Abstract
Background
Weight-related problems are prevalent in adolescent girls.
Purpose
To evaluate New Moves, a school-based program aimed at preventing weight-related problems in adolescent girls.
Design
School-based group-randomized controlled design.
Setting/participants
356 girls (mean age=15.8± 1.2 years) from six intervention and six control high schools. Over 75% of the girls were racial/ethnic minorities and 46% were overweight or obese. Data were collected in 2007–2009 and analyzed in 2009–2010.
Intervention
An all-girls physical education class, supplemented with nutrition and self-empowerment components, individual sessions using motivational interviewing, lunch meetings, and parent outreach.
Main outcome measures
Percent body fat, BMI, physical activity, sedentary activity, dietary intake, eating patterns, unhealthy weight control behaviors, and body/self-image.
Results
New Moves did not lead to significant changes in the girls’ percent body fat or BMI but improvements were seen for sedentary activity, eating patterns, unhealthy weight control behaviors, and body/self-image. For example, in comparison to control girls, at 9-month follow-up, intervention girls decreased their sedentary behaviors by approximately one 30-minute block a day (p=.050); girls increased their portion control behaviors (p=.014); the percentage of girls using unhealthy weight control behaviors decreased by 13.7% (p=.021), and improvements were seen in body image (p=.045) and self-worth (p=.031). Additionally, intervention girls reported more support by friends, teachers, and families for healthy eating and physical activity.
Conclusions
New Moves provides a model for addressing the broad spectrum of weight-related problems among adolescent girls. Further work is needed to enhance the effectiveness of interventions to improve weight status of youth.
Weight-related problems, including obesity, inadequate physical activity, poor eating behaviors, unhealthy weight control practices, and body dissatisfaction, are prevalent among adolescent girls.1, 2 The prevalence of obesity, while high among all subgroups of adolescents, tends to be somewhat higher among ethnic and racial minorities. Among African American adolescent girls, 45% are overweight or obese, compared to 37% of white girls.3 Further, girls from low-SES backgrounds tend to have higher levels of obesity than girls from higher SES backgrounds.4 Research shows that weight-related problems are inter-related. For example, 76% of obese adolescent girls engage in unhealthy weight control behaviors, (e.g., skipping meals, fasting, taking diet pills or smoking cigarettes for weight control) as compared to 51% of normal weight girls. Similarly, 66% of obese girls have low levels of body satisfaction, compared to 38% of normal weight girls.2 Unhealthy weight control behaviors and body dissatisfaction have been found to longitudinally predict excessive weight gain in adolescent girls, even after adjusting for differences in baseline weight status.5, 6 The high prevalence and co-occurrence of weight–related problems among adolescent girls points to a need for interventions aimed at preventing a spectrum of weight-related problems, particularly among underserved adolescents from racial/ethnic minority and low-SES backgrounds.
This paper describes the main findings from a group-RCT designed to evaluate the impact of a school-based intervention aimed at preventing weight-related problems in adolescent girls: New Moves. It was hypothesized that girls in the intervention condition would decrease their percent body fat and BMI, increase physical activity, decrease sedentary behavior, improve eating behaviors, and decrease body dissatisfaction and the use of unhealthy weight control behaviors, as compared to girls in the comparison condition.7–10 In addition to examining these outcomes, perceived changes in the social environments of the participating girls were assessed, given the importance placed on providing a supportive environment within New Moves. Finally, program satisfaction among participating girls and their parents were examined.
METHODS
Overview of New Moves
New Moves aims to meet the needs of adolescent girls who are overweight or at risk for becoming overweight due to sedentary lifestyles 7–10. New Moves is novel in its approach, in that it incorporates principles from both the eating disorders and obesity fields.11–13 Thus, weight loss goals are not discussed and the program focuses on behavioral change. New Moves is implemented within schools, as an all-girls physical education class, with supplementary group and individual activities. The program strives to provide a supportive environment in which all girls feel comfortable being physically active and discussing weight-related issues, regardless of their size, shape, or level of physical activity. The underlying program philosophy is that if girls feel good about themselves, they will want to take care of their bodies 6, 14.
Study design and study population
New Moves was evaluated using a group-randomized controlled design, with six intervention and six control high schools in the Minneapolis/St. Paul metropolitan area of Minnesota. Three intervention and three control schools participated in the study during the 2007–2008 school year and another three intervention and three control schools participated in 2008–2009. High schools were recruited into the study on the condition that they would participate as either control or intervention sites and were randomized into these conditions. The study was approved by the University of Minnesota’s IRB and by participating school districts. Participants provided written assent and parent consent.
Girls in both intervention and control schools participated in an all-girls physical education class during the first semester of the school year. Additionally, intervention girls received the New Moves curriculum during their physical education class and participated in New Moves activities throughout the rest of the school year. Teachers within control schools did not receive training on New Moves until after the study period and were free to conduct their physical education classes as they desired during the study period. Thus, the study design allows for an evaluation of the New Moves program above and beyond any effects of participating in an all-girls physical education class.
Participating schools were in urban and first-ring suburban areas and were selected because of their diverse student bodies. The percentage of students eligible for free or reduced school breakfast and lunch was 58% in the intervention schools (range: 25%–87%) and 56% in the control schools (range: 22%–92%). Table 1 describes the baseline characteristics of the 356 girls who participated in the study. Over 75% of the girls were racial/ethnic minorities and nearly half were overweight or obese.
Table 1.
