Abstract
Objectives. We examined the feasibility and effectiveness of using culturally sensitive collaborative treatment (CSCT) to improve recognition, engagement, and treatment of depressed Chinese Americans in primary care.
Methods. Chinese American patients in a primary care setting (n = 4228) were screened for depression. The primary study outcome was treatment engagement rate, and the secondary outcome was treatment response.
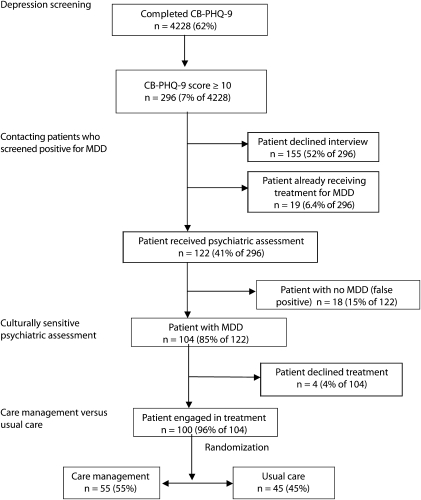
Results. Of the study participants, 296 (7%) screened positive for depression, 122 (41%) of whom presented for a psychiatric assessment; 104 (85%) were confirmed with major depressive disorder, and 100 (96%) of these patients were randomized into treatment involving either care management or usual care. Patients in the care management and usual care groups did not differ in terms of their outcomes. CSCT resulted in a nearly 7-fold increase in treatment rate among depressed patients in primary care.
Conclusions. CSCT is both feasible and effective in improving recognition and treatment engagement of depressed Chinese Americans. Care management may have limited effects on depressed patients treated by psychiatrists, given that these patients tend to have favorable responses in general.
Asian Americans underuse mental health services, even though studies have shown that major depressive disorder (MDD) is common among this group,1 with a prevalence comparable to that among the US mainstream population.2,3 Most Asian Americans with MDD seek help at primary care settings,4 but in the majority of cases their depression remains unrecognized by care providers.5
Katon et al. proposed a collaborative model for treating depression in primary care settings.6 The model involved a multidisciplinary approach in which primary care physicians, psychiatrists, and care managers work together to provide intervention, patient education, and surveillance of adherence to medication treatment. Using a randomized control study, Katon et al. demonstrated that collaborative care results in more favorable outcomes and improved satisfaction among patients with MDD.6
There are significant cultural barriers to implementing collaborative management of depression for Asian American immigrants. Many of these individuals are unfamiliar with the concept of MDD, have language barriers, and schedule physician visits only if they have physical symptoms. Physicians with inadequate cultural sensitivity may overlook depression among this population.7 When diagnosed with MDD, many Chinese Americans avoid mental health services because of their culture's strong stigma toward psychiatric disorders.4,8
To overcome such barriers, we designed the culturally sensitive collaborative treatment (CSCT) model by adding a cultural component to the collaborative management model with the goal of serving Asian immigrants who have traditional beliefs regarding mental illnesses.9 CSCT contains 4 components: systematic depression screening, contacting those who screen positive for MDD to recommend an assessment, culturally sensitive psychiatric assessment via the Engagement Interview Protocol (EIP), and care management. The first 2 components are integral parts of CSCT because, without the screening and contacting steps, most depressed Asian American patients would remain unrecognized in primary care clinics.5
Our team designed the EIP by adding a cultural component to the standard psychiatric interview. This cultural component explores patients’ illness beliefs by using the questions designed by Kleinman10 so that clinicians can develop co-constructed illness narratives with patients by reframing the Western concept of depression into more culturally resonant forms.
In this study, conducted among patients in a primary care clinic serving predominantly Chinese immigrants, we examined the feasibility of systematically screening patients for depression, contacting patients who screened positive, and conducting culturally sensitive psychiatric assessments to recognize and engage patients in treatment. Using a randomized trial, we investigated the efficacy of adding care management to the treatment of MDD.
METHODS
Participants were recruited from South Cove Community Health Center (hereafter South Cove) in Boston, Massachusetts, between September 2004 and February 2007. South Cove served 12 000 patients during the study period, predominantly (more than 94%) Chinese Americans with financial, language, and cultural barriers to health care. Participants were limited to Chinese American adults (18 years or older) who attended South Cove's primary care clinic. Patients with unstable medical conditions, a high risk of suicide, psychotic disorders, dysthymic disorder, bipolar disorder, and substance use disorders were excluded.
