Abstract
Objectives. We describe age and gender trends in long-term use of prescribed opioids for chronic noncancer pain in 2 large health plans.
Methods. Age- and gender-standardized incident (beginning in each year) and prevalent (ongoing) opioid use episodes were estimated with automated health care data from 1997 to 2005. Profiles of opioid use in 2005 by age and gender were also compared.
Results. From 1997 to 2005, age–gender groups exhibited a total percentage increase ranging from 16% to 87% for incident long-term opioid use and from 61% to 135% for prevalent long-term opioid use. Women had higher opioid use than did men. Older women had the highest prevalence of long-term opioid use (8%–9% in 2005). Concurrent use of sedative-hypnotic drugs and opioids was common, particularly among women.
Conclusions. Risks and benefits of long-term opioid use are poorly understood, particularly among older adults. Increased surveillance of the safety of long-term opioid use is needed in community practice settings.
Long-term use of opioid analgesics for chronic noncancer pain has increased considerably in recent years,1–5 but little is known about trends in long-term use of prescribed opioids among specific age and gender groups. The American Geriatric Society recently recommended that opioids be preferred over nonsteroidal anti-inflammatory drugs (NSAIDs) for management of moderate-to-severe chronic pain among older adults,6 so it is timely to examine recent trends in opioid use among this population. Potential adverse effects of opioid use include overdose, falls and fractures, respiratory insufficiency, hyperalgesia, interactions with other medications or substances, risk of addiction, and diversion for nonmedical use. These risks differ by age and gender. For example, risks for abuse of prescribed opioid medications may be greatest among young men,7 whereas risks for fractures due to falls associated with opioid use may be greatest among older women.8 To minimize such risks, an important initial step is to understand the prevalence and long-term trends in opioid use in the general population by age and gender.
Women are more likely than are men to report a wide range of chronic pain conditions,9 including most musculoskeletal and arthritic pain conditions, common forms of headache, temporomandibular disorders, carpal tunnel syndrome, irritable bowel syndrome, and fibromyalgia.10 Women report greater severity of pain, longer-lasting and more frequent pain, and more anatomically diffuse pain than do men, and women are more likely to experience multiple pain problems.10,11 It is therefore not surprising that women use prescribed opioids at higher rates than do men.12,13 However, prior research has not determined the extent of long-term prescription opioid use among women relative to men.
Pain prevalence may change across the life course; some pain conditions increase with age (e.g., joint pain) and some decrease (e.g., abdominal pain and headache).11,14 Older persons have more chronic pain15,16 and thus may be more likely to be prescribed opioids for long periods.12,17 Findings on age differences in prescription opioid use have been contradictory12,18,19 Because older adults generally use more prescribed medications than do younger adults, older adults’ potential for medication interactions with opioid analgesics is greater.17,20 Older adults have higher prevalence of insomnia,21 so concomitant use of pain medications and sedative hypnotics may be common. Other concerns include cognitive impairment, respiratory depression, and ataxia (lack of muscle coordination), which increases risks of falls.20 Undertreatment of pain in older persons may be a consequence,17,22 although some guidelines recommend opioid analgesics for chronic pain among older adults in preference to NSAIDs.6
We describe trends over a 9-year period (1997–2005) in long-term use of prescribed opioid analgesics by age and gender in 2 large integrated health plans that together serve more than 1% of the US population. On the basis of prior research, we expected large increases in long-term opioid use over the study period, with higher prevalence for women than men and higher prevalence for older persons than younger adults.12 We also provide new information on age–gender differences in patterns of long-term opioid use, including type of medication, dosage levels, and concomitant use of sedative-hypnotic medications.
METHODS
The CONSORT study (Consortium to Study Opioid Risks and Trends) was developed to investigate trends and risks of long-term opioid therapy for noncancer pain from 1997 to 2005. Details of the methods have been published previously23; we briefly describe the study population and methods.
Study Setting and Population
The CONSORT study was conducted in 2 large, integrated health plans—Kaiser Permanente Northern California (KPNC) and Group Health Cooperative (GHC) in Washington State. Together, they provide care to approximately 4 000 000 individuals. Each health plan's membership generally reflects the demographic profile of the communities in which it is located, and enrollment has remained stable over time.24,25 KPNC's membership has a wide range of income and education levels. Compared with the region's general population, KPNC has fewer members at the extreme ends of the income distribution,24,26 members with more years of education,26 and a similar racial/ethnic distribution, except for a lower percentage of Latino women.24,26 GHC's membership includes about 10% of Washington State residents. GHC members’ age, gender, and racial/ethnic compositions are similar to those of the region's general population,25 but with fewer members at the extreme ends of the income distribution. GHC members have comparatively high levels of education and GHC membership is predominately White, with Asians comprising the largest minority population. Both health plans serve Medicaid and Medicare enrollees, the self-insured, and those insured through their employers. Analyses included data from all adult members aged 18 years or older, excluding persons who had been diagnosed with cancer. A diagnosis of cancer was determined from the Surveillance, Epidemiology and End Results (SEER) registries at both GHC and KPNC.
