Abstract
This study examined the association between childhood ADHD and juvenile delinquency by examining data from the Pittsburgh ADHD Longitudinal Study (PALS), a follow-up study of individuals diagnosed with ADHD in childhood (ages 5–12) and recontacted in adolescence and young adulthood for yearly follow-up (age at first follow-up interview M= 17.26, SD=3.17). Participants were 288 males with childhood ADHD and 209 demographically similar males without ADHD who were recruited into the follow-up study. Delinquency information gathered yearly during the second through eighth follow-up provided a comprehensive history of juvenile delinquency for all participants. Four childhood diagnostic groups [ADHD-only (N=47), ADHD+ODD (N=135), ADHD+CD (N=106), and comparison (N=209)] were used to examine group differences on delinquency outcomes. Analyses were conducted across three dimensions of delinquency (i.e., severity, age of initiation, and variety). Individuals with childhood ADHD+CD displayed significantly worse delinquency outcomes than the other three groups, across almost all indices of offending. When compared to comparison participants, boys with ADHD-only and ADHD+ODD in childhood displayed earlier ages of delinquency initiation, a greater variety of offending, and higher prevalence of severe delinquency. These findings suggest that although childhood ADHD+CD creates the greatest risk for delinquency, boys with ADHD-only and ADHD+ODD also appear at a higher risk for later offending. The patterns of offending that emerged from the PALS are discussed in the context of the relationship between ADHD, comorbidity, and delinquency.
Keywords: ADHD, Delinquency, Conduct Disorder
Every year thousands of individuals fall victim to criminal acts committed by juveniles in the United States. In 2006, 19.1% of property crimes and 12.1% of violent crimes involved only juveniles (U.S. Department of Justice, 2007). The young individuals who commit these crimes are at a high risk of continuing this criminality into adulthood (Loeber, 1982; Moffitt, Caspi, Harrington, & Milne, 2002), which also incurs a high economic cost to society. By one estimate, a lifetime criminal costs the public between $1.3 million and $1.5 million (Cohen, 1998). In addition to the increased risk of adult criminality, delinquent adolescents are also more likely to experience multiple negative personal outcomes in adulthood, ranging from substance abuse to work-related problems (Loeber, Stouthamer-Loeber, & White, 1999; Moffitt et al., 2002).
Given the gravity of juvenile offending, much attention has been directed toward identifying developmental pathways to serious delinquency in order to identify children who are most at risk for this costly outcome. Although minor delinquency appears to be somewhat normative and transient in adolescence, a subset of offenders display a pattern of severe and persistent offending that begins in childhood (Loeber, 1988; Moffitt 1993; 2003). These individuals are most troublesome as they are more likely to continue their criminal behavior into adulthood, commit more severe and violent crimes, and experience a variety of poor personal outcomes (Moffit & Caspi, 2001; Stouthamer-Loeber & Loeber, 2002). There is currently consensus that the progression to serious delinquency begins early, with problems at school, at home, and with peers. Most agree with the hypothesis that this troubling path begins with impulsivity, ADHD, undercontrolled temperament, or some variant thereof (Loeber, 1988; McMahon & Kotler, 2006; Moffitt, 1993; Patterson, DeGarmo, & Knutson, 2000). Negative environmental factors (e.g., poor parenting, life stressors) are thought to lead to an escalation of antisocial behavior that qualifies many for a comorbid diagnosis of Oppositional Defiant Disorder (ODD) and, eventually, Conduct Disorder (CD; Burke, Loeber, Lahey, & Rathouz, 2005; Lahey & Loeber, 1994; Patterson et al., 2000). By one estimate, the progression to comorbid ODD develops in 59% of school-aged children with ADHD (Barkley, 2006). In about two-thirds of these children diagnosed with ADHD+ODD, CD later develops (Greene, 2005). In these children, antisocial behavior often becomes chronic and evolves into a pattern of problematic delinquency.
Data from many longitudinal samples of children with ADHD support the hypothesis that these children are at an increased risk of qualifying for CD in adolescence (Gittelman, Mannuzza, Shenker, & Bonagura, 1985; Lambert, 1988; Mannuzza, Klein, Abikoff, & Moulton, 2004). However, few studies examine the relation between childhood ADHD and subsequent delinquent offending (Lee & Hinshaw, 2004; Loeber, Brinthaupt, & Green, 1990; Molina et al., 2007a; Satterfield, Hoppe, & Schell, 1982; Satterfield, Swanson, Schell, & Lee, 1994). The distinction between these outcomes is important as the overlap between CD and delinquency is only partial. The CD criteria include non-criminal acts such as lying, staying out past curfew, and bullying (APA, 2000), and they do not provide a comprehensive list of delinquent behaviors. As such, delinquency is present in a minority of children with CD (Burke, Loeber, Mutchka, & Lahey, 2002), and many children who commit delinquent acts fail to qualify for a diagnosis of CD (Molina et al., 2007a). The studies cited above provide evidence that children with ADHD are more likely than those without ADHD to offend in adolescence; however, most data suggest that this relationship is influenced by the development of childhood conduct problems subsequent to the onset of ADHD (Biederman, Mick, Faraone, & Burback, 2001; Lee et al., 2004; Lilienfeld & Waldman, 1990; Loeber, Burke, Lahey, Winters, & Zera, 2000). This repeated finding is consistent with the hypothesis that many children with ADHD follow a maladaptive pathway to serious delinquency, but that only those who develop childhood CD become severe and persistent offenders.
Some evidence also suggests that children with ADHD who do not have serious conduct problems in childhood are also at a higher risk for later delinquent offending. Several studies have found elevated rates of later delinquency in children with ADHD who were not diagnosed with comorbid ODD or CD (Loeber et al., 1990; Farrington, Loeber, & Van Kammen, 1990; Satterfield et al., 1994; Molina et al., 2007a). There are also established links between the core symptoms of ADHD and delinquent offending (Carroll et al., 2006; Kagan & Zentner, 1996; Klinteberg, 1997; Loeber, Pardini, Stouthamer-Loeber, & Raine, 2007; White et al., 1994), even after controlling for conduct problems (Babinski et al., 1999; Pardini, Obradovic, & Loeber, 2006), although exceptions to these findings exist (Lahey et al., 2000; Satterfield & Schell, 1997) Mixed findings on the relationship between ADHD and delinquency highlight the need for further studies with more exhaustive techniques for examining this association.
Notably, a number of questions remain about the relationship between childhood ADHD and delinquency. For example, although studies have examined the presence of offending within the ADHD population (Biederman et al., 2001; Satterfield, 1982; 1994), there has been less emphasis on delinquency severity (Lee et al., 2004; Molina et al., 2009a) and variety (Loeber et al., 1990). Delinquency severity is an important characteristic of the persistent offender (Loeber, 1988) and delinquency variety shows associations with lower self-control and a greater propensity to offend repeatedly (Mazerolle, Brame, Paternoster, Piquero, & Dean, 2000). Furthermore, examinations of severity and variety outcomes in ADHD samples have involved very young adolescents who have not likely reached their offending peak (Lee et al., 2004; Loeber et al., 1990; Molina et al., 2007a). Variety of offending (i.e., the number of different delinquent acts that a participant endorses in the lifetime) is also likely to increase with age simply due to the passage of time and increased opportunity. Consequently, follow-up studies that span adolescence are needed to investigate the timing of delinquency initiation in ADHD samples. In addition, almost no research examines risk for delinquency among children with ADHD and comorbid ODD (Satterfield et al., 1994). Given the important role of ODD in the progression from ADHD to CD (Burke et al., 2005), better understanding of this association may elucidate the relative contributions of ADHD, ODD, and CD toward the later development of delinquency.