Procedure
Systematic depression screening. Depression screening has been a quality improvement measure at South Cove since 1999. Patients were asked to complete the Chinese Bilingual Patient Health Questionnaire-9 (CB-PHQ-9) and return the questionnaire before their clinic visit. Patients who had participated in the past 3 months were exempted from repeat screening.
Establishing contact patients with who screened positive for depression. The research team telephoned patients who screened positive for depression (a CB-PHQ-9 score of 10 or above) to inform them about the results of their screening. During this call, patients were also informed about our study.
Culturally sensitive psychiatric assessment. Participants completed an informed consent form before they received a psychiatric assessment via the EIP from one of the bilingual research psychiatrists. The EIP has 2 components: a standard psychiatric interview component and a cultural component that uses Kleinman's questions (described subsequently) to explore patients’ illness beliefs. With knowledge of patients’ illness beliefs, the psychiatrist introduced information on depression in ways that were compatible with patients’ beliefs.10 In addition to the EIP, we used the stigma scale of the Explanatory Model of Interview Catalogue11 to measure patients’ perceived level of stigma regarding their illness, a potential confounder of depression treatment outcomes.
After their psychiatric assessments, patients with confirmed MDD were encouraged to seek treatment of their depression from their primary care physicians, who would receive a letter about the patient's diagnosis and a recommended treatment plan. Patients could also choose to seek treatment or consultation from a psychiatrist or a therapist at South Cove.
Efficacy of care management. To assess the efficacy of care management, we used a computer-generated table to randomize participants who agreed to receive treatment for depression into 2 groups: care management or usual care. Patients in both groups were encouraged to discuss depression treatment with their primary care physicians. Patients could also choose to be treated by psychologists or psychiatrists at South Cove.
At the beginning of the study, a bilingual care manager met with patients in the care management group to establish rapport, explain the roles of the care manager, and provide education on MDD. Subsequent contacts, which occurred at the 2nd, 4th, 8th, 12th, 16th, 20th, and 24th weeks through telephone calls, focused on monitoring of depressive symptoms, adherence to medication treatment, management of adverse events, and knowledge of self-management strategies. Care managers were accessible to patients via telephone and served as a link between patients, primary care physicians, and consulting psychiatrists, facilitating patients’ depression treatment. The principal investigator provided weekly supervision to care managers, as well as consultations with patients and their primary care physicians. Participants in the usual care group did not receive the care management component.
Bilingual blind assessors evaluated treatment outcomes of patients in both the care management group and the usual care group at 1.5, 3.5, and 6 months. The 17-item Hamilton Rating Scale for Depression (HAM-D-17) was the primary outcome measurement instrument, and the Clinical Global Impression (CGI) scale was the secondary instrument.
Instruments
Chinese Bilingual Patient Health Questionnaire-9. The Patient Health Questionnaire-9 (PHQ-9) is a self-administered instrument designed to detect MDD in primary care settings; the PHQ-9 has a sensitivity of 88% and a specificity of 88%.12 Our team translated the PHQ-9 into Chinese to create the CB-PHQ-9, a questionnaire shown to have excellent sensitivity (92%) and specificity (95%)13 for depression screening among Chinese Americans.
Hamilton Rating Scale for Depression. The HAM-D-1714,15 is a 17-item clinician rating scale for depression. Questions focus on neurovegetative and other depressive symptoms experienced by patients over the preceding 7 days. Items are rated on a scale of zero to 4 or zero to 2, with higher scores indicating more severe pathology. Scores on the HAM-D-17 are grouped into the following categories: not depressed (0–6), mildly depressed (7–14), moderately depressed (15–25), and severely depressed (above 25). The HAM-D-17 is a widely used instrument for assessing depression, and its reliability and validity are high.16
Engagement Interview Protocol. The EIP is a semistructured interview protocol developed by our team. We created the instrument by combining the Chinese-bilingual Structured Clinical Interview for Axis I DSM-IV Disorders (κ > 0.75 for interrater reliability in diagnosing MDD)17,18 with patients’ illness narratives and beliefs derived from Kleinman's set of questions: “What do you call your problem? What do you think has caused your problem? Why do you think it started when it did? What does your sickness do to you? How does it work? How severe is it? Will it have a short or long course? What do you fear most about your sickness? What are the chief problems the sickness has caused for you? What kind of treatment do you think you should receive? What are the most important results you hope to receive from the treatment?”10
Patients’ illness narratives provide clinicians with information on how patients conceptualize their illness, as expressed in their own language and words. Building on patients’ illness beliefs enhances communication of psychiatric diagnoses through a framework that the patient can understand.
