Abstract
Background/Aims
Technetium-99m (99mTc)-pertechnetate single photon emission computed tomography (SPECT) allows non-invasive measurement of gastric accommodation (GA) and has been reported to provide the results comparable to the gold standard barostat. The reproducibility of the test when it is performed at different time of the day is not known. The aim of this study was to assess the reproducibility of GA measurement by 99mTc-pertechnetate SPECT at the same and different time of the day.
Methods
Three GA studies were performed in each of 20 healthy volunteers (9 males, age 35 ± 9 years), 2 studies in the morning and 1 study in the afternoon. Each study was performed on separate days at least 3 days apart, in random order. The fasting gastric scintigraphy images were acquired using SPECT at 30 minutes after iv 99mTc-pertechnetate. Then, the scintigraphic images were acquired 50 minutes after liquid meal (250 mL, Ensure®) ingestions. Gastric volumes were calculated from transaxial gastric images using Image J software. The GA was defined as the maximum postprandial gastric volume minus fasting gastric volume.
Results
GA measurement by SPECT show good reproducibility at both the same and different time of the day. The intraclass correlation coefficients of GA results for the same time, the first different time and the second different time studies were 0.681, 0.630 and 0.774, respectively, and the intra-subject coefficients of variation were 13.9%, 14.1% and 8.7%, respectively.
Conclusions
GA measurement by 99mTc-pertechnetate SPECT shows good reproducibility at both the same and different time of the day. This result suggests that the schedule time does not appear to extremely affect the gastric accommodation value.
Keywords: Reproducibility, Single photon emission computed tomography, Sodium pertechnetate Tc99m
Introduction
Impaired gastric accommodation (GA) in response to meal ingestion has been shown to be associated with functional dyspepsia.1 It has been reported that about 40 percents of functional dyspeptic patients have impaired GA and this impairment was associated with early satiety.2 The gold standard for GA measurement is gastric barostat.3 Due to an invasive nature of barostat, there have been attempts to develop alternative non-invasive measurement.3 99mTechnetium-99m (99mTc)-pertechnetate single photon emission computed tomography (SPECT) technique has been used as a non-invasive method for GA measurements.4-11 Several studies evaluated it's reliability and found no significant differences of the GA (postprandial-fasting gastric volume) and postprandial/fasting gastric volume ratios measured by this technique compared with the gold standard barostat.5-7 There has been only one study to date addressing the reproducibility of GA measurement by pertechnetate SPECT using commercially available analysis software.11 In clinical practice, GA study cannot be performed at the same time of the day in every patient. Previous studies suggested that fasting gastric volume was not affected by the fasting durations.12-14 However, it has not been known whether GA studies at different times of the day bring different results. Therefore, the aim of the present study was to assess the reliability of GA measurement in healthy volunteers at both the same and different time of the day by 99mTc-pertechnetate SPECT using freely available National Institutes of Health Image J software.15
Materials and Methods
1. Subjects
Twenty healthy volunteers (11 females, body mass index 23 ± 4 kg/m2, age 35 ± 9 years) were invited to participate with the studies via campus advertisement. Those who had any gastrointestinal symptoms, previous intra-abdominal surgery except for appendectomy or tubal ligation, an underlying medical condition, current medication(s) except contraceptive pill, smoking or alcohol drinking without ability to withdraw for 24 hours before the study, a positive serologic test for Helicobacter pylori antibody, pregnancy or lactation women were not allowed to participate in this study. All subjects provided written informed consent before entering the study. The study was approved by the ethics committee of the Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand.
