Abstract
Acute and chronic hypoxia exists within the 3D microenvironment of solid tumors and drives therapy resistance, genetic instability and metastasis. Replicating cells exposed to either severe acute hypoxia (16 h with 0.02% O2) followed by reoxygenation or moderate chronic hypoxia (72 h with 0.2% O2) treatments have decreased homologous recombination (HR) protein expression and function. As HR defects are synthetically lethal with poly(ADP-ribose) polymerase 1 (PARP1) inhibition, we evaluated the sensitivity of repair-defective hypoxic cells to PARP inhibition. Although PARP inhibition itself did not affect HR expression or function, we observed increased clonogenic killing in HR-deficient hypoxic cells following chemical inhibition of PARP1. This effect was partially reversible by RAD51 over-expression. PARP1−/− MEFs showed a proliferative disadvantage under hypoxic gassing when compared to PARP1+/+ MEFs. PARP-inhibited hypoxic cells accumulated γH2AX and 53BP1 foci as a consequence of altered DNA replication firing during S phase-specific cell killing. In support of this proposed mode of action, PARP inhibitor treated xenografts displayed increased γH2AX and cleaved caspase-3 expression in RAD51-deficient hypoxic subregions in vivo which was associated with decreased ex vivo clonogenic survival following experimental radiotherapy. This is the first report of selective cell killing of HR-defective hypoxic cells in vivo as a consequence of microenvironment-mediated “contextual synthetic lethality”. As all solid tumors contain aggressive hypoxic cells, this may broaden the clinical utility of PARP and DNA repair inhibition either alone, or in combination with radiotherapy and chemotherapy, even in tumor cells lacking synthetically lethal, genetic mutations.
Keywords: hypoxia, poly(ADP-ribose) polymerase (PARP), homologous recombination, synthetic lethality
Introduction
Solid tumors contain subregions of dynamic O2 gradients which can be described as acute and chronic hypoxia. Severe acute hypoxia (and subsequent reoxygenation) results from temporary changes in blood perfusion. Chronic hypoxia arises in regions distant from the blood vasculature as a function of decreased oxygen diffusion and leads to gradients of moderate to severe hypoxia.
Intratumoral hypoxia is an adverse clinical prognostic factor associated with decreased disease-free survival for many solid cancers (1-5). Hypoxia can increase resistance to both radiotherapy and chemotherapy (6). Additionally hypoxia can increase metastatic spread and decrease DNA repair (7-9).
Severe hypoxia can lead to an S phase arrest in the absence of DNA damage; while subsequent re-oxygenation increases reactive oxygen species (ROS) production and DNA damage to trigger a CHK2-dependent G2 arrest (10-14). Alternatively, tumor cells can adapt to moderate chronic hypoxia with minimal changes in proliferation, cell cycle distribution or clonogenic survival suggesting a bypass of cell cycle checkpoints (15, 16). In both types of hypoxia, the homologous recombination (HR) pathway involved in the repair of DNA double strand breaks (DSBs) is compromised (15-17). Recent studies have shown that HR defects (e.g. BRCA1/2-deficient) are synthetically lethal with inhibition of the DNA single-strand break (SSB) repair protein, poly(ADP-ribose) polymerase 1 (PARP1) (18-20). In response to DNA breaks, PARP1 catalyzes the addition of poly(ADP-ribose) (PAR) polymers from NAD+ onto nuclear acceptor proteins including histones, p53 and PARP1 itself, in order to attract repair proteins and change chromatin conformation (21). Inhibition of PARP1 results in the accumulation of SSBs, which are converted to DSBs when encountered by a replication fork. These collapsed replication forks require HR for repair and continued DNA replication (22). As BRCA1/2-deficient cells are HR-deficient and incapable of repairing DNA replication-associated DSBs, treatment of these tumors with PARP inhibitors leads to synthetic lethality (18).
At present, the use of PARP inhibitors in the clinic is limited to trials in patients with genetic defects in BRCA1/2 (23). Given the existence of HR-defective hypoxic cells, we hypothesized that these cells might also be sensitized to PARP inhibition. To investigate this hypothesis, we studied both acutely- and chronically-hypoxic tumor cell cultures and hypoxic subregions of tumor xenografts and show that repair-defective hypoxic cells are sensitized to PARP inhibition; a consequence of “contextual synthetic lethality”. As all solid tumors contain hypoxic cells, our observations may increase the clinical utility of PARP (or other) inhibitors in combination with radiotherapy or chemotherapy to target treatment-resistant hypoxic tumor cells.
Materials and Methods
Cell culture, Hypoxia treatments and PARP inhibitors
The origin and culture of HCT116, 22RV1, DU145, MCF-7, PC3 and H1299 cell lines has been reported previously (13, 15, 16). Immortalized murine embryonic fibroblasts (MEFs) wild-type or deficient for PARP1 or HIF-1α were derived from day 13.5 embryos; derivation, culture and characteristics as previously described (24, 25).
Logarithmically-growing cells were exposed to 0.2% O2 with 5% CO2 and balanced N2 using an Invivo2 400 Hypoxic Workstation (Ruskinn). To achieve lower oxygen levels, cells were plated on glass dishes and incubated in a Bactron II anaerobic chamber (Shell labs) at an <0.02% O2.
ABT-888 was obtained from Abbott Laboratories through the National Institutes of Health Cancer Therapy Evaluation Program (CTEP) and reconstituted in water. 4-amino-1,8-naphthalimide (ANI) was purchased from Acros Organics and reconstituted in dimethyl sulfoxide (DMSO). ABT-888 and ANI were used at concentrations of 2.5 μM and 10 μM respectively unless otherwise stated. Enzymatic PARP activity was assessed using the Universal Chemiluminescent PARP assay kit (Trevigen) as previously described (26).
Synchronized cell populations were generated by the G2 mitotic shake off technique and confirmed with flow cytometry. Clonogenic assays were performed to determine cell viability as previously described (15).