Clinical Global Impression Severity scale (CGI-S) and CGI-Improvement scale (CGI-I). These 2 clinician-rated scales assess patients’ overall improvement with respect to their illnesss.19 The CGI-S scale measures the current condition of the patient on a scale of 1 (normal) to 7 (severe illness); the CGI-I scale measures the patient's degree of improvement, as perceived by the clinician, since the start of treatment on a scale of 1 to 7 (1 = very much improved, 7 = very much worse). Improvement in CGI ratings is used to determine the degree of response over time to a given treatment.
Data Analyses
To examine the feasibility and acceptability of CSCT and its components, we used descriptive statistics to determine the number and percentage of patients who completed depression screening, the percentage of patients who screened positive for MDD, the success rate achieved in terms of contacting patients with positive results and asking them whether they would agree to receive a psychiatric assessment, and the success rate of the culturally sensitive psychiatric assessment in engaging depressed Chinese American patients in treatment.
To examine the efficacy of the CSCT care management component, we used the χ2 test to compare the care management and usual care groups with respect to their response rates and remission rates, and we used the Student t test to compare group members’ final CGI-S and CGI-I scores. A positive response to treatment was defined as a decrease of 50% or more in a patient's HAM-D-17 score, and remission was defined as a score of 7 or less on the HAM-D-17 at the patient's most recent assessment. We also compared the demographic characteristics and clinical histories of participants in the 2 groups to explore potential confounders of treatment outcomes. SPSS software was used in conducting the statistical analyses.20
Finally, we examined the overall effectiveness of CSCT by calculating the percentage of patients screened for depression and comparing the percentages of patients engaged in treatment before their exposure to CSCT (as determined at the depression screening) and after they had been contacted and had completed a psychiatric assessment.
RESULTS
The outcomes from the implementation of the key CSCT elements (depression screening, contacting patients with positive results, culturally sensitive psychiatric assessment, care management, and overall effectiveness) are described in the sections to follow.
Depression Screening
During the 30-month study period, 6820 copies of the CB-PHQ-9 were distributed to patients who visited the South Cove primary care clinic. After exclusion of 2169 (32%) forms that were returned blank, 409 (6%) forms from individuals who had undergone screening within the preceding 3 months, and 14 (0.2%) forms from patients with duplicate positive screens, 4228 (62%) completed forms were available for the data analysis. During the study period, South Cove treated approximately 12 000 patients. Thus, we screened 35% of the clinic's patients. We compared the demographic characteristics of patients who agreed to be interviewed with the characteristics of those patients who declined psychiatric interviews or did not respond to requests and found that the 2 groups did not differ significantly in terms of mean age (50 years, SD = 17 vs 49 years, SD = 15, respectively) or gender composition (72% female vs 66% female).
Contacting Patients Who Screened Positive
Of the 4228 participants who completed the CB-PHQ-9, a total of 296 (7%) screened positive for MDD; among those screening positive, 19 (6.5%) had been receiving psychiatric treatment for depression, and 155 (52%) either declined a psychiatric interview or did not return our telephone calls. The remaining 122 (41%) participants who screened positive agreed to and showed up for a psychiatric assessment.
Culturally Sensitive Psychiatric Assessment
Among the 122 patients who received a culturally sensitive psychiatric assessment, 104 (85%) were confirmed with MDD. This finding indicates that the CB-PHQ-9 has a true-positive rate of 85% (104/122) and a false-positive rate of 15% ([122 − 104]/122). Most patients were not aware they were suffering from depression and attributed their symptoms to medical illnesses or difficulties in their lives. Of the 104 patients identified with MDD, 100 (96%) agreed to receive treatment for depression and 4 (4%) declined treatment (Figure 1).
FIGURE 1.
Recognition and treatment engagement outcomes of culturally sensitive collaborative treatment of depressed Chinese Americans in primary care: Boston, MA, 2004–2007.
Note. CB-PHQ-9 = Chinese Bilingual Patient Health Questionnaire-9; MDD = major depressive disorder.
