In contrast to organic diseases, functional disorders are increasing and considered important in recent days. However, because of the heterogenecity in pathogenesis of functional dyspepsia and drawbacks of each study, functional study was limited in clinical practice. Reduced gastric accommodation is a major pathophysiologic mechanism in functional dyspepsia presented more commonly than the abnormal gastric emptying.1 Associated symptoms with impaired accommodation are early satiety, fullness, postprandial discomfort and weight loss. Compared to other pathophysiologic factors, a variety of methods have been developed to assess gastric accommodation, including barostat, single photon emission computed tomography (SPECT), MRI, ultrasonography and water drinking test. Barostat balloon test is a gold standard for its measurement but has severe disadvantages in its invasiveness and non-physiologic character. A balloon in fundus of stomach may alter the intragastric distribution of meal and exaggerate antral relaxation.2 Alternative to barostat would be SPECT or MRI because these studies are non-invasive and well validated.3,4
SPECT was first proposed and validated for quantification of gastric accommodation by the Mayo group.5 This application was based on the fact that the oxyntic parietal cells and non-parietal mucous cells excrete technetium 99m-pertechnetate from the circulating blood pool and gastric scintiscanning correlated well with gastric luminal 99m technetium activity.6 As described in the paper by Gonlachanvit et al in this issue of the journal, transaxial tomographic images are acquired using a gamma camera system after intravenous administration of the pertechnetate radiomarker. Three-dimensional reconstruction of data enables to measure the changes of gastric volume during fasting and post-prandial periods using commercially available software. In addition, this method also permits simultaneous assessment of gastric emptying and accommodation. Gastric accommodation was maximal soon after meal ingestion and persisted for several hours despite the nearly complete emptying of liquid or solid meal.7 Magnitude of the volume response is greater after liquid meal compared with isocaloric mixed meal.8
Gastric volumes measured with SPECT were compared to data with barostat. SPECT is considered to be less suitable than barostat in detecting changes in gastric tone.9 However, mean volumes of post-prandial to fasting volumes measured by SPECT were comparable to that of barostat.10 SPECT can distinguish normal person from dyspepsia patient with impaired gastric accommodation.1 Reduced gastric accommodation was observed in two-fifths of dyspeptic patients as the same proportion measured by using barostat.11 Effects of age or body mass index on SPECT imaging of the stomach were not noticed but in females, postprandial gastric volumes and changes were lower than in males.10 The paper by Gonlachanvit et al in this issue suggested racial difference in fasting gastric volumes and provided a reference for Asian people. Gastric mucosal secretion of technetium-99m-pertechnetate is reduced with the use of histamine H2 receptor antagonists and stomach wall imaging would be improved due to the increased uptake.12 Gastric accommodation response may be affected by some agents. Erythromycin reduces accommodation response13 but nitric oxide donors, α2-adrenergic agonists and 5-HT1 agonists enhance gastric relaxation.14,15 As the gastric volume changes, a region of interest based on fasting stomach may need to be modified for postprandial measurements. When the incisura is not pronounced, division of stomach compartments into proximal and distal regions may be arbitrary.
Reproducibility study of gastric barostat in healthy controls and in dyspeptic patients was reported.16 Repeated measurements were highly reproducible with excellent correlation in healthy subjects and dyspeptic patients (R = 0.71 and 0.74, respectively). The intraday and the day-to-day variabilities of gastric accommodation were quantified by calculating the individual coefficient of variation (CV = 100 × SD/mean, expressed in %). The mean change in gastric volume post-meal was 450 mL and the standard deviation of the change was 75 mL. The sample sizes required to show a 25% difference in volume are 9 per group for a parallel-group design (eg, disease vs control and drug vs placebo) and 6 for a crossover design study. SPECT imaging is a more sensitive method to detect differences in gastric volume change. SPECT imaging could detect an effect size of 10%, but 25% with barostat with a sample size of 45 per group in a parallel-group design and 24 per group in a crossover study.3
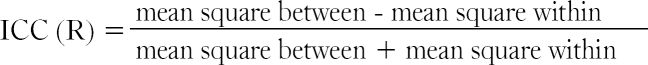
Gonlachanvit et al in this issue have conducted measurements of gastric accommodation by SPECT performed at the same time and different time of the day. Reproducibility was demonstrated by intraclass correlation coefficient (ICC) and coefficient of variation. ICC is a descriptive statistics that can be used to describe how strongly the measurements resemble each other and assessment of consistency or reproducibility of quantitative measurements made by different observers. Compared with Cohen's kappa for the category data, ICC is used for numeric measurements and same value with weighted kappa. ICC is a ratio of measurement error to total error. Total error is a summation of subject error and measurement error.
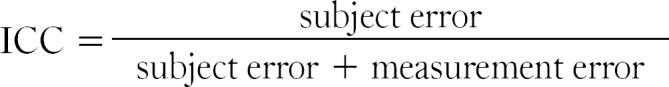
Therefore, the smaller the measurement error is, the closer the ICC approaches to 1. For example, if the measurement error is zero, the value of ICC becomes 1. Subject error means variance of measurements between subjects and measurement error means the variance within subject. Measurement error is same as mean squares within subject and could be calculated, whereas subject error cannot be calculated independently. Mean square between subjects equals total error and following equation could be made.