Each volunteer underwent 3 99mTc-pertechnetate SPECT studies, 2 studies in the morning at 8:00 am after an overnight fasting for same time reproducibility study and the other study in the afternoon at 1:00 pm with at least 6 hours of fasting after breakfast for different time reproducibility study. Each study in the same subject was performed at least 3 days apart in random orders. For each study, acquisition of 10 minute fasting gastric SPECT was performed in supine position to determine the fasting gastric volume at 30 minutes after intravenous administration of 185 MBq 99mTc-pertechnetate. Subsequently, the postprandial gastric scintigraphic images were acquired every 10 minutes for 50 minutes after the subject ingested a standard liquid meal including 64% carbohydrate, 22% fat and 14% protein (250 mL and 266 kcal of Ensure®, Abbott, Hoofddorp, Netherlands). This standard liquid meal has been used in the range of 237-300 mL and 250-317 kcal for GA studies in several studies.4,6,8,9,11,16 Five sets of postprandial SPECT data were succeedingly acquired to determine maximal postprandial gastric volume. All subjects were informed to ingest all of the standard liquid meal within 3 minutes.
2. Single photon emission computed tomography technique
SPECT was performed using a triple-head gamma camera (Triad XLT 20, Trionix, Twinsburg, OH, USA) equipped with low-energy ultrahigh-resolution collimators. Gastric scintigraphic images were acquired into a 128 × 128 matrix, every 5° at 20 seconds per image, taking 10 minutes to complete 360°. These data were subsequently reconstructed using filtered back-projection (Ramp-Butterworth filter, order 10, cut-off 0.45 Nyquist) to produce transaxial images of the stomach.
The transaxial images of the stomachs were subsequently analyzed using the freely available Image J software (National Institute of Health, Bethesda, Maryland, USA) similar to the study by Simonian et al.10 Total gastric volume calculation from the transaxial images of the stomach was performed by the following steps: (1) using the thresholding technique with arbitrary cut-off number to eliminate the activity from outside of the stomach wall, (2) manual deletion of extragastic activity that cannot be eliminated by thresholding technique, (3) manual line drawing to complete gastric wall defect caused by thresholding technique, (4) filling the activity in the stomach space to produce solid stomach area and (5) counting all gastric voxels and multiplied by voxel volume to produce gastric volume. The GA was the maximal postprandial gastric volume minus the fasting gastric volume.
The volume calculations were blindly performed by 2 nuclear medicine physicians to assess inter-observer reliability and blindly repeated by 1 nuclear medicine physician to assess intra-observer reliability.
3. Sample size calculation
From intraclass correlation power analysis table, the sample size of 20 would have power of 0.91 with intraclass correlation coefficient (ICC) of 0.6 and significant level of 0.05.
4. Statistical methods
Data were expressed as means ± SD. Intra- and inter-observer reliabilities were determined as ICC and coefficient of variation (CV, expressed in percent).
ICC and intrasubject CV were calculated to assess the same time (2 morning studies), the first different time (first morning study and afternoon study) and the second different time (second morning study and afternoon study) reproducibility. The reproducibility was considered very good, good, fair, poor and very poor if ICC value was 0.8-1.0, 0.6-0.8, 0.4-0.6, 0.2-0.4 and 0.0-0.2, respectively. All data were analyzed by the SPSS software (version 15.0, SPSS Inc, Chicago, USA).
Results
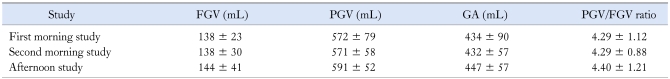
All volunteers completed the studies without any adverse events. The fasting gastric volumes, maximal postprandial gastric volumes, GA and maximal postprandial/fasting gastric volume ratios derived from all GA studies of the first morning, second morning and the afternoon were showed in Table 1. There were no significant differences in fasting gastric volumes, maximal postprandial gastric volumes, GA volumes and maximal postprandial/fasting gastric volume ratios among the 3 study sessions (p > 0.05).
Table 1.
Fasting Gastric Volumes (FGV), Maximal Postprandial Gastric Volumes (PGV), Gastric Accommodation and Maximal PGV/FGV Ratios in the First and Second Morning Study and the Afternoon Study
GA, gastric accommodation.
Data were presented as means ± SD.