Efficacy of Care Management
Of the 100 depressed Chinese Americans who agreed to receive treatment for depression (68% female; mean age = 49 years, SD = 15), 55 (55%) were randomized to receive care management via telephone and 45 (45%) were randomized to usual care. The baseline and demographic characteristics and the treatment outcomes of the participants in the 2 groups are presented in Table 1. The percentage of female patients in the care management group was higher than was the percentage in the usual care group (80% vs 55%; P = .005), and fewer patients in the care management group had a history of psychiatric disorder (27% vs 53%; P = .01).
TABLE 1.
Baseline Characteristics and Treatment Outcomes of Participants Randomized Into the Care Management and Usual Care Groups: Boston, MA, 2004–2007
| Care Management | Usual Care | t | χ2 | df | P | |
| Characteristic | ||||||
| Age, y, mean (SD) | 51 (17) | 48 (15) | −1.0 | 97 | .3 | |
| Female, % | 80 | 55 | 8.0 | 1 | .005 | |
| Years in United States, mean (SD) | 11 (9) | 11 (8) | −0.07 | 96 | .9 | |
| Education, y, mean (SD) | 10 (4) | 9 (5) | −1.0 | 96 | .3 | |
| Baseline HAM-D-17 score, mean (SD) | 21 (5) | 21 (5) | −0.4 | 96 | .4 | |
| Baseline CB-PHQ-9 score, mean (SD) | 18 (4) | 18 (4) | 0.19 | 84 | .8 | |
| Baseline CGI-S score, mean (SD) | 4 (0) | 4 (0.2) | 1.0 | 43 | .3 | |
| Stigma score, mean (SD) | 13 (14) | 11 (14) | −0.5 | 95 | .9 | |
| Psychiatric history, % | 27 | 53 | 7.0 | 1 | .01 | |
| Family psychiatric history, % | 18 | 10 | 1.4 | 1 | .4 | |
| Treated by psychiatrist, % | 64 | 54 | 1.3 | 1 | .3 | |
| Depression treatment outcomes | ||||||
| Response rate, % | 60 | 50 | 1.2 | 1 | .2 | |
| Remission rate, % | 48 | 37 | 1.2 | 1 | .2 | |
| Most recent CGI-S score, mean | 2.7 | 2.5 | 0.8 | 88 | .8 | |
| Most recent CGI-I score, mean | 2.8 | 2.8 | −0.3 | 76 | .2 | |
Note. HAM-D-17 = Hamilton Rating Scale for Depression; CB-PHQ-9 = Chinese Bilingual Patient Health Questionnaire-9; CGI-S = Clinical Global Impression Severity scale; CGI-I = Clinical Global Impression Improvement scale.
However, regression analyses in which treatment response, treatment remission, CGI-S score, or CGI-I score was the dependent variable showed that none of the baseline or demographic characteristics, including gender and positive psychiatric history, were related to treatment outcomes (data available on request). As a result, there were no confounders to control for in treatment outcome analyses. The care management group and the usual care group did not differ significantly in their treatment outcomes; the groups’ respective response rates were 60% and 50%, their remission rates were 48% and 37%, their mean CGI-S scores were 2.7 and 2.5, and their mean CGI-I scores were 2.8 and 2.8 (Table 1).
Overall Effectiveness of Culturally Sensitive Collaborative Treatment
During the 30-month study period, we successfully screened 4228 patients, or 35% of the primary care clinic's patients. Before CSCT, only 6.5% of patients (19 of 296) who screened positive for MDD in this study were receiving psychiatric treatment. After exclusion of the 19 patients who were already being treated and the 44 patients who were estimated not to have MDD (based on the 15% false-positive rate of the CB-PHQ-9), we identified 233 Chinese Americans with untreated MDD. By implementing the first 3 CSCT components (systematic depression screening, contacting those who screen positive, and culturally sensitive psychiatric assessment), we engaged 100 untreated Chinese American patients (43% of those identified) in MDD treatment, a nearly 7-fold increase from the initial (pre-CSCT) 6.5% treatment rate.