Western blotting, siRNA treatments and microscopy
Western blot analysis was performed as previously described (13, 15). Primary antibodies included: ACTIN (Sigma-Aldrich, Inc.); PAR and PARP1 (Trevigen); HIF-1α (BD Transduction Laboratories) and RAD51 (Santa Cruz). RAD51 siRNA were obtained from Invitrogen and used at a concentration of 0.25 nM for 24 h with Lipofectamine 2000 (Invitrogen). Immunofluorescent microscopy was carried out as previously described (13, 26). The primary antibodies included: RAD51 (Santa Cruz); γH2AX (Epitomics); PAR (Trevigen); and 53BP1 (Novus Biologicals).
DR-GFP HR assay
The DR-GFP assay was used to evaluate HR as previously described (15). Briefly, H1299 cells containing the DR-GFP construct were transfected with a vector encoding for the I-SceI endonuclease to generate a DSB. Flow cytometry was used to detect GFP positive cells that have undergone HR.
Human xenograft assays
A 200 μl solution containing 2×106 HCT116, 22RV1 or RKO cells were injected subcutaneously into the hind flank of CD1 nude mice (Charles River). Tumors were grown to a volume of 250 mm3 and tumor-bearing mice were given an intraperitoneal injection with 30 mg/kg EF5 (Varian) 3 h prior to sacrifice. Tumors were excised and fixed in 10% formalin, paraffin imbedded and sectioned to 4 micron thickness. For ABT-888 treatments, RKO xenografts were treated twice daily with 50 mg/kg ABT-888 or vehicle for 5 days. Tumors were excised 2 h after the final ABT-888 treatment and prepared for immunohistochemical staining for γH2AX (Epitomics); RAD51 (Santa Cruz); and Cleaved Caspase-3 (Cell Signaling) as previously described (17).
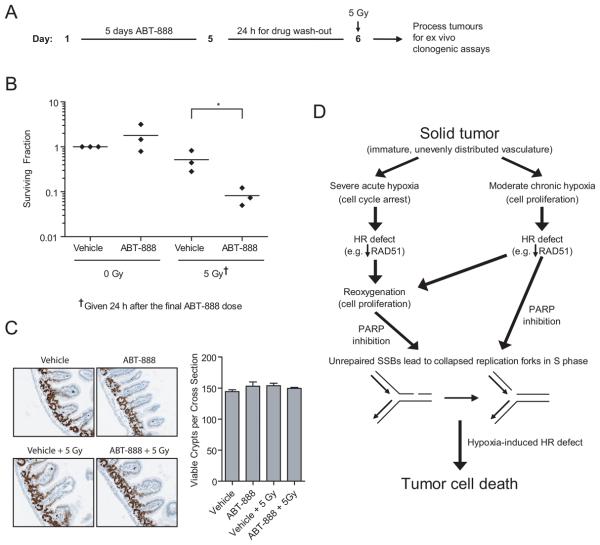
Normal gut epithelium toxicity assay
Normal tissue toxicity was determined by measuring intestinal clonogenic survival in vivo. Tumor-bearing mice were treated with 5 days ABT-888 or vehicle as described above. Where indicated, whole-body irradiation with 5 Gy (Gammacell 40 Extractor) was administered 24 h after the final ABT-888 dose. Three days after the radiation, the small intestines were removed, washed, and fixed in formalin. Gut cross-sections were stained with Ki-67 (brown) and hematoxylin (blue, nuclear counterstain). Analysis based on 5 cross sections per mouse for 3 mice per treatment group.
DNA Fiber assay
DNA fiber spreads were obtained as previously described (27) with the following modifications. Aerobic samples were sequentially labeled with 25 μM CIdU and 250 μM IdU (30 min pulses). For hypoxic samples CldU containing media was added to cells immediately prior to hypoxic treatment and incubated for 5 h after which media was replaced with hypoxic equilibrated IdU containing media for 1 h. Reoxygenation samples were treated with CldU the same as the hypoxic samples and incubated for 6 h prior to reoxygenation at which point the media was replaced with aerobic IdU containing media and further incubated for 1 h. Fiber spreads were imaged using a Biorad Radiance confocal microscope and analyzed using ImageJ software (National Institutes of Health). At least 100 replication tracks were measured and 200 replication structures counted per experiment.
Statistics
Results are presented as the mean ± SE with significance calculated by Student's t test with a standard software package (GraphPad Prism). Significance was assigned for a P value of <0.05.
Results
Hypoxia decreases homologous recombination independent of PARP
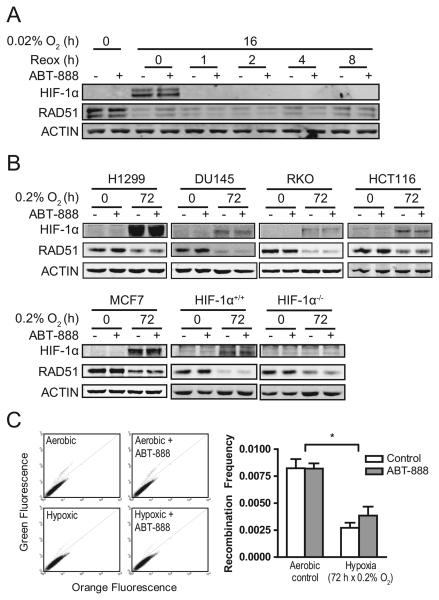
Hypoxia can decrease the expression of a number of HR proteins including RAD51, RAD51C, XRCC3, RAD52, RAD54, BRCA1 and BRCA2 (15, 17). In order to explore the relationship between hypoxia, altered HR protein expression and PARP activity in vitro, we assessed the expression of RAD51 in PARP-inhibited cells under aerobic or hypoxic conditions. RAD51 expression was down-regulated after treatment with severe acute hypoxia (16 h × 0.02% O2) mimicking hypoxic conditions caused by reversible changes in tumor vessel perfusion (Fig.1A). RAD51 levels remained suppressed for at least 8 h after reoxygenation. At longer time points, we also observed decreased RAD51 expression across multiple cell lines (H1299, DU145, RKO, MCF7, HCT116 and MEFs) even at less severe oxygen levels (72 h × 0.2% O2), mimicking hypoxic conditions found distant from the tumor vasculature (Fig. 1B). This RAD51 effect was observed at O2 concentrations less than 0.5% (Supplementary Fig. S1A) and is consistent with our previous report of hypoxia-mediated decreases in the translation of HR proteins (15). Additionally, this is the first report using a genetic knockout model to show that this effect is independent of HIF-1α status (Fig. 1B).
