.16,21 We further hypothesized that anxiety and substance use disorders would have lower PAF values for suicide attempts, on the basis of previous studies that often showed lower PAF values.14,18,22 The limited literature on the PAFs of personality disorders for suicide attempts suggested that we would find low PAF values; however, because of its consistently demonstrated association with suicide attempts, we anticipated that borderline personality disorder would have a relatively high PAF value.
METHODS
We used data from the NESARC, which was designed by the National Institute on Alcohol Abuse and Alcoholism.30,31 This survey is a large, nationally representative data set that sampled the noninstitutionalized adult US population. The NESARC featured 2 waves of assessment: wave 1 (2001–2002) and wave 2 (2004–2005). Of the 43 093 individuals assessed in wave 1, a total of 34 653 were reassessed at wave 2. The wave 2 sample was the primary data source for this study. All variables used in the study came from the wave 2 assessment, with the exception of certain personality disorders that were assessed only at wave 1 (see the “Measures” section). Trained lay interviewers administered both waves of the NESARC survey via in-person interviews. Only those respondents who completed both waves of the survey were included in the final sample, yielding an overall response rate for both waves of 70.2%. Before data collection, each respondent was informed of the nature of the survey and its potential uses, was assured of confidentiality, and was told that participation was voluntary. The US Census Bureau and the US Office of Management and Budget reviewed and approved the ethics protocol. Statistical weights were used to ensure representativeness of the sample. Detailed information about the NESARC sampling frame has been presented elsewhere.31–33
Measures
Eight sociodemographic variables were assessed in both waves of the NESARC survey: income, race/ethnicity, education level, marital status, age, gender, region, and urban status (urbanicity). Income was divided into 4 categories ($0–$19 999, $20 000–$34 999, $35 000–$59 999, and ≥ $60 000), as were age (20–29, 30–44, 45–64, and ≥ 65 years) and region (Northeast, Midwest, South, and West). Racial/ethnic identity was divided into 5 categories: White, Black, American Indian or Alaskan, Asian or Hawaiian, and Hispanic. Marital status was defined as 1 of the following 3: married or cohabitating; divorced, separated, or widowed; or never married. Education was similarly trichotomized into less than high school, high school only, and some college or higher.
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnoses were made by using the Alcohol Use Disorders and Associated Disabilities Interview Schedule IV (AUDADIS-IV).34 The reliability and validity of this instrument range from good to excellent and have been examined in detail elsewhere.30,33,35 For our study, we included lifetime mental disorder diagnoses including mood disorders (major depressive disorder, dysthymic disorder, and bipolar I and bipolar II disorders), anxiety disorders (panic disorder, social phobia, specific phobia, PTSD, and generalized anxiety disorder), and substance use disorders (alcohol abuse and dependence, drug abuse and dependence, and nicotine dependence). Psychotic disorders were assessed with the following question: “Did a doctor or other health professional ever diagnose you with schizophrenia or psychotic illness or episode?” Positive responses were assigned a diagnosis of schizophrenia or psychotic illness or episode. Studies have found this self-report method to yield prevalence rates similar to what is expected in North America and therefore appropriate for use.36,37 We also assessed all 10 Axis II personality disorders. Seven of the personality disorders were diagnosed at Wave 1 (avoidant, antisocial, dependent, obsessive-compulsive, paranoid, schizoid, and histrionic) and the remaining 3 (schizotypal, borderline, and narcissistic) were assessed at wave 2. All Axis I disorders were assessed at both waves with the exception of PTSD, which was assessed only at wave 2. Diagnoses were categorical, meaning that to receive a diagnosis, participants had to endorse the minimum number of symptoms required by the DSM-IV.
Past-year physical disability was assessed with the following item: “During the last 12 months, did you have a serious PERMANENT physical disability? Do not include serious TEMPORARY physical disabilities.” Seventeen medical conditions were also assessed in the NESARC survey. These included conditions such as high cholesterol, diabetes, liver disease, and AIDS. On the basis of previous research, we computed a summary comorbidity variable by assigning a specific weight to each condition (e.g., “6” for AIDS, “1” for high cholesterol). We then summed the weight scores of all conditions38,39 to give a single score that was used as a continuous variable.
All wave 2 participants were asked about previous suicide attempts with the following question: “In your entire life did you ever attempt suicide?” Responses were coded as either “yes” or “no.”
Statistical Analyses
We applied appropriate statistical weights to ensure representativeness of the NESARC data. Because of the complex sampling design of the NESARC, we performed all analyses with SUDAAN's Taylor Series Linearization process.40 We used cross-tabulation and logistic regression analyses to determine prevalence rates and odds ratios (ORs) of suicide attempts within the 8 sociodemographic variables described above. Next, we calculated prevalence rates, adjusted ORs (AORs), and PAFs for suicide attempts among individual Axis I and II disorders captured by the AUDADIS-IV. All examined mental disorders were entered simultaneously into a multivariate regression model that generated AORs describing the odds of suicide attempt for each mental disorder. The proportion of suicide attempts that could be attributed to a particular mental disorder, compared with the absence of this disorder, was determined by using PAFs. In accordance with comparable population health and biostatistics research,12,41 PAFs were calculated by using the following equation:
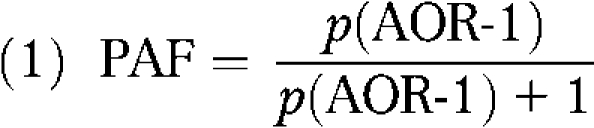 |
where p is the proportion of individuals in the entire population diagnosed with the particular mental disorder in question and AOR is the previously calculated adjusted odds of suicide attempts within the given mental disorder category. AORs were calculated by using suicide attempts as the dependent variable, whereas all mental disorders (independent variables) and covariates (sociodemographic and physical disease and disability variables) were entered simultaneously into the model. The same analytic procedure was used to calculate prevalence rates, AORs, and PAFs for suicide attempts among 5 mental disorder aggregate variables: any substance use disorder, any anxiety disorder, any mood disorder, any psychotic disorder, and any personality disorder. Each aggregate variable contained all individuals who met the criteria for any of the individual disorders within that mental disorder category. Interaction terms were tested for significance where possible and added to the model if the terms significantly improved the model fit. Hosmer–Lemeshow goodness-of-fit tests were performed for the final analytic models.