The current study seeks to address the questions raised above by examining the delinquent behavior of the males in the Pittsburgh ADHD Longitudinal Study (PALS; Molina et al., 2007b). The PALS is a study of individuals diagnosed with and treated for ADHD in childhood (baseline) and recontacted in adolescence and young adulthood for yearly follow-up visits. In the current study, we examined the contribution of childhood diagnosis (ADHD-only, ADHD+ODD, ADHD+CD, and no diagnosis) to the prediction of later lifetime delinquency severity and variety as well as to the age of initiation at each delinquency severity level (i.e., mild, moderate, severe). We hypothesized the following: 1) that overall prevalence of severe offending would increase incrementally with the severity of childhood diagnostic group, but mild and moderate offending would not due to the more normative nature of these lesser offense categories (Junger-Tas, Terlouw, & Klein, 1994), 2) that across delinquency severity levels, earlier ages of initiation would correspond with the severity of childhood diagnosis, and (3) that variety of offending would also increase in a stepwise fashion along with the severity of childhood diagnosis.
Method
Participants
Probands
At the start of the follow-up study, probands were recruited from a pool of 466 study-eligible adolescent and young adult males who were previously diagnosed with DSM-III-R or DSM-IV ADHD and treated at the ADD clinic at the Western Psychiatric Institute and Clinic in Pittsburgh, PA in childhood (baseline). In the current study, probands were 288 males in the PALS who were age 12 or younger at baseline. Of the 466 study eligible adolescent and young adult males, 23 could not be located at follow-up, 129 refused or failed to participate, and 26 were older than 12 at initial referral to the clinic (baseline). Age at baseline evaluation ranged from 5.0 to 12.83 years (M= 8.92, SD=1.79).
In childhood (baseline), all probands participated in the Summer Treatment Program (STP) for children with ADHD, an 8-week intervention that included behavioral modification, parent training, and psychoactive medication trials where indicated (Pelham & Hoza, 1996). Children were referred to the STP from across Allegheny County, PA by several large public sources, such as Pittsburgh Public Schools. Diagnostic information for probands was collected at baseline using parent and teacher DSM-III-R and DSM-IV symptom ratings scales (DBD; Pelham, Evans, Gnagy, & Greenslade, 1992) and a semi-structured diagnostic interview administered to parents by a Ph.D. level clinician. The interview consisted of the DSM-III-R or DSM-IV descriptors for ADHD, ODD, and CD with supplemental probe questions regarding situationality and severity. It also included queries about other comorbidities to determine whether additional assessment was needed (instrument available at http://ccf.fiu.edu). Following DSM guidelines, diagnoses of ADHD, ODD, and CD were made if a sufficient number of symptoms were endorsed (considering information from both parents and teachers) to result in diagnosis. Two Ph.D. level clinicians independently reviewed ratings and interviews to confirm diagnoses and when disagreement occurred, a third clinician reviewed the file and the majority decision was used. Exclusion criteria for probands were assessed at this baseline assessment and included a full-scale IQ < 80, a history of seizures or neurological problems, and/or a history of pervasive developmental disorder, schizophrenia, or other psychotic or organic mental disorders.
Probands began participation in the follow-up study an average of 8.35 (SD=2.79) years after baseline assessment and treatment at the ADD clinic. They were recontacted and admitted to the study on a rolling basis as adolescents and young adults (11 to 28 years of age; all but three <25) and completed their first follow-up interview upon enrollment. Participants in the follow-up study were compared with the eligible individuals who did not enroll on demographic (i.e., age at first treatment, race, parental education level, and marital status) and diagnostic (i.e., parent and teacher ratings of ADHD and related symptomatology) variables collected at baseline. Only one of 14 comparisons was statistically significant at the p<.05 significance level. Participants had a slightly lower average CD symptom rating on a four point scale as indicated by a composite of parent and teacher ratings (participants M = .43, non-participants M = .53).
Comparison Group
Comparison participants were 209 males without ADHD. Comparison participants were recruited for the PALS from the greater Pittsburgh community at the same time as probands were recontacted to enroll in the follow-up study. These individuals were recruited from several sources including pediatric practices in Allegheny County (40.8%), advertisements in local newspapers (27.5%), local universities and colleges (20.8%), and other methods (10.9%) such as Pittsburgh Public Schools and word of mouth. Like probands, comparison participants were recruited on a rolling basis. Comparison recruitment lagged three months behind proband enrollment in order to facilitate efforts to obtain demographic similarity (discussed below). A telephone screening interview was administered to parents of potential comparison participants to gather basic demographic characteristics, history of diagnosis or treatment for ADHD and other behavior problems, presence of exclusionary criteria as previously listed for probands, and a full checklist of ADHD symptoms. Older individuals (age 18+) also provided self-report. ADHD symptoms were counted as present if reported by either the parent or the young adult. Individuals who met DSM-III-R criteria for ADHD, either currently or historically, were immediately excluded from study consideration. Although a history of ODD and CD were not exclusion criteria for comparison participants, parent and self-report indicated that only one comparison participant had a history of ODD-like behaviors in childhood and no comparison participants displayed a history of CD-like behaviors. At recruitment, average ADHD symptom severity for the comparison group was .65 (0–3 scale).
If a potential comparison participant passed the initial phone screen, senior research staff members met to determine whether he was demographically appropriate for the study. Four demographic characteristics were examined for each potential comparison participant: 1) age, 2) gender, 3) race, and 4) parent education level. A comparison participant was deemed study-eligible if his enrollment increased the comparison group's demographic similarity to the probands. At the end of the recruitment process, the proband and comparison groups were equivalent on the four demographic variables noted above. An unsuccessful attempt was made to obtain equivalence on the proportion of parents who were married (see Table 1).
Table 1.
Characteristics of the Sample at Baseline and First Follow-up Visit
| Comparison (N=209) | ADHD-only (N=47) | ADHD+ODD (N=135) | ADHD+CD (N= 106) | |
|---|---|---|---|---|
| Diagnostic Variables at Baseline | ||||
| ADHD | ||||
| Symptoms Endorsed | ---------- | 11.23(1.90) | 12.88(1.60) | 13.09(1.34) |
| Severity Score | ---------- | 2.05 (.44) | 2.28(.41) | 2.40(.36) |
| ODD | ||||
| Symptoms Endorsed | ---------- | 2.57 (1.17) | 7.08(1.35) | 7.82(1.20) |
| Severity Score | ---------- | .83 (.32) | 1.93(.51) | 2.23(.44) |
| CD | ||||
| Symptoms Endorsed | ---------- | .38 (.61) | 1.13(.76) | 4.14(1.39) |
| Severity Score | ---------- | .15 (.11) | .32(.18) | .72(.27) |
| Demographics at First Follow-up | ||||
| Age (M, SD) | 17.00 (3.15) | 17.68 (3.02) | 16.84(3.04) | 17.59(3.38) |
| Racial Minority (%) | 14.4 | 15.6 | 21.2 | 15.5 |
| African-American (%) | 8.1 | 11.1 | 14.4 | 5.8 |
| Other (%) | 6.3 | 4.5 | 6.8 | 9.7 |
| Highest Parent Education† | ||||
| High School Grad or GED (%) | 9.1 | 4.9 | 8.3 | 9.1 |
| Partial College (%) | 29.9 | 46.3 | 31.7 | 47.7 |
| College or University Grad (%) | 26.4 | 19.5 | 31.7 | 25.0 |
| Graduate Training (%) | 34.5 | 29.3 | 28.3 | 18.2 |
| % Single Parent Household† | 24.7 | 31.7 | 36.3 | 32.6 |
Note. Symptom endorsed is total number of symptoms reported by either parent or teacher on the DBD rating scale or DBD interview. Severity score is the higher score reported by either parent or teacher on the DBD rating scale, calculated by taking the average symptom level on a scale from 0 “not at all present” to 3 “very much present
p<.25.