Figure 1.
Hypoxia decreases homologous recombination independent of PARP activity. (A) RAD51 protein expression is decreased in RKO cells following 16 h × 0.02% O2 and remains suppressed for at least after 8 h of reoxygenation with or without ABT-888. (B) RAD51 protein expression is decreased in H1299, DU145, RKO, HCT116, and MCF7 cancer cells as well as HIF-1α-isogenic MEFs following 72 h × 0.2% O2 with or without ABT-888. (C) Functional HR (as assessed by the DR-GFP assay) is decreased following 72 h × 0.2% O2 but is unaffected by ABT-888 in H1299 cells. Representative dot plots are shown. Columns, mean of 3 experiments; bars, SE; *, P<0.05.
A similar phenomenon is observed in vivo as RAD51 expression is inversely correlated with hypoxia (EF5 staining) in multiple xenograft models (Supplementary Fig. S1B-D). These conditions were also sufficient to decrease functional HR as assessed by the DR-GFP HR reporter assay (Fig. 1C). However, in contrast to a recent report (28), PARP inhibition itself did not alter RAD51 expression or HR function under either aerobic or hypoxic conditions (Fig. 1A-C; Supplementary Fig. S2). We conclude that hypoxia leads to defective HR function and that this is independent of PARP activity.
PARP suppression kills homologous recombination defective hypoxic cancer cells in S phase
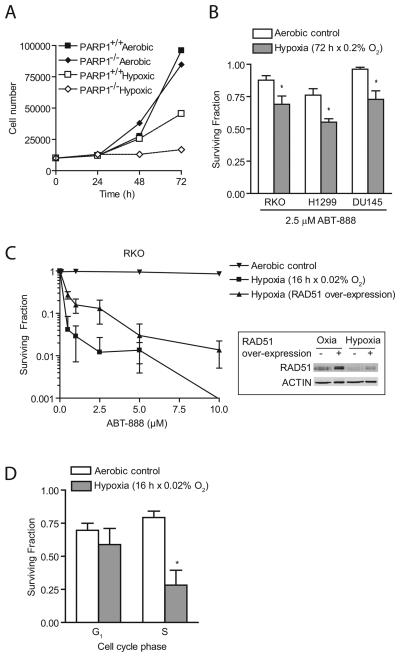
As cells with genetic defects in HR proteins such as BRCA1/2 are exquisitely sensitive to PARP inhibition due to genetic synthetic lethality (18, 19), we assessed whether HR-defective hypoxic cells are also sensitive to PARP inhibition to illustrate the concept of “contextual” synthetic lethality due to the tumor microenvironment. We observed that PARP1−/− MEFs had a profound proliferation defect under hypoxic conditions in comparison to matched PARP1+/+ MEFs (Fig. 2A) indicating an inability of PARP deficient cells to adapt to hypoxic conditions. As an important translational endpoint, we tested PARP inhibitors as potential sensitizers of HR-deficient hypoxic cells. Proliferating cells gassed under conditions of moderate chronic hypoxia, which led to suppressed HR, had decreased clonogenic survival when treated with PARP inhibitors across multiple tumor cell types (Fig. 2B; Supplementary Fig. S3A). Similarly, siRNA knockdown of RAD51 expression to levels observed under hypoxic conditions also resulted in increased sensitivity to PARP inhibition (Supplementary Fig. S3B). A more profound sensitization was observed when cells were treated with PARP inhibitors under severe acute hypoxia followed by reoxygenation (Fig. 2C). The increased clonogenic cell kill may be due to synergy between PARP inhibition and oxidative damage caused by reactive oxygen species (ROS) generated upon reoxygenation from severe hypoxia or anoxia (11). To understand the role of RAD51 in this phenotype, we over-expressed RAD51 in hypoxic cells and observed partial rescue of cellular lethality (Fig. 2C). Complete rescue is probably not achieved due to suppression of multiple members of the HR pathway by hypoxia, in addition to RAD51 (15).
Figure 2.
PARP suppression kills homologous recombination defective hypoxic cancer cells in S phase. (A) PARP1-deficient MEFs proliferate slower under hypoxic (0.2% O2) conditions than their isogenic counterparts. (B) Pharmacologic inhibition of PARP1 sensitized RKO, H1299 and DU145 cells when treated with 72 h × 0.2% O2. (C) Pharmacologic inhibition of PARP1 sensitized RKO cells when treated with 16 h × 0.02% O2. Partial rescue is achieved by over-expression of RAD51. (D) Hypoxic S phase RKO cells generated by mitotic shake-off were more sensitive than G1 phase cells to PARP inhibition. Points and columns, mean of 3 to 5 experiments; bars, SE; *, P<0.05.
Given the role of PARP1 in preventing the collapse of replication forks into replication-associated DSBs, we hypothesized that PARP inhibition is toxic to hypoxic cells in a cell-cycle specific manner. Using synchronized cell populations, we observed that hypoxic cells in S phase, but not G1 phase, were preferentially sensitized to PARP inhibition when compared to aerobic cells (Fig. 2D).
