Abstract
Study Design
Cross-sectional study with prospective recruitment.
Objective
To determine the accuracy of the physical examination for the diagnosis of midlumbar nerve root impingement (L2, L3, or L4), low lumbar nerve root impingement (L5 or S1) and level-specific lumbar nerve root impingement on magnetic resonance imaging (MRI), using individual tests and combinations of tests.
Summary of Background Data
The sensitivity and specificity of the physical examination for the localization of nerve root impingement has not been previously studied.
Methods
Sensitivities, specificities and LRs were calculated for the ability of individual tests and test combinations to predict the presence or absence of nerve root impingement at midlumbar, low lumbar, and specific nerve root levels.
Results
LRs ≥5.0 indicate moderate to large changes from pre-test probability of nerve root impingement to post-test probability. For the diagnosis of midlumbar impingement, the femoral stretch test (FST), crossed femoral stretch test (CFST), medial ankle pinprick sensation, and patellar reflex testing demonstrated LRs ≥5.0 (LR ∞). LRs ≥5.0 were seen with the combinations of FST and either patellar reflex testing (LR 7.0; 95% CI 2.3–21), or the sit-to-stand test (LR ∞). For the diagnosis of low lumbar impingement, the Achilles reflex test demonstrated a LR ≥5.0 (LR 7.1; CI 0.96–53); test combinations did not increase LRs. For the diagnosis of level-specific impingement, LRs ≥5.0 were seen for anterior thigh sensation at L2 (LR 13; 95% CI 1.8–87); FST at L3 (LR 5.7 ; 95% CI 2.3–4.4); patellar reflex testing (LR 7.7; 95% CI 1.7–35), medial ankle sensation (LR ∞), or CFST (LR 13; 95% CI 1.8–87) at L4; and hip abductor strength at L5(LR 11; 95% CI 1.3–84). Test combinations increased LRs for level-specific root impingement at the L4 level only.
Conclusions
Individual physical examination tests may provide clinical information which substantially alters the likelihood that midlumbar impingement, low lumbar impingement, or level-specific impingement is present. Test combinations improve diagnostic accuracy for midlumbar impingement.
INTRODUCTION
Midlumbar nerve root impingement, or nerve root impingement at the L2, L3, or L4 levels, is a cause of lumbosacral radicular syndrome found with increasing frequency in older adults1, 2. Although early studies estimated the prevalence of midlumbar nerve root impingement at 5–11%,2, 3 results from recent studies of lumbar disk herniation suggest that the prevalence of midlumbar nerve root impingement may be substantially higher.4–6 As our population ages, midlumbar nerve root impingement may be seen with increasing frequency in specialty spine clinics7.
Although the classic presentation of radicular pain in midlumbar nerve root impingement is in the groin or anterior thigh, pain may also commonly be experienced in the calf, ankle, or foot8. The diagnosis of midlumbar nerve root impingement may therefore be quite challenging, with a clinical presentation resembling lower lumbar nerve root impingement, hip osteoarthritis, and other causes of referred pain9. The physical examination may be helpful in clinical decision-making by altering the post-test probability that nerve root impingement localized to a region or a specific level is responsible for the production of symptoms. Establishing a clear picture of clinical deficits prior to obtaining advanced imaging is necessary in order to avoid a situation where the physical examination becomes biased by prior knowledge of an abnormality on imaging, especially in light of the well-documented prevalence of asymptomatic disk herniations using lumbar spine MRI10, and the common clinical occurrence of multiple imaging abnormalities in a single patient.
Although prior studies have examined the performance characteristics of the physical examination in patients with radicular pain, there are deficits in the existing literature. First, prior studies have examined the physical examination in reference to lumbar disk herniation, but not in reference to lumbar nerve root impingement. This fact is noteworthy, considering that decompression of nerve impingement (and not diskectomy alone) is the primary goal of decompression surgery. Second, the basis of the most commonly utilized physical examination tests in the evaluation of lumbosacral radicular pain, including the straight leg raise test (SLR), rests on the assumption that nerve root pathology affects the low lumbar nerve roots (L5 or S1)11. The performance characteristics of most common physical examination tests in the setting of midlumbar nerve root impingement, where the L5 or S1 nerve roots are not affected, is unclear. Third, although data exist on the accuracy of the physical examination for detecting lumbar disk herniation without regard to herniation level, there are no accuracy studies on the performance of the physical examination tests for the neuroanatomic localization of nerve root impingement. The conceptual localization of nerve root impingement by the examining physician prior to reviewing MRI results is vital to ensure that imaging is correlated with the clinical picture, rather than vice versa.
We sought to characterize the accuracy of physical examination testing over the range of lumbar nerve root impingement, and to elucidate how the physical examination may aid in neuroanatomic localization of pathology. In this prospective study of patients with lumbosacral radicular pain, we examined the performance characteristics of single physical examination tests in relation to three different reference standards using lumbar spine magnetic resonance imaging (MRI): 1) midlumbar nerve root impingement (L2, L3, or L4), 2) low lumbar nerve root impingement (L5 or S1), and 3) level-specific nerve root impingement at the L2-S1 levels. We also examined the performance characteristics of test combinations, in order to optimize diagnostic performance, and to simulate how the physical examination is commonly employed in clinical practice.
METHODS
Study Participants
This work was an ancillary study to a prospective study of the outcomes of lumbar disk herniation. The study was approved by the hospital’s institutional review board. Participants were recruited from a hospital spine center between January 2008 and March 2009. All consecutive patients aged 18 and older with lower extremity radiating pain for less than 12 weeks were eligible for participation. Inclusion criteria were a history of radicular pain in a L2, L3, L4, L5, or S1 dermatome, with or without neurological symptoms. Exclusion criteria were known pregnancy and severe active medical or psychiatric comorbidities that would limit study participation. The presence of symptomatic hip arthritis, prior total hip arthroplasty, hip flexion contractures, and other hip disorders were not criteria for exclusion. Patients with lumbar spine MRI available to the examining physician at the time of the physical examination were ineligible for this ancillary study, in order to ensure blinding to the reference standard and eliminate potential bias from knowledge of nerve root compression prior to performing the physical examination.
Information on participant demographics and clinical characteristics was collected prospectively, including participant age, gender, and symptom duration. Comorbidity burden was measured by the Self-Acquired Comorbidity Questionnaire (SACQ), which is a commonly used, valid, and reliable measure12. Disability was measured by the Oswestry Disability Index (ODI). The ODI is a condition-specific measure of disability which has been used extensively in prior studies of radiculopathy, and has demonstrated validity and reliability in these contexts13. Pain was measured by the visual analogue scale (VAS) for leg pain and back pain14
Physical Examination
Each participant was examined by one of six board-certified physiatrists specializing in spine care. The physical examination included a standard battery of tests, administered by the physiatrist in a consistent and stereotyped manner. All physical examination tests were performed bilaterally. Testing results were documented by the examiner in reference to the symptomatic limb; for example, a positive SLR was documented if reproduction of radicular pain was elicited in the symptomatic limb. In a minority of cases, where bilateral symptoms existed, the results of testing were documented in reference to the limb that was most symptomatic. The examining physician recorded all information at the time of the examination using a standardized data sheet.