Procedure
As noted, baseline diagnoses were gathered for probands at initial referral to the clinic during childhood. Follow-up interviews in adolescence and young adulthood were conducted by post-baccalaureate research staff. All questionnaires (paper and pencil or web-based) in the current study were completed privately. During informed consent, participants were assured of the confidentiality of disclosed materials. In cases where distance prevented participant travel to WPIC, information was collected through mail, telephone correspondence, and home visits. PALS follow-up interviews were conducted yearly beginning in the year of enrollment. As a result, the year (e.g., 2000) in which a participant completed a given interview (e.g., follow-up interview 1) varied across individuals. The collection of lifetime delinquency data began at the second annual interview. Data for the current study were from the second through the eighth annual interviews. By the 8th interview, all participants had turned 18 years old which provided a cumulative record of delinquency through age 18 for all participants.
Measures of Delinquency
Delinquency ratings were calculated from data collected by the Self-Reported Delinquency questionnaire (SRD; Elliott, Huizinga, & Ageton, 1985). During the second (age M = 18.11, SD= 3.18), third (age M = 19.15, SD= 3.16), and fourth (age M = 20.22, SD= 3.23) annual interviews, all participants and parents were asked to provide information about lifetime engagement in 37 delinquent acts (e.g., Have you ever snatched someone's purse or wallet?), including initiation age (e.g., How old were you when you first snatched someone's purse or wallet?), setting (e.g., Did any of these occur at school?), and the value of damages (e.g., What was the dollar value?). At least three lifetime reports were available for most participants (88.7%). A minority provided lifetime delinquency information at only two interviews (6.5%) or at one interview (4.8%). At the fifth follow-up interview, only participants who were still under 18 at the previous interview (18%) were administered the SRD. These individuals were asked to report on delinquency during the past year until the follow-up interview at which they reached the age of 18. Past-year reporting continued for 12.3% of the sample at the sixth follow-up interview, 7.8% at the seventh follow-up interview, and 3.2% at the eighth follow-up interview.
At each follow-up interview, parent report was compared to self-report and an act was counted if endorsed by either reporter. In a few cases (N=12), follow-up interviews were not conducted with parents and youth report alone was used. Because the current study concerns itself only with juvenile delinquency, acts reported as being committed after the age of 18 (according to SRD follow-up questions) were not included in analyses. All available reports were integrated to provide a comprehensive lifetime history of juvenile offending for all participants.
Severity
Lifetime severity ratings were coded according to the scheme developed by Wolfgang, Figlio, Tracey, and Singer (1985) and used extensively in the Pittsburgh Youth Study (Loeber et al., 1991). Three levels of delinquency severity were coded at each follow-up interview based on whether or not a participant or his parent reported an act at a given level: mild = minor delinquency outside of the home (e.g., vandalism with damages less than $100, avoiding payment, theft of less than $5); moderate = moderately serious delinquency (e.g., credit card fraud, theft of $5 or more, arson with damages over $100, joyriding); severe = serious delinquency (e.g., breaking and entering, vehicle theft, attacking someone with a weapon with the intent to seriously hurt or kill, rape). For each participant, codes from each available follow-up interview were integrated to indicate the presence of offending (yes/no) and age of initiation (up to age 18) for each severity level of delinquency (based on the SRD follow-up questions).
Variety
A lifetime estimate of delinquency variety was obtained by summing the total number of types of acts (out of 34) that a participant or his parent endorsed as occurring before age 18 (Loeber et al., 1990; Mazerolle et al., 2000). Three acts are routinely omitted from coding due to deviation from the delinquency construct (i.e., arrest, carrying a concealed weapon, drug selling). The variety categorization did not account for the number of times each act was committed, rather served as a measure of variety across category. A participant's variety score consisted of the total number of acts a participant endorsed across all follow-up interviews.
Analytic Plan
Prior to the analyses all demographic characteristics were examined by the four childhood diagnostic subgroups [ADHD-only (N=47), ADHD+ODD (N=135), ADHD+CD (N=106), no diagnosis (N=209)]. Single parent household and parental education tended toward group differences but were not statistically significant (p<.25). Nevertheless, these variables were included as covariates in all models to ensure that they were not contributing to subgroup differences in delinquency outcomes. The three proband diagnostic groups did not significantly differ in their average age at baseline [F(2,285)= .60, p=.55]; however, given the wide age range (11–28) at enrollment into the follow-up study, age at the first follow-up interview was also entered into all models to control for any differential recall that may have occurred as a result of the participant's age at follow-up.
Severity
Three survival analyses were conducted to examine potential childhood diagnostic group differences (ADHD-only, ADHD+ODD, ADHD+CD, no diagnosis) in the prevalence of offending at each severity level (mild, moderate, severe). Survival rates were expressed as percentages of youth who had offended at a given severity level through age 18 calculated using the Cox regression method. Cox regression curves and log-likelihood tests were used to test the difference between the groups' offending curves. For severe delinquency, additional planned comparisons (ADHD-only vs. ADHD+ODD; ADHD-only vs. ADHD+CD; ADHD+ODD vs. ADHD+CD) were conducted in order to further examine the relative risk of childhood diagnosis in predicting this most clinically significant variable. A Bonferroni correction for three planned comparisons set a pre-established alpha-level of .02 for this analysis.
Age of Initiation
A Generalized Linear Model using a normal distribution and an identity link function was employed to compare the four childhood diagnostic groups on age of initiation for mild, moderate, and severe delinquency. Comparison participants were used as a reference group and childhood diagnosis dummy codes (ADHD-only: yes vs. no; ADHD + ODD: yes vs. no; ADHD + CD: yes vs. no) as the independent variable. Additional planned comparisons (ADHD-only vs. ADHD+ODD; ADHD-only vs. ADHD+CD; ADHD+ODD vs. ADHD+CD) were conducted to examine the relative risk of comorbid ODD and CD diagnosis. A Bonferroni correction for three planned comparisons set a pre-established alpha-level of .02 for this analysis. Generalized Linear Modeling has been shown to be a powerful method of detecting relationships involving normally and non-normally distributed variables (McCullagh & Nelder, 1989).
Variety
A Generalized Linear Model using a normal distribution and an identity link function was employed to compare the four childhood diagnostic groups on delinquency variety. Comparison participants were used as a reference group and childhood diagnosis dummy codes (ADHD-only: yes vs. no; ADHD + ODD: yes vs. no; ADHD + CD: yes vs. no) as the independent variable. Additional planned comparisons (ADHD-only vs. ADHD+ODD; ADHD-only vs. ADHD+CD; ADHD+ODD vs. ADHD+CD) were conducted in order to further examine the relative risk of comorbid ODD and CD diagnosis. A Bonferroni correction for three planned comparisons set a pre-established alpha-level of .02 for this analysis.