RESULTS
The associations between suicide attempts and the sociodemographic variables that we examined in the study are shown in Table 1. Compared with men, women were more likely to have made a suicide attempt (OR = 1.69; 95% CI = 1.47, 1.94). People older than 65 years were less likely to have attempted suicide than were younger adults (OR = 0.22; 95% CI= 0.15, 0.30). Suicide attempts were associated with marital breakup, either by separation, divorce, or death of a spouse (OR = 1.67; 95% CI = 1.41, 1.97). Differences were observed among the various racial/ethnic groups. Compared with Whites, Blacks and people of Hispanic descent were less likely to have made a suicide attempt (OR = 0.67; 95% CI = 0.54, 0.83, and OR = 0.74; 95% CI = 0.60, 0.91, respectively), whereas American Indians and Alaskan Natives were more likely to have attempted suicide (OR = 1.56; 95% CI = 1.12, 2.18). Compared with other income brackets, poverty (defined as having a household income <$20 000) was more often associated with suicide attempts. No relationship was observed between level of education and history of suicide attempt.
TABLE 1.
Sociodemographic Correlates of Suicide Attempts: National Epidemiologic Survey on Alcohol and Related Conditions, Wave 2, 2004–2005
| Suicide Attempta |
Prevalence of Suicide Attempt by Sociodemographic Characteristic, % | |||
| Sociodemographic Characteristic | No (n = 33 167), No. (%)b | Yes (n = 1265), No. (%)b | OR (95% CI) | |
| Gender | ||||
| Male (Ref) | 14 110 (48.5) | 363 (32.3) | 1.00 | 2.3 |
| Female | 19 057 (51.5) | 902 (67.7) | 1.69*** (1.47, 1.94) | 4.4 |
| Age, y | ||||
| 20–29 (Ref) | 4659 (16.1) | 236 (21.1) | 1.00 | 4.4 |
| 30–44 | 10 061 (29.4) | 473 (39.0) | 1.19 (0.97, 1.46) | 4.5 |
| 45–64 | 11 407 (34.6) | 488 (35.3) | 0.83 (0.67, 1.04) | 3.5 |
| ≥ 65 | 7040 (19.8) | 68 (4.5) | 0.22*** (0.15, 0.30) | 0.8 |
| Ethnicity | ||||
| White (Ref) | 19 295 (71.0) | 750 (71.9) | 1.00 | 3.5 |
| Black | 6337 (11.1) | 214 (10.1) | 0.67*** (0.54, 0.83) | 3.1 |
| American Indian or Alaskan Native | 524 (2.1) | 47 (4.16) | 1.56** (1.12, 2.18) | 6.5 |
| Asian or Hawaiian | 920 (4.3) | 27 (2.6) | 0.95 (0.56, 1.62) | 2.1 |
| Hispanic | 6091 (11.6) | 227 (11.2) | 0.74** (0.60, 0.91) | 3.3 |
| Marital status | ||||
| Married (Ref) | 18 242 (64.3) | 524 (51.4) | 1.00 | 2.7 |
| Widowed, separated, or divorced | 8629 (18.5) | 446 (27.9) | 1.67*** (1.41, 1.97) | 5.0 |
| Never married | 6296 (17.2) | 295 (20.7) | 1.09 (0.87, 1.37) | 4.1 |
| Region | ||||
| Northwest (Ref) | 5822 (17.8) | 235 (18.4) | 1.00 | 3.5 |
| Midwest | 6285 (18.5) | 245 (18.3) | 0.93 (0.73, 1.18) | 3.4 |
| South | 12 598 (38.4) | 472 (37.7) | 1.01 (0.83, 1.25) | 3.3 |
| West | 8462 (25.3) | 313 (25.6) | 0.96 (0.77, 1.20) | 3.4 |
| Income | ||||
| $0–$19 999 (Ref) | 7486 (18.0) | 471 (31.1) | 1.00 | 5.7 |
| $20 000–$34 999 | 6583 (18.5) | 252 (19.7) | 0.61*** (0.49, 0.74) | 3.6 |
| $35 000–$59 999 | 8120 (25.2) | 279 (23.5) | 0.49*** (0.40, 0.62) | 3.2 |
| ≥ $60 000 | 10 978 (38.3) | 263 (25.7) | 0.36*** (0.28, 0.46) | 2.3 |
| Education level | ||||
| Less than high school (Ref) | 5233 (13.9) | 231 (16.0) | 1.00 | 3.9 |
| High school | 9054 (27.5) | 331 (24.9) | 0.82 (0.66, 1.03) | 3.1 |
| Some college or more | 18 880 (58.6) | 703 (59.0) | 0.90 (0.73, 1.12) | 3.4 |
| Urbanicity | ||||
| Urban (Ref) | 11 028 (32.7) | 434 (34.7) | 1.00 | 3.6 |
| Rural | 22 139 (67.3) | 831 (65.3) | 0.97 (0.84, 1.12) | 3.3 |
Note. CI = confidence interval; OR = odds ratio.