DISCUSSION
In this study, we have demonstrated the feasibility of using the CSCT model to improve recognition and treatment of depressed Chinese Americans in primary care. Before implementation of CSCT, only 6.5% (Figure 1) of depressed patients in the clinic received psychiatric treatment. The present findings are compatible with results from our earlier studies indicating that the majority of Chinese immigrants with depression remain underrecognized and undertreated.5
With CSCT, we successfully recognized and engaged 43% of untreated Chinese American patients with MDD in depression treatment, with additional care management or without care management (the usual care group). The treatment outcomes of both groups of patients were comparable to the outcomes of the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study,21 the largest clinical trial on depression conducted among the mainstream US population. These favorable outcomes are particularly encouraging given that many of our participants were underserved Chinese immigrants who generally hold on to their traditional beliefs regarding depression, underreport their mood symptoms, and underuse mental health services.5
Systematic Depression Screening and Contact With Patients
In 2002, the US Preventive Services Task Force recommended that adult patients be screened for depression in clinical practices that have systems in place to ensure accurate diagnoses and effective treatment and follow-up.22 However, implementation of this recommendation has been sporadic in primary care clinics. In this study, we systematically screened Chinese American patients for depression, actively contacted those with positive results to alert them to their illness, and recommended psychiatric assessments. Our results demonstrate the feasibility and importance of systematically screening and approaching depressed Chinese Americans in primary care; 7% of our participants screened positive for MDD, and among them 41% agreed to a psychiatric assessment when they were contacted.
Culturally Sensitive Psychiatric Assessment
In our earlier studies, we found that many Chinese immigrants were unfamiliar with mental disorders, and cultural barriers were key reasons for disparities in treatment of MDD between this group and the mainstream US population. Stockdale et al. argued that quality improvement efforts are needed to address cultural and linguistic barriers to care.23 In this study, we employed culturally sensitive psychiatric assessments so that clinicians could overcome cultural barriers by communicating illness information in a way that is comprehensible to patients. In total, 96% of depressed Chinese immigrants who completed assessments agreed to be treated for their illness. If replicated in future studies, CSCT could be a viable model to decrease MDD treatment disparities among Asians and other ethnic minority populations in the United States who face cultural barriers in seeking help for their mental illnesses.
Care Management
Care management is a key component of collaborative management, and is effective in treating depression.24–26 In this study, we found no significant differences in treatment outcomes between members of the care management group and the usual care group. One possible interpretation is that care management is not effective for this population. Many depressed Chinese immigrants face obstacles to treatment for depression, including lack of health insurance, inability to make copayments for doctors’ visits and medications, difficulties in arranging transportation, and prejudice against use of psychotropic medications.
The treatment outcomes, however, were good among the care management group as well as among the usual care group; response rates and remission rates for both groups were comparable with or even better than were the rates reported among the mainstream population.21 Such findings suggest a more plausible interpretation for the lack of significant differences—that high percentages of patients from both the care management and usual care groups (64% and 54%, respectively) chose to receive treatment from psychiatrists at South Cove, resulting in favorable outcomes among both groups. This interpretation is compatible with the results of Simon et al., who found that a telephone care management program did not lead to significant improvements among patients treated by psychiatrists.27
Implementation of collaborative models is undoubtedly influenced by the culture of the host institution and the preferences of its providers. In this study, many primary care physicians encouraged patients to seek help at the South Cove behavioral health department for their depression, leading to a high level of involvement of psychiatrists in the patients’ treatment. We observed that when psychiatric services are delivered with cultural sensitivity, Chinese Americans will accept and use these services despite their stigma regarding mental health disorders.
Future studies assessing the efficacy of care management may need to be performed separately among patients who are treated by primary care physicians and patients who are treated by mental health providers to account for the potential influence of provider type on treatment outcomes. In addition, to eliminate potential ceiling effects resulting from treatment by psychiatrists, psychiatrists should provide consultations only when necessary. That a higher percentage of female participants than of male participants in our study engaged in treatment may reflect lower help-seeking tendencies among Asian men.28,29 The imbalance of numbers and gender representation between the 2 groups could be a chance finding resulting from our relatively small sample.
Limitations
There were several limitations associated with this study. First, we used a descriptive, uncontrolled design to examine the CSCT components of depression screening, patient contact, and psychiatric assessment. Given that this was the first study on CSCT, our focus was on investigating its feasibility and overall effectiveness in decreasing disparities in depression treatment among Chinese Americans.