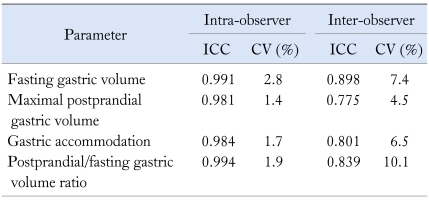
1. Intra-observer and inter-observer reliability
The intra and inter-observer ICC and CV for the fasting gastric volume, maximal postprandial gastric volume, GA and postprandial/fasting gastric volume ratio were demonstrated in Table 2. The results suggest that this technique was highly reliable for both the intra- and inter-observer measurements.
Table 2.
Intra-observer and Inter-observer Intraclass Correlation Coefficient and Coefficient of Variation
ICC, intraclass correlation coefficient; CV, coefficient of variation.
2. Reproducibility of the gastric accommodation studied at the same time and different time of the day
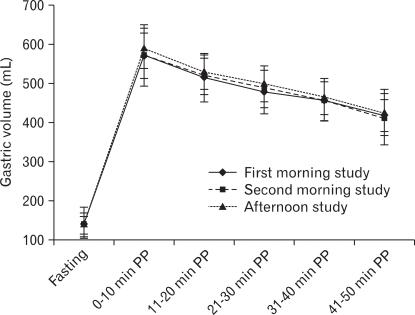
The mean fasting and postprandial gastric volumes measured at each time point from the first and second morning study and the afternoon studies were plotted in Figure 1. The postprandial gastric volumes were similar through the entire the 50 minute postprandial periods among the 3 study sessions (p > 0.05). The maximal postprandial gastric volumes occurred in the first 10 minutes in all studies of all volunteers.
Figure 1.
Mean fasting and postprandial gastric volumes in the first and second morning study and the afternoon study. PP, postprandial.
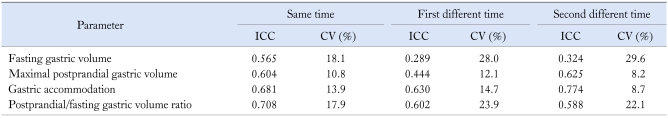
The intrasubject ICC and CV of the same time (2 morning studies), the first different time (first morning study and afternoon study) and the second different time (second morning study and afternoon study) studies for fasting gastric volume, maximal postprandial gastric volume, GA and postprandial/fasting gastric volume ratio were demonstrated in Table 3. GA measured by SPECT showed good reproducibility for both the same and different time of the day. Maximal postprandial gastric volume and postprandial/fasting gastric volume ratio were also reproducible with higher reproducibility for the same time of the day than the different time of the day. Although, the reproducibility of fasting gastric volume was acceptable for the same time study but was poor for the first and second different times of the day.
Table 3.
The Same Time (2 Morning Studies), the First Different Time (First Morning Study and Afternoon Study) and the Second Different Time (Second Morning Study and Afternoon Study) Intrasubject Intraclass Correlation Coefficient and Coefficient of Variation
ICC, intraclass correlation coefficient; CV, coefficient of variation.
The intersubject CV of fasting gastric volumes, maximal postprandial gastric volumes, GA volumes and the postprandial/fasting gastric volume ratios were 16.7%, 13.8%, 20.7% and 26.1%, respectively, in the first morning, 21.7%, 10.2%, 13.1% and 20.5%, respectively, in the second morning and 28.3%, 8.7%, 12.7% and 27.5%, respectively, in the afternoon studies.
Discussion
GA is a reflex relaxation of the proximal stomach in response to meal ingestions.2,17,18 Several studies demonstrated that impaired GA is associated with functional dyspepsia1,8,19 whereas excessive GA is associated with gastroesophageal reflux disease.20 The impaired GA may lead to increased intragastric distribution to the antrum in functional dyspepsia.21 There has been a report that symptoms score of bloating was significantly related to the cross sectional area of antrum.22 Since the proximal stomach contributes to the majority of total gastric volume, the total gastric volume changes after meal ingestion, therefore, reflect the proximal stomach volume changes. The upper gastrointestinal symptoms associated with proximal gastric motor functions have been reported.23 The measurement of proximal gastric motor function or GA is important especially in clinical research studies for identifying gastric function abnormality, which may underlie patients' upper gastrointestinal problems.