PARP inhibition of hypoxic cells induces DNA damage in proliferating cells during reoxygenation or chronic adaptation to hypoxia
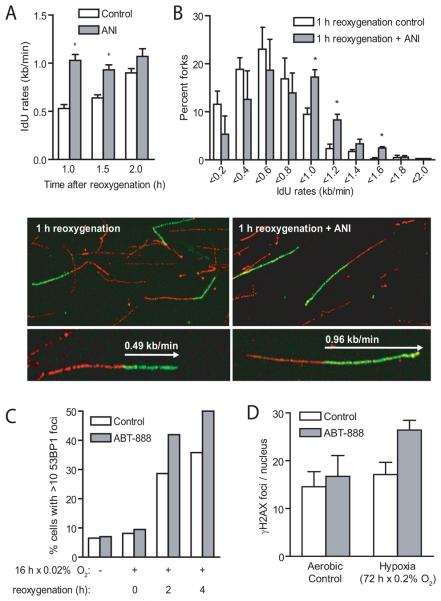
PARP inhibition results in the accumulation of collapsed replication forks requiring HR for their repair (18, 19). We hypothesized that HR-deficient hypoxic cells would have increased difficulty in repairing collapsed replication forks resulting in cell death. The rate of replication re-start after reoxygenation was determined by DNA replication fiber analysis. This confirmed that PARP inhibition increased the rate of replication re-start during reoxygenation after severe hypoxia. Thus indicating that PARP functions to reduce DNA replication kinetics in the presence of accumulating DNA damage (Fig. 3A,B). Consistent with this finding, PARP inhibition in HR-defective hypoxic cells led to elevated 53BP1 and γH2AX foci following either acute or chronic hypoxic exposure (Fig. 3C,D). Hypoxia results in replication fork stalling (10, 29) and it has recently been shown that PARP is activated at stalled replication forks (30). To test if the increase in PARP activity in hypoxic cells is related to an increased amount of hypoxia-stalled replication forks, we co-localized hypoxia-induced PAR foci with induced RPA foci that form at stalled replication forks. We found that PAR foci co-localize well with RPA foci (Supplementary Fig. S4), suggesting that PARP is indeed activated at hypoxia-stalled replication forks.
Figure 3.
PARP inhibition induces DNA damage in proliferating hypoxic cells. (A, B) Replication fiber analysis indicates that PARP inhibition using 4-amino-1,8-naphthalimide (ANI) increased the rate of replication restart during reoxygenation after 16 h × 0.02% O2 in RKO cells. Representative replication fiber images are shown. (C) Immunofluorescent staining of 53BP1 foci in RKO cells shows further elevation following reoxygenation after 16 h × 0.02% O2 when treated with 2.5 μM ABT-888. (D) Immunofluorescent staining of γH2AX foci in H1299 cells shows elevated foci following treatment with 72 h × 0.2% O2 plus 2.5 μM ABT-888. Columns, mean of 3 experiments; bars, SE; *, P<0.05.
We conclude that PARP inhibition leads to accumulation of DNA breaks in cycling hypoxic cells (during reoxygenation or as a consequence of chronic hypoxic adaptation) similar to that reported for tumor cells that are genetically null for HR (18, 19).
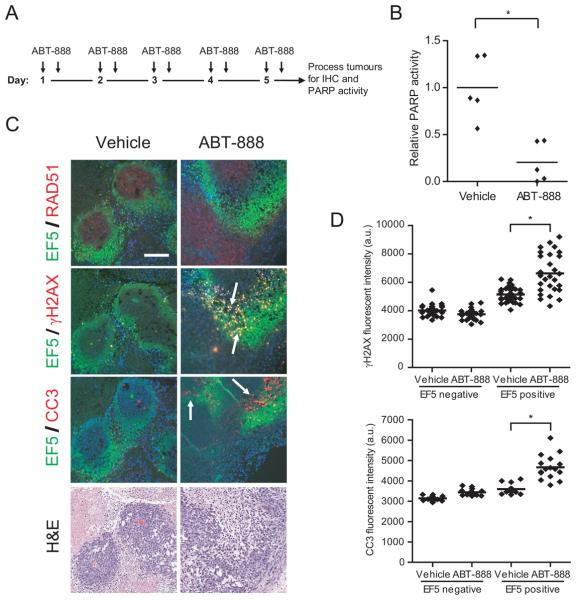
PARP inhibition induces kills hypoxic tumor cells in vivo
Single agent dosing with PARP inhibitors can lead to growth delay in wild-type BRCA1/2 tumor xenograft models (31). We therefore tested whether our observation of synthetic lethality between hypoxia-mediated HR defects and PARP inhibition also occurred in vivo. RKO xenografts were treated twice daily with 50 mg/kg ABT-888 or vehicle for 5 days and assayed for DNA damage within hypoxic tumor subregions. A schematic of the treatment protocol is shown in Figure 4A. Tumor lysates were collected and used to confirm that inhibition of PARP activity was achieved in vivo (Fig. 4B). Immunohistochemical (IHC) staining confirmed decreased expression of RAD51 in hypoxic (EF5-avid) tumor subregions in both the vehicle and PARP-inhibited tumors (Fig. 4C). Importantly, hypoxic regions of the PARP-inhibited tumors displayed significantly elevated expression of γH2AX and cleaved caspase-3 (CC3) selectively across the EF5 gradient (Fig. 4C,D).
Figure 4.
PARP inhibition of hypoxic tumor cells in vivo induces DNA damage. (A) Schematic of ABT-888 treatment. RKO xenografts were treated twice daily for 5 days with 50 mg/kg ABT-888 and then collected for immunohistochemical (IHC) staining and determination of PARP activity. (B) Relative enzymatic PARP activity of tumor lysates collected 2 h after the final ABT-888 treatment verifies PARP inhibition in vivo. (C) Representative IHC staining of vehicle and ABT-888 treated tumors show decreased RAD51 staining in EF5-avid subregions. ABT-888 treated tumors show increased γH2AX and cleaved caspase-3 (CC3) staining (white arrows) in EF5 positive subregions compared to vehicle treated tumors. Scale bar represents 100 microns. (D) Quantification of γH2AX and CC3 fluorescent intensity within aerobic (EF5 negative) and hypoxic (EF5 positive) tumor subregions. Analysis based on 4-8 fields per tumor for 3-5 tumors per treatment group. *, P<0.05.