Baseline description of New Moves study population by intervention condition
| Total N=356 M (SD) |
Intervention n=182 M (SD) |
Control n=174 M (SD) |
Pa | |
|---|---|---|---|---|
| Age | 15.8 (1.17) | 15.7 (1.13) | 15.8 (1.22) | 0.296 |
| n (%) | n (%) | n (%) | ||
| Weight Status | 0.572 | |||
| < 85th percentile | 191 (53.8) | 96 (53.0) | 95 (54.6) | |
| 85th – 95th percentile | 64 (18.0) | 30 (16.6) | 34 (19.5) | |
| ≥95th percentile | 100 (28.2) | 55 (30.4) | 45 (25.9) | |
| Race/ethnicity | 0.046 | |||
| African-American/ | ||||
| Black | 101 (28.4) | 59 (32.4) | 42 (24.1) | |
| White | 87 (24.4) | 49 (26.9) | 38 (21.8) | |
| Asianb | 82 (23.0) | 30 (16.5) | 52 (29.9) | |
| Hispanic | 51 (14.3) | 24 (13.2) | 27 (15.5) | |
| Mixed/Other | 26 (7.3) | 14 (7.7) | 12 (6.9) | |
| American Indian | 9 (2.5) | 6 (3.3) | 3 (1.7) |
P-values are for comparisons between intervention and control groups at baseline
The majority (86%) of the Asians self-identified as Hmong
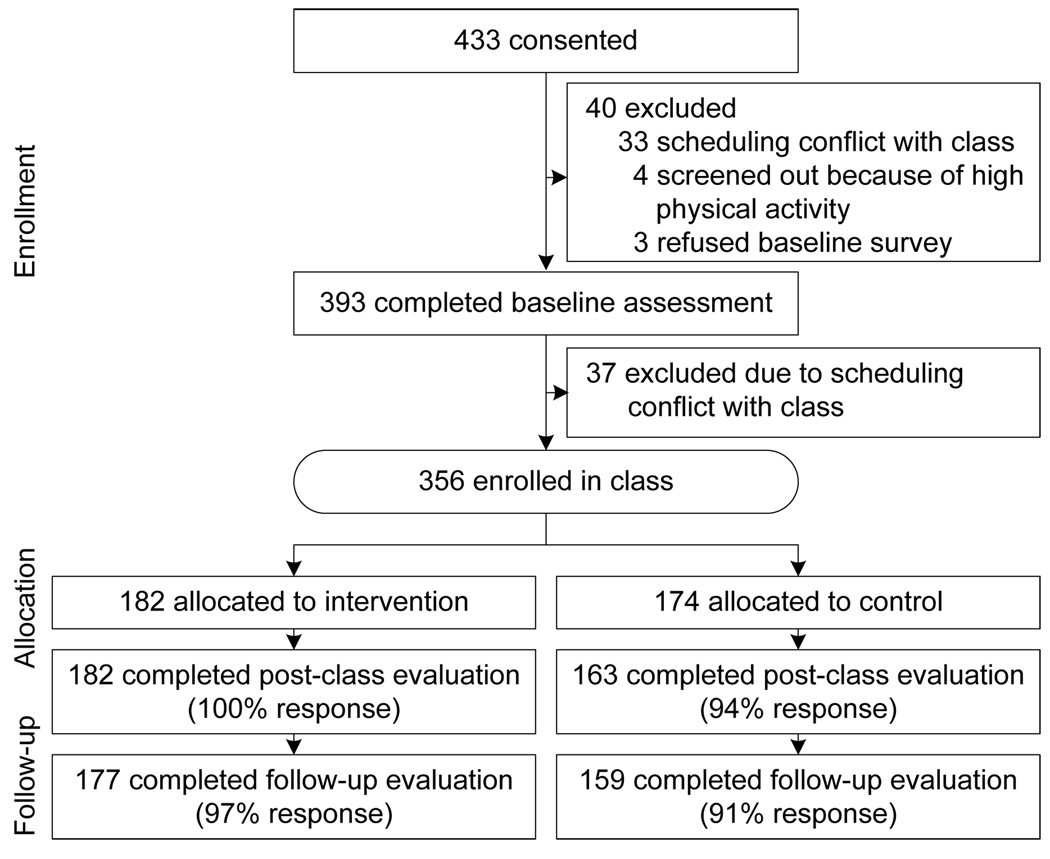
Girls participated in evaluation assessments at three points: baseline (prior to the fall physical education class), post-class (immediately after the fall class), and follow-up (end of school year, approximately 9 months from the beginning of the intervention). Additionally, parents of intervention girls were mailed process surveys at follow-up. Baseline and follow-up assessments were conducted at the University of Minnesota General Clinical Research Center and post-class assessments were done at school. As shown in Figure 1, the overall response at follow-up was 94% (intervention: 97%; control: 91%).
Figure 1.
Flow chart showing response patterns in intervention and control conditions
Recruitment
Girls in intervention and control schools were invited to register for an all-girls physical education class as an alternative to the regular coeducational class. In participating schools, students were required to take either one or two physical education classes to graduate from high school; participation in this class counted toward that requirement. Recruitment materials were designed to appeal to inactive girls interested in healthy weight management. Care was used to avoid stigmatizing the class in any way. A class description was included in the school catalogue used for class registration. Additionally, posters and flyers about the program were displayed at schools. Girls were screened for physical activity and eating disorder behaviors. Four girls were excluded because of high levels of physical activity (≥1 hour/day). No girls were excluded because of eating disorder behaviors (vomiting or laxative use weekly or more).
Description of New Moves intervention
The development of New Moves was guided by extensive formative research 15–21 and pilot-testing.9 In accordance with Social Cognitive Theory, which provided the primary theoretic framework for New Moves,22, 23 the program targets socio-environmental factors (e.g., peer support), personal factors (e.g., body image), and behavioral factors (e.g., goal- setting), to bring about changes in physical activity, eating, and weight control behaviors. In addition, the Transtheoretical Model 24–26 informed program content and structure. New Moves targeted girls in the precontemplation, contemplation, and preparation stages for physical activity and aimed to move girls forward in their stages of change for physical activity and other behaviors. Motivational interviewing was used as it takes into account readiness for change 27. Eight behavioral objectives, targeted throughout the program, include: (1) be more physically active; (2) limit sedentary time; (3) increase fruit and vegetable intake; (4) limit sugar-sweetened beverages; (5) eat breakfast every day; (6) pay attention to portion sizes and your body’s signs of hunger and satiety; (7) avoid unhealthy weight control behaviors; and (8) focus on your positive traits.
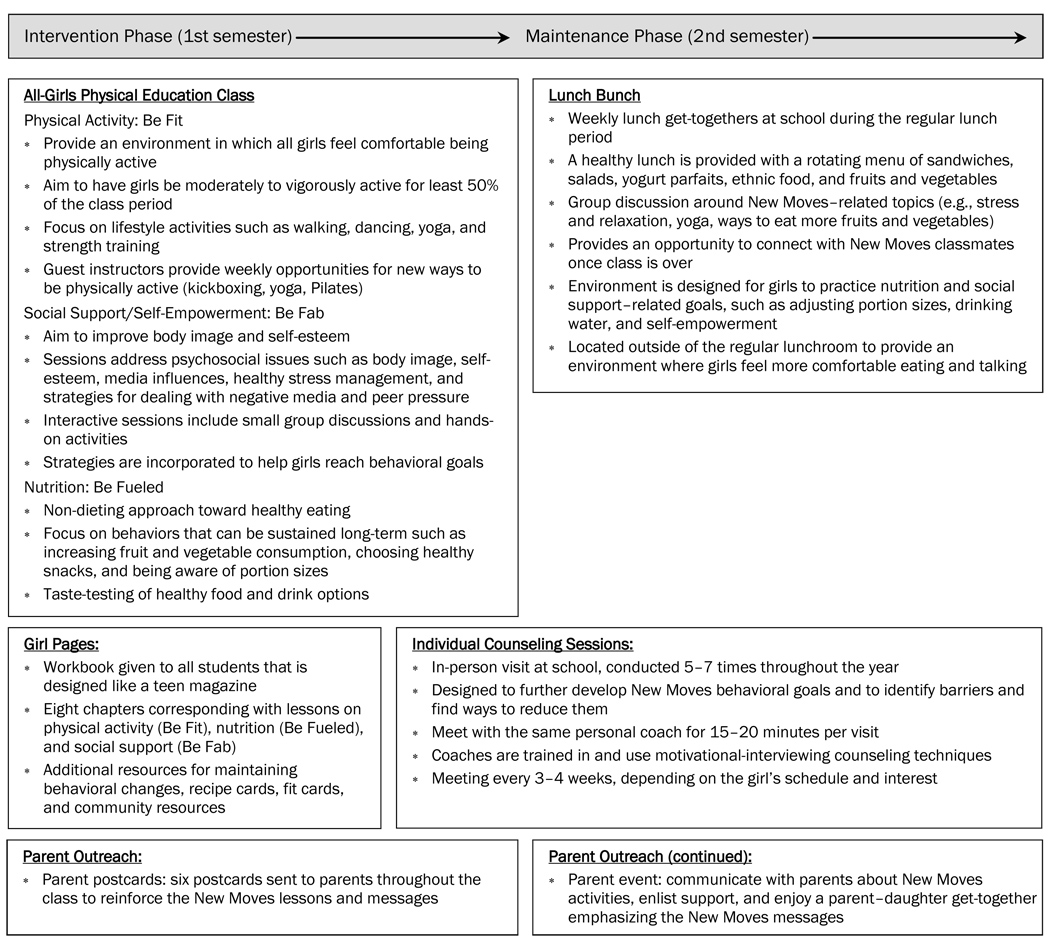
New Moves program components included: (1) the New Moves physical education class, which incorporated nutrition and social support/self-empowerment sessions; (2) individual counseling sessions using motivation interviewing techniques; (3) lunch get-togethers (lunch bunches) once a week during the maintenance period; and (4) minimal parent outreach activities.7, 10 Program components are described in Figure 2. Additionally, intervention materials are available at www.newmovesonline.com.