Second, systematic depression screening is a laborious procedure. Systematic screening may not be sustainable without additional resources provided by health insurance plans or health care institutions after support from research studies has ended. Yet, there have been some encouraging developments in support of depression screening in primary care. One is the growing use of computerized medical records, which is an inexpensive means of patient tracking that facilitates implementation of depression screening in primary care. The Veterans Affairs hospital systems have pioneered the use of depression screening as part of patients’ annual physical examinations. In Massachusetts, a law was passed in 2008 that requires primary care physicians to routinely screen children for behavioral health problems and requires health insurance companies to reimburse the costs of such screening.30
Third, only 41% of our participants who screened positive agreed to be interviewed, and a high percentage of those with positive results (52%) declined or did not respond. The cutoff point for positive results (a CB-PHQ-9 score of 10 or above) may have been too low, which would have led to screening being performed with high sensitivity but relatively low specificity, and subsequently many patients with positive results were not clinically depressed. Future studies are needed to investigate whether use of a higher threshold would be more cost-effective for depression screening in primary care settings. It is also possible that depressed patients who screened positive were in denial of their condition or avoided mental health services because they were concerned about stigma. In an earlier study investigating the reasons why patients with positive screening results declined psychiatric interviews, patients indicated they did not consider themselves as having a psychiatric condition or they preferred to hold off on treatment.5
Finally, although a very high percentage (96%) of patients confirmed with MDD were treated for their depression after the EIP interview, it is possible that factors other than the EIP, such as our inclusion of experienced, native-speaking clinicians, contributed to the success of the intervention. Future research is needed to show that our results are generalizable to other settings, particularly those where clinicians and patients have different cultural backgrounds.
Conclusions
Depression is common among Chinese Americans in primary care settings, and many depressed Chinese Americans remain untreated by their primary care providers. We found that CSCT, a comprehensive approach with key elements including depression screening, actively contacting patients with positive results, culturally sensitive psychiatric assessment, and care management improved the recognition and treatment engagement of depressed Chinese Americans in primary care.
Acknowledgments
This project was supported by a grant (MH67085) from the National Institute of Mental Health.
Human Participant Protection
This study was approved by the institutional review board of Massachusetts General Hospital. Patients provided informed consent before undergoing psychiatric assessments.
References
- 1.Mental Health: A Report of the Surgeon General—Executive Summary. Washington, DC: US Department of Health and Human Services; 1999 [Google Scholar]
- 2.Yeung A, Chan R, Mischoulon D, et al. Prevalence of major depressive disorder among Chinese-Americans in primary care. Gen Hosp Psychiatry. 2004;26(1):24–30 [DOI] [PubMed] [Google Scholar]
- 3.Takeuchi DT, Chung RC, Lin KM, et al. Lifetime and twelve-month prevalence rates of major depressive episodes and dysthymia among Chinese Americans in Los Angeles. Am J Psychiatry. 1998;155(10):1407–1414 [DOI] [PubMed] [Google Scholar]
- 4.Yeung A, Kung WW, Chung H, et al. Integrating psychiatry and primary care improves treatment acceptability among Asian Americans. Gen Hosp Psychiatry. 2004;26(4):256–260 [DOI] [PubMed] [Google Scholar]
- 5.Yeung A, Yu SC, Fung F, et al. Recognizing and engaging depressed Chinese Americans in treatment in a primary care setting. Int J Geriatr Psychiatry. 2006;21(9):819–823 [DOI] [PubMed] [Google Scholar]
- 6.Katon W, Korff MV, Lin E, et al. Collaborative management to achieve treatment guidelines: impact on depression in primary care. JAMA. 1995;273(13):1026–1031 [PubMed] [Google Scholar]
- 7.Yeung AS, Kam R. Illness beliefs of depressed Asian Americans in primary care. : Georgiopoulos AM, Rosenbaum JF, Perspectives in Cross-Cultural Psychiatry. Philadelphia, PA: Lippincott Williams & Wilkins; 2005:21–36 [Google Scholar]