The reference group was individuals without suicide attempts.
Numbers are unweighted values; percentages are weighted values.
*P < .05; **P < .01; ***P < .001.
The associations between mental disorders and suicide attempts are presented in Table 2. Of the substance use disorders examined, alcohol dependence, drug abuse, and nicotine dependence were all associated with having made a suicide attempt in the past (AOR = 1.34; 95% CI = 1.04, 1.73; AOR = 1.43; 95% CI = 1.10, 1.86; and AOR = 1.42; 95% CI = 1.16, 1.73, respectively). PTSD (AOR = 1.65; 95% CI = 1.32, 2.07) was the only anxiety disorder independently associated with suicide attempts in the multivariate model. Dysthymic disorder, bipolar I disorder, and major depressive disorder were all associated with suicide attempts, with the latter having the strongest association (AOR = 2.58; 95% CI = 2.10, 3.17). Schizophrenia or psychotic illness or episode was significantly associated with a lifetime history of suicide attempt (AOR = 1.82; 95% CI = 1.34, 2.46). Several personality disorders were associated with suicide attempts including schizotypal, borderline, antisocial, avoidant, and dependent personality disorders. The strongest relationship was observed with borderline personality disorder (AOR = 4.45; 95% CI = 3.42, 5.80). People with narcissistic personality disorder were significantly less likely to have made a suicide attempt compared to people without narcissistic personality disorder (AOR = 0.58; 95% CI = 0.43, 0.80).
TABLE 2.
Population-Attributable Fractions of DSM-IV Mental Disorders for Suicide Attempts: National Epidemiologic Survey on Alcohol and Related Conditions, Wave 2, 2004–2005
| Suicide Attempta |
||||
| Lifetime DSM-IV Diagnosis | No (n = 33167), No. (%)b | Yes (n = 1265), No. (%)b | AORc (95% CI) | PAF (95% CI) |
| Substance use disorders | ||||
| Alcohol abuse | 6126 (18.5) | 229 (18.1) | 1.27 (0.97, 1.67) | 4.7 (−0.6, 11.0) |
| Alcohol dependence | 4441 (13.4) | 456 (36.0) | 1.34* (1.04, 1.73) | 4.6 (0.6, 9.4) |
| Drug abuse | 2556 (7.7) | 223 (17.6) | 1.43** (1.10, 1.86) | 3.4 (0.8, 6.5) |
| Drug dependence | 905 (2.7) | 207 (16.4) | 1.38 (0.99, 1.91) | 1.2 (0.0, 2.8) |
| Nicotine dependence | 6913 (20.8) | 611 (48.3) | 1.42*** (1.16, 1.73) | 8.4 (3.4, 13.7) |
| Anxiety disorders | ||||
| Panic disorder | 2290 (6.9) | 384 (30.6) | 1.16 (0.91, 1.48) | 1.2 (−0.7, 3.6) |
| Posttraumatic stress disorder | 3093 (8.47) | 525 (39.6) | 1.65*** (1.32, 2.07) | 6.3 (3.2, 10.0) |
| Social phobia | 2096 (6.3) | 337 (27.1) | 1.10 (0.85, 1.44) | 0.7 (−1.1, 3.0) |
| Specific phobia | 5015 (14.4) | 450 (37.3) | 1.03 (0.81, 1.30) | 0.5 (−3.1, 4.5) |
| Generalized anxiety disorder | 2316 (6.8) | 399 (31.1) | 1.01 (0.81, 1.26) | 0.1 (−1.5, 2.0) |
| Mood disorders | ||||
| Major depressive disorder | 7011 (20.3) | 881 (68.9) | 2.58*** (2.10, 3.17) | 26.6 (20.1, 33.2) |
| Dysthymic disorder | 1556 (4.3) | 366 (26.7) | 1.53*** (1.20, 1.95) | 2.9 (1.1, 5.1) |
| Bipolar I disorder | 1472 (4.4) | 369 (29.1) | 1.31* (1.01, 1.71) | 1.6 (0.1, 3.6) |
| Bipolar II disorder | 632 (1.7) | 114 (9.1) | 1.14 (0.79, 1.63) | 0.3 (−0.5, 1.4) |
| Psychotic disorders | ||||
| Schizophrenia or psychotic illness or episode | 1001 (2.7) | 198 (15.1) | 1.82*** (1.34, 2.46) | 2.5 (1.0, 4.3) |
| Personality disorders | ||||
| Borderline | 1660 (4.6) | 562 (43.7) | 4.45*** (3.42, 5.80) | 18.1 (13.4, 23.5) |
| Schizotypal | 1220 (3.3) | 307 (23.0) | 1.33 (0.97, 1.81) | 1.4 (−0.1, 3.4) |
| Narcissistic | 2208 (5.9) | 237 (16.3) | 0.58*** (0.43, 0.80) | −3.1 (−4.2, −1.4) |
| Avoidant | 634 (1.9) | 181 (15.0) | 1.57* (1.09, 2.27) | 1.3 (0.2, 3.0) |
| Antisocial | 959 (3.2) | 189 (15.8) | 1.94*** (1.37, 2.75) | 3.0 (1.2, 5.5) |
| Dependent | 92 (0.2) | 52 (5.0) | 2.02 (0.98, 4.16) | 0.4 (0.0, 1.2) |
| Obsessive-compulsive | 2483 (7.6) | 258 (21.5) | 1.08 (0.83, 1.40) | 0.6 (−1.4, 3.1) |
| Paranoid | 1412 (3.8) | 266 (19.1) | 0.84 (0.62, 1.15) | −0.8 (−1.9, 0.7) |
| Schizoid | 976 (2.7) | 163 (12.8) | 0.91 (0.63, 1.31) | −0.3 (−1.2, 1.0) |
| Histrionic | 550 (1.58) | 95 (7.9) | 0.95 (0.64, 1.41) | −0.1 (−0.7, 0.8) |
Note. AOR = adjusted odds ratio; CI = confidence interval; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; PAF = population-attributable fraction.