Results
Severity
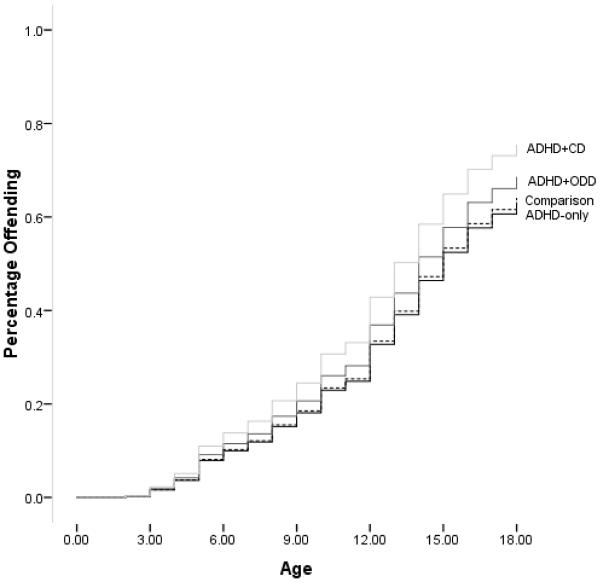
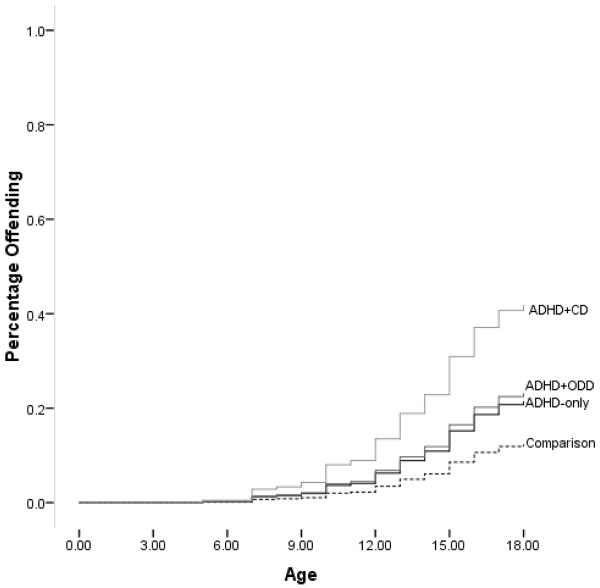
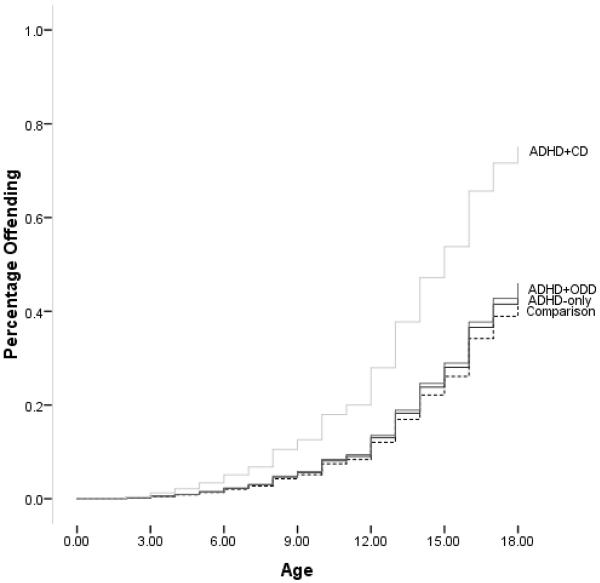
Figures 1a–1c display prevalence of offending for the childhood diagnostic groups across mild, moderate, and severe delinquency. Only 23.9% of comparison participants, 29.8% of ADHD-only, 25.9% of ADHD+ODD, and 17.8% of ADHD+CD completely abstained from delinquent offending at any severity level. For mild delinquency, the overall test of the model was non-significant [X2(8)=6.55, p=.59], indicating that all four groups showed a similar prevalence of mild offendng (see Table 2). For moderate delinquency, the overall test of the model was significant [X2(58)=46.99, p<.01], and after controlling for the covariates, only probands with a childhood diagnosis of ADHD+CD displayed a pattern of moderate offending that was significantly different from that of comparison participants (see Table 2). For severe delinquency, the overall test of the model was also significant [X2(5)=37.35, p<.01], and after controlling for the covariates, probands with childhood ADHD+CD and ADHD+ODD displayed a prevalence of severe offending that was significantly higher than comparison participants. ADHD-only probands did not significantly differ from comparison participants (p=.12), despite displaying a nearly identical pattern of severe offending to the ADHD+ODD group (see Table 2 & Figure 1c). Planned comparisons revealed that risk for severe offending did not differ significantly between the ADHD-only and the ADHD+ODD groups (OR=1.63, p=.36) or between the ADHD+ODD and the ADHD+CD groups (OR=1.58, p=.22); however, individuals with a childhood diagnosis of ADHD+CD (OR= 2.57, p=.07) were more likely than individuals with a childhood diagnosis of ADHD-only to engage in severe delinquency.
Figure 1a. Mild Delinquency.
Note. Y-axis represents % initiating mild delinquency at the mean of the covariates (single parent status, parental education, and age at follow-up).
Figure 1c. Severe Delinquency Pattern.
Note. Y-axis represents % initiating severe delinquency at the mean of the covariates (single parent status, parental education, and age at follow-up).
Table 2.
Group Differences in the Initiation of Mild, Moderate, and Severe Delinquency
| Age of Initiationa | Rate | b | SE | Wald | Sig. | OR | |
|---|---|---|---|---|---|---|---|
| Mild Acts | |||||||
| Comparison | 12.46 | 67.9% | -- | -- | -- | -- | -- |
| ADHD-only | 11.42 | 59.6% | −.03 | .22 | .01 | .91 | .98 |
| ADHD+ODD | 10.96 | 67.4% | .12 | .15 | .72 | .40 | 1.13 |
| ADHD+CD | 10.36 | 70.8% | .32 | .16 | 3.97 | .05 | 1.37 |
| Moderate Acts | |||||||
| Comparison | 14.50 | 43.1% | -- | -- | -- | -- | -- |
| ADHD-only | 13.36 | 46.8% | .08 | .26 | .10 | .75 | 1.09 |
| ADHD+ODD | 13.43 | 45.9% | .12 | .18 | .48 | .49 | 1.13 |
| ADHD+CD | 11.99 | 67.9% | .94 | .17 | 29.11 | <.01 | 2.55 |
| Severe Acts | |||||||
| Comparison | 13.76 | 13.4% | -- | -- | -- | -- | -- |
| ADHD-only | 13.99 | 23.4% | .61 | .39 | 2.39 | .12 | 1.84 |
| ADHD+ODD | 14.59 | 25.2% | .70 | .28 | 6.23 | .01 | 2.01 |
| ADHD+CD | 12.87 | 45.3% | 1.42 | .27 | 27.33 | <.01 | 4.13 |
Note: Mild offenses include: property damage<$100, minor fire-setting, theft<$5, avoiding payment, cheating others. Moderate offenses include: gang fighting, property damage>$100, fire-setting with major damage, theft>$5, purse snatching, picking pocket, stealing from a car, dealing stolen goods, joyriding, check fraud, credit card fraud, counterfeiting. Severe offenses include: forcible theft, breaking and entering, vehicle theft, rape, attacking someone with the intent to seriously injure or kill, attack with a weapon.
Represents the estimated marginal mean age of initiation after controlling for demographic covariates.
Age of Initiation
For mild delinquency, the overall test of the model was significant [X2(8)=388.42, p<.01]. Results revealed that after controlling for the covariates, the ADHD-only (Estimated M=11.42, SE=.21, b=−1.04, SE=.22, Wald= 22.38, p<.01), ADHD+ODD (Estimated M=10.96, SE=.12, b=−1.50, SE=.15, Wald=105.76, p<.01), and ADHD+CD (Estimated M=10.36, SE=.14, b=−2.10, SE=.16, Wald=175.53, p<.01) groups initiated mild delinquency at significantly earlier ages than the comparison group (Estimated M=12.46, SE=.10). Additional planned comparisons revealed that after controlling for the covariates, the ADHD+CD group also initiated mild delinquency at significantly earlier ages than the ADHD+ODD and ADHD-only groups.