1. Provocative Manuevers
Straight leg raise/Crossed straight leg raise - The straight leg raise (SLR) and crossed straight leg raise (CSLR) have been well described previously15. Reproduction of the patient's typical lower extremity pain constitutes a positive result for both the SLR and the CSLR.
Femoral stretch test/Crossed femoral stretch test)- The femoral stretch test (FST) is performed with the patient lying prone. The examiner grasps the patient's ankle on the symptomatic (ipsilateral) side and facilitates gentle ipsilateral knee flexion; reproduction of typical lower extremity pain constitutes a positive test. The crossed femoral stretch test (CFST) is performed similarly, except that contralateral knee flexion instead reproduces typical (ipsilateral) lower extremity pain.
2. Motor testing
For assessment of knee extensor strength, ankle dorsiflexor strength, and ankle plantarflexor strength, the examiner performs a maximally challenging and ‘functional’ test of strength to identify subtle deficits. If the participant is able to complete the functional test, they receive a grade of normal strength (5), and no further strength testing is performed for that muscle group. If an impairment is detected with the functional test, normal strength is not present, and the degree of weakness is quantified (0–4) using manual muscle testing16.
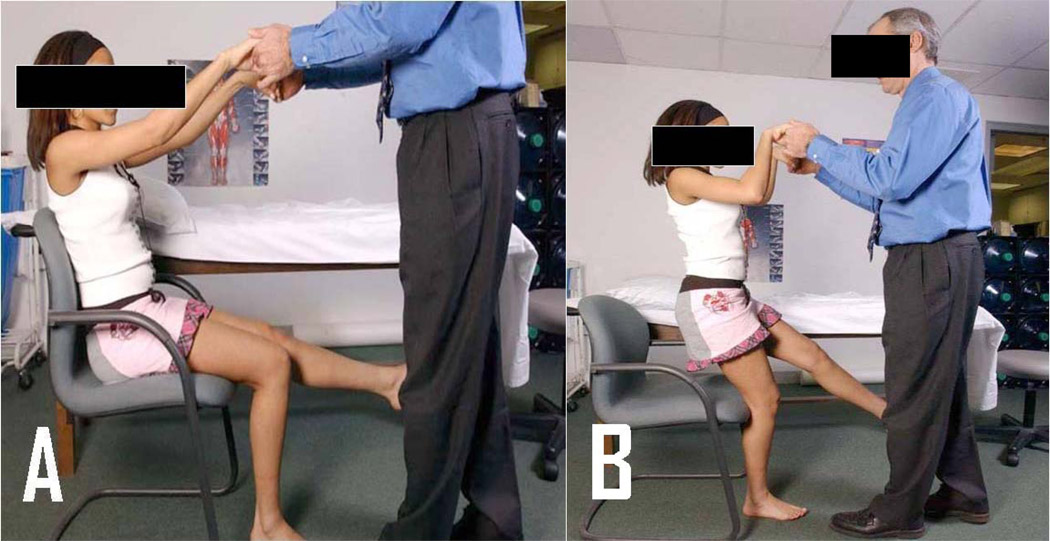
Knee extensor strength- The single leg sit-to-stand test is performed as the primary assessment of knee extensor strength8. The performance of this test is demonstrated in figure 1. The test is performed first on the unaffected leg, and second on the affected leg.
Ankle dorsiflexor strength- The heel walk test is performed as the primary assessment of ankle dorsiflexion strength. The patient walks on heels only while avoiding contacting the floor with the forefeet, using the examiner’s hands for balance as needed; inability to maintain the forefoot off the ground is a positive result.
Ankle plantarflexor strength- The single leg heel raise test is performed as the primary assessment of ankle plantarflexion strength. The patient stands on one foot while flexing the contralateral knee, while holding the examiner’s hands or a countertop for balance. The patient plantarflexes the ankle, raising the heel of the supporting limb off the floor to maximal plantarflexion. Inability to perform 10 successive heel raises is a positive result.
Great toe extensor strength- The patient fully dorsiflexes the great toe and maintains this position as the examiner applies a plantarflexion force.
Hip abductor strength- The patient is positioned in side-lying with the asymptomatic limb against the table surface and the symptomatic thigh abducted to 30 degrees from horizontal. The patient maintains the abducted position as the examiner applies an adduction force.
Figure 1. The single leg sit-to-stand test.
A) Starting position- The seated patient fully extends one knee and avoids contacting the floor with that foot during testing. The examiner holds the patient’s hands as a balance aid only.
B) Finishing position- The patient rises to the standing position using only the strength of the supporting limb. Inability to transfer to standing constitutes a positive test.
3) Sensory testing
Sensory impairments are assessed by pinprick testing at the mid-anterior thigh, the medial aspect of the knee, the medial aspect of the ankle, the dorsal aspect of the great toe, and the lateral border of the foot. Sensation is graded on a standard three grade scale (0–2), with ‘2’ representing normal sensation, ‘1’ representing impairment, and ‘0’ representing absent sensation17.
4) Reflex testing
Deep tendon reflexes are assessed at the patellar tendon and Achilles tendon, using a standard 5 point grading scale18.
Magnetic Resonance Imaging Studies
MR imaging was performed for the majority of participants within 7 days of their physical examination. MRI imaging scans consisted at minimum of T1 and T2 weighted images of the lumbar spine in the sagittal and axial planes. Each MRI scan was evaluated by one of eight board-certified neuroradiologists, who were blinded to study design and research questions. The classification of the most severe level of nerve root impingement according to the neuroradiologist final impression was used as the reference standard for this study. Inter-rater reliability of the most severe level of nerve root impingement at the L2-S1 root levels on each MRI was excellent (к=0.92) in a subsample of 18 scans which were interpreted by an independent and blinded musculoskeletal radiologist who did not participate in the primary MRI assessments. The evaluation of nerve root impingement on MRI has previously been validated in reference to operative findings.19
Statistical Analysis
To characterize the demographics, clinical characteristics, and radiographic features of the study population, we calculated means and standard deviations for continuous variables, and frequencies and proportions for categorical variables. We calculated the frequencies of pain symptom locations by root impingement level. For analytic purposes, the results of physical examination tests with a categorical grading were dichotomized: motor strength testing was dichotomized as negative (5) vs. positive (0–4); sensory testing was dichotomized as negative (2) vs. positive (0 or 1); and reflex testing was considered positive if the reflex grade in the symptomatic limb was diminished by at least one grade as compared to the same reflex in the contralateral limb. We used the reference standard of the most severe level of nerve root impingement on lumbar spine MRI.