The reference group was individuals without suicide attempts.
Numbers are unweighted values; percentages are weighted values.
Simultaneously adjusted for significant sociodemographic variables (gender, age, race/ethnicity, marital status, region, income, education level, and urbanicity), permanent physical disability, physical disease, and all mental disorders in the model.
*P < .05; **P < .01; ***P < .001.
The PAFs for each mental disorder for suicide attempts are also shown in Table 2. The highest proportion of suicide attempts was attributable to major depressive disorder, which independently accounted for more than one quarter of all suicide attempts in the sample (PAF = 26.6%; 95% CI = 20.1, 33.2). Nearly 20% of suicide attempts were attributable to borderline personality disorder (PAF = 18.1%; 95% CI = 13.4, 23.5). The disorders that accounted for the next highest proportions of suicide attempts were nicotine dependence (PAF = 8.4%; 95% CI = 3.4, 13.7) and PTSD (PAF = 6.3%; 95% CI = 3.2, 10.0). The remaining 21 disorders had lower PAF values; all were less than 5%.
Model fit indexes revealed the model to be a poor fit (χ2 = 20.85; P < .01). Therefore, consideration was given to the inclusion of possible interactions between correlates. However, the addition of interaction terms to the model was not feasible given the very high number of possible interactions and the size of the current model.
The percentage of suicide attempts attributable to mental disorder categories is shown in Table 3. In the multivariate model, both the highest odds and highest proportion of suicide attempts were attributable to mood disorders. Mood disorders accounted for almost 40% of all suicide attempts (PAF = 36.6%; 95% CI = 31.0, 42.4). Having a personality disorder was associated with 3-fold higher odds of a lifetime suicide attempt and accounted for almost one third of suicide attempts. Similar results were observed with substance use disorders. Despite exhibiting almost 3-fold increased odds of suicide attempt, psychotic disorders had a PAF value of 4.9% (95% CI = 3.2, 7.1). Like all the other diagnostic categories examined, anxiety disorders were independently associated with suicide attempts, but showed the lowest odds for suicide attempts (AOR = 1.51; 95% CI = 1.27, 1.80) and had a lower PAF value than did most other categories (PAF = 11.5%; 95% CI = 6.4, 16.9). The Hosmer–Lemeshow test determined the final model presented in Table 3 to be a good fit (χ2 = 3.47; P > .05). The addition of significant interaction terms did not improve the model fit.
TABLE 3.
Population-Attributable Fractions of Mental Disorder Categories for Suicide Attempts: National Epidemiologic Survey on Alcohol and Related Conditions, Wave 2, 2004–2005
| Suicide Attempta |
||||
| Lifetime DSM-IV Diagnosis | No (n = 33 167), No. (%)b | Yes (n = 1265), No. (%)b | AORc (95% CI) | PAF (95% CI) |
| Any substance use disorder | 13 028 (39.3) | 880 (69.6) | 2.10*** (1.75, 2.51) | 31.8 (24.1, 39.0) |
| Any anxiety disorder | 9680 (28.1) | 903 (70.7) | 1.51*** (1.27, 1.80) | 11.5 (6.4, 16.9) |
| Any mood disorder | 7756 (22.4) | 941 (73.7) | 3.40*** (2.86, 4.05) | 36.6 (31.0, 42.4) |
| Any psychotic disorder | 1001 (2.7) | 198 (15.1) | 2.67*** (2.07, 3.46) | 4.9 (3.2, 7.1) |
| Any personality disorder | 6612 (19.2) | 829 (65.2) | 3.09*** (2.61, 3.67) | 30.2 (25.0, 35.6) |
Note. AOR = adjusted odds ratio; CI = confidence interval; DSM-IV = Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition; PAF = population-attributable fraction.
The reference group was individuals without suicide attempts.
Numbers are unweighted values; percentages are weighted values.
Simultaneously adjusted for sociodemographic variables (gender, age, race/ethnicity, marital status, region, income, education level, and urbanicity), permanent physical disability, physical disease, and all mental disorder categories in the model.