An ICC of below 0.4 indicates poor reproducibility, 0.4 to 0.75 indicates fair to good reproducibility and 0.75 or more indicates excellent reproducibility.
Footnotes
Financial support: None.
Conflicts of interest: None.
References
- 1.Kim DY, Delgado-Aros S, Camilleri M, et al. Noninvasive measurement of gastric accommodation in patients with idiopathic nonulcer dyspepsia. Am J Gastroenterol. 2001;96:3099–3105. doi: 10.1111/j.1572-0241.2001.05264.x. [DOI] [PubMed] [Google Scholar]
- 2.Mundt MW, Hausken T, Samsom M. Effect of intragastric barostat bag on proximal and distal gastric accommodation in response to liquid meal. Am J Physiol Gastrointest Liver Physiol. 2002;283:G681–G686. doi: 10.1152/ajpgi.00499.2001. [DOI] [PubMed] [Google Scholar]
- 3.De Schepper HU, Cremonini F, Chitkara D, Camilleri M. Assessment of gastric accommodation: overview and evaluation of current methods. Neurogastroenterol Motil. 2004;16:275–285. doi: 10.1111/j.1365-2982.2004.00497.x. [DOI] [PubMed] [Google Scholar]
- 4.Fruehauf H, Goetze O, Steingoetter A, et al. Intersubject and intrasubject variability of gastric volumes in response to isocaloric liquid meals in functional dyspepsia and health. Neurogastroenterol Motil. 2007;19:553–561. doi: 10.1111/j.1365-2982.2007.00904.x. [DOI] [PubMed] [Google Scholar]
- 5.Kuiken SD, Samsom M, Camilleri M, et al. Development of a test to measure gastric accommodation in humans. Am J Physiol. 1999;277:G1217–G1221. doi: 10.1152/ajpgi.1999.277.6.G1217. [DOI] [PubMed] [Google Scholar]
- 6.O'Connor MK, O'Connell R, Keane FB, Byrne PJ, Hennessy TP. The relationship between technetium 99m pertechnetate gastric scanning and gastric contents. Br J Radiol. 1983;56:817–822. doi: 10.1259/0007-1285-56-671-817. [DOI] [PubMed] [Google Scholar]
- 7.Simonian HP, Maurer AH, Knight LC, et al. Simultaneous assessment of gastric accommodation and emptying: studies with liquid and solid meals. J Nucl Med. 2004;45:1155–1160. [PubMed] [Google Scholar]
- 8.De Schepper H, Camilleri M, Cremonini F, Foxx-Orenstein A, Burton D. Comparison of gastric volumes in response to isocaloric liquid and mixed meals in humans. Neurogastroenterol Motil. 2004;16:567–573. doi: 10.1111/j.1365-2982.2004.00533.x. [DOI] [PubMed] [Google Scholar]
- 9.Van den Elzen BD, Bennink RJ, Wieringa RE, Tytgat GN, Boeckxstaens GE. Fundic accommodation assessed by SPECT scanning: comparison with the gastric barostat. Gut. 2003;52:1548–1554. doi: 10.1136/gut.52.11.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bouras EP, Delgado-Aros S, Camilleri M, et al. SPECT imaging of the stomach: comparison with barostat, and effects of sex, age, body mass index, and fundoplication. Gut. 2002;51:781–786. doi: 10.1136/gut.51.6.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tack J, Piessevaux H, Coulie B, Caenepeel P, Janssens J. Role of impaired gastric accommodation to a meal in functional dyspepsia. Gastroenterology. 1998;115:1346–1352. doi: 10.1016/s0016-5085(98)70012-5. [DOI] [PubMed] [Google Scholar]
- 12.Berardi C, Twardock AR, Wheaton LG, Schaeffer DJ. Nuclear imaging of the stomach of healthy dogs. Am J Vet Res. 1991;52:1081–1088. [PubMed] [Google Scholar]
- 13.Bruley des Varannes S, Parys V, Ropert A, Chayvialle JA, Rozé C, Galmiche JP. Erythromycin enhances fasting and postprandial proximal gastric tone in humans. Gastroenterology. 1995;109:32–39. doi: 10.1016/0016-5085(95)90266-x. [DOI] [PubMed] [Google Scholar]
- 14.Thumshirn M, Camilleri M, Choi MG, Zinsmeister AR. Modulation of gastric sensory and motor functions by nitrergic and alpha2-adrenergic agents in humans. Gastroenterology. 1999;116:573–585. doi: 10.1016/s0016-5085(99)70179-4. [DOI] [PubMed] [Google Scholar]
- 15.Coulie B, Tack J, Maes B, Geypens B, De Roo M, Janssens J. Sumatriptan, a selective 5-HT1 receptor agonist, induces a lag phase for gastric emptying of liquids in humans. Am J Physiol. 1997;272:G902–G908. doi: 10.1152/ajpgi.1997.272.4.G902. [DOI] [PubMed] [Google Scholar]
- 16.Sarnelli G, Vos R, Cuomo R, Janssens J, Tack J. Reproducibility of gastric barostat studies in healthy controls and in dyspeptic patients. Am J Gastroenterol. 2001;96:1047–1053. doi: 10.1111/j.1572-0241.2001.03520.x. [DOI] [PubMed] [Google Scholar]