To determine if PARP inhibition in vivo selectively kills hypoxic tumor cells, we performed ex vivo clonogenic assays on ABT-888 pre-treated tumors that were exposed to 5 Gy ionizing radiation (IR) 24 h after the final ABT-888 dose. After drug washout, IR should selectively kill any remaining aerobic cells without bias from PARP inhibitor radiosensitization. A schematic of the treatment protocol is shown in Figure 5A. Clonogenic survival following tumor irradiation in vivo is an established assay to measure changes in the hypoxic tumor fraction as the radiosensitive aerobic tumor cells are preferentially killed over more radioresistant hypoxic cells. The radiation was delivered 24 h after the final ABT-888 dose, a time when pharmacokinetic and pharmacodynamic studies have shown a return to background levels (32). We observed that ABT-888 pre-treated tumors had lower survival than vehicle-treated tumors following irradiation (Fig. 5B). This is consistent with PARP inhibitor-induced killing of hypoxic HR-defective cells prior to challenge with IR. However, given the effects of PARP inhibition of tumor vasculature (33) and the relatively low hypoxic fraction of the RKO xenografts, it would be difficult to see differences in growth delay that could be directly attributed to sensitization of hypoxic cells to PARP inhibition.
Figure 5.
PARP inhibition of hypoxic tumor cells in vivo induces cell death. (A) Schematic of ABT-888 treatment. RKO xenografts were treated twice daily for 5 days with 50 mg/kg ABT-888. Mice were left for 24 h to allow for drug wash-out before treatment with 5 Gy of ionizing radiation (IR) followed by ex vivo clonogenic assays. This protocol unmasks the hypoxic cell kill without bias from aerobic cell radiosensitization by PARP inhibition. (B) Ex vivo clonogenic assays show decreased survival of ABT-888 treated tumors following exposure to 5 Gy IR. (C) Analysis of mouse intestinal crypts shows no toxicity from PARP inhibition or IR. (D) Model for hypoxia-mediated contextual synthetic lethality with PARP inhibition. Solid tumors have substandard vasculature leading to gradients of moderate to severe hypoxia. Severe acute hypoxia decreases HR capacity and leads to cell cycle arrest which is reversible upon reoxygenation. Moderate chronic hypoxia also decreases HR capacity but still allows for proliferation. PARP inhibition results in unrepaired SSBs which collapse replication forks in S phase. These collapsed replication forks are lethal to tumor cells with hypoxia-induced HR defects potentially though apoptosis, mitotic catastrophe, autophagy or terminal senescence. *, P<0.05.
Importantly, this regimen of PARP inhibition, even in combination with the radiation treatment, did not kill normal tissue clonogens as measured by a gut clonogenic assay (Fig. 5C). This demonstrates the increased therapeutic ratio of PARP inhibitor treatment as resistant, hypoxic tumor tissues are targeted without killing normal tissues. We conclude hypoxic sensitization of tumor cells to PARP inhibition occurs in vivo. A model for the proposed mechanism of hypoxic cell death due to contextual synthetic lethality is shown in Figure 5D.
Discussion
Currently the use of PARP inhibitors as single agents has been limited to clinical trials for patients with genetic deficiencies in BRCA1/2 (23). There is active interest in identifying additional genetic, epigenetic or microenvironmental changes that could lead to a “BRCAness” phenotype with increased sensitivity to PARP inhibitors. To this end, high-throughput screens have identified several potential targets showing sensitivity to PARP inhibition including the transcription coupled DNA repair proteins DDB1 and XAB2 and the cyclin dependent kinase 5 (CDK5) (34, 35). Recently, PTEN deficiency leading to suppressed RAD51 has also been shown to sensitize tumor cells to PARP inhibition (36). In this report, we have shown that hypoxia induced-HR defects can also yield a “BRCAness” phenotype. Unlike a recent report from Hegan and colleagues (28), our findings are independent of any direct PARP-mediated effects on RAD51 expression or HR function. Instead, ABT-888 had no effect on RAD51 protein (Fig. 1A,B) or mRNA (Supplemental Fig. S2A) expression, nor did it alter the efficiency of DR-GFP measured HR (Fig. 1C) or sensitivity to MMC (Supplemental Fig. 2C). Additionally, PARP inhibition alone did not induce a statistically significant increase in γH2AX expression in vitro (Fig. 3D) or in vivo (Fig. 4D). Only in conjunction with hypoxia do we observe decreased HR and synthetic lethality that translates to increased clonogenic killing. This may expand the utility of PARP inhibitors when used alone, or in combination with radiotherapy or chemotherapy, by targeting the hypoxic subpopulation of tumor cells that are otherwise resistant to therapy and possibly responsible for distant metastatic spread (9). Indeed, the use of PARP inhibitors in combined therapy has already shown promise in pre-clinical models with improved growth delay in radiation, temolozolomide, cisplatin, carboplatin or cyclophosphamide treated tumors (31-33, 37). In future clinical trials we foresee the need to determine the hypoxic fraction of tumors to select for patients that would most benefit from this strategy.
It has been demonstrated that PARP1 has a role in HIF-1α stabilization and signaling mediated by nitric oxide and oxidative stress (38, 39). It is conceivable that PARP inhibition could also inhibit HIF-1α accumulation and signaling leading to a blockade of hypoxic responses and more cell death. However, in our model systems we do not observe any altered stabilization of HIF-1α (Fig. 1A,B) or altered HIF-1 transcriptional activity (Fig. S2B).
Two groups have reported PARP inhibitor and cisplatin resistant phenotypes in BRCA2 defective cells based on a reverting BRCA2 mutation (40, 41). In contrast, our contextual synthetic lethality model would not lead to acquired genetic resistance given an alternate pathway of decreased HR based on the decreased transcription and translation of HR genes (15, 42).