***P < .001.
DISCUSSION
Our findings need to be considered in the context of the limitations of the PAF as a statistical method. PAF values are based on the assumption that the risk factors examined have a causal connection to the outcome of interest.12,41 The design of this study was cross-sectional, however; therefore, we could not make causal inferences between suicide attempts and the psychiatric disorders examined. The variables used in this analysis were lifetime disorders and thus may not have been temporally related to suicide attempts. It is possible that a person attempted suicide early in life for other unmeasured reasons and subsequently developed an Axis I or Axis II disorder. It is also possible that the relationship between mental disorders and suicide attempts is explained by noncausal common factors, such as environmental or genetic factors. Thus, although our study cannot be used to infer causality, the disorders in our analyses have been established as risk factors for suicide attempts in several previous studies.7–9,16,25 Cross-sectional studies have been identified as a data source for which PAFs can be applied,42 and indeed the majority of studies examining the PAF of mental disorders for suicide attempts have been of cross-sectional design.15 However, we must recognize this important limitation when interpreting the results of our study and recognize that these preliminary findings require replication in longitudinal studies.
Another limitation relating to PAF analyses is the assumption of a decrease in risk to the population after the removal of exposure to the identified risk factor.15 PAFs are of greater utility when the potential risk factors are modifiable, and in the case of this study, if decreased exposure to mental disorders resulted in a reduced risk of suicide attempt. Evidence has shown that treatment of mental illness is associated with diminished rates of suicide attempts,43–45 which suggests that reducing exposure to mental disorders through treatment reduces the risk of suicide attempt. Nevertheless, the PAF values of our study represent estimations not testable presently.
Bearing these limitations in mind, our study had several notable findings. To our knowledge, ours is the first study to examine the PAFs of both Axis I and Axis II mental disorders for suicide attempts in a nationally representative sample. This study also used multivariate modeling that adjusted for the effects of all 25 disorders examined, thereby accounting for comorbidity and providing an improved estimate of the independent PAFs of mental disorders for suicide attempts. The main finding was the high PAF values observed with a select few disorders, specifically, major depressive disorder, borderline personality disorder, nicotine dependence, and PTSD. This finding emphasizes the importance of those 4 illnesses as risk factors for suicide attempts. Furthermore, this study extends our knowledge of suicide attempts by illustrating the importance of both PAFs and ORs as methods of examining candidate risk factors.
Our finding that nicotine dependence independently accounted for a high proportion of suicide attempts is intriguing. Smoking has received very little attention in the literature of suicide attempt risk factors and, to our knowledge, smoking has never been examined by using PAFs. Recent studies have revealed mixed results regarding the relationship between smoking and suicide attempts, with some studies finding a positive association46,47 and others showing no relationship once confounding factors were adjusted for.22,48,49 We found that nicotine dependence was independently associated with suicide attempts among the general population. The nicotine dependence PAF of 8.4% has considerable public health implications. Smoking is already established as the leading cause of preventable death in the United States50 and was estimated to be responsible for 4.83 million premature deaths worldwide in 2000.51 With increasing evidence of smoking as a risk factor for suicidal behavior,46,47 the effects of smoking are of further concern. The lifetime prevalence of suicide attempts in the United States in the NESARC wave 2 sample was 3.4% and in the National Comorbidity Survey was 4.6%.8 With a current estimated US population of more than 308 million,52 approximately 10 to 14 million persons in the United States will attempt suicide over the course of their lifetimes. Bearing in mind the limitations of PAFs, our results suggest that in the absence of nicotine dependence among the population, 1 million fewer Americans would attempt suicide. These findings need to be interpreted cautiously, however, because the observed relationship between nicotine dependence and suicide attempts was a cross-sectional correlation not based on a confirmed causal relationship and conflicts with findings in some of the existing literature.
The high proportion of suicide attempts associated with PTSD also deserves particular attention. Significant controversy has arisen regarding anxiety disorders as risk factors for suicide attempts, with considerable focus on the role of panic disorder.53,54 More recent reports have consistently demonstrated a relationship between anxiety disorders and suicide attempts.9,11,22,26,55,56 Studies examining individual anxiety disorders have often identified independent associations between suicide attempts and PTSD.10,26,56 The results from our study are consistent with those previous findings and further emphasize the relationship between PTSD and suicidal behavior. The PAF results from this study suggest that a high percentage of suicide attempts are attributable to PTSD.
Borderline personality disorder was also strongly associated with suicide attempts in the multivariate model and had a PAF of 18.1%. To our knowledge, ours is the first study to examine the PAF of borderline personality disorder for suicide attempts. Borderline personality disorder has a well-established association with suicide attempts in the psychiatric literature,23 with most studies focusing on clinical populations. Our study extends previous knowledge to include the general population. Our findings show that 25% of persons with borderline personality disorder will attempt suicide at some point in their lives, and that the disorder is associated with almost 5-fold increased odds of suicide attempt. This strong association and high attributable fraction of suicide attempts among the general population underscores the importance of treatment efforts for borderline personality disorder, not only at the level of the individual but also from a public health policy perspective.