We began by calculating sensitivities, specificities, and likelihood ratios (LRs), including 95% confidence intervals (CIs), for all individual tests using the reference standard of MRI midlumbar nerve root impingement. This analytic approach has been recommended by recent research guidelines for studies of diagnostic accuracy.20, 21 Positive LRs were calculated as ‘sensitivity/(1-specificity)’, and negative LRs were calculated as ‘(1-sensitivity)/specificity’.21 We then repeated these calculations for all individual tests using a reference standard of MRI low lumbar nerve root impingement, and a reference standard of MRI level-specific nerve root impingement.
Next, we calculated the performance characteristics of test combinations for the diagnosis of midlumbar nerve root impingement. We combined tests in a manner designed to optimize sensitivity, by considering a test combination to be positive if any test in the combination had a positive result. In order to limit the number of possible test combinations, we included only individual tests which demonstrated LR 95% confidence intervals ≥1.0, and LR point estimates ≥2.0. We chose a LR point estimate threshold of 2.0 due to the fact that LRs ≥2.0 reflect small but sometimes important changes in post-test probability22. We expected that certain test combinations would result in more substantial LRs ≥5.0, which indicate moderate to large changes from the pre-test probability of nerve root impingement to post-test probability22. We then repeated these analyses of test combinations, using a reference standard of low lumbar nerve root impingement, and a reference standard of level-specific root impingement. All analyses were performed using SAS software, version 9.0 (SAS Institute, Cary, NC).
RESULTS
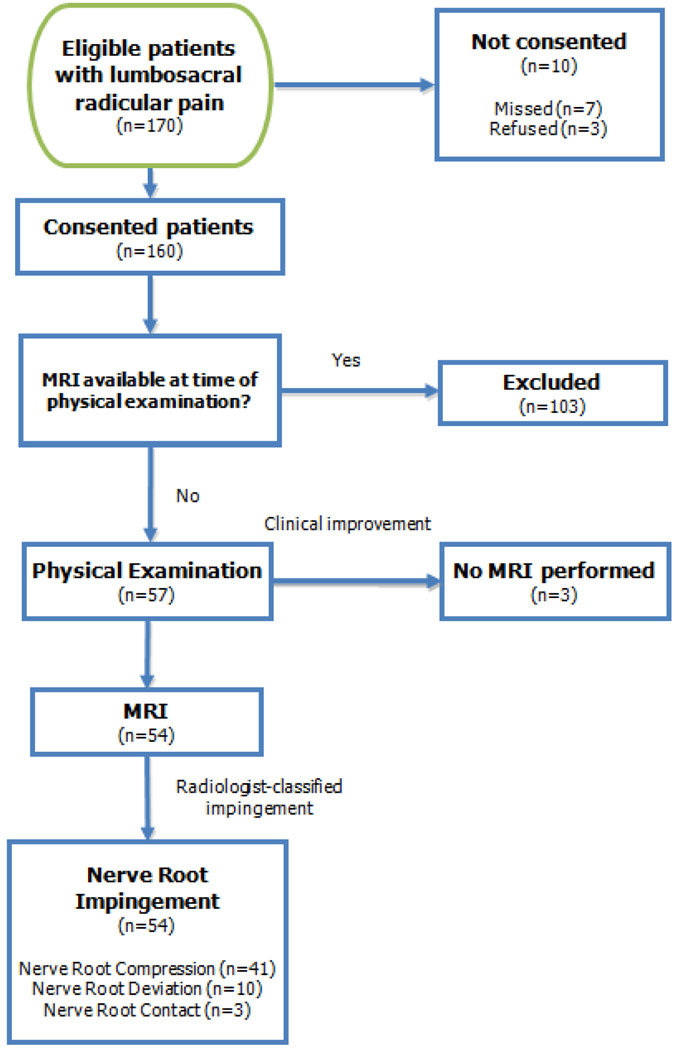
Participant recruitment for this study is depicted in Figure 2. Of 170 potential participants, 10 individuals either declined to participate or were missed by the recruiting physicians. 160 participants were consented, including 57 participants who had no imaging available, and 103 participants who had imaging available at the time of the examination. All 103 participants with imaging available to the examiner were ineligible for this study due to lack of blinding to the reference standard. Of the 57 participants who had no imaging available, three participants did not go on to receive MRI due to clinical improvement, leaving 54 participants who received MRI and neuroradiologist interpretation; these individuals reported a slightly shorter duration of symptoms (4.3 ± 2.8 vs. 5.2 ± 3.1; p=0.08), but were otherwise not materially different from the 103 individuals who had no imaging available (data not shown).
Figure 2. Flowchart of patient recruitment and participation.
Demographics and clinical characteristics of the study sample are presented in Table 1. The three participants who did not go on to receive MRI were not materially different from those who did go on to MRI (data not shown). Table 2 demonstrates the prevalence of radicular pain experienced by the patient in each anatomic region of the lower extremities, according to the specific level of nerve root impingement. Fifty-one participants had nerve root impingement primarily due to lumbar disk herniation, though concurrent mild to moderate bony stenosis at the affected level was not uncommon. One participant had a synovial cyst, and two participants had bony stenosis as the primary cause of impingement. 40 participants (74%) had nerve root compression, 11 (20%) had nerve root deviation, and 3 (6%) had nerve root contact. All three participants with nerve root contact had only single-level involvement. 15 individuals (28%) also had nerve contact at another level.
Table 1.
Characteristics of the Study Sample
| Characteristic | Midlumbar Nerve Root Impingement- L2, L3, or L4+ (n=25) |
Low Lumbar Nerve Root Impingement- L5 or S1+ (n=29) |
Nerve Root Impingement at any level+ (n=54) |
|---|---|---|---|
| Age (yrs) | 61.4 (13.8) | 48.6 (13.6) | 54.5 (15.0) |
| Female (%) | 9 (36.0%) | 4 (13.8%) | 13 (24.1%) |
| Symptom duration (wks) | 3.9 (2.5) | 4.6 (3.0) | 4.3 (2.8) |
| Oswestry Disability index (0–100) | 42 (21) | 49 (21) | 46 (21) |
| VAS Leg Pain (0–10) | 7.2 (2.2) | 7.0 (2.7) | 7.1 (2.5) |
| VAS Back Pain (0–10) | 4.8 (3.2) | 5.4 (3.4) | 5.1 (3.3) |
| Self-Acquired Comorbidity Questionnaire (0–45) |
4.6 (4.0) | 1.4 (2.3) | 2.8 (3.5) |
Mean (S.D.) or N (%)
Table 2.