Data Sources
The CONSORT study uses automated health plan data, which include information on pharmacy use, patient demographics (age and gender), enrollment, clinical diagnoses, and health services utilization. Information on medical encounters and pharmacy utilization is captured for all services provided directly by the health plans and through claims data for any services provided outside of the health plan by contracted providers and pharmacies. Pharmacy data capture about 97% of membership prescriptions.24,25
Episodes of Opioid Use
CONSORT uses an episode approach to define long-term opioid use. The beginning of an episode is defined by the date of dispensing of an opioid (oral or transdermal) without a previous dispensing in the prior 6 months. An episode has no maximum length—the episode ends if there is no dispensing for 6 months. The end date is defined as the date of last prescription plus days supply (i.e., the number of days for which the opioid is prescribed) for that prescription. “Total days supply” is defined as the sum of days supply for all opioids dispensed during an episode.27 Days supply is calculated by the pharmacist when a prescription is dispensed and is based on the maximum dose permitted by the prescriber. “Incident” opioid use episodes are those episodes beginning in the calendar year of interest. The prevalence of opioid use episodes reflects period prevalence for a year—that is, episodes that continue in the year of interest.
We defined episodes as long-term if they were longer than 90 days and were associated either with a total days supply of at least 120 or with 10 or more opioid prescriptions of any type dispensed. Our previous work found that persons who surpassed this threshold were likely to continue frequent opioid use 1 year later.23
We also determined the type of pain condition associated with each episode. The first opioid prescription in the episode was linked to an “index visit”—that is, a visit with the physician who prescribed the first opioid in the episode during the 2 weeks prior to the episode start date.26 International Classification of Diseases, Ninth Revision (ICD-9) codes28 for the index visit were then evaluated to identify associated pain conditions. Persons could be classified with more than 1 condition.
Medication Use Profiles
Medication use profiles were developed for prevalent long-term opioid users in 2005 to compare subpopulations. Prevalent users were persons in an episode of long-term opioid use on January 1, 2005, who also met the criteria for long-term use in 2005 (i.e., 90 or more days with 120 or more total days supply or 10 or more opioid dispensations); thus, the profile covers the calendar year 2005. Profiles are presented here for the most recent study year (2005) since profiles were similar across study years for long-term opioid users.
We calculated morphine equivalent dose (MED) for each opioid dispensed by multiplying the quantity times the strength (i.e., milligrams per unit dispensed) times drug-specific conversion factors.23 We calculated total MED by adding the morphine equivalents for each opioid dispensed during the episode. Average daily dose for an episode, which we calculated by using the total MED divided by episode duration in days, is an estimate of mean daily consumption.23,27 Frequent use of sedative-hypnotic drugs was defined as receiving a supply of benzodiazepines, barbiturates, or muscle relaxants of 180 days or more in 2005.27
Opioid medications were divided into 3 types (based on established federal classifications and pharmaceutical designation): (1) non–Schedule II, (2) short-acting Schedule II, and (3) long-acting Schedule II.23 If more than 1 type of opioid was dispensed over an episode, the opioid with the largest total days supply in the episode was identified as the most frequently prescribed or predominant opioid in that episode.
Analyses
The study's focus was on long-term trends by age and gender, not on comparison of the health plans; thus, study analyses were done separately by health plan. We first described the characteristics of members initiating long-term opioid therapy in 2005 at KPNC and GHC. We then presented opioid use episodes per 1000 individuals, separately by health plan. Findings are presented by gender and by 3 age categories (18–44 years, 45–64 years, and ≥ 65 years) standardized to the 2005 age–gender distribution of each population. Incident long-term opioid use and prevalent long-term use are reported. We estimated the percent change annualized (PCA) across the study period with 95% confidence intervals (CIs) by using a linear regression method.29 The linearized PCA estimates the constant annual (multiplicative) rate of change over a fixed time period. To allow adequate follow-up time to observe long-term use after an episode began, only members who were enrolled for the entire year of interest plus 182 days following the end of the year were used.
