Abstract
Objectives. We investigated a cluster of tuberculosis (TB) cases among persons using methamphetamines in Snohomish County, Washington, to determine the extent of the outbreak, examine whether methamphetamine use contributed to TB transmission, and implement strategies to prevent further infections.
Methods. We screened contacts to find and treat persons with TB disease or infection. We then formed a multidisciplinary team to engage substance abuse services partners and implement outreach strategies including novel methods for finding contacts and a system of incentives and enablers to promote finding, screening, and treating patients with TB and their infected contacts.
Results. We diagnosed and completed treatment with 10 persons with TB disease. Eight of 9 adult patients and 67% of their adult contacts reported using methamphetamines. Of the 372 contacts, 319 (85.8%) were screened, 80 (25.1%) were infected, 71 (88.8%) started treatment for latent infection, and 57 (80.3%) completed treatment for latent infection.
Conclusions. Collaborative approaches integrating TB control, outreach, incentives, and enablers resulted in high rates of treatment adherence and completion among patients and infected contacts. TB control programs should collaborate with substance abuse programs to address addiction, overcome substance abuse–related barriers to treatment, treat TB, and prevent ongoing transmission.
Illegal drug use is a risk factor for tuberculosis (TB).1 Numerous studies have documented that alcohol abuse and illegal drug use (hereafter referred to as substance abuse) are factors that contribute to TB transmission and act as barriers to TB control and prevention.2–8 Persons who abuse substances are less likely to seek medical care9,10 and initiate, adhere to, and complete treatment for latent TB infection (LTBI)11–13 or TB disease.14–16 Nearly 1 out of every 3 US-born persons with TB who is aged older than 15 years abuses substances.17 Substance abuse among persons with TB is important to public health because it is associated with sputum-smear positivity at diagnosis and failure to complete treatment of TB, both indicators of increased transmission.17 Additionally, substance abuse often takes place in enclosed spaces with poor ventilation and high volumes of human traffic, potentially increasing the likelihood of TB transmission.17
TB control programs have been slow to engage the substance abuse treatment community in collaboratively addressing substance abuse–fueled transmission of TB.10,18 We are not aware of national guidelines that specifically address the control of TB transmission among populations that abuse alcohol and use illegal drugs. Our review of the scientific literature indicates that this is the first report documenting methamphetamine use as a barrier to controlling TB transmission.
In 2006, the incidence of TB disease in Snohomish County, Washington, was 3.8 cases per 100 000 persons; the incidence of TB disease for the state of Washington was 4.1 per 100 000 persons.19 From August 2005 through January 2006, the Snohomish Health District TB Control Program detected an emerging cluster of 6 persons with TB. Five of the 6 persons were known to spend time together (i.e., they were socially linked) and reported using methamphetamines. The recent clustering of these persons in time and space, along with matching genotype patterns of M. tuberculosis, suggested recent transmission of TB.20
Initial attempts to identify contacts of the cluster (i.e., persons exposed to and potentially infected by the original 6 persons with TB) were unsuccessful. Even after repeated interviews, patients refused or remained reluctant to name their contacts. Local TB control staff suspected that this reluctance was related to the patients' use of methamphetamines and their unwillingness to provide names of persons with whom they used illegal substances. To address the substance abuse–related barriers to controlling the outbreak, we expanded our epidemiological investigation and TB control efforts to include alternative measures to find additional persons with TB, provide treatment of these persons, identify and screen their contacts, and provide treatment to those who tested positive for LTBI.