Distribution of Radicular Pain Symptoms According to Level of Nerve Root Impingement
| Midlumbar nerve root impingement L2, L3, or L4 (n=25 ) |
Low lumbar nerve root impingement L5 or S1 (n=29) |
||||
|---|---|---|---|---|---|
| L2 (n=2 ) | L3 (n= 10) | L4 (n=13 ) | L5 (n=18 ) | S1 (n=11 ) | |
| Groin | 1 (50.0%) | 2 (20.0%) | 0 (0%) | 1 (5.6%) | - |
| Thigh | |||||
| Anterior | 2 (100%) | 10 (100%) | 5 (38.5%) | - | - |
| Lateral | - | 1 (10.0%) | 8 (61.5%) | 8 (44.4%) | 2 (18.2%) |
| Posterior | - | - | - | 11 (61.1%) | 8 (72.7%) |
| Knee | |||||
| Anterior | - | 5 (50.0%) | 3 (23.1%) | 1 (5.6%) | - |
| Posterior | - | - | - | 2 (11.1%) | 1(9.1%) |
| Calf | |||||
| Medial | - | - | 1 (7.7%) | - | - |
| Anterior | - | 3 (30.0%) | 7 (53.9%) | 1 (5.6%) | - |
| Lateral | - | - | 3 (23.1%) | 13 (72.2%) | 2 (18.2%) |
| Posterior | - | - | - | 8 (44.4%) | 7 (63.6%) |
| Foot/ankle | |||||
| Medial | - | - | 1 (7.7%) | 1 (5.6%) | - |
| Dorsum | - | - | - | 1 (5.6%) | 1 (9.1%) |
| Lateral | - | - | - | 2 (11.1%) | 1 (9.1%) |
| Heel | - | - | - | 1 (5.6%) | 3 (27.3%) |
The distributions of patient-reported radicular pain symptoms are presented in Table 2. Anterior vs. posterior location of thigh pain symptoms showed notable differences by location of impingement. For example, all patients who reported anterior thigh pain had midlumbar nerve root impingement, while all patients who reported posterior thigh pain had low lumbar nerve root impingement. Anterior vs. posterior location of calf pain symptoms also showed notable differences by location of impingement. For example, all but one patient with anterior calf pain had midlumbar nerve root impingement, while all patients with posterior calf pain had low lumbar nerve root impingement. All but one patient with pain in the foot or ankle had low lumbar nerve root impingement.
The performance characteristics of individual physical examination tests for the diagnosis of midlumbar nerve root impingement and low lumbar nerve root impingement are presented in Table 3. Positive results on four physical examination tests had both LR point estimates ≥5.0 and 95% confidence intervals ≥1.0 for the diagnosis of midlumbar nerve root impingement on MRI: the FST (∞), CFST (∞), medial ankle pinprick sensation (∞), and patellar reflex testing (∞). An impaired Achilles reflex was the only test with a LR point estimate ≥5.0 and 95% confidence intervals ≥1.0 for the diagnosis of low lumbar nerve root impingement on MRI. Although the crossed SLR test demonstrated higher specificity as compared to the SLR (96% vs 84%, respectively) the FST demonstrated such high specificity (100%) that the crossed FST could provide no additional gain in specificity. Furthermore, the CFST was positive in only one participant, and therefore the interpretation of performance characteristics for this test should be viewed in this context.
Table 3.
Performance Characteristics of Physical Examination Tests for the Diagnosis of Midlumbar Nerve Root Impingement and Low Lumbar Nerve Root Impingement on MRI*
| Midlumbar Nerve Root Impingement (L2, L3, L4) |
Low Lumbar Nerve Root Impingement (L5, S1) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Physical Examination Test |
Sens. (95% CI) |
Spec. (95% CI) |
LR+ (95% CI) |
LR− (95% CI) |
Sens. (95% CI) |
Spec. (95% CI) |
LR+ (95% CI) |
LR− (95% CI) |
| Provocative testing | ||||||||
| Straight Leg Raise (SLR) |
16 (6–35) |
31 (17–49) |
0.23 (0.09–0.59) |
2.7 (1.5–4.8) |
69 (51–83) |
84 (65–94) |
4.3 (1.7–11) |
0.37 (0.21–0.65) |
| Crossed Straight Leg Raise (CSLR) |
4 (1–20) |
93 (78–98) |
0.58 (0.06–6.0) |
1.0 (0.91–1.1) |
7 (2–22) |
96 (81–99) |
1.7 (0.17–18) |
0.97 (0.85–1.1) |
| Femoral Stretch Test (FST) |
50 (31–69) |
100 (88–100) |
NA (∞) |
0.50 (0.34–0.75) |
0 | 50 (31–69) |
0 |
2.0 (1.3–3.0) |
| Crossed Femoral Stretch Test (CFST) |
5 (1–22) |
100 (87–100) |
NA (∞) | 0.96 (0.87–1.1) |
0 | 96 (78–99) |
0 |
1.1 (1.0–1.2) |
| Motor testing | ||||||||
| Sit-to-stand test | 48 (30–67) |
90 (74–96) |
4.6 (1.5–15) |
0.58 (0.39–0.86) |
10 (4–26) |
52 (34–70) |
0.22 (0.07–0.68) |
1.7 (1.2–2.6) |
| Heel raise test | 4 (1–20) |
86 (69–95) |
0.29 (0.04–2.4) |
1.1 (0.94–1.3) |
14 (6–31) |
96 (81–99) |
3.5 (0.41–29) |
0.90 (0.76–1.1) |
| Heel walk test | 20 (9–39) |
86 (69–95) |
1.1 (0.33–3.7) |
0.98 (0.80–1.2) |
14 (6–31) |
80 (61–91) |
0.69 (0.21–2.3) |
1.1 (0.84–1.4) |
| Great toe extensors |
20 (9–39) |
62 (44–77) |
0.53 (0.21–1.3) |
1.3 (0.91–1.8) |
38 (23–56) |
80 (61–91) |
1.9 (0.76–4.7) |
0.78 (0.55–1.1) |
| Hip abductors | 4 (1–20) |
82 (64–92) |
0.22 (0.03–1.8) |
1.2 (0.97–1.4) |
18 (8–36) |
96 (81–99) |
4.5 (0.56–36) |
0.86 (0.71–1.0) |
| Sensory testing | ||||||||
| Anterior thigh | 8 (2–26) |
96 (82–99) |
2.3 (0.23–24) |
0.95 (0.83–1.1) |
4 (1–18) |
92 (74–98) |
0.43 (0.04–4.4) |
1.1 (0.91–1.2) |
| Medial knee | 17 (7–36) |
96 (82–99) |
4.7 (0.56–39) |
0.86 (0.71–1.1) |
4 (1–19) |
83 (64–93) |
0.21 (0.03–1.8) |
1.2 (1.0–1.4) |
| Medial ankle | 17 (7–36) |
100 (88–100) |
NA (∞) |
0.83 (0.70–1.0) |
0 | 83 (64–93) |
0 |
1.2 (1.0–1.4) |
| Great toe | 13 (5–32) |
82 (64–92) |
0.73 (0.20–2.7) |
1.1 (0.84–1.3) |
18 (8–36) |
87 (68–96) |
1.4 (0.37–5.1) |
0.94 (0.75–1.2) |
| Lateral foot | 8 (2–26) |
79 (61–90) |
0.39 (0.06–1.8) |
1.2 (0.93–1.5) |
21 (10–40) |
92 (74–98) |
2.6 (0.57–12) |
0.86 (0.68–1.1) |
| Reflex testing | ||||||||
| Patella | 28 (14–48) |
100 (88–100) |
NA (∞) |
0.72 (0.56–0.92) |
0 | 72 (52–86) |
0 |
1.4 (1.1–1.8) |
| Ankle | 4 (1–20) |
71 (53–85) |
0.14 (0.02–1.0) |
1.3 (1.1–1.7) |
29 (15–47) |
96 (81–99) |
7.1 (0.96–53) |
0.74 (0.58–0.95) |
Physical examination tests with positive likelihood ratio 95% confidence intervals ≥ 1.0 or ≤1.0 in bold
Sens. – Sensitivity (%)
Spec. – Specificity (%)
LR+ – Positive likelihood ratio
LR− – Negative likelihood ratio
CI – Confidence interval
The performance characteristics of selected physical examination tests for the diagnosis of level-specific nerve root impingement are presented in Table 4. Only physical examination tests with LR 95% confidence intervals ≥1.0 for the diagnosis of level-specific nerve root impingement are presented, due to space limitations. Six tests had positive LRs ≥5.0 for level-specific impingement: anterior thigh sensation for L2 impingement (12.5), the FST for L3 impingement (5.7), patellar reflex testing for L4 impingement (7.7), medial ankle sensation for L4 impingement (∞), crossed femoral stretch testing for L4 impingement (∞), and hip abductor strength for L5 impingement (10.6).