Figure 2.
Key components of the New Moves intervention during a 9-month school year
The New Moves physical education class was approximately 16 weeks long. Girls participated in physical activity (Be Fit) 4 days/week and nutrition (Be Fueled) or social support/self-empowerment (Be Fab) classes 1 day/week. Most girls (91%) attended at least 80% of the classes. Be Fit sessions were taught 3 days/week by school physical education teachers and 1 day/week by different community guest instructors who exposed the girls to fun activities (e.g., dance, hip hop, kickboxing) available in the community. New Moves intervention staff ran all other program components. Physical education teachers participated in a full-day training prior to the start of the intervention and a half-day training in the middle of the program. Additionally, teachers received regular, ongoing support from New Moves staff throughout the program.
Girls also participated in individual counseling sessions with their New Moves coach in which they personal goals for behavioral change based on eight New Moves behavioral objectives.8 The girls explored how to best achieve their goals and, if ready, made a plan for change. Motivational interviewing strategies were used to assist the girls in moving toward change.27–29 The majority of the girls (80.8%) participated in 5–7 sessions (range: 0–7). New Moves coaches were intervention staff who received training and ongoing support in motivational interviewing techniques.
During the maintenance period (second semester), lunch get-togethers (lunch bunches) were held at school 1 day/week; 56% of the girls attended at least half of the lunch bunches. At lunch bunches, girls were served healthy food and engaged in informal discussions on New Moves topics with New Moves staff.
Finally, New Moves included a minimal parent outreach component. Six postcards were sent home to reinforce New Moves messages. On process surveys, which were mailed home and completed by 116 parents (of 182 intervention girls), 84% of the responding parents indicated that they read the postcards. Additionally, during the maintenance period, there was a parent–daughter retreat day at a local community center that focused on New Moves messages; 21% of the girls had a parent attend.
Measures
Variables included in the current analysis related directly to the eight behavioral objectives targeted in New Moves: physical activity, sedentary behaviors, dietary intake, eating patterns, unhealthy weight control behaviors, and body/self image. Self-efficacy for physical activity and goal-setting for physical activity and eating behaviors were also included given their centrality within Social Cognitive Theory.22, 23 Stages of change were assessed for key behaviors in order to detect progression toward behavioral change (e.g., from precontemplation to contemplation).24–26 Given the importance of a supportive environment to facilitate changes in weight-related attitudes and behaviors, changes in perceived social support were also assessed. All variables are described in Appendix A, available online at www.ajpm-online.net.
Percent body fat was assessed with dual-energy x-ray absorptiometry (DXA) (Lunar Model, Madison, WI). Trained research staff measured participants’ height and weight using standard procedures.52 BMI was calculated and participants were classified as non-overweight (BMI < 85th percentile), overweight (85th percentile ≤ BMI < 95th percentile) or obese (BMI ≥ 95th percentile) based on their BMI percentile for age and gender using the CDC Growth Charts.30, 31 Physical activity was assessed with the 3-Day Physical Activity Recall (3-DPAR) survey.32, 36 Dietary intake was assessed with one 24-hour dietary recall conducted by trained research staff (Nutrition Data System for Research software version 2006 developed by the Nutrition Coordinating Center (NCC), University of Minnesota, Minneapolis, MN.) Other measures were assessed with the New Moves survey (available at www.newmovesonline.com). Most survey items were from previous studies and had high reliability and/or validity. Additionally, the New Moves survey was pilot-tested with 48 adolescents for overall comprehension and item/scale psychometrics, including 2-week test–retest of variables. Cronbach’s alpha values shown in Appendix A (available online at www.ajpm-online.net) are from the final sample of 356 girls, whereas the test-retest values are from the pilot sample. All variables were assessed at the three time-points, with the exception of the DXA measures of body fat and the 24-hour recalls of dietary intake, which were assessed only at baseline and at follow-up.
Statistical analysis
The experimental design was a group-randomized trial in 12 schools involving measurement of a cohort of girls at baseline, post-class, and follow-up. For descriptive purposes the baseline means and individual SDs adjusted for age and ethnicity/race were generated. The post-class and follow-up means (and the differences by experimental condition) were obtained from a two time-point repeated measures analysis of post-class and follow-up, adjusted for the baseline measure, age and ethnicity/race, and with school nested in the experimental condition as a random effect.53 Each p-value is derived from the associated t-statistic, having 10 df as required by the group-randomized design. P-values have not been adjusted for multiple testing. Some outcomes are assessed by categoric scales; however because ultimately it is the means per school that drive the analysis of a group-randomized trial, the assumption of normality in the mixed model is appropriate.54 Data for this paper were analyzed in 2009–2010.
RESULTS
Program impact on body composition and key areas targeted for change
Table 2 shows the intervention effect on body composition and key areas targeted for change within the domains of physical activity, sedentary activity, dietary intake, eating patterns, unhealthy weight control practices and body and self-image. Changes were all in the hypothesized and desired direction; although not all reached significance. Changes in percent body fat and BMI were not significant and, in general, changes for determinants of behaviors (e.g., goal-setting) were seen more often than for actual behaviors. Changes that were significant are discussed below.
Table 2.