METHODS
We conducted the investigation using guidelines developed by the National TB Controllers Association and the Centers for Disease Control and Prevention for the investigation of contacts of persons with infectious TB.21 We defined outbreak cases as persons diagnosed with culture-confirmed or clinically diagnosed TB disease and with genotyping results that matched the outbreak strain in Snohomish County from April 2005 (the estimated start of the index patient's infectious period) through February 2006 (the conclusion of our investigation). Persons diagnosed during the same time period without genotyping results were also defined as outbreak cases if they were epidemiologically linked with (i.e., named as a contact of or known to have been exposed to) another patient already included in the outbreak. Contacts of persons included in the outbreak were screened for LTBI and TB disease. In accordance with national guidelines, we diagnosed LTBI when contacts had a tuberculin skin test (TST) result of 5 mm or greater induration, normal chest radiograph, and no signs or symptoms of TB disease.21 Contacts with TST reactions of 5 mm or greater induration were then screened for TB disease on the basis of sputum smear examination, culture of sputum, and chest radiograph.
Epidemiological Investigation
We reviewed patients' medical records to ascertain their demographic and disease characteristics. We interviewed patients to document their contacts (i.e., persons with whom they spent time during their estimated infectious periods), locations of potential transmission, health conditions that placed them at greater risk of LTBI progressing to TB disease (e.g., HIV infection or diabetes), and behaviors that often are barriers to initiating and adhering to treatment (e.g., substance abuse). We measured methamphetamine use among patients and contacts by including a questionnaire with the clinical intake form, by reviewing medical records, and through personal interviews. Patients and their contacts were classified as users of methamphetamines if use during the past year was documented in their medical records or was self-reported when interviewed. Contacts were also classified as users of methamphetamines if another contact or patient reported using with them.
To compensate for incomplete reporting of contacts, we utilized several indirect methods for identifying contacts. First, we asked the patients with TB about locations they frequented so we could screen persons at congregate settings frequented by the patients. Next, we interviewed contacts named by multiple patients, because these contacts were likely to have some of the same contacts as the patients; thus, interviews with these contacts served as proxies for identifying contacts not named by patients. Last, we conducted outreach activities to identify and screen both named and location-based contacts.
We conducted screening and provided directly observed therapy at sites frequented by persons using illegal drugs, namely a needle-exchange program, a homeless shelter, and an alley next to a drug-use venue frequented by some of the patients and their contacts (hereafter referred to as the “drug house”). An informational flyer was distributed informing contacts that they could receive screening and treatment at specified dates and times at the drug house alley. To establish trust, flyers were distributed by a cooperative contact who was already trusted by many of the patients and contacts, and law enforcement officers were notified and asked not to be visible or intervene around the time of the screenings.
Public Health Response
Frequent methamphetamine use and other substance abuse among patients and their contacts was a barrier to traditional TB control methods. Substance abuse is a barrier to TB control because patients who abuse substances are less likely to name contacts, and patients and contacts who abuse substances are less likely to be screened or to start or complete treatment for TB disease or infection.17 To address this barrier we collaborated with internal and external partners who had extensive experience working with persons addicted to alcohol and drugs. They worked with staff from the Snohomish Health District's substance abuse and sexually transmitted disease units to locate contacts, perform TB screening, and conduct directly observed therapy with patients and their contacts. External partners included a needle-exchange program, a homeless shelter, and the county jail. Staff at the needle-exchange program and the shelter helped us identify, locate, establish trust with, and conduct TB screening among contacts addicted to alcohol and illegal drugs. Illegal drug use among patients and their contacts resulted in frequent interactions with the legal system. We received daily rosters of bookings from the county jail to cross-reference with our list of contacts. Partnering with the jail allowed us to screen contacts, identify those who were infected, and start treatment with contacts before they were released from the jail or transferred to another detention facility.
Incentives and enablers were used to reduce barriers to accessing services and to promote adherence to screening activities and treatment. Patients and contacts received $5 coupons or restaurant gift cards for getting screened, identifying and locating other contacts, and keeping appointments for medical evaluations. In some cases they received an additional $3 for taking anti-TB medications. Incentives were also tailored for special circumstances; some patients and contacts received diapers, baby food, or even a car battery. Enabling strategies included providing gas cards and contracting with a taxi service to provide transportation for noncontagious patients and contacts.