Table 4.
Performance Characteristics of Physical Examination Tests for Level-Specific Nerve Root Impingement on MRI*
| Physical Examination Test |
Level of Nerve Root Impingement on MRI |
Sens. (95% CI) |
Spec. (95% CI) |
Positive LR (95% CI) |
Negative LR (95% CI) |
|---|---|---|---|---|---|
| Provocative Testing | |||||
| Femoral Stretch Test (FST) |
L3 | 70 (40–89) |
88 (75–95) |
5.7 (2.3–4.4) |
0.34 (0.13–0.89) |
| Crossed Femoral Stretch Test (CFST) |
L4 | 9 (2–38) |
100 (91–100) |
NA (∞) | 0.91 (0.75–1.1) |
| Straight Leg Raise (SLR) |
L5 | 67 (44–84) |
67 (50–80) |
2.0 (1.1–3.5) |
0.50 (0.25–1.0) |
| Straight Leg Raise (SLR) |
S1 | 73 (43–90) |
63 (48–76) |
2.0 (1.2–3.3) |
0.43 (0.16–1.2) |
| Motor testing | |||||
| Sit-to-stand test | L3 | 50 (24–76) |
77 (63–87) |
2.2 (1.0–5.0) |
0.65 (0.34–1.23) |
| Sit-to-stand test | L4 | 54 (29–77) |
81 (66–90) |
2.8 (1.2–6.1) |
0.57 (0.31–1.1) |
| Great toe extensor | L5 | 61 (39–80) |
86 (71–94) |
4.4 (1.8–11) |
0.45 (0.25–0.82) |
| Hip abductor | L5 | 29 (13–53) |
97 (86–100) |
11 (1.3–84) |
0.73 (0.53–0.99) |
| Sensory testing | |||||
| Anterior thigh | L2 | 50 (10–91) |
96 (87–99) |
13 (1.8–87) |
0.52 (0.13–2.1) |
| Medial ankle | L4 | 31 (13–57) |
100 (91–100) |
NA (∞) | 0.69 (0.48–1.0) |
| Reflex testing | |||||
| Patella | L4 | 39 (18–65) |
95 (84–99) |
7.7 (1.7–35) |
0.65 (0.42–1.0) |
| Achilles | L5 | 33 (16–56) |
91 (78–97) |
3.9 (1.1–14) |
0.73 (0.52–1.0) |
Including only physical examination tests with positive likelihood ratio 95% confidence intervals ≥ 1.0 for level-specific nerve root impingement; tests with positive likelihood ration point estimates ≥ 5.0 in bold
Sens. – Sensitivity (%)
Spec. – Specificity (%)
LR+ – Positive likelihood ratio
LR− – Negative likelihood ratio
CI – Confidence interval
The performance characteristics of selected combinations of physical examination tests for the diagnosis of midlumbar nerve root impingement are presented in Table 5. Multiple test combinations demonstrated LRs ≥5.0, as well as increased sensitivity over individual tests; we have presented data for the most parsimonious combinations that either demonstrated the greatest improvements in sensitivity over individual tests while preserving high specificity (≥90%), or were more feasible to administer as screening tests in a clinical setting. The combination of the SLR and Achilles reflex testing for the diagnosis of low lumbar nerve root impingement demonstrated increased sensitivity (79%), but a decreased LR+ (4.0) as compared to the individual tests, due to decreased specificity (80%). In general, the progressive addition of more tests in combination for the diagnosis of either midlumbar or low lumbar impingement did not improve LRs+, due to the fact that increases in sensitivity were offset by decreased specificity (data not shown).
Table 5.
Selected Combinations of Physical Examination Tests for the Diagnosis of Midlumbar Nerve Root Impingement on MRI*
| Midlumbar Nerve Root Impingement (L2, L3, L4) |
||||
|---|---|---|---|---|
| Physical Examination Test Combinations |
Sens. (95% CI) |
Spec. (95% CI) |
LR+ (95% CI) |
LR− (95% CI) |
| Two test combinations | ||||
| Patellar reflex or FST | 60 (41–77) |
100 (88–100) |
NA (∞) | 0.40 (0.25–0.65)) |
| FST or Sit-to-stand test | 72 (52–86) |
90 (74–96) |
7.0 (2.3–21) |
0.31 (0.17–0.59) |
| Multiple test combinations | ||||
| Medial ankle sensation or patellar reflex or FST |
64 (45–80) |
100 (88–100) |
NA (∞) | 0.36 (0.21–0.61) |
| Medial ankle sensation or FST or sit-to-stand test |
76 (57–89) |
90 (74–96) |
7.4 (2.5–22) |
0.27 (0.13–0.54) |
| Medial ankle sensation or patellar reflex or FST or sit- to-stand test |
80 (61–91) |
90 (74–96) |
7.7 (2.6–23) |
0.22 (0.10–0.49) |
| Clinically useful combinations (able to be performed in seated position) | ||||
| Patellar reflex or sit-to-stand test |
60 (41–77) |
90 (74–96) |
5.8 (1.9–18) |
0.45 (0.27–0.73) |
| Medial ankle sensation or patellar reflex |
40 (23–59) |
100 (88–100) |
NA (∞) | 0.60 (0.44–0.83) |
| Medial ankle sensation or patellar reflex or sit-to-stand test |
68 (48–83) |
90 (74–96) |
6.6 (2.2–20) |
0.36 (0.20–0.64) |
Selected combinations with positive likelihood ratio point estimates ≥ 5.0, chosen for either improved sensitivity over individual tests while preserving high specificity, or for feasibility of administration in a clinical setting.