The medication use profiles for each health plan for the year 2005 also present information by gender and by age group.
RESULTS
Table 1 reports descriptive information (age and pain condition) for incident long-term opioid use in 2005 by gender. The average ages for women and men were 57 years and 54 years at KPNC and 55 years and 53 years at GHC, respectively.
TABLE 1.
Characteristics and Most Prevalent Pain Conditions of Adult Members Initiating Long-Term Opioid Therapy: Kaiser Permanente Northern California and Group Health Cooperative, California and Washington State, 2005
| Kaiser Permanente Northern California |
Group Health Cooperative |
|||
| Women (n = 9501) | Men (n = 6275) | Women (n = 1007) | Men (n = 658) | |
| Mean age, y, (SD) | 56.5 (16.7) | 54.0 (15.2) | 55.0 (17.2) | 52.7 (14.7) |
| Index visit 2 wk before episode,a % | 63.0 | 66.4 | 74.8 | 76.2 |
| Type of pain diagnosed at index visit, % | ||||
| Back | 25.5 | 29.6 | 26.9 | 35.0 |
| Extremity | 20.9 | 21.7 | 21.9 | 24.5 |
| Osteoarthritis | 11.7 | 8.5 | 12.2 | 9.4 |
| Neck | 5.7 | 4.9 | 4.9 | 6.1 |
| Headache | 5.5 | 2.6 | 4.7 | 3.0 |
| Fracture | 5.0 | 4.7 | 6.7 | 5.5 |
| Abdominal | 4.2 | 2.9 | 4.9 | 3.2 |
| Neuropathy | 2.6 | 2.9 | 1.2 | 1.7 |
| Rheumatoid | 1.7 | 0.5 | 1.6 | 0.8 |
| Chest | 1.4 | 1.6 | 1.0 | 0.9 |
| Menstrual | 1.3 | NA | 3.2 | NA |
| Kidney | 0.6 | 0.7 | 0.5 | 0.8 |
| TMD | 0.4 | 0.1 | 0.1 | 0.2 |
Note. TMD = temporomandibular disorders; NA = not applicable. Long-term use was defined as episodes with a duration of 90 or more days and 10 or more prescriptions received or total days supply of at least 120.
”Index visit” was defined as visit with prescribing physician in 2 weeks prior to episode start date. The denominator for calculating percentages included only those persons for whom an index visit was identified. Episode start date was defined as an initial dispensing for oral or transdermal opioid with no dispensing of opioids in the prior 6 months.
Among KPNC incident long-term opioid users in 2005, 63% of women and 66.4% of men had a visit to the prescribing physician within 2 weeks prior to initiating opioids, permitting linkage to diagnostic data for that index visit. At GHC, the respective numbers were 74.8% for women and 76.2% for men. At KPNC and GHC, the most prevalent pain conditions for both women and men were back pain, extremity pain, and osteoarthritis.
Across age groups, the most common diagnoses were back pain and extremity pain (results not shown). Osteoarthritis pain was more prevalent among those aged 65 years and older than among the younger age groups.
Incidence of Long-Term Opioid Use
Table 2 shows incident long-term opioid use for 1997 and 2005. (Findings for intervening years were highly stable, showing an increasing pattern, and are not shown here. Data are available upon request). Older women (aged 65 years and older) at KPNC and GHC had higher incident long-term opioid use than did any of the other age–gender groups. Overall, the trend toward higher incident long-term opioid use over time was found in all age groups and both genders. Across all age and gender groups, the PCA in the incidence of long-term opioid use was about 4% to 8%. From 1997 to 2005, the overall percentage increase in the onset of new episodes of long-term opioid use ranged from 16% to 87%, depending on the age–gender group.
TABLE 2.