For moderate delinquency, the overall test of the model was significant [X2(8)=258.27, p<.01] and after controlling for the covariates, the ADHD-only (Estimated M=13.36, SE=.24, b=−1.14, SE=.26, Wald= 19.03, p<.01), ADHD+ODD (Estimated M=13.43, SE=.14, b=−1.08, SE=.18, Wald=35.37, p<.01), and ADHD+CD (Estimated M=11.99, SE=.14, b=−2.52, SE=.17, Wald=218.82, p<.01) groups initiated moderate delinquency at significantly earlier ages than comparisons (Estimated M=14.50, SE=.12). Additional planned comparisons revealed that after controlling for the covariates, the ADHD+CD group initiated moderate delinquency at significantly earlier ages than the ADHD+ODD and ADHD-only groups.
For severe delinquency, the overall test of the model was significant [X2(8)=88.99, p<.01] and the analysis revealed that after controlling for the covariates, the ADHD+CD group (Estimated M=12.87, SE=.18, b=−.89, SE=.27, Wald= 10.75, p<.01) initiated severe delinquency at significantly earlier ages than the comparison group (Estimated M=13.76, SE=.22). The ADHD+ODD (Estimated M=14.59, SE=.19, b=.83, SE=.29, Wald=8.13, p<.01) group initiated severe delinquency at significantly later ages than the comparison group. The ADHD-only group (Estimated M=13.99, SE=.34, b=−.23, SE=.40, Wald=.33, p=.57) was not significantly different from the comparison group on age of severe delinquency initiation. Additional planned comparisons revealed that after controlling for the covariates, the ADHD+CD group initiated severe delinquency at significantly earlier ages than the ADHD+ODD and ADHD-only groups.
Variety
The overall model was significant [X2(5)=644.32, p<.01] and the analysis revealed that after controlling for the covariates, the ADHD-only (Estimated M=6.19, SE=.16, b=.82, SE=.17, Wald= 22.33, p<.01), ADHD+ODD (Estimated M=6.72, SE=.10, b=1.35, SE=.12, Wald=129.58, p<.01), and ADHD+CD (Estimated M=8.69, SE=.12, b=3.32, SE=.13, Wald=630.30, p<.01) groups committed a significantly higher variety of delinquent acts than the comparison group (Estimated M=5.37, SE=.08). In addition, all planned comparisons were significant indicating that the three proband groups also significantly differed from each other.
Discussion
The findings of this study suggest that regardless of comorbidity, all children with ADHD are at some type of increased risk for delinquency. Specific findings were that: (a) compared to the other three childhood diagnostic subgroups (no diagnosis, ADHD-only, ADHD+ODD), children with ADHD+CD were at a higher risk for all but one index of delinquency examined in this study (prevalence of mild delinquency); b) children with ADHD-only and ADHD+ODD displayed a slightly elevated prevalence of severe offending, were at risk for earlier initiation of mild and moderate delinquency, and committed a greater variety of acts than the comparison group; and (c) the risks exhibited by the ADHD-only and ADHD+ODD groups were very similar, only differing on variety of offending. We shall discuss each of these findings in turn.
The clearest finding that emerged from this study was that children diagnosed with ADHD+CD were at the highest risk for delinquent offending across measures of severity, variety, and age of initiation. This finding is consistent with most if not all studies that examine the relationship between childhood ADHD, childhood conduct problems, and adolescent delinquency (Loeber et al., 1990; 2000). The pervasiveness of this finding highlights the grave trajectory shared by these individuals. Most of these boys (≈70%) initiated mild and moderate delinquency, doing so early (mild Estimated M=10.36, moderate Estimated M=11.99). A subset of the boys with ADHD+CD (45.3%) also initiated severe delinquency, again doing so at earlier ages than offenders in the other groups (Estimated M=12.87). These boys also committed a greater variety of acts than the other subgroups. Although these results implicate childhood CD as a precursor to severe delinquent offending, at least when it co-occurrs with ADHD, only half (51.6%) of severe offenders with childhood ADHD were diagnosed with CD at baseline, despite the high rate of CD in our sample. Thus, something other than CD appears to account for the development of severe delinquency in about half of the PALS severe offenders. Of course, it is possible that some of these boys developed CD after baseline assessment (Lahey et al., 1995).
The only exception to the elevated risk displayed by ADHD+CD probands was prevalence of mild delinquency. Our data show a high prevalence of mild delinquency in all four childhood diagnostic groups, which suggests that mild offending may be normative in adolescence. In fact, a high proportion of participants in all four childhood diagnostic groups committed at least one delinquent act (Range= 70.2%–82.2%). This finding is consistent with cross-national prevalence rates that suggest that most adolescents will self-report at least one criminal act during their youth (Junger-Tas et al., 1994). Thus, group differences did not emerge on mild delinquency because of prevalent normative offending in the comparison group.
Our data also revealed that boys with childhood ADHD-only and childhood ADHD+ODD showed elevated risks for delinquent offending by age 18. Specifically, these two groups were more likely to offend earlier, commit a greater variety of crimes, and initiate severe delinquency than comparison participants (see Table 2). These findings suggest that boys with ADHD who are low on antisocial behaviors in elementary school are still at risk for later delinquent offending. This risk is concerning given that early offending and varied offending are both associated with non-normative offending trajectories (Mazerolle et al., 2000; Moffitt, 2003). This claim is also consistent with other studies showing that adolescents with ADHD begin offending earlier than those without this disorder (Forehand, Wierson, Frame, Kempton, & Armistead, 1991; Moffitt, 1990). With respect to severe delinquency, boys with ADHD-only (23.4%, OR=1.84) and with ADHD+ODD (25.4%, OR=2.01) were at a similar risk (see Figure 1c); however, this risk was non-significant in the ADHD-only group (p=.12). Despite this non-significance– perhaps because the sample size was about 1/3 of that for the ADHD+ODD group - both groups were about twice as likely as comparison participants to engage in severe delinquency, such as forcible theft, breaking and entering, vehicle theft, rape, or murder.
Only delinquency variety displayed the stepwise risk that we predicted would occur in correspondence with childhood diagnostic severity. This finding was consistent with the only other study of ADHD and delinquency variety (Loeber et al., 1990), which reported that variety scores in youth with ADHD+CD were higher than those possessed by youth with ADHD-only, which in turn were higher than the comparison group. Studies of delinquency volume draw a similar conclusion. These findings suggest that ADHD is related to overall volume of crime, but not any particular type of crime, with high rates of offending across a wide variety of crimes (Barkley et al., 2007; Dalteg & Levander, 1998; Torgersen et al., 2006). It is not surprising that the variety variable displayed our hypothesized incremental risk, as delinquency variety is an index that is conceptualized by some to reflect low self-control (Hirschi & Gottfredson, 1993), which is also a hallmark feature of ADHD (Barkley, 2006). Indeed, one characteristic of the PALS sample was that baseline ADHD severity increased with the severity of one's childhood diagnosis (see Table 1), which may account for some of the relative increased delinquency variety.