Sens. – Sensitivity (%)
Spec. – Specificity (%)
LR+ – Positive likelihood ratio
LR− – Negative likelihood ratio
CI – Confidence interval
FST– Femoral stretch test
The performance characteristics of selected combinations of physical examination tests for the diagnosis of level-specific nerve root impingement are presented in Table 6. Only those combinations with LR+ point estimates ≥5.0 are presented. Combining tests substantially increased LRs, increased sensitivity, and maintained high specificity for L4 nerve root impingement only.
Table 6.
Combinations of Physical Examination Tests Chosen to Optimize Performance Characteristics for the Diagnosis of Level Specific Nerve Root Impingement on MRI*
| Physical Examination Test Combinations | Sens. (95% CI) |
Spec. (95% CI) |
LR+ (95% CI) |
LR− (95% CI) |
|---|---|---|---|---|
| L4 nerve root | ||||
| Ankle sensation or patellar reflex | 62 (36–82) |
95 (84–99) |
12 (3.0–51) |
0.41 (0.20–0.81) |
| Ankle sensation or patellar reflex or CFST | 62 (36–82) |
95 (84–99) |
13 (3.1–52) |
0.40 (0.20–0.81) |
| CFST or patellar reflex | 38 (18–64) |
95 (84–99) |
7.9 (1.7–36) |
0.65 (0.42–1.0) |
| L5 nerve root | ||||
| Achilles reflex or hip abduction | 61 (39–80) |
89 (75–96) |
5.5 (2.0–15) |
0.44 (0.24–0.79) |
Combinations with positive likelihood ratio point estimates ≥ 5.0
Sens. – Sensitivity (%)
Spec. – Specificity (%)
LR+ – Positive likelihood ratio
LR− – Negative likelihood ratio
CI – Confidence interval
FST – Femoral stretch test
CFST – Crossed femoral stretch test
DISCUSSION
This study differs from prior studies of diagnostic accuracy in radicular pain in that it uses a specific reference standard of either a region of impingement (for example midlumbar impingement at the L2, L3, or L4 levels) or impingement at a specific level (for example, the L5 nerve root), and not a reference standard of nerve root impingement or disk herniation at any level. This should not affect our understanding of the estimates of sensitivity (which is based on prevalence in the cases) in this study, however it does have implications for estimates of specificity (which is based on prevalence in the non-cases). In prior studies, the question of relevance with regards to specificity has been ‘Does the finding occur in people who do not have nerve root impingement?’; in this study, the relevant question is ‘Does the finding occur in people who have nerve root impingement at a different level?’.
Our findings demonstrate that individual physical examination tests may provide valuable clinical information which substantially alter the post-test probability that midlumbar nerve root impingement is present in patients presenting with lumbosacral radicular pain. However, while many physical examination tests are highly specific for midlumbar nerve root impingement, no single test is highly sensitive. The FST (sensitivity 50%) and the single leg sit-to-stand test (sensitivity 48%) showed the highest sensitivities for the diagnosis of midlumbar nerve root impingement. Therefore, screening with individual physical examination tests may not detect many cases of midlumbar nerve root impingement. This is expected since many cases of nerve root impingement do not have detectable impaired neurological function or pain produced with nerve root tension signs. Certain combinations of physical examination tests increase sensitivity while maintaining high LRs, but other test combinations do not increase overall diagnostic accuracy, due to a trade-off of decreasing specificity with the addition of more tests.
The SLR showed moderate sensitivity (69%) for low lumbar nerve root impingement. Although the diagnostic accuracy of the SLR in our study showed decreased sensitivity as compared to some prior studies of diagnostic accuracy in surgical populations with lumbar disk herniation2, 23, it is consistent with prior findings in nonsurgical populations with lumbar disk herniation24. This systematic difference between performance characteristics from surgical and nonsurgical studies has been previously noted25. We did not find any improvement in diagnostic accuracy with the addition of other tests in combination with the SLR.
Once midlumbar or low lumbar nerve root impingement is suspected, the physical examination may help to distinguish which specific nerve root is involved. A positive result on the FST, CFST, hip abduction strength, anterior thigh sensation, medial ankle sensation, and patellar reflex testing indicates a moderate to large increase in the post-test probability of nerve root impingement at a specific level. A positive finding on one of these tests in practical terms also substantially decreases the probability that another root level is responsible for symptoms. Test combinations are only useful for the diagnosis of level-specific root impingement at the L4 level. From a clinical perspective, localization of nerve root involvement allows the physician to characterize relevant functional limitations at the baseline visit, and monitor for progression of deficits or new deficits at follow-up.
No prior study has examined the performance characteristics of the blinded physical exam in reference to midlumbar nerve root impingement. The results of this study, however, are consistent with the limited prior reports of physical examination characteristics in midlumbar disk herniation, when methodologic differences are taken into account. Although early reports using a surgical reference standard have stated a prevalence of 84–95% for a positive FST in known high lumbar disc herniation26–28, these estimates may have been affected by the well-documented overestimation of sensitivity seen due to spectrum bias25, 29. Indeed, our findings of FST sensitivity are concordant with the results of a prior study using a reference standard of impingement on MRI, which reported a prevalence of 43–60% of the FST in non-surgical patients with midlumbar radiculopathy8.
A notable exception to the trend of poor sensitivities with single tests for midlumbar nerve root impingement in our study was with the assessment of quadriceps strength using the single leg sit-to-stand test, which demonstrated a sensitivity of 48% for the diagnosis of midlumbar nerve root impingement. This is likely explained by the superiority of the sit-to-stand test over manual muscle testing. A prior study of manual muscle testing found that a 50% loss of quadriceps strength was necessary in order to be detectable by manual testing30. The single leg sit-to-stand test detects many cases of quadriceps weakness missed on manual testing8 . In addition, the sit-to-stand test has other advantages which may favor its use as a screening test for midlumbar nerve root impingement. First, the sit-to-stand test not only provides highly specific diagnostic information, but also informs as to functional limitations. Poor performance on the sit-to-stand test may be associated with alterations in stair climbing ability8, and impaired quadriceps strength is associated with poor balance and mobility31. Second, the sit-to-stand test has high reliability (к=0.85)8, which may be due to the objectiveness of the test result (ability to stand vs. inability). This means that the sit-to-stand test can be readily compared between different examiners. Furthermore, a deterioration in performance of the test is likely to represent a true change, and unlikely to represent the variability of the test itself. Finally, the sit-to-stand test can be efficiently integrated into the standard office exam, and is easily performed after completion of the history, at the point when the patient needs to come to a standing position for the examination. Other tests described above may be used in combination with the sit-to-stand test to improve diagnostic accuracy, and can also be readily performed with the patient seating. These combinations may have clinical utility as a screening tool in patients where the history- including location of radicular pain- suggests midlumbar nerve root impingement.