Incidence of Long-Term Opioid Use for Noncancer Pain Among Adult Members of Kaiser Permanente Northern California and Group Health Cooperative, California and Washington State, 1997 and 2005
| Women |
Men |
|||||||||
| 1997 |
2005 |
1997 |
2005 |
|||||||
| Age, y | No. | Incidence (95% CI) | No. | Incidence (95% CI) | PCAa (95% CI) | No. | Incidence (95% CI) | No. | Incidence (95% CI) | PCAa (95% CI) |
| Kaiser Permanente Northern California | ||||||||||
| 18–44 | 389 652 | 4.6 (4.4, 4.8) | 423 102 | 5.8 (5.6, 6.1) | 4.5 (4.0, 5.1) | 355 267 | 3.0 (2.8, 3.2) | 396 010 | 4.5 (4.3, 4.7) | 5.9 (5.3, 6.6) |
| 45–64 | 284 231 | 7.6 (7.3, 7.9) | 369 502 | 10.8 (10.5, 11.2) | 6.5 (6.1, 7.0) | 264 197 | 5.8 (5.5, 6.1) | 341 830 | 8.8 (8.5, 9.1) | 6.4 (5.9, 7.0) |
| ≥ 65 | 125 934 | 14.7 (14.0, 15.4) | 170 293 | 17.9 (17.2, 18.5) | 4.3 (3.8, 4.8) | 100 306 | 9.0 (8.4, 9.7) | 126 947 | 11.9 (11.3, 12.5) | 4.7 (4.0, 5.4) |
| Group Health Cooperative | ||||||||||
| 18–44 | 70 582 | 7.5 (6.9, 8.2) | 49 901 | 10.5 (9.6, 11.4) | 6.3 (5.2, 7.4) | 54 693 | 3.8 (3.3, 4.3) | 40 144 | 7.1 (6.3, 8.0) | 8.4 (6.7, 10.0) |
| 45–64 | 49 721 | 9.2 (8.4, 10.2) | 58 879 | 13.1 (12.2, 14.1) | 6.2 (5.1, 7.2) | 47 188 | 6.9 (6.2, 7.8) | 51 523 | 11.7 (10.8, 12.7) | 7.7 (6.4, 9.0) |
| ≥ 65 | 26 143 | 17.1 (15.5, 18.9) | 27 793 | 19.9 (18.2, 21.6) | 3.3 (2.2, 4.4) | 18 875 | 10.3 (8.8, 11.9) | 20 149 | 12.9 (11.4, 14.6) | 4.3 (2.6, 6.0) |
Note. CI = confidence interval; PCA = percent change annualized.
The linearized PCA estimates the constant annual (multiplicative) rate of change over the study period.
Prevalence of Long-Term Opioid Use
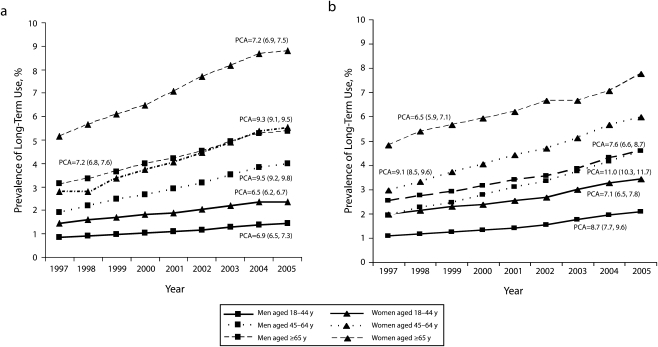
Figure 1 describes trends in prevalent long-term opioid use for KPNC and GHC members. For women, there were large increases in prevalent long-term use among all age groups. The greatest increase was for women aged 45–64 years at both KPNC (PCA = 9.3; 95% CI = 9.1, 9.5) and GHC (PCA = 9.1; 95% CI = 8.5, 9.6). The highest long-term use was among older women, which was consistent across the study period. At KPNC, older women had prevalence of long-term opioid use of 51.6 per 1000 population (i.e., 5.2%) in 1997 and 88.0 per 1000 population (8.9%) in 2005. At GHC, the corresponding prevalence of long-term opioid use was 48.2 per 1000 population in 1997 and 77.5 per 1000 population in 2005. Thus, at the end of the study period, 8% to 9% of women older than 65 years were on long-term opioid use in both health plans. Over the 9-year study period, the total percentage increase in the prevalence of long-term opioid use among women at KPNC ranged from 62% among those aged 19 to 44 years to 98% among those aged 45–64 years. At GHC, the total percentage increase in the prevalence of long-term opioid use for women ranged from 61% among those aged 65 or older to 102% among those aged 45–64 years.
FIGURE 1.
Prevalence of long-term opioid use for noncancer pain among adult members of (a) Kaiser Permanente Northern California and (b) Group Health Cooperative, by gender and year: 1997–2005.
Note. PCA = percent change annualized.