HR-compromised hypoxic cells replicating under moderate hypoxia or following reoxygenation showed elevated expression of the DNA damage markers γH2AX and 53BP1 when treated with PARP inhibitors (Fig. 3C,D). A similar finding was reported for BRCA2−/− cells exposed to PARP inhibition (18, 19). Severe hypoxia leads to stalled replication which can be overcome during reoxygenation. However, in the presence of PARP inhibition our DNA repair foci and replication fiber data supports that HR-deficient reoxygenated or chronically hypoxic cells acquire collapsed/damaged replication forks (Fig. 3A,B). Consistent with this data, the toxicity was primarily manifested in S phase cells (Fig. 2D). Our findings agree with those of Sugimura et al. who showed that PARP1 is required for replication fork slowing on damaged DNA and that fork slowing is HR-dependent (43). The epistasis between PARP and HR is explained by PARP being recruited to hypoxia-stalled forks to activate a slow HR repair process (30). This model is also supported by the co-localization of PAR polymers and RPA foci in hypoxia treated cells (Supplementary Fig. S4).
The development of drugs designed to exploit tumor hypoxia has been focused on prodrugs that are activated by metabolic reduction under hypoxic conditions to form free radical based cell cytotoxins causing DNA strand breaks, base damage and DNA-protein crosslinks (6). Our work here supports another novel treatment strategy to sensitize traditionally resistant hypoxic cells using PARP inhibitors which may have a unique therapeutic ratio in killing hypoxic cancer cells over aerobic normal cells. This is specifically true given recent clinical trial data in which PARP inhibition had minimal side-effects (23, 44, 45). There may also be a role for combined PARP and HIF-1α-targeting as PARP may modify HIF-1α accumulation through differential oxidative stress under aerobic versus hypoxic conditions and anti-HIF-1α agents are currently being tested in pre-clinical and clinical settings (39, 46, 47).
Hypoxic tumor cells may have suppression of other DNA repair pathways beyond HR including non-homologous end-joining, mismatch and base excision repair (48). Further understanding of the contextual synthetic lethality to these and other DNA damage signaling pathways could define new approaches to individualized cancer therapy. Indeed, it has recently been reported that deficiency in the mismatch repair (MMR) proteins MSH2 and MLH1 are synthetically lethal with disruption of the DNA polymerases POLB and POLG respectively (49). Both of these MMR proteins are known to be down-regulated by hypoxia and therefore inhibition of POLB or POLG may also show contextual synthetic lethality with hypoxia. At the moment, clinically useful inhibitors of POLB or POLG are not yet available but given the strong inhibition of MSH2 and MLH1 by hypoxia this is a concept that warrants further study.
Elevated levels of endogenous γH2AX or 53BP1 foci and decreased RAD51 expression in hypoxic subregions of tumor biopsies may be biomarkers of potential cell kill with PARP inhibitors. The efficacy of this treatment can also be tracked in hypoxic subregions with sequential biopsies during and after treatment similar to the published use of hair follicle γH2AX foci as a normal tissue biomarker of PARP inhibition (23). Taken together our data describes a model of hypoxia-mediated contextual synthetic lethality with PARP inhibition which supports the development of novel biomarkers for prediction of PARP inhibitor treatment susceptibility and response (Fig. 5D).
Supplementary Material
Acknowledgments
ABT-888 was provided by Abbott Laboratories, Inc., and the National Cancer Institute (NIH) through the Cancer Therapy Evaluation Program (CTEP).
Grant Support
The studies were supported by grants from the Terry Fox Foundation-NCIC Hypoxia PMH Program Grant (15004) and a NCIC operating grant (17154) to RGB. RGB is a Canadian Cancer Society Research Scientist. EMH, IMP, and ZB are supported by the Cancer Research UK, grant reference C6515/A9321 awarded to EMH.
References
- 1.Birner P, Schindl M, Obermair A, Plank C, Breitenecker G, Oberhuber G. Overexpression of hypoxia-inducible factor 1alpha is a marker for an unfavorable prognosis in early-stage invasive cervical cancer. Cancer Res. 2000;60:4693–6. [PubMed] [Google Scholar]
- 2.Birner P, Schindl M, Obermair A, Breitenecker G, Oberhuber G. Expression of hypoxia-inducible factor 1alpha in epithelial ovarian tumors: its impact on prognosis and on response to chemotherapy. Clin Cancer Res. 2001;7:1661–8. [PubMed] [Google Scholar]
- 3.Aebersold DM, Burri P, Beer KT, et al. Expression of hypoxia-inducible factor-1alpha: a novel predictive and prognostic parameter in the radiotherapy of oropharyngeal cancer. Cancer Res. 2001;61:2911–6. [PubMed] [Google Scholar]
- 4.Bos R, Zhong H, Hanrahan CF, et al. Levels of hypoxia-inducible factor-1 alpha during breast carcinogenesis. J Natl Cancer Inst. 2001;93:309–14. doi: 10.1093/jnci/93.4.309. [DOI] [PubMed] [Google Scholar]
- 5.Nordsmark M, Bentzen SM, Rudat V, et al. Prognostic value of tumor oxygenation in 397 head and neck tumors after primary radiation therapy. An international multi-center study. Radiother Oncol. 2005;77:18–24. doi: 10.1016/j.radonc.2005.06.038. [DOI] [PubMed] [Google Scholar]