This study has other methodological features that distinguish it from prior studies. We used nerve root impingement on MRI as the reference standard, in contrast to many prior studies, which used a surgical reference standard. The value of using an imaging reference standard in diagnostic studies of radiculopathy has been affirmed in recent publications, including an upcoming Cochrane review29, 32. Although the use of an imaging reference standard creates the potential for bias due to false positive test results, it should be noted that prior imaging studies have found the prevalence of incidental nerve root impingement in asymptomatic subjects to be considerably lower than the prevalence of incidental disk herniation33, 34. Furthermore, there are known disadvantages to the use of a surgical reference standard. A surgical reference standard is most affected by spectrum bias, in which patients studied have more severe manifestations of disease.25 Verification bias, in which the reference standard is preferentially ordered as a result of the diagnostic test result, is likely to be more pronounced in studies using operative findings as the reference standard25, 34. Finally, the accuracy and consistency of operative findings is unknown. It is unclear whether intraoperative observations reflect true pathological states of the nerve root, or whether varying degrees of exposure of the operative field in different surgical techniques affect the validity of observations made during the procedure25.
The use of nerve root impingement as the anatomic reference of interest in this study, as opposed to lumbar disk herniation, is also worthy of further discussion. Although the majority of prior studies have utilized a disk herniation reference standard, a reference standard of nerve root impingement has greater validity from a conceptual standpoint. Given that the most sensitive and specific physical examination tests for the evaluation of radicular pain are conceptually based on the detection of neural tension (ie, SLR) or nerve root dysfunction (sensorimotor deficits)- and are only indirectly related to the disk herniation itself- the appropriateness of a disk herniation reference standard is questionable29.
We chose to highlight likelihood ratios as a measure of diagnostic accuracy in this study. The reporting of likelihood ratios has long been advocated by experts and is a central recommendation in established guidelines for diagnostic studies21. The penetrance of LRs in the spine literature has been less than in other areas of clinical research. LRs are able to summarize in a single number how the initial assessment of the likelihood of disease (‘pre-test probability’) is changed by a test result (‘post-test probability)35. Positive LRs describe how the likelihood of disease is changed by a positive test result, and negative LRs describe how the likelihood of disease is changed by a negative test result. LRs have the advantage over predictive values in that they are independent of disease prevalence, and can be used to quickly calculate a discrete probability of disease that is contingent on the physician’s pre-test suspicion of disease for any given patient20.
This study has limitations. First, this study was performed in a referral center for spine disorders. As such, our patient population has a higher prevalence of nerve root impingement, as well as a different spectrum of severity, than in primary care settings. Furthermore, while the neuroanatomic localization is a matter of great importance to the spine specialist, it may be beyond the scope of a standard diagnostic workup in a busy primary care practice Our findings are likely not generalizable to the primary care setting. Second, only patients with lower extremity radiating pain were considered for entry into this study. Given that a history of lower extremity pain is itself sensitive for the diagnosis of sciatica36, the sensitivities and specificities determined in this study should be viewed in this context. However, it could be argued that these physical examination tests for the localization of nerve root impingement should only be performed in situations where there is some a priori suspicion of impingement, such as may be suggested by a history of sciatica. Therefore, our use of lower extremity pain as criterion for inclusion is consistent with clinical practice in specialty spine clinics. A final limitation of this study is that the relatively small sample size studied resulted in wide confidence intervals for some estimates of accuracy; future studies may wish to include larger sample sizes.
In conclusion, this study demonstrates that the physical examination may yield useful diagnostic information for the detection of midlumbar nerve root impingement, low lumbar nerve root impingement, or level-specific nerve root impingement on MRI. As our population ages and the cost of care rises, the development and refinement of diagnostic tools which can be applied cheaply and broadly is of great importance.37 Optimizing the accuracy of the physical examination is a goal worthy of further study, in order to improve the array of cost-effective diagnostic tools available in specialty spine care.
Acknowledgments
Funding sources:
Dr. Suri is funded by the Rehabilitation Medicine Scientist Training Program (RMSTP) and the National Institutes of Health (K12 HD 01097). Dr. Katz is funded in part by NIH/NIAMS K24 AR 02123.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Blower PW. Neurologic patterns in unilateral sciatica. A prospective study of 100 new cases. Spine. 1981;6:175–179. doi: 10.1097/00007632-198103000-00013. [DOI] [PubMed] [Google Scholar]
- 2.Spangfort EV. The lumbar disc herniation. A computer-aided analysis of 2,504 operations. Acta Orthop Scand Suppl. 1972;142:1–95. doi: 10.3109/ort.1972.43.suppl-142.01. [DOI] [PubMed] [Google Scholar]
- 3.Hsu K, Zucherman J, Shea W, et al. High lumbar disc degeneration. Incidence and etiology. Spine. 1990;15:679–682. doi: 10.1097/00007632-199007000-00012. [DOI] [PubMed] [Google Scholar]
- 4.Pearson AM, Blood EA, Frymoyer JW, et al. SPORT lumbar intervertebral disk herniation and back pain: does treatment, location, or morphology matter? Spine. 2008;33:428–435. doi: 10.1097/BRS.0b013e31816469de. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT) observational cohort. Jama. 2006;296:2451–2459. doi: 10.1001/jama.296.20.2451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weinstein JN, Tosteson TD, Lurie JD, et al. Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. Jama. 2006;296:2441–2450. doi: 10.1001/jama.296.20.2441. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bressler HB, Keyes WJ, Rochon PA, Badley E. The prevalence of low back pain in the elderly. A systematic review of the literature. Spine. 1999;24:1813–1819. doi: 10.1097/00007632-199909010-00011. [DOI] [PubMed] [Google Scholar]
- 8.Rainville J, Jouve C, Finno M, Limke J. Comparison of four tests of quadriceps strength in L3 or L4 radiculopathies. Spine. 2003;28:2466–2471. doi: 10.1097/01.BRS.0000090832.38227.98. [DOI] [PubMed] [Google Scholar]
- 9.Nadler SF, Campagnolo DI, Tomaio AC, Stitik TP. High lumbar disc: diagnostic and treatment dilemma. Am J Phys Med Rehabil. 1998;77:538–544. doi: 10.1097/00002060-199811000-00018. [DOI] [PubMed] [Google Scholar]
- 10.Battie MC, Videman T, Parent E. Lumbar disc degeneration: epidemiology and genetic influences. Spine. 2004;29:2679–2690. doi: 10.1097/01.brs.0000146457.83240.eb. [DOI] [PubMed] [Google Scholar]
- 11.Goddard MD, Reid JD. Movements Induced by Straight Leg Raising in the Lumbo-Sacral Roots, Nerves and Plexus, and in the Intrapelvic Section of the Sciatic Nerve. J Neurol Neurosurg Psychiatry. 1965;28:12–18. doi: 10.1136/jnnp.28.1.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Katz JN, Chang LC, Sangha O, Fossel AH, Bates DW. Can comorbidity be measured by questionnaire rather than medical record review? Medical care. 1996;34:73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25:2940–2952. doi: 10.1097/00007632-200011150-00017. discussion 52. [DOI] [PubMed] [Google Scholar]
- 14.Collins SL, Moore RA, McQuay HJ. The visual analogue pain intensity scale: what is moderate pain in millimetres? Pain. 1997;72:95–97. doi: 10.1016/s0304-3959(97)00005-5. [DOI] [PubMed] [Google Scholar]
- 15.Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? Jama. 1992;268:760–765. [PubMed] [Google Scholar]
- 16.O'Brien MD, editor. Aids to the Examination of the Peripheral Nervous System. 4 ed. London: WB Saunders for The Guarantors of Brain; 2000. Brain. Introduction; pp. 1–2. [Google Scholar]
- 17. [Accessed 4/4/2009];Standard Neurological Classification of Spinal Cord Injury. 2006 (at http://www.asia-spinalinjury.org/publications/2006_Classif_worksheet.pdf.)