RESULTS
The index patient was diagnosed in an emergency room where he sought care for advanced TB disease in August 2005. He was underweight, short of breath, abusing alcohol, and using methamphetamines, and had a history of smoking cigarettes. At the time of his diagnosis he was living in his truck and had delayed seeking care. During his initial interview he reported only 2 contacts. To improve the likelihood of his completing anti-TB treatment and to minimize exposure to other persons, he was provided a hotel room where he received directly observed therapy. In November 2005, a second patient was diagnosed after he had hemoptysis while detained in the Snohomish County jail. The first patient had not named the second patient as a contact; however, during the course of our investigation we learned that the first and second patient had spent time with each other and thus were socially linked.
We found 10 patients with illness meeting the outbreak case definition. Nine patients were adults, and 1 patient was a 2-year-old child. All patients were born in the United States, the median age was 35 years, and 7 patients were male (Table 1). Seven of the 9 adult patients had pulmonary TB, of whom 5 were sputum-smear positive and 4 had pulmonary cavities that were detected by radiography. The other 2 adults had pleural TB. The pediatric patient had culture-negative pulmonary TB diagnosed by clinical presentation and radiographic improvement during treatment with anti-TB medicines. Three patients had both pulmonary cavities and positive sputum smear results. All patients had negative serology results for HIV infection. Eight out of 9 adult patients used methamphetamines. Patients reported smoking, insufflating, and injecting methamphetamines, as well as drinking methamphetamines mixed with coffee. One patient reported a method of methamphetamine use known as “booty bumping,” or anally inserting methamphetamines.22
TABLE 1.
Demographic and Disease Characteristics of Patients With TB (N = 10): Snohomish County, WA, 2005–2006
| No. of Patients | |
| Patient characteristics | |
| Male | 7 |
| Median age, y | 35a |
| Born in the United States | 10 |
| White race | 8 |
| American Indian race | 2 |
| Family member of another patient | 8 |
| Methamphetamine use | 8 |
| Disease characteristics | |
| Pulmonary | 8 |
| Pulmonary cavity | 4 |
| Sputum smear positive | 5 |
| Culture confirmed | 7 |
| Matching M. tuberculosis genotype | 7b |
| Symptomatic | 7 |
| HIV-infected | 0c |
Range 2–54 years.
Genotyping can only be performed on culture-confirmed cases of M. tuberculosis.
All 10 patients were tested.
Links Between Outbreaks
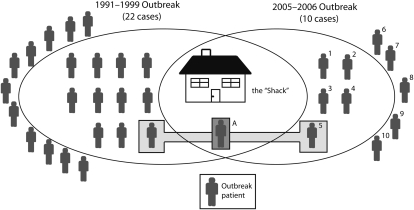
The outbreak included persons linked by social interactions involving substance abuse and by marriage among multiple families. Five patients (patients 1 through 5) were known to spend time in a house they called the “Shack,” where persons would gather to use methamphetamines, other drugs, and alcohol (Figure 1). Patients 6 through 9 were indirectly linked to the Shack by being either a friend or a family member of patients who spent time in the Shack (patients 1 through 4). Patient 10 was a niece (aged 2 years) of patient 1. Eight of the outbreak patients were family members of another outbreak patient.
FIGURE 1.
Social link between past and current TB outbreaks: Snohomish County, WA, 1991–1999 and 2005–2006.
Note. TB = tuberculosis. Patients inside the ovals used drugs at the Shack. Patient in dark box labeled A was infected during the 1991–1999 outbreak, did not complete prophylactic treatment, and later developed and was treated for TB disease in 2002. Patients in boxes connected to Contact/Patient A represent a link between the 1991–1999 and 2005–2006 outbreaks.