- 6.Brown JM, Wilson WR. Exploiting tumour hypoxia in cancer treatment. Nat Rev Cancer. 2004;4:437–47. doi: 10.1038/nrc1367. [DOI] [PubMed] [Google Scholar]
- 7.Reynolds TY, Rockwell S, Glazer PM. Genetic instability induced by the tumor microenvironment. Cancer Res. 1996;56:5754–7. [PubMed] [Google Scholar]
- 8.Chan N, Milosevic M, Bristow RG. Tumor hypoxia, DNA repair and prostate cancer progression: new targets and new therapies. Future Oncol. 2007;3:329–41. doi: 10.2217/14796694.3.3.329. [DOI] [PubMed] [Google Scholar]
- 9.Bristow RG, Hill RP. Hypoxia and metabolism. Hypoxia, DNA repair and genetic instability. Nat Rev Cancer. 2008;8:180–92. doi: 10.1038/nrc2344. [DOI] [PubMed] [Google Scholar]
- 10.Hammond EM, Denko NC, Dorie MJ, Abraham RT, Giaccia AJ. Hypoxia links ATR and p53 through replication arrest. Mol Cell Biol. 2002;22:1834–43. doi: 10.1128/MCB.22.6.1834-1843.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hammond EM, Dorie MJ, Giaccia AJ. ATR/ATM targets are phosphorylated by ATR in response to hypoxia and ATM in response to reoxygenation. J Biol Chem. 2003;278:12207–13. doi: 10.1074/jbc.M212360200. [DOI] [PubMed] [Google Scholar]
- 12.Freiberg RA, Hammond EM, Dorie MJ, Welford SM, Giaccia AJ. DNA damage during reoxygenation elicits a Chk2-dependent checkpoint response. Mol Cell Biol. 2006;26:1598–609. doi: 10.1128/MCB.26.5.1598-1609.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bencokova Z, Kaufmann MR, Pires IM, Lecane PS, Giaccia AJ, Hammond EM. ATM activation and signaling under hypoxic conditions. Mol Cell Biol. 2009;29:526–37. doi: 10.1128/MCB.01301-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gibson SL, Bindra RS, Glazer PM. Hypoxia-induced phosphorylation of Chk2 in an ataxia telangiectasia mutated-dependent manner. Cancer Res. 2005;65:10734–41. doi: 10.1158/0008-5472.CAN-05-1160. [DOI] [PubMed] [Google Scholar]
- 15.Chan N, Koritzinsky M, Zhao H, et al. Chronic hypoxia decreases synthesis of homologous recombination proteins and therapeutic resistance. Cancer Res. 2008;68:605–14. doi: 10.1158/0008-5472.CAN-07-5472. [DOI] [PubMed] [Google Scholar]
- 16.Meng AX, Jalali F, Cuddihy A, et al. Hypoxia down-regulates DNA double strand break repair gene expression in prostate cancer cells. Radiother Oncol. 2005;76:168–76. doi: 10.1016/j.radonc.2005.06.025. [DOI] [PubMed] [Google Scholar]
- 17.Bindra RS, Schaffer PJ, Meng A, et al. Down-regulation of Rad51 and decreased homologous recombination in hypoxic cancer cells. Mol Cell Biol. 2004;24:8504–18. doi: 10.1128/MCB.24.19.8504-8518.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bryant HE, Schultz N, Thomas HD, et al. Specific killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) polymerase. Nature. 2005;434:913–7. doi: 10.1038/nature03443. [DOI] [PubMed] [Google Scholar]
- 19.Farmer H, McCabe N, Lord CJ, et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature. 2005;434:917–21. doi: 10.1038/nature03445. [DOI] [PubMed] [Google Scholar]
- 20.McCabe N, Turner NC, Lord CJ, et al. Deficiency in the repair of DNA damage by homologous recombination and sensitivity to poly(ADP-ribose) polymerase inhibition. Cancer Res. 2006;66:8109–15. doi: 10.1158/0008-5472.CAN-06-0140. [DOI] [PubMed] [Google Scholar]
- 21.Plummer ER, Calvert H. Targeting poly(ADP-ribose) polymerase: a two-armed strategy for cancer therapy. Clin Cancer Res. 2007;13:6252–6. doi: 10.1158/1078-0432.CCR-07-0617. [DOI] [PubMed] [Google Scholar]
- 22.Arnaudeau C, Lundin C, Helleday T. DNA double-strand breaks associated with replication forks are predominantly repaired by homologous recombination involving an exchange mechanism in mammalian cells. J Mol Biol. 2001;307:1235–45. doi: 10.1006/jmbi.2001.4564. [DOI] [PubMed] [Google Scholar]
- 23.Fong PC, Boss DS, Yap TA, et al. Inhibition of poly(ADP-ribose) polymerase in tumors from BRCA mutation carriers. N Engl J Med. 2009;361:123–34. doi: 10.1056/NEJMoa0900212. [DOI] [PubMed] [Google Scholar]
- 24.Schipani E, Ryan HE, Didrickson S, Kobayashi T, Knight M, Johnson RS. Hypoxia in cartilage: HIF-1alpha is essential for chondrocyte growth arrest and survival. Genes Dev. 2001;15:2865–76. doi: 10.1101/gad.934301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Trucco C, Oliver FJ, de Murcia G, Menissier-de Murcia J. DNA repair defect in poly(ADP-ribose) polymerase-deficient cell lines. Nucleic Acids Res. 1998;26:2644–9. doi: 10.1093/nar/26.11.2644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Liu SK, Coackley C, Krause M, Jalali F, Chan N, Bristow RG. A novel poly(ADP-ribose) polymerase inhibitor, ABT-888, radiosensitizes malignant human cell lines under hypoxia. Radiother Oncol. 2008;88:258–68. doi: 10.1016/j.radonc.2008.04.005. [DOI] [PubMed] [Google Scholar]