Interesting findings came from the analysis examining disorders grouped by category. Among the cohort of individuals who had attempted suicide at some point in their lives, there was an almost equal prevalence of substance use, anxiety, mood, and personality disorders (ranging from 65.2%–73.7%). The multivariate regression, however, demonstrated different strengths of association across the aggregate diagnostic categories. The presence of a mood disorder had the highest odds of a suicide attempt, significantly higher than the odds posed by an anxiety or substance use disorder. The PAF results suggested that if mood disorders were eliminated from the population, people attempting suicide would decrease by almost 40%. This finding is consistent with findings in other studies that examined the population-attributable risk for affective disorders.14,18 Together, these studies underscore the relationship between mood disorders and suicidal behavior. Although personality disorders have a significantly greater association with suicide attempts compared with substance use disorders, the 2 groups account for a similar proportion of suicide attempts among the general population. The existing literature on the population-attributable risk of substance use disorders for suicide attempts has generally reported much lower values, in the range of 7.7% to 15.4%.14,18 The higher PAF in our study is likely a result of the inclusion of nicotine dependence as a substance use disorder. A study using the National Comorbidity Survey reported much higher PAF rates for substance use disorders, with values of approximately 30% for women and 52.9% to 61.4% for men, depending on the seriousness of the suicide attempt.57 Anxiety disorders maintained an independent association with suicide attempts even after control for confounding factors; however, anxiety disorders had a lower PAF than did all other diagnostic categories, with the exception of psychotic disorders. Previous studies have had discrepant findings regarding the PAF of anxiety disorders for suicide attempts, with some PAF values as low as 7%22 and others as high as 37%.14 Such inconsistent findings indicate a need for further investigation into the role of anxiety disorders in suicide attempts.
Other limitations of our study need to be recognized. One limitation relates to the accuracy of diagnoses. The diagnoses by trained lay interviewers may differ from the diagnoses by clinicians. The established reliability and validity of NESARC diagnoses address this limitation to some extent. Limitations also exist regarding the assessment of suicide attempts. We were unable to examine the severity of suicide attempts. When compared with people who choose less lethal means, more lethal suicide attempts may characterize people who are closer in profile to suicide completers.58,59 We were also unable to examine the PAF of completed suicide because this was not examined in the NESARC survey. One study examining the PAF of mental disorders for completed suicide by use of results from psychological autopsy studies found a range of 47% to 74%.60 Suicidal ideation was not assessed in the full NESARC sample and therefore could not be included in our analysis. This omission is a limitation given previous work showing that suicidal ideation accounts for much of the PAF of suicide attempts and that accounting for the effect of suicidal ideation reduces the proportion of suicide attempts independently attributable to mental disorders.10 Further reports examining the PAF of completed suicide and suicidal ideation are needed.
Another limitation is that the analytic model yielding the results in Table 2 was a poor fit. It is possible that the addition of other variables may have improved the model fit. We considered the inclusion of interaction terms; however, because of the large number of mental disorders examined in the analytic model, there were several hundred possible interactions. Testing and including so many additional variables would not have been feasible, given the already large model size. Despite this limitation, the model in our study examined a much higher number of mental disorders than did models in previous studies. Furthermore, with the inclusion of all 10 personality disorders, our study represents a significant advance in the understanding of the risk of suicide attempts associated with mental disorders. Future studies examining variables unmeasured in this data set may improve the predictive ability of analytic models of suicide attempt risk factors. Finally, we could not examine the effects of multiple suicide attempts by the same individual.
In conclusion, the results of the present study extend our understanding of suicide attempts by clarifying the risk attributable to specific disorders among the general population. Major depressive disorder and borderline personality disorder were strong risk factors and accounted for a large proportion of suicide attempts. Nicotine dependence and PTSD are emerging as important risk factors for suicide attempts, and the high PAFs of nicotine dependence and PTSD call for more assertive public policy measures targeting treatment at the population level. Although many mental disorders are correlated with suicidal behavior, successfully treating the 4 disorders (major depressive disorder, borderline personality disorder, nicotine dependence, PTSD) may substantially reduce the number of persons attempting suicide.
Acknowledgments
Preparation of this article was supported by research grants from the Manitoba Health Research Council (to J. M. Bolton) and by a graduate studentship from the Canadian Institutes for Health Research (to J. Robinson).
We acknowledge Shay-Lee Belik, MSc, for her assistance with the statistical analysis.