The SPECT method could be used as a non-invasive method for measuring gastric volume and GA.4-10 However, reproducibility of this technique has only been addressed in a limited number of studies.10 In addition, the reproducibility of this test when performing at the same and different time of the day has not been known. This information is important since the limited number of equipment makes the study of GA by SPECT at the same time in every patient impossible.
In this study, we demonstrated the measurement of GA by SPECT using the freely available Image J software to be reliable and reproducible. When the results were interpreted either by different or same observer, there were fairly high levels of inter- and intra-observer reliability. In addition, whether the study was performed at the same or different time of the day, the results of GA showed good reproducibility.
There were some difficulties in gastric images processing due to interfering activity from bowel or kidneys and nonuniformity of gastric wall activity in some volunteers requiring manual deletion of extragastic activity and manual drawing of some parts of gastric wall which were operator-dependent. The other potential pitfall was the inclusion of gastric wall in gastric volume counting which might have overestimated the actual internal gastric volume.
The mean fasting gastric volume derived from this study (138 mL) was relatively less than the mean fasting gastric volume from most of other studies using SPECT in subjects in Western countries, which ranged from 174 mL to 397 mL.4,6-10 This might be explained by the ethnic differences (Asian vs White) and implies that fasting gastric volumes of Asian (Thai) people are smaller than Western people.
The same time day-to-day intrasubject CV of GA volumes measurement from our study (13.9%) which used Image J software was comparable to that from the study by De Schepper et al which used commercial analysis software (13.8%)11 and was less than that of barostat (19%)24 but higher than that of MRI technique (4%).25
The intrasubject CVs from this study are comparable with that of 2 hour gastric emptying from the gold standard, well-established, 99mTc-labeled solid meal gastric emptying scintigraphy (14%)26 and even less than that of gastric emptying from 99mTc-labeled liquid meal scintigraphy (25%).27 The results in our study suggest that 17 and 4 subjects will be required for clinical research studies of 2 independent groups and 2 related groups respectively, to demonstrate the 25% change of GA volume (α = 0.05 and β = 0.1).
In conclusion, GA (postprandial-fasting gastric volume difference) measured by 99mTc-pertechnetate SPECT and Image J software shows good reproducibility at both the same and different time of the day in healthy volunteers, although the reproducibility of fasting gastric volume measurement in the different times of the day was poor. Therefore, the schedule time in the morning or in the afternoon does not appear to significantly affect the GA value.
Acknowledgements
The authors thank Dr. Vana Sangsasri for being the second physician who processed the gastric images by the Image J software to calculate the gastric volume. We also thank Mr. Wasan Panwasang, statistician, Faculty of Medicine, Chulalongkorn University for statistical advice.
Footnotes
The results of this study were presented at the second Joint International Meeting of Neurogastroenterology and Motility 2008 in Luzern, Switzerland 2008 with abstract appearing in Neurogastroenterology and Motility 2008;20(suppl 2):89 and at the Asian Pacific Digestive Disease Week 2008 in New Delhi, India with abstract appearing in Journal of Gastroenterology and Hepatology 2008;23(suppl 5):A5.
Financial support: This study was funded by a grant from the Rachadapisek Sompoch Research Fund, Faculty of Medicine, Chulalongkorn University, Bangkok, Thailand (grant No. RA7/50) and the Ratchadapisek Sompotch Endowment Fund (GI Motility Research Unit grant).
Conflicts of interest: None.