Body composition and behavioral outcomes: Means and intervention effect estimatesa
| M | Test of intervention effect | ||||||
|---|---|---|---|---|---|---|---|
| Baselineb | Post Classc |
Follow-upc | Post-classd | Follow-upd | |||
| M (SD) | M | M | Intervention Effect |
p-value | Intervention Effect |
p-value | |
|
BODY COMPOSITION % Body fat (DXA)e |
|||||||
| Intervention | 37.3 (9.55) | — | 37.2 | — | — | –0.46 | 0.216 |
| Control | 36.6 (8.84) | — | 37.7 | ||||
| BMI | |||||||
| Intervention | 25.9 (7.11) | 25.8 | 26.0 | –0.08 | 0.512 | –0.10 | 0.446 |
| Control | 25.5 (6.49) | 25.9 | 26.1 | ||||
|
PHYSICAL ACTIVITY (PA) Total physical activity (30-minute blocks/day) |
|||||||
| Intervention | 4.80 (3.52) | 3.83 | 4.92 | 0.08 | 0.894 | 1.20 | 0.068 |
| Control | 4.23 (3.65) | 3.75 | 3.72 | ||||
|
Moderate and vigorous PA (30-minute blocks/day) |
|||||||
| Intervention | 3.04 (2.84) | 2.62 | 2.80 | 0.22 | 0.555 | 0.53 | 0.186 |
| Control | 2.92 (2.98) | 2.40 | 2.27 | ||||
| Stage of change: PA(range: 1–5) | |||||||
| Intervention | 3.19 (1.11) | 3.27 | 3.56 | 0.04 | 0.777 | 0.32 | 0.039 |
| Control | 3.01 (0.97) | 3.23 | 3.24 | ||||
| Goal-setting for PA (range: 5–25) | |||||||
| Intervention | 12.9 (4.38) | 13.8 | 14.4 | 0.86 | 0.066 | 1.15 | 0.021 |
| Control | 12.7 (4.20) | 13.0 | 13.3 | ||||
| Self-efficacy: PA (range: 6–30) | |||||||
| Intervention | 18.1 (5.76) | 19.0 | 19.4 | 0.67 | 0.228 | 2.02 | 0.003 |
| Control | 18.0 (5.64) | 18.4 | 17.4 | ||||
| SEDENTARY ACTIVITY | |||||||
| Sedentary activity | |||||||
| (30-minute blocks/day) | |||||||
| Intervention | 31.0 (3.82) | 32.1 | 31.0 | –0.12 | 0.834 | –1.26 | 0.050 |
| Control | 31.4 (3.89) | 32.2 | 32.3 | ||||
| TV (30-minute blocks/day) | |||||||
| Intervention | 2.78 (2.80) | 2.90 | 2.29 | 0.51 | 0.158 | –0.05 | 0.883 |
| Control | 2.44 (2.66) | 2.39 | 2.34 | ||||
| Stage of change: TV (range: 1–5) | |||||||
| Intervention | 2.74 (1.35) | 2.72 | 2.95 | –0.18 | 0.226 | –0.02 | 0.905 |
| Control | 2.61 (1.30) | 2.90 | 2.97 | ||||
| DIETARY INTAKE | |||||||
| Fruits/vegetables (servings/day) | |||||||
| Intervention | 1.96 (2.18) | — | 2.06 | — | — | 0.24 | 0.365 |
| Control | 1.60 (1.76) | — | 1.82 | ||||
| Sugar-sweetened beverages | |||||||
| (servings/day) | |||||||
| Intervention | 1.33 (1.65) | — | 1.25 | — | — | –0.05 | 0.751 |
| Control | 1.04 (1.31) | — | 1.30 | ||||
| Stage of Change: | |||||||
| Fruits/vegetables (range: 1–5) | |||||||
| Intervention | 2.96 (1.08) | 3.14 | 3.34 | 0.13 | 0.276 | 0.28 | 0.033 |
| Control | 2.91 (1.11) | 3.01 | 3.06 | ||||
| Goal-setting for healthy eating | |||||||
| (range: 4–20) | |||||||
| Intervention | 10.5 (3.54) | 11.8 | 12.5 | 0.91 | 0.028 | 1.57 | 0.002 |
| Control | 10.7 (3.79) | 10.9 | 10.9 | ||||
| EATING PATTERNS | |||||||
| Breakfast (days/week) | |||||||
| Intervention | 3.29 (2.65) | 4.13 | 4.69 | 0.26 | 0.401 | 0.61 | 0.067 |
| Control | 3.55 (2.55) | 3.88 | 4.08 | ||||
| Portion control (range: 4–16) | |||||||
| Intervention | 8.16 (2.83) | 9.04 | 9.55 | 0.81 | 0.041 | 1.03 | 0.014 |
| Control | 8.34 (3.05) | 8.23 | 8.52 | ||||
| Stage of change: | |||||||
| breakfast (range: 1–5) | |||||||
| Intervention | 3.16 (1.21) | 3.49 | 3.78 | 0.11 | 0.387 | 0.32 | 0.028 |
| Control | 3.24 (1.17) | 3.37 | 3.46 | ||||
| Stage of change: | |||||||
| portion control (range: 1–5) | |||||||
| Intervention | 2.77 (1.23) | 3.02 | 3.31 | 0.23 | 0.197 | 0.56 | 0.006 |
| Control | 2.73 (1.11) | 2.80 | 2.75 | ||||
| UNHEALTHY WEIGHT CONTROL BEHAVIORS | |||||||
| Unhealthy weight control behaviors (%) | |||||||
| Intervention | 66.4 (0.48) | 56.6 | 49.5 | –9.57 | 0.083 | –13.7 | 0.021 |
| Control | 71.1 (0.45) | 66.2 | 63.3 | ||||
| Binge eating (%) | |||||||
| Intervention | 11.1 (0.31) | 6.00 | 6.04 | –5.41 | 0.120 | –3.93 | 0.250 |
| Control | 15.3 (0.37) | 11.4 | 10.0 | ||||
| BODY AND SELF IMAGE | |||||||
| Body satisfaction (range: 10–60) | |||||||
| Intervention | 37.4 (12.8) | 39.8 | 40.7 | 3.18 | 0.094 | 3.95 | 0.045 |
| Control | 34.9 (12.4) | 36.6 | 36.7 | ||||
| Harter athletic competence | |||||||
| (range: 5–20) | |||||||
| Intervention | 11.7 (3.02) | 12.4 | 12.8 | 0.70 | 0.085 | 0.86 | 0.044 |
| Control | 11.7 (2.90) | 11.7 | 11.9 | ||||
| Harter appearance (range: 5–20) | |||||||
| Intervention | 13.6 (4.06) | 14.1 | 14.4 | 1.10 | 0.063 | 1.06 | 0.071 |
| Control | 12.6 (3.83) | 13.0 | 13.4 | ||||
| Harter self worth (range: 5–20) | |||||||
| Intervention | 15.1 (3.51) | 15.3 | 15.5 | 0.90 | 0.024 | 0.85 | 0.031 |
| Control | 14.6 (3.29) | 14.4 | 14.7 | ||||
n = 182 girls in the intervention condition and 174 girls in the control condition, although numbers may vary for individual analyses due to missing values.
Baseline means are adjusted for age, race, and school as a random effect.
Post-class and follow-up means are adjusted for baseline value of the outcome in addition to age, race, and school as a random effect.
Intervention effects are estimates that represent the difference in the outcome variable at post-class or follow-up in intervention condition compared to control condition, adjusted for age, race, and school as a random effect in addition to baseline value of the outcome. P-values are calculated from the associated t-statistic having 10 df.
Percent body fat was measured with dual-energy x-ray absorptiometry (DXA).
At follow-up, intervention girls increased their stage of change for physical activity (p=.039), physical activity goal-setting behaviors (p=.021) and their self-efficacy to overcome barriers to physical activity (p=.003), as compared to control girls. Based on the 3-DPAR, which assesses activity in 30-minute blocks throughout the day (e.g., main activity done between 5:00 and 5:30), total sedentary activity decreased by 1.26 blocks a day among the intervention girls as compared to the control girls at follow-up (p=.050).