Human Participant Protection
No approval was required because the data were obtained from secondary sources.
References
- 1.Suicide Prevention (SUPRE) Geneva, Switzerland: World Health Organization; Available at: http://www.who.int/mental_health/prevention/suicide/suicideprevent/en. Accessed December 12, 2009 [Google Scholar]
- 2.US Public Health Service The Surgeon General's Call to Action to Prevent Suicide. Washington, DC: US Public Health Service; 1999 [Google Scholar]
- 3.Kessler RC, Berglund P, Borges G, Nock M, Wang PS. Trends in suicide ideation, plans, gestures, and attempts in the United States, 1990–1992 to 2001–2003. JAMA. 2005;293(20):2487–2495 [DOI] [PubMed] [Google Scholar]
- 4.Harris EC, Barraclough B. Suicide as an outcome for mental disorders. A meta-analysis. Br J Psychiatry. 1997;170:205–228 [DOI] [PubMed] [Google Scholar]
- 5.Jenkins GR, Hale R, Papanastassiou M, Crawford MJ, Tyrer P. Suicide rate 22 years after parasuicide: cohort study. BMJ. 2002;325(7373):1155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suominen K, Isometsa E, Suokas J, Haukka J, Achte K, Lonnqvist J. Completed suicide after a suicide attempt: a 37-year follow-up study. Am J Psychiatry. 2004;161(3):562–563 [DOI] [PubMed] [Google Scholar]
- 7.Joiner TE, Jr, Brown JS, Wingate LR. The psychology and neurobiology of suicidal behavior. Annu Rev Psychol. 2005;56:287–314 [DOI] [PubMed] [Google Scholar]
- 8.Kessler RC, Borges G, Walters EE. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56(7):617–626 [DOI] [PubMed] [Google Scholar]
- 9.Nock MK, Hwang I, Sampson N, et al. Cross-national analysis of the associations among mental disorders and suicidal behavior: findings from the WHO World Mental Health Surveys. PLoS Med. 2009;6(8): e1000123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nock MK, Hwang I, Sampson NA, Kessler RC. Mental disorders, comorbidity and suicidal behavior: Results from the National Comorbidity Survey Replication. Mol Psychiatry. 2010;15(8):868–876 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bolton JM, Belik SL, Enns MW, Cox BJ, Sareen J. Exploring the correlates of suicide attempts among individuals with major depressive disorder: findings from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(7):1139–1149 [DOI] [PubMed] [Google Scholar]
- 12.Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health. 1998;88(1):15–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goldney RD, Wilson D, Dal GE, Fisher LJ, McFarlane AC. Suicidal ideation in a random community sample: attributable risk due to depression and psychosocial and traumatic events. Aust N Z J Psychiatry. 2000;34(1):98–106 [DOI] [PubMed] [Google Scholar]
- 14.Pirkis J, Burgess P, Dunt D. Suicidal ideation and suicide attempts among Australian adults. Crisis. 2000;21(1):16–25 [DOI] [PubMed] [Google Scholar]
- 15.Krysinska K, Martin G. The struggle to prevent and evaluate: application of population attributable risk and preventive fraction to suicide prevention research. Suicide Life Threat Behav. 2009;39(5):548–557 [DOI] [PubMed] [Google Scholar]
- 16.Beautrais AL. A case control study of suicide and attempted suicide in older adults. Suicide Life Threat Behav. 2002;32(1):1–9 [DOI] [PubMed] [Google Scholar]
- 17.Bernal M, Haro JM, Bernert S, et al. Risk factors for suicidality in Europe: results from the ESEMED study. J Affect Disord. 2007;101(1-3):27–34 [DOI] [PubMed] [Google Scholar]
- 18.Carter GL, Child C, Page A, Clover K, Taylor R. Modifiable risk factors for attempted suicide in Australian clinical and community samples. Suicide Life Threat Behav. 2007;37(6):671–680 [DOI] [PubMed] [Google Scholar]
- 19.Cheung YB, Law CK, Chan B, Liu KY, Yip PS. Suicidal ideation and suicidal attempts in a population-based study of Chinese people: risk attributable to hopelessness, depression, and social factors. J Affect Disord. 2006;90(2-3):193–199 [DOI] [PubMed] [Google Scholar]
- 20.Goldney RD, Dal GE, Fisher LJ, Wilson D. Population attributable risk of major depression for suicidal ideation in a random and representative community sample. J Affect Disord. 2003;74(3):267–272 [DOI] [PubMed] [Google Scholar]
- 21.Tsoh J, Chiu HF, Duberstein PR, et al. Attempted suicide in elderly Chinese persons: a multi-group, controlled study. Am J Geriatr Psychiatry. 2005;13(7):562–571 [DOI] [PubMed] [Google Scholar]
- 22.Boden JM, Fergusson DM, Horwood LJ. Cigarette smoking and suicidal behaviour: results from a 25-year longitudinal study. Psychol Med. 2008;38(3):433–439 [DOI] [PubMed] [Google Scholar]
- 23.Soloff PH, Lis JA, Kelly T, Cornelius J, Ulrich R. Risk factors for suicidal behavior in borderline personality disorder. Am J Psychiatry. 1994;151(9):1316–1323 [DOI] [PubMed] [Google Scholar]
- 24.Verona E, Sachs-Ericsson N, Joiner TE., Jr. Suicide attempts associated with externalizing psychopathology in an epidemiological sample. Am J Psychiatry. 2004;161(3):444–451 [DOI] [PubMed] [Google Scholar]
- 25.Yen S, Shea MT, Pagano M, et al. Axis I and axis II disorders as predictors of prospective suicide attempts: findings from the collaborative longitudinal personality disorders study. J Abnorm Psychol. 2003;112(3):375–381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cougle JR, Keough ME, Riccardi CJ, Sachs-Ericsson N. Anxiety disorders and suicidality in the National Comorbidity Survey-Replication. J Psychiatr Res. 2009;43(9):825–829 [DOI] [PubMed] [Google Scholar]
- 27.Sareen J, Houlahan T, Cox BJ, Asmundson GJ. Anxiety disorders associated with suicidal ideation and suicide attempts in the National Comorbidity Survey. J Nerv Ment Dis. 2005;193(7):450–454 [DOI] [PubMed] [Google Scholar]
