Abstract
Anorectal manometry is the most well established and widely available tool for investigating anorectal function. Anal sphincter tone can be quantified by anorectal manometry. The anorectal sensory response, anorectal reflexes, rectal compliance, and defecatory function are also assessed by anorectal manometry. This report will focus on defining parameters for measurement and interpretation of anorectal manometry tests.
Keywords: Anal canal, Manometry, Rectum
Introduction
The anorectum plays an important role in regulation of defecation and in the maintenance of continence.1 The most widely used test for anorectal function is anorectal manometry. A comprehensive assessment of anorectal function consists of measuring at a minimum each of the following parameters: (1) anal sphincter function, (2) rectoanal reflex activity, (3) rectal sensation, (4) changes in anal and rectal pressures during attempted defecation, (5) rectal compliance and (6) performance of a balloon expulsion test.2
Anal Sphincter Function
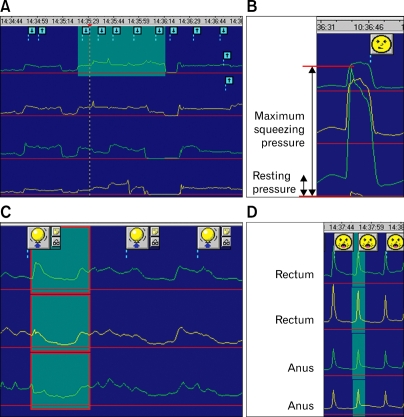
Anal sphincter function is assessed by measurement of resting sphincter pressure, squeeze sphincter pressure, and the functional length of the anal canal. Maximum resting anal canal tone predominantly reflects internal anal sphincter function, while voluntary anal squeeze pressure reflects external anal sphincter (EAS) function. Functional anal canal length is defined as the length of the anal canal over which resting pressure exceeds that of the rectum by greater than 5 mmHg or, alternatively, as the length of the anal canal over which pressures are greater than half of the maximal pressure at rest (Fig. 1A). Maximal resting anal pressure is defined as the difference between intrarectal pressure and the highest recorded anal sphincter pressure at rest, and is generally recorded 1-2 cm from the anal verge. Maximum squeeze pressure is defined as the difference between the intrarectal pressure and the highest pressure that is recorded at any level within the anal canal during the squeeze maneuver (Fig. 1B).
Figure 1.
(A) Station-pull through manometry of the anal sphincter at rest. A perfused-tube catheter is pulled through the anal sphincter in 1 cm increments (arrows). Rectal pressure is used as a baseline (red line). The anal canal is indicated in green. (B) Normal squeeze response. Maximum squeeze pressure is defined as the difference between intrarectal pressure and the highest pressure that is recorded at any level within the anal canal during the squeeze maneuver. (C) Rectoanal inhibitory reflex. The presence of rectoanal inhibitory reflex is recorded when the balloon is distended with a 50 mL volume of air. (D) Cough reflex. Manometric findings in a patient with fecal incontinence, showing a negative anus-to-rectum pressure gradient during coughing.
Rectoanal Reflex Activity
Rapid distention of the rectum induces a transient increase in rectal pressure, followed by a transient increase in anal pressure associated with EAS contraction (the rectoanal contractile reflex), and in turn, a more prolonged reduction in anal pressure due to relaxation of the internal anal sphincter (the rectoanal inhibitory reflex, Fig. 1C). The rectoanal contractile reflex is a compensatory guarding mechanism that allows a positive anorectal pressure gradient to be maintained during transient increases in intra-abdominal pressure (such as coughing), which is essential for preserving continence. In fecal incontinence patients, anal sphincter pressure is not increased over the intra-abdominal pressure during coughing (Fig. 1D).3
Rectal Sensation
The lowest volume of air that evokes sensation and a desire to defecate, and the maximum tolerable volume are recorded.4 Assessment of rectal sensation is useful in patients with fecal incontinence or rectal hyposensitivity. Neuromuscular conditioning using biofeedback techniques can be effective in improving impaired rectal sensation.2
Changes in Anal and Rectal Pressures During Attempted Defecation
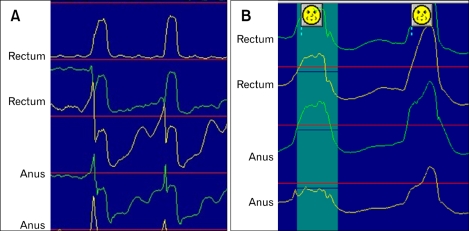
When an individual is requested to 'bear down,' as if attempting to defecate, the normal response consists of an increase in rectal pressure that is coordinated with a relaxation of the EAS (Fig. 2A). Inability to perform this coordinated maneuver suggests a diagnosis of dyssynergic or obstructive defecation, a common cause of constipation.5 This response can be quantified using the defecation index = maximum rectal pressure during attempted defecation/minimum anal residual pressure during attempted defecation. A normal defecation index is > 1.5.5 Three types of dyssynergic defecation are recognized.6 Most patients show paradoxical increase in anal sphincter pressure during attempted defecation with normal adequate pushing force (type 1, Fig. 2B). Some patients are unable to generate an adequate pushing force, and exhibit a paradoxical anal contraction (type 2). In type 3, the patient can generate an adequate pushing force, but has absent or incomplete (< 20%) sphincter relaxation.