Through our investigation we learned that patient 5 was indirectly linked with a TB outbreak that had occurred in the same area 15 years previously. In 1991, a person who was homeless and using illegal drugs at the same Shack implicated in the current outbreak was diagnosed with pulmonary TB disease. The nurse that provided his treatment reported that his use of drugs was a barrier to directly observed therapy and his completion of treatment. This patient took 5 years (and ultimately required court-mandated guarded isolation) to complete an anti-TB treatment regimen that normally takes 6 months. The subsequent TB outbreak lasted until 1999 and involved 22 socially linked patients, at least 11 of whom used drugs at the Shack (Figure 1).23
During the 1991 through 1999 outbreak, a contact designated as “contact A” had a positive TST result (Figure 1). Contact A was known to abuse alcohol and use illegal drugs at the Shack. She initiated but did not complete treatment for LTBI. Contact A subsequently developed active TB disease that was diagnosed and treated in 2002. Contact A is a family member of patient 5 in the current outbreak and represents a direct person-to-person link between the past and current TB outbreaks. In 2006, only 1 isolate from the original 1991 through 1999 outbreak was available for genotyping, and it had a genotype pattern matching the current outbreak strain of M. tuberculosis.
Screening and Treatment
Contact screening efforts in 2006 identified 372 contacts who were named by the recently diagnosed patients, who were named by the patients' contacts, or who were exposed to patients in congregate settings. All contacts but 1 were US born. The contacts were classified as having been exposed either in the community (n = 223), the local jail (n = 143), or the courthouse (n = 6; Table 2). TB control staff located and screened 191 (85.7%) community contacts, 76 (82.6%) jail inmates, 48 (94.1%) jail staff, and 4 (66.7%) courthouse staff. Of those screened, the community contacts had the highest rate of positive TST results (29.8%), followed by jail inmates (22.4%) and jail staff (12.5%). No courthouse staff had a positive TST result. Among community contacts, 52 (91.2%) of those with a positive TST result started treatment of LTBI, and 42 (80.1%) of those who started treatment of LTBI went on to complete it. Among jail inmates, 13 (76.5%) of those with a positive TST result initiated treatment of LTBI, and 9 of those (69.2%) completed treatment. All 6 jail staff who had a positive TST result completed treatment of LTBI.
TABLE 2.
TST Results and Completion of Treatment of LTBI Among Contacts of Patients With TB (N = 372): Snohomish County, WA, 2005–2006
| Contact Groups | Total No. of Contacts | No. Screened with TST (%) | No. With Positive TST Result (%a) | No. of Infected Contacts Who Started LTBI Treatment (%b) | No. of Contacts Who Completed 6 Mo of LTBI Treatment (%c) |
| Total | 372 | 319 (85.8) | 80 (25.1) | 71 (88.8) | 57 (80.3) |
| Community | 223 | 191 (85.7) | 57 (29.8) | 52 (91.2) | 42 (80.1) |
| Jail inmates | 92 | 76 (82.6) | 17 (22.4) | 13 (76.5) | 9 (69.2) |
| Jail staff | 51 | 48 (94.1) | 6 (12.5) | 6 (100) | 6 (100) |
| Courthouse staff | 6 | 4 (66.7) | 0 | 0 | 0 |
Note. LTBI = latent TB infection; TB = tuberculosis; TST = tuberculin skin test.
Percent of those screened.
Percent of those with positive TST.
Percent of those who started LTBI treatment.
Methamphetamine Use Among Contacts
During the initial stage of the investigation, we interviewed contacts about any use of methamphetamines in the previous year. We were able to collect data on methamphetamine use for 67 (56%) of the first 119 community contacts. Methamphetamine use in the previous year was reported by 45 (67%) of the 67 adult community contacts. We had data on methamphetamine use and skin-test results for 34 adult community contacts. Of the adult community contacts who used methamphetamines, 14 (64%) of 22 had a positive skin test indicating LTBI, compared with 3 (25%) of 12 adult named contacts who did not use methamphetamines.