Improvements were seen for dietary goal-setting (p=.002) and for stage of change for fruit and vegetable intake (p=.002) among intervention girls as compared to control girls. Additionally, at follow-up, intervention girls advanced in their stage of change toward regular breakfast eating (p=.028). Intervention girls also showed increases in portion control behaviors (p=.014) and for stage of change for portion control (p=.006).
As noted above, progression forward in stage of change (e.g., from precontemplation to contemplation) was found for a number of physical activity and dietary behaviors. Baseline-adjusted mean stage of change scores at follow-up averaged about 0.3 higher in the intervention girls than in the control girls. This corresponds to about 13% more intervention girls progressing in stage of change and about 3% fewer intervention girls regressing in their stage of change, as compared to control girls.
At follow-up, the percentage of intervention girls engaging in unhealthy weight control behaviors decreased by 13.7% (p=.021) as compared to control girls. Additionally, intervention girls showed significant improvements in body satisfaction (p=.045), perceived athletic competence (p=.044), and self-worth (.031) as compared to control girls.
Support from friends, teachers, and parents
Differences in perceived support for physical activity and healthy eating from friends, teachers, and parents were explored, given the strong emphasis placed on providing a supportive environment for the girls. At follow-up, intervention reported significantly more support for physical activity from friends, teachers, and family members than control girls (Table 3). For healthy eating, significant increases were found for friend and teacher support, but not for parent support.
Table 3.
Support for physical activity and healthy eating: Means and intervention effect estimatesb
| M | Test of intervention effect | ||||||
|---|---|---|---|---|---|---|---|
| Baselineb | Post-Classc | Follow-upc | Post-Classd | Follow-upd | |||
| M (SD) | M | M | Intervention Effect |
p-value | Intervention Effect |
p-value | |
| SUPPORT FOR PHYSICAL ACTIVITY (PA) | |||||||
| Friend support: PA (range: 1–4) | |||||||
| Intervention | 2.37 (0.96) | 2.38 | 2.55 | 0.10 | 0.376 | 0.25 | 0.045 |
| Control | 2.25 (0.98) | 2.29 | 2.30 | ||||
| Teacher support: PA (range: 1–4) | |||||||
| Intervention | 2.55 (0.76) | 2.78 | 2.74 | 0.19 | 0.098 | 0.26 | 0.034 |
| Control | 2.47 (0.85) | 2.59 | 2.48 | ||||
| Family support: PA (range: 5–25) | |||||||
| Intervention | 13.2 (4.91) | 13.2 | 14.1 | 0.54 | 0.284 | 1.38 | 0.016 |
| Control | 13.0 (4.74) | 12.7 | 12.7 | ||||
| SUPPORT FOR HEALTHY EATING | |||||||
| Friend support: | |||||||
| healthy eating (range: 1–4) | |||||||
| Intervention | 2.05 (0.95) | 2.34 | 2.44 | 0.22 | 0.109 | 0.36 | 0.018 |
| Control | 2.08 (1.03) | 2.12 | 2.09 | ||||
| Teacher support: | |||||||
| healthy eating (range: 1–4) | |||||||
| Intervention | 2.55 (0.80) | 2.83 | 2.81 | 0.21 | 0.083 | 0.25 | 0.044 |
| Control | 2.52 (0.86) | 2.62 | 2.55 | ||||
| Parent support: | |||||||
| healthy eating (range: 2–8) | |||||||
| Intervention | 2.64 (0.91) | 2.83 | 2.84 | 0.06 | 0.493 | 0.13 | 0.198 |
| Control | 2.77 (0.94) | 2.76 | 2.71 | ||||
n = 182 girls in the intervention condition and 174 girls in the control condition, although numbers may vary for individual analyses due to missing values.
Baseline means are adjusted for age, race, and school as a random effect.
Post-class and follow-up means are adjusted for baseline value of the outcome in addition to age, race, and school as a random effect.
Intervention effects are estimates that represent the difference in the outcome variable at post-class or follow-up in intervention condition compared to control condition, adjusted for age, race, and school as a random effect in addition to baseline value of the outcome. P-values are calculated from the associated t-statistic having 10 df.
Program satisfaction
Among intervention girls who completed process evaluation surveys at follow-up (n=175 of 182), 98% indicated that they were satisfied (24%) or very satisfied (74%) with the program and 100% said they would recommend New Moves to a friend. Among parents completing process evaluation surveys (n=116), 91% were satisfied (38%) or very satisfied (53%) with the program and 100% said they would recommend New Moves for other girls.
DISCUSSION
New Moves was designed to prevent a broad range of weight-related problems in adolescent girls. The intervention did not lead to significant changes in the girls’ percent body fat or BMI, but improvements were seen within the domains of sedentary activity, physical activity (stage of change, goal-setting, and self-efficacy), dietary intake (stage of change and goal-setting), eating patterns (portion control behaviors and stage of change for breakfast eating), unhealthy weight control behaviors, and body/self image. Additionally, intervention girls reported that they felt more support for being physically active from friends, teachers, and family members and more support for healthy eating by friends and teachers. Finally, the vast majority of the girls and their parents indicated high levels of satisfaction with New Moves and 100% said they would recommend the program to others.
School-based obesity prevention programs have had limited success in changing weight status, with greater success in changing weight-related knowledge, attitudes, and behaviors. 55–61 Similarly, in the current study, no change was seen in weight status, but changes were seen in attitudes and behaviors. A large focus of New Moves was on goal-setting, and notable increases were found in goal-setting for both physical activity and eating behaviors. The decrease in sedentary behaviors of approximately 30 minutes/day among intervention girls was a positive change. Additionally, while control girls tended to decrease their physical activity, levels remained fairly constant in the intervention girls. Intervention girls advanced in their stage of change for breakfast eating, which is important given that breakfast has been found to be protective for excessive weight gain.62, 63 Given the large portion sizes of food to which young people are exposed 64, 65; the changes found in portion control behaviors among intervention girls were positive.
Girls participating in New Moves decreased their use of unhealthy weight control behaviors and had improved body image and self-worth. Given that unhealthy weight control behaviors predict excessive weight gain, extreme weight control behaviors, and binge eating among adolescents 66; the decrease in unhealthy weight control behaviors may help in preventing future weight gain and risk for eating disorders. Similar to findings described in the obesity prevention literature, interventions aimed at preventing risk factors for eating disorders have shown mixed results. In a meta-analytic review of eating disorder prevention programs, 51% of the programs reduced risk factors for eating disorders, such as dieting and body dissatisfaction.67 Thus, although New Moves addressed a broader range of weight-related outcomes than most eating disorder prevention programs, it compared favorably in terms of its impact on risk factors for eating disorders. Of note, binge eating was not targeted as one of the key objectives in New Moves and differences were not found between the two conditions. Given its relevance for both obesity and eating disorders 5, 68, 69 and the girls’ discussions of emotional eating, it is suggested that future interventions target binge eating.