There were similar increases in prevalent long-term opioid use for men. For men, as for women, the greatest increase occurred among those aged 45–64 years (at KPNC, PCA = 9.5; 95% CI = 9.2, 9.8; at GHC, PCA = 11.0; CI = 10.3, 11.7). However, in the later study years at GHC, there was little difference between the middle age group and the older men. Opioid use was highest for older men—at KPNC, 31.5 per 1000 population in 1997 and 53.8 per 1000 population in 2005; at GHC, 25.3 per 1000 population in 1997 and 45.7 per 1000 population in 2005. Over the study period, the total percentage of increase in the prevalence of long-term opioid use among men at KPNC ranged from 71% (among those aged 18–44 years and those 65 years or older) to 106% (among those aged 45–64 years). At GHC, the total percentage increase in the prevalence of long-term opioid use among men ranged from 81% (among those aged 65 years or older) to 135% (among those aged 45–64 years).
Medication Use Profiles 2005
Table 3 shows medication use profiles for prevalent long-term opioid users in 2005 for both health plans. At KPNC, women had only a slightly lower average daily dose than did men (46.0 mg MED vs 51.5 mg MED; P < .001). However, significantly more women than men with long-term opioid use received a supply of sedative-hypnotic drugs of 180 days or more (33% vs 25%; P < .001). At KPNC, gender differences in both the percentage prescribed of mainly Schedule II medications and in the percentage prescribed mainly of long-acting Schedule II medications were small but statistically significant because of the large sample size. The pattern of findings at GHC was similar.
TABLE 3.
Medication Use Profiles for Prevalent Long-Term Opioid Use Among Adult Members of Kaiser Permanente Northern California and Group Health Cooperative, 2005
| Average Daily Dose,a Mean (SD) | Mainly Schedule IIb Opioids, % | Mainly Long-Acting Schedule II Opioids, % | ≥ 180 Days Supply of Sedative-Hypnotic Drugs, % | |
| Kaiser Permanente Northern California | ||||
| Gender | ||||
| Women (n = 24 189) | 46.0 (104.1) | 17.3 | 12.7 | 33.1 |
| Men (n = 13 392) | 51.5 (129.1) | 18.4 | 13.7 | 24.9 |
| Age, y | ||||
| 18–44 (n = 7686) | 58.0 (141.9) | 17.8 | 13.3 | 30.6 |
| 45–64 (n = 18 595) | 52.5 (125.6) | 18.9 | 14.3 | 32.9 |
| ≥ 65 (n = 11 300) | 33.6 (50.8) | 15.7 | 10.9 | 25.6 |
| Group Health Cooperative | ||||
| Gender | ||||
| Women (n = 4056) | 41.3 (79.3) | 42.3 | 22.0 | 31.7 |
| Men (n = 2159) | 52.7 (109.9) | 51.6 | 26.9 | 22.6 |
| Age, y | ||||
| 18–44 (n = 1205) | 49.2 (92.2) | 46.9 | 21.7 | 27.9 |
| 45–64 (n = 3277) | 50.0 (104.2) | 45.7 | 24.3 | 31.6 |
| ≥ 65 (n = 1734) | 33.9 (59.5) | 44.1 | 24.1 | 23.4 |
Note. Prevalent long-term opioid use is defined as opioid use for at least 90 days with a 120 or more total days supply or 10 or more opioid prescription dispensations in an episode.
Average daily dose is the total morphine equivalents of all filled prescriptions divided by episode duration in days.
Schedule II = morphine sulfate, codeine sulfate, hydromorphone, meperidine, fentanyl transmucosal, oxymorphone, oxycodone, morphine sulfate SR, fentanyl transdermal, levorphanol, oxycodone CR, methadone, hydromorphone SR, and oxymorphone SR.
At KPNC, the oldest age group (65 years or older) was less likely to use mainly Schedule II opioids, was less likely to use mainly long-acting opioids, used a lower average daily dose, and was less likely to receive a supply of sedative-hypnotic drugs of 180 days or more (all significant at P < .001).
At GHC, the oldest age group also received a lower average daily dose (P < .001) and was less likely to receive a supply of sedative-hypnotic drugs of 180 days or more (P < .001); however, the youngest age group (aged 18–44 years) was least likely to use mainly long-acting opioids (P < .001).
DISCUSSION
Over the 9-year study period, older women by far had the greatest exposure to long-term opioid therapy. By 2005, the prevalence of long-term opioid use was 8% to 9% among older women in both health plans. Long-term opioid use was substantially higher among older women than it was among younger women or men in any age group.