DISCUSSION
In this report we describe transmission of M. tuberculosis within a network of persons linked by marriage, friendship, and frequent use of methamphetamines and other illegal drugs. We found 10 cases that were linked by epidemiogical findings, 7 of which were linked by genotyping. These 10 cases are linked to a previous outbreak of 22 cases that lasted from 1991 through 1999. The outbreaks involved overlapping networks of persons using drugs and abusing alcohol. Although drug use and alcohol abuse were noted during the 1991 through 1999 outbreak, we could not confirm whether methamphetamines were used by patients or their contacts during the earlier outbreak. Methamphetamine use was frequent among the adult patients and their contacts involved in the more recent 2005 through 2006 outbreak.
Illegal drug use and alcohol abuse are common among patients with TB in the United States. These behaviors are associated with sputum smear–positive disease and treatment failure, both indicators of increased transmission.17 In these outbreaks, illegal drug use and alcohol abuse appear to have fueled transmission of M. tuberculosis. Use of methamphetamines and other drugs was the behavior that brought many of the patients and their contacts together. The rate of skin-test positivity was higher among contacts who reported methamphetamine use, suggesting that the risk of exposure to TB was greater among persons who used methamphetamines. Perhaps these patients and contacts were at increased risk for infection because of close person-to-person contact (i.e., using drugs in vans, motel rooms, the Shack, or the drug house), repeated exposure because of chronic use, and poor ventilation in the drug-use sites.21
Methamphetamine use is associated with numerous side effects, including appetite suppression, severe weight loss,24 binge use of the drug,25 periods of sleeplessness,25 and sexual risk behaviors.26 There are no data on methamphetamine use and risk of TB infection or progression from infection to disease, but there are data demonstrating that patients with compromised immune systems are at greater risk for progressing from infection to disease,27 as well as evidence that methamphetamine use leads to immunologic impairments.28
Treating persons for TB disease and finding and treating contacts who have been infected are top priorities of the US strategy for TB elimination.21 Recent outbreaks have highlighted how substance abuse remains a barrier to this strategy at many stages.6,7,29 First, persons who use illegal drugs may delay seeking care,5,7,9,30 are more likely to have positive sputum smear results at diagnosis,17 and are less likely to complete treatment,15 all of which can lead to prolonged transmission and preventable secondary cases. In this outbreak, illegal drug use contributed to patient delays in seeking medical care until the severity of their symptoms led them to seek care at hospital emergency departments for advanced TB disease. We prevented additional cases by providing temporary housing until patients were no longer infectious, then we used incentives and enablers to promote adherence and ensure that all 10 patients completed treatment. Local TB control staff also facilitated entry of patients and contacts into substance abuse treatment. At least 2 of the patients entered substance abuse treatment and were no longer using methamphetamines when they completed their 6-month anti-TB treatment.
Persons who use illegal drugs are also less likely or unable to name their contacts.5,7,12,29 The patients in Snohomish County did not provide complete lists of contacts because (1) they were reluctant to reveal the identities of other persons who used illegal drugs, (2) drug use may have impaired their memory, and (3) they did not know the names or addresses of some of the persons with whom they spent time. The inability to generate a comprehensive list of contacts can result in incomplete contact investigations, ongoing transmission, and preventable cases of TB. None of the current outbreak patients were listed as contacts during the 1991 through 1999 TB outbreak, but at least 5 of the current patients are known to have spent time at the Shack during the initial outbreak.
In an attempt to avoid missing potential cases, we screened persons who had been exposed to patients through social interactions or in a congregate setting, and we interviewed contacts named by multiple patients as if they were outbreak patients to develop a more complete list of contacts for the investigation. All names were entered into a master database used to manage resources during the outbreak. We did not include a variable in the database to retrospectively quantify how many additional contacts were named as a result of each activity, but the use of proxy interviews and location-based finding of contacts resulted in a more complete list of contacts than was generated from the initial patient interviews. We were therefore able to find, screen, and treat more contacts with infection, thereby decreasing the likelihood of missing contacts who could later develop TB disease and continue the chain of transmission.