- 27.Wilsker D, Petermann E, Helleday T, Bunz F. Essential function of Chk1 can be uncoupled from DNA damage checkpoint and replication control. Proc Natl Acad Sci U S A. 2008;105:20752–7. doi: 10.1073/pnas.0806917106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hegan DC, Lu Y, Stachelek GC, Crosby ME, Bindra RS, Glazer PM. Inhibition of poly(ADP-ribose) polymerase down-regulates BRCA1 and RAD51 in a pathway mediated by E2F4 and p130. Proc Natl Acad Sci U S A. 2010;107:2201–6. doi: 10.1073/pnas.0904783107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pires IM, Bencokova Z, Milani M, et al. Effects of acute versus chronic hypoxia on DNA damage responses and genomic instability. Cancer Res. 2010;70:925–35. doi: 10.1158/0008-5472.CAN-09-2715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bryant HE, Petermann E, Schultz N, et al. PARP is activated at stalled forks to mediate Mre11-dependent replication restart and recombination. Embo J. 2009;28:2601–15. doi: 10.1038/emboj.2009.206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Albert JM, Cao C, Kim KW, et al. Inhibition of poly(ADP-ribose) polymerase enhances cell death and improves tumor growth delay in irradiated lung cancer models. Clin Cancer Res. 2007;13:3033–42. doi: 10.1158/1078-0432.CCR-06-2872. [DOI] [PubMed] [Google Scholar]
- 32.Palma JP, Rodriguez LE, Bontcheva-Diaz VD, et al. The PARP inhibitor, ABT-888 potentiates temozolomide: correlation with drug levels and reduction in PARP activity in vivo. Anticancer Res. 2008;28:2625–35. [PubMed] [Google Scholar]
- 33.Donawho CK, Luo Y, Penning TD, et al. ABT-888, an orally active poly(ADP-ribose) polymerase inhibitor that potentiates DNA-damaging agents in preclinical tumor models. Clin Cancer Res. 2007;13:2728–37. doi: 10.1158/1078-0432.CCR-06-3039. [DOI] [PubMed] [Google Scholar]
- 34.Lord CJ, McDonald S, Swift S, Turner NC, Ashworth A. A high-throughput RNA interference screen for DNA repair determinants of PARP inhibitor sensitivity. DNA Repair (Amst) 2008;7:2010–9. doi: 10.1016/j.dnarep.2008.08.014. [DOI] [PubMed] [Google Scholar]
- 35.Turner NC, Lord CJ, Iorns E, et al. A synthetic lethal siRNA screen identifying genes mediating sensitivity to a PARP inhibitor. Embo J. 2008;27:1368–77. doi: 10.1038/emboj.2008.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Mendes-Pereira AM, Martin SA, Brough R, et al. Synthetic lethal targeting of PTEN mutant cells with PARP inhibitors. EMBO Mol Med. 2009;1:315–22. doi: 10.1002/emmm.200900041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Russo AL, Kwon HC, Burgan WE, et al. In vitro and in vivo radiosensitization of glioblastoma cells by the poly (ADP-ribose) polymerase inhibitor E7016. Clin Cancer Res. 2009;15:607–12. doi: 10.1158/1078-0432.CCR-08-2079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Martinez-Romero R, Canuelo A, Martinez-Lara E, Javier Oliver F, Cardenas S, Siles E. Poly(ADP-ribose) polymerase-1 modulation of in vivo response of brain hypoxia-inducible factor-1 to hypoxia/reoxygenation is mediated by nitric oxide and factor inhibiting HIF. J Neurochem. 2009;111:150–9. doi: 10.1111/j.1471-4159.2009.06307.x. [DOI] [PubMed] [Google Scholar]
- 39.Martinez-Romero R, Martinez-Lara E, Aguilar-Quesada R, Peralta A, Oliver FJ, Siles E. PARP-1 modulates deferoxamine-induced HIF-1alpha accumulation through the regulation of nitric oxide and oxidative stress. J Cell Biochem. 2008;104:2248–60. doi: 10.1002/jcb.21781. [DOI] [PubMed] [Google Scholar]
- 40.Edwards SL, Brough R, Lord CJ, et al. Resistance to therapy caused by intragenic deletion in BRCA2. Nature. 2008;451:1111–5. doi: 10.1038/nature06548. [DOI] [PubMed] [Google Scholar]
- 41.Sakai W, Swisher EM, Karlan BY, et al. Secondary mutations as a mechanism of cisplatin resistance in BRCA2-mutated cancers. Nature. 2008;451:1116–20. doi: 10.1038/nature06633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bindra RS, Glazer PM. Repression of RAD51 gene expression by E2F4/p130 complexes in hypoxia. Oncogene. 2007;26:2048–57. doi: 10.1038/sj.onc.1210001. [DOI] [PubMed] [Google Scholar]
- 43.Sugimura K, Takebayashi S, Taguchi H, Takeda S, Okumura K. PARP-1 ensures regulation of replication fork progression by homologous recombination on damaged DNA. J Cell Biol. 2008;183:1203–12. doi: 10.1083/jcb.200806068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Plummer R, Jones C, Middleton M, et al. Phase I study of the poly(ADP-ribose) polymerase inhibitor, AG014699, in combination with temozolomide in patients with advanced solid tumors. Clin Cancer Res. 2008;14:7917–23. doi: 10.1158/1078-0432.CCR-08-1223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kummar S, Kinders R, Gutierrez ME, et al. Phase 0 clinical trial of the poly (ADP-ribose) polymerase inhibitor ABT-888 in patients with advanced malignancies. J Clin Oncol. 2009;27:2705–11. doi: 10.1200/JCO.2008.19.7681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dewhirst MW, Cao Y, Moeller B. Cycling hypoxia and free radicals regulate angiogenesis and radiotherapy response. Nat Rev Cancer. 2008;8:425–37. doi: 10.1038/nrc2397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Rankin EB, Giaccia AJ. The role of hypoxia-inducible factors in tumorigenesis. Cell Death Differ. 2008;15:678–85. doi: 10.1038/cdd.2008.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mihaylova VT, Bindra RS, Yuan J, et al. Decreased expression of the DNA mismatch repair gene Mlh1 under hypoxic stress in mammalian cells. Mol Cell Biol. 2003;23:3265–73. doi: 10.1128/MCB.23.9.3265-3273.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Martin SA, McCabe N, Mullarkey M, et al. DNA polymerases as potential therapeutic targets for cancers deficient in the DNA mismatch repair proteins MSH2 or MLH1. Cancer Cell. 2010;17:235–48. doi: 10.1016/j.ccr.2009.12.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.