While it came as no surprise that boys with ADHD+CD offended at the highest rates, the similar pattern of offending displayed by boys with ADHD-only and ADHD+ODD was somewhat unexpected (see Table 2 & Figure 1a–c). A full understanding of this finding requires careful consideration of the composition of these groups. Although as discussed above, the ADHD+ODD group showed somewhat elevated levels of baseline ADHD symptomatology, compared to the ADHD-only group, they differed vastly on ODD symptomatology (see Table 1). Furthermore, the ADHD+ODD and ADHD+CD shared very similar levels of baseline ODD symptoms, but displayed disparate risks for later offending (see Tables 1 & 2 & Figures 1b–c). Consequently, these data seem to suggest that elevations in ODD symptomatology do not increase the risk for most of the delinquency indices examined in this study. Although theory heavily implicates coercive family processes and subsequent ODD in the development of conduct problems and later delinquency (Moffitt, 1990; Patterson et al., 2000; Snyder, Cramer, Afrank, & Patterson, 2005), our data suggest that oppositional behavior may carry a limited risk for non-normative delinquency if this disorder does not evolve into symptoms of CD. However, given the finding that about two-thirds of children with ADHD+ODD develop CD (Greene, 2005), it may be particularly effective to intervene with boys with ADHD+ODD in order to prevent the especially severe offending trajectory demonstrated by boys with ADHD+CD.
Figure 1b. Moderate Delinquency Pattern.
Note. Y-axis represents % initiating moderate delinquency at the mean of the covariates (single parent status, parental education, and age at follow-up).
These trends suggest that while individuals without ADHD are mostly at risk for committing delinquent acts of mild to moderate severity during adolescence, individuals with childhood ADHD are at an earlier and unremitting risk for offending at all delinquency severity levels and across a wider variety of crimes (see Table 2). Unfortunately, earlier and more severe offending would seem to suggest that children with ADHD, and especially with comorbid CD, are also at risk for offending that persists into adulthood (Moffitt, 1993; 2003). Our data also indicate that clinically significant levels of childhood conduct problems propel the risk for earlier, more severe, and more varied delinquency. However, given the incremental gains in ADHD symptomatology as one moves to a more severe childhood diagnosis (see Table 1; Waschbusch, 2002), it is also possible that some of the risk accrued by comorbidity may be attributable to more severe ADHD symptoms. Unfortunately, without childhood measures on the comparison group, we were unable to fully investigate the contribution of childhood symptom severity to the development of later delinquency. This is an important limitation to our study.
There are other limitations as well. As a clinic-referred sample, the outcomes found in the PALS may not generalize to epidemiological samples of children with ADHD. Thus, there is a need to replicate these results using a community sample. Another limitation to our study is that our baseline data represents a diagnostic snapshot of each proband in childhood. Therefore, it is also possible that some of the probands without a baseline diagnosis of comorbid CD (age range: 5–12 years; M = 8.92, SD= 1.79) might have developed CD between baseline and follow-up. It is also possible that some participants who met criteria for ODD or CD during baseline may have experienced a remission of these symptoms after the baseline assessment. In addition, eligible participants who did not enroll in the study possessed slightly higher baseline CD severity scores than enrollees. It is possible that had these eligible participants enrolled, delinquency estimates in the proband groups could have been different. For probands with a comorbid diagnosis of CD, delinquent acts committed prior to initial assessment may have actually been the cause of a CD diagnosis. Although we attempted to reduce this possibility by excluding participants who were over age 12 at baseline, we were regrettably unable to completely remove these acts from our analyses due to the nature of the SRD questionnaire (Elliot et al., 1985). It is also the case that some of the delinquency history collected from our sample was based on retrospective report. We attempted to safeguard against the complications associated with retrospective report of delinquency (Kazemian & Farrington, 2005) by asking participants and parents to report lifetime delinquency three times and using age at follow-up as a covariate. However, it is possible that we were unable to identify all acts ever committed by the participants. Given that our delinquency measure did not assess for the number of times each act was committed, we were also unable to examine differential patterns in delinquency volume.
Given the small number of boys in our sample who qualified for diagnosis of ADHD-Predominantly Inattentive Subtype, we were also unable to examine whether offending patterns differed amongst the subtypes of ADHD. In addition, while our sample was demographically representative of the county in which the study occurred, it is important to note that many of our participants came from middle-class families. As a result, our findings may be most generalizable to middle-class, racial-majority males with parents who are high school graduates. For example, evidence suggests that females display different normative and non-normative patterns of offending than males (Silverthorn & Frick, 1999).
Future Directions
An important future line of research is the investigation of symptom clusters and child characteristics that give rise to non-normative delinquency. For example, Callous-Unemotional (CU) traits show evidence of a unique pathway to severe offending (Frick, 2004); however, no study has examined the role of these traits in predicting delinquency outcomes in a childhood ADHD sample. Future research must also address influences, such as parenting, that occur between childhood and adolescence and likely influence whether or not a child with ADHD initiates or maintains an antisocial pathway. Additionally, future work should address the adulthood persistence of criminal offending within the ADHD population, thereby extending the patterns examined in the current study and addressing whether the early-onset offending found in the ADHD group represents life-course persistent criminality.
Clinical Implications
For children with ADHD, an elevated risk for non-normative delinquency is just one of a slew of probable negative life outcomes, including school drop-out, interpersonal difficulties, substance use, and unemployment (Barkley et al., 2007; Mannuzza, Gittelman-Klein, Bessler, Malloy & LaPadula, 1993; Molina et al., 2007b; Weiss & Hechtman, 1993). These outcomes highlight the intense need for treatment in individuals diagnosed with ADHD. All PALS probands participated in an 8-week intensive Summer Treatment Program and their parents received a standard course of behavioral parent training (Pelham & Hoza, 1996). They also received an average of 6 years of pharmacological intervention. However, the findings of this study and others from this same sample (Molina et al., 2007b; Kent et al., under review) suggest that these interventions were not sufficient to prevent the negative outcomes that are common for children with ADHD. This is especially true for children with comorbid CD. Our findings suggest that in individuals with ADHD, there is a need for chronic treatment that begins early in childhood and persists into adolescence (Eyberg, Nelson, & Boggs, 2008; Pelham & Fabiano, 2008). For many children with ADHD, antisocial behavior begins in childhood but peaks in adolescence. However, treatment for adolescents with ADHD (Smith, Waschbusch, Willoughby, & Evans, 2000) is not well-researched and scarcely offered in most communities. Further work is sorely needed to develop prevention and intervention efforts in childhood and effective interventions for adolescents with ADHD.
Acknowledgments
This study was supported by grants DA12414, DA05605, F31 DA017546 from the National Institute on Drug Abuse and additionally, AA11873 from the National Institute of Alcohol Abuse and Alcoholism. Research was also supported in part by AA00202, AA08746, AA12342, AA0626, and grants from the National Institute on Mental Health (MH12010, MH4815, MH47390, MH45576, MH50467, MH53554, MH069614), the National Institute of Environmental Health Sciences (ES0515-08), and Institute of Education Sciences (IESLO3000665A, IESR324B060045).