Finally, persons who use illegal drugs are less likely to be screened for TB and LTBI; once screened, users of illegal drugs are less likely to initiate and complete treatment.11–13 Persons who do not adhere to treatment may remain infectious. Treatment failure is the primary risk factor for developing drug resistance8 and leads to ongoing transmission. Incentives and enablers were provided to address barriers to treatment adherence (e.g., lack of transportation to access services, homelessness, malnourishment). The total cost of incentives and enablers (less than $15 000) was far less than the average cost ($125 000) of treating a single case of MDR-TB that could result from incomplete treatment.31 None of the outbreak patients developed resistance to anti-TB drugs.
To improve access to TB screening services, we screened for TB and LTBI in a variety of nontraditional settings. We screened a total of 319 contacts for LTBI; of those screened, 80 (25%) had positive TST results. The treatment completion rate for contacts with a positive TST result was 71%, which exceeds the 43% to 51% reported for other contact investigations.32–35 Although this investigation was not designed to study and quantify the impact of the outbreak interventions (e.g., enhanced incentives, enablers, screening outreach), the markedly greater treatment success rate for a population characterized by frequent methamphetamine use likely represents the impact of local staff simultaneously addressing TB disease and the social influences on health associated with abuse of alcohol and use of illegal drugs.
The current outbreak may have been preventable because a contact who used drugs from the 1991 through 1999 outbreak was diagnosed with LTBI, did not complete preventive treatment, later developed TB disease, and is a contact of a patient in the current outbreak. The contact's inability to complete treatment was not a result of poor TB-control practices but rather an example of how substance abuse disorders introduce multiple barriers to TB control. TB control programs need the expertise of substance abuse treatment and support organizations to integrate TB control with substance abuse treatment services. For this reason, TB control programs need to reach out to substance abuse programs and develop a plan for collaboration to simultaneously address substance abuse and TB control.
Controlling the current outbreak required that we recognize and address the barriers to care common among persons using drugs and abusing alcohol such as homelessness or unstable housing, lack of transportation, malnourishment, and the amount of time and resources dedicated to acquiring and using drugs. The Snohomish Health District TB Control Program's multidisciplinary collaborative approach, which integrated TB control, outreach, enhanced incentives and enablers, and substance abuse treatment, resulted in high rates of treatment adherence and completion. This experience highlights the resources needed—and the potential impact—when TB control programs collaborate with substance abuse treatment providers and other partners to address the barriers that substance abuse presents to controlling and preventing TB disease.
Acknowledgments
We would like to acknowledge Maggie Osborn, Holliane Bruce, Peggy Schmaus, and the rest of the Snohomish Health District TB Control Program for their contributions to the investigation and response to the outbreak. We would also like to acknowledge Paul Tribble of the Field Services and Evaluation Branch, within the Division of TB Elimination at the Centers for Disease Control and Prevention, and Kimberly Field with the Washington Department of Health for their guidance and support. We are grateful to John Jereb, Kevin Cain, and Lisa Jeannotte for their critical reviews of the article and to Sharon McAleer for her graphics support.
Human Participant Protection
This investigation was deemed to be an urgent public health response and, under the federal regulation for the protection of human research participants (CFR title 45, part 46), was determined not to be human subject research by the National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention. Therefore, no protocol approval was necessary.