The risks and benefits of long-term opioid use among older women are not well understood.30 Older women have lower risk for opioid misuse3,31 but may be more vulnerable to adverse medical effects of opioid use such as sedation, falls, constipation, respiratory depression, accidental overdose, and medication interactions.20,30 They also have higher prevalence of concurrent use of other psychoactive medications30 and increased prevalence of comorbid chronic physical disease and frailty.18,20,30 The risks of opioid therapy for older women are likely very different from those of younger men. A recent report on unintentional overdose deaths in West Virginia reported that over two thirds of such deaths involved young males, of whom fewer than half had ever been prescribed the overdose drugs. The likelihood of diversion (use without a documented prescription) decreased with age of the decedents. Among those who overdosed, obtaining prescriptions from multiple providers was more common for women than for men.32
The recent increase of long-term opioid use appears to reflect a considerable change in the prescribing of opioid analgesics for chronic pain among community physicians. In the absence of well-controlled studies evaluating the safety and effectiveness of long-term opioid use, it is not possible to say whether the benefits of increased opioid prescribing outweigh the risks. However, our results indicate that large numbers of adults of all ages are now using opioids over extended periods of time, suggesting that even low rates of serious adverse events could have large effects on morbidity and mortality on a population basis. Given the large population exposure to long-term opioid use, increased surveillance of the health risks associated with extended use of these medications is needed.
We know little about how patients and their physicians make decisions regarding continuation of opioid use. The increases observed over time may be due to a variety of factors, including successful use of opioids in postoperative and hospice care,33 policies and guidelines aiming to reduce the risk faced by physicians when prescribing opioids,33,34 aggressive pharmaceutical company marketing,35 and greater availability of opioid medications. Although the data reported here cannot tell us why, it was clear that increased use of opioids occurred among persons of all ages and both genders.
The similarities across the 2 health plans in age and gender differences, and in trends of use over time, are striking. Although women in the oldest age group demonstrated the highest use, women in all 3 age groups had higher initiation as well as sustained long-term opioid use compared with men. These gender differences were observed in both health plans over all 9 years of this study. Although higher in women, increased long-term opioid use was also observed over time among males of all ages.
Although women typically report more pain conditions and greater pain severity than do men, this did not translate to use of more long-acting Schedule II medications. However, a higher percentage of women than men used sedative hypnotics concurrently with opioid medications, raising a concern about potential interactions and risks. These data cannot address the appropriateness of treatment but highlight the need for research that assesses how patients with long-term opioid use are being managed in community practice, including research on drug safety, pain, and functional outcomes.
The observed differences in opioid use between men and women could be caused by several factors, including differences in prevalence and type of pain and variables that influence the experience and severity of the pain.14 These variables include physiological factors such as hormone levels, psychosocial factors such as depression (more prevalent among women than men), different perceptual styles and coping strategies, and cultural factors, such as gender differences in norms for reporting pain.14,36,37 It is also plausible that physicians respond differently to pain problems among women and men, and hold beliefs concerning the appropriateness of prescribing opioids for different demographic subgroups. These factors have received little attention in the pain literature.38,39
Our finding of higher prevalence of long-term opioid use in older age groups, for both men and women, is consistent with most other research. For example, a telephone survey of a national sample of adults found that those aged 70 years and older were more likely to be regular opioid users.12 In one study, however, which used national data from outpatient hospital and community settings, those aged 75 years and older were more likely than were others to use NSAIDs and less likely to use opioids.19 Some clinicians may be hesitant to prescribe opioids to older patients because of their side effects and potential risks, and several studies have concluded that older patients remain at risk for undertreatment of pain.15,40 Recent guidelines from the American Geriatric Association recommend opioids over NSAIDs, which may result in a further increase in the rate at which older adults are prescribed opioid medications.6 Given the large percentage of older adults now prescribed opioids for long-term use, there is a need for large, controlled studies to assess its safety and effectiveness.
This study has several limitations. It relied on automated health care data. Information from patients on pain severity and function was not available. This study did not address the benefits or risks of opioid prescribing or use. KPNC and GHC pharmacy data are considered accurate and complete, but we do not have information on actual opioid consumption.24,25 KPNC and GHC are integrated health plans, and findings may not generalize to other types of health plans. Nevertheless, these plans cover more than 1% of the US population and results are consistent with those from general population surveys.
Our findings showed that long-term use of opioids doubled over the study period, from 1997 to 2005. The highest prevalence of long-term opioid use was among women and older persons, with 8% to 9% of older women maintaining long-term opioid use in 2005. Among persons with long-term opioid use, dosage levels were typically in the low to moderate range, predominate use of short-acting opioids was most common, and a significant minority was prescribed both opioid and sedative-hypnotic medications. Given the large and rapidly increasing level of long-term opioid use among the population at large, particularly among older persons, improved information on the safety and effectiveness of these medications is needed.