Study strengths and limitations need to be taken into account in interpreting the findings. The diverse nature of the participants, drawn from schools serving high percentages of low-income youth, with over 75% of the girls from racial/ethnic minorities, is a study strength, as it is crucial to find ways to meet the needs of these girls. The implementation of New Moves within a school setting makes the program accessible to all students; however, there are difficulties inherent to involving parents and helping youth make changes in their eating and activity behaviors within a school setting. For example, only one fifth of parents attended the parent–daughter retreat day. The high level of response (94% at follow-up) and the strong evaluation tools are study strengths, although 26% of the girls were missing DXA assessments of body composition at either baseline or follow-up assessments, primarily due to concerns about doing a required urine test and logistic difficulties in getting to the clinic (e.g., moved, did not want to miss class).
The use of a control group that received an all-girls physical education class allowed for the recruitment of similar girls into both conditions and an examination of the effect of New Moves activities above and beyond the all-girls physical education class. However, in examining the findings it is important to note that the control group also received an intervention (i.e., an all-girls class composed of girls with sedentary lifestyles). Some studies have found that all-girls physical education classes provide a more positive learning experience than coeducational classes and lead to more active participation of girls.70, 71 The control girls’ participation in a physical education class during the intervention period may explain the larger differences found at follow-up than at post-class, particularly with regard to physical activity outcomes and measures of a supportive environment. The intervention effect may have been larger had it also been possible to evaluate the impact of an all-girls physical activity environment. Additionally, given the program’s focus on long-term behavioral change, and trends toward improvements in outcomes from post-class to follow-up assessments in intervention girls as compared to control girls, a longer follow-up period may have revealed further differences between the groups.
CONCLUSION
Findings indicate very high levels of satisfaction with the program among girls and their parents. New Moves appears to fill a niche within schools by meeting the needs of girls who are not comfortable in regular physical education classes, have sedentary lifestyles, and are at risk for weight-related problems. 9 New Moves was effective in improving key weight-related attitudes and behaviors. However, in order to lead to changes in weight status, it may be necessary to integrate New Moves into more comprehensive school-based interventions 72–74 that involve ongoing educational efforts, changes in the school food and physical activity environments, and more intensive parent and community outreach activities.
Supplementary Material
Acknowledgments
“New Moves: Obesity prevention among adolescent girls” (Clinical Trials number: NCT00250497) was supported by Grant R01 DK063107 (D. Neumark-Sztainer, principal investigator) from the National Institute of Diabetes and Digestive and Kidney Diseases, NIH. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Kidney Diseases or the NIH. Research was supported in part by grant M01-RR00400 from the National Center for Research Resources, the NIH.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
No financial disclosures were reported by the authors of this paper.
References
- 1.Kimm SY, Glynn NW, Kriska AM, Barton BA, Kronsberg SS, Daniels SR, et al. Decline in physical activity in black girls and white girls during adolescence. N Engl J Med. 2002;347(10):709–715. doi: 10.1056/NEJMoa003277. [DOI] [PubMed] [Google Scholar]
- 2.Neumark-Sztainer D, Story M, Hannan PJ, Perry CL, Irving LM. Weight-related concerns and behaviors among overweight and non-overweight adolescents: Implications for preventing weight-related disorders. Arch Pediatr Adolesc Med. 2002;156(2):171–178. doi: 10.1001/archpedi.156.2.171. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among U.S. children and adolescents, 2003–2006. JAMA. 2008;299(20):2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 4.Sherwood NE, Wall M, Neumark-Sztainer D, Story M. Effect of socioeconomic status on weight change patterns in adolescents. Prev Chronic Dis. 2009;6(1) [PMC free article] [PubMed] [Google Scholar]
- 5.Haines J, Neumark-Sztainer D, Wall M, Story M. Personal, behavioral, and environmental risk and protective factors for adolescent overweight. Obes Res. 2007;15:2748–2760. doi: 10.1038/oby.2007.327. [DOI] [PubMed] [Google Scholar]
- 6.van den Berg P, Neumark-Sztainer D. Fat 'n happy 5 years later: Is it bad for overweight girls to like their bodies? J Adolesc Health. 2007;41:415–417. doi: 10.1016/j.jadohealth.2007.06.001. [DOI] [PubMed] [Google Scholar]
- 7.Neumark-Sztainer D, Flattum CF, Story M, Feldman S, Petrich CA. Dietary approaches to healthy weight management for adolescents: The New Moves model. Adolesc Med. 2008;19(3):421–430. [PMC free article] [PubMed] [Google Scholar]
- 8.Flattum C, Friend S, Neumark-Sztainer D, Story M. Motivational interviewing as a component of a school-based obesity prevention program for adolescent girls. J Am Diet Assoc. 2009;109(1):91–94. doi: 10.1016/j.jada.2008.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Neumark-Sztainer D, Story M, Hannan PJ, Rex J. New Moves: A school-based obesity prevention program for adolescent girls. Prev Med. 2003;37:41–51. doi: 10.1016/s0091-7435(03)00057-4. [DOI] [PubMed] [Google Scholar]
- 10.Neumark-Sztainer D, Flattum C, Feldman S, Petrich C. Striving to prevent obesity and other weight-related problems in adolescent girls: The New Moves approach. In: O'Dea JA, Eriksen M, editors. Childhood Obesity Prevention—International Research, Controversies, and Interventions. Oxford University Press; In Press. [Google Scholar]
- 11.Neumark-Sztainer D. Can we simultaneously work toward the prevention of obesity and eating disorders in children and adolescents. Int J Eat Disord. 2005;38:220–227. doi: 10.1002/eat.20181. [DOI] [PubMed] [Google Scholar]
- 12.Neumark-Sztainer D. The interface between the eating disorders and obesity fields: Moving toward a model of shared knowledge and collaboration. Eat Weight Disord. 2009;14(1):51–58. doi: 10.1007/BF03327795. [DOI] [PubMed] [Google Scholar]
- 13.Irving LM, Neumark-Sztainer D. Integrating primary prevention of eating disorders and obesity: Feasible or futile? Prev Med. 2002;34(3):299–309. doi: 10.1006/pmed.2001.0997. [DOI] [PubMed] [Google Scholar]