References
- 1.Reichman LB, Felton CP, Edsall JR. Drug dependence, a possible new risk factor for tuberculosis disease. Arch Intern Med. 1979;139(3):337–339 [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Crack cocaine use among persons with tuberculosis—Contra Costa County, California, 1987–1990. MMWR Morb Mortal Wkly Rep. 1991;40(29):485–489 [PubMed] [Google Scholar]
- 3.Kline SE, Hedemark LL, Davies SF. Outbreak of tuberculosis among regular patrons of a neighborhood bar. N Engl J Med. 1995;333(4):222–227 [DOI] [PubMed] [Google Scholar]
- 4.Leonhardt KK, Gentile F, Gilbert BP, Aiken M. A cluster of tuberculosis among crack house contacts in San Mateo County, California. Am J Public Health. 1994;84(11):1834–1836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Malakmadze N, Gonzalez IM, Oemig T, et al. Unsuspected recent transmission of tuberculosis among high-risk groups: implications of universal tuberculosis genotyping in its detection. Clin Infect Dis. 2005;40(3):366–373 [DOI] [PubMed] [Google Scholar]
- 6.McElroy PD, Rothenberg RB, Varghese R, et al. A network-informed approach to investigating a tuberculosis outbreak: implications for enhancing contact investigations. Int J Tuberc Lung Dis. 2003;7(12, suppl 3):S486–S493 [PubMed] [Google Scholar]
- 7.Oeltmann JE, Oren E, Haddad MB, et al. Tuberculosis outbreak in marijuana users, Seattle, Washington, 2004. Emerg Infect Dis. 2006;12(7):1156–1159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Deiss RG, Rodwell TC, Garfein RS. Tuberculosis and illicit drug use: review and update. Clin Infect Dis. 2009;48(1):72–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chin DP, Crane CM, Diul MY, et al. Spread of Mycobacterium tuberculosis in a community implementing recommended elements of tuberculosis control. JAMA. 2000;283(22):2968–2974 [DOI] [PubMed] [Google Scholar]
- 10.Curtis R, Friedman SR, Neaigus A, Jose B, Goldstein M, Des Jarlais DC. Implications of directly observed therapy in tuberculosis control measures among IDUs. Public Health Rep. 1994;109(3):319–327 [PMC free article] [PubMed] [Google Scholar]
- 11.Brassard P, Bruneau J, Schwartzman K, Senecal M, Menzies D. Yield of tuberculin screening among injection drug users. Int J Tuberc Lung Dis. 2004;8(8):988–993 [PubMed] [Google Scholar]
- 12.Howard AA, Klein RS, Schoenbaum EE, Gourevitch MN. Crack cocaine use and other risk factors for tuberculin positivity in drug users. Clin Infect Dis. 2002;35(10):1183–1190 [DOI] [PubMed] [Google Scholar]
- 13.LoBue PA, Moser KS. Use of isoniazid for latent tuberculosis infection in a public health clinic. Am J Respir Crit Care Med. 2003;168(4):443–447 [DOI] [PubMed] [Google Scholar]
- 14.Goble M, Iseman MD, Madsen LA, Waite D, Ackerson L, Horsburgh CR. Treatment of 171 patients with pulmonary tuberculosis resistant to isoniazid and rifampin. N Engl J Med. 1993;328(8):527–532 [DOI] [PubMed] [Google Scholar]
- 15.Burman WJ, Cohn DL, Rietmeijer CA, Judson FN, Sbarbaro JA, Reves RR. Noncompliance with directly observed therapy for tuberculosis. Epidemiology and effect on the outcome of treatment. Chest. 1997;111(5):1168–1173 [DOI] [PubMed] [Google Scholar]
- 16.Blackwell B. Drug therapy: patient compliance. N Engl J Med. 1973;289(5):249–252 [DOI] [PubMed] [Google Scholar]
- 17.Oeltmann JE, Kammerer JS, Pevzner ES, Moonan PK. Tuberculosis and substance abuse in the United States, 1997–2006. Arch Intern Med. 2009;169(2):189–197 [DOI] [PubMed] [Google Scholar]
- 18.Snyder DC, Paz EA, Mohle-Boetani JC, Fallstad R, Black RL, Chin DP. Tuberculosis prevention in methadone maintenance clinics. Effectiveness and cost-effectiveness. Am J Respir Crit Care Med. 1999;160(1):178–185 [DOI] [PubMed] [Google Scholar]