Figure 2.
Manometric findings during attempted defecation. (A) Normal rectal and anal pressure changes during defecation. (B) Rectal and anal pressure changes during attempted defecation in a constipated patient with type 1 dyssynergic defecation.
Rectal Compliance
Rectal compliance reflects the capacity and distensibility of the rectum. Rectal compliance is calculated by plotting the relationship between balloon volume (dV) and steady state intrarectal pressure (dP). Higher compliance indicates lower resistance to distention and vice versa.
Balloon Expulsion Test
The balloon expulsion test is used to assess rectoanal co-ordination during defecatory maneuvers.7 The test evaluates a patient's ability to expel a filled balloon from the rectum, providing a simple and more physiologic assessment of defecation dynamics. Most normal subjects can expel the balloon within 1 minute.5 If the patient is unable to expel the balloon within 3 minutes, dyssynergic defecation should be suspected.
Conclusion
Conventional anorectal manometry provides many useful data regarding anorectal function. Appropriate interpretation of these tests will further increase their clinical utility.
Footnotes
Financial support: None.
Conflicts of interest: None.
References
- 1.Barnett JL, Hasler WL, Camilleri M American Gastroenterological Association. American Gastroenterological Association medical position statement on anorectal testing techniques. Gastroenterology. 1999;116:732–760. doi: 10.1016/s0016-5085(99)70194-0. [DOI] [PubMed] [Google Scholar]
- 2.Sun WM, Rao SS. Manometric assessment of anorectal function. Gastroenterol Clin North Am. 2001;30:15–32. doi: 10.1016/s0889-8553(05)70165-5. [DOI] [PubMed] [Google Scholar]
- 3.Jorge JM, Wexner SD. Anorectal manometry: techniques and clinical applications. South Med J. 1993;86:924–931. doi: 10.1097/00007611-199308000-00016. [DOI] [PubMed] [Google Scholar]
- 4.Rao SS, Azpiroz F, Diamant N, Enck P, Tougas G, Wald A. Minimum standards of anorectal manometry. Neurogastroenterol Motil. 2002;14:553–559. doi: 10.1046/j.1365-2982.2002.00352.x. [DOI] [PubMed] [Google Scholar]
- 5.Rao SS, Hatfield R, Soffer E, Rao S, Beaty J, Conklin JL. Manometric tests of anorectal function in healthy adults. Am J Gastroenterol. 1999;94:773–783. doi: 10.1111/j.1572-0241.1999.00950.x. [DOI] [PubMed] [Google Scholar]
- 6.Rao SS. Dyssynergic defecation. Gastroenterol Clin North Am. 2001;30:97–114. doi: 10.1016/s0889-8553(05)70169-2. [DOI] [PubMed] [Google Scholar]
- 7.Scott SM, Gladman MA. Manometric, sensorimotor, and neurophysiologic evaluation of anorectal function. Gastroenterol Clin North Am. 2008;37:511–538. vii. doi: 10.1016/j.gtc.2008.06.010. [DOI] [PubMed] [Google Scholar]