Acknowledgments
Support for this study came from the National Institute of Drug Abuse (grant R01 DA022557). M. J. Silverberg's effort was supported in part by the National Institute of Allergy and Infectious Diseases (grant number K01AI071725).
Human Participant Protection
The study was approved by the institutional review board at Kaiser Permanente Northern California and at the Group Health Research Institute.
References
- 1.Gilson AM, Ryan KM, Joranson DE, et al. A reassessment of trends in the medical use and abuse of opioid analgesics and implications for diversion control: 1997–2002. J Pain Symptom Manage. 2004;28(2):176–188 [DOI] [PubMed] [Google Scholar]
- 2.Novak S, Nemeth WC, Lawson KA. Trends in medical use and abuse of sustained-release opioid analgesics: a revisit. Pain Med. 2004;5(1):59–65 [DOI] [PubMed] [Google Scholar]
- 3.Denisco RA, Chandler RK, Compton WM. Addressing the intersecting problems of opioid misuse and chronic pain treatment. Exp Clin Psychopharmacol. 2008;16(5):417–428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Caudill-Slosberg MA, Schwartz LM, Woloshin S. Office visits and analgesic prescriptions for musculoskeletal pain in US: 1980 vs 2000. Pain. 2004;109(3):514–519 [DOI] [PubMed] [Google Scholar]
- 5.Sullivan MD, Edlund MJ, Fan MY, et al. Trends in use of opioids for non-cancer pain conditions 2000–2005 in commercial and Medicaid insurance plans: the TROUP study. Pain. 2008;138(2):440–449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.The American Geriatrics Society (AGS), Foundation for Health in Aging AGS clinical practice guideline: pharmacological management of persistent pain in older persons. 2008. Available at: http://www.americangeriatrics.org/health_care_professionals/clinical_practice/clinical_guidelines_recommendations/2009. Accessed May 7, 2009
- 7.Banta-Green CJ, Merrill JO, Doyle SR, et al. Measurement of opioid problems among chronic pain patients in a general medical population. Drug Alcohol Depend. 2009;104(1–2):43–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saunders KW, Dunn KM, Merrill JO, et al. Relationship of opioid use and dosage levels to fractures in older chronic pain patients. J Gen Intern Med. 2010;25(4):310–315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Unruh AM. Gender variations in clinical pain experience. Pain. 1996;65(2–3):123–167 [DOI] [PubMed] [Google Scholar]
- 10.Hurley RW, Adams MC. Sex, gender, and pain: an overview of a complex field. Anesth Analg. 2008;107(1):309–317 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.LeResche L. Epidemiologic perspectives on sex differences in pain. : Fillingim RG, Sex, Gender, and Pain. Seattle, WA: IASP Press; 2000:233–249 [Google Scholar]
- 12.Parsells Kelly J, Cook SF, Kaufman DW, et al. Prevalence and characteristics of opioid use in the US adult population. Pain. 2008;138(3):507–513 [DOI] [PubMed] [Google Scholar]
- 13.Simoni-Wastila L. The use of abusable prescription drugs: the role of gender. J Womens Health Gend Based Med. 2000;9(3):289–297 [DOI] [PubMed] [Google Scholar]
- 14.LeResche L. Sex, gender, and clinical pain. : Flor H, Kalso E, Dostrovsky JO, Proceedings of the 11th World Congress on Pain. Sydney, Australia: IASP Press; 2006:543–554 [Google Scholar]
- 15.Sawyer P, Bodner EV, Ritchie CS, et al. Pain and pain medication use in community-dwelling older adults. Am J Geriatr Pharmacother. 2006;4(4):316–324 [DOI] [PubMed] [Google Scholar]
- 16.Helme RD, Gibson SJ. The epidemiology of pain in elderly people. Clin Geriatr Med. 2001;17(3):417–431 [DOI] [PubMed] [Google Scholar]
- 17.Herr K. Chronic pain in the older patient: management strategies. J Gerontol Nurs. 2002;28(2):28–34; quiz, 54–25 [DOI] [PubMed] [Google Scholar]
- 18.Hudson TJ, Edlund MJ, Steffick DE, et al. Epidemiology of regular prescribed opioid use: results from a national, population-based survey. J Pain Symptom Manage. 2008;36(3):280–288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Federman AD, Litke A, Morrison RS. Association of age with analgesic use for back and joint disorders in outpatient settings. Am J Geriatr Pharmacother. 2006;4(4):306–315 [DOI] [PubMed] [Google Scholar]