- 14.Neumark-Sztainer D, Paxton SJ, Hannan PJ, Haines J, Story M. Does body satisfaction matter? Five-year longitudinal associations between body satisfaction and health behaviors in adolescent females and males. J Adolesc Health. 2006;39:244–251. doi: 10.1016/j.jadohealth.2005.12.001. [DOI] [PubMed] [Google Scholar]
- 15.Neumark-Sztainer D, Story M. Recommendations from overweight youth regarding school-based weight control programs. J Sch Health. 1997;67(10):428–433. doi: 10.1111/j.1746-1561.1997.tb01289.x. [DOI] [PubMed] [Google Scholar]
- 16.Neumark-Sztainer D, Story M, Faibisch L. Perceived stigmatization among overweight African American and Caucasian adolescent girls. J Adolesc Health. 1998;23(5):264–270. doi: 10.1016/s1054-139x(98)00044-5. [DOI] [PubMed] [Google Scholar]
- 17.Neumark-Sztainer D, Story M, Faibisch L, Ohlson J, Adamiak M. Issues of self-image among overweight African American and Caucasian adolescent girls: A qualitative study. J Nutr Educ. 1999;31(6):311–320. [Google Scholar]
- 18.Neumark-Sztainer D, Martin SL, Story M. School-based programs for obesity prevention: What do adolescents recommend? Am J Health Promot. 2000;14(4):232–235. doi: 10.4278/0890-1171-14.4.232. [DOI] [PubMed] [Google Scholar]
- 19.Neumark-Sztainer D, Story M. Dieting and binge eating among adolescents: What do they really mean? J Am Diet Assoc. 1998;98(4):446–450. doi: 10.1016/S0002-8223(98)00101-1. [DOI] [PubMed] [Google Scholar]
- 20.Neumark-Sztainer D, Story M, Coller T. Perceptions of secondary school staff toward the implementation of school-based activities to prevent weight-related disorders: A needs assessment. Am J Health Promot. 1999;13(3):153–156. doi: 10.4278/0890-1171-13.3.153. [DOI] [PubMed] [Google Scholar]
- 21.Neumark-Sztainer D, Harris T, Story M. Beliefs and attitudes about obesity among teachers and school health care providers working with adolescents. J Nutr Educ. 1999;31:3–9. [Google Scholar]
- 22.Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall, Inc.; 1986. [Google Scholar]
- 23.Baranowski T, Perry CL, Parcel GS. How individuals, environments, and health behavior interact: Social Cognitive Theory. In: Glanz K, Rimer BK, Lewis MF, editors. Health Behavior and Health Education: Theory Research and Practice. San Francisco, CA: Jossey-Bass; 2002. pp. 165–184. [Google Scholar]
- 24.Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51(3):390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- 25.Di Noia J, Prochaska JO. Mediating Variables in a Transtheoretical Model Dietary Intervention Program. Health Educ Behav. 2009 doi: 10.1177/1090198109334897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Prochaska JO, Velicer WF. The Transtheoretical Model of Health Behavior Change. Am J Health Promot. 1997;12(1):38–48. doi: 10.4278/0890-1171-12.1.38. [DOI] [PubMed] [Google Scholar]
- 27.Resnicow K, Davis R, Rollnick S. Motivational interviewing for pediatric obesity: Conceptual issues and evidence review. J Am Diet Assoc. 2006;106(12):2024–2033. doi: 10.1016/j.jada.2006.09.015. [DOI] [PubMed] [Google Scholar]
- 28.Miller WR, Rollnick S. Motivational interviewing: Preparing people to change addictive behavior. New York: Guilford Press; 1991. [Google Scholar]
- 29.Channon S, Smith VJ, Gregory JW. A pilot study of motivational interviewing in adolescents with diabetes. Arch Dis Child. 2003;88(8):680–683. doi: 10.1136/adc.88.8.680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007;(120 Suppl 4):S193–S228. doi: 10.1542/peds.2007-2329D. [DOI] [PubMed] [Google Scholar]
- 31.Kuczmarski RJ, Ogden CL, Grummer-Strawn LM, Flegal KM, Guo SS, Wei R, et al. CDC Growth Charts: U.S. Adv Data. 2000;314:1–27. [PubMed] [Google Scholar]
- 32.Pate RR, Ross R, Dowda M, Trost SG, Sirard JR. Validation of a three-day physical activity recall instrument in female youth. Pediatric Exercise Science. 2003;15:257–265. [Google Scholar]
- 33.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(9 Suppl):S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 34.Ainsworth BE, Haskell WL, Leon AS, Jacobs DR, Jr, Montoye HJ, Sallis JF, et al. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993;25(1):71–80. doi: 10.1249/00005768-199301000-00011. [DOI] [PubMed] [Google Scholar]
- 35.Pate RR, Dowda M, O'Neill JR, Ward DS. Change in physical activity participation among adolescent girls from 8th to 12th grade. Journal of Physical Activity and Health. 2007;4(1):3–16. doi: 10.1123/jpah.4.1.3. [DOI] [PubMed] [Google Scholar]
- 36.McMurray RG, Ring KB, Treuth MS, Welk GJ, Pate RR, Schmitz KH, et al. Comparison of two approaches to structured physical activity surveys for adolescents. Med Sci Sports Exerc. 2004;36(12):2135–2143. doi: 10.1249/01.mss.0000147628.78551.3b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Marcus BH, Selby VC, Niaura RS, Rossi JS. Self-efficacy and the stages of exercise behavior change. Research Quarterly for Exercise and Sports. 1992;63(1):60–66. doi: 10.1080/02701367.1992.10607557. [DOI] [PubMed] [Google Scholar]
- 38.Saelens B, Gehrman C, Sallis J, Calfas K, Sarkin J, Caparosa S. Use of self-management strategies in a 2-year cognitive-behavioral intervention to promote physical activity. Behavior Therapy. 2000;31:365–379. [Google Scholar]
- 39.Neumark-Sztainer D, Story M, Hannan PJ, Tharp T, Rex J. Factors associated with changes in physical activity: A cohort study of inactive adolescent girls. Arch Pediatr Adolesc Med. 2003;157:803–810. doi: 10.1001/archpedi.157.8.803. [DOI] [PubMed] [Google Scholar]
- 40.Dowda M, Pate RR, Felton GM, Saunders R, Ward DS, Dishman RK, et al. Physical activities and sedentary pursuits in African American and Caucasian girls. Research Quarterly in Exercise and Sport. 2004;75(4):352–360. doi: 10.1080/02701367.2004.10609168. [DOI] [PubMed] [Google Scholar]
- 41.Dowda M, Saunders RP, Hastings L, Gay JM, Evans AE. Physical activity and sedentary pursuits of children living in residential children's homes. Journal of Physical Activity and Health. 2009;6(2):195–202. doi: 10.1123/jpah.6.2.195. [DOI] [PubMed] [Google Scholar]
- 42.McPherson RS, Hoelscher DM, Alexander M, Scanlon KS, Serdula MK. Dietary assessment methods among school-aged children: Validity and reliability. Prev Med. 2000;31:S11–S33. [Google Scholar]
- 43.Neumark-Sztainer D, Wall MM, Hannan PJ, Story M, Croll J, Perry C. Correlates of fruit and vegetable intake among adolescents: Findings from Project EAT. Prev Med. 2003;37(3):198–208. doi: 10.1016/s0091-7435(03)00114-2. [DOI] [PubMed] [Google Scholar]
- 44.Cusatis DC, Shannon BM. Influences on adolescent eating behavior. J Adolesc Health. 1996;18(1):27–34. doi: 10.1016/1054-139X(95)00125-C. [DOI] [PubMed] [Google Scholar]