References
- 1.Tack J, Piessevaux H, Coulie B, Caenepeel P, Janssens J. Role of impaired gastric accommodation to a meal in functional dyspepsia. Gastroenterology. 1998;115:1346–1352. doi: 10.1016/s0016-5085(98)70012-5. [DOI] [PubMed] [Google Scholar]
- 2.Tack J, Lee KJ. Pathophysiology and treatment of functional dyspepsia. J Clin Gastroenterol. 2005;39(5 suppl 3):S211–S216. doi: 10.1097/01.mcg.0000156109.97999.d1. [DOI] [PubMed] [Google Scholar]
- 3.De Schepper HU, Cremonini F, Chitkara D, Camilleri M. Assessment of gastric accommodation: overview and evaluation of current methods. Neurogastroenterol Motil. 2004;16:275–285. doi: 10.1111/j.1365-2982.2004.00497.x. [DOI] [PubMed] [Google Scholar]
- 4.Kuiken SD, Samsom M, Camilleri M, et al. Development of a test to measure gastric accommodation in humans. Am J Physiol. 1999;277:G1217–G1221. doi: 10.1152/ajpgi.1999.277.6.G1217. [DOI] [PubMed] [Google Scholar]
- 5.Bennink RJ, van den Elzen BD, Kuiken SD, Boeckxstaens GE. Noninvasive measurement of gastric accommodation by means of pertechnetate SPECT: limiting radiation dose without losing image quality. J Nucl Med. 2004;45:147–152. [PubMed] [Google Scholar]
- 6.Bouras EP, Delgado-Aros S, Camilleri M, et al. SPECT imaging of the stomach: comparison with barostat, and effects of sex, age, body mass index, and fundoplication. Single photon emission computed tomography. Gut. 2002;51:781–786. doi: 10.1136/gut.51.6.781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.van den Elzen BD, Bennink RJ, Wieringa RE, Tytgat GN, Boeckxstaens GE. Fundic accommodation assessed by SPECT scanning: comparison with the gastric barostat. Gut. 2003;52:1548–1554. doi: 10.1136/gut.52.11.1548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim DY, Delgado-Aros S, Camilleri M, et al. Noninvasive measurement of gastric accommodation in patients with idiopathic nonulcer dyspepsia. Am J Gastroenterol. 2001;96:3099–3105. doi: 10.1111/j.1572-0241.2001.05264.x. [DOI] [PubMed] [Google Scholar]
- 9.Liau SS, Camilleri M, Kim DY, Stephens D, Burton DD, O'Connor MK. Pharmacological modulation of human gastric volumes demonstrated noninvasively using SPECT imaging. Neurogastroenterol Motil. 2001;13:533–542. doi: 10.1046/j.1365-2982.2001.00287.x. [DOI] [PubMed] [Google Scholar]
- 10.Simonian HP, Maurer AH, Knight LC, et al. Simultaneous assessment of gastric accommodation and emptying: studies with liquid and solid meals. J Nucl Med. 2004;45:1155–1160. [PubMed] [Google Scholar]
- 11.De Schepper H, Camilleri M, Cremonini F, Foxx-Orenstein A, Burton D. Comparison of gastric volumes in response to isocaloric liquid and mixed meals in humans. Neurogastroenterol Motil. 2004;16:567–573. doi: 10.1111/j.1365-2982.2004.00533.x. [DOI] [PubMed] [Google Scholar]
- 12.Brady M, Kinn S, Stuart P. Preoperative fasting for adults to prevent perioperative complications. Cochrane Database Syst Rev. 2003;(4):CD004423. doi: 10.1002/14651858.CD004423. [DOI] [PubMed] [Google Scholar]
- 13.Crawford M, Lerman J, Christensen S, Farrow-Gillespie A. Effects of duration of fasting on gastric fluid pH and volume in healthy children. Anesth Analg. 1990;71:400–403. doi: 10.1213/00000539-199010000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Ingebo KR, Rayhorn NJ, Hecht RM, Shelton MT, Silber GH, Shub MD. Sedation in children: adequacy of two-hour fasting. J Pediatr. 1997;131:155–158. doi: 10.1016/s0022-3476(97)70141-0. [DOI] [PubMed] [Google Scholar]