- 18.Manschot S, van Passel L, Buskens E, Algra A, van Gijn J. Mayo and NINDS scales for assessment of tendon reflexes: between observer agreement and implications for communication. J Neurol Neurosurg Psychiatry. 1998;64:253–255. doi: 10.1136/jnnp.64.2.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pfirrmann CW, Dora C, Schmid MR, Zanetti M, Hodler J, Boos N. MR image-based grading of lumbar nerve root compromise due to disk herniation: reliability study with surgical correlation. Radiology. 2004;230:583–588. doi: 10.1148/radiol.2302021289. [DOI] [PubMed] [Google Scholar]
- 20.Deeks JJ, Altman DG. Diagnostic tests 4: likelihood ratios. BMJ (Clinical research ed. 2004;329:168–169. doi: 10.1136/bmj.329.7458.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Simel DL, Rennie D, Bossuyt PM. The STARD statement for reporting diagnostic accuracy studies: application to the history and physical examination. J Gen Intern Med. 2008;23:768–774. doi: 10.1007/s11606-008-0583-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pinksy LE, Wipf JE, Ramsey SD. Evidence-Based Medicine Glossary. In: Geyman JP, Deyo RA, Ramsey SD, editors. Evidence-Based Clinical Practice: Concepts and Approaches. Boston, MA: Butterworth-Heinemann; 2000. pp. 165–172. [Google Scholar]
- 23.Uden A, Landin LA. Pain drawing and myelography in sciatic pain. Clinical orthopaedics and related research. 1987:124–130. [PubMed] [Google Scholar]
- 24.Haldeman S, Shouka M, Robboy S. Computed tomography, electrodiagnostic and clinical findings in chronic workers' compensation patients with back and leg pain. Spine. 1988;13:345–350. doi: 10.1097/00007632-198803000-00021. [DOI] [PubMed] [Google Scholar]
- 25.Vroomen PC, de Krom MC, Knottnerus JA. Diagnostic value of history and physical examination in patients suspected of sciatica due to disc herniation: a systematic review. J Neurol. 1999;246:899–906. doi: 10.1007/s004150050480. [DOI] [PubMed] [Google Scholar]
- 26.Abdullah AF, Wolber PG, Warfield JR, Gunadi IK. Surgical management of extreme lateral lumbar disc herniations: review of 138 cases. Neurosurgery. 1988;22:648–653. doi: 10.1227/00006123-198804000-00005. [DOI] [PubMed] [Google Scholar]
- 27.Christodoulides AN. Ipsilateral sciatica on femoral nerve stretch test is pathognomonic of an L4/5 disc protrusion. J Bone Joint Surg Br. 1989;71:88–89. doi: 10.1302/0301-620X.71B1.2915013. [DOI] [PubMed] [Google Scholar]
- 28.Porchet F, Fankhauser H, de Tribolet N. Extreme lateral lumbar disc herniation: clinical presentation in 178 patients. Acta Neurochir (Wien) 1994;127:203–209. doi: 10.1007/BF01808767. [DOI] [PubMed] [Google Scholar]
- 29.Vroomen PC, de Krom MC, Wilmink JT, Kester AD, Knottnerus JA. Diagnostic value of history and physical examination in patients suspected of lumbosacral nerve root compression. J Neurol Neurosurg Psychiatry. 2002;72:630–634. doi: 10.1136/jnnp.72.5.630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Beasley WC. Quantitative muscle testing: principles and applications to research and clinical services. Arch Phys Med Rehabil. 1961;42:398–425. [PubMed] [Google Scholar]
- 31.Visser M, Goodpaster BH, Kritchevsky SB, et al. Muscle mass, muscle strength, and muscle fat infiltration as predictors of incident mobility limitations in well-functioning older persons. J Gerontol A Biol Sci Med Sci. 2005;60:324–333. doi: 10.1093/gerona/60.3.324. [DOI] [PubMed] [Google Scholar]
- 32.van den Windt DAWM, Simons E, Riphagen I, et al. Physical examination for lumbar radiculopathy due to disc herniation in patients with low-back pain (Protocol) The Cochrane Collaboration. 2009 doi: 10.1002/14651858.CD007431.pub2. [DOI] [PubMed] [Google Scholar]
- 33.Boden SD, Davis DO, Dina TS, Patronas NJ, Wiesel SW. Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation. The Journal of bone and joint surgery. 1990;72:403–408. [PubMed] [Google Scholar]
- 34.Weishaupt D, Zanetti M, Hodler J, Boos N. MR imaging of the lumbar spine: prevalence of intervertebral disk extrusion and sequestration, nerve root compression, end plate abnormalities, and osteoarthritis of the facet joints in asymptomatic volunteers. Radiology. 1998;209:661–666. doi: 10.1148/radiology.209.3.9844656. [DOI] [PubMed] [Google Scholar]
- 35.Dawson B, Trapp RG. Basic & Clinical Biostatistics. 4 ed. New York: Lange Medical Books/McGraw-Hill; 2004. Methods of Evidence-Based Medicine and Decision Analysis; p. 326. [Google Scholar]
- 36.Kerr RS, Cadoux-Hudson TA, Adams CB. The value of accurate clinical assessment in the surgical management of the lumbar disc protrusion. J Neurol Neurosurg Psychiatry. 1988;51:169–173. doi: 10.1136/jnnp.51.2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weiner DK, Kim YS, Bonino P, Wang T. Low back pain in older adults: are we utilizing healthcare resources wisely? Pain Med. 2006;7:143–150. doi: 10.1111/j.1526-4637.2006.00112.x. [DOI] [PubMed] [Google Scholar]