References
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed-TR Author; Washington, DC: 2000. [Google Scholar]
- Babinski LM, Hartsough CS, Lambert NM. Childhood conduct problems, hyperactivity-impulsivity, and inattention as predictors of adult criminal activity. Journal of Child Psychology and Psychiatry. 1999;40:347–355. [PubMed] [Google Scholar]
- Barkley RA. Attention-Deficit Hyperactivity Disorder: A handbook for diagnosis and treatment. 3rd ed Guilford; New York: 2006. [Google Scholar]
- Biederman J, Mick E, Faraone SV, Burback M. Patterns of remission and symptom decline in conduct disorder: A four-year prospective study of an ADHD sample. Journal of the American Academy of Child & Adolescent Psychiatry. 2001;40:290–298. doi: 10.1097/00004583-200103000-00008. [DOI] [PubMed] [Google Scholar]
- Burke JD, Loeber R, Lahey BB, Rathouz PJ. Developmental transitions among affective and behavioral disorders in adolescent boys. Journal of Child Psychology and Psychiatry. 2005;46:1200–1210. doi: 10.1111/j.1469-7610.2005.00422.x. [DOI] [PubMed] [Google Scholar]
- Burke J, Loeber R, Mutchka J, Lahey B. A question for DSM-V: Which better predicts persistent conduct disorder--delinquent acts or conduct symptoms? Criminal Behaviour and Mental Health. 2002;12:37–52. doi: 10.1002/cbm.485. [DOI] [PubMed] [Google Scholar]
- Carroll A, Hemingway F, Bower J, Ashman A, Houghton S, Durkin K. Impulsivity in juvenile delinquency: Differences among early-onset, late-onset, and non-offenders. Journal of Youth and Adolescence. 2006;35(4):519–529. [Google Scholar]
- Cohen MA. The monetary value of saving high-risk youth. Journal of Quantitative Criminology. 1998;14:5–33. [Google Scholar]
- Dalteg A, Levander S. Twelve-thousand crimes by 75 boys: A 20-year follow up study of childhood hyperactivity. Journal of Forensic Psychiatry. 1998;9:39–57. [Google Scholar]
- Elliot DZ, Huizinga D, Ageton SS. Explaining delinquency and drug use. Sage; Beverley Hills, CA: 1985. [Google Scholar]
- Eyberg S, Nelson M, Boggs S. Evidence-based psychosocial treatments for children and adolescents with disruptive behavior. Journal of Clinical Child and Adolescent Psychology. 2008;37:215–237. doi: 10.1080/15374410701820117. [DOI] [PubMed] [Google Scholar]
- Farrington DP, Loeber R, Van Kammen WB. Long-term criminal outcomes of hyperactivity-impulsivity-attention deficit and conduct problems in childhood. In: Robins LN, Rutter M, editors. Straight and Deviant Pathways from Childhood to Adulthood. Cambridge University Press; New York: 1990. [Google Scholar]
- Forehand RL, Wierson M, Frame C, Kempton T, Armistead Juvenile delinquency entry and persistence: Do attention problems contribute to conduct problems? Journal of Behavior Therapy and Experimental Psychiatry. 1991;22:261–264. doi: 10.1016/0005-7916(91)90042-4. [DOI] [PubMed] [Google Scholar]
- Frick P. Developmental pathways to conduct disorder: Implications for serving youth who show severe aggressive and antisocial behavior. Psychology in the Schools. 2004;41:823–834. [Google Scholar]
- Gittelman R, Mannuzza S, Shenker R, Bonagura N. Hyperactive boys almost grown up: I. Psychiatric Status. Archives of General Psychiatry. 1985;42(10):937–947. doi: 10.1001/archpsyc.1985.01790330017002. [DOI] [PubMed] [Google Scholar]
- Greene RW. Oppositional Defiant Disorder. In: Hersen M, Thomas JC, editors. Comprehensive Handbook of Personality and Psychopathology. 3rd ed. John Wiley & Sons; New York: 2005. [Google Scholar]
- Hirschi T, Gottfredson M. Commentary: Testing the general theory of crime. Journal of Research in Crime and Delinquency. 1993;30:47–54. [Google Scholar]
- Junger-Tas J, Terlouw GJ, Klein MW, editors. Delinquent behavior among young people in the western world. Kugler; New York: 1994. [Google Scholar]
- Kagan J, Zentner M. Early childhood predictors of adult psychopathology. Harvard Review of Psychiatry. 1996;3(6):341–350. doi: 10.3109/10673229609017202. [DOI] [PubMed] [Google Scholar]
- Kazemian L, Farrington DP. Comparing the validity of prospective, retrospective, and official onset for different offending categories. Journal of Quantitative Criminology. 2005;21:127–147. [Google Scholar]
- Kent KM, Pelham WE, Molina BSG, Waschbusch DA, Yu J, Sibley MH, et al. The academic experience of male high school students with ADHD. doi: 10.1007/s10802-010-9472-4. under review. Paper submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klinteberg B. Hyperactive behaviour and aggressiveness as early risk indicators for violence: Variable and person approaches. Studies on Crime & Crime Prevention. 1997;6:21–34. [Google Scholar]
- Lahey BB, Loeber R. Framework for a developmental model of oppositional defiant disorder and conduct disorder. In: Routh DK, editor. Disruptive Behavior Disorders in Childhood. Plenum Press; New York: 1994. [Google Scholar]
- Lahey B, Loeber R, Hart E, Frick P, Applegate B, Zhang Q, et al. Four-year longitudinal study of conduct disorder in boys: Patterns and predictors of persistence. Journal of Abnormal Psychology. 1995;104:83–93. doi: 10.1037/0021-843X.104.1.83. [DOI] [PubMed] [Google Scholar]
- Lee SS, Hinshaw SP. Severity of adolescent delinquency among boys with and without attention deficit hyperactivity disorder: Prediction from early antisocial behavior and peer status. Journal of Clinical Child and Adolescent Psychology. 2004;33:705–716. doi: 10.1207/s15374424jccp3304_6. [DOI] [PubMed] [Google Scholar]
- Lilienfeld S, Waldman I. The relation between childhood attention-deficit hyperactivity disorder and adult antisocial behavior reexamined: The problem of heterogeneity. Clinical Psychology Review. 1990;10:699–725. [Google Scholar]
- Loeber R. The stability of antisocial and delinquent child behavior: A review. Child Development. 1982;53:1431–1446. [PubMed] [Google Scholar]
- Loeber R. Natural histories of conduct problems, delinquency, and associated substance use: Evidence for developmental progressions. In: Lahey BB, Kazdin AE, editors. Advances in clinical child psychology. Vol. 11. Plenum Press; New York: 1988. pp. 73–123. [Google Scholar]
- Loeber R, Brinthaupt VP, Green SM. Behavior disorders of adolescence: Research, intervention, and policy in clinical and school settings. Plenum Press; New York, NY US: 1990. Attention deficits, impulsivity, and hyperactivity with or without conduct problems: Relationships to delinquency and unique contextual factors; pp. 39–61. [Google Scholar]
- Loeber R, Burke JD, Lahey BB, Winters A, Zera M. Oppositional defiant and conduct disorder: A review of the past ten years, Part I. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:1468–1484. doi: 10.1097/00004583-200012000-00007. [DOI] [PubMed] [Google Scholar]
- Loeber R, Pardini DA, Stouthamer-Loeber M, Raine A. Do cognitive, physiological, and psychosocial risk and promotive factors predict desistance from delinquency in males? Development and Psychopathology. 2007;19(3):867–887. doi: 10.1017/S0954579407000429. [DOI] [PubMed] [Google Scholar]
- Loeber R, Stouthamer-Loeber M, Van Kammen WB, Farrington DP. Initiation, escalation and desistance in juvenile offending and their correlates. Journal of Criminal Law and Criminology. 1991;82:36–82. [Google Scholar]