- 45.Neumark-Sztainer D, Croll J, Story M, Hannan PJ, French S, Perry C. Ethnic/racial differences in weight-related concerns and behaviors among adolescent girls and boys: Findings from Project EAT. J Psychosom Res. 2002;53:963–974. doi: 10.1016/s0022-3999(02)00486-5. [DOI] [PubMed] [Google Scholar]
- 46.Neumark-Sztainer D, Wall M, Story M, Fulkerson JA. Are family meal patterns associated with disordered eating behaviors among adolescents? J Adolesc Health. 2004;35(5):350–359. doi: 10.1016/j.jadohealth.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 47.Yanovski SZ. Binge eating disorder: Current knowledge and future directions. Obes Res. 1993;1(4):306–324. doi: 10.1002/j.1550-8528.1993.tb00626.x. [DOI] [PubMed] [Google Scholar]
- 48.Harter S. Manual for the Self-Perception Profile for Adolescents. Denver: University of Denver; 1988. [Google Scholar]
- 49.Pingitore R, Spring B, Garfield D. Gender differences in body satisfaction. Obes Res. 1997;5(5):402–409. doi: 10.1002/j.1550-8528.1997.tb00662.x. [DOI] [PubMed] [Google Scholar]
- 50.Secord PF, Jourard SM. The appraisal of body-cathexis: body cathexis and the self. J Consult Clin Psychol. 1953;17(5):343–347. doi: 10.1037/h0060689. [DOI] [PubMed] [Google Scholar]
- 51.Prochaska JJ, Rodgers MW, Sallis JF. Association of parent and peer support with adolescent physical activity. Research Quarterly in Exercise and Sport. 2002;73(2):206–210. doi: 10.1080/02701367.2002.10609010. [DOI] [PubMed] [Google Scholar]
- 52.Webber LS, Catellier DJ, Lytle LA, Murray DM, Pratt CA, Young DR, et al. Promoting physical activity in middle school girls: Trial of Activity for Adolescent Girls. Am J Prev Med. 2008;34(3):173–184. doi: 10.1016/j.amepre.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Murray DM. The Design and Analysis of Group-Randomized Trials. New York: Oxford University Press; 1998. [Google Scholar]
- 54.Hannan P, Murray D. Gauss or Bernoulli: A Monte Carlo comparison of the performance of the linear mixed model and the logistic mixed model analyses in simulated community trials with a dichotomous outcome variable at the individual level. Education Review. 1996;20(3):338–352. doi: 10.1177/0193841X9602000306. [DOI] [PubMed] [Google Scholar]
- 55.Baranowski T, Cullen KW, Nicklas T, Thompson D, Baranowski J. School-based obesity prevention: a blueprint for taming the epidemic. Am J Health Behav. 2002;26(6):486–493. doi: 10.5993/ajhb.26.6.9. [DOI] [PubMed] [Google Scholar]
- 56.Summerbell C, Waters E, Edmunds L, Kelly S, Brown T, Campbell K. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 2005;((3)):CD001871. doi: 10.1002/14651858.CD001871.pub2. [DOI] [PubMed] [Google Scholar]
- 57.Stice E, Shaw H, Marti CN. A meta-analytic review of obesity prevention programs for children and adolescents: The skinny on interventions that work. Psychol Bull. 2006;132(5):667–691. doi: 10.1037/0033-2909.132.5.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Harris KC, Kuramoto LK, Schulzer M, Retallack JE. Effect of school-based physical activity interventions on body mass index in children: A meta-analysis. CMAJ. 2009;180(7):719–726. doi: 10.1503/cmaj.080966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kropski JA, Keckley PH, Jensen GL. School-based obesity prevention programs: An evidence-based review. Obesity. 2008;16(5):1009–1018. doi: 10.1038/oby.2008.29. [DOI] [PubMed] [Google Scholar]
- 60.Sharma M. School-based interventions for childhood and adolescent obesity. Obesity Reviews. 2006;7(3):261–269. doi: 10.1111/j.1467-789X.2006.00227.x. [DOI] [PubMed] [Google Scholar]
- 61.Gonzalez-Suarez C, Worley A, Grimmer-Somers K, Dones V. School-based interventions on childhood obesity: A meta-analysis. Am J Prev Med. 2009;37(5):418–427. doi: 10.1016/j.amepre.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 62.Timlin M, Pereira MA, Story M, Neumark-Sztainer D. Breakfast eating and weight change in a 5-year prospective analysis of adolescents: Project EAT (Eating Among Teens) Pediatrics. 2008;121(3):e638–e645. doi: 10.1542/peds.2007-1035. [DOI] [PubMed] [Google Scholar]
- 63.Barton BA, Eldridge AL, Thompson D, Affenito SG, Striegel-Moore RH, Franko DL, et al. The relationship of breakfast and cereal consumption to nutrient intake and body mass index: The National Heart, Lung, and Blood Institute Growth and Health Study. J Am Diet Assoc. 2005;105(9):1383–1389. doi: 10.1016/j.jada.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 64.Young LR, Nestle M. The contribution of expanding portion sizes to the U.S. obesity epidemic. Am J Public Health. 2002;92(2):246–249. doi: 10.2105/ajph.92.2.246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.French SA, Story M, Jeffrey RW. Environmental influences on eating and physical activity. Annu Rev Public Health. 2001;22:309–335. doi: 10.1146/annurev.publhealth.22.1.309. [DOI] [PubMed] [Google Scholar]
- 66.Neumark-Sztainer D, Wall M, Guo J, Story M, Haines J, Eisenberg M. Obesity, disordered eating, and eating disorders in a longitudinal study of adolescents: How do dieters fare five years later? J Am Diet Assoc. 2006;106:559–568. doi: 10.1016/j.jada.2006.01.003. [DOI] [PubMed] [Google Scholar]
- 67.Stice E, Shaw H, Marti CN. A meta-analytic review of eating disorder prevention programs: Encouraging findings. Annual Review of Clinical Psychology. 2007;3:207–231. doi: 10.1146/annurev.clinpsy.3.022806.091447. [DOI] [PubMed] [Google Scholar]
- 68.Stice E, Presnell K, Spangler D. Risk factors for binge eating onset in adolescent girls: A 2-year prospective investigation. Health Psychol. 2002;21(2):131–138. [PubMed] [Google Scholar]
- 69.Tanofsky-Kraff M, Yanovski SZ, Wilfley DE, Marmarosh C, Morgan CM, Yanovski JA. Eating-disordered behaviors, body fat, and psychopathology in overweight and normal-weight children. J Consult Clin Psychol. 2004;72(1):53–61. doi: 10.1037/0022-006X.72.1.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Derry JA, Phillips DA. Comparisons of selected student and teacher variables in all-girls and coeducational phsyical education environments. Physical Educator. 2004;61(1):23–34. [Google Scholar]
- 71.Hannon JC, Ratliffe T. Opportunities to participate and teacher interactions in coed versus single-gender physical education settings. Physical Educator. 2007;64(1):11–21. [Google Scholar]
- 72.O'Dea J, Maloney D. Preventing eating and body image problems in children and adolescents using the Health Promoting Schools Framework. J Sch Health. 2000;70(1):18–21. doi: 10.1111/j.1746-1561.2000.tb06441.x. [DOI] [PubMed] [Google Scholar]
- 73.Story M. School-based approaches for preventing and treating obesity. Int J Obes Relat Metab Disord. 1999;23 Suppl 2:S43–S51. doi: 10.1038/sj.ijo.0800859. Review. [DOI] [PubMed] [Google Scholar]
- 74.Neumark-Sztainer D. School-based programs for preventing eating disturbances. J Sch Health. 1996;66(2):64–71. doi: 10.1111/j.1746-1561.1996.tb07912.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.