- 28.Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):617–627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Hasin DS, Keyes KM, Alderson D, Wang S, Aharonovich E, Grant BF. Cannabis withdrawal in the United States: results from NESARC. J Clin Psychiatry. 2008;69(9):1354–1363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71(1):7–16 [DOI] [PubMed] [Google Scholar]
- 31.Grant BF, Harford TC, Muthen BO, Yi HY, Hasin DS, Stinson FS. DSM-IV alcohol dependence and abuse: further evidence of validity in the general population. Drug Alcohol Depend. 2007;86(2-3):154–166 [DOI] [PubMed] [Google Scholar]
- 32.Grant BF, Stinson FS, Dawson DA, et al. Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61(8):807–816 [DOI] [PubMed] [Google Scholar]
- 33.Grant BF, Chou SP, Goldstein RB, et al. Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2008;69(4):533–545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grant BF, Stinson FS, Harford TC. Age at onset of alcohol use and DSM-IV alcohol abuse and dependence: a 12-year follow-up. J Subst Abuse. 2001;13(4):493–504 [DOI] [PubMed] [Google Scholar]
- 35.Ruan WJ, Goldstein RB, Chou SP, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug Alcohol Depend. 2008;92(1-3):27–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mueser KT, McGurk SR. Schizophrenia. Lancet. 2004;363(9426):2063–2072 [DOI] [PubMed] [Google Scholar]
- 37.Supina AL, Patten SB. Self-reported diagnoses of schizophrenia and psychotic disorders may be valuable for monitoring and surveillance. Can J Psychiatry. 2006;51(4):256–259 [DOI] [PubMed] [Google Scholar]
- 38.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383 [DOI] [PubMed] [Google Scholar]
- 39.Needham DM, Scales DC, Laupacis A, Pronovost PJ. A systematic review of the Charlson comorbidity index using Canadian administrative databases: a perspective on risk adjustment in critical care research. J Crit Care. 2005;20(1):12–19 [DOI] [PubMed] [Google Scholar]
- 40.Research Triangle Institute SUDAAN User's Manual, Version 8. Research Triangle Park, NC: Research Triangle Institute; 2001 [Google Scholar]
- 41.Young TK. Population Health: Concepts and Methods. 2. New York, NY: Oxford University Press; 2005 [Google Scholar]
- 42.Eide GE, Heuch I. Attributable fractions: fundamental concepts and their visualization. Stat Methods Med Res. 2001;10(3):159–193 [DOI] [PubMed] [Google Scholar]
- 43.Simon GE, Savarino J. Suicide attempts among patients starting depression treatment with medications or psychotherapy. Am J Psychiatry. 2007;164(7):1029–1034 [DOI] [PubMed] [Google Scholar]
- 44.Gibbons RD, Hur K, Brown H, Mann JJ. Relationship between antiepileptic drugs and suicide attempts in patients with bipolar disorder. Arch Gen Psychiatry. 2009;66(12):1354–1360 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Tondo L, Baldessarini RJ. Long-term lithium treatment in the prevention of suicidal behavior in bipolar disorder patients. Epidemiol Psichiatr Soc. 2009;18(3):179–183 [DOI] [PubMed] [Google Scholar]
- 46.Breslau N, Schultz LR, Johnson EO, Peterson EL, Davis GC. Smoking and the risk of suicidal behavior: a prospective study of a community sample. Arch Gen Psychiatry. 2005;62(3):328–334 [DOI] [PubMed] [Google Scholar]
- 47.Riala K, Hakko H, Rasanen P. Nicotine dependence is associated with suicide attempts and self-mutilation among adolescent females. Compr Psychiatry. 2009;50(4):293–298 [DOI] [PubMed] [Google Scholar]
- 48.Kessler RC, Berglund PA, Borges G, et al. Smoking and suicidal behaviors in the National Comorbidity Survey: replication. J Nerv Ment Dis. 2007;195(5):369–377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kessler RC, Borges G, Sampson N, Miller M, Nock MK. The association between smoking and subsequent suicide-related outcomes in the National Comorbidity Survey panel sample. Mol Psychiatry. 2009;14(12):1132–1142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.US Department of Health and Human Services Health Consequences of Smoking Cessation: A Report of the Surgeon General. Washington, DC: Government Printing Office; 1994 [Google Scholar]
- 51.Ezzati M, Lopez AD. Estimates of global mortality attributable to smoking in 2000. Lancet. 2003;362(9387):847–852 [DOI] [PubMed] [Google Scholar]
- 52.US Census Bureau U.S. POPClock Projection. Available at: http://www.census.gov/population/www/popclockus.html. Accessed December 12, 2009
- 53.Hornig CD, McNally RJ. Panic disorder and suicide attempt. A reanalysis of data from the Epidemiologic Catchment Area study. Br J Psychiatry. 1995;167(1):76–79 [DOI] [PubMed] [Google Scholar]
- 54.Weissman MM, Klerman GL, Markowitz JS, Ouellette R. Suicidal ideation and suicide attempts in panic disorder and attacks. N Engl J Med. 1989;321(18):1209–1214 [DOI] [PubMed] [Google Scholar]
- 55.Nock MK, Borges G, Bromet EJ, et al. Cross-national prevalence and risk factors for suicidal ideation, plans and attempts. Br J Psychiatry. 2008;192(2):98–105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sareen J, Cox BJ, Afifi TO, et al. Anxiety disorders and risk for suicidal ideation and suicide attempts: a population-based longitudinal study of adults. Arch Gen Psychiatry. 2005;62(11):1249–1257 [DOI] [PubMed] [Google Scholar]
- 57.Molnar BE, Berkman LF, Buka SL. Psychopathology, childhood sexual abuse and other childhood adversities: relative links to subsequent suicidal behaviour in the US. Psychol Med. 2001;31(6):965–977 [DOI] [PubMed] [Google Scholar]
- 58.Linehan MM. Suicidal people. One population or two? Ann N Y Acad Sci. 1986;487:16–33 [DOI] [PubMed] [Google Scholar]
- 59.Mann JJ. A current perspective of suicide and attempted suicide. Ann Intern Med. 2002;136(4):302–311 [DOI] [PubMed] [Google Scholar]
- 60.Cavanagh JT, Carson AJ, Sharpe M, Lawrie SM. Psychological autopsy studies of suicide: a systematic review. Psychol Med. 2003;33(3):395–405 [DOI] [PubMed] [Google Scholar]