- 19.Snohomish Health District Communicable Disease Report, 2003–2007. Everett, WA: Snohomish Health District; 2009. Available at: http://www.snohd.org/snoComDisease/tempdocs/CD_Report_2007.pdf. Accessed August 1, 2009 [Google Scholar]
- 20.Barnes PF, Cave MD. Molecular epidemiology of tuberculosis. N Engl J Med. 2003;349(12):1149–1156 [DOI] [PubMed] [Google Scholar]
- 21.Centers for Disease Control and Prevention Guidelines for the investigation of contacts of persons with infectious tuberculosis. Recommendations from the National Tuberculosis Controllers Association and CDC. MMWR Recomm Rep. 2005;54(RR-15):1–47 [PubMed] [Google Scholar]
- 22.Cantrell FL, Breckenridge HM, Jost P. Transrectal methamphetamine use: a novel route of exposure. Ann Intern Med. 2006;145(1):78–79 [DOI] [PubMed] [Google Scholar]
- 23.Spitters CM, Columbel C, Yang Z, Cave MD. Control of an ongoing tuberculosis outbreak involving a disadvantaged social network. Poster presented at: Third Annual Meeting of the International Union Against Tuberculosis and Lung Disease—North American Region; February 26–29, 1998; Vancouver, BC, Canada [Google Scholar]
- 24.Nordahl TE, Salo R, Leamon M. Neuropsychological effects of chronic methamphetamine use on neurotransmitters and cognition: a review. J Neuropsychiatry Clin Neurosci. 2003;15(3):317–325 [DOI] [PubMed] [Google Scholar]
- 25.Sommers I, Baskin D, Baskin-Sommers A. Methamphetamine use among young adults: health and social consequences. Addict Behav. 2006;31(8):1469–1476 [DOI] [PubMed] [Google Scholar]
- 26.Mansergh G, Purcell DW, Stall R, et al. CDC consultation on methamphetamine use and sexual risk behavior for HIV/STD infection: summary and suggestions. Public Health Rep. 2006;121(2):127–132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Iseman MD. A Clinician's Guide to Tuberculosis. Philadelphia, PA: Lippincott Williams & Wilkins; 2000 [Google Scholar]
- 28.Mahajan SD, Hu Z, Reynolds JL, Aalinkeel R, Schwartz SA, Nair MP. Methamphetamine modulates gene expression patterns in monocyte derived mature dendritic cells: implications for HIV-1 pathogenesis. Mol Diagn Ther. 2006;10(4):257–269 [DOI] [PubMed] [Google Scholar]
- 29.Fitzpatrick LK, Hardacker JA, Heirendt W, et al. A preventable outbreak of tuberculosis investigated through an intricate social network. Clin Infect Dis. 2001;33(11):1801–1806 [DOI] [PubMed] [Google Scholar]
- 30.Storla DG, Yimer S, Bjune GA. A systematic review of delay in the diagnosis and treatment of tuberculosis. BMC Public Health. 2008;8:15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rajbhandary SS, Marks SM, Bock NN. Costs of patients hospitalized for multidrug-resistant tuberculosis. Int J Tuberc Lung Dis. 2004;8(8):1012–1016 [PMC free article] [PubMed] [Google Scholar]
- 32.Reichler MR, Reves R, Bur S, et al. Treatment of latent tuberculosis infection in contacts of new tuberculosis cases in the United States. South Med J. 2002;95(4):414–420 [PubMed] [Google Scholar]
- 33.Jereb J, Etkind SC, Joglar OT, Moore M, Taylor Z. Tuberculosis contact investigations: outcomes in selected areas of the United States, 1999. Int J Tuberc Lung Dis. 2003;7(12, suppl 3):S384–S390 [PubMed] [Google Scholar]
- 34.Marks SM, Taylor Z, Qualls NL, Shrestha-Kuwahara RJ, Wilce MA, Nguyen CH. Outcomes of contact investigations of infectious tuberculosis patients. Am J Respir Crit Care Med. 2000;162(6):2033–2038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sprinson JE, Flood J, Fan CS, et al. Evaluation of tuberculosis contact investigations in California. Int J Tuberc Lung Dis. 2003;7(12, suppl 3):S363–S368 [PubMed] [Google Scholar]