- 20.Fine PG. Pharmacological management of persistent pain in older patients. Clin J Pain. 2004;20(4):220–226 [DOI] [PubMed] [Google Scholar]
- 21.Morin CM, Colecchi C, Stone J, et al. Behavioral and pharmacological therapies for late-life insomnia: a randomized controlled trial. JAMA. 1999;281(11):991–999 [DOI] [PubMed] [Google Scholar]
- 22.Schneider JP. Chronic pain management in older adults: with coxibs under fire, what now? Geriatrics. 2005;60(5):26–28, 30–21 [PubMed] [Google Scholar]
- 23.Von Korff M, Saunders K, Thomas Ray G, et al. De facto long-term opioid therapy for noncancer pain. Clin J Pain. 2008;24(6):521–527 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Selby JV, Smith DH, Johnson ES, et al. Kaiser Permanente Medical Care Program. : Strom BL, Pharmacoepidemiology. 4th ed New York, NY: Wiley; 2005:241–259 [Google Scholar]
- 25.Saunders KW, Davis RL, Stergachis A. Group Health Cooperative. : Strom BL, Pharmacoepidemiology. 4th ed New York, NY: Wiley; 2005:223–239 [Google Scholar]
- 26.Gordon NP.How does the adult Kaiser Permanente membership in northern California compare with the larger community? 2006. Available at: http://www-dor.kaiser.org/dor/mhsnet/public/pdf_supplemental_public/comparison_kaiser_vs_nonKaiser_adults_kpnc.pdf. Accessed Dec 14, 2009.
- 27.Boudreau D, Von Korff M, Rutter CM, et al. Trends in long-term opioid therapy for chronic non-cancer pain. Pharmacoepidemiol Drug Saf. 2009;18(12):1166–1175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.International Classification of Diseases, Ninth Revision. Geneva, Switzerland: World Health Organization; 1980 [Google Scholar]
- 29.Fay MP, Tiwari RC, Feuer EJ, et al. Estimating average annual percent change for disease rates without assuming constant change. Biometrics. 2006;62(3):847–854 [DOI] [PubMed] [Google Scholar]
- 30.Simoni-Wastila L, Yang HK. Psychoactive drug abuse in older adults. Am J Geriatr Pharmacother. 2006;4(4):380–394 [DOI] [PubMed] [Google Scholar]
- 31.Tetrault JM, Desai RA, Becker WC, Fiellin DA, Concato J, Sullivan LE. Gender and non-medical use of prescription opioids: results from a national US survey. Addiction. 2008;103(2):258–268 [DOI] [PubMed] [Google Scholar]
- 32.Hall AJ, Logan JE, Toblin RL, et al. Patterns of abuse among unintentional pharmaceutical overdose fatalities. JAMA. 2008;300(22):2613–2620 [DOI] [PubMed] [Google Scholar]
- 33.Cancer Pain Relief. With a Guide to Opioid Availability. 2nd ed Geneva, Switzerland: World Health Organization; 1996 [Google Scholar]
- 34.The Federation of State Medical Boards of the United States Inc Model guidelines for the use of controlled substances for the treatment of pain. Adopted May 2, 1998. Available at: http://www.medsch.wisc.edu/painpolicy/domestic/model.htm. Accessed November 23, 2009 [PubMed]
- 35.Government Accounting Office OxyContin abuse and diversion and efforts to address the problem: highlights of a government report. J Pain Palliat Care Pharmacother. 2004;18(3):109–113 [PubMed] [Google Scholar]
- 36.Greenspan JD, Craft RM, LeResche L, et al. Studying sex and gender differences in pain and analgesia: a consensus report. Pain. 2007;132(suppl 1):S26–S45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Munce SE, Stewart DE. Gender differences in depression and chronic pain conditions in a national epidemiologic survey. Psychosomatics. 2007;48(5):394–399 [DOI] [PubMed] [Google Scholar]
- 38.Weisse CS, Sorum PC, Sanders KN, et al. Do gender and race affect decisions about pain management? J Gen Intern Med. 2001;16(4):211–217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Safdar B, Heins A, Homel P, et al. Impact of physician and patient gender on pain management in the emergency department—a multicenter study. Pain Med. 2009;10(2):364–372 [DOI] [PubMed] [Google Scholar]
- 40.Fishman SM, Papazian JS, Gonzalez S, et al. Regulating opioid prescribing through prescription monitoring programs: balancing drug diversion and treatment of pain. Pain Med. 2004;5(3):309–324 [DOI] [PubMed] [Google Scholar]