- Loeber R, Stouthamer-Loeber M, White HR. Developmental aspects of delinquency and internalizing problems and their association with persistent juvenile substance use between ages 7 and 18. Journal of Clinical Child Psychology. 1999;28:322–332. doi: 10.1207/S15374424jccp280304. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Gittelman-Klein R, Bessler A, Malloy P, LaPadula M. Adult outcome of hyperactive boys: educational achievement, occupational rank, and psychiatric status. Archives of General Psychiatry. 1993;50:565–576. doi: 10.1001/archpsyc.1993.01820190067007. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Abikoff H, Moulton JL., III Significance of childhood conduct problems to later development of conduct disorder in among children with ADHD: A prospective follow-up study. Journal of Abnormal Child Psychology. 2004;32:565–573. doi: 10.1023/b:jacp.0000037784.80885.1a. [DOI] [PubMed] [Google Scholar]
- Mazerolle P, Brame R, Paternoster R, Piquero A, Dean C. Onset, age, persistence, and offending versatility: Comparisons across gender. Criminology. 2000;38:1143–1172. [Google Scholar]
- McCullagh P, Nelder JA. Generalized Linear Models. Chapman and Hall; London: 1989. [Google Scholar]
- McMahon RJ, Kotler JS. Conduct problems. In: Wolfe DA, Mash EJ, editors. Behavioral and Emotional Disorders in Adolescents: Nature, Assessment, and Treatment. Guilford; New York: 2006. [Google Scholar]
- Moffitt TE. Juvenile delinquency and Attention Deficit Disorder: Boys' developmental trajectories from age 3 to age 15. Child Development. 1990;61:893–910. doi: 10.1111/j.1467-8624.1990.tb02830.x. [DOI] [PubMed] [Google Scholar]
- Moffitt TE. Adolescent-limited and life-course-persistent antisocial behavior: A developmental taxonomy. Psychological Review. 1993;100:674–701. [PubMed] [Google Scholar]
- Moffitt TE. Life-course-persistent and adolesence-limited antisocial behavior: A 10-year research review and a research agenda. In: Lahey BB, Moffitt TE, Caspi A, editors. Causes of conduct disorder and juvenile delinquency. Guilford Press; New York: 2003. pp. 49–75. [Google Scholar]
- Moffitt T, Caspi A. Childhood predictors differentiate life-course persistent and adolescence-limited antisocial pathways among males and females. Development and Psychopathology. 2001;13:355–375. doi: 10.1017/s0954579401002097. [DOI] [PubMed] [Google Scholar]
- Moffitt T, Caspi A, Harrington H, Milne BJ. Males on the life-course-persistent and adolescence-limited antisocial pathways: Follow-up at age 26 years. Development and Psychopathology. 2002;14:179–207. doi: 10.1017/s0954579402001104. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Flory K, Hinshaw SP, Greiner AR, Arnold LE, Swanson JM, et al. Delinquent behavior and emerging substance use in the MTA at 36 months: Prevalence, course, and treatment effects. Journal of the American Academy of Child and Adolescent Psychiatry. 2007a;46:1028–1040. doi: 10.1097/chi.0b013e3180686d96. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Pelham WE, Gnagy EM, Thompson AL, Marshal MP. Attention-deficit/hyperactivity disorder risk for heavy drinking and alcohol use disorder is age specific. Alcoholism: Clinical and Experimental Research. 2007b;31:643–654. doi: 10.1111/j.1530-0277.2007.00349.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pardini D, Obradovic J, Loeber R. Interpersonal callousness, hyperactivity/impulsivity, inattention, and conduct problems as precursors to delinquency persistence in boys: A comparison of three grade-based cohorts. Journal of Clinical Child and Adolescent Psychology. 2006;35:46–59. doi: 10.1207/s15374424jccp3501_5. [DOI] [PubMed] [Google Scholar]
- Patterson GR, DeGarmo DS, Knutson N. Hyperactive and antisocial behaviors: Comorbid or two points in the same process? Development and Psychopathology. 2000;12:91–106. doi: 10.1017/s0954579400001061. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Evans SW, Gnagy EM, Greenslade KE. Teacher ratings of DSM-III--R symptoms for the disruptive behavior disorders: Prevalence, factor analyses, and conditional probabilities in a special education sample. School Psychology Review. 1992;21:285–299. [Google Scholar]
- Pelham W, Fabiano G. Evidence-based psychosocial treatments for attention-deficit/hyperactivity disorder. Journal of Clinical Child and Adolescent Psychology. 2008;37:184–214. doi: 10.1080/15374410701818681. [DOI] [PubMed] [Google Scholar]
- Pelham WE, Hoza B. Intensive treatment: A summer treatment program for children with ADHD. In: Hibbs ED, Jensen PS, editors. Psychosocial Treatments for Child and Adolescent Disorders: Empirically Based Strategies for Clinical Practice. American Psychological Association Press; New York: 1996. [Google Scholar]
- Satterfield JH, Hoppe CM, Schell AM. A prospective study of delinquency in 110 adolescent boys with attention deficit disorder and 88 normal adolescent boys. American Journal of Psychiatry. 1982;139:795–798. doi: 10.1176/ajp.139.6.795. [DOI] [PubMed] [Google Scholar]
- Satterfield J, Swanson J, Schell A, Lee F. Prediction of antisocial behavior in attention-deficit hyperactivity disorder boys from aggression/defiant scores. Journal of the American Academy of Child & Adolescent Psychiatry. 1994;33:185–190. doi: 10.1097/00004583-199402000-00005. [DOI] [PubMed] [Google Scholar]
- Silverthorn P, Frick PJ. Developmental pathways to antisocial behavior: The delayed-onset pathway in girls. Development and Psychopathology. 11:101–126. doi: 10.1017/s0954579499001972. [DOI] [PubMed] [Google Scholar]
- Smith B, Waschbusch D, Willoughby M, Evans S. The efficacy, safety and practicality of treatments for adolescents with attention-deficit/hyperactivity disorder (ADHD) Clinical Child and Family Psychology Review. 2000;3:243–267. doi: 10.1023/a:1026477121224. [DOI] [PubMed] [Google Scholar]
- Snyder J, Cramer A, Afrank J, Patterson GR. The contribution of ineffective discipline and parental hostile attributions of child misbehavior to the development of conduct problems at home and school. Developmental Psychology. 2005;41:30–41. doi: 10.1037/0012-1649.41.1.30. [DOI] [PubMed] [Google Scholar]
- Stouthamer-Loeber M, Loeber R. Lost opportunities for intervention: Undetected markers for the development of serious juvenile delinquency. Criminal Behaviour and Mental Health. 2002;12:69–82. doi: 10.1002/cbm.487. [DOI] [PubMed] [Google Scholar]
- Torgersen T, Gjervan B, Rasmussen K. ADHD in adults: A study of clinical characteristics, impairment, and comorbidity. Nordic Journal of Psychiatry. 2006;60:38–43. doi: 10.1080/08039480500520665. [DOI] [PubMed] [Google Scholar]
- United States Department of Justice, Federal Bureau of Investigation Crime in the United States. 20072006 [Google Scholar]
- Waschbusch DA. A meta-analytic examination of comorbid hyperactive-impulsive-attention problems and conduct problems. Psychological Bulletin. 2002;128(1):118–150. doi: 10.1037/0033-2909.128.1.118. [DOI] [PubMed] [Google Scholar]
- Weiss G, Hechtman L. Hyperactive Children Grown Up. 2nd edition Guilford; New York: 1993. [Google Scholar]
- White JL, Moffitt TE, Caspi A, Bartusch DJ, Needles DJ, Stouthamer-Loeber M. Measuring impulsivity and examining its relationship to delinquency. Journal of Abnormal Psychology. 1994;103(2):192–205. doi: 10.1037//0021-843x.103.2.192. [DOI] [PubMed] [Google Scholar]
- Wolfgang M, Figlio RM, Tracey PE, Singer FI. The National Survey of Crime Severity. Washington, DC: U.S.: 1985. [Google Scholar]