- 8.Fogel J, Ford DE. Stigma beliefs of Asian Americans with depression in an Internet sample. Can J Psychiatry. 2005;50(8):470–478 [DOI] [PubMed] [Google Scholar]
- 9.Yeung A, Fisher L, Wang WC, et al. Culturally sensitive treatment of depressed Chinese Americans in primary care: outcomes of six-months’ intervention. Paper presented at: 160th Annual Meeting of the American Psychiatric Association, May 19–24, 2007, San Diego, CA [Google Scholar]
- 10.Kleinman A. Patients and Healers in the Context of Culture: An Exploration of the Borderline Between Anthropology, Medicine, and Psychiatry. Berkeley: University of California Press; 1980 [Google Scholar]
- 11.Weiss MG, Doongaji DR, Siddhartha S, et al. The Explanatory Model Interview Catalogue (EMIC): contribution to cross-cultural research methods from a study of leprosy and mental health. Br J Psychiatry. 1992;160(6):819–830 [DOI] [PubMed] [Google Scholar]
- 12.Spitzer RL, Kroenke K, Williams JBW. Validity and utility of a self-report version of PRIME-MD: the PHQ Primary Care Study. JAMA. 1999;282(18):1737–1744 [DOI] [PubMed] [Google Scholar]
- 13.Yeung A, Fung F, Yu SC, et al. Validation of the Patient Health Questionnaire-9 for depression screening among Chinese Americans. Compr Psychiatry. 2008;49(2):211–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23(1):56–62 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ryder AG, Goldbloom DS, Schuller DR, et al. Use of psychometric principles in evaluating the Hamilton Depression Rating Scale. Dir Psychiatry. 2005;25(21):241–255 [Google Scholar]
- 16.Dozois DJ. The psychometric characteristics of the Hamilton Depression Inventory. J Pers Assess. 2003;80(1):31–40 [DOI] [PubMed] [Google Scholar]
- 17.Kam ESI, Leung CM, Chung D, et al. The Chinese-Bilingual SCID-I/P Project: stage 1—reliability for mood disorders and schizophrenia. Hong Kong J Psychiatry. 2003;13(1):7–18 [Google Scholar]
- 18.First MB, Gibbon M, Spitzer RL, et al. Structured Clinical Interview for Axis I DSM-IV Disorders—Patient Edition. New York, NY: New York State Psychiatric Institute; 1996 [Google Scholar]
- 19.Guy W. Assessment Manual for Psychopharmacology. Washington, DC: US Government Printing Office; 1976 [Google Scholar]
- 20.SPSS Base 16 for Windows: User's Guide. Chicago, IL: SPSS Inc;2008 [Google Scholar]
- 21.Trivedi MH, Rush AJ, Wisniewski SR, et al. Evaluation of outcomes with citalopram for depression using measurement-based care in STAR*D: implications for clinical practice. Am J Psychol. 2006;163(1):28–40 [DOI] [PubMed] [Google Scholar]
- 22.US Preventive Services Task Force Screening for depression: recommendations and rationale. Available at: http://www.ahrq.gov/clinic/3rduspstf/depression/depressrr.htm. Accessed September 5, 2010
- 23.Stockdale SE, Lagomasino IT, Siddique J, et al. Racial and ethnic disparities in detection and treatment of depression and anxiety among psychiatric and primary health care visits, 1995–2005. Med Care. 2008;46(7):668–677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wang PS, Simon GE, Avorn J, et al. Telephone screening, outreach, and care management for depressed workers and impact on clinical and work productivity outcomes: a randomized controlled trial. JAMA. 2007;298(12):1401–1411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Simon GE, VonKorff M, Rutter C, et al. Randomised trial of monitoring, feedback, and management of care by telephone to improve treatment of depression in primary care. BMJ. 2000;320(7234):550–554 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Unutzer J, Katon W, Callahan CM, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288(22):2836–2845 [DOI] [PubMed] [Google Scholar]
- 27.Simon GE, Ludman EJ, Tutty S, et al. Telephone psychotherapy and telephone care management for primary care patients starting antidepressant treatment: a randomized controlled trial. JAMA. 2004;292(8):935–942 [DOI] [PubMed] [Google Scholar]
- 28.Yi SH, Tidwell R. Adult Korean Americans: their attitudes toward seeking professional counseling services. Community Ment Health J. 2005;41(5):571–580 [DOI] [PubMed] [Google Scholar]
- 29.Sen B. Adolescent propensity for depressed mood and help seeking: race and gender differences. J Ment Health Policy Econ. 2004;7(3):133–145 [PubMed] [Google Scholar]
- 30.Goldberg C. Mental screening for young to begin. Available at: http://www.boston.com/news/local/articles/2007/12/27/mental_screening_for_young_to_begin/?page=2. Accessed September 5, 2010