- 15.National Institutes of Health Image J software. Image processing and analysis in Java. [Google Scholar]
- 16.Delgado-Aros S, Kim DY, Burton DD, et al. Effect of GLP-1 on gastric volume, emptying, maximum volume ingested, and postprandial symptoms in humans. Am J Physiol Gastrointest Liver Physiol. 2002;282:G424–G431. doi: 10.1152/ajpgi.2002.282.3.G424. [DOI] [PubMed] [Google Scholar]
- 17.Smith ML. Functional dyspepsia pathogenesis and therapeutic options - implications for management. Dig Liver Dis. 2005;37:547–558. doi: 10.1016/j.dld.2005.04.001. [DOI] [PubMed] [Google Scholar]
- 18.Choung RS, Talley NJ. Novel mechanisms in functional dyspepsia. World J Gastroenterol. 2006;12:673–677. doi: 10.3748/wjg.v12.i5.673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gilja OH, Hausken T, Wilhelmsen I, Berstad A. Impaired accommodation of proximal stomach to a meal in functional dyspepsia. Dig Dis Sci. 1996;41:689–696. doi: 10.1007/BF02213124. [DOI] [PubMed] [Google Scholar]
- 20.Tefera S, Gilja OH, Hatlebakk JG, Berstad A. Gastric accommodation studied by ultrasonography in patients with reflux esophagitis. Dig Dis Sci. 2001;46:618–625. doi: 10.1023/a:1005619803917. [DOI] [PubMed] [Google Scholar]
- 21.Troncon LE, Bennett RJ, Ahluwalia NK, Thompson DG. Abnormal intragastric distribution of food during gastric emptying in functional dyspepsia patients. Gut. 1994;35:327–332. doi: 10.1136/gut.35.3.327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hausken T, Berstad A. Wide gastric antrum in patients with non-ulcer dyspepsia. Effect of cisapride. Scand J Gastroenterol. 1992;27:427–432. doi: 10.3109/00365529209000100. [DOI] [PubMed] [Google Scholar]
- 23.Gonlachanvit S, Maurer AH, Fisher RS, Parkman HP. Regional gastric emptying abnormalities in functional dyspepsia and gastro-oesophageal reflux disease. Neurogastroenterol Motil. 2006;18:894–904. doi: 10.1111/j.1365-2982.2006.00811.x. [DOI] [PubMed] [Google Scholar]
- 24.Sarnelli G, Vos R, Cuomo R, Janssens J, Tack J. Reproducibility of gastric barostat studies in healthy controls and in dyspeptic patients. Am J Gastroenterol. 2001;96:1047–1053. doi: 10.1111/j.1572-0241.2001.03520.x. [DOI] [PubMed] [Google Scholar]
- 25.Fruehauf H, Goetze O, Steingoetter A, et al. Intersubject and intrasubject variability of gastric volumes in response to isocaloric liquid meals in functional dyspepsia and health. Neurogastroenterol Motil. 2007;19:553–561. doi: 10.1111/j.1365-2982.2007.00904.x. [DOI] [PubMed] [Google Scholar]
- 26.Cremonini F, Mullan BP, Camilleri M, Burton DD, Rank MR. Performance characteristics of scintigraphic transit measurements for studies of experimental therapies. Aliment Pharmacol Ther. 2002;16:1781–1790. doi: 10.1046/j.1365-2036.2002.01344.x. [DOI] [PubMed] [Google Scholar]
- 27.Pomerri F, Muzzio PC, Mastropaolo G, Gasparini G, Romani S. Measurement of gastric emptying with Tc 99m. Technique and reliability of the test. Radiol Med (Torino) 1991;82:339–342. [PubMed